Abstract
Purpose:
The purpose of the present study was to investigate the effect of the different irrigant combinations used in final irrigation on the push-out bond strength of root canal sealers that have different compositions.
Materials and methods:
In total 60 dentinal slices in 1 mm thickness were collected from 15 extracted mandibular premolar teeth; 4 slices from each tooth. 3 canal-like artificial cavities were opened on each dentinal slice. Samples were divided into 4 experimental groups, each of which consisted of 15 samples. In group 1, samples were immersed in 5.25% NaOCl and 17% EDTA solutions respectively; in group 2, immersed in 5.25% NaOCl and 2% CHX solutions respectively; in group 3, immersed in 5.25% NaOCl, 17% EDTA and 2% CHX solutions respectively; and in group 4 immersed in distilled water. After drying with absorbent papers, each cavity in dentinal slice sample was filled with different sealer (Endoseal MTA, Tech Biosealer Endo or AH Plus). Two days later, the push-out bond examination was performed.
Results:
AH Plus showed higher push-out bond strength value in two combinations (group 2 and 3) in which final irrigants contained CHX (p<0.001). Dentinal push-out bond strengths of root canal sealers from Endoseal MTA and Tech BioSealer Endo were not affected by final irrigant (p=0.965).
Conclusion:
Using CHX after NaOCl in final irrigant increases push-out strength of epoxy resinbased sealer but, did not create any difference in dentinal push-out bond strength of calcium silicate-based sealers.
Keywords: Calcium silicate-based sealer, chlorhexidine gluconate, precipitate, pushout bond strength, root canal irrigants
Introduction
It is widely accepted thaat there is a positive correlation between the outcome of endodontic treatment and the technical quality of the root canal sealing (1, 2). One of the main aims of root canal filling is to seal the prepared canal to prevent the tissue fluids, bacteria and/or bacterial products to enter into it (3). In order to achieve this aim in root canal filling procedure, it is critical that the sealer used with gutta-percha provides an optimum adhesion to root canal walls (4, 5).
Final irrigation of the root canal is performed after root canal shaping in order to reduce the pre-obturation microbial load within the canal system and to minimize future failure (6). Successive administration of sodium hypochlorite (NaOCl) solution and ethylenediaminetetraacetic acid (EDTA) is the most common final irrigation method used all around the world in order to ensure the chemical debridement of root canals and to remove the smear layer take place on dentinal surfaces after the instrumentation (7, 8). On the other hand, it was claimed that it is not expected to see a positive therapeutic effect of NaOCl solution while there is EDTA in the canal (9). Besides the high concentrations of NaOCl is toxic and can irritate the periapical tissues (10). Therefore, chlorhexidine gluconate (CHX) was suggested as an alternative irrigant solution for NaOCl (11). Even though CHX has substantivity property along with antimicrobial activity, it does not have the capability of dissolving vital or necrotic tissues (12). In fact, an irrigant with all the desired physiochemical and ideal microbiological properties has yet to be introduced (13, 14). Therefore, different irrigation solutions that have positive effects on antimicrobial properties of NaOCl can be used after NaOCl for effective irrigation ((13, 15). However, it is important to be aware of the possibility that irrigation solutions used successively can chemically react with each other. For example, a mixture of NaOCl and CHX produces an orange-brown, hard-to-remove precipitate that colors the walls of the pulpal cavity (16). Previous researches reported that this precipitate contains para-chloroaniline (PCA), a toxin produces methemoglobin and has a potential carcinogenic effect in time (17, 18). However, recent studies that used advanced analysis techniques showed that the precipitate produced by a mixture of these solutions do not contain PCA (6, 19, 20).
There is a limited data on the effect of precipitates that accumulated in canal walls on the push-out bond strength of sealers to the canal walls. Graziele Magro et al. (14) reported that the produced precipitates after final irrigation, which used 2% CHX solutions with different formulas, did not change the push-out bond strength of AH Plus, an epoxy- based sealer. Neelakantan et al. (21) reported that using EDTA in final irrigation increased the adhesion force of AH Plus sealer to the root dentin significantly when it is compared with a final irrigation that used NaOCl.
Recently, a number of calcium-silicate based root canal sealers that have the positive attributes of bioceramic cement were introduced. Endoseal MTA and Tech Biosealer Endo are the two examples of these type of sealers. In literature, there is limited knowledge about whether final irrigants affects the push-out bond strength of calcium silicate-based sealers to root canal dentin. The purpose of the present study was to evaluate influence of NaOCl+EDTA, NaOCl+CHX or NaOCl+EDTA+CHX final irrigation regimens on the bond-strength of two calcium silicate based (Endoseal MTA and Tech Biosealer Endo) and one epoxy resin based (AH Plus) sealer. The null hypothesis is that the order of the irrigant solutions used in final irrigation does not affect the dentinal push-out bond strength of these root canal sealers.
Materials and methods
Ethical statement
This study was reviewed and approved by the Research Ethics Committee of Karadeniz Technical University (Protocol Number: 2021/75). The manufacturers and the material contents of root canal sealers tested in this study can be found in Table 1.
Table 1.
The ingredients and manufacturers of the tested materials.
| Sealer | Manufacturer | Composition |
|---|---|---|
| Endoseal MTA | Maruchi, Wonju, Korea | Calcium silicates, calcium aluminates, calcium aluminoferrite, calcium sulfates, radiopacifier, thickening agent |
| Tech BioSealer Endo | Isasan SRL, Revello Porro, Italy | Powder: White Portland cement, bismuth oxide, anhydride, sodium fluoride |
| Liquid: Alfacaine SP solution (4% articaine + 1/100.000 epinephrine | ||
| AH Plus | Dentsply DeTrey GmbH, Konstanz, Germany | Epoxy paste: diepoxy, calcium tungstate, zirconium oxide, aerosol, and dye |
| Amine paste: 1-adamantane amine, N.N'dibenzyl-5 oxanonandiamine-1,9, TCD-diamine, calcium tungstate, zirconium oxide, aerosol, and silicone oil |
Sample preparation
Samples were prepared by following the technique described by Scelza et al. (22). Newly extracted 15 mandibular premolars were chosen. Teeth were stored in 0.02% sodium azide solution at 4°C until the experiment. Soft tissue residuals on teeth were removed by using a scalpel and crowns were removed by using a low-speed diamond disc (Micracut 125; Metkon, Bursa, Turkey) under continuous water wash. The same low-speed diamond disc was used in order to create 4 horizontal cross-sections (1 ± 0.1 mm thick) in each root in coronal to apical direction. 60 root slices were obtained through this protocol. In each root slice, 1 mm thick cylindrical carbide bur was used in order to open three canal-like cavities parallel to the root canal (Figure 1).
Figure 1.
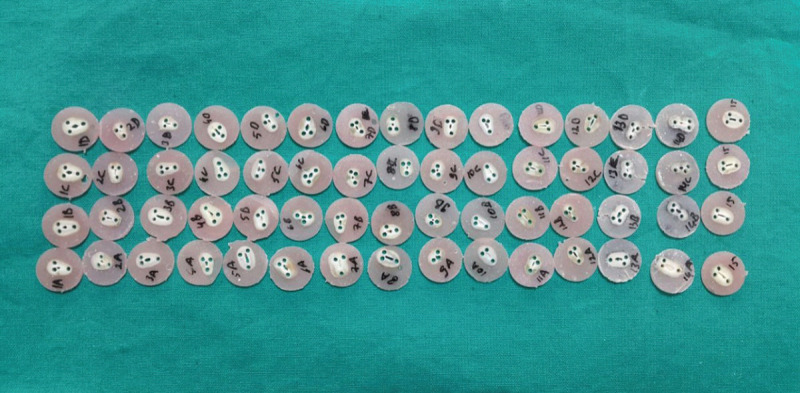
1.0 mm thick slices were obtained from the roots and three canal-like cavities were opened on each slice.
The cavities were opened perpendicular to the surface under continuous water wash. The cavities were preserved so as to the distance between the external cement and root canal wall to be 1 mm in minimum. All root slices were divided into 4 different experimental groups according to the final irrigant administration, so each group has 15 slices: Group-1; the samples were immersed in 5 mL 5.25% NaOCl (Wizard; Rehber Kimya, Istanbul, Turkey) for 15 minutes and then in 5 mL 17% EDTA (Wizard; Rehber Kimya, Istanbul, Turkey) for 3 minutes.Group-2; the samples were immersed in 5 mL 5.25% NaOCl for 15 minutes, then after drying with absorbent papers, they were immersed in 5 mL 2% CHX (Consepsis; Ultradent, South Jordan, UT, USA) for a minute. Group-3; the samples were immersed in 5 mL 5.25% NaOCl for 15 minutes and then in 5 mL 17% EDTA for 3 minutes. After drying with the absorbent paper, they were immersed in 5 mL 2% CHX for a minute. Group-4; the samples were immersed in 5 mL distilled water for 15 minutes.
Then the cavities were dried with absorbent papers and each of the cavities in each of the root slice was randomly filled with one of the chosen sealers: Endoseal MTA (Endoseal; Maruchi, Wonju, Korea), Tech Biosealer Endo (Isasan; Rovello Porro, Italy) or AH Plus (Dentsply DeTrey GmbH, Konstanz, Germany). All of the sealers were mixed and put in cavities according to the protocols provided by the manufacturers. In order to prevent the bubble formation, a weak vibration was applied while placing the sealers into cavities. Lastly, root slices filled with 3 different sealers was incubated at 37° C and 95% relative humidity for 48 hours before pushout analysis in order to harden them completely (Figure 2).
Figure 2.
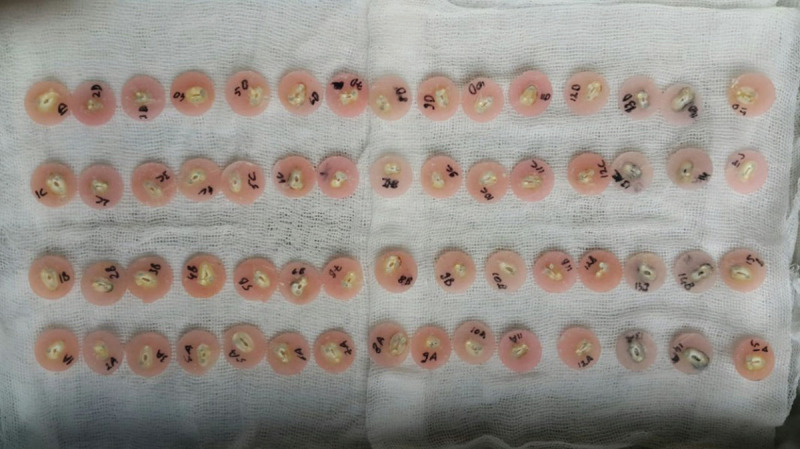
Each cavity in the dentinal slices was filled with a different sealer.
Push-out bond strength test
A plunger tip (0.8 mm in diameter) was placed in a way that it was on top of only the test material. The force was always applied in coronal-apical direction. Loading was performed on a universal testing machine (Lloyd Instruments, Foreham, UK) at 0.5 mm/min speed until material dislocation occurred (Figure 3). The load at failure was recorded (in Newtons) and the values were used to calculate the push-out strength in megapascals according to the formula used by Bitter et al. (23).
Figure 3.

Loading was performed on a universal testing machine at 0.5 mm/min speed until material dislocation occurred.
Statistical analysis
The collected data from all groups were imported to Statistical Package for Social Sciences (SPSS) for Windows software, version 17.0 (SPSS Inc., Chicago, IL, USA). The fitness of the data to a normal distribution was analyzed with the Kolmogorov-Smirnov test. The mean, and standard deviation values of the data belong to the independent variables that affect the push-out bond strength (irrigants and canal sealers) were calculated. The mean values of these groups were compared by using one-way ANOVA test (p<0.05) and the irrigation protocol values corrected by Bonferroni test with a new threshold level, p=0.00833.
Results
The dentinal push-out bond value for each group and the comparison of the groups are summarized in Table 2. AH Plus showed higher push-out bond strength value on CHX groups (Group 2 and 3) than the other two groups (p<0.001). The push-out bond strength of Endoseal MTA and Tech BioSealer Endo root canal sealers to dentine were not influenced by the final irrigation protocol (p=0.965).
Table 2.
Push-out bond strength (MPa, means±standard deviations) of root canal sealers in canal-like cavities irrigated with different regimes.CHX: chlorhexidine; EDTA: ethylenediamine tetra acetic acid; NaOCl: sodium hypochlorite. The different small letters indicate significantly differences between final irrigation groups (p less than 0.05).The different capital letters indicate significantly differences between sealers (p less than 0.05)
| Sealer | NaOCl + EDTA | NaOCl + CHX | NaOCl + EDTA + CHX | Distilled water | Total |
|---|---|---|---|---|---|
| AH Plus | 8.12 ± 2.37a | 12.87 ± 3.89b | 10.54 ± 4.65b | 6.68 ± 2.59a | 9.55 ± 4.16A |
| Endoseal MTA | 5.98 ± 2.2 | 6.07 ± 2.25 | 6.87 ± 3.63 | 5.22 ± 1.6 | 6.04 ± 2.53B |
| TechBiosealer Endo | 4.02 ± 0.96 | 5.17 ± 2.1 | 5.19 ± 2.11 | 4.41 ± 1.39 | 4.7 ± 1.74B |
Regardless of the root canal sealer, the use of CHX in final canal irrigation resulted in higher bond strength than the other two groups (p=0.003). No difference occurred between the two CHX combinations, likewise, the push-out bond strengths of the other two groups were also similar to each other (p=0.26).
AH Plus showed stronger dentinal push-out bond strength than bioceramic based root canal sealers independently of the final irrigation solutions (p<0.001).
Discussion
The present findings indicate a significant difference in the performance of the tested materials. AH Plus produced stronger push-out bond-strength to the root dentin than Endoseal MTA and Tech Biosealer Endo. Moreover, the pushout bond strength of AH Plus was affected by final irrigant. AH Plus presented stronger push-out bond strength when NaOCl-CHX used as a final irrigant rather than NaOCl-EDTA or distilled water. The push-out bond strength of Endoseal MTA and Tech Biosealer Endo to the root dentin were not affected by final irrigant. Therefore, the null hypothesis was partially rejected.
Different from the previous studies, there is a methodological aspect of this study to be considered. Standard canal- like holes were opened on dentin slices obtained from extracted human teeth in order to establish a more standardized groundwork. Moreover, sealers and irrigants were compared in the same dental samples which allow for better control on confounding factors such as dental age, sclerosis, micro-stiffness of dentine, canal shape, etc. Thus, this experimental setup overcomes the effects of different dentine sources on study design by allowing for placing three different sealers in the same slice (22, 24, 25). All of these biological-chemical-physical variances of the root dentine can increase sealer retention in the undercut nonprepared areas of natural root canals. Also, all the canal-like cavities were opened as a cylinder-shape with 1mm in diameter in order to maintain a standard root canal anatomy between the groups (25). In addition, the holes were filled only with sealers so that the load is fully applied to this material. Thus, erroneous interpretations of the performance of the gutta- percha are avoided (26). Although this method does not exactly reflect clinical practice is very useful for standardizing examples.
After discovering that the precipitate produced after successive usage of CHX and NaOCl does not contain a carcinogenic PCA, CHX solution, which has a potential to contribute to the antimicrobial activity of NaOCl, can be added to the standard irrigation protocol more easily (6, 19, 20). As it is planned to examine the effects of the precipitates, which emerge upon mixing the two solutions, on the dentinal adhesions of root canal sealers, neutralizing solutions were not used between the successive irrigants in the CHX groups of the present study. Push-out bond strength of calcium silicate-based sealers was not affected by irrigant combinations, while the push-out bond strength of AH Plus sealer to the dentine surprisingly increased compared to NaOCl-EDTA combination in dentinal samples that were immersed in NaOCl and CHX solutions successively. In a previous study, different CHX formulations used in final irrigant caused a higher chemical precipitate and smear layer on radicular dentin compared to irrigation protocol that contains 17% EDTA and 2.5% NaOCl (14). However, these residuals did not change the push-out bond strength of epoxy resin-based sealer (AH Plus) on radicular dentin (14, 27). The reason for this difference between the result of the present study and the results of previous studies may be due to the fact that the push-out bond strength experiments in those studies are performed on the main root canals. AH Plus can chemically bond to dentinal collagen amino groups. In order to establish a good bonding, it is necessary to bring out and more importantly to protect the collagen network (28, 29). From this perspective, amino groups that were dwelled on dentine depending on the irrigation solution can affect the adhesion of resin-based sealer to the canal walls (30).
There is a limited data in the literature about the dentinal push-out bond strength of both calcium silicate-based sealers, Endoseal MTA and Tech Biosealer Endo. In the present study, when final irrigant is not taken into account, Endoseal MTA and Tech Biosealer Endo root canal sealers showed weak dentinal push-out bond strength compared to AH Plus. Similarly, Oliveira et al. reported that AH Plus had significantly higher bond strength than both MTA Fillapex and iRoot SP (31). Furthermore, in a recent systematic review and meta- analysis, it has been reported that bioceramic sealers do not perform better than traditional epoxy sealers in terms of dislodgement resistance (32). Silva et al. used artificial canals opened in dentinal slices for push-out strength experiment, as the present study, and found that push-out strength of Endoseal MTA is weaker than of AH Plus but stronger than of MTA Fillapex (25). The push-out bond strength of Tech Biosealer Endo did not improve with the irrigation protocols in the present study. These results are in accordance with an earlier report that presented the push-out strength of Tech Biosealer Endo when root canals were irrigated with NaOCl- EDTA or NaOCl-CHX (33).
Conclusion
Within the limitations of this in vitro study, using CHX after NaOCl in final irrigation leads to increase in push-out bond strength of epoxy resin-based sealers, whereas it does not affect the dentinal bond strength of calcium silicate-based sealers.
Footnotes
Ethics committee approval:This study was reviewed and approved by the Research Ethics Committee of Karadeniz Technical University (Protocol Number: 2021/75).
Informed consent:Participants provided informed constent.
Peer review: Externally peer-reviewed.
Author contributions: DC, TT participated in designing the study. ATOK, TK participated in generating the data for the study. ATOK, TK participated in gathering the data for the study. DC participated in the analysis of the data. DC, TT wrote the majority of the original draft of the paper. DC, TT participated in writing the paper. ATOK has had access to all of the raw data of the study. DC, TT have reviewed the pertinent raw data on which the results and conclusions of this study are based. DC, ATOK, TK, TT have approved the final version of this paper. DC, ATOK, TK, TT guarantee that all individuals who meet the Journal’s authorship criteria are included as authors of this paper.
Conflict of interest:The authors had no conflict of interest to declare.
Financial disclosure:The authors declared that they have received no financial support.
References
- 1.Dugas NN, Lawrence HP, Teplitsky PE, Pharoah MJ, Friedman S. Periapical health and treatment quality assessment of root-filled teeth in two Canadian populations. Int Endod J. 2003. March;36(3):181–92. 10.1046/j.1365-2591.2003.00640.x [DOI] [PubMed] [Google Scholar]
- 2.Ureyen Kaya B, Kececi AD, Guldas HE, Orhan H. A retrospective radiographic study of coronal-periapical status and root canal filling quality in a selected adult Turkish population. Med Princ Pract. 2013;22(4):334–9. 10.1159/000346940 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Elayouti A, Achleithner C, Löst C, Weiger R. Homogeneity and adaptation of a new gutta-percha paste to root canal walls. J Endod. 2005. September;31(9):687–90. 10.1097/01.don.0000157991.83577.e0 [DOI] [PubMed] [Google Scholar]
- 4.Saleh IM, Ruyter IE, Haapasalo M, Ørstavik D. The effects of dentine pretreatment on the adhesion of root-canal sealers. Int Endod J. 2002. October;35(10):859–66. 10.1046/j.1365-2591.2002.00585.x [DOI] [PubMed] [Google Scholar]
- 5.Schwartz RS. Adhesive dentistry and endodontics. Part 2: bonding in the root canal system-the promise and the problems: a review. J Endod. 2006. December;32(12):1125–34. 10.1016/j.joen.2006.08.003 [DOI] [PubMed] [Google Scholar]
- 6.Thomas JE, Sem DS. An in vitro spectroscopic analysis to determine whether para-chloroaniline is produced from mixing sodium hypochlorite and chlorhexidine. J Endod. 2010. February;36(2):315–7. 10.1016/j.joen.2009.10.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zehnder M. Root canal irrigants. J Endod. 2006. May;32(5):389–98. 10.1016/j.joen.2005.09.014 [DOI] [PubMed] [Google Scholar]
- 8.Haapasalo M, Shen Y, Wang Z, Gao Y. Irrigation in endodontics. Br Dent J. 2014. March;216(6):299–303. 10.1038/sj.bdj.2014.204 [DOI] [PubMed] [Google Scholar]
- 9.Clarkson RM, Podlich HM, Moule AJ. Influence of ethylenediaminetetraacetic acid on the active chlorine content of sodium hypochlorite solutions when mixed in various proportions. J Endod. 2011. April;37(4):538–43. 10.1016/j.joen.2011.01.018 [DOI] [PubMed] [Google Scholar]
- 10.Hülsmann M, Rödig T, Nordmeyer S. Complications during root canal irrigation. Endod Topics. 2009;16(1):27–63. 10.1111/j.1601-1546.2009.00237.x [DOI] [Google Scholar]
- 11.Hashem AA, Ghoneim AG, Lutfy RA, Fouda MY. The effect of different irrigating solutions on bond strength of two root canal-filling systems. J Endod. 2009. April;35(4):537–40. 10.1016/j.joen.2009.01.003 [DOI] [PubMed] [Google Scholar]
- 12.Naenni N, Thoma K, Zehnder M. Soft tissue dissolution capacity of currently used and potential endodontic irrigants. J Endod. 2004. November;30(11):785–7. 10.1097/00004770-200411000-00009 [DOI] [PubMed] [Google Scholar]
- 13.Zehnder M. Root canal irrigants. J Endod. 2006. May;32(5):389–98. 10.1016/j.joen.2005.09.014 [DOI] [PubMed] [Google Scholar]
- 14.Graziele Magro M, Kuga MC, Regina Victorino K, Vázquez-Garcia FA, Aranda-Garcia AJ, Faria-Junior NB, et al. Evaluation of the interaction between sodium hypochlorite and several formulations containing chlorhexidine and its effect on the radicular dentin—SEM and push-out bond strength analysis. Microsc Res Tech. 2014. January;77(1):17–22. 10.1002/jemt.22307 [DOI] [PubMed] [Google Scholar]
- 15.Kuruvilla JR, Kamath MP. Antimicrobial activity of 2.5% sodium hypochlorite and 0.2% chlorhexidine gluconate separately and combined, as endodontic irrigants. J Endod. 1998. July;24(7):472–6. 10.1016/S0099-2399(98)80049-6 [DOI] [PubMed] [Google Scholar]
- 16.Bui TB, Baumgartner JC, Mitchell JC. Evaluation of the interaction between sodium hypochlorite and chlorhexidine gluconate and its effect on root dentin. J Endod. 2008. February;34(2):181–5. 10.1016/j.joen.2007.11.006 [DOI] [PubMed] [Google Scholar]
- 17.Burkhardt-Holm P, Oulmi Y, Schroeder A, Storch V, Braunbeck T. Toxicity of 4-chloroaniline in early life stages of zebrafish (Danio rerio): II. Cytopathology and regeneration of liver and gills after prolonged exposure to waterborne 4-chloroaniline. Arch Environ Contam Toxicol. 1999. July;37(1):85–102. 10.1007/s002449900493 [DOI] [PubMed] [Google Scholar]
- 18.Basrani BR, Manek S, Sodhi RN, Fillery E, Manzur A. Interaction between sodium hypochlorite and chlorhexidine gluconate. J Endod. 2007. August;33(8):966–9. 10.1016/j.joen.2007.04.001 [DOI] [PubMed] [Google Scholar]
- 19.Orhan EO, Irmak Ö, Hür D, Yaman BC, Karabucak B. Does Para-chloroaniline really form after mixing sodium hypochlorite and chlorhexidine? J Endod. 2016. March;42(3):455–9. 10.1016/j.joen.2015.12.024 [DOI] [PubMed] [Google Scholar]
- 20.Irmak Ö, Orhan EO, Görgün K, Yaman BC. Nuclear magnetic resonance spectroscopy and infrared spectroscopy analysis of precipitate formed after mixing sodium hypochlorite and QMix 2in1. PLoS One. 2018. August;13(8):e0202081. 10.1371/journal.pone.0202081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Neelakantan P, Sharma S, Shemesh H, Wesselink PR. Influence of irrigation sequence on the adhesion of root canal sealers to dentin: a fourier transform infrared spectroscopy and push-out bond strength analysis. J Endod. 2015. July;41(7):1108–11. 10.1016/j.joen.2015.02.001 [DOI] [PubMed] [Google Scholar]
- 22.Scelza MZ, da Silva D, Scelza P, de Noronha F, Barbosa IB, Souza E, et al. Influence of a new push-out test method on the bond strength of three resin-based sealers. Int Endod J. 2015. August;48(8):801–6. 10.1111/iej.12378 [DOI] [PubMed] [Google Scholar]
- 23.Bitter K, Meyer-Lueckel H, Priehn K, Kanjuparambil JP, Neumann K, Kielbassa AM. Effects of luting agent and thermocycling on bond strengths to root canal dentine. Int Endod J. 2006. October;39(10):809–18. 10.1111/j.1365-2591.2006.01155.x [DOI] [PubMed] [Google Scholar]
- 24.Silva EJ, Carvalho NK, Zanon M, Senna PM, De-Deus G, Zuolo ML, et al. DE-Deus G, Zuolo ML, Zaia AA. Push-out bond strength of MTA HP, a new high-plasticity calcium silicate-based cement. Braz Oral Res. 2016;30(1):e84. 10.1590/1807-3107BOR-2016.vol30.0084 [DOI] [PubMed] [Google Scholar]
- 25.Silva EJ, Carvalho NK, Prado MC, Zanon M, Senna PM, Souza EM, et al. Push-out bond strength of injectable Pozzolan-based root canal sealer. J Endod. 2016. November;42(11):1656–9. 10.1016/j.joen.2016.08.009 [DOI] [PubMed] [Google Scholar]
- 26.Silva EJ, Carvalho NK, Prado MC, Senna PM, Souza EM, De-Deus G. Bovine teeth can reliably substitute human dentine in an intra-tooth push-out bond strength model? Int Endod J. 2019. July;52(7):1063–9. 10.1111/iej.13085 [DOI] [PubMed] [Google Scholar]
- 27.Magro MG, Kuga MC, Aranda-Garcia AJ, Victorino KR, Chávez-Andrade GM, Faria G, et al. Effectiveness of several solutions to prevent the formation of precipitate due to the interaction between sodium hypochlorite and chlorhexidine and its effect on bond strength of an epoxy-based sealer. Int Endod J. 2015. May;48(5):478–83. 10.1111/iej.12337 [DOI] [PubMed] [Google Scholar]
- 28.Prati C, Chersoni S, Pashley DH. Effect of removal of surface collagen fibrils on resin-dentin bonding. Dent Mater. 1999. September;15(5):323–31. 10.1016/S0109-5641(99)00052-4 [DOI] [PubMed] [Google Scholar]
- 29.Fisher MA, Berzins DW, Bahcall JK. An in vitro comparison of bond strength of various obturation materials to root canal dentin using a push-out test design. J Endod. 2007. July;33(7):856–8. 10.1016/j.joen.2007.02.011 [DOI] [PubMed] [Google Scholar]
- 30.Güzel C, Uzunoglu E, Dogan Buzoglu H. Effect of low–surface tension EDTA solutions on the bond strength of resin-based sealer to young and old root canal dentin. J Endod. 2018. March;44(3):485–8. 10.1016/j.joen.2017.09.007 [DOI] [PubMed] [Google Scholar]
- 31.Oliveira DS, Cardoso ML, Queiroz TF, Silva EJ, Souza EM, De-Deus G. Suboptimal push-out bond strengths of calcium silicate-based sealers. Int Endod J. 2016. August;49(8):796–801. 10.1111/iej.12519 [DOI] [PubMed] [Google Scholar]
- 32.Silva EJ, Canabarro A, Andrade MR, Cavalcante DM, Von Stetten O, Fidalgo TK, et al. Dislodgment resistance of bioceramic and epoxy sealers: a systematic review and meta-analysis. J Evid Based Dent Pract. 2019. September;19(3):221–35. 10.1016/j.jebdp.2019.04.004 [DOI] [PubMed] [Google Scholar]
- 33.Neelakantan P, Nandagopal M, Shemesh H, Wesselink P. The effect of root dentin conditioning protocols on the push-out bond strength of three calcium silicate sealers. Int J Adhes Adhes. 2015;60:104–8. 10.1016/j.ijadhadh.2015.04.006 [DOI] [Google Scholar]


