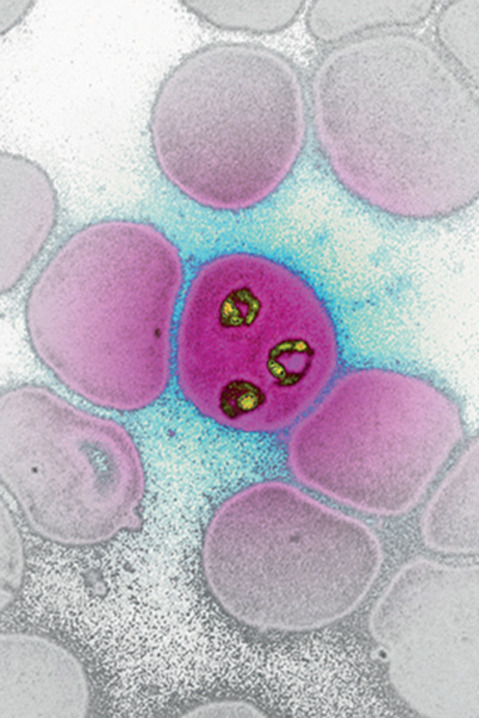
Although we currently focus our efforts on the understanding, treatment, and control of SARS-CoV-2 infections, malaria remains a major public health problem. In 2019, there were 229 million new malaria infections causing 409 000 deaths.1
Over the past 20 years, impressive progress has been made in the fight against malaria; however, parasites developed mutations in the K13 propeller gene that resulted in delayed clearance of parasites following artesunate treatment.2, 3 This emergence of partial resistance to artesunate treatment was swiftly followed by the acquisition of resistance to partner drugs, resulting in the reduced efficacy of artesunate combination treatments.4 Resistance to artesunate in southeast Asia was first reported in 2008, and this year reports from Africa indicated a similar development, with parasites harbouring mutations in the K13 gene, resulting in delayed clearance.5
To ensure that the gains in the fight against malaria can be extended to achieve eradication of this disease, new combination treatments and simplified treatment regimens are necessary to replace the existing treatments. It is important that these new combination treatments are comprised of drugs that have not yet been widely deployed and have different mechanisms of action.6 One of the new molecules in development is M5717 (previously DDD107498), an inhibitor of the translational elongation factor 2, which was discovered at Dundee University's Drug Development Unit, Scotland, UK, by Baragaña and colleagues.7 This molecule is now being developed by Merck KGaA (Darmstadt, Germany), in collaboration with the Medicines for Malaria Venture (MMV).
In The Lancet Infectious Diseases, James McCarthy and colleagues report the results of a combined first-in-human, randomised, placebo-controlled, double-blind, single ascending dose study and a volunteer infection study with M5717.8 The study design was similar to previous first-in-human volunteer infection studies:9 in the single ascending dose part of the study, single doses of up to 2100 mg were tested in healthy adult volunteers, and in the volunteer infection study, participants were infected with Plasmodium falciparum-infected red blood cells and treated with 150, 400, or 800 mg M5717. A total of 88 volunteers were enrolled: 66 in the single ascending dose study and 22 in the volunteer infection study. M5717 was well tolerated up to 1250 mg; at doses of 1800 and 2100 mg, transient oral hypoesthesia (in three participants) and blurred vision (in four participants) were observed, and further dosing was suspended after dosing of the two sentinel participants in the 2100 mg cohort.
In the volunteer infection study, parasite clearance was biphasic, showing an initial plateau with slow parasite clearance lasting for approximately 35–55 h, followed by a steep decline of blood-stage parasitaemia. Recrudescence occurred in three (50%) of six participants dosed with 150 mg and two (25%) of eight dosed with 400 mg. No recrudescence was observed in participants who received a single dose of 800 mg. Parasites of the five cases of recrudescence were genetically analysed, and mutations were detected in four cases that are associated with resistance to M5717 (in two participants dosed with 150 mg and two dosed with 400 mg).
These results are encouraging for further development of M5717, yet important questions remain. What is the role of a drug for which resistance can be induced after a single dose? Partner drug selection for the development of a combination treatment must carefully assess this risk and evaluate early in the development of the combination whether it will be possible to prevent the emergence of resistance. As the initial parasite clearance of M5717 is slow, the partner drug should also exhibit a rapid elimination to ensure fast symptomatic and parasitological relief and avoid M5717-treated parasites replicating and acquiring mutations that could lead to the emergence of resistance. To ensure that the selection of a suitable partner molecule to M5717 follows a data-driven process, Merck KGaA has joined a platform with other organisations that have antimalarial drug candidates in translational development, which is hosted by MMV. This platform allows sharing of information and data, the conduct of in-vitro and in-vivo combination experiments, and the identification of the most appropriate drug combinations for further investment. The first combinations emerging from this platform are expected to enter clinical studies in 2022.
© 2021 Science Photo Library
I an employee of the Medicines for Malaria Venture.
References
- 1.WHO World malaria report. 2020. https://www.who.int/publications/i/item/9789240015791
- 2.Noedl H, Se Y, Schaecher K, Smith BL, Socheat D, Fukuda MM. Evidence of artemisinin-resistant malaria in western Cambodia. N Engl J Med. 2008;359:2619–2620. doi: 10.1056/NEJMc0805011. [DOI] [PubMed] [Google Scholar]
- 3.Dorndop AM, Nosten F, Yi P, et al. Artemisinin resistance in Plasmodium falciparum malaria. N Engl J Med. 2009;361:455–467. doi: 10.1056/NEJMoa0808859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.van der Pluijm RW, Imwong M, Chau NH, et al. Determinants of dihydroartemisinin–piperaquine treatment failure in Plasmodium falciparum malaria in Cambodia, Thailand, and Vietnam: a prospective clinical, pharmacological, and genetic study. Lancet Infect Dis. 2019;19:952–961. doi: 10.1016/S1473-3099(19)30391-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Uwimana A, Umulisa N, Venkatesan M, et al. Association of Plasmodium falciparum kelch13 R561H genotypes with delayed parasite clearance in Rwanda: an open-label, single-arm, multicentre, therapeutic efficacy study. Lancet Infect Dis. 2021;21:1120–1128. doi: 10.1016/S1473-3099(21)00142-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Burrows JN, Duparc S, Gutteridge WE, et al. New developments in anti-malarial target candidate and product profiles. Malar J. 2017;16:26. doi: 10.1186/s12936-016-1675-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Baragaña B, Hallyburton I, Lee MCS, et al. A novel, multiple stage antimalarial agent that inhibits protein synthesis. Nature. 2015;522:315–320. doi: 10.1038/nature14451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McCarthy JS, Yalkinoglu Ö, Odedra A, et al. Safety, pharmacokinetics, and antimalarial activity of the novel plasmodium eukaryotic translation elongation factor 2 inhibitor M5717: a first-in-human, randomised, placebo-controlled, double-blind, single ascending dose study and volunteer infection study. Lancet Infect Dis. 2021 doi: 10.1016/S1473-3099(21)00252-8. published online Oct 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McCarthy JS, Lotharius J, Rückle T, et al. Safety, tolerability, pharmacokinetics, and activity of the novel long-acting antimalarial DSM265: a two-part first-in-human phase 1a/1b randomised study. Lancet Infect Dis. 2017;17:626–635. doi: 10.1016/S1473-3099(17)30171-8. [DOI] [PMC free article] [PubMed] [Google Scholar]


