Abstract
Background
Victoria experienced the greatest burden of COVID-19 in Australia in 2020. This report describes key epidemiological characteristics and corresponding control measures between 17 January 2020 and 26 March 2021.
Methods
COVID-19 notifications made to the State Government Department of Health were used in this analysis. Epidemiological features are described over 4 phases, including enhancements to testing, contact tracing and public health interventions. Demographic and clinical features of cases are described.
Findings
Victoria recorded 20,483 cases of COVID-19, of which 1073 (5•2%) were acquired overseas and 19,360 (95%) were locally acquired. The initial epidemic (Phase I) was well-contained through public health interventions and was followed by relaxation of restrictions and low-level community transmission (Phase II). However, an outbreak in a hotel used to quarantine returned travellers led to wide-scale community transmission accounting for a majority (91%) of cases (Phase III). Outbreaks occurred in vulnerable settings including aged care and hospitals, contributing to high hospitalisation (12%) and case fatality rates (3•7%). Aggressive restrictions ultimately led to local elimination, and subsequent outbreaks have been swiftly managed with improved processes (Phase IV). The demographic composition of cases evolved across phases from an older, wealthier population to a less advantaged younger population, with many from culturally and linguistically diverse backgrounds.
Interpretation
Over time, adaptations to the public health response have strengthened capacity to respond to new cases and outbreaks in a more effective manner. The Victorian experience underscores the importance of authentic engagement with diverse communities and balancing restrictions with livelihoods.
Keywords: SARS-CoV-2, outbreak, non-pharmaceutical interventions, travel restricitions, hotel quarantine
Research in context.
Evidence before this study
The effectiveness of non-pharmaceutical interventions for controlling COVID-19 has been demonstrated in a number of countries. However, in many cases suppression has been the goal, not elimination. We conducted a pubmed search using the terms ("novel coronavirus" OR "nCoV" OR "COVID-19" OR "severe acute respiratory syndrome coronavirus 2" OR "SARS-CoV-2") AND ("elimination" OR "suppression") AND ("nonpharmaceutical" OR "non-pharmaceutical" OR "lockdown" OR "restrictions"). Of 109 articles identified, many were modelling studies or described suppression of COVID-19 without elimination. Where elimination was achieved, case numbers were in the hundreds (e.g. Beijing in June 2020) or low thousands (e.g. New Zealand in early 2020).
Added value of this study
We describe successful elimination after a sizeable (∼18,703 cases) point-source community outbreak in Victoria, Australia, that was achieved through aggressive control strategies, including restrictions on travel, work, school attendance, and gatherings, augmented by enhanced contact tracing, effective isolation of cases and close contacts, and widespread availability of free testing. This is the first study, to our knowledge, since Wuhan to describe local elimination after such a large outbreak of non-delta SARS-CoV-2.
Implications of all the available evidence
This study adds to the existing evidence that a comprehensive, multifaceted control strategy could achieve local elimination of SARS-CoV-2. Although the delta variant of SARS-CoV-2 is proving more resistant to these measures, the lessons learnt remain instructive for future pandemic plans.
Alt-text: Unlabelled box
Introduction
Australia's first case of coronavirus disease 2019 (COVID-19), caused by the severe acute respiratory syndrome coronavirus 2 virus (SARS-CoV-2), was notified to the Victorian Government Department of Health (formerly the Department of Health and Human Services) on 25 January 2020. The case was a traveller returning from Wuhan, China [1]. In the following months, multiple returning international travellers infected with SARS-CoV-2 seeded local outbreaks and community transmission. In response, national and state public health control measures were implemented, including travel restrictions, mandatory hotel quarantine for international arrivals, case isolation and contact tracing, and community measures including school closures and working from home policies. These measures saw the suppression of the first epidemic across Australia by mid-May 2020.
Infection of staff at a quarantine hotel initiated a second, larger epidemic that took 5 months to suppress. This was Australia's largest SARS-CoV-2 epidemic in 2020, accounting for around 70% of the total cases notified in the country. Here we describe the epidemiology of COVID-19 epidemic phases in Victoria, including case demographics, morbidity and mortality, and details of effective public health measures that suppressed community transmission in the absence of vaccination.
Methods
Case detection
On 29 January 2020, COVID-19 was made a notifiable condition in Victoria, requiring all suspected and confirmed cases to be notified to the Department of Health by both medical practitioners and laboratories. All SARS-CoV-2 test results were received centrally and entered in the state's Public Health Event Surveillance System (PHESS). Direct electronic notification from laboratories was rapidly operationalised by March 2020.
Testing for SARS-CoV-2 was available by mid-January using in-house assays developed at the Victorian Infectious Diseases Reference Laboratory (VIDRL). Commercial kits became available in late February 2020, with scale-up at commercial and hospital laboratories (Figure 1) enabled by a validation panel supplied by VIDRL. Confirmation of “weak positive” results by VIDRL was introduced in June 2020 to rule out false positives.
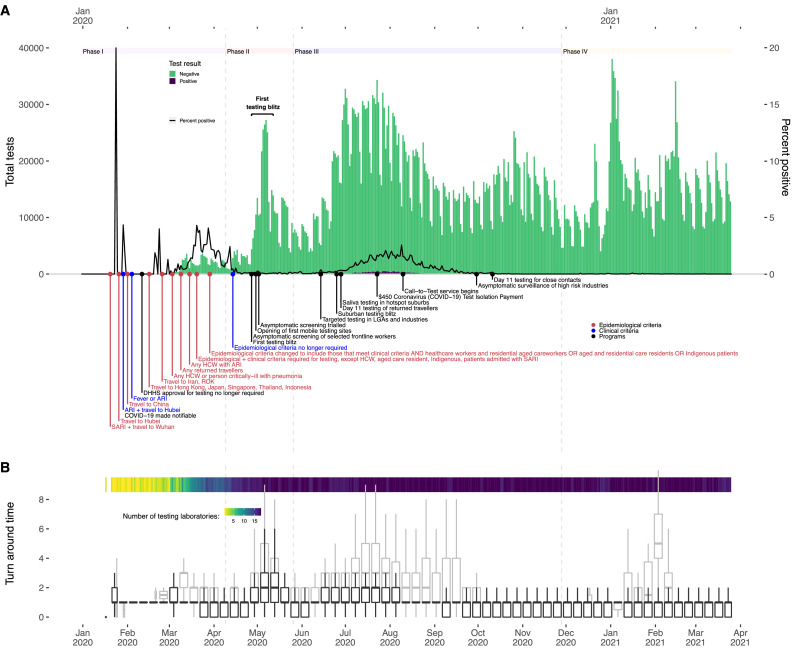
Figure 1.
Testing capacity by sample collection date, Victoria 17 Jan 2020 – 26 Mar 2021: A. Daily number of tests performed (green bars) and percent of samples positive for SARS-CoV-2 (black line). Annotations indicate key changes to testing criteria. B. Weekly turn-around times from sample collection to test (black boxplots; outliers not shown) and from sample collection to notification (grey boxplots). Shaded bar shows the number of laboratories performing testing.
Notes: SARI: Severe Acute Respiratory Infection; ARI: Acute Respiratory Infection; ROK: Republic of Korea; HCW: Healthcare worker; LGA: Local government area.
Testing criteria evolved between January and May 2020 (Figure 1). Initially, both epidemiological (travel to Wuhan, China) and clinical criteria (symptoms) were required. Other countries with COVID-19 transmission and high-risk professions such as healthcare workers were later added, until epidemiological criteria were dropped altogether in April. Clinical criteria initially included fever or acute respiratory infection (ARI), but were later broadened to any respiratory symptoms. Changes to the criteria were influenced by global shortages of consumables, including swabs, and initial uncertainty around the positive predictive value of tests. As concerns about pre-symptomatic transmission increased, routine testing, including asymptomatic screening, was introduced to target high-risk industries (e.g. aged care, abattoirs) or geographic regions with high case incidence. Testing was free-of-charge and financial support was provided to people unable to work while isolating [2,3].
Cases were also detected through testing of symptomatic and, later, asymptomatic close contacts. Clearance testing was offered to close contacts 11 days post-symptoms onset from early July and, from 11 October 2020, individuals refusing day 11 testing were required to quarantine for a further 10 days. Widespread testing to identify possible acquisition source cases was instigated in outbreak settings where the index case was unknown and testing of waste water commenced.
Public health management
On 16 March 2020, Victoria declared a ‘state of emergency’ under the Public Health and Wellbeing Act 2008, which provided the Chief Health Officer emergency powers to issue directions and set requirements to eliminate or reduce risks to public health. On 2 August 2020, a ‘state of disaster’ was further declared in Victoria under the Emergency Management Act 1986, giving police greater power to enforce public health orders [4].
Case and contact management
All notified cases were contacted by the Department of Health and a detailed questionnaire was used to assess risk and probable source of infection. Upstream contact tracing—also referred to as backward tracing [5], the process whereby cases are asked to identify everyone with whom they had contact during their acquisition period two weeks prior to symptoms onset—was undertaken to support the identification of possible source cases to each index case as well as downstream contact tracing to identify individuals with whom they had contact during their infectious period. In July interdisciplinary outbreak teams were established for case, contact and outbreak management in certain settings (e.g. aged care, schools, health care). Between mid-July and the end of August, when case numbers peaked, detailed interviews covering the acquisition source period were truncated, focussing on the infectious period (48 hours before symptom onset) to support rapid identification and isolation of infectious cases.
All cases were required to isolate for a minimum period of 10 days from date of symptom onset or swab if asymptomatic. Clearance criteria initially required two negative PCR tests following the resolution of symptoms, but was later made automatic, depending on severity. Severely immunocompromised cases continued to require clearance tests.
Clinical and sociodemographic data about cases were captured in PHESS, along with indicators of disease severity including hospitalisation, intensive care and/or ventilation status. These data elements were further augmented via enhanced hospital-based surveillance implemented in April [6]. Case mortality status was supplemented by record linkage with the State's register of deaths.
Data sources
De-identified data for all cases and SARS-CoV-2 test results were extracted from PHESS on 30 April 2021 for the period 17 January 2020 to 26 March 2021. Data extracted included demographic, clinical and epidemiological risk information.
Population denominators and maps were derived from official state government projections of population and households for age and sex [7] or the 2016 Australian Census for other measures, including spatial data and socio-economic position [8,9]. The geographic spread of cases per population per square kilometre was plotted using risk surfaces (see Supplementary Material).
Data analyses
Information for cases with PCR-confirmed illness were extracted from PHESS for analysis. Data were analysed separately for four distinct phases based on epidemiological characteristics: 1) 17 January – 9 April 2020, the period between the first SARS-CoV-2 test and the day before the first day with no community cases (10 April); 2) 10 April – 25 May 2020 during which case numbers were sporadic; and 3) 26 May – 27 November 2020, the period between an outbreak in hotel quarantine that led to community transmission and local elimination (28 days without a new case); 4) 28 November 2020 – 26 March 2021, during which sporadic outbreaks were swiftly suppressed.
Allocation of cases to each phase was based on the date of symptom onset (or date of test if asymptomatic), which was decided a priori to be more indicative of the true status of infection in the community independent of testing, test processing and notification delays. Key demographic and clinical data were summarised as frequency and percent or median and interquartile range (IQR). Incidence rates were calculated per population by key demographic characteristics. The effective reproduction number (Reff) was calculated using the EpiNow R package for periods with sufficient cases (see Supplementary Material). Data were analysed using R version 4.0.3 [10].
Ethics
Analyses of disease notifications presented in this report were conducted under the Public Health and Wellbeing Act 2008 (Victoria) to evaluate and inform local public health interventions. Additional approval was provided by the University of Melbourne Human Research Ethics Committee (2020-20308-12480-3).
Role of the funding source
This study did not receive any specific funding source and utilised routinely collected public health data.
Results
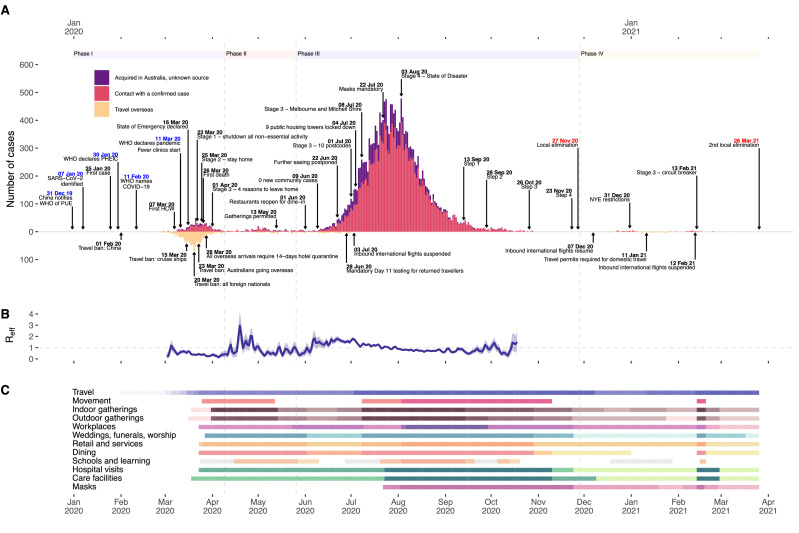
There were 20,483 cases of SARS-CoV-2 notified in Victoria between 17 January 2020 and 26 March 2021 (Figure 2), representing a crude incidence rate of 302 per 100,000 population. Characteristics of all cases are summarised in Table 1 and Table 2.
Figure 2.
Epidemic situation: A. Epidemic curve of daily new cases by symptoms onset date or diagnosis date if asymptomatic, and key events in the epidemic and response. The first case had symptoms onset on 19 Jan 2020, the last locally-acquired case had symptoms onset on 8 Mar 2021; B. Effective reproduction number (Reff) estimates Mar-Oct 2020. Reff not estimated for periods with sporadic cases due to uncertainty around estimates; C. Key mitigation measures implemented during each phase of the epidemic. Darker shading indicates more stringent restrictions. The full list of measures is shown in Supplementary Figure 1, which details the restrictions associated with the colours.
Notes: WHO: World Health Organization; PUE: pneumonia of unknown aetiology; SARS-CoV-2: Severe Acute Respiratory Syndrome Coronavirus 2; PHEIC: Public Health Event of International Concern; COVID-19: Coronavirus Disease 2019; HCW: Healthcare worker; NYW: New Year's Eve. Refer to the Supplementary information for a description of the calculation of Reff.
Table 1.
Demographic characteristics of COVID-19 cases in Victoria, 17 Jan 2020-26 Mar 2021, by epidemic phase
| Victorian populationc | Phase I 17 Jan – 9 Apr 2020 |
Phase II 10 Apr – 25 May 2020 |
Phase III 26 May – 27 Nov 2020 |
Phase IV 28 Nov 2020 – 26 Mar 2021 |
|||||
|---|---|---|---|---|---|---|---|---|---|
| n (%) | Incidence per100,000 py (95%CI) | n (%) | Incidence per100,000 py (95%CI) | n (%) | Incidence per100,000 py (95%CI) | n (%) | Incidence per100,000 py (95%CI) | ||
| Total cases | 6,729,626 | 1323 | 87 (82,91) | 317 | 38 (34,43) | 18703 | 549 (541,557) | 140 | 6.5 (5.4,7.6) |
| Age (median (IQR)) | - | 46 (29,61) | - | 39 (24,52) | - | 40 (23,54) | - | 34 (25,43) | - |
| Age Group | |||||||||
| <15 years | 1,235,363 | 21 (1•6%) | 7•5 (4•6,11) | 31 (9•8%) | 20 (14,29) | 1,983 (11%) | 317 (303,331) | 16 (11%) | 4•0 (2•3,6•5) |
| 15-59 years | 4,087,225 | 945 (71%) | 102 (95,108) | 237 (75%) | 47 (41,53) | 13,095 (70%) | 633 (622,644) | 115 (82%) | 8•7 (7•2,10) |
| 60-79 years | 1,131,673 | 324 (24%) | 128 (114,143) | 39 (12%) | 28 (20,39) | 1,837 (9•8%) | 325 (311,341) | 9 (6•4%) | 2•5 (1•1,4•8) |
| 80+ years | 275,365 | 33 (2•5%) | 57 (39,79) | 10 (3•2%) | 32 (15,58) | 1,788 (9•6%) | 1375 (1312,1441) | 0 | 0•000 (0•000,4•5) |
| Sex | |||||||||
| Female | 3,397,788 | 634 (47•9%) | 82 (76,89) | 141 (44%) | 34 (28,40) | 9,852 (53%) | 573 (561,584) | 70 (50%) | 6•4 (5•0,8•1) |
| Male | 3,331,838 | 689 (52•1%) | 91 (85,98) | 176 (56%) | 43 (37,50) | 8,840 (47%) | 526 (515,537) | 70 (50%) | 6•5 (5•1,8•3) |
| Other | - | 0 | - | 0 | - | 3 (0•02%) | - | 0 | - |
| Missing/not stated | - | 0 | - | 0 | - | 8 (0•04%) | - | 0 | - |
| Indigenous Status | |||||||||
| Aboriginal and/or Torres Strait Islander | 47,509 | 2 (0•15%) | 19 (2•2,67) | 3 (0•95%) | 51 (11,150) | 70 (0•37%) | 291 (227,368) | 0 | 0•000 (0•000,24) |
| Not Aboriginal or Torres Strait Islander | 5,526,028 | 1,257(95%) | 100 (95,106) | 305 (96%) | 45 (40,50) | 17,178 (92%) | 614 (605,623) | 137 (98%) | 7•7 (6•5,9•1) |
| Missing/not stated | - | 64 (4.8%) | 9 (2•8%) | - | 1455 (7.8%) | - | 3 (2•1%) | - | |
| Metro/Rural residence | |||||||||
| Metro | 4,139,719 | 1,069 (81%) | 114 (107,121) | 270 (85%) | 53 (47,60) | 17,598 (94%) | 840 (827,852) | 90 (64%) | 6•8 (5•4,8•3) |
| Rural | 1,433,818 | 213 (16%) | 66 (58,76) | 20 (6•3%) | 11 (7•0,18) | 969 (5•2%) | 135 (127,144) | 1 (0•71%) | 0•22 (0•006,1•2) |
| Interstate | - | 34 (2•6%) | - | 23 (7•3%) | - | 48 (0•26%) | - | 5 (3•6%) | - |
| Overseas | - | 6 (0•45%) | - | 1 (0•32%) | - | 1 (0•005%) | - | 13 (9•3%) | - |
| Missing/not stated | - | 1 (0•08%) | - | 3 (0953%) | - | 87 (0•47%) | - | 31 (22%) | - |
| Country of Birth | |||||||||
| Australia | 4,280,650 | 829 (63%) | 85 (80,91) | 113 (36%) | 21 (18,26) | 6,998 (37%) | 323 (315,330) | 42 (30%) | 3•0 (2•2,4•1) |
| Overseas- English maind | 439,570 | 160 (12%) | 164 (140,192) | 28 (8•8%) | 53 (35,77) | 704 (3•8%) | 324 (300,349) | 14 (10%) | 10 (5•5,17) |
| Overseas- English non-main | 1,453,000 | 254 (19%) | 77 (68,87) | 147 (46%) | 83 (70,97) | 8,788 (47%) | 1204 (1179,1229) | 65 (46%) | 14 (11,18) |
| Missing/not stated | - | 81 (6•1%) | - | 29 (9.1%) | - | 2,213 (12%) | - | 19 (14%) | - |
| Language spoken at home | |||||||||
| English | 4,026,811 | 81 (6•1%) | 8•9 (7•0,11) | 13 (4•1%) | 2•6 (1•4,4•5) | 9,263 (50%) | 454 (445,464) | 80 (57%) | 6•2 (4•9,7•7) |
| Language other than English | 1,538,776 | 27 (2•0%) | 7•8 (5•1,11) | 64 (20%) | 34 (26,44) | 5,618 (30%) | 728 (709,747) | 41 (29%) | 8•4 (6•0,11) |
| Non-verbal | - | 2 (0•15%) | - | 0 | - | 13 (0•01%) | - | 0 | - |
| Missing/not stated | - | 1,213 (92%) | - | 240 (76%) | - | 3,908 (20%) | - | 19 (14%) | - |
| Aged care residentf | |||||||||
| Aged care resident | 58,535f | 0 | - | 4 (1•3%) | 55 (15,142) | 1,959 (10%) | 6608 (6319,6907) | 0 | - |
| Not recorded as aged care resident | 6,671,091 | 1,323 (100%) | 87 (83,92) | 313 (99%) | 38 (34,43) | 16,744 (90%) | 496 (488,503) | 140 (100%) | 6•5 (5•5,7•7) |
| Public housing residence | |||||||||
| Lives in public housing | 86,266 | 13 (0•98%) | 86 (46,147) | 9 (2•8%) | 110 (50,208) | 910 (4•9%) | 2694 (2522,2875) | 2 (1•4%) | 9•4 (1•1,34) |
| Not recorded as living in public housing | 6,643,360 | 1,310 (99%) | 87 (82,92) | 308 (97%) | 38 (34,42) | 17,793 (95%) | 529 (521,537) | 138 (99%) | 6•4 (5•4,7•6) |
| Socioeconomic disadvantageg | |||||||||
| First quintile – lowest | 1,180,673 | 142 (11%) | 53 (45,62) | 93 (29%) | 64 (52,78) | 5,629 (30%) | 941 (917,966) | 16 (11%) | 4•2 (2•4,6•8) |
| Second quintile | 931,389 | 143 (11%) | 68 (57,80) | 49 (15%) | 43 (32,57) | 3,119 (17%) | 665 (642,689) | 20 (14%) | 6•7 (4•1,10) |
| Third quintile | 1,097,814 | 189 (14%) | 76 (66,88) | 63 (20%) | 47 (36,60) | 4,452 (24%) | 808 (784,832) | 5 (3•6%) | 1•4 (0•46,3•3) |
| Fourth quintile | 1,264,006 | 257 (19%) | 90 (80,102) | 38 (12%) | 25 (17,34) | 2,839 (15%) | 448 (432,465) | 14 (10%) | 3•5 (1•9,5•8) |
| Fifth quintile – highest | 1,442,431 | 551 (42%) | 170 (156,185) | 47 (15%) | 27 (20,36) | 2,579 (14%) | 357 (344,371) | 39 (28%) | 8•5 (6•0,12) |
| Missing/not stated | - | 1 (0•001%) | - | 2 (0•63%) | - | 35 (0•19%) | - | 29 (21%) | - |
| Non-resident | - | 40 (3•0%) | - | 24 (7•6%) | - | 49 (0•26%) | - | 19 (14%) | - |
Population denominators are from official state government population projections for age and sex (8) or the 2016 Census for other metrics (9, 10). Incidence rates may therefore be slightly overestimated. py: person years, calculated from start to the end of each phase.
Includes the United Kingdom, Ireland, New Zealand, Canada, the United States and Singapore.
Based on the number of operational places in Residential Aged Care in Victoria, excluding transition care (23)
Quintiles are based on the total Australian population and a person’s quintile is determined by post code. Higher quintiles represent higher socioeconomic advantage. Population denominators from 2016 census.
Table 2.
Epidemiological and clinical characteristics of COVID-19 cases in Victoria, 17 Jan 2020-26 Mar 2021, by epidemic phase
| Phase I17 Jan – 9 Apr 2020 | Phase II10 Apr – 25 May 2020 | Phase III26 May – 27 Nov 2020 | Phase IV28 Nov 2020 – 26 Mar 2021 | ||
|---|---|---|---|---|---|
| Acquisition | Contact with a confirmed case | 428 (32%) | 174 (55%) | 14,995 (80%) | 50 (36%) |
| Acquired in Australia, unknown source | 108 (8•2%) | 60 (18•9%) | 3,593 (19•2%) | 2 (1•4%) | |
| Travel overseas | 787 (60%) | 83 (26%) | 115 (0•6%) | 88 (63%) | |
| Days from onset to test | median days, (IQR) | 6 (3,9) | 3 (0,6) | 2 (0,5) | 0 (0,2) |
| Number of days from symptoms onset to isolation (excludes travel overseas) | Isolated before or as soon as symptoms started | 216 (40%) | 72 (31%) | 8,601 (46%) | 22 (42%) |
| 1 or more symptomatic days in the community prior to isolation | 314 (59%) | 121 (52%) | 6,065 (33%) | 19 (37%) | |
| Missing | 6 (1•1%) | 41 (18%) | 3,922 (21%) | 11 (21%) | |
| Symptomatic status at or prior to testing | Asymptomatic at Testing | 19 (1•4%) | 83 (26•2%) | 5,136 (28%) | 61 (44%) |
| Symptomatic at Testing | 1,299 (98%) | 231 (73%) | 13,510 (72%) | 78 (56%) | |
| Missing | 5 (0•38%) | 3 (0•95%) | 57 (0•30%) | 1 (0•71%) | |
| Healthcare Worker | Medical practitioner | 46 (3•5%) | 1 (0•32%) | 163 (0•87%) | 1 (0•71%) |
| Nurse | 54 (4•1%) | 11 (3•5%) | 1,272 (6•8%) | 1 (0•71%) | |
| Other Healthcare Workerb | 61 (4•6%) | 9 (2•8%) | 1,941 (10%) | 3 (2•1%) | |
| Not a healthcare worker but works in a healthcare setting | 1,161 (88%) | 293 (92%) | 14,942 (80%) | 113 (81%) | |
| Not stated or under investigation | 1 (0•08%) | 3 (0•95%) | 385 (2•1%) | 22 (16%) | |
| Ever hospitalizedc | Admitted to hospital | 169 (13%) | 24 (7•6%) | 2,295 (12%) | 6 (4•3%) |
| Not admitted | 1,154 (87%) | 293 (92%) | 16,408 (88%) | 134 (96%) | |
| Ever admitted to ICU | Admitted to ICU | 37 (2•8%) | 7 (2•2%) | 258 (1•4%) | 3 (2•1%) |
| Not admitted | 1,286 (97%) | 310 (98%) | 18,445 (99%) | 137 (98%) | |
| Ever ventilated | Received ventilation | 18 (1•4%) | 4 (1•3%) | 128 (0•68%) | 0 |
| Never ventilated | 1,305 (99%) | 313 (99%) | 18,575 (99%) | 140 (100%) | |
| Died | Alive | 1,305 (99%) | 316 (100%) | 17,901 (96%) | 140 (100%) |
| Died due to COVID-19 | 18 (1•4%) | 1 (0•32%) | 730 (3•9%) | 0 | |
| Died from other/unknown causes | 0 | 0 | 71 (0•38%) | 0 |
†Other healthcare workers include aged and disability care workers, allied health professionals (e•g• physiotherapists, podiatrists and occupational therapists), dental professionals, medical imaging professionals, paramedics, pharmacists and other healthcare professionals not classified as medical or nursing•
Other healthcare workers include aged and disability care workers, allied health professionals (e.g. physiotherapists, podiatrists and occupational therapists), dental professionals, medical imaging professionals, paramedics, pharmacists and other healthcare professionals not classified as medical or nursing.
Includes people transferred to hospital as part of aged care outbreaks management.
Phase I, 25 January – 9 April 2020
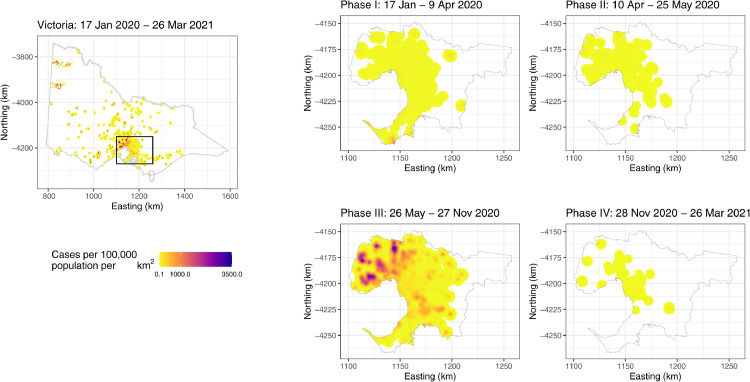
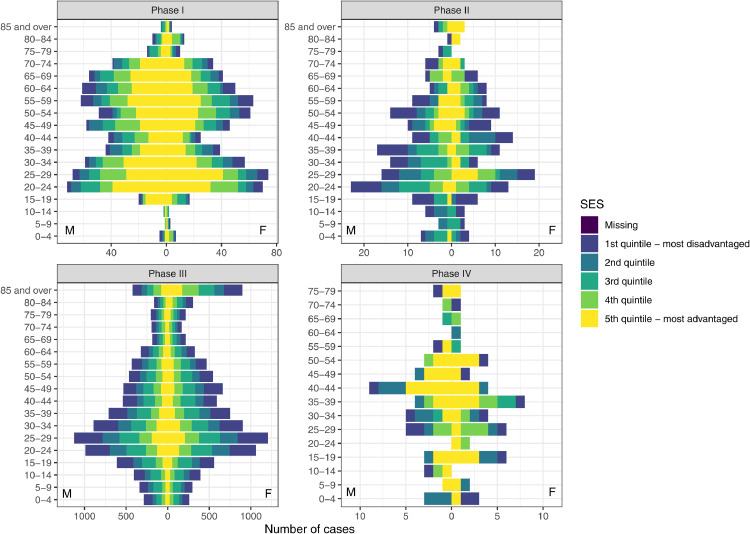
There were 1,323 cases notified during Phase 1 (Table 1), 787 (59•5%) of whom acquired infection overseas. Median age was 46 years (IQR: 29, 61), and there were slightly more males (52%) than females (48%). Most cases were Australian-born (63%) with 81% living in metropolitan Melbourne (Figure 3) and tended to be from areas of higher socioeconomic position (42% in highest quintile; Figure 4), consistent with the high number (60%) of returned travellers.
Figure 3.
Geographic distribution of COVID-19 incidence for Metropolitan Melbourne (cases per 100,000 population per square kilometre), by epidemic phase.
Note: Refer to the Supplementary information for a description of the calculation of incidence rates and mapping.
Figure 4.
The distribution of cases by age, sex and socio-economic position, by epidemic phase.
The median time from symptom onset to test was six days (IQR:3,9). Nearly all (98%) cases were symptomatic at testing, reflecting testing criteria at the time (Figure 1). Only 40% of locally-acquired cases were isolating when tested (216/536; Table 2). One-hundred and sixty-nine (13%) cases were hospitalised with a median age 62 years (IQR:51,71), and 53% were male. The threshold for hospitalisation was low, and not necessarily indicative of disease severity. The median length of stay was 6 days (IQR:3,13), 37 (2•8%) patients were admitted to ICU and 18 (1•4%) were ventilated. Eighteen deaths (1•4%) were recorded, 16 of which were among hospitalised cases. The median age at death was 79 years (IQR: 69-82y), and 61% were female.
Fifty-nine percent of infections were overseas-acquired, which is apparent in the genomic diversity of viruses recovered from cases [11]. Many of these cases were associated with cruise ship outbreaks (see Supplementary Table 1). The Australian Government incrementally implemented travel restrictions between January and March 2020, initially banning entry from selected countries, then requiring all returned travellers to self-isolate (18 March), banning entry for foreign nationals (20 March), and finally mandating 14-day hotel quarantine (28 March; Supplementary Figure 1). By the first week in April, the proportion of cases attributed to overseas travel reduced below 50% as overseas arrivals curtailed.
There were outbreaks of varying sizes in Phase I, largely associated with social gatherings, such as weddings, including one at a licenced venue that led to over 50 cases and seeded outbreaks in healthcare and education settings (Supplementary Table 1).
Various restrictions on movement and socialising were implemented from 23 March 2020 (Figure 2; Supplementary Figure 1). Stay-at home orders were issued with four exceptions: attending work (if unable to work from home) or school; care or caregiving; daily exercise; and buying food and other essentials. Many office buildings and all entertainment venues (indoor and outdoor), beauty and personal care outlets were closed. Schools closed a week early for holidays (24 April) and remained closed until 26 May, except for children of essential workers or vulnerable children. Religious ceremonies, including weddings and funerals, had strict guest limits, households were not allowed visitors and outdoor gatherings were also banned. Visitors to hospitals and aged care facilities were permitted under special circumstances only (e.g. birth support, end of life). Non-emergency and non-urgent surgeries were cancelled. Community compliance with restrictions was enforced by the Victorian police, authorised officers and the health and safety regulator, WorkSafe.
Phase II, 10 April – 25 May 2020
Although community transmission was minimised during Phase I it was not completely eliminated, and 317 new cases were reported over the ensuing 2 months; a rate of ∼7/day. During this period there was a notable shift in the demographic profile of cases towards younger age (median age 39 years; IQR: 24,52), and lower socio-economic status (Table 1, Figure 4). More than half of cases were born outside Australia. This shift in the demographic and risk profile was accompanied by several key outbreaks, including a large outbreak in a meat processing facility (Supplementary Table 1).
Testing “blitzes” were introduced. The first, 27 April to 12 May, set a then-ambitious target to test 100,000 people in a 2-week period, including screening of 1 in every 5 asymptomatic people presenting for testing. During the blitz there was a noticeable increase in turn-around times (Figure 1B), with associated delays to contact tracing. Compared with phase 1—and consistent with changes to testing criteria which increased screening of asymptomatic cases—a higher proportion of cases in Phase reported no symptoms at or prior to testing (26%), had no clear epidemiological link to a known case (19%), and were already isolating when tested (31% of cases, excluding those in hotel quarantine).
Hospital admissions were substantially reduced compared with Phase I with just 24 admissions (8% v 13% in phase 1), half of whom were women. The median age of hospitalised cases was 54 years (range:19-93y) and the median length of stay was 9•5 days (IQR: 6•5-18). Seven (2•2%) patients were admitted to ICU with 4 (1•3%) ventilated. There was one death (0•32%), a female in her 80s who died while hospitalised.
Restrictions eased during this period, beginning with increased allowances for elective surgeries in late April (Supplementary Figure 1). Small indoor and outdoor social gatherings were permitted from 13 May, and visitors were allowed back at hospitals and aged care facilities. Office workers were encouraged to continue to work from home.
Phase III, 26 May – 27 November 2020
Victoria's main epidemic, Phase III, was primarily associated with an outbreak in a hotel being used to quarantine SARS-CoV-2-positive returned travellers. The first case in this outbreak, a staff member at the hotel, was detected on 26 May 2020. A number of hotel staff, security guards and medical staff were infected. The outbreak among hotel staff and their close contacts was thought to have been contained. From June 8, however, a period of uninterrupted, daily increases in community cases commenced (effective reproductive number, Reff>1; Figure 2B). Ultimately, 99% of the viral samples recovered from cases during this phase clustered within the same genetic group linked to the hotel outbreak [12].
As this phase commenced (26 May), a staged return to school began, and from 9 June caps on indoor and outdoor gatherings, including weddings, funerals and religious services, increased. Restaurants and personal services were allowed to reopen. The easing of restrictions was accompanied by clusters associated with social gatherings and onwards transmission to schools and workplaces. School outbreaks were generally contained, with a median of fewer than 13 cases. However, a notable outbreak at a large school attended by children from across metropolitan Melbourne involved 209 cases in school children, families, and social contacts over seven weeks. This outbreak involved multiple introductions and interrelated communities; a complexity highly characteristic of Phase III.
Rising case numbers in particular suburbs triggered a testing blitz from 25 June to 4 July with 220,967 swabs collected from which 994 cases were detected (0•45%). Stay-at-home orders were issued in 10 postcodes from 1 July. Many cases were identified among residents in nine public housing towers, which prompted unprecedented measures, including public health orders to remain in place for a period of 14 days. Borders were closed to international arrivals on 7 July, and stay-at-home orders were re-implemented throughout Metropolitan Melbourne from 8 July, including the re-closing of schools. As case numbers rose, testing turn-around times and actioning of notifications slowed leading to delays in contact tracing (Figure 1B). Masks were made mandatory from 23 July and a State of Disaster was declared on 2 August, which coincided with additional restrictions including a 1-hour limit per person for outdoor exercise, one household member per day permitted to shop for groceries, an 8pm curfew, closure of child care centres (except for essential workers), and no indoor or outdoor gatherings permitted (Supplementary Figure 1). Essential workers required permits to travel to work. Travel for non-work-related reasons was not permitted beyond a 5km radius of home with permits required for travel between Metropolitan Melbourne and Regional Victoria, enforced by metropolitan checkpoints. Other Australian states and territories closed their borders to Victoria.
The median age of cases was 40 years (IQR:23,54), and more females (53%) than males were infected. A number of cases were essential workers, associated with outbreaks in manufacturing, logistics, meat processing, supermarket distribution, healthcare and aged care. Many essential workers were from culturally and linguistically diverse communities; 47% of all cases were born in non-English speaking countries and incidence was highest in people of low socio-economic position (Table 1; Figure 4). Responses to the challenges presented by essential workplaces included implementing plastic partitions between workstations, reducing the number of staff per shift, income support during isolation, and hotel accommodation for workers who could not isolate at home.
Outbreaks in the essential workforce were hardest felt in the aged care sector where there were 168 outbreaks, involving 647 resident deaths (see Supplementary Table 1). Hospitals and aged care were inextricably linked, with some aged care resident cases seeding outbreaks in hospitals and vice versa. There were 87 outbreaks in hospitals and healthcare, involving over 1,000 clinical staff, 73% of whom acquired infection in the workplace. Hospitals responded with interventions such as changes to personal protective equipment requirements, asymptomatic staff testing, review of ventilation and closure of some wards.
Owing to the high burden in aged care, this phase was characterised by high hospitalisation risk (HR) and case fatality risks (CFR); 84% of hospitalised cases and 81% of deaths were aged care residents. There were 2,295 cases admitted to hospitals (HR=12%), with median age 73 years (range: 0-103 years) and a majority female (54%); 258 (1•4%) received treatment in ICU and 128 (0•68%) were ventilated. The median length of stay was 13 days (IQR: 5-27). There were 730 deaths resulting from infections acquired during this Phase (CFR=3•9%), and a further 71 deaths among cases determined to be due to other causes. The median age at death was 88 years (range: 27-101 years), 53% were women, and 88% of deaths were hospitalised (hospitalised fatality risk (HFR)=22%).
Phase IV: 28 November to 26 March
Local elimination—28 days with 0 cases—was achieved on 27 November 2020. International flights resumed on 7 December 2020 and since that time SARS-CoV-2 cases have been predominantly identified in hotel quarantine. An outbreak seeded from a neighbouring state involving just 27 cases was swiftly suppressed in January 2021. A further outbreak seeded from hotel quarantine on 7 February was controlled under a 5-day reimplementation of Stage 4 restrictions from 13-18 February 2021. Local elimination was re-achieved on 26 March 2020.
COVID-19 vaccines were made available to frontline healthcare workers, hotel quarantine workers and aged care residents on 22 February. Progressive roll-out to other groups has been primarily managed thereafter under a framework guided by the Australian Government.
Discussion
Due to the comprehensive control measures implemented, Victoria's epidemic was small in comparison with many regions internationally. The overall attack rate of 3,023 per million at the end of 2020 was far less than the US (56,341/million), UK (33,232/million), and Canada (14,289 per million), but far more than some regional neighbours, including Thailand (86/million), Vietnam (15/million) and Fiji (51/million) [13]. There were 111 deaths per million, reflecting the high burden in residential aged care, despite the relatively small incidence, as has been documented internationally [14,15].
Our assessment of the epidemic phases experienced in Victoria has several strengths, chiefly the virtually complete capture of diagnosed cases and test results, arising from the coordinated, centralized public health response that occurred under an enforced legislative framework. In addition, there was enhanced data collection and data linkage to State-level hospitalization and death notifications to facilitate the recording of morbidity [6] and mortality impacts. However, data limitations included quality, usability, evolving definitions and modification of data collection practices. For example, the proportion of cases symptomatic at the time of testing should be interpreted in light of changes to testing criteria and the completeness of data collection at the height of Phase 3, when case interviews were shortened and symptoms data were not systematically collected, especially in some large outbreak settings, such as aged care and healthcare.
The epidemiological characteristics of Victoria's COVID-19 epidemics described here highlight the challenges with effective prevention and control of SARS-CoV-2, none of which are unique to our setting. There were some notable differences in the key epidemiological characteristics of Victoria's epidemic phases. There was a shift towards younger age groups: the highest cumulative incidence rates (adjusted for population size) in Phase I were in the 20-29y and 50-74y age groups, whereas the highest cumulative incidence rates in Phase III was in those aged 80+ (associated with aged care) and 18-29y (associated with essential workforces). Phase I (and later IV) was also characterised by overseas-acquired infection among cases of high socioeconomic position, whereas Phase III was characterised by locally-acquired infections among younger, socially-disadvantaged communities. During this Phase, proportionally more cases were from non-English speaking backgrounds.
Consistent with the increase in cases among culturally and linguistically diverse communities, Phase III was also characterised by a large number of transmission events occurring in essential workplaces such as manufacturing, meat processing, and aged care. The increase in cases occurring among older Victorians and those residing in aged care thus altered the clinical characteristics of Phase III to that of an epidemic with considerably higher morbidity and mortality burden compared to earlier epidemic Phases. These complexities necessitated several enhancements to public health prevention and control activities including: improved community engagement and testing among culturally and linguistically diverse communities, income support for those required to isolate, hotel accommodation for essential workers unable to safely isolate at home, enhanced testing and furloughing of healthcare staff and – for aged care residents – a lower threshold for hospitalisation to both minimise risk of transmission within the home as well as to manage clinical deterioration of individual cases.
The transition from older, wealthier cases to younger, socially-disadvantaged communities that was observed in Victoria was also a feature of early epidemics in Singapore, where infections among migrant workers living in dormitories dominated their epidemic in early 2020 [16,17]. High incidence and burden of disease in communities experiencing disadvantage has also been a feature of COVID-19 epidemics in the US [18] and UK [19]. People from culturally and linguistically diverse communities are overrepresented as workers in essential settings, such as aged care and abattoirs, underscoring the need to ensure that pandemic control measures are enacted without further entrenching disadvantage [20]. Meaningful engagement with higher exposure-risk communities is critical for ensuring future public health actions [21]. To that end, Victoria designed and implemented public health interventions that sought to engage authentically with diverse communities to maximize trust and cooperation and mitigate negative impacts [22].
The escape of SARS-CoV-2 from Victoria's hotel quarantine program at the start of Phase III also highlighted the challenges of this pandemic control strategy, which utilised facilities not built for such a purpose. The substantial onward transmission from hotel quarantine magnified the need for programmatic reform. Inquiries into the hotel quarantine program have since led to key risk mitigation measures including: improved governance and establishment of a single agency to manage that program (COVID-19 Quarantine Victoria), the employment of a full hierarchy of infection prevention and control measures including engineering controls to reduce the potential for aerosol transmission, and prioritised vaccination of hotel quarantine workers [23]. Returned travellers in hotel quarantine continued to be Australia's principal source of new SARS-CoV-2 outbreaks for the first half of 2021.
Conclusions
Victoria's experience serves as a cautionary tale, highlighting several challenges to COVID-19 control. First, the prevention of transmission in hotel settings not purpose-built for quarantine. Second, the requirement for public health interventions that authentically engage with diverse communities to support prevention and control efforts. Third, ensuring that testing rates remain high – even after suppression or elimination is achieved – to enable ongoing detection of new cases in support of rapid containment both in key at-risk communities as well as the population at large. In Victoria, these challenges were met in the context of a strategy that aimed for no community transmission. This required a delicate balance between ensuring that public health interventions were proportionate to the impact on society, including easing restrictions as soon as possible whilst also minimizing the risk of resurgence.
Australia has moved from a pandemic mitigation goal to an aggressive suppression goal, rapidly employing many of the aggressive containment strategies first implemented in Victoria, which have subsequently limited onward community spread in Adelaide, Brisbane, Perth and Melbourne. Although Victoria and the rest of Australia have largely continued to enjoy limited periods of restrictions, the risk of incursion remains. Control of outbreaks driven by the delta variant are proving to be particularly challenging and underscore the need for flexible re-implementation of public health interventions to ensure the health and wellbeing of residents.
Role of the Funding Source
No special funding was obtained for this study.
Data sharing
Data used can be requested from the Department of Health, Victoria. All R-Scripts used to summarise these data can be shared upon request.
Authors
Sheena G. Sullivan, COVID-19 Public Health Division, Department of Health, Victoria and WHO Collaborating Centre for Reference and Research on Influenza, Royal Melbourne Hospital, at the Peter Doherty Institute for Infection and Immunity, Victoria, Australia
Julia ML Brotherton, COVID-19 Public Health Division, Department of Health, Victoria and VCS Foundation, Victoria, Australia
Brigid M Lynch, COVID-19 Public Health Division, Department of Health, Victoria and Cancer Council Victoria, Australia
Allison Cheung, COVID-19 Public Health Division, Department of Health and Faculty of Veterinary and Agricultural Sciences, University of Melbourne, Victoria, Australia
Michael Lydeamore, Department of Infectious Diseases, The Alfred and Central Clinical School, Monash University, Victoria, Australia
Mark Stevenson, Faculty of Veterinary and Agricultural Sciences, University of Melbourne, Victoria, Australia
Simon Firestone, Faculty of Veterinary and Agricultural Sciences, University of Melbourne, Victoria, Australia
Jose Canevari, COVID-19 Public Health Division, Department of Health, Victoria, Australia
Huu Nghia Joey Nguyen, Department of Education and Training, Victoria, Australia
Kylie S. Carville, COVID-19 Public Health Division, Department of Health and Victorian Infectious Diseases Reference Laboratory, Victoria, Australia
Hazel J. Clothier, COVID-19 Public Health Division, Department of Health, Victoria, Australia
Jessie Goldsmith, COVID-19 Public Health Division, Department of Health, Victoria, Australia
Naveen Tenneti, COVID-19 Public Health Division, Department of Health, Victoria, Australia
Carrie Barnes, COVID-19 Public Health Division, Department of Health, Victoria, Australia
Nectaria Tzimourtas, COVID-19 Public Health Division, Department of Health, Victoria, Australia
Rebecca F. Gang, COVID-19 Public Health Division, Department of Health, Victoria, Australia
James Armstrong, Health Protection Branch, Department of Health, Victoria, Australia
Lucinda Franklin, Health Protection Branch, Department of Health, Victoria, Australia
Daneeta Hennessy, Health Protection Branch, Department of Health, Victoria, Australia
Kara Martin, Health Protection Branch, Department of Health, Victoria, Australia
Mohana Baptista, COVID-19 Public Health Division, Department of Health, Victoria, Australia
Michael Muleme, COVID-19 Public Health Division, Department of Health, Victoria, Australia
Aaron Osborne, North East Public Health Unit, Victoria, Australia
Charles Alpren, Western Public Health Unit, Victoria, Australia
Frances H. Ampt, Western Public Health Unit, Victoria, Australia
Natasha Castree, COVID-19 Public Health Division, Department of Health, Victoria, Australia
Andres Hernandez, COVID-19 Public Health Division, Department of Health, Victoria, Australia
Annaliese van Diemen, North East Public Health Unit, Victoria, Australia
Allen C. Cheng, COVID-19 Public Health Division, Department of Health, Victoria and Alfred Health, Victoria, Australia
Simon Crouch, South East Public Health Unit, Victoria, Australia
Kira Leeb, COVID-19 Public Health Division, Department of Health, Australia
Kate Matson, COVID-19 Public Health Division, Department of Health, Victoria, Australia
Finn Romanes, Western Public Health Unit, Victoria, Australia
Clare Looker, COVID-19 Public Health Division, Department of Health, Victoria, Australia
Evelyn Wong, COVID-19 Public Health Division, Department of Health, Victoria, Australia
Euan Wallace, COVID-19 Public Health Division, Department of Health, Victoria, Australia
Brett Sutton, COVID-19 Public Health Division, Department of Health, Victoria, Australia
Stacey L Rowe, COVID-19 Public Health Division, Department of Health, Victoria, Australia
Author contributions
SLR, CA and BS conceived the study; SLR developed the outline and BML and JMLB developed the first draft; SGS, AC, ML, MS, and SF performed data analyses, data visualisation and contributed relevant text for the Methods and Results; JMLB drafted the Introduction and Discussion; HNJN, KSC, HJC, JG contributed text specific to outbreaks and culturally and linguistically diverse communities; NTe, CB, NTz, RFG, FA, JA contributed sections on case identification, including testing, and case and contacts management; DH, KM, MM, RFG, AO, MB contributed to data curation. BS, AvD, SC, FR, CL, LF, CA, ACC, EvW provided administrative support and management that enabled this work; BS, CL, EvW, ACC, SC, KeM, KL, EuW, NT, FR provided content and/or advice on the overall development and direction of the manuscript; SGS managed submission and revisions. All authors read and provided feedback on the drafts and have read the submitted version.
Declaration of Competing Interest
None declared
Acknowledgments
We wish to thank the Victorian Infectious Diseases Reference Laboratory, the Microbiological Diagnostic Unit, and the Victorian Nosocomial Infections Surveillance Service (VICNISS) at the Peter Doherty Institute for Infection and Immunity for their contributions to ongoing COVID-19 surveillance efforts in Victoria. We also wish to thank the custodians of the Victorian Admitted Episode Dataset and the Victorian Death Index at the Department of Health, Victoria. Finally, we wish to thank the people of Victoria for their resilience throughout this pandemic.
Footnotes
Funding: None
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.lanwpc.2021.100297.
Appendix. Supplementary materials
References
- 1.Thevarajan I, Nguyen THO, Koutsakos M, Druce J, Caly L, van de Sandt CE. Breadth of concomitant immune responses prior to patient recovery: a case report of non-severe COVID-19. Nat Med. 2020;26(4):453–455. doi: 10.1038/s41591-020-0819-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Premier of Victoria. Emergency Relief Packages For Victorians Who Need It Most Melbourne: oGvernment of Victoria; 2020 [updated 22 March 2020. Available from: https://www.premier.vic.gov.au/emergency-relief-packages-victorians-who-need-it-most.
- 3.Government of Victoria. Supporting Victorian workers to get tested and stay home Melbourne: Government of Victoria; 2020 [updated 23 July 2020. Available from: https://www.dhhs.vic.gov.au/updates/coronavirus-covid-19/supporting-victorian-workers-get-tested-and-stay-home.
- 4.Mclean H, Huf B. Emergency Powers, Public Health and COVID-19 In: Parliamentary Library & Information Service PoV, editor. Research Paper No 2, August 2020 Melbourne: Government of Victoria; 2020.
- 5.Kojaku S, Hébert-Dufresne L, Mones E, Lehmann S, Ahn Y-Y. The effectiveness of backward contact tracing in networks. Nature Physics. 2021;17(5):652–658. doi: 10.1038/s41567-021-01187-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Curtis SJ, Cutcher Z, Brett JA, Burrell S, Richards MJ, Hennessy D. An evaluation of enhanced surveillance of hospitalised COVID-19 patients to inform the public health response in Victoria. Commun Dis Intell. 2018:44. doi: 10.33321/cdi.2020.44.98. 2020. [DOI] [PubMed] [Google Scholar]
- 7.Department of Environment L, Water and Planning. Victoria in Future: Population Projections 2016 to 2056. 2019.
- 8.Australian Bureau of Statistics . Australian Bureau of Statistics. Government of Australia; Canberra: 2018. 2071.0 - Census of Population and Housing: Reflecting Australia - Stories from the Census, 2016. editor. [Google Scholar]
- 9.Australian Bureau of Statistics. Socio-Economic Advantage and Disadvantage . Government of Australia; Canberra: 2018. Australian Bureau of Statistics. editor. [Google Scholar]
- 10.R Core Team . R Foundation for Statistical Computing; Vienna, Austria: 2021. R: A Language and Environment for Statistical Computing. [Google Scholar]
- 11.Seemann T, Lane CR, Sherry NL, Duchene S, Gonçalves da Silva A, Caly L. Tracking the COVID-19 pandemic in Australia using genomics. Nature Communications. 2020;11(1):4376. doi: 10.1038/s41467-020-18314-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.COVID-19 Hotel Quarantine Inquiry . Government of Victoria; Melbourne: 2020. Final Report and Recommendations. Volume I. In: (2018–2020) Ppn, editor. [Google Scholar]
- 13.World Health Organization. Weekly operational update on COVID-19 - 29 December 2020 Geneva: World Health Organization; 2020 [Available from: https://www.who.int/publications/m/item/weekly-epidemiological-update—29-december-2020.
- 14.Yanez ND, Weiss NS, Romand J-A, Treggiari MM. COVID-19 mortality risk for older men and women. BMC Public Health. 2020;20(1):1742. doi: 10.1186/s12889-020-09826-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Garg S, Kim L, Whitaker M, O'Halloran A, Cummings C, Holstein R. Hospitalization Rates and Characteristics of Patients Hospitalized with Laboratory-Confirmed Coronavirus Disease 2019 - COVID-NET, 14 States, March 1-30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(15):458–464. doi: 10.15585/mmwr.mm6915e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ngiam JN, Chew N, Tham SM, Beh DL-L, Lim ZY, Li TYW. Demographic shift in COVID-19 patients in Singapore from an aged, at-risk population to young migrant workers with reduced risk of severe disease. International Journal of Infectious Diseases. 2021;103:329–335. doi: 10.1016/j.ijid.2020.11.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Koh D. Migrant workers and COVID-19. Occupational and Environmental Medicine. 2020;77(9):634–636. doi: 10.1136/oemed-2020-106626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Islam N, Lacey B, Shabnam S, Erzurumluoglu AM, Dambha-Miller H, Chowell G. Social inequality and the syndemic of chronic disease and COVID-19: county-level analysis in the USA. Journal of Epidemiology and Community Health. 2021 doi: 10.1136/jech-2020-215626. jech-2020-215626. [DOI] [PubMed] [Google Scholar]
- 19.Public Health England . Epi cell ScaHIt. London: Public Health England; 2020. Disparities in the risk and outcomes of COVID-19. editor. [Google Scholar]
- 20.Reid A, Ronda-Perez E, Schenker MB. Migrant workers, essential work, and COVID-19. American Journal of Industrial Medicine. 2021;64(2):73–77. doi: 10.1002/ajim.23209. [DOI] [PubMed] [Google Scholar]
- 21.Wild A, Kunstler B, Goodwin D, Onyala S, Zhang L, Kufi M. Communicating COVID-19 health information to culturally and linguistically diverse communities: insights from a participatory research collaboration. Public health research & practice. 2021;31(1) doi: 10.17061/phrp3112105. [DOI] [PubMed] [Google Scholar]
- 22.Department of Health and Human Services. Contact_Tracing_2020__government_response 2020 [Available from: https://www.parliament.vic.gov.au/images/stories/committees/SCLSI/Inquiry_into_the_Victorian_Governments_COVID19_Contact_Tracing_System_and_Testing_Regime_/government_response/Contact_Tracing_2020__government_response.pdf.
- 23.Victorian Government. Victorian Government response to the Hotel Quarantine Inquiry 2021 [Available from: https://www.vic.gov.au/hotel-quarantine-inquiry-victorian-government-response.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.