Supplemental Digital Content is available in the text.
Keywords: coronavirus disease 2019, critical care, intensive care unit, modified Delphi consensus process, patient- and family-centered care, visitation
OBJECTIVES:
To create evidence-based consensus statements for restricted ICU visitation policies to support critically ill patients, families, and healthcare professionals during current and future pandemics.
DESIGN:
Three rounds of a remote modified Delphi consensus process.
SETTING:
Online survey and virtual polling from February 2, 2021, to April 8, 2021.
SUBJECTS:
Stakeholders (patients, families, clinicians, researchers, allied health professionals, decision-makers) admitted to or working in Canadian ICUs during the coronavirus disease 2019 pandemic.
MEASUREMENTS AND MAIN RESULTS:
During Round 1, key stakeholders used a 9-point Likert scale to rate experiences (1—not significant, 9—significant impact on patients, families, healthcare professionals, or patient- and family-centered care) and strategies (1—not essential, 9—essential recommendation for inclusion in the development of restricted visitation policies) and used a free-text box to capture experiences/strategies we may have missed. Consensus was achieved if the median score was 7–9 or 1–3. During Round 2, participants used a 9-point Likert scale to re-rate experiences/strategies that did not meet consensus during Round 1 (median score of 4–6) and rate new items identified in Round 1. During Rounds 2 and 3, participants ranked items that reached consensus by order of importance (relative to other related items and experiences) using a weighted ranking system (0–100 points). Participants prioritized 11 experiences (e.g., variability of family’s comfort with technology, healthcare professional moral distress) and developed 21 consensus statements (e.g., communicate policy changes to the hospital staff before the public, permit visitors at end-of-life regardless of coronavirus disease 2019 status, creating a clear definition for end-of-life) regarding restricted visitation policies.
CONCLUSIONS:
We have formulated evidence-informed consensus statements regarding restricted visitation policies informed by diverse stakeholders, which could enhance patient- and family-centered care during a pandemic.
Patient- and family-centered care (PFCC) is an essential component of high-quality critical care medicine (1). In response to the increasing number of patients with coronavirus disease 2019 (COVID-19) infection and limited knowledge regarding viral transmission, hospitals enacted strict visitation restrictions to mitigate potential spread of COVID-19 and preserve personal protective equipment (2–4). These restricted visitation policies prohibited the presence of family members for all hospitalized patients, including ICUs, with limited exceptions (e.g., end-of-life) (4).
Family members are key partners in PFCC, especially in the ICU (5). Family members act as surrogate decision-makers, advocate and communicate on behalf of an ICU patient, provide emotional support for patients (6, 7), and may participate in patient care activities (5, 8). Evidence suggests that family presence in the ICU may reduce the length of ICU stay (9) and reduces symptoms of anxiety in family members (10–12).
Research is emerging on the impact that this dramatic shift in visitation policies may have had on patients, families (13–16), and clinicians, including exacerbated family distress, increased length of ICU stay (17), and delayed decision-making about use of advanced life support for dying patients (17). Healthcare professionals were less often able to develop meaningful relationships with patients and families (18) and end-of-life discussions normally performed in person were often held virtually (16). There is no conclusive evidence that restricted visitation policies reduced transmission of COVID-19 (3), and evidence-informed policy is needed.
We undertook a program of research to identify the extent of visitor restrictions across Canada (4), describe the impact of restricted visitation on patients, families, and healthcare professionals (18), and review the relevant literature examining the impacts of restricted visitation (19). The aim of this study was to engage a diverse panel of stakeholders, including patients, families, and healthcare professionals, to reach consensus on key experiences of stakeholders impacted by COVID-19 restricted visitation policies and guidance on restricted visitation policies to support critically ill patients in the current and future pandemics.
MATERIALS AND METHODS
Selection of Key Stakeholders
Key stakeholders (patients, family members, physicians, registered nurses, physiotherapists, respiratory therapists, social workers, and decision-makers including managers, department heads, and medical officers of health) impacted or involved in the development and implementation of restricted visitation policies for Canadian ICUs were invited to participate. We aimed to have at least one stakeholder from each group and geographic representation from each Canadian province/territory. We purposively recruited healthcare professionals by contacting professional societies (Canadian Critical Care Society, Canadian Critical Care Trials Group, Canadian Association of Critical Care Nurses, Canadian Society of Respiratory Therapists). We recruited former ICU patients and family members, physicians, and nurses directly from our research program, and through nontraditional channels, including social media. Interested participants contacted the study team and were screened for eligibility (≥ 18 yr, English-speaking, able to consent).
Study Design
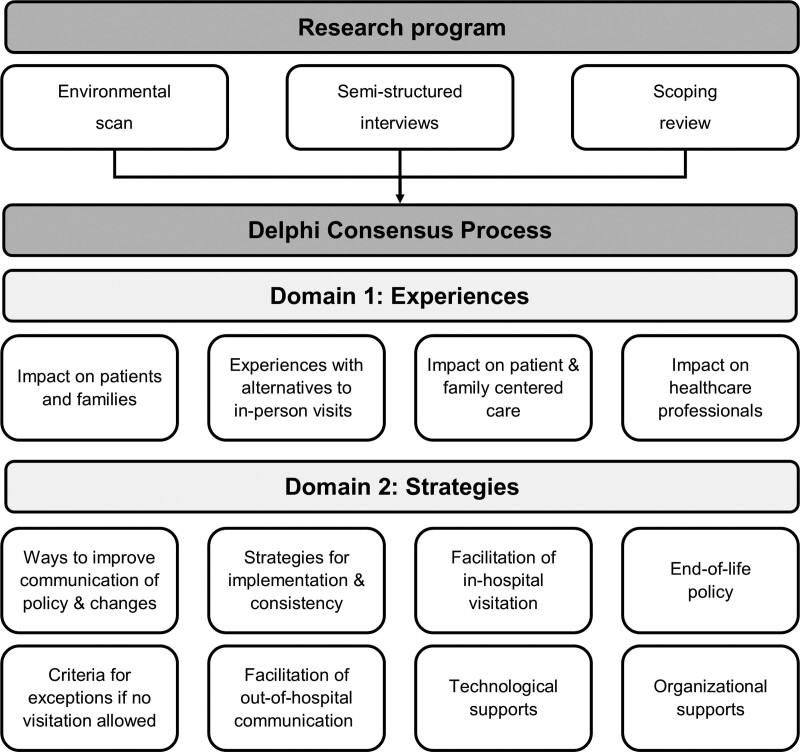
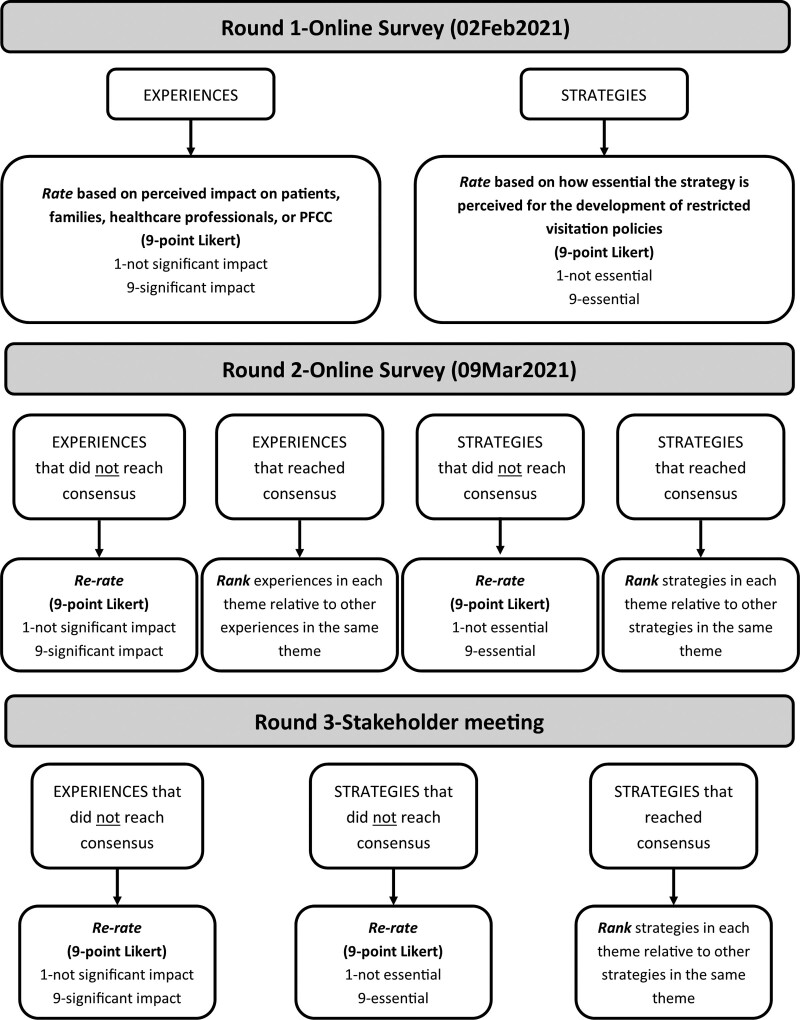
We conducted a modified Delphi consensus process that was informed by the RAND-UCLA appropriateness method (20) and followed the Conducting and REporting DElphi Studies reporting guidelines (21). Items informed by a scoping review, environmental scan of hospital policies, and semi-structured interviews were thematically analyzed to create 12 themes (Fig. 1) that were divided into two domains: 1) experiences related to restricted visitation during the COVID-19 pandemic (n = 50 items) and 2) strategies to mitigate the impact of restricted visitation during the COVID-19 pandemic (n = 104 items). Key stakeholders reviewed, “rated” (based on importance of individual items), and “ranked” (order of importance relative to other items in the same theme) key experiences (rating scale: 1—not significant, 9—significant impact on patients, families, healthcare professionals, or PFCC) and strategies (rating scale: 1—not essential, 9—essential recommendation for inclusion in the development of restricted visitation policies) on restricted visitation policies that were enacted during the COVID-19 pandemic. This involved three rounds of modified Delphi consensus voting. Round 1 and Round 2 were self-administered, using a secure and encrypted online platform (Qualtrics, Provo, UT). Round 3 was conducted during a two-day virtual National Stakeholder Meeting, using digital tools Vevox (vevox.com) and Mentimeter (mentimeter.com). The overall modified Delphi process is depicted in Figure 2, with details of each round included in Appendix 1 (http://links.lww.com/CCX/A825). All surveys were developed and pilot-tested by team members and patient partners to ensure that questions were appropriate, clear, and comprehensive (Appendix 2 and 3, http://links.lww.com/CCX/A825). In addition, members of the study team were available to answer participant questions. Participants provided informed consent prior to participating in the modified Delphi consensus process. The University of Calgary Conjoint Health Research Ethics Board approved this study (Ethics identification: REB20-0944).
Figure 1.
Overview of the components of the research program that informed the modified Delphi consensus process. The results of this research program were divided into two domains (i.e., experiences and strategies) and 12 themes. These domains and themes were used for all rounds of the modified Delphi process.
Figure 2.
Description of the three rounds of the modified Delphi consensus process, including steps to rate (based on importance of individual items) and rank (order of importance relative to other items in the same theme) experiences and strategies. PFCC = patient- and family-centered care.
Data Analysis
After Rounds 1 and 2, we emailed participants a summary of the results (i.e., their rating/ranking and the median score for each item). After Round 3, we summarized participant rankings. We determined consensus for any statement a priori as a median score of 1–3 (not significant/not essential) or 7–9 (significant/essential). An item was assessed to be a priority item if the item’s mean ranking was equal to or greater than one sd above the theme’s mean ranking. For example, if a theme had a mean of 20.0 and a sd of 3.3, items with a mean score greater than 23.3 were considered priority items. This strategy was used to equalize themes that had an unequal number of experiences or strategies. Analyses were conducted using Stata 14.1 (StataCorp, College Station, TX).
RESULTS
Modified Delphi Participant Characteristics
Participants of the modified Delphi consensus process represented 10 provinces/territories from nine stakeholder groups (Table 1). Ninety-four participants (100%) completed Round 1 and 77 (81.9%) completed Round 2.
TABLE 1.
Participant Characteristics of All Rounds of Modified Delphi Consensus Process (n = 94)
| Characteristic | Round 1 Delphi, n = 94 (%) | Round 3 Delphi, n = 45 (%) |
|---|---|---|
| Age category, yr | ||
| 20–29 | 7 (7.4) | 4 (8.9) |
| 30–39 | 28 (29.8) | 12 (26.7) |
| 40–49 | 31 (33.0) | 15 (33.3) |
| 50–59 | 21 (22.3) | 10 (22.2) |
| 60–69 | 7 (7.4) | 4 (8.9) |
| Sex | ||
| Female | 62 (66.0) | 25 (55.6) |
| Ethnic origina | ||
| North American | 56 (59.6) | 26 (57.8) |
| British Isles | 22 (23.4) | 12 (26.7) |
| Western European | 19 (20.2) | 9 (20.0) |
| East and Southeast Asian | 7 (7.4) | 4 (8.9) |
| South Asian | 5 (5.3) | 4 (8.9) |
| Eastern European | 4 (4.3) | 2 (4.4) |
| Northern European | 2 (2.1) | 1 (2.2) |
| Indigenous | 2 (2.1) | 1 (2.2) |
| Prefer not to answer | 2 (2.1) | 0 (0.0) |
| Southern European | 1 (1.1) | 0 (0.0) |
| Latin, Central, and South American | 1 (1.1) | 0 (0.0) |
| Ocean and Pacific Islands | 1 (1.1) | 1 (2.2) |
| Province | ||
| British Columbia | 2 (2.1) | 1 (2.2) |
| Alberta | 40 (42.6) | 20 (44.4) |
| Saskatchewan | 7 (7.4) | 3 (6.7) |
| Manitoba | 5 (5.3) | 2 (4.4) |
| Ontario | 25 (26.6) | 12 (26.7) |
| Quebec | 4 (4.3) | 3 (6.7) |
| Nova Scotia | 4 (4.3) | 2 (4.4) |
| New Brunswick | 3 (3.2) | 0 (0) |
| Newfoundland | 0 (0.0) | 0 (0) |
| Prince Edward Island | 3 (3.2) | 1 (2.2) |
| Territories (Northwest Territories, Nunavut, and Yukon) | 1 (1.1) | 1 (2.2) |
| Stakeholder groupa | ||
| Patient | 3 (3.2) | 3 (6.7) |
| Family membersb | 8 (8.5) | 2 (4.4) |
| Nurse | 27 (28.7) | 9 (20) |
| Physician | 28 (29.8) | 20 (44.4) |
| Researcher | 15 (16.0) | 8 (17.8) |
| Respiratory therapist | 12 (12.8) | 5 (11.1) |
| Social worker | 5 (5.3) | 1 (2.2) |
| Physiotherapist | 7 (7.4) | 3 (6.7) |
| Decision-maker | 12 (12.8) | 8 (17.8) |
| Other | 4 (4.3) | 0 (0.0) |
aParticipants self-selected their ethnic origin and stakeholder group. As such, responses are not mutually exclusive and add up to more than 100%.
bParticipants included family members of ICU survivors and nonsurvivors.
National Stakeholder Meeting Participant Characteristics
Forty-five participants (47.8%) (Table 1) attended the National Stakeholder Meeting, of which 36 (80%) completed Round 3 (day 1) and 30 (66.7%) completed Round 3 (day 2). Variation in participation was due to scheduling conflicts that did not align with the two, half-day National Stakeholder Meeting.
Modified Delphi Results
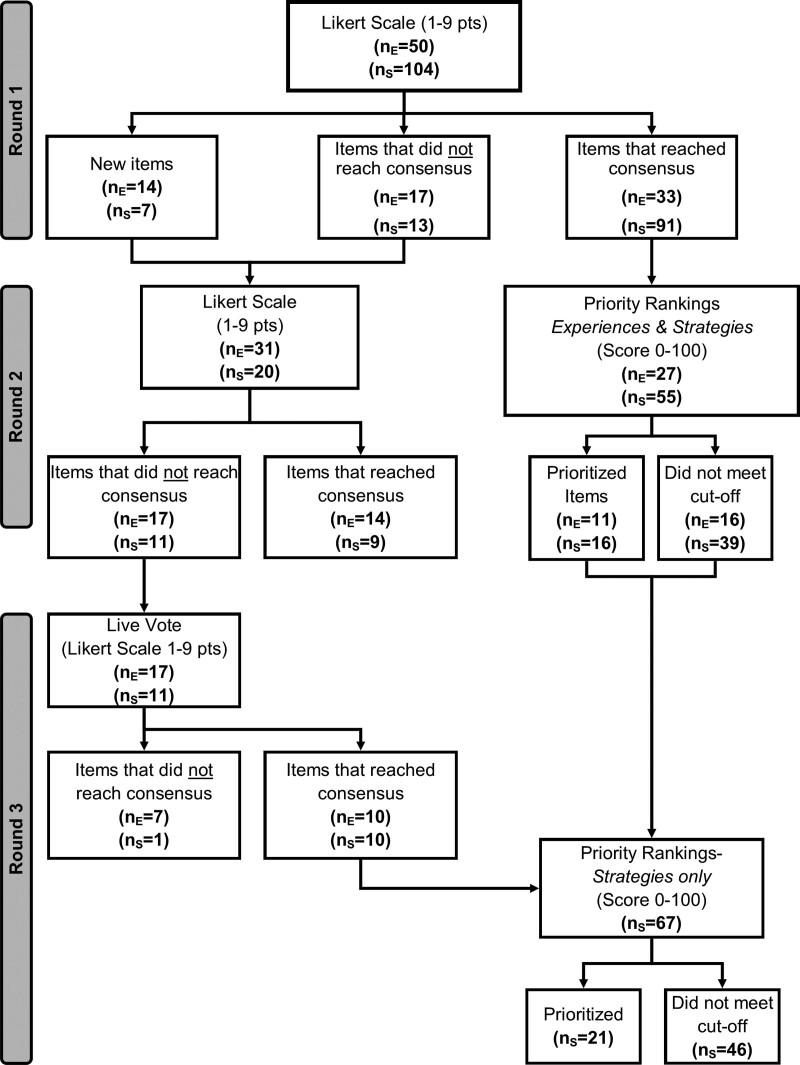
We provide the results from Rounds 1–3 in supplementary files (Supplementary Tables 1–6, http://links.lww.com/CCX/A825) and the overall results of Rounds 1–3 in Figure 3. Round 1 resulted in consensus for 124 of 154 items (80.5%) across the two domains. Round 2 included 51 items (30 did not reach consensus during Round 1 and 21 new items), of which 23 reached consensus (23/51; 45.1%). During priority ranking, 27 consensus items from Round 1 met the threshold and were considered a priority (Table 2). Round 3 (day 1 of the National Stakeholder Meeting) included the 28 items, of which 20 reached consensus (71.4%). Round 3 (day 2 of the National Stakeholder Meeting) included 67 items, of which 21 (31.3%) met the threshold and were considered priority items (Supplementary Table 1, http://links.lww.com/CCX/A825).
Figure 3.
Overview of the modified Delphi process for experiences (nE) and strategies (nS). Likert scale items must have a median between 1 and 3, or 7–9 to reach consensus. Priority ranked items had to have a mean score that was greater than the theme mean plus one sd to be considered priority.
TABLE 2.
Prioritized Experiences Identified in Round 2a
| Domain 1: ExperiencesPrioritized Experiences From Round 2 | Theme Mean (sd) | Item Mean (sd) |
|---|---|---|
| Theme 1: Impact on patients and their families during restricted visitation | ||
| Patients experienced isolation, loneliness or decreased interaction and connection with the healthcare team | 16.7 (2.7) | 23.2 (15.4) |
| Family absence at the end-of-life or did not visit before their loved one was sedated or intubated | 20.2 (12.6) | |
| Families did not understand how sick the patient was | 19.5 (11.8) | |
| Theme 2: Impact on patient- and family-centered care during restricted visitation | ||
| It was challenging to accurately convey the patient’s clinical status and appropriateness of care to families. It is important for family to understand treatment and therapy to be able to make appropriate choices | 16.7 (1.6) | 20.7 (12.4) |
| Family was not present to take part in key elements of patient care (e.g., physiotherapy), which may have impacted the health status of their loved one | 19.4 (10.8) | |
| Theme 3: Impact on healthcare professionals | ||
| Psychosocial impact to healthcare professionals due to moral distress (e.g., gatekeepers to family visitation, patients dying alone) and anxiety due to ever changing restricted visitation policies | 10.0 (0.9) | 14.4 (8.6) |
| Difficult to communicate rapidly changing visitation policies to family, or when communication about changes to visitation policies were distributed on weekends, evenings, or end of day on Friday | 12.7 (8.5) | |
| Healthcare professionals were conflicted between advocating against the policy (to prioritize patient well-being) and advocating for the policy (to protect the healthcare system) | 11.8 (8.5) | |
| Sense of tension and lack of trust among healthcare professionals and policy makers. This was often due to variation in the interpretation or application of restricted visitation policy details | 11.4 (6.7) | |
| Theme 4: Alternatives to in-person visitation | ||
| Clinical circumstances limited the capacity for patients to communicate or interact with families (e.g., patient who were intubated, patients who were proned, etc.) | 20.0 (2.8) | 27.9 (12.4) |
| Variability in patients, families, and healthcare professional’s comfort and access to technology for supported virtual communication | 23.7 (13.9) | |
aFor full list of item rankings in Round 2 (see Supplementary Table 5, http://links.lww.com/CCX/A825).
Domain 1: Stakeholder Experiences With Restricted Visitation
In Round 1, 33 items (33/50; 66%) related to stakeholder experiences with restricted visitation reached consensus (median = 7–9). These items were considered significant experiences and were ranked during Round 2. During Round 2, 11 (11/27; 40.7%) of these ranked items met the threshold for priority items (Table 2). Items focused on impacts to patients and families (3/11, 27.3%); healthcare professionals (4/11; 36.4%); PFCC (2/11; 18.2%); and experiences with alternatives to in-person visits (2/11; 18.2%).
Participants suggested 14 additional experiences during Round 1. Together with experience items that did not reach consensus during Round 1 (17/50; 34%; Supplementary Table 2, http://links.lww.com/CCX/A825), 31 items were re-rated during Round 2. Of these, 14 (14/31; 45.2%) were considered consensus items (median = 7–9). This included impacts to patients and families (3/14; 21.4%); healthcare professionals (5/14; 35.7%); PFCC (4/14; 28.6%); and experience with alternatives to in-person visits (2/14; 14.3%) (Supplementary Table 3, http://links.lww.com/CCX/A825). Seventeen items (17/31; 54.8%) did not reach consensus and were re-rated during Round 3 (Supplementary Table 4, http://links.lww.com/CCX/A825).
Domain 2: Strategies to Mitigate the Impact of Restricted Visitation Policies
In Round 1, 91 strategies to mitigate the impact of restricted visitation policies (91/104; 87.5%) reached consensus (median = 7–9) and, as such, were considered essential strategies that were ranked during Rounds 2 and 3. During the Round 2 ranking, 16 (16/91; 17.6%) of these strategies met the threshold to be considered a priority (Supplementary Table 5, http://links.lww.com/CCX/A825). These included ways to improve communication of restricted visitation policies/policy changes (2/16; 12.5%), strategies for policy implementation and consistency (3/16; 18.7%), strategies for facilitation of inhospital visitation (3/16; 18.7%), strategies to facilitate out-of-hospital visitation (2/16; 12.5%), end-of-life policy (1/16; 6.2%), criteria for exceptions (1/16; 6.2%), and for technological and organizational supports (1/16; 6.2% and 3/16; 18.7%, respectively).
Participants suggested seven additional strategies during Round 1. Together with the strategies that did not reach consensus during Round 1 (13/104; 12.5%), 20 items were re-rated during Round 2. Of these 20 items, 9 (9/20; 45%) had were considered essential (median = 7–9) strategies. All strategies that reached consensus during Rounds 1–3 were re-ranked during day 2 of the National Stakeholder Meeting (n = 67) (Supplementary Table 6, http://links.lww.com/CCX/A825). Of these 67 strategies, 21 (21/67; 31.3%) met the cutoff to be considered a priority (Supplementary Table 1, http://links.lww.com/CCX/A825). These included ways to improve communication of policies/policy changes (2/21; 9.5%), strategies for policy implementation and consistency (5/21; 23.8%), strategies for facilitation of in-hospital visitation (4/21, 19.0%), end-of-life policy (2/21; 9.5%), criteria for exceptions (2/21; 9.5%), facilitation of out-of-hospital visitation (3/21; 14.3%), technological supports (1/21; 4.8%), and organizational supports (2/21; 9.5%).
DISCUSSION
We engaged a national panel of stakeholders to determine consensus on two domains of ICU restricted visitation policies (experiences and strategies) during the COVID-19 pandemic. Participants prioritized 21 strategies that should be considered when developing, revising, or implementing restricted visitation policies. These strategies focused on the need for clear and consistent policy communication (e.g., during regular working hours) and implementation (e.g., implement a process for exceptions and appeals), facilitation of inhospital communication (e.g., implement a “visitor advisor”), out-of-hospital communication (e.g., designate family spokespersons), end-of-life (e.g., creating a clear definition for end-of-life) and offering of various supports (e.g., considering family members as integral part of the care team, increasing the number of technological devices, and clear messaging to the staff about visitation policies).
The impacts of restricted visitation policies on patients, families, and healthcare professionals identified by our group are consistent with existing data. Studies suggest that prior to the COVID-19 pandemic, some ICUs restricted the frequency or duration of family visits to the ICU (22–25). A recent study reported that family members in ICUs with restricted visiting policies (duration of visit of 1 hr/d) endorsed lower satisfaction with care and impact to family participation in care, compared with families from an ICU with open visitation policies (26). Restricted visitation has also been shown to have negative psychologic impacts on family members of critically ill patients (11), especially during end-of-life (27). A study on the psychologic impacts of the COVID-19 pandemic reported that critical care clinicians perceived that restricted visitation policies were associated with symptoms of anxiety and depression among patients and families (28) and moral distress in healthcare professionals (29). Similarly, in the current study, a panel of stakeholders prioritized items that described psychologic impacts of restricted visitation on patients (e.g., isolation, loneliness), families (e.g., not visiting loved ones before sedated or intubated), and healthcare professionals (e.g., moral distress).
Stakeholders prioritized several items that addressed the psychologic impacts of restricted visitation policies on opportunities to debrief with colleagues or access mental health supports for patients, families, and staff. Stakeholders also prioritized several items that may improve patient, family, and healthcare professional well-being such as videoconferencing options for family members and patients who are separated and provision of frequent medical updates. Recent studies demonstrate that families report successful remote communication (i.e., functional remote technology or staff that kept family informed) with the patient and healthcare team were associated with improved family end-of-life care experience (30, 31) and enhanced staff morale (32).
The value of remote communication is evident but there may be additional considerations. For example, psychologic distress was measured in family members who were identified as the designed spokesperson during the COVID-19 pandemic at admission, discharge, and 3-month follow-up. Family members who received communication only via phone or device (e.g., mobile phone or iPad) experienced negative psychologic outcomes (i.e., high prevalence of symptoms of anxiety and depression and post-traumatic stress disorder) (33). Stakeholders prioritized increased availability of teleconferencing devices but there are several challenges, such as coordinating device use (i.e., scheduling calls, holding devices for patients), and inaccessible virtual communication opportunities for marginalized populations. Although healthcare professionals value communicating with families, adding on the use of technology can be challenging and could require more time to negotiate by the healthcare worker or family member (34, 35). A teleconferencing initiative during the COVID-19 pandemic (Life Lines) that used simple, intuitive technology that functions independent of the hospital Wi-Fi, still encountered barriers, especially insufficient staff time to prepare virtual communication (32). Research is emerging on how best to implement video conferencing platforms into ICUs (36).
Our study has offers suggestions to manage communication when visitation restrictions are enacted. The current study and recent articles prioritize visitors to be permitted for end-of-life regardless of a patient’s COVID-19 status (35, 37). Most importantly, stakeholders emphasized the need for policies to create a clear for definition of end-of-life that balances the challenges of predicting end-of-life for clinicians, while respecting the needs of families to be at bedside at end-of-life or prior to discussions about end-of-life care. This includes broad policy that allows visitors to be present while the patient can interact (i.e., not comatose at end-of-life), which is imperative given that an important family experience identified was their absence at the end-of-life and inability to visit their loved one prior to sedation and intubation. Furthermore, though a patient may be at the end-of-life, the focus does not shift to end-of-life care until a plan is established with the family (who may not have been allowed to visit because patient was not designated to be at end-of-life and may not be aware of how ill the patient is). As such, enhanced clarity and communication is needed to prepare the family for when the patient is nearing end-of-life (even if death is not imminent). Policies that allow clinicians leniency when predicting end-of-life, while allowing families to be present during the end-of-life process and participate in end-of-life-care communication or ceremonies with their loved one may reduce negative effects such as increased symptoms of depression or anxiety or complicated grief (38, 39).
Strengths of our study include the engagement of a diverse group of stakeholders, including patients and family members, with a high response rate for each round, and rigorous methodology. In addition, stakeholders were recruited from 10 different Canadian provinces and territories that each had a different severe acute respiratory syndrome coronavirus 2 infection rate and COVID-19 policy response (i.e., variations in restricted visitation policies, government mitigation efforts) and, as such, each participant brought differing experiences and perspectives to this study. This study also has several limitations. First, the number of patients and families who participated was lower than that of healthcare professionals, which may contribute to sampling bias. However, several stakeholder groups were included in the modified Delphi Consensus process, thereby limiting the chance that any single group could have influenced the results in an impactful manner. The purpose of the current study was to prioritize evidence-informed consensus statements that should be further discussed and adapted to the local context with a diverse group of stakeholders. Second, as with any consensus process, priorities can vary widely. To address this limitation, we included stakeholders from the beginning, reviewed the COVID-19 literature, and included free-text boxes in each round to capture variations we may have missed. Third, the burden of COVID-19 cases varied across Canada. As such, items asking about specific experiences may not have been applicable to all stakeholder groups within each jurisdiction and may have impacted consensus rankings. Fourth, as with any remote survey, participant interpretation of items may have varied. To address this, we pilot-tested the survey with multiple team members and patient partners to mitigate points of uncertainty and provided participants an opportunity to discuss/reword during the National Stakeholder Meeting. Fifth, the study occurred before vaccinations were made available to the general public. With the vaccination rate increasing, existing consensus statements will need to be revisited and revised based on emerging evidence of risk and transmissibility to inform visitation policies that consider a visitor’s vaccination status. Sixth, the generalizability of these findings is limited to setting such as Canada where, pre-pandemic, most ICUs had open visitation (24 hr) (4) and, as such, may not be applicable to jurisdictions with restricted/limited visitation. Future work is needed to understand the barriers to the implementation and facilitators/barriers of adoption of these evidence-informed consensus statements and their sustained uptake during the current and future pandemics.
CONCLUSIONS
During the first wave of COVID-19 pandemic, hospitals enacted restricted visitation policies per public health policies. This study reports key impacts of restricted visitation policies: isolation of critically ill patients, family absence at the end-of-life, and moral distress among healthcare professionals. Key stakeholders prioritized evidence-informed consensus statements on how to best facilitate PFCC during a pandemic. These strategies include suggestions to improve communication and access to patients during end-of-life (while they can communicate) and developing a more consistent approach to communicating and enacting policy changes.
ACKNOWLEDGMENTS
We would like to thank Rebecca Brundin-Mather, Stephana J. Moss, Melanie Columbus, Emily Fitzgerald, Chloe M. de Grood, Regan King, Madison Leia, Sara Mizen, and Kara Plotnikoff for assisting with breakout sessions. This article underwent an internal peer review process with the Canadian Critical Care Trials Group, and we thank the helpful contributions made by Dr. Geeta Mehta and Dr. Kim Lewis.
Canadian Critical Care Trials Group: Kusum Menon (Vice-President/Chair-Elect), Vazquez Grande (Treasurer), Mark Duffet (Secretary), Jennifer Foster (Governance), Dominique Piquette (Career Development & Mentorship), Nicole Zytaruk (Scientific Meeting Planning), Sylvie Debigaré (Patient & Family Partnerships), Srinivas Murthy (Partnerships & International Collaborations), Danaë Tassy (Communication & Website), and Sangeeta Mehta (Equity, Diversity, and Inclusion).
Supplementary Material
Footnotes
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s website (http://journals.lww.com/ccejournal).
Dr. Fiest has full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Supported, in part, by a Coronavirus Disease 2019 Rapid Response Funding Grant to Dr. Fiest from the Canadian Institutes of Health Research.
The authors have disclosed that they do not have any potential conflicts of interest.
This work was performed at University of Calgary, Calgary, AB, Canada.
Contributor Information
Collaborators: Kusum Menon, Vazquez Grande, Mark Duffet, Jennifer Foster, Dominique Piquette, Nicole Zytaruk, Sylvie Debigaré, Srinivas Murthy, Danaë Tassy, and Sangeeta Mehta
REFERENCES
- 1.Davidson JE, Aslakson RA, Long AC, et al. Guidelines for family-centered care in the neonatal, pediatric, and adult ICU. Crit Care Med. 2017; 45:103–128 [DOI] [PubMed] [Google Scholar]
- 2.Andrist E, Clarke RG, Harding M. Paved with good intentions: Hospital visitation restrictions in the age of coronavirus disease 2019. Pediatr Crit Care Med. 2020; 21:e924–e926 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Munshi L, Evans G, Razak F. The case for relaxing no-visitor policies in hospitals during the ongoing COVID-19 pandemic. CMAJ. 2021; 193:E135–E137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fiest K, Krewulak K, Hiploylee C, et al. An environmental scan of visitation policies in Canadian ICUs during the first wave of the COVID-19 pandemic. Can J Anaesth. 2021; 68:1474–1484 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hammond F. Involving families in care within the intensive care environment: A descriptive survey. Intensive Crit Care Nurs. 1995; 11:256–264 [DOI] [PubMed] [Google Scholar]
- 6.Jackson JC, Mitchell N, Hopkins RO. Cognitive functioning, mental health, and quality of life in ICU survivors: An overview. Crit Care Clin. 2009; 25:615–628, x [DOI] [PubMed] [Google Scholar]
- 7.Tate JA, Devito Dabbs A, Hoffman LA, et al. Anxiety and agitation in mechanically ventilated patients. Qual Health Res. 2012; 22:157–173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Olding M, McMillan SE, Reeves S, et al. Patient and family involvement in adult critical and intensive care settings: A scoping review. Health Expect. 2016; 19:1183–1202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Segers E, Ockhuijsen H, Baarendse P, et al. The impact of family centred care interventions in a neonatal or paediatric intensive care unit on parents’ satisfaction and length of stay: A systematic review. Intensive Crit Care Nurs. 2019; 50:63–70 [DOI] [PubMed] [Google Scholar]
- 10.Kamali SH, Imanipour M, Emamzadeh Ghasemi HS, et al. Effect of programmed family presence in coronary care units on patients’ and families’ anxiety. J Caring Sci. 2020; 9:104–112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rosa RG, Falavigna M, da Silva DB, et al. ; ICU Visits Study Group Investigators and the Brazilian Research in Intensive Care Network (BRICNet). Effect of flexible family visitation on delirium among patients in the intensive care unit: The ICU visits randomized clinical trial. JAMA. 2019; 322:216–228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fumis RR, Ranzani OT, Faria PP, et al. Anxiety, depression, and satisfaction in close relatives of patients in an open visiting policy intensive care unit in Brazil. J Crit Care. 2015; 30:440.e1–e6 [DOI] [PubMed] [Google Scholar]
- 13.Hwang DY, Zhang Q, Andrews A, et al. The initial impact of the coronavirus disease 2019 pandemic on ICU family engagement: Lessons learned from a collaborative of 27 ICUs. Crit Care Explor. 2021; 3:e0401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hart JL, Turnbull AE, Oppenheim IM, et al. Family-centered care during the COVID-19 era. J Pain Symptom Manage. 2020; 60:e93–e97 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen C, Wittenberg E, Sullivan SS, et al. The experiences of family members of ventilated COVID-19 patients in the intensive care unit: A qualitative study. Am J Hosp Palliat Care. 2021; 38:869–876 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cook DJ, Takaoka A, Hoad N, et al. Clinician perspectives on caring for dying patients during the pandemic: A mixed-methods study. Ann Intern Med. 2021; 174:493–500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Azad TD, Al-Kawaz MN, Turnbull AE, et al. Coronavirus disease 2019 policy restricting family presence may have delayed end-of-life decisions for critically ill patients. Crit Care Med. 2021; 49:e1037–e1039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fiest KM, Krewulak KD, Jaworska N, et al. Impact of restricted visitation policies during COVID-19 on critically ill adults, their families, critical care clinicians, and decision-makers: A qualitative interview study. CMAJ. 2021. Under review [Google Scholar]
- 19.Moss SJ, Krewulak KD, Stelfox HT, et al. Restricted visitation policies in acute care settings during the COVID-19 pandemic: A scoping review. Crit Care. 2021; 25:347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fitch K, Bernstein SJ, Aguilar MD, et al. The RAND/UCLA Appropriateness Method User’s Manual: RAND Corporation. 2001 Available at: https://www.rand.org/content/dam/rand/pubs/monograph_reports/2011/MR1269.pdf. Accessed November 4, 2020
- 21.Jünger S, Payne SA, Brine J, et al. Guidance on Conducting and REporting DElphi Studies (CREDES) in palliative care: Recommendations based on a methodological systematic review. Palliat Med. 2017; 31:684–706 [DOI] [PubMed] [Google Scholar]
- 22.Liu V, Read JL, Scruth E, et al. Visitation policies and practices in US ICUs. Crit Care. 2013; 17:R71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Garrouste-Orgeas M, Vinatier I, Tabah A, et al. Reappraisal of visiting policies and procedures of patient’s family information in 188 French ICUs: A report of the Outcomerea Research Group. Ann Intensive Care. 2016; 6:82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Giannini A, Miccinesi G, Leoncino S. Visiting policies in Italian intensive care units: A nationwide survey. Intensive Care Med. 2008; 34:1256–1262 [DOI] [PubMed] [Google Scholar]
- 25.Tabah A, Ramanan M, Bailey RL, et al. Family visitation policies, facilities, and support in Australia and New Zealand intensive care units: A multicentre, registry-linked survey. Aust Crit Care. 2021. Aug 2. [online ahead of print] [DOI] [PubMed] [Google Scholar]
- 26.Rodriguez-Ruiz E, Campelo-Izquierdo M, Estany-Gestal A, et al. Impact of different visiting policies on family satisfaction in two Spanish ICUs before and during COVID-19. Intensive Care Med. 2021; 47:1165–1166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tang ST, Huang CC, Hu TH, et al. End-of-life-care quality in ICUs is associated with family surrogates’ severe anxiety and depressive symptoms during their first 6 months of bereavement. Crit Care Med. 2021; 49:27–37 [DOI] [PubMed] [Google Scholar]
- 28.Azoulay E, Cariou A, Bruneel F, et al. Symptoms of anxiety, depression, and peritraumatic dissociation in critical care clinicians managing patients with COVID-19. A cross-sectional study. Am J Respir Crit Care Med. 2020; 202:1388–1398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Maaskant JM, Jongerden IP, Bik J, et al. ; FAM-Corona Group. Strict isolation requires a different approach to the family of hospitalised patients with COVID-19: A rapid qualitative study. Int J Nurs Stud. 2021; 117:103858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ersek M, Smith D, Griffin H, et al. End-of-life care in the time of COVID-19: Communication matters more than ever. J Pain Symptom Manage. 2021; 62:30975–30971 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Feder S, Smith D, Griffin H, et al. “Why Couldn’t I Go in To See Him?” Bereaved families’ perceptions of end-of-life communication during COVID-19. J Am Geriatr Soc. 2021; 69:587–592 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rose L, Yu L, Casey J, et al. Communication and virtual visiting for families of patients in intensive care during COVID-19: A UK National Survey. Ann Am Thorac Soc. 2021; 18:1685–1692 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cattelan J, Castellano S, Merdji H, et al. Psychological effects of remote-only communication among reference persons of ICU patients during COVID-19 pandemic. J Intensive Care. 2021; 9:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Eccleston C, Blyth FM, Dear BF, et al. Managing patients with chronic pain during the COVID-19 outbreak: Considerations for the rapid introduction of remotely supported (eHealth) pain management services. Pain. 2020; 161:889–893 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ritchey KC, Foy A, McArdel E, et al. Reinventing palliative care delivery in the era of COVID-19: How telemedicine can support end of life care. Am J Hosp Palliat Care. 2020; 37:992–997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Thomas KAS, O’Brien BF, Fryday AT, et al. Developing an innovative system of open and flexible, patient-family-centered, virtual visiting in ICU during the COVID-19 pandemic: A collaboration of staff, patients, families, and technology companies. J Intensive Care Med. 2021; 36:1130–1140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mistraletti G, Giannini A, Gristina G, et al. Why and how to open intensive care units to family visits during the pandemic. Crit Care. 2021; 25:191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Otani H, Yoshida S, Morita T, et al. Meaningful communication before death, but not present at the time of death itself, is associated with better outcomes on measures of depression and complicated grief among bereaved family members of cancer patients. J Pain Symptom Manage. 2017; 54:273–279 [DOI] [PubMed] [Google Scholar]
- 39.Gesi C, Carmassi C, Cerveri G, et al. Complicated grief: What to expect after the coronavirus pandemic. Front Psychiatry. 2020; 11:489. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.