Abstract
Background:
Phalangeal and metacarpal fractures are the second and third most common upper extremity fractures after distal radius fractures with varying methods of fixation techniques. Intramedullary screw fixation is an increasingly preferred method of fixation. Benefits include early range of motion, faster recovery, limited dissection, and reduced complications. Improper technique, which is readily avoidable, can lead to suboptimal results.
Methods:
A review of recent literature on current techniques aims to summarize the biomechanics of intramedullary screw fixation and outline appropriate technique of placing headless compression screws for metacarpal and phalangeal fractures.
Results:
We discuss through images and videos the indications, preoperative workup, and technical pearls and pitfalls to encourage surgeons to add this technique to their armamentarium and improve outcomes.
Conclusions:
intrameduallry screw fixation is a powerful option for metacarpal and phalanx fixation that allows rigid stability, enabling early return of function with excellent rates of union and total active motion. With knowledge of technical pearls presented in this article, common mistakes can be avoided to improve efficiency of screw placement and optimize patient outcomes.
Takeaways
Question: What techniques, pearls, and pitfalls do surgeons need to follow for best outcomes and to avoid complications?
Findings: Intramedullary screw fixation is a powerful option for metacarpal and phalanx fixation that allows rigid stability, enabling early joint range of motion, faster return of function with excellent rates of union, and minimal complications. With knowledge of technical pearls presented in this article and its supplementary videos, common mistakes can be avoided to improve efficiency of screw placement and optimize patient outcomes.
Meaning: Intramedullary screw fixation is an increasingly preferred method of fixation that requires attention to techniques summarized in this article for best results.
INTRODUCTION
Phalangeal and metacarpal fractures are the second and third most common upper extremity fractures after fractures of the distal radius.1–4 For fractures of the proximal phalanx and metacarpal, no method of fixation has been determined to be superior to another. Plate fixation is able to provide reduction and stability for early range of motion with mixed clinical results.5–7 Reported complications requiring surgical intervention include stiffness, proximal interphalangeal joint fixed flexion contracture, and extensor lag.5,6 There are minimally invasive techniques, including the use of K-wires, lag screws, cerclage wiring, and external fixation that limit soft tissue dissection. These options have drawbacks of malunion, nonunion, infection, need for hardware removal, and stiffness.8–10
Intramedullary screw fixation (IMF) is an emerging alternative to K-wire or plate fixation in treating displaced and unstable phalangeal and metacarpal fractures. The goal of reconstruction is to provide rigid fixation that can support early range of motion. IMF is a fixation option that offers rigid stability, early active range of motion, and simplicity of insertion. Due to the minimally invasive nature of this technique, patients experience better outcomes in terms of range of motion, earlier return to work, and minimal complications. Pinal et al demonstrate complete fracture healing in 69 patients, mean total active motion of 247 degrees and full return to activity at an average of 76 days.11 The purpose of this study was to review intermedullary screw fixation of metacarpal and phalanx fractures while summarizing the pearls and pitfalls to maximize successful surgical outcomes.
BIOMECHANICAL PROPERTIES
IMF biomechanical properties are well described in orthopedic literature as load-sharing devices.12 Initially, the majority of load and anatomic alignment across fracture is supported by the screw, but as the fracture heals, the load is transferred to the bone. Two forces that need to be adequately addressed are bending and torsional forces during MCP or PIP joint flexion. In biomechanical studies, the surface area of bone resisting bending is a function of using a screw wide enough to engage the intramedullary cortical bone with good purchase, while avoiding blow out, and utilizing the longest allowable screw length on each side of the fracture. As the width of the nail increases, there is more bone-to-nail friction, thereby making the fixation more resistant to both bending and torsional forces.13
Metacarpal and phalanx fractures have low rates of nonunion regardless of fixation technique.14–19 Although most intramedullary screw fixation devices rely on variable pitch threads to achieve compression, in these types of fractures, compression is not mandatory for successful healing. This is in stark contrast to scaphoid fractures that rely on compression of the fracture site for optimal healing.20 Fixation can be achieved with a variety of screw designs, including variable pitch fully threaded, variable pitch partially threaded, and consistent pitch fully threaded. The consistent screw pitch avoids compression, allowing fractures which otherwise tend to be over-compressed to be more reliably treated (eg, long, oblique, or comminuted fractures of the metacarpal).
INDICATIONS
This technique is ideal for patients needing swift return to activity with minimal to no need for splinting. Although occupational therapy is always recommended for patients undergoing fracture fixation, this fixation method is strong enough to support early range of motion in patients who may be reticent or unable to attend hand therapy. This provides an opportunity to avoid the stiffness that may be associated with more traditional methods of fixation, such as K-wires that require prolonged immobilization. In patients at a high risk of loss to follow-up or noncompliance, this technique prevents prolonged K-wire fixation, potential tract infection, and self-removal of wires.
In general, IMF is indicated in metacarpal and phalanx fractures that are displaced and unstable. In metacarpal shaft fractures, transverse and short oblique patterns (less than two times the shaft diameter) are reasonable indications. The surgeon must note the potential for minimal fracture segment displacement with the compressive mechanism of compression screws, albeit generally well tolerated from a clinical standpoint. Other indications include those situations where early range of motion is advisable and potentially mandatory, multiple metacarpal shaft fractures, open fracture with severe soft tissue injury, and osteotomies.
ABSOLUTE/RELATIVE CONTRAINDICATIONS
Due to the compressive mechanism associated with compression screws, long oblique fractures (greater than two times the shaft diameter) are at risk of fracture displacement and shortening. Comminuted fractures are also at risk for shortening and over compression when treated with Intramedullary (IM) compression screws, and a number of complex configurations (eg, fragment lag screw) have been developed to countermand this issue.12 These relative contraindications can be potentially countermanded by use of nonvariable pitch screws because there is no compressive or shortening mechanism.20,21 Metacarpal fractures of the proximal one-third make passing distal screw thread past fracture difficult. However, Hoang et al describe using an anterograde approach to fixate these fractures.22
Head-splitting fractures are avoided due to risk in worsening fracture with placement of screw. Lastly, infection and pediatric fractures with open physis are absolute contraindications to IMF.12
PREOPERATIVE PLANNING
Standard history and physical should include handedness, occupation, physical examination, including rotation and shortening, and chronicity of fracture. Radiograph evaluation is important to note comminution, location of fracture, and fracture pattern (transverse, short oblique, long oblique, and butterfly segments).
The full width of the bone and the narrowest width of medullary canal isthmus should be measured. The surgeon should be mindful that each metacarpal has consistent differences in width, as the ring finger has the narrowest isthmus at an average of 2.6 mm and small finger largest at 3.6 mm.23,24 The narrowest canal width in metacarpal bones should be measured in the PA view, and narrowest canal width of the phalanx is measured on the lateral radiograph. The width of the narrowest part of the isthmus is the most important factor to guide the choice of the appropriately sized screw to ensure contact between screw and bone without causing blow out. General guidelines are outlined below with preference for wider diameter screw after canal reaming (Table 1). Screw length is recommended to be 4–6 mm shorter than full bone length (Fig. 1).
Table 1.
HCS Diameter General Recommendations
| Index and middle metacarpal | 3.5–4.0 mm |
| Ring metacarpal | 2.5–3.0 mm |
| Small metacarpal | 3.5–4.5 mm |
| Proximal phalanx | 2.5–3.0 mm |
Fig. 1.
A, Proximal phalanx fracture is measured on lateral radiograph. An isthmus of 2.5 mm (yellow) and length of 43 mm (red). B, A 38-mm Synthes screw of 2.5-mm diameter is chosen and superimposed with immediate intraoperative fluoroscopic imaging on lateral view.
OPERATIVE TECHNIQUE FOR METACARPAL FRACTURES
Retrograde Placement
The operation is performed under regional block with sedation, under general anesthesia, or using wide awake local anesthetic no tourniquet techniques. After preparation, attempts at closed reduction under fluoroscopy are performed. If rapid reduction cannot be obtained in a closed manner, then an open reduction is performed. A 1.5-cm transverse incision is made dorsally over the metacarpal head and neck with #15 blade. Dissection is carried to the extensor apparatus and the extensor tendon split longitudinally, exposing the metacarpal head. Percutaneous considerations are addressed below. Before driving the guide wire, the appropriately sized screw is overlaid over the bone, and fluoroscopy is used to confirm appropriate sizing. This includes the appropriate width and length. Then, the appropriate guide wire is selected and driven into the dorsal one-third of metacarpal head and advanced retrograde to the level of fracture under fluoroscopic guidance. The fracture is then reduced, confirmed under fluoroscopy, and the K-wire is advanced across the fracture site to base of metacarpal. The flexion cascade is evaluated, and time is spent in assuring correction of any malrotation. Measurements of the K-wire are performed, and 4–6 mm are generally subtracted to get final screw length (for partially threaded screws, measurements must accommodate for the distal threads to be placed past the fracture line). The K-wire is then advanced through the carpometacarpal joint to avoid inadvertent removal when reaming over the wire. The metacarpal is drilled just past the fracture site while ensuring the narrowest part of the canal is reamed to accommodate the screw threads. A countersink is used to ensure screw head will be seated subchondral bone. To prevent rotational deformity during screw placement, the fingers are all flexed into the palm to set the appropriate flexion cascade and prevent malrotation. (See Video 1 [online], which displays the fifth metacarpal transverse fracture technique. Digits are flexed into palm during screw insertion to prevent malrotation, especially when proximal screw head engages.)
Video 1. Video 1 from “Intra-medullary Screw Fixation Comprehensive Technique Guide for Metacarpal and Phalanx Fractures: Pearls, and Pitfalls.” This video which demonstrates the 5th metacarpal transverse fracture technique. Digits are flexed into palm during screw insertion to prevent malrotation, especially when proximal screw head engages.
The screw is then hand driven with the fingers flexed. The screw should engage the canal with good purchase as the threads of the screw engage the intramedullary cortical bone and should be buried just beneath the subchondral bone. The surgeon should confirm screw placement under fluoroscopy and again check for malrotation. The guidewire is then removed. Extensor tendon and skin are closed. A bulky soft dressing is placed immediately postoperative and removed between 3 and 5 days for early range of motion to begin. There is no need for rigid immobilization if good purchase is achieved. The patient is expected to reach full range of motion by 4 weeks, and start strengthening and progressively heavier activities at 4–8 weeks. Unlimited unrestricted usage is recommended by 8 weeks.
OPERATIVE TECHNIQUE FOR PHALANGEAL FRACTURES
Proximal Phalanx Anterograde Intra-articular Placement
The operation is performed under regional block with sedation, under general anesthesia, or using wide awake local anesthetic no tourniquet techniques. (See Video 2 [online], which displays the small finger proximal phalanx placement of 2.5-mm screw under wide awake local anesthetic no tourniquet techniques).
Video 2. Video 2 from “Intra-medullary Screw Fixation Comprehensive Technique Guide for Metacarpal and Phalanx Fractures: Pearls, and Pitfalls.” This video which demonstrates the small finger proximal phalanx placement of 2.5 mm screw under wide awake local anesthetic no tourniquet techniques.
Attempts at closed reduction under fluoroscopy are performed. If rapid reduction cannot be obtained in a closed manner, then a limited open reduction is performed. The narrowest portion of the intramedullary canal helps determine the size of the screw. Both trans-articular and intra-articular approaches have been described, with our preference for single screw with intra-articular placement.25 Of note, the use of two anterograde screws has been shown as a viable option for proximal phalanx fracture fixation. In a limited series, two screws showed improved rotational stability compared with single screw.26
After closed reduction under fluoroscopy, a small transverse incision of no more than 0.5 cm in length is made over the metacarpophalangeal (MP) joint, which is then flexed 60–75 degrees while the proximal end of the phalanx is translated dorsally to expose articular surface of proximal phalanx base. Before driving the guide wire, the appropriately sized screw is overlaid over the bone, and fluoroscopy is used to confirm appropriate sizing. This includes the appropriate width and length. Under fluoroscopic control, insert the appropriate guidewire dorsally through the flexed MCP joint into the center of the proximal phalanx base in the longitudinal axis. Advance the wire into distal cortex to avoid inadvertent removal of wire during reaming. Drill the phalanx just past the fracture site. To ensure an absence of rotational deformity during screw placement, flex all fingers into the palm to set the appropriate flexion cascade and prevent malrotation. A 2.5–3.0 mm screw is then hand driven under direct visualization with the fingers flexed. Patients are placed into a soft dressing if stable fixation is achieved and start hand therapy within 3–5 days.
PEARLS AND PITFALLS
Concern for Articular Cartilage Disruption
Several studies have looked at the size of articular defects from placement of intramedullary screws. Ten Berg performed three-dimensional CT quantitative analysis looking at retrograde 2.4 mm and 3.0 mm headless compression screw (HCS) fixation of metacarpal fractures to determine the extent of articular cartilage violation in 32 metacarpals.27 They compared the metacarpal head articular and screw insertion hole surface area. The screw articular defect over the dorsal central aspect of the joint surface makes contact with only the base of the proximal phalanx during joint hyperextension due to the intrinsic shape of MC head and dorsal entry point of HCS. The phalangeal base does not engage the entry site for 95%–96% of the 120-degree sagittal arc. These data demonstrate that the screw surface defect that contacts the proximal phalanx base in range of motion is minimal. Furthermore, headless compression screw is the gold standard for treating scaphoid fractures, a bone that has 80% articular surface.28 Although there is no literature analyzing scaphoid articular defect, screws are placed without concern for cartilage violation. Overall, the concern for articular cartilaginous disruption appears to be largely theoretical.
Percutaneous Placement
Considerations can be given to a true percutaneous technique when taking into consideration the potential for injury to the extensor mechanism. Urbanschitz et al demonstrated an avoidance of extensor tendon injury with open technique when compared with percutaneous in both metacarpal and phalangeal fractures.29 Upon dissection analysis of tendon, there was significantly less damage in the open technique (P < 0.001) due to direct tendon visualization and protection. The authors also found a higher incidence of tendon injury in fixating phalanges compared with metacarpal regardless of anterograde or retrograde percutaneous technique. However, it is critical to note that ALL recorded tendon injuries were less than 50% of the entirety of the tendon. As classic teaching follows that no acute surgical treatment is indicated in extensor tendon injuries less than 50% tendon diameter,30 the damage to the extensor tendon during percutaneous techniques may not actually be clinically relevant. To determine whether open or percutaneous technique is superior in outcomes, further clinical comparison is needed. In vitro studies have shown that extensor tendon rupture after drill injury is rare, and even lacerations of up to 75% may not fail under physiological load.31
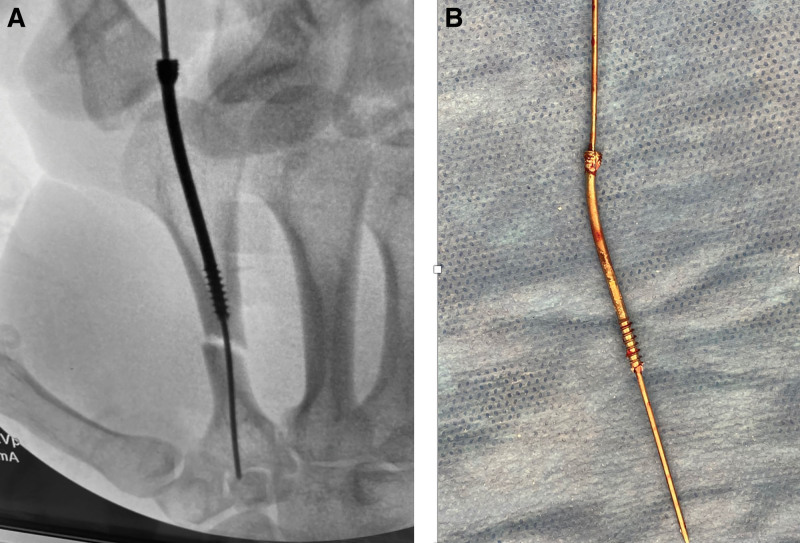
Respect the Canal and Reaming
The authors want to emphasize the importance of properly sizing the screw to the canal isthmus diameter through the use of preoperative imaging as described above. An oversized screw combined with reaming may risk a blow-out fracture upon screw insertion. Furthermore, placing a screw that is wider than the canal without reaming can lead to disastrous outcomes, including bending or breakage of the screw (Fig. 2). Especially in young patients, the cortical bone is too firm for self-tapping screws to pass without reaming. An undersized screw does not follow the appropriate biomechanical properties and will not engage inner cortex for maximal stability; therefore, the fracture will not be rigidly fixated. If it is difficult to pass a K-wire (1.1 mm) for the chosen screw diameter (eg, 2.5 mm) due to the narrowness of the canal (<1.1 mm), serial drilling of canal can be performed. A K-wire one size down (0.8 mm) can be placed, and the bone can be reamed with the appropriate size drill bit (1.6 mm) followed by upsizing the K-wire (1.1 mm) and the drill bit (2.0 mm) to allow passage of the chosen screw diameter (2.5 mm).
Fig. 2.
A, Placement of headless compression screw in second metacarpal without predrilling resulting in bent screw. B, Bent screw, requiring removal.
Multiple Fractures
We present a demonstrative case to document the clear utility of intramedullary screws in multiple fractures to demonstrate the excellent range of motion that can be achieved in high energy trauma. (See Video 3 [online], which displays the third to fifth metacarpal and first proximal phalanx fracture with full range of motion at 6-week follow-up. Placement of 3.0 mm (small and ring finger), 3.5mm (middle finger), and 2.5 mm (index proximal phalanx) headless compression screws.) Multiple fractures lead to significant swelling and significant stiffness, which often lead to major limitations in range of motion. This is an excellent indication for this technique because patients can engage in early active motion for better and faster return to preoperative range of motion. IMF technique can be effectively performed in 15–20 minutes for each bone. The proposed technique can limit operative time, periosteal stripping, and soft tissue dissection associated with plate fixation. This thereby minimizes the chances of soft tissue adhesions, rate of tenolysis, permanent swelling, scarring, and stiffness. Furthermore, the use of IM screws allows for early range of motion even in the face of multiple fractures due to the stability provided by the construct.
Video 3. Video 3 from “Intra-medullary Screw Fixation Comprehensive Technique Guide for Metacarpal and Phalanx Fractures: Pearls, and Pitfalls.” This video which demonstrates the 3-5th metacarpal and 1st proximal phalanx fracture with full range of motion at 6-week follow-up. Placement of 3.0 mm (small and ring finger), 3.5mm (middle finger), and 2.5 mm (index proximal phalanx) headless compression screws.
Anterograde versus Retrograde for Phalanx
Intermedullary screws for proximal phalanx fixation have been described with both anterograde through metacarpophalangeal joint and retrograde approaches through the proximal interphalangeal joint.32, 33 The retrograde technique is technically less demanding but a larger relative area of the distal joint surface of the proximal phalanx is violated in comparison with the anterograde technique. The mean head of proximal phalanx articular surface defects were 13%–18% for a 2.5-mm screw, and 19%–25% for a 3.0-mm screw, estimated from computed tomographic scans of healthy fingers.12 Furthermore, the central slip of the extensor mechanism may be compromised by this retrograde technique.27,32,34 We prefer the anterograde approach whenever possible as violation of the proximal interphalangeal joint in our anecdotal experience does seem to confer diminished outcomes in terms of range of motion.
Flexion of Fingers into Palm during Screw Placement
To prevent easy malrotation as screw engages strong cortical bone within canal, keep the fingers flexed into palm to tighten intermetacarpal ligaments and set appropriate cascade.
DISCUSSION
IMF is emerging as a popular method of stabilizing metacarpal and phalangeal fractures. The advantages and disadvantages of this technique are outlined in Table 2. A metaanalysis by Beck et al examined 169 metacarpal fractures fixated with IM screws and reported no major complications, 100% union rate, and full composite fist range of motion with average follow-up time of 11 months.34 The major advantage of IMF over other techniques is faster recovery to daily living and work-related activities. Furthermore, it leads to lower operative time, costs, soft tissue trauma, periosteal stripping, and extensor tendon complications than plating.
Table 2.
Advantages and Disadvantages of HCS
| Advantages | Disadvantages |
|---|---|
| • Immediate range of motion with excellent stability | • Higher cost compared with K-wire |
| • Potential canal-screw mismatch | |
| • Limited dissection that could cause tendon irritation and scarring | • Technique learning curve |
| • Quick and reliable | • Less rigid fixation than plates |
| • Cost effective | |
| • Limited visible incisional scarring | |
| • Limited reliance on unreliable patients | |
| • Improved stability compared with K-wires | |
| • No pin tract (decreased infection risk) | |
| • No hardware removal | |
| • Lower cost compared with that of the plates |
Advantages over K-wire fixation include a significantly lower rate of stiffness stemming from the benefits of early range of motion and limited immobilization. The complication rates for IMF are much lower when compared with K-wire fixation, which range from 15%–18%, including pin tract infection (7%), pin loosening or migration (5%), and nonunion (4%).8,9
Multiple studies demonstrate plates to have higher breaking strength than HCS.25,31,35 Melamed et al found an average load of failure in 2.4 mm IM screw of 75 ± 20 N in human cadaveric bone models.30 This is compared with an average load of failure of over 200 N in 1.5 mm, 2.0 mm, locking, and nonlocking plate constructs. However, it is important to note that testing was done with a four-point bending apparatus that in no way simulates the stress incurred during true in vivo physiologic loads. (Of note, the average bending moment during metacarpophalangeal joint flexion has been reported to be 0.35 Nm.)36 Plates and screws may allow superior strength in vitro but have higher rates of complications and higher costs in vivo without clear benefit over IMF. Fusetti et al reported complications, including stiffness, delayed healing, plate loosening or breakage, complex regional pain syndrome, and deep infection in 35% of patients.37 Page and Stern found a similar major complication rate of 36% in 105 metacarpal and/or phalangeal fractures fixated with plates. IMF allows for early mobilization while also avoiding the multiple planes of dissection, soft tissue scarring, periosteal stripping, and soft tissue swelling that is associated with plate and screw fixation.
SUMMARY
IMF is a powerful option for metacarpal and phalanx fixation that allows rigid stability, enabling early return of function with excellent rates of union and total active motion. With knowledge of technical pearls presented in this article, common mistakes can be avoided to improve efficiency of screw placement and optimize patient outcomes.
Footnotes
Published online 26 October 2021.
Disclosure: The authors have no financial interest in relation to the content of this article.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.Nakashian MN, Pointer L, Owens BD, et al. Incidence of metacarpal fractures in the US population. Hand (N Y). 2012;7:426–430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Court-Brown CM, Caesar B. Epidemiology of adult fractures: a review. Injury. 2006;37:691–697. [DOI] [PubMed] [Google Scholar]
- 3.Karl JW, Olson PR, Rosenwasser MP. The epidemiology of upper extremity fractures in the United States, 2009. J Orthop Trauma. 2015;29:e242–e244. [DOI] [PubMed] [Google Scholar]
- 4.Chung KC, Spilson SV. The frequency and epidemiology of hand and forearm fractures in the United States. J Hand Surg Am. 2001;26:908–915. [DOI] [PubMed] [Google Scholar]
- 5.Page SM, Stern PJ. Complications and range of motion following plate fixation of metacarpal and phalangeal fractures. J Hand Surg Am. 1998;23:827–832. [DOI] [PubMed] [Google Scholar]
- 6.Robinson LP, Gaspar MP, Strohl AB, et al. Dorsal versus lateral plate fixation of finger proximal phalangeal fractures: a retrospective study. Arch Orthop Trauma Surg. 2017;137:567–572. [DOI] [PubMed] [Google Scholar]
- 7.Verver D, Timmermans L, Klaassen RA, et al. Treatment of extra-articular proximal and middle phalangeal fractures of the hand: a systematic review. Strategies Trauma Limb Reconstr. 2017;12:63–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Botte MJ, Davis JLW, Rose BA, et al. Complication of smooth pin fixation of fracture and dislocation in the hand and wrist. Clin Orthop. 1992;276:194–201. [PubMed] [Google Scholar]
- 9.Stahl S, Schwartz O. Complications of K-wire fixation of fractures and dislocations in the hand and wrist. Arch Orthop Trauma Surg. 2001;121:527–530. [DOI] [PubMed] [Google Scholar]
- 10.Eberlin KR, Babushkina A, Neira JR, et al. Outcomes of closed reduction and periarticular pinning of base and shaft fractures of the proximal phalanx. J Hand Surg Am. 2014;39:1524–1528. [DOI] [PubMed] [Google Scholar]
- 11.del Piñal F, Moraleda E, Rúas JS, et al. Minimally invasive fixation of fractures of the phalanges and metacarpals with intramedullary cannulated headless compression screws. J Hand Surg Am. 2015;40:692–700. [DOI] [PubMed] [Google Scholar]
- 12.Bong MR, Kummer FJ, Koval KJ, et al. Intramedullary nailing of the lower extremity: biomechanics and biology. J Am Acad Orthop Surg. 2007;15:97–106. [DOI] [PubMed] [Google Scholar]
- 13.Russell TA, Taylor JC, LaVelle DG, et al. Mechanical characterization of femoral interlocking intramedullary nailing systems. J Orthop Trauma. 1991;5:332–340. [DOI] [PubMed] [Google Scholar]
- 14.Wong TC, Ip FK, Yeung SH. Comparison between percutaneous transverse fixation and intramedullary K-wires in treating closed fractures of the metacarpal neck of the little finger. J Hand Surg Br. 2006;31:61–65. [DOI] [PubMed] [Google Scholar]
- 15.Ozer K, Gillani S, Williams A, et al. Comparison of intramedullary nailing versus plate-screw fixation of extra-articular metacarpal fractures. J Hand Surg Am. 2008;33:1724–1731. [DOI] [PubMed] [Google Scholar]
- 16.Jupiter JB, Koniuch MP, Smith RJ. The management of delay union and nonunion of the meta- carpals and phalanges. J Hand Surg. 1985;10:457–466. [DOI] [PubMed] [Google Scholar]
- 17.Kozin SH, Thoder JJ, Lieberman G. Operative treatment of metacarpal and phalangeal shaft fractures. J Am Acad Orthop Surg. 2008;8:111–121. [DOI] [PubMed] [Google Scholar]
- 18.Herbert TJ, Fisher WE. Management of the fractured scaphoid using a new bone screw. J Bone Joint Surg Br. 1984;66:114–123. [DOI] [PubMed] [Google Scholar]
- 19.McQueen MM, Gelbke MK, Wakefield A, et al. Percutaneous screw fixation versus conservative treatment for fractures of the waist of the scaphoid: a prospective randomised study. J Bone Joint Surg Br. 2008;90:66–71. [DOI] [PubMed] [Google Scholar]
- 20.Boulton CL, Salzler M, Mudgal CS. Intramedullary cannulated headless screw fixation of a comminuted subcapital metacarpal fracture: case report. J Hand Surg Am. 2010;35:1260–1263. [DOI] [PubMed] [Google Scholar]
- 21.Tobert DG, Klausmeyer M, Mudgal CS. Intramedullary fixation of metacarpal fractures using headless compression screws. J Hand Microsurg. 2016;8:134–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hoang D, Huang J. Antegrade intramedullary screw fixation: a novel approach to metacarpal fractures. J Hand Surg Global Online. 2019;1:229-235. [Google Scholar]
- 23.Dunleavy ML, Candela X, Darowish M. Morphological analysis of metacarpal shafts with respect to retrograde intramedullary headless screw fixation. Hand (N Y). 2020:1558944720937362 (E-pub ahead of print.). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Okoli M, Chatterji R, Ilyas A, et al. Intramedullary headless screw fixation of metacarpal fractures: a radiographic analysis for optimal screw choice. Hand (N Y). 2020:1558944720919897 (E-pub ahead of print.). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Giesen T, Gazzola R, Poggetti A, et al. Intramedullary headless screw fixation for fractures of the proximal and middle phalanges in the digits of the hand: a review of 31 consecutive fractures. J Hand Surg Eur Vol. 2016;41:688–694. [DOI] [PubMed] [Google Scholar]
- 26.West J, Mason B. Limited incision open reduction and internal fixation of proximal phalanx fractures with headless screws. Presented at the 2020 AAHS Annual Meeting, Ft Lauderdale, Florida. Jan 8-11, 2020. [Google Scholar]
- 27.ten Berg PW, Mudgal CS, Leibman MI, et al. Quantitative 3-dimensional CT analyses of intramedullary headless screw fixation for metacarpal neck fractures. J Hand Surg Am. 2013;38:322–330. e2. [DOI] [PubMed] [Google Scholar]
- 28.Berger RA. The anatomy of the scaphoid. Hand Clin. 2001;17:525–532. [PubMed] [Google Scholar]
- 29.Urbanschitz L, Dreu M, Wagner J, et al. Cartilage and extensor tendon defects after headless compression screw fixation of phalangeal and metacarpal fractures. J Hand Surg Eur Vol. 2020;45:601–607. [DOI] [PubMed] [Google Scholar]
- 30.Melamed E, Hinds RM, Gottschalk MB, et al. Comparison of dorsal plate fixation versus intramedullary headless screw fixation of unstable metacarpal shaft fractures: a biomechanical study. Hand (N Y). 2016;11:421–426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mahylis JM, Burwell AK, Bonneau L, et al. Drill penetration injury to extensor tendons: a biomechanical analysis. Hand (N Y). 2017;12:301–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Borbas P, Dreu M, Poggetti A, et al. Treatment of proximal phalangeal fractures with an antegrade intramedullary screw: a cadaver study. J Hand Surg Eur Vol. 2016;41:683–687. [DOI] [PubMed] [Google Scholar]
- 33.Gaspar MP, Gandhi SD, Culp RW, et al. Dual antegrade intramedullary headless screw fixation for treatment of unstable proximal phalanx fractures. Hand (N Y). 2019;14:494–499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Beck CM, Horesh E, Taub PJ. Intramedullary screw fixation of metacarpal fractures results in excellent functional outcomes: a literature review. Plast Reconstr Surg. 2019;143:1111–1118. [DOI] [PubMed] [Google Scholar]
- 35.Curtis BD, Fajolu O, Ruff ME, et al. Fixation of metacarpal shaft fractures: biomechanical comparison of intramedullary nail crossed K-wires and plate-screw constructs. Orthop Surg. 2015;7:256–260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Vanik RK, Weber RC, Matloub HS, et al. The comparative strengths of internal fixation techniques. J Hand Surg Am. 1984;9:216–221. [DOI] [PubMed] [Google Scholar]
- 37.Fusetti C, Meyer H, Borisch N, et al. Complications of plate fixation in metacarpal fractures. J Trauma. 2002;52:535–539. [DOI] [PubMed] [Google Scholar]