Abstract
Background
Multiple survey studies have demonstrated a mental health (MH) burden of COVID-19 globally. However, few studies have examined relevant risk factors for pandemic-related MH issues.
Methods
A link to an online survey was posted from April 8th - June 11th, 2020 which included questions regarding COVID-19 experience, perceived impact of the pandemic on life domains (e.g., social communication, finances), behavioural alterations (e.g., online activities, substance use), and MH treatment history. Current psychiatric symptom severity and impairment were evaluated using the Generalized Anxiety Disorder-7, Patient Health Questionnaire-9, and the Perceived Stress Scale.
Results
Overall, 632 individuals (82% female, mean age:42.04 ± 16.56) in Canada and the United States completed the survey. While few reported contracting COVID-19 (0.5%), the impact of the pandemic was evident, with a vast majority reporting anxiety around COVID-19 infecting loved ones (88%). Almost half (43%) reported previous MH treatment and 31% met criteria for GAD, 29% for MDD and 63% reported significantly high levels of stress. Female sex, younger age and past MH treatment emerged as significant predictors of these issues(p < .01). Age-related differences in the impact of COVID-19 on life domains, substance use, and online activity were also noted.
Conclusion
The findings from the current sample add to the growing literature suggesting negative effects of COVID-19 on MH, while highlighting specific risk factors. Age may be an important factor in predicting MH during this pandemic.
Keywords: Coronavirus, Mental health, Anxiety, Depression, Stress, COVID-19
1. Introduction
In December 2019, the World Health Organization (WHO) China Country Office reported cases of an unknown pneumonia in the city of Wuhan, Hubei. The disease, now known as the coronavirus disease 2019 (COVID-19), spread rapidly throughout China and internationally, leading the WHO to declare a global pandemic on March 11th, 2020 (Cucinotta and Vanelli, 2020). To curb the spread of COVID-19, governments have enacted travel bans, lockdowns, and stay-at-home orders. Businesses and educational institutions have closed, group gatherings have been cancelled, and non-essential employees have been ordered to work from home. While these unprecedented measures have been effective in reducing the spread of the virus, it is feared that new problems are emerging, including an upcoming mental health (MH) crisis in the aftermath of this COVID-19 pandemic.
Previous epidemics and traumatic global events (SARS, 9/11) have documented increased psychological distress and exacerbation of previous MH symptoms (Lancee et al., 2008; Marshall and Galea, 2004; Nickell et al., 2004). These effects often arise immediately in response to the aftermath of the event and persist for many years thereafter (Galea et al., 2020). Given that COVID-19 is a traumatic event with global impact, it is anticipated that increases in depression, anxiety, substance use, grief, and loneliness will be widespread, due in part to the lasting impacts of fear, social isolation, and economic hardships associated with the pandemic (Galea et al., 2020; Holmes et al., 2020). To date, data from China, the first epicenter of the COVID-19 outbreak, have shown markedly high levels of stress, anxiety and depression (Gao et al., 2020; Li et al., 2020; Lu et al., 2020; C. Wang, Pan, Wan, Tan, Xu, McIntyre, et al., 2020; J. Zhang et al., 2020a; Zhu et al., 2020). Surveys from other hard-hit countries such as Italy, Spain, and Iran have also documented alarming rates of MH symptoms (Cellini et al., 2020; Moccia et al., 2020; Moghanibashi-Mansourieh, 2020; Ozamiz-Etxebarria et al., 2020).
As COVID-19 spread across North America, the MH status of individuals also declined. Crowdsourced data published by Statistics Canada revealed that from April to May 2020, 24% of participants reported fair or poor MH, which represents a three-fold increase from previous years (7.7% and 8.1% in 2018 and 2019, respectively) (Statistics Canada, 2020a, 2020b). This suggests that MH has worsened notably since the onset of physical distancing (Statistics Canada, 2020a, 2020b). High stress levels were reported by 28% of the overall sample, and these were exacerbated for those who reported worsening MH (41%) (Statistics Canada, 2020a). More recent data from June 2020 found 19.50% of respondents (N = 1005) to be experiencing moderate to severe anxiety, and 18.40% experienced moderate to severe depression (Centre for Addictions and Mental Health, 2020). The United States (U.S.) became the most recent epicenter of the outbreak with over 4.7 million cases and 155,000 deaths as of August 4th, 2020 (Johns Hopkins University and Medicine, 2020). A nationally representative sample of U.S. adults (N = 10,368) found high depressive symptoms, with over 25% reporting moderate to severe anxiety symptoms (Fitzpatrick et al., 2020). Additionally, 13.6% of U.S. adults (N = 1468) reported symptoms of serious psychological distress, almost 10% higher relative to 2018 (McGinty et al., 2020). Self-reported stress levels of Americans are decreasing slightly but remain in the moderate range, with average ratings of 5.4/10 from April–May and 5.0/10 in June–July (American Psychological Association, 2020). Overall, these statistics suggest that the COVID-19 pandemic has taken a toll on the psychological well-being of the North American population, and there is clearly a need to evaluate these changes in the long-term.
Survey studies from around the world have identified several candidate risk factors for increased MH health problems during COVID-19. These include MH or medical comorbidity, being a healthcare provider, COVID-19 exposure, and female sex (Huang and Zhao, 2020; Lai et al., 2020; A. M. Lee et al., 2007). Age is also proving to be a strong predictor of MH status in the context of the pandemic. Surveys from around the world have documented greater anxiety and depression related to COVID-19 in young adults (Alonzi et al., 2020; Huang and Zhao, 2020; S. A. Lee et al., 2020; Moghanibashi-Mansourieh, 2020; Y. Wang, Di, Ye and Wei, 2020; Bruine de Bruin, 2020). In the U.S., participants in the Household Pulse Survey aged 18–39 reported higher rates of anxiety, depression, and combined anxiety and depression (Centers for Disease Control and Prevention, 2020). On the contrary, older adults (aged 60+) self-report lower levels of anxiety and depression compared to their younger counterparts, despite reporting higher rates of perceived COVID-19 fatality (Centers for Disease Control and Prevention, 2020). A similar picture has emerged in Canada, where specifically young adults (ages 18–39) reported higher rates of moderate to severe anxiety and depression compared to those aged 60+ (Centre for Addictions and Mental Health, 2020).
Presently, few studies have investigated the specific factors underlying risks for poor MH during COVID-19. Poor MH status has been consistently linked to difficulties in several major life domains, including financial challenges, lack of social support, poor physical health and diet, and increased internet and substance use (Evans et al., 2007) all of which have been negatively impacted by the COVID-19 pandemic. The economy declined significantly as workplaces shut down and businesses filed for bankruptcy, leading to significant job loss (F. Ayittey et al., 2020).Opportunities for social engagement also reduced drastically due to lockdown measures (Holmes et al., 2020). Home confinement has also led to changes in specific physical health-related behaviours (Ammar et al., 2020). Public recreational facilities have become inaccessible, and this may also be accompanied by increased engagement in sedentary screen time activities (Colley et al., 2020). Changes in food intake, alcohol consumption, and drug use are also common responses to psychological distress, thereby increasing the risk of poor diet and problematic substance use during the COVID-19 pandemic (Rolland et al., 2020) Furthermore, sleep disruptions may occur as a result of increased MH symptoms (Cellini et al., 2020). Taken together, these changes warrant an in-depth examination of behavioural changes instigated by COVID-19 and their relation to MH status. This knowledge will provide insight into the mechanisms underlying different MH health outcomes and inform interventions and guidelines to mitigate the impact of the pandemic on those who are most vulnerable.
The current study therefore aims to understand the predictors of significant MH problems (depression, anxiety and stress) in a sample of North Americans. Given the developing literature on the age-specific effects of COVID-19 on MH, we examine differences in behaviour across several life domains, based on age. This manuscript provides a snapshot of baseline data from a longitudinal survey in Canada and the U.S. examining the psychological impact of the COVID-19 pandemic.
2. Materials and methods
2.1. Study design and participants
Study data for this baseline assessment were collected using the Research Electronic Data Capture (REDCap) software (Harris et al., 2009) between April 8th and June 11th, 2020, 3 weeks after a state of emergency was declared in Ontario, Canada and 5 weeks in New York, U.S. A link to an online survey hosted on a secure McMaster University (Hamilton, ON, Canada) server was posted to Facebook, Twitter and Reddit. The survey was also sent out via email campaigns to the Department of Psychiatry at the University of Rochester, staff and faculty at Hamilton Health Sciences and the McMaster Alumni Association mailing list. It was posted on the MacAnxiety Research Centre website (www.macanxiety.com) and emails with a link to the survey was sent out to residents and fellows from the Centre for Addiction and Mental Health. Following completion of this questionnaire, participants interested in completing the follow-up assessments provided consent to be contacted at two additional time points spaced 4 weeks apart. Informed consent was obtained after the participants had been provided with the details of the study. This analysis reports findings from the first baseline assessment.
Eligibility criteria were intentionally broad, requiring participants be age 16 years or older, be able to read and understand English (>8th grade level) and acknowledge an online informed consent statement. This study was approved by the Hamilton Integrated Research Ethics Board. This study was carried out in accordance with the latest version of the Declaration of Helsinki.
2.2. Assessments
The survey was developed for the purpose of this project. Participants provided demographic information regarding their age, geographic location, education, occupation, marital status, and living situation. Given that pre-existing MH conditions are a risk factor to further psychological distress during COVID-19, participants provided information regarding their MH history. MH treatment questions included past/current medication status, dosage changes since the escalation of the COVID-19 pandemic, past/current therapy status, and whether therapy frequency had increased since the escalation of the pandemic.
Participants also answered questions regarding their COVID-19 pandemic experiences. These included self-isolation and physical distancing measures, living arrangements, work and education alterations, worries related to the virus, and knowledge of others who contracted or passed away from the virus. Additionally, participants reported on changes in their behaviours over the past month. Questions utilized 5-point or 6-point (where applicable) Likert type questions indicating the extent to which behaviours increased or decreased (e.g. “To what degree has the COVID-19 Pandemic altered your sleep?“). The specific Likert options presented to participants were as follows: very much decreased, slightly decreased, no change, slightly increased, very much increased. For many variables including alcohol, cannabis and drug use, social media, online gaming or pornography, a sixth option, “I do not do this”, was added. The areas of finances, social communication, exercise, eating behaviours, time spent engaging in various recreational online activities (shopping, gambling, video chatting, reading news, etc), and consumption of various substances (alcohol, cannabis, illicit substances) were examined.
Current psychiatric symptoms were evaluated using the validated Generalized Anxiety Disorder-7 (GAD-7; Spitzer et al., 2006), the Patient Health Questionnaire- 9 (PHQ-9; Kroenke and Spitzer, 2002) and the Perceived Stress Scale (PSS; Lee, 2012).
The GAD-7 (Spitzer et al., 2006) was used to assess participants' levels of anxiety over the past two weeks. Items are rated on a 4-point Likert scale and total scores are calculated based on the sum of all items. In the present study, a cut score of ≥10 was used to indicate significant anxiety, (Spitzer et al., 2006). This scale has demonstrated strong reliability(Cronbach's ɑ = 0.89–.92; Spitzer et al., 2006) and validity (r = .72 with the Beck Anxiety Inventory; Spitzer et al., 2006) in clinical and community samples and is widely used in mental health research (Kroenke et al., 2007; Löwe et al., 2008).
Participants also completed the PHQ-9, a 9-item tool measuring depressive symptoms over the past two weeks, often used to screen for symptoms in research studies, (Kroenke et al., 2001). Items on the PHQ-9 are rated on a 4-point Likert scale and summed to obtain total scores. A cut score of ≥10 was used to indicate significant depression in the present study, (Kroenke et al., 2001). The PHQ-9 shows strong reliability (Cronbach's ɑ =.86–.89; Kroenke et al., 2001) and validity,(r = .71 with the Beck Depression Inventory; Kroenke et al., 2001).
The PSS-10 was administered to evaluate participants' stress levels. This 10-item scale uses a 5-point Likert scale to measure the degree to which situations in one's life are appraised as stressful over the past month (Cohen, 1994; Cohen et al., 1983). Final scores are obtained by reverse-scoring positively phrased items and summing across all items. The PSS-10 shows robust reliability (Cronbach's ɑ >.70, Lee, 2012) and validity as it has been positively correlated with other gold-standard measures, (Lee, 2012). Scores of ≥ 14 indicate significant levels of stress, (Lee, 2012).
In addition, participants were asked to complete The Quality of Life Enjoyment and Satisfaction Questionnaire Short Form (Q-LES-Q-SF) to evaluate their current perceived quality of life (Endicott et al., 1993). This validated questionnaire contains 16 questions, rated on a 5-point Likert scale and assesses overall enjoyment and satisfaction across various areas of life, including physical health, mood, work, and relationships (Stevanovic, 2011). Participants get a point value ranging from 1 to 5 on each item. The scores from all items are summed, such that higher scores indicate higher satisfaction, with the highest possible score of 70 and lowest possible score of 16.
2.3. Statistical analyses
Descriptive statistics were conducted to characterize the impacts of COVID-19 and rates of MH disorders. Logistic regression analysis was performed to explore potential predictors of high levels of anxiety, depression, and significant stress during COVID-19. Given significant comorbidity between GAD ad MDD, a combined GAD or MDD variable was created for this model comprised of respondents who scored ≥ 10 on either the GAD-7 or PHQ-9, (n = 248, 39.2%). We selected variable that seemed relevant to the relationship between MH and the pandemic. The model included sex, age (<35 years, 35–59 years and ≥60 years), living situation, frontline worker status and past MH treatment. Employment and education were considered a priori; however, were excluded due to the high proportions of highly educated individuals and individuals who maintained employment, making these variables less relevant. Further, there were no appreciable differences in model fit with either covariate, so they were excluded from the final model.
Finally, differences in behavioural alterations were examined across age groups (<35 years, 35–59 years and ≥60 years) using ANOVAs and Tukey's test (two-tailed) to identify which comparisons were significant. All analyses were conducted in SPSS (Version 26) and an alpha value of 0.05 was used to denote statistical significance.
3. Results
3.1. Sample demographics
A total of 632 participants (69% Canadian; 31% American) were included in analyses. The sample was predominantly middle-aged (42.04 ± 16.56; range 16–93 years), female (82%) and highly educated with 46% having a postgraduate or professional degree (Table 1 ). No differences in age, sex or education were noted between the Canadian and U.S. samples (all p > .05), therefore all analyses were conducted collapsing these categories. A majority (84%) of the sample reported living with a partner or with family or with roommates (43%), while only 16% lived alone during COVID-19. One-third (29%) were healthcare practitioners, while an additional 15% worked in research or healthcare support fields. Similarly, 124 (19%) respondents identified as frontline workers.
Table 1.
Characteristics of the sample.
| VARIABLE | TOTAL SAMPLE (N = 632) |
CANADA (n = 437) |
USA (n = 195) |
|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | |
| Age | 42.04 (16.56) | 42.49 (16.9) | 41.01 (15.8) |
| N (%) | N (%) | N (%) | |
| Female | 517 (81.8) | 358 (81.9) | 159 (81.8) |
| EDUCATION | |||
| High School or less | 15 (2.3) | 11 (2.5) | 4 (2.0) |
| Some College/University | 47 (7.4) | 35 (8.0) | 12 (6.2) |
| College Diploma/University Degree | 236 (37.3) | 172 (39.4) | 64 (32.8) |
| Some Professional/Post-graduate | 59 (9.3) | 40 (9.2) | 19 (9.7) |
| Professional or Postgraduate Degree | 275 (43.5) | 179 (41.0) | 96 (49.2) |
| LIVING SITUATION | |||
| Alone | 101 (16.0) | 65 (14.9) | 36 (18.5) |
| With Family/Relatives | 236 (37.3) | 180 (41.2) | 56 (28.7) |
| With Partner/Spouse | 259 (41.0) | 173 (39.6) | 86 (44.1) |
| With Roommate/Friends | 36 (5.7) | 19 (4.3) | 17 (8.7) |
| OCCUPATION | |||
| Healthcare Practitioner/Medical Technician | 183 (29.0) | 117 (26.8) | 66 (33.8) |
| Full-time Student | 68 (10.8) | 57 (13.0) | 11 (5.6) |
| Healthcare Support | 49 (7.8) | 23 (5.3) | 26 (13.3) |
| Health Research or Research | 46 (7.3) | 30 (6.9) | 16 (8.2) |
| Educational Instruction or Library | 40 (6.3) | 27 (6.2) | 13 (6.7) |
| Management | 33 (5.2) | 27 (6.2) | 6 (3.1) |
| Community and Social Sciences | 32 (5.1) | 22 (5.0) | 10 (5.1) |
| Retired | 32 (5.1) | 30 (6.9) | 2 (1.0) |
| Other | 149 (23.6) | 104 (23.8) | 45 (23.1) |
| CURRENT PSYCHIATRIC SYMPTOM SEVERITY | Mean (SD) | Mean (SD) | Mean (SD) |
| Generalized Anxiety Disorder-7 | 7.36 (5.9) | 7.19 (5.9) | 7.74 (6.0) |
| Patient Health Questionnaire −9 | 6.89 (6.0) | 6.80 (5.9) | 7.10 (6.2) |
| Perceived Stress Scale | 16.62 (7.8) | 16.39 (7.8) | 17.14 (7.8) |
| Quality of Life Enjoyment and Satisfaction Questionnaire Short Form (mean raw scores) | 50.4 (9.0) | 50.2 (9.0) | 50.7 (8.9) |
| PROBABLE DSM-5 DIAGNOSIS BY CUT SCORE | N (%) | N (%) | N (%) |
| GAD (GAD-7 ≥ 10) | 194 (30.7) | 132 (30.2) | 62 (31.8) |
| MDD (PHQ-9≥ 10) | 186 (29.4) | 130 (29.7) | 56 (28.7) |
| Significant Stress (PSS ≥ 14) | 395 (62.5) | 270 (61.8) | 125 (64.1) |
3.2. Impact of COVID-19
At the time of the survey, most participants (77%) continued to work daily. Working from home with pay was most common (40%), followed by 32% going into work as usual. Only 5% reported being laid off since the onset of COVID-19, while 17% were not working prior to the pandemic. The vast majority (98%) practiced physical distancing.
Although only three participants tested positive for COVID-19 at the time of this baseline assessment, 43% knew someone who contracted the virus and 12% knew someone who had died from the virus. A majority of participants reported being mildly/very anxious about their loved ones (88%) or themselves (67%) getting COVID-19. Most respondents strongly identified with having access to emotional help if it was needed (47%) and being able to talk to family or friends about their problems (48%). Finally, 93% agreed with governmental restrictions to some degree and most (79%) did not feel that the caution being exercised by the public was excessive. Over 85% of participants also agreed that there would be permanent changes to life post-COVID-19, and that this pandemic would have a long-lasting impact on the economy.
3.3. Mental health during COVID-19
Roughly 43% of the sample reported having received treatment for a MH problem prior to the COVID-19 pandemic, while 23% were currently receiving treatment. As noted in Table 1, mean symptom severity scale scores indicated on average participants reported mild symptoms of GAD (GAD-7 score between 6 and 10, Spitzer et al., 2006) and MDD (PHQ-9 score between 5 and 9, Kroenke et al., 2001) in the overall sample. On average, perceived stress levels were high (PSS≥14, Lee et al., 2012) (Table 1). Despite mild psychiatric symptom severity in the overall sample, almost one-third met screening DSM-5 criteria for GAD (31%) and MDD (29%) during the pandemic. Over 60% reported high levels of stress (PSS≥14). The mean raw score of quality of life satisfaction was 50.4, which is 64% of the maximum score of 70. In community samples, normal score ranges of the Q-LES-Q-SF translate to 70%−100% of the maximum score (Lee et al., 2014), indicating below average quality of life scores in this sample. Older individuals (≥age 60) reported significantly better QOL than respondents under 60, (F = 1.88, p = .001). The mean raw Q-LES-Q-SF score for respondents ≥ age 60 was 55.4 ± 7.7, which translates to 73% of the maximum score and falls within community norms.
Predictors of significant levels of GAD or MDD and stress were evaluated, and the results of these logistic regression models are presented in Table 2 . In both models, younger age, female sex and past MH treatment emerged as significant predictors of GAD/MDD and significant stress. Living situation and being a frontline worker did not prove to be significant predictors of either outcome.
Table 2.
Predictors of clinically significant levels of GAD or MDD and Stress.
| Variable [reference category] | GAD or MDD OR (95% CI) |
Stress OR (95% CI) |
|---|---|---|
| Age [≥60 years] | ||
| <35 years | 2.51 (1.39–4.54)** | 3.01 (1.82–5.00)*** |
| 35–59 years | 2.46 (1.36–4.46)** | 2.16 (1.31–3.58)** |
| Female [No] | ||
| Yes | 2.53 (1.47–4.36)*** | 1.79(1.13–2.78)* |
| Living situation [living alone] | ||
| Living with Family | 1.67 (0.98–2.84) | 1.43 (0.84–2.44) |
| Living with Partner | 1.13 (0.67–1.91) | 0.91 (0.55–1.52) |
| Living with Roommate(s) | 1.32 (0.55–3.16) | 0.95 (0.40–2.26) |
| Frontline Worker [No] | ||
| Yes | 1.17 (0.76–1.80) | 1.01 (0.65–1.58) |
| Past MH treatment [No] | ||
| Yes | 3.72 (2.61–5.30)*** | 2.82(1.96–4.06)*** |
*p < .05, **p < .01, ***p < .001.
3.4. Changes in behaviour following pandemic onset
In the overall sample, most (54%) reported no change in finances (40% decreased; 6% increased). However, approximately half (52%) reported “very much or slightly decreased” daily communication with loved ones or friends (36% increased; 12% no change). Over half (56%) reported decreased exercise (25% increased; 19% no change), while an overwhelming majority reported increases (83%) in screen time (2% decreased; 14% no change; 1% did not use screens). With regard to specific online behaviours, increases were observed in video streaming (72%), reading or watching the news (72%), online messaging (70%) and social media use (62%) in the majority of respondents. Increases were also reported in online information-seeking (54%) (41% no change; 2% decreased; 3% did not use), and online shopping (43%) (32% no change; 14% decreased; 11% did not do). Nearly half (45%) reported increases in eating behaviour, while 36% reported no change and 19% reported decreases. With regard to substance use, 38% reported no change in alcohol intake, while 32% reported an increase, 10% reported a decrease and 20% did not consume alcohol. Most of the sample did not use cannabis or illicit drugs during this time (77% and 91%, respectively). Amongst those who did use these agents, 63% of those using cannabis (n = 143) and 94% of those using illicit drugs (n = 53) reported no change in their use; 34% reported increased cannabis use, 6% increased illicit drug use and 3% decreased their cannabis use. Lastly, 43% reported decreases in sleep during the pandemic; 34% reported “no change” and 23% reported increases in sleep.
3.5. Age-related differences in behaviour
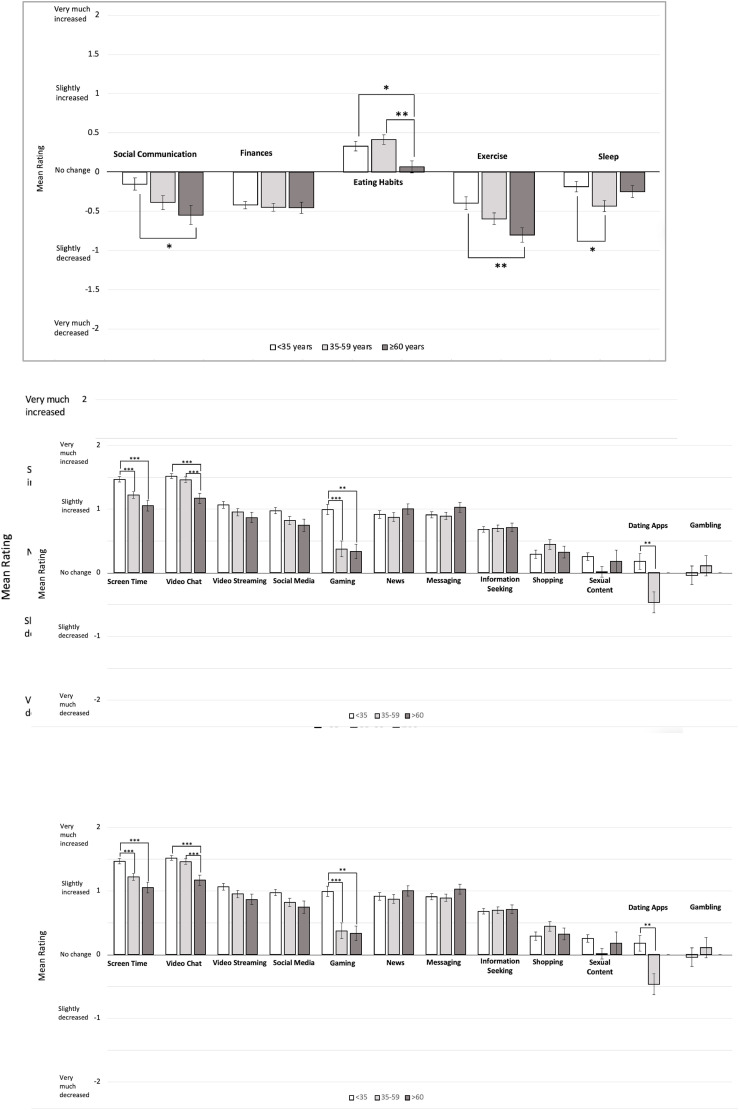
Differences in impacts of COVID-19 on participants’ behaviour also emerged across age groups. Specifically, age-related differences were found in social communication, eating habits, exercise and sleep. Compared to those <35 years, respondents >60 years reported greater decreases in daily communication (p < .05) and exercise (p < .01; Fig. 1 A). Non-senior groups exhibited more increases in eating behaviour when compared to those ≥60 years (p < .05; Fig. 1A). Significant differences in decreased sleep only emerged when comparing individuals 35–59 years with those under 35 (p < .05; Fig. 1A). Overall substance use (illict drugs, alcohol, and cannabis) decreased (Fig. 1B), while significant increases in cannabis use were found among participants <35 years compared to those ≥60.
Fig. 1.
A. Mean ratings of perceived change in life domain. Values range from “Very much decreased” to “Very much increased” (−2 to +2), 0 indicates no change. Statistically significant findings are denoted by * p < 0.05, ** p < 0.01, *** p < 0.001. B. Mean rating of perceived change in substance use. Statistically significant findings are denoted by * p < 0.05, ** p < 0.01, *** p < 0.001. C. Mean ratings of perceived change in online activities/behaviour. Statistically significant findings are denoted by * p < 0.05, ** p < 0.01, *** p < 0.001.
In terms of screen time (Fig. 1C), increases were noted in most activities. Age-related differences emerged in overall screen time, time spent gaming, video chatting and using dating apps. Those <35 years reported increased screen time (p < .001 both older age groups) and time spent gaming (35-59-year-olds: p < .001; ≥60-year-olds, p < .01) compared to both older age groups. Video chatting increased significantly in both age groups under 60 when compared to those 60 and above (both p < .001). Although use of dating apps was not particularly high, individuals under 35 reported a greater use than those between 35 and 59 years (p < .01), with the latter group reporting decreased use.
4. Discussion
This study reveals significant levels of anxiety, depression and stress in an online convenience sample during the early stages of the COVID-19 pandemic. While overall levels of MH symptom severity indicated mild symptoms, almost one-third of respondents met validated cut scores for GAD and MDD, while over 60% reported significant stress. Interestingly, age, female sex and past MH treatment emerged as significant predictors of these issues. During the pandemic, most reported reductions in daily communication, however compensatory online social behaviours may have increased with 70% reporting increased use of video chat and messaging for non-work/school related reasons. Most also reported reductions in exercise and sleep. Overall increases were noted in most internet-based behaviours. Substance use in general was low, with the exception of alcohol which almost one-third reported increasing to some level. Age-related differences also emerged, specifically with cannabis use and all assessed life domains, with the exception of finances. Similarly, younger individuals (<35 years) reported increased overall screen time during the pandemic than either older age group. Specifically, use of video chat, gaming and dating apps seem to be contributing modalities.
The early MH impacts of COVID-19 have been demonstrated globally. Rates of GAD in the current sample (30.7%) fall within previously reported ranges of 19.6% (J. Zhang et al., 2020b) to 35.1% (Huang and Zhao, 2020) in China. Similarly, the present sample's rates of MDD (29.4%) fall within the ranges of 9.8% (J. Zhang et al., 2020b) to 48.3% (Gao et al., 2020), which were also reported when China was hit most severely by COVID-19. This suggests that the MH of North Americans may be particularly at risk; participants in the present study showed similar levels of concerning symptomology prior to the peak of the COVID-19 pandemic. This is further corroborated by the sample's high rate of perceived stress. Crowd-sourced survey data from Statistics Canada in 2018 and 2019 reported that approximately 22% of adults aged 18 and older to have perceived most days in their life to be quite a bit or extremely stressful (Statistics Canada, 2020a). In the present sample, 62.5% reported significant stress, which almost triples rates from year prior to the pandemic. This further highlights the strong negative toll of the COVID-19 pandemic and indicates the need for strong supports to ensure optimal mental well-being.
The results of our logistic regression model also revealed several predictors for significant MH issues. Pre-existing MH issues have been highlighted as a risk factor for the negative MH effects of the COVID-19 pandemic across the world (Galea et al., 2020; Holmes et al., 2020). This highlights the exacerbated impact of the COVID-19 pandemic on those who were already vulnerable, and illustrates the need for both immediate supports and long-term observation for individuals with prior MH concerns. Female sex also emerged as a high-risk characteristic for MH problems in the present sample. This aligns with the results of many studies in the pandemic literature (Lu et al., 2020; C. Wang, Pan, Wan, Tan, Xu, Ho, et al., 2020; Y. Wang, Di, Ye and Wei, 2020; W. R. Zhang et al., 2020b) as well as in non-pandemic samples (Altemus et al., 2014). However, rates of MDD and GAD in females are generally double those found in males in a non-pandemic context (Altemus et al., 2014). Therefore, it is difficult to conclude the degree to which female sex reflects epidemiological differences in MH symptoms or acts as a risk factor for poor MH due to COVID-19. Nevertheless, concerns regarding the MH effects of this pandemic may also arise from consequences of the public health interventions implemented to limit the spread of COVID-19. Specifically, social/physical distancing, government-mandated shutdowns and downstream potential negative economic impacts of such interventions may be potential drivers of a MH pandemic post-COVID-19.
In the present study, younger age also emerged as a predictor of poor MH and was also associated with lower perceived QOL. As with female sex, this aligns with previous findings (Centre for Addictions and Mental Health, 2020; Vahia et al., 2020) but may reflect typical non-pandemic differences found in epidemiological studies. The prevalence rates of GAD and MDD peak in early adulthood and decrease naturally with older age (Bandelow and Sophie, 2015). This has been noted specifically for GAD, such that older adults have the lowest prevalence of all ages (Brenes, 2006; Brenes et al., 2008). A similar course has also been noted in MDD (Kessler et al., 2011). Previous non-pandemic research has also documented consistent age differences in behavioural stress responses, (Folkman et al., 1987). In the current sample, we note reduced frequency in behaviours that would be seen as protective for MH, specifically, social communication and physical exercise. However, in this sample, older adults reported greater decreases in communication and exercise than younger adults. Although these patterns would lead us to anticipate worse MH in older adults, young adults report greater severity of MH issues despite revealing smaller reductions in these domains. Throughout this pandemic, reports indicate that older adults are experiencing particularly high levels of social isolation (Armitage and Nellums, 2020) due to serious COVID-19 related health complications, high mortality rates, and severe outbreaks in long-term care homes. While younger adults also report reduced social communication, they may be compensating through alternate online modalities. Participants across all age groups reported slightly higher screen time, but younger adults reported the greatest increases in use of non-work-related video chatting, gaming, and use of dating apps. Although these online activities may be used to facilitate social relationships, the relationship between greater time spent online and MH problems has been well-documented in the literature (Gao et al., 2020; Kardefelt-Winther, Rees, Livingstone, 2020). Experts have further expressed concerns regarding unprecedented levels of screen time since the onset of the COVID-19 pandemic. It can be speculated that younger adults in the present sample may be experiencing higher levels of MDD and GAD in relation with prolonged digital media use, however, pre-pandemic levels of disorder were not assessed, (Gao et al., 2020; Kardefelt-Winther, Rees, Livingstone, 2020). Similar to the current sample, reduced physical activity has been noted worldwide (Ammar et al., 2020; Tison et al., 2020); an expected change given the implementation of stay-at-home orders and closure of gyms and recreation centres. However, this decline in activity was least pronounced for younger adults. While some research suggests that physical activity declines progressively with age (Hickey and Mason, 2017), the pandemic may have instigated shifts to home-based exercise (Hammami et al., 2020) which are reliant on technology and consequently may be more accessible to younger groups. Our results suggest the possibility that other factors may be negatively impacting the well-being of individuals under the age of 35 during COVID-19.
Aside from reductions in positive behaviours, younger adults may be engaging in more maladaptive behaviours such as over-eating and substance use. Early survey studies reveal increased levels of unhealthy food consumption, snacking, and more large meals during home confinement compared to pre-confinement (Ammar et al., 2020). A large-scale survey of participants from France (N = 10,771) revealed that being <49 years was a main factor in increased caloric food intake (Rolland et al., 2020). It has been suggested that greater levels of uncontrolled eating may be in response to boredom, reduced motivation to exercise or maintain healthy eating or as an attempt to improve mood or reduce anxiety during home confinement ((Adams, 2020; Ammar et al., 2020; Di Renzo et al., 2020). Although cannabis use in the overall sample was low, adults under 35 years reported significantly greater increases in cannabis use compared to older age groups. This finding may be partially attributable to pre-existing age differences in cannabis use (Mauro et al., 2018) or to free-time and boredom (Canadian Centre on Substance Use, 2020), however, it may be an attempt to cope with pandemic-related MH issues, as many pursue cannabis to alleviate stress, anxiety, and depression (Kosiba et al., 2019; Rolland et al., 2020). Taken together, our findings suggest that young people may be particularly impacted by behaviour changes due to the early months of the COVID-19 pandemic, and this may be compounded by other factors not evaluated within the present study.
Overall, these findings should be considered in light of the study's strengths and limitations. Although we utilized validated and reliable self-report symptom severity scales to examine prevalence and severity of the relevant conditions, these do not replace a formal clinical assessment. Further, the sample size was moderately large, but composed primarily of highly educated females, which reduces the generalizability of the findings. Additionally, we did not collect data on participant race and ethnicity. This might have allowed for further interpretation as it has been established that COVID-19 disproportionality effects racially marginalized communities in both Canada and the United States, (Muñoz-Price et al., 2020; Millett et al., 2020; Subedi et al., 2020). A recent report found that U.S. counties with higher proportions of Black residents had more COVID-19 diagnoses and deaths even after adjusting for county-level characteristics such as age, poverty, comorbidities, and epidemic duration, (Millett et al., 2020). While, in another recent report of 2595 American hospital inpatients, both Black race and poverty were associated with hospitalization, (Muñoz-Price et al., 2020). Similar COVID-19 findings have been reported in Canada where neighbourhoods with the highest proportion of visible minorities in Toronto and Montreal have a standardized age-mortality rate three times higher than those neighbourhood with low proportions of visible minorities, (Subedi et al., 2020). COVID-19 racial disparities in both Canada and the United States can be attributed to systemic racial inequality. Black residents often occupy the majority of the essential workforce, where risk of exposure is much higher (Muñoz-Price et al., 2020). Additionally, Black residents are less able to abide by physical distancing practices compared to White residents, due to racially disparities in housing access. A recent report proposed that racial bias in mortgage lending practices along with existing socioeconomic depravities might be the source of this racially segregated housing (Muñoz-Price et al., 2020). Further, both the US and Canadian samples were not recruited using a population sampling strategy, and primarily drawn from two middle-sized cities with differing public health systems and COVID-19 intervention approaches. Due to the online nature of this study, all responses were self-report and retrospective in nature and likely subject to sampling and self-selection biases. Although the cross-sectional nature of the current study limits our interpretation of MH changes from prior to the pandemic to during the COVID-19 pandemic at this point in time, we are following this sample longitudinally and will characterize long-term within-sample differences. The high rate of previous MH treatment in this sample further limits our interpretation on whether the significant MH symptoms noted are in response to COVID-19; regardless, longitudinal follow-up of this group is especially valuable and will provide greater insight to the effects of COVID-19 on this vulnerable group.
5. Conclusion
Overall, the current study suggests that the COVID-19 pandemic is taking a clear toll on the population's mental well-being. The present sample exhibited significant levels of anxiety, depression, and stress, with female sex, younger age and prior MH treatment as significant predictors. Specifically, older adults (>60 years) revealed lower risk for MH problems during the COVID-19 pandemic compared to younger adults (<35 years). These results suggest that older adults may be exhibiting better adjustment to the COVID-19 pandemic, though findings may have been influenced by pre-existing age differences and MH epidemiology. Nonetheless, findings from the present study provide an important anchor point for changes to come in the aftermath of the COVID-19 pandemic. More importantly, findings highlight the importance of further exploring relations between MH status and behavioural alterations in the context of the COVID-19 pandemic. Age-related differences are particularly key to understand in these associations. Doing so will help clinicians understand specific risk factors for MH symptoms, enabling them to provide more targeted and effective care strategies.
Author data statement
Authors can confirm that all relevant data are included in the article and/or its supplementary information files.
Declaration of competing interest
Dr. Turna has nothing to disclose.
Ms. Zhang has nothing to disclose.
Ms. Lamberti has nothing to disclose.
Ms. Patterson has nothing to disclose.
Dr. Simpson has nothing to disclose.
Dr. Francisco has nothing to disclose.
Dr. Goldman Bergmann reports grants from Coordenação de Aperfeiçoamento de Pessoal de Nivel Superior – Brasil (CAPES), outside the submitted work.
Dr. Van Ameringen reports personal fees from Allergan, personal fees from Almatica, personal fees from Brainsway, personal fees from Lundbeck, personal fees from Myriad Neuroscience, personal fees from Otsuka, grants and personal fees from Purdue Pharma (Canada), other from Janssen-Ortho Inc, personal fees from Pfizer, grants from Hamilton Academic Health Sciences Organization, Innovation Grant, outside the submitted work.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jpsychires.2021.02.059.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Adams C. 2020. Eating Well during Coronavirus/COVID-19.https://www.bda.uk.com/resource/eating-well-during-coronavirus-covid-19.html [Google Scholar]
- Alonzi S., La Torre A., Silverstein M.W. The psychological impact of preexisting mental and physical health conditions during the COVID-19 pandemic. Psychological Trauma: Theor. Res. Pract. Pol. 2020;12(S1):S236–S238. doi: 10.1037/tra0000840. [DOI] [PubMed] [Google Scholar]
- Altemus M., Sarvaiya N., Neill Epperson C. Sex differences in anxiety and depression clinical perspectives. Front. Neuroendocrinol. 2014;35(3):320–330. doi: 10.1016/j.yfrne.2014.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychological Association . 2020. Stress In AmericaTM2020: Stress In the Time of COVID-19, Volume Three.https://www.apa.org/news/press/releases/stress/2020/stress-in-america-covid-july.pdf [Google Scholar]
- Ammar A., Brach M., Trabelsi K., Chtourou H., Boukhris O., Masmoudi L., Bouaziz B., Bentlage E., How D., Ahmed M., Müller P., Müller N., Aloui A., Hammouda O. Effects of COVID-19 home confinement on eating behaviour and physical activity: results of the ECLB-COVID19 International Online Survey. Nutrients. 2020;12:1583–1596. doi: 10.3390/nu12061583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armitage R., Nellums L.B. COVID-19 and the consequences of isolating the elderly. Lancet Public Health. 2020;5(5):e256. doi: 10.1016/S2468-2667(20)30061-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ayittey F.K., Ayittey M.K., Chiwero N.B., Kamasah J.S., Dzuvor C. Economic impacts of Wuhan 2019‐nCoV on China and the world. J. Med. Virol. 2020;92(5):473–475. doi: 10.1002/jmv.25706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandelow B., Sophie M. Epidemiology of anxiety disorders in the 21st century. Dialogues Clin. Neurosci. 2015;17(3):327–335. doi: 10.1016/j.siny.2015.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brenes G.A. Age differences in the presentation of anxiety. Aging Ment. Health. 2006;10(3):298–302. doi: 10.1080/13607860500409898. [DOI] [PubMed] [Google Scholar]
- Brenes G.A., Knudson M., McCall W.V., Williamson J.D., Miller M.E., Stanley M.A. Age and racial differences in the presentation and treatment of Generalized Anxiety Disorder in primary care. J. Anxiety Disord. 2008;22(7):1128–1136. doi: 10.1016/j.janxdis.2007.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruine de Bruin W. Age differences in COVID-19 risk perceptions and mental health: evidence from a mational U.S. survey conducted in March 2020. J. Gerontol.: Ser. Bibliogr. 2020:1–6. doi: 10.1093/geronb/gbaa074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canadian Centre on Substance Use . 2020. COVID-19 and Increased Alcohol Consumption: NANOS Poll Summary Report.https://www.ccsa.ca/covid-19-and-increased-alcohol-consumption-nanos-poll-summary-report [Google Scholar]
- Cellini N., Canale N., Mioni G., Costa S. Changes in sleep pattern, sense of time and digital media use during COVID-19 lockdown in Italy. J. Sleep Res. 2020;29(4) doi: 10.1111/jsr.13074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention . 2020. Mental Health - Household Pulse Survey.https://www.cdc.gov/nchs/covid19/pulse/mental-health.htm [Google Scholar]
- Centre for Addictions and Mental Health . 2020. COVID-19 National Survey Dashboard.https://www.camh.ca/en/health-info/mental-health-and-covid-19/covid-19-national-survey [Google Scholar]
- Cohen S., Kamarck T., Mermelstein R. A global measure of perceived stress. J. Health Soc. Behav. 1983;24(4):385–396. doi: 10.2307/2136404. [DOI] [PubMed] [Google Scholar]
- Colley R.C., Bushnik T., Langlois K. Exercise and screen time during the COVID-19 pandemic. Health Rep. 2020;31:3–11. doi: 10.25318/82-003-x202000600001-eng. [DOI] [PubMed] [Google Scholar]
- Cucinotta D., Vanelli M. WHO declares COVID-19 a pandemic. Acta Biomed. 2020;91(1):157–160. doi: 10.23750/abm.v91i1.9397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Renzo L., Gualtieri P., Cinelli G., Bigioni G., Soldati L., Attinà A., Bianco F.F., Caparello G., Camodeca V., Carrano E., Ferraro S., Giannattasio S., Leggeri C., Rampello T., Lo Presti L., Tarsitano M.G., De Lorenzo A. Psychological aspects and eating habits during COVID-19 home confinement: results of EHLC-COVID-19 Italian Online Survey. Nutrients. 2020;12(7):2152. doi: 10.3390/nu12072152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Endicott J., Nee J., Harrison W., Blumenthal R. Quality of life enjoyment and satisfaction questionnaire: a new measure. Psychopharmacol. Bull. 1993;29(2):321–326. [PubMed] [Google Scholar]
- Evans S., Banerjee S., Leese M., Huxley P. The impact of mental illness on quality of life: a comparison of severe mental illness, common mental disorder and healthy population samples. Qual. Life Res. 2007;16(1):17–29. doi: 10.1007/s11136-006-9002-6. [DOI] [PubMed] [Google Scholar]
- Fitzpatrick K.M., Harris C., Drawve G. Fear of COVID-19 and the mental health consequences in America. Psychological Trauma: Theor. Res. Pract. Pol. 2020;12(S1):17–21. doi: 10.1037/tra0000924. [DOI] [PubMed] [Google Scholar]
- Folkman S., Lazarus R.S., Pimley S., Novacek J. Age differences in stress and coping processes. Psychol. Aging. 1987;2(2):171–184. doi: 10.1037/0882-7974.2.2.171. [DOI] [PubMed] [Google Scholar]
- Galea S., Merchant R.M., Lurie N. The mental health consequences of COVID-19 and physical distancing: the need for prevention and early intervention. JAMA Int. Med. 2020;180(6):817–818. doi: 10.1001/jamainternmed.2020.1562. [DOI] [PubMed] [Google Scholar]
- Gao J., Zheng P., Jia Y., Chen H., Mao Y., Chen S., Wang Y., Fu H., Dai J. Mental health problems and social media exposure during COVID-19 outbreak. PloS One. 2020;15(4):1–10. doi: 10.1371/journal.pone.0231924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammami A., Harrabi B., Mohr M., Krustrup P. Physical activity and coronavirus disease 2019 (COVID-19): specific recommendations for home-based physical training. Manag. Sport Leisure. 2020:1–6. doi: 10.1080/23750472.2020.1757494. [DOI] [Google Scholar]
- Harris P.A., Taylor R., Thielke R., Payne J., Gonzalez N., Conde J.G. Research electronic data capture (REDCap) -- A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inf. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hickey M., Mason S. Age and gender differences in particpation rates, motivators for, and barriers to exercise. Modern Psychol. Stud. 2017;22(2):3. [Google Scholar]
- Holmes E.A., O'Connor R.C., Perry V.H., Tracey I., Wessely S., Arseneault L., Ballard C., Christensen H., Cohen Silver R., Everall I., Ford T., John A., Kabir T., King K., Madan I., Michie S., Przybylski A.K., Shafran R., Sweeney A., et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatr. 2020;7(6):547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang Y., Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatr. Res. 2020;288(March):112954. doi: 10.1016/j.psychres.2020.112954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johns Hopkins University, Medicine . 2020. COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University.https://coronavirus.jhu.edu/map.html [Google Scholar]
- Kardefelt‐Winther D., Rees G., Livingstone S. Contextualising the link between adolescents' use of digital technology and their mental health: a multi‐country study of time spent online and life satisfaction. JCPP (J. Child Psychol. Psychiatry) 2020;61(8):875–889. doi: 10.1111/jcpp.13280. [DOI] [PubMed] [Google Scholar]
- Kessler R.C., Birnbaum H., Bromet E., Hwang I., Sampson N., Shahly V. Age differences in major depression: results from the national comorbidity surveys replication. NCS-R). 2011;40(2):1–18. doi: 10.1017/S0033291709990213.Age. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kosiba J.D., Maisto S.A., Ditre J.W. Patient-reported use of medical cannabis for pain, anxiety, and depression symptoms: systematic review and meta-analysis. Soc. Sci. Med. 2019;233(July):181–192. doi: 10.1016/j.socscimed.2019.06.005. [DOI] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L. The PHQ-9: a new depression diagnostic and severity measure. Psychiatr. Ann. 2002;32(9):509–515. doi: 10.3928/0048-5713-20020901-06. [DOI] [Google Scholar]
- Lai J., Ma S., Wang Y., Cai Z., Hu J., Wei N., Wu J., Du H., Chen T., Li R., Tan H., Kang L., Yao L., Huang M., Wang H., Wang G., Liu Z., Hu S. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Network Open. 2020;3(3) doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lancee W.J., Maunder R.G., Goldbloom D.S. Prevalence of psychiatric disorders among Toronto hospital workers one to two years after the SARS outbreak. Psychiatr. Serv. 2008;59(1):91–95. doi: 10.1176/ps.2008.59.1.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee A.M., Wong J.G.W.S., McAlonan G.M., Cheung V., Cheung C., Sham P.C., Chu N.M., Wong P.C., Tsang K.W.T., Chua S.E. Stress and psychological distress among SARS survivors 1 year after the outbreak. Can. J. Psychiatr. 2007;52(4):233–240. doi: 10.1177/070674370705200405. [DOI] [PubMed] [Google Scholar]
- Lee Y.T., Liu S.I., Huang H.C., Sun F.J., Huang C.R., Yeung A. Validity and reliability of the Chinese version of the short form of quality of life enjoyment and satisfaction questionnaire (Q-LES-Q-SF) Qual. Life Res. 2014;23(3):907–916. doi: 10.1007/s11136-013-0528-0. [DOI] [PubMed] [Google Scholar]
- Lee S.A., Mathis A.A., Jobe M.C., Pappalardo E.A. Clinically significant fear and anxiety of COVID-19: a psychometric examination of the Coronavirus Anxiety Scale. Psychiatr. Res. 2020;290(May):113112. doi: 10.1016/j.psychres.2020.113112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li S., Wang Y., Xue J., Zhao N., Zhu T. The impact of covid-19 epidemic declaration on psychological consequences: a study on active weibo users. Int. J. Environ. Res. Publ. Health. 2020;17(6) doi: 10.3390/ijerph17062032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu W., Wang H., Lin Y., Li L. Psychological status of medical workforce during the COVID-19 pandemic: a cross-sectional study. Psychiatr. Res. 2020;288(March):1–5. doi: 10.1016/j.psychres.2020.112936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall R.D., Galea S. Science for the community: assessing mental health after 9/11. J. Clin. Psychiatr. 2004;65(Suppl. 1):37–43. [PubMed] [Google Scholar]
- Mauro P.M., Carliner H., Brown Q.L., Hasin D.S., Shmulewitz D., Rahim-Juwel R., Sarvet A.L., Wall M.M., Martins S.S. Age differences in daily and nondaily cannabis use in the United States, 2002–2014. J. Stud. Alcohol Drugs. 2018;79(3):423–431. doi: 10.15288/jsad.2018.79.423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGinty E.E., Presskreischer R., Han H., Barry C.L. Psychological distress and loneliness reported by US Adults in 2018 and April 2020. J. Am. Med. Assoc. 2020;324(1):93–94. doi: 10.1001/jama.2020.9740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Millett G.A., Jones A.T., Benkeser D., Baral S., Mercer L., Beyrer C., et al. Assessing differential impacts of COVID-19 on Black communities. Ann. Epidemiol. 2020;47:37–44. doi: 10.1016/j.annepidem.2020.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moccia L., Janiri D., Pepe M., Dattoli L., Molinaro M., De Martin V., Chieffo D., Janiri L., Fiorillo A., Sani G., Di Nicola M. Affective temperament, attachment style, and the psychological impact of the COVID-19 outbreak: an early report on the Italian general population. Brain Behav. Immun. 2020;87(July):75–79. doi: 10.1016/j.bbi.2020.04.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moghanibashi-Mansourieh A. Assessing the anxiety level of Iranian general population during COVID-19 outbreak. Asian J. Psychiatr. 2020;51(June):102076. doi: 10.1016/j.ajp.2020.102076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muñoz-Price L.S., Nattinger A.B., Rivera F., Hanson R., Gmehlin C.G., Perez A., Singh S., Buchan B.W., Ledeboer N.A., Pezzin L.E. Racial disparities in incidence and outcomes among patients with COVID-19. JAMA Network Open. 2020;3(9) doi: 10.1001/jamanetworkopen.2020.21892. https://doi-org.libaccess.lib.mcmaster.ca/10.1001/jamanetworkopen.2020.21892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nickell L.A., Crighton E.J., Tracy C.S., Al-Enazy H., Bolaji Y., Hanjrah S., Hussain A., Makhlouf S., Upshur R.E.G. Psychosocial effects of SARS on hospital staff: survey of a large tertiary care institution. Can. Med. Assoc. J. 2004;170(5):793–798. doi: 10.1503/cmaj.1031077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ozamiz-Etxebarria N., Dosil-Santamaria M., Picaza-Gorrochategui M., Idoiaga-Mondragon N. Stress, anxiety, and depression levels in the initial stage of the COVID-19 outbreak in a population sample in the northern Spain. Cad. Saúde Pública. 2020;36(4):1–9. doi: 10.1590/0102-311X00054020. [DOI] [PubMed] [Google Scholar]
- Rolland B., Haesebaert F., Zante E., Benyamina A., Haesebaert J., Franck N. Global changes and factors of increase in caloric food, screen and substance use during the early COVID-19 containment phase in France: a general population online survey. JMIR Public Health Surveill. 2020;6(3):e19630. doi: 10.2196/19630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B.W., Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Statistics Canada . 2020. Canadians' Mental Health during the COVID-19 Pandemic.https://www150.statcan.gc.ca/n1/daily-quotidien/200527/dq200527b-eng.htm [Google Scholar]
- Statistics Canada . 2020. Mental Health of Canadians during the COVID-19 Pandemic.https://www150.statcan.gc.ca/n1/pub/11-627-m/11-627-m2020039-eng.htm [Google Scholar]
- Stevanovic D. Quality of Life Enjoyment and Satisfaction Questionnaire–short form for quality of life assessments in clinical practice: a psychometric study. J. Psychiatr. Ment. Health Nurs. 2011;18(8):744–750. doi: 10.1111/j.1365-2850.2011.01735.x. [DOI] [PubMed] [Google Scholar]
- Subedi R., Greenberg L., Turcotte M. COVID-19 mortality rates in Canada's ethno-cultural neighbourhoods. StatCan COVID-19: Data to insights for a better Canada. Released Octover. 2020;28:2020. [Google Scholar]
- Tison G., Avram R., Kuhar P., Abreau S., Marcus G., Pletcher M., Olgin J. Worldwide effect of COVID-19 on physical activity: a descriptive study. Ann. Intern. Med. 2020;173(9):767–770. doi: 10.7326/M20-2665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vahia I.V., Jeste D.V., Reynolds C.F., III Older adults and the mental health effects of COVID-19. J. Am. Med. Assoc. 2020;324(22):2253–2254. doi: 10.1001/jama.2020.21753. published online November 20, 2020. [DOI] [PubMed] [Google Scholar]
- Wang Y., Di Y., Ye J., Wei W. Study on the public psychological states and its related factors during the outbreak of coronavirus disease 2019 (COVID-19) in some regions of China. Psychol. Health Med. 2020:1–10. doi: 10.1080/13548506.2020.1746817. [DOI] [PubMed] [Google Scholar]
- Zhang J., Lu H., Zeng H., Zhang S., Du Q., Jiang T., Du B. The differential psychological distress of populations affected by the COVID-19 pandemic Coronavirus. Brain Behav. Immun. 2020;87(July):49–50. doi: 10.1016/j.bbi.2020.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang W.R., Wang K., Yin L., Zhao W.F., Xue Q., Peng M., Min B.Q., Tian Q., Leng H.X., Du J.L., Chang H., Yang Y., Li W., Shangguan F.F., Yan T.Y., Dong H.Q., Han Y., Wang Y.P., Cosci F., Wang H.X. Mental health and psychosocial problems of medical health workers during the COVID-19 epidemic in China. Psychother. Psychosom. 2020;89(4):242–250. doi: 10.1159/000507639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu S., Wu Y., Zhu C., Hong W., Yu Z., Chen Z., Chen Z., Jiang D., Wang Y. The immediate mental health impacts of the COVID-19 pandemic among people with or without quarantine managements. Brain Behav. Immun. 2020;87(July):56–58. doi: 10.1016/j.bbi.2020.04.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.