Abstract
Introduction
After the World Health Organization declared COVID-19 a pandemic, a hand full of cases and deaths have been recorded globally, Nigeria inclusive.
Methods
A retrospective analysis of the COVID-19 weekly disease update report by the Nigeria Centre for Disease Control (NCDC) covering February 29, 2020 (Week 9) and March 28, 2021 (Week 12) was adopted for this study. Data were curated from the NCDC database.
Results
As of March 28, 2021, Nigeria is the 5th most affected African country and the 77th most affected country globally with 162,593 COVID-19 cases and 2,048 COVID-19 related deaths. COVID-19 has been reported in all 36 States and the Federal Capital Territory. However, Lagos has remained the epicenter of the pandemic accounting for 35.4% of the pandemic in Nigeria while Kogi State is the least affected State (0.003%). The trend showed male predilection while the age bracket 35-39 years was the most affected. The attack rate was found to be 78.8 per 100,000 of the population while the cumulative death per 100,000 of the population was found to be 1.0. The case fatality rate was found to be 1.30. Approximately 1,778,105 COVID-19 tests have been performed while 923,623 doses of vaccine have been administered.
Conclusions
COVID-19 has been reported in all states in Nigeria as well as the Federal Capital Territory with many of the cases involving males. The case trend showed a bimodal form indicating a second wave occurrence. Nigeria government has initiated some combative measures as well as vaccine initiation.
Keywords: COVID-19, SARS-CoV-2, COVID-19 in Nigeria, coronavirus, pandemic
Introduction
The inception of the COVID-19 pandemic has precipitated a dramatic loss of human life globally and had posed an inestimable obstacle to public health, food security, and economic impact. The socio-economic impact has been devastating as tens of millions of people are at the risk of slipping into extreme poverty with nearly 3.3 billion global workforce at the risk of losing their job.1 The public health impact includes disruption in the medical supply chain, blood transfusion services, diagnosis and management of chronic diseases.2-5 The global epidemiological indices as of August 26, 2021, showed 213,752,662 confirmed cases with the African Region being the 6th most affected region among the World Health Organization (WHO) regions behind the Region of Americas, Europe, South East Asia, Eastern Mediterranean, and Western Pacific.6 Nigeria like other African countries has had its own share of the impact of the pandemic. Epidemiological indices as of August 26, 2021, showed 188,880 confirmed cases and 2,288 deaths in Nigeria.6 In Nigeria, the pandemic and the ensuing lockdown/border closure have impacted the food system, economic activities, and poverty. Nigeria was faced with declining remittance and export demand: GDP fell by 23% during the lockdown, while the Agricultural food system fell by 11% owing to restriction on food services.7 However, Nigeria has put up response and preventive measures to combat the pandemic since the detection of the initial case reported on February 27, 2020.
This present article is aimed at describing the current situation of COVID-19 in Nigeria, the combative measures and lessons learned, one year after the first case.
Methods
Study design
We conducted a retrospective analysis of Nigeria Centre for Disease Control (NCDC) surveillance data reported weekly from week 9 (February 29, 2020), which marked the inception of the pandemic in Nigeria, until week 12 of the following year (March 28, 2021).
Study setting
Nigeria is a country in the West African region. Administratively, Nigeria is divided into six geopolitical zones comprising 36 states and the Federal Capital Territory. All 36 states and the Federal Capital territory have reported COVID-19 cases and COVID-19 related deaths from the inception of the pandemic.
Data collection
Epidemiological indices of COVID-19 from February 29, 2020, to March 28, 2021 (week 9, 2020 - week 12, 2021) were downloaded from the official update database of the Nigeria Centre for Disease Control (NCDC).8 The data were exported to SPSS for analysis. The confirmed cases and deaths were extracted directly while the fatality rates were computed. Also, data were extracted from the WHO weekly report within the same period of this study.9
Definition of terms
Confirmed cases/cumulative confirmed cases: This refers to the total number of confirmed COVID-19 cases within the period of study. It is represented as frequency.
Deaths/cumulative deaths: This refers to the total number of deaths that resulted owing to COVID-19 infection within the study period. It is represented as frequency.
Percentage of deaths: This refers to the proportion of COVID-19 deaths recorded in a particular State to the cumulative deaths recorded in all the States assessed within the study period. It is represented in percentage.
Attack rate / Attack rate per 100,000 of population: The index refers to the number of persons infected with COVID-19 per 100,000 of the country’s population. It is represented as frequency per 100,000 of population.
Case fatality rate: It refers to the proportion of cumulative deaths recorded in a state/country to the cumulative confirmed cases. It is represented in percentage.
Statistical analysis
Data were curated and analyzed using SPSS version 22. Epidemiological indices were represented in frequencies and proportions. Daily trends of epidemiological indices were represented in trend line-graph.
Results
Origin and incidence case
On February 27, 2020, Nigeria recorded its first confirmed case of COVID-19, which was a 44-year-old Italian Citizen who had arrived in Murtala Mohammed International Airport, Lagos, Nigeria at about 10 pm on February 24, 2020, via a Turkish airline from Milan Italy. He subsequently travelled to his company site in Ogun State on February 25, 2020. On 26th February of same the year, he presented at the staff clinic in Ogun State and there was a high index of suspicion by the managing physician. He was referred to Infectious Disease Hospital (IDH) Lagos and COVID-19 was confirmed on 27th February.10 This observation placed Nigeria second on the line of inception of the COVID-19 incident case, second to Algeria that reported her index case on February 25, 2020. The initial cases were mostly with overseas origin. However, Nigeria COVID-19 has progressed to community transmission.
Epidemiological trend/evolution
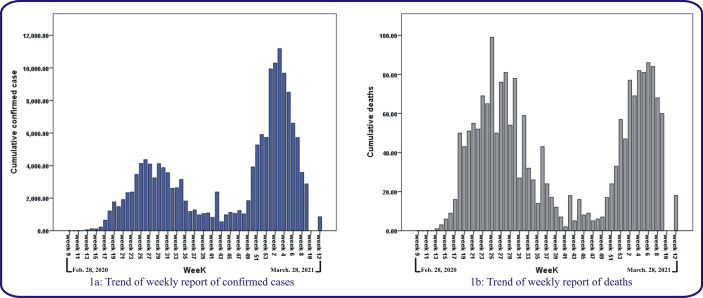
Figure 1a shows the weekly report of the COVID-19 epidemic in Nigeria within the study period. There was a progressive increase in the number of confirmed cases from week 9 (February 29, 2020) when the index case was reported, until it peaks in week 26 (June 21-27, 2020) and subsequently started to decrease again until week 43 (October 19-25, 2021) where the lowest incidence of the pandemic was recorded within that period. The case incidences were almost stable from week 44 (October 26 – November 1) to week 48 (November 23 – 29, 2020). The incidence of COVID-19 cases then rose from week 49 (November 30 – December 6, 2020) until they peaked again at week 3 of the following year (January 18 – 24, 2021) which recorded the all-round highest case count (11,179) throughout the pandemic. However, after week 3, the reported number of cases started to decline until the time of this report (Week 12: March 22-28, 2021).
Figure 1.
Trend of weekly report of COVID-19 morbidity and mortality in Nigeria
Figure 1b shows the weekly trend of COVID-19 related deaths within the studied period. Just like the case of COVID-19 morbidity, data from COVID-19 mortality were also bimodal with peaks at week 25 (June 14 – 20, 2020) and week 6 of the subsequent year (February 8 – 14, 2021). Results however, showed a decline in COVID-19 related deaths after week 6 until the time of this report.
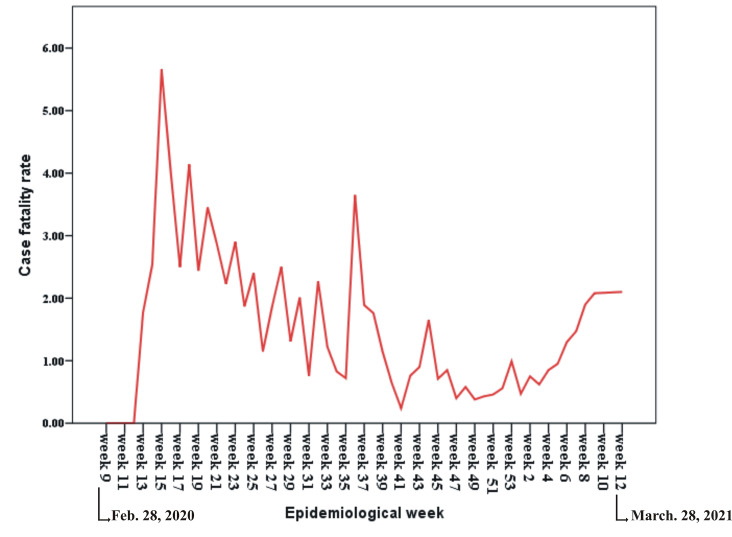
Figure 2.
Trend of weekly report of COVID-19 case fatality report in Nigeria
Figure 2 shows the weekly trend of the case fatality rate of COVID-19 in Nigeria. The case fatality rate fluttered; it rose from the inception of the pandemic and continued to flutter within 0 (minimum value) observed in the first week of the pandemic (Week 9) and 5.66 (maximum value) recorded within week 15 (April 7 – 11, 2020).
Morbidity
Since the inception of the index case until March 28, 2021, Nigeria recorded a total of 162,593 confirmed COVID-19 cases (Table 1). Stratification by states showed that Lagos State, Federal Capital Territory, Plateau State, Kaduna State, Rivers State, and Oyo State recorded the highest number of confirmed cases. Lagos State is the epicenter of the pandemic and accounted for approximately 35.4% (n=57,581) of all the COVID-19 cases (Table 2). Figure 3 shows the geographical representation of morbidity by states.
Table 1. Summary of epidemiological indices of COVID-19 pandemic in Nigeria from week 9 (February 29, 2020) to week 12 (March 28, 2021).
| Epidemiological indices | Frequency |
|---|---|
| Cumulative confirmed cases | 162,593 |
| Cumulative recoveries | 150,308 |
| Cumulative deaths | 2,048 |
| Total active cases | 10,237 |
| Attack rate per 100,000 of population | 78.8 |
| Cumulative deaths per 100,000 of population | 1.0 |
| Case fatality rate | 1.3 |
| Total tests performed | 1,778,105 |
| PCR | 1,608,186 (90.4%) |
| RDT | 169,919 (9.6%) |
| Total dose of vaccines administered | 923,623 |
| Vaccine approved for use | AstraZeneca/Oxford vaccine |
PCR – polymerase chain reaction; RDT – rapid diagnostic test.
Table 2. Stratification of COVID-19 data in Nigeria by state from week 9 (February 29, 2020) to week 12 (March 28, 2021).
| State | No. of cases | % of cases | No. of deaths | % of deaths | CFR | No. of tests |
|---|---|---|---|---|---|---|
| Lagos | 57,581 | 35.41 | 439 | 21.43 | 0.76 | 428,499 |
| FCT | 19,617 | 12.06 | 156 | 7.62 | 0.75 | 242,845 |
| Plateau | 9,024 | 5.55 | 57 | 2.78 | 0.63 | 66,908 |
| Kaduna | 8,914 | 5.48 | 65 | 3.17 | 0.73 | 77,538 |
| Rivers | 6,909 | 4.25 | 100 | 4.88 | 1.45 | 160,199 |
| Oyo | 6,838 | 4.20 | 123 | 6.00 | 1.80 | 56,286 |
| Edo | 4,875 | 3.00 | 185 | 9.03 | 3.79 | 33,739 |
| Ogun | 4,617 | 2.84 | 49 | 2.39 | 1.06 | 69,821 |
| Kano | 3,902 | 2.40 | 110 | 5.37 | 2.82 | 91,948 |
| Ondo | 3,168 | 1.95 | 62 | 3.03 | 1.96 | 23,566 |
| Kwara | 3,078 | 1.89 | 55 | 2.68 | 1.79 | 23,684 |
| Delta | 2,599 | 1.60 | 71 | 3.47 | 2.73 | 34,499 |
| Osun | 2,524 | 1.55 | 52 | 2.54 | 2.06 | 18,352 |
| Nasarawa | 2,318 | 1.42 | 13 | 0.63 | 0.56 | 22,546 |
| Enugu | 2,237 | 1.37 | 29 | 1.42 | 1.30 | 22,183 |
| Katsina | 2,083 | 1.28 | 34 | 1.66 | 1.63 | 37,909 |
| Gombe | 2,030 | 1.25 | 44 | 2.15 | 2.17 | 43,517 |
| Ebonyi | 2,007 | 1.23 | 32 | 1.56 | 1.59 | 14,959 |
| Anambra | 1,909 | 1.17 | 19 | 0.93 | 0.99 | 23,999 |
| Akwaibom | 1,762 | 1.08 | 14 | 0.68 | 0.79 | 16,708 |
| Abia | 1,665 | 1.02 | 21 | 1.02 | 1.26 | 21,141 |
| Imo | 1,642 | 1.01 | 37 | 1.81 | 2.25 | 33,517 |
| Bauchi | 1,521 | 0.93 | 17 | 0.83 | 1.12 | 24,498 |
| Borno | 1,327 | 0.82 | 38 | 1.85 | 2.86 | 19,760 |
| Benue | 1,188 | 0.73 | 22 | 1.07 | 1.85 | 16,639 |
| Adamawa | 1,051 | 0.64 | 32 | 1.56 | 3.04 | 18,255 |
| Niger | 930 | 0.57 | 17 | 0.83 | 1.83 | 17,505 |
| Taraba | 910 | 0.56 | 22 | 1.07 | 2.42 | 12,578 |
| Ekiti | 865 | 0.53 | 11 | 0.54 | 1.27 | 16,090 |
| Bayelsa | 852 | 0.52 | 26 | 1.27 | 3.05 | 16,735 |
| Sokoto | 774 | 0.48 | 28 | 1.37 | 3.62 | 18,749 |
| Jigawa | 518 | 0.32 | 16 | 0.78 | 3.09 | 8,987 |
| Kebbi | 442 | 0.27 | 16 | 0.78 | 3.62 | 14,878 |
| Cross River | 366 | 0.22 | 17 | 0.83 | 4.64 | 6,871 |
| Yobe | 313 | 0.19 | 9 | 0.44 | 2.87 | 10,410 |
| Zamfara | 232 | 0.14 | 8 | 0.39 | 3.45 | 7,392 |
| Kogi | 5 | 0.003 | 2 | 0.10 | 40.00 | 4,600 |
FCT – federal capital territory.
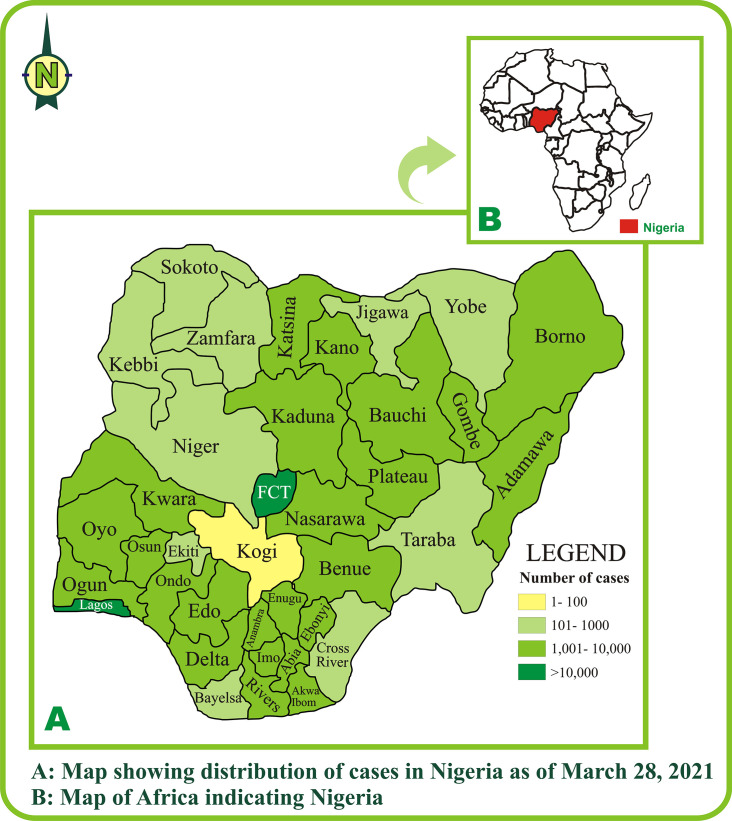
Figure 3.
Geographical representation of COVID-19 epidemic in Nigeria by state
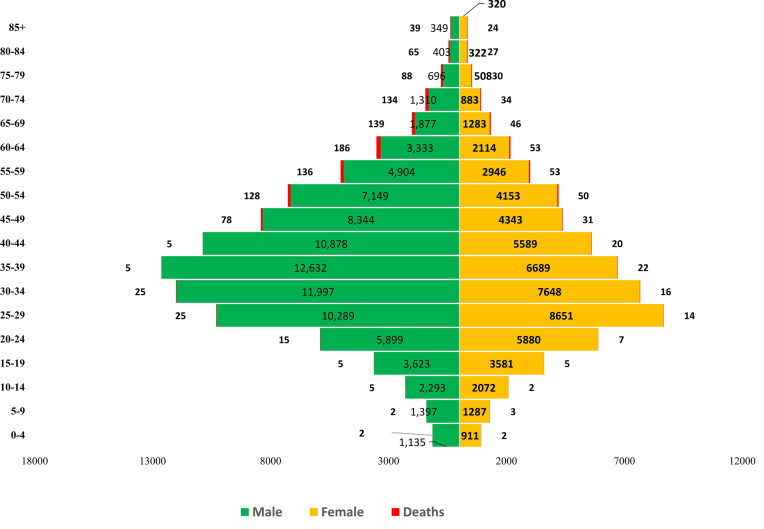
Demographic consideration showed that males were more affected than women, while the age bracket 25-39 years was the most affected. Specifically, those within the age bracket 35-39 years constituted the majority of the male COVID-19 morbidity while those within the age bracket 25-29 years constituted the bulk of the female COVID-19 morbidities (Figure 4).
Figure 4.
Gender-age representation of COVID-19 morbidity and mortality
Mortality
The total number of deaths due to COVID-19 in Nigeria from the time of the index case until March 28, 2021, was 2,048 (Table 1). Stratification of mortality by states showed Lagos, Edo, FCT, Oyo, Kano, and Rivers as the most affected with COVID-19 related deaths accounting for 21.43%, 9.03%, 7.62%, 6.00%, 5.37%, and 4.88% of all COVID-19 deaths in Nigeria (Table 2).
Demographic stratification showed male preponderant death relating to COVID-19 within the age range of ≥45 years (Figure 4).
Case fatality rate
The average case fatality rate of COVID-19 from the inception of the index case until March 28, 2020, is 1.30 (Table 1). The results further showed that Kogi, Cross River, Edo, Kebbi, Jigawa and Zamfara States had the top six case fatality rates in Nigeria with relation to COVID-19 deaths (Table 2).
Recoveries
Documented data showed that there were 150,308 documented recoveries from COVID-19 morbidity in Nigeria as of March 28, 2021 (Table 1).
Attack rate per 100,000 population
As of 28th March 2021, the attack rate per 100,000 of population of COVID-19 in Nigeria is 78.8 (Table 1).
Laboratory testing
As of the time of the study, a total of 1,778,105 COVID-19 tests had been performed in Nigeria. Of these, 1,608,186 (90.4%) were PCR based tests while 169,119 (9.6%) were rapid diagnostic-based tests (Table 1). Within the time of the study, 76 government (non-paid) laboratories11 and 44 private fee-paying laboratories12 across the country have been established for COVID-19 diagnosis. The states with the highest proportion of COVID-19 testing in Nigeria as of the time of this study were Lagos (428,499), FCT (242,845), Rivers (1160,199), Kano (91,948), Ogun (69,821), Plateau, (66,908) and Oyo (56,286) (Table 2).
Treatment
The Nigeria Centre for Disease Control developed interim guidelines for clinical management of COVID-19 with the recommended general principle for the treatment governed by: supplemental oxygen therapy, cautious, and conservative use of fluids (to prevent fluid overload), empiric use of antibiotics, and close monitoring of patients with signs of clinical deterioration. The NCDC however, cautioned on the lack of evidence on the efficacy of chloroquine and hydroxychloroquine (±azithromycin), lopinavir/ritonavir, remdesivir, umifenovir, favipiravir, tocilizumab, interferon-B-1a, except during clinical trials.
The guidelines for the clinical management of complications of COVID-19 are anchored on the two common complications of COVID-19: hypoxemic respiratory failure (HRF) and acute respiratory distress syndrome (ARDS); sepsis and septic shock.13
Vaccination
As of April 6, 2021, 923,623 vaccine doses had been administered in Nigeria out of the 3.94 million doses of AstraZeneca/Oxford vaccine, manufactured by the Serum Institute of India (SII) received in the country on March 2, 2021.14 On March 5, 2021, a doctor, Cyprian Ngong became the first person in Nigeria to receive the COVID-19 vaccine. The priorities plans for the administration of COVID-19 vaccines in Nigeria first considered health workers and supporting staff; frontline workers and first responders; persons aged 60 years and above; persons aged 50-59 years; persons aged 18-49 years with co-morbidities; then, the rest of the eligible population aged 18-49 years. Various surveys in Nigeria have shown wide hesitancy and negative perception on uptake of the COVID-19 vaccines in the Nigerian population15,16 with some “No vaccine” advocates believing that vaccines are unwholesome tools for government control over the masses while others had hesitancy due to lack of trust in the government system and perceived risk of side effects of the vaccines.
Response
In response to the pandemic, the Nigeria government on 28th February 2020 activated a multi-sectoral Emergency Operations Centre (EOC) at Level 3 which is the highest emergency level in Nigeria. This is led by NCDC in close coordination with the State Public Health EOCs (PHEOC) and through the deployment of 52 Rapid Response Teams (RRT) to states.
Currently, response activities include: ongoing technical supports and deployment of diagnostic kits, personal protective equipment, and consumables to various states, activation of government non-paid laboratories and private fee-paying laboratories, support and verification of travelers’ COVID-19 test results and active role in infodemic management.
Preventive measures
In the wake of the pandemic, the Nigerian government made frantic moves towards the prevention of the disease, including screening of passengers at international airports using temperature scanners, implementation of compulsory wearing of non-medical masks in public places and observation of social distancing, temporary border closures, and regulation of public gatherings.10
Discussion
The cumulative confirmed cases of COVID-19 recorded in Nigeria within the study period were observed to be 162,593. This value placed Nigeria as the 5th most-affected African country after South Africa (1,554,466), Tunisia (249,703), Egypt (199,364), and Ethiopia (198,794) and the 77th most affected country in the world; accounting for 0.12% (162,593/129,359,540) of the global COVID-19 pandemic within the same period of time.9 Juxtaposed to the global data, United States (29,859,706), Brazil (12,404,414), India (11,971,624), France (4,435,057) Russia (4,519,832) and United Kingdom (4,329,184) had remained the top six most affected countries at same period.9 However, adjusting for population, the data showed a lower attack rate per 100,000 of the population (78.8) unlike African countries with very high attack rates like Seychelles (4,122.1/100,000), Cape Verde (3,060.9/100,000), South Africa (2,604.1/100,000), Namibia (1,711.9/100,000) and Botswana (1,635.7/100,000).9
The younger age group of 25-39 years constituted the bulk of the confirmed cases. This could be explained by the fact that young people account for over 60% of Nigeria’s population.17 More so, children under 5 years and those aged between 5-9 years accounted for 1.26% and 1.65%, respectively of COVID-19 confirmed cases in Nigeria. Although there is no clear reason for the incidence of COVID-19 in children, some authors have suggested a difference in immune system function.18,19
Gender stratification showed male preponderance in the trend of COVID-19 infection in Nigeria. This observation aligns with an earlier report by World Health Organization African Region20 and studies from China21 and Italy.22 This male predilection has been hypothesized to be due to genetic and physiologic factors which include wider distribution of SARS-CoV-2 cellular receptor, angiotensin-converting enzyme 2 (ACE-2) in males than in females.19,23 In another perspective, in Nigeria society that is largely patriarchal, males are more likely to put up with socioeconomic activities that are outside the confines of home, and subsequently have higher chances of exposure to COVID-19.19
There was also variation in the incidence of COVID-19 among different states in Nigeria and Federal Capital Territory with Lagos State and Federal Capital Territory sitting far on top of the table, and accounting for nearly half (47.48%) of the total COVID-19 pandemic in Nigeria. This is not surprising as both states house the two busiest airports in the country with the highest number of destinations in Nigeria. The explanations for these variations are possible due to the volume of international travels in the states, variation of populations in each state, the difference in testing capacities of each state,19 and largely the heterogeneous makeup of the Nigerian state.
Generally, the incidence of COVID-19 in Sub-Saharan Africa (except few cases) is relatively low as compared to the Americas, Asia, Europe, and North Africa. Before now, Africa has been predicted to be the most vulnerable continent in terms of COVID-19 infection and mortality and was predicted as the region where COVID-19 will have a major impact. The prediction was based on the continent’s weak health care system and large immune-compromised population.24,25 However the present reality proved the prediction otherwise. Some researchers have attributed the low impact of COVID-19 in the region to the low volume of air travel, large youthful population, favorable climate and immunity from prior immunizations, and poor report of events.26-28
The trend in COVID-19 in Nigeria showed a bimodal trend. This shows a pandemic that restarted after flattening, with the second rise representing the second wave of COVID-19.
The cumulative deaths recorded in Nigeria within the study period are 2,058. This value placed Nigeria as the 7th most-affected African country in terms of COVID-19 related deaths just after South Africa (52,648), Egypt (11,845), Tunisia (8,705), Algeria (3,077), Ethiopia (2,784) and Kenya (2,104) and the 79th most-affected country globally, accounting for 0.07% of COVID-19 related deaths globally. These values are far from those obtained in the Americas and Asia: USA (543,003), Brazil (307,112), Mexico (300,862) and India (161,552), that sits on top of the mortality table.
When adjusted for population, the cumulative deaths per 100,000 of the population in Nigeria is 1.0. This value is quite low when compared to other African countries such as South Africa (88.8), Tunisia (73.7), Eswatini (57.4), Cape Verde (29.7), and Botswana (21.5). This places Nigeria in the 153rd position globally on cumulative deaths per 100,000 of population. Higher values have been reported in United Kingdom (186.4), Mexico (155.8), Brazil (144.5), France (143.8), and India (11.7).9
The cumulative case fatality rate recorded in Nigeria within the study period is 1.30. This value is lower than the global case fatality rate of 2.2% (2,769,473/129,359,540) as of April 6. Higher values have been reported in Yemen (21.0%), Mexico (9.0%), Syria (6.7%), Sudan (6.5%), Egypt (5.9%), Ecuador (5.2%), China (4.7%), Bolivia (4.5%), Somalia (4.5%), Afghanistan (4.3%), Zimbabwe (4.1%), Liberia (4.1%), Tanzania (4.1%) and Bosnia and Herzegovina (3.8%).10 Generally, the case fatality rate of COVID-19 in sub-Saharan Africa (except few cases) is relatively low as compared to the Americas, Asia, Europe, and North Africa.
The prompt response to the COVID-19 pandemic is thought to be enhanced by previous pandemics such as Ebola.29 Amidst the pandemic and its response in Nigeria, varying lessons have been learned. Social mobilization using a multimodal approach was evident in Nigeria’s response to COVID-19. The efficacy of information dissemination via social media such as Facebook, Twitter, and WhatsApp has been documented30 and the response to COVID-19 portrayed this too, considering the fact that the use of smart phones and social media has become a norm even in resource-limited settings. This, therefore, calls for full utilization of social media to drive behavioral changes during disease outbreaks30 given “table full” of rumors that accompany outbreaks. Among these are rumors of the origin of the pandemic and cures for the disease. From the public health perspective, the present pandemic has made significant progressive modifications. Water and other sanitary materials are now provided in public places and hand hygiene has become part of the daily routine among Nigerians. This will go a long way if sustained to reduce the trend of other infectious diseases that anchor on poor hygiene. More so, despite the lockdowns, the use of technology for virtual meetings, teaching, and learning has impacted positively on the social and academic well-being of Nigerians. This has come to stay and is currently adopted in many spheres as the most preferred means for social gathering, business transactions, and educational systems.
Conclusions
This study has provided insight into epidemiological events, responses, combative measures, and lessons learned from the COVID-19 pandemic. Nigeria has a lower impact of COVID-19 on the population when compared to other countries in the Americas, Asia, and Europe. COVID-19 has been reported in all states in Nigeria as well as the Federal Capital Territory with much of the cases involving males. The majority of the cases were found in young persons. The case trend showed a bimodal form indicating a second wave occurrence. Nigeria government has initiated some combative measures as well as vaccine initiation.
Footnotes
Authors’ contributions statement: HUO conceived the study, performed data curation, performed literature search, performed data analysis, wrote the initial manuscript draft and drew all maps. COO performed data curation, performed data analysis, edited the original manuscript. RIE performed quality check and edited the initial manuscript data. DAA performed data curation, performed data analysis and edited the manuscript draft. GME performed quality check and edited the initial manuscript data. All authors read and approved the final version of the manuscript.
Conflicts of interest: All authors – none to declare.
Funding: None to declare.
Ethics approval and consent to participate: This study is based on analysis from secondary data, thus, did not require ethical clearance.
Availability of data and material: Datasets generated and analyzed in this study are within the article. The primary source of data, NCDC database is publicly available.
References
- 1.World Health Organization. Impact of COVID-19 on people’s livelihoods, their health and our food systems: Joint statement by ILO, FAO, IFAD and WHO. [Accessed on: 16 May 2021]. Available at: https://www.who.int/news/item/13-10-2020-impact-of-covid-19-on-people’s-livelihoods-their-health-and-our-food-systems.
- 2.Okafor UG, Olalaye MA, Asobara HC, Umeodinka EF. Global impact of COVID-19 pandemic on public health supply chains. IntechOpen. 2021 [Google Scholar]
- 3.Ogar CO, Okoroiwu HU, Obeagu EI, Etura JE, Abunimye DA. Assessment of blood supply and usage pre- and during COVID-19 pandemic: a lesson from non-voluntary donation. Transfus Clin Biol. 2021;28:68–72. doi: 10.1016/j.tracli.2020.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Okoroiwu HU, Okafor IM, Asemota EA, Ogar CO, Uchenna IK. Coping with COVID-19 pandemic in blood transfusion services in West Africa: the need to restrategize. Hematol Transfus Cell Ther. 2021;43:119–25. doi: 10.1016/j.htct.2021.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pley CM, McNaughton AL, Matthews PC, Lourenço J. The global impact of COVID-19 pandemic on the prevention, diagnosis and treatment of hepatitis B virus (HBV) infection. BMJ Global Health. 2021;6:e004275. doi: 10.1136/bmjgh-2020-004275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization. WHO Coronavirus (COVID-19) Dashboard. [Accessed on: 26 August 2021]. Available at: https://covid19.who.int/
- 7.Andam K, Edeh H, Oboh V, Pauw K, Thurlow J. Impacts of COVID-19 on food systems and poverty in Nigeria. Adv Food Secur Sustain. 2020;5:145–74. doi: 10.1016/bs.af2s.2020.09.002. [DOI] [Google Scholar]
- 8.Nigeria Centre for Disease Control. An update of COVID-19 outbreak in Nigeria. [Accessed on: 6 April 2021]. Available at: https://ncdc.gov.ng/diseases/sitreps/?cat=14&name=An%20update%20of%20COVID-19%20outbreak%20in%20Nigeria.
- 9.World Health Organization. COVID-19 weekly epidemiological update: data as received by WHO from national authorities, as of 28 March 2021, 10 am CET. [Google Scholar]
- 10.Okoroiwu HU, Uchendu IK, Ogar CO, Okafor IM. COVID-19 in Nigeria: situation update and combative measures taken by the government. Germs. 2020;10:274–8. doi: 10.18683/germs.2020.1218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nigeria Centre for Disease Control (NCDC) Government Laboratories. [Accessed on: 6 April 2021]. Available at: https://covid19.ncdc.gov.ng/laboratory/
- 12.Nigeria Centre for Disease Control (NCDC) Fee paying laboratories. [Accessed on: 6 April 2021]. Available at: https://covid19.ncdc.gov.ng/privatelabs/
- 13.Nigeria Center for Disease Control (NCDC) Nigeria Center for Disease Control. 2020. National Interim guidelines for Clinical Management of COVID-19. Version 3. [Google Scholar]
- 14.World Health Organization. COVID-19 vaccines shipped by COVAX arrived Nigeria. [Accessed on: 9 April 2021]. Available at: https://www.afro.who.int/news/covid-19-vaccines-shipped-covax-arrive-nigeria.
- 15.Enitan SS, Oyekale OA, Akele RY, et al. Assessment of knowledge, perception and readiness to participate in COVID-19 vaccine trial. Int J Vaccine Immun. 2020;4:1–13. [Google Scholar]
- 16.Eniade OD, Olarinmoye A, Otovwe A, Akintunde FE, Okedare OO, Aniyeloye AO. Willingness to accept COVID-19 vaccine and its determinants among Nigerian citizens: a web based cross sectional study. J Adv Med Med Res. 2021;33:13–22. doi: 10.9734/jammr/2021/v33i830881. [DOI] [Google Scholar]
- 17.World Health Organization. Nigeria Youth call for action to improve adolescent’s health: Deliberations center on revitalizing healthcare services threatened by COVID-19. [Accessed on: 10 April 2021]. Available at: https://www.who.int/pmnch/media/news/2021/nigeria-adolescent-health/en/
- 18.Balasubramanian S, Rao NM, Goenka A, Roderick M, Ramanan AV. Coronavirus disease 2019 (COVID-19) in children - what we know so far and what we do not. Indian Pediatr. 2020;57:435–42. doi: 10.1007/s13312-020-1819-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Elimian KO, Ochu CL, Ilori E, et al. Descriptive epidemiology of coronavirus disease 2019 in Nigeria, 27 February - 6 June 2020. Epidemiol Infect. 2020:148–e208. doi: 10.1017/S095026882000206X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.World Health Organization. Africa. Weekly bulletin on outbreaks and other emergencies. 2020;23:1–7. [Google Scholar]
- 21.Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Grasseli G, Zangrillo A, Zanela A, et al. Baseline characteristics and outcomes of 1591 patients infected with SaRS-CoV-2 admitted to ICUs of the Lombardy Region, Italy. JAMA. 2020;323:1574–81. doi: 10.1001/jama.2020.5394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Patel SK, Velkoska E, Burrell LM. Emerging markers in cardiovascular disease: where does angiotensin-converting enzymes 2 fit? Clin Exp Pharmacol Physiol. 2013;40:551–9. doi: 10.1111/1440-1681.12069. [DOI] [PubMed] [Google Scholar]
- 24.Lone SA, Ahmed A. COVID-19 pandemic in African perspective. Emerg Microbes Infect. 2020;9:1300–8. doi: 10.1080/22221751.2020.1775132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.World Economic Forum. Why Sub-Sahara Africa needs a unique response to COVID-19. [Accessed on: 9 April 2021]. Available at: https://www.nytimes.com/2020/03/17/world/africa/coronavirus-africa-burkina-faso.html.
- 26.David JB, Andriano L, Brazel DM, et al. Demographic science aids in understanding the spread and fatality rates of COVID-19. Proc Natl Acad Sci USA. 2020;117:9696–8. doi: 10.1073/pnas.2004911117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sadaji MM, Habibzabeh P, Vintzileos A, Shokouli S, Miralles-Wilhelm,Amoroso A. Temperature, humidity, latitude analysis to estimate potential spread and seasonality of coronavirus disease 2019 (COVID-19) JAMA Netw Open. 2020;3:e2011834. doi: 10.1001/jamanetworkopen.2020.11834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Escobar LE, Molina-Crus A, Barillas-Murry C. BCG vaccine protection from severe coronavirus disease 2019 (COVID-19) Proc Natl Acad Sci USA. 2020;117:17720–6. doi: 10.1073/pnas.2008410117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Abayomi A, Balogun MR, Bankole M, et al. From Ebola to COVID-19: emergency preparedness and response plans and actions in Lagos, Nigeria. Global Health. 2021;17:79. doi: 10.1186/s12992-021-00728-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Otu A, Ameh S, Osifo-Dawodu E, Alade E, Ekuri S, Idris J. An account of the Ebola virus disease outbreak in Nigeria: implications and lessons learnt. BMC Public Health. 2017;18:3. doi: 10.1186/s12889-017-4535-x. [DOI] [PMC free article] [PubMed] [Google Scholar]