Abstract
Objective:
Sleep problems among youth are highly prevalent and associated with adjustment difficulties. When considering influences on youth’s sleep, bidirectional links between youth’s sleep health and family functioning have been suggested. Parenting practices are among the many familial factors that could be transactionally related to poor sleep in youth; however, research is lacking on potential longitudinal associations between parenting practices and sleep problems in youth. Additionally, sensitive periods for this link are mostly unknown. The current study examined longitudinal relations between constellations of parenting practices and youth sleep health to identify profiles of parenting practices that are predictive of sleep problems in youth across different developmental stages.
Method:
Participants were 292 parents (M = 36.51, SD = 7.3) of children between the ages of 3 and 14 (M = 8.4, SD = 3.6). A person-centered approach was employed to create profiles across traditionally-labeled positive and negative parenting practices, as well as supportive and unsupportive parental emotion socialization strategies. Parenting profiles were then examined as longitudinal predictors of youth sleep problems.
Results:
Findings revealed three distinct parenting profiles, which were differentially associated with sleep problems in youth, with the first profile predicting the lowest levels of sleep problems and the third profile predicting the highest levels of sleep problems, particularly among peripubertal youth.
Conclusion:
This study extends previous findings by elucidating distinct constellations of parenting practices that are differentially predictive of youth sleep problems and highlighting parenting among the various family processes that can longitudinally contribute to youth’s sleep health.
Keywords: Parenting, youth sleep health, youth sleep problems
Sleep problems among youth are highly prevalent and associated with difficulties across several developmental domains (e.g., emotional, behavioral, cognitive, and physical health).1,2 Indeed, sleep problems (e.g., insufficient sleep, poor quality sleep) are pervasive in mental health disorders and among the most prominent clinical symptoms of several mood and anxiety disorders.3 Further, sleep health, characterized by dimensions of duration, regularity, satisfaction, alertness, timing, and efficiency4, is a pivotal predictor of socioemotional adjustment,5 and evidence supports that dimensions in sleep health that are problematic may precede internalizing pathology in childhood and adolescence.6 Specifically, poor sleep in youth has been demonstrated to prospectively predict depression7, suicide8, risk taking behavior8, and low academic achievement9 among other negative outcomes. Consequently, sleep problems in youth are recognized as a serious health risk and public health concern that necessitates urgent attention.10
Youth’s Sleep Within the Context of Family Functioning and Parenting
Attempts at elucidating contributors to poor sleep health in youth have identified family functioning as intrinsically interconnected with youth’s sleep behaviors.5 For example, research has demonstrated higher youth sleep problems in families with high levels of conflict and parenting stress. Conversely, youth who live in supportive family environments sleep better and longer.5 Research on the influence of family functioning on youth’s sleep has predominantly considered parenting behaviors and the parent-youth relationship.11 For instance, parental monitoring of sleep-wake activities (e.g., bedtime routine) has been linked to longer sleep duration in youth.12 Conversely, parent-child interactions that lack consistent limit setting, especially during bedtime routines, have been associated with youth bedtime resistance, difficulty initiating sleep, and nightmares.13 Importantly, parenting practices are among the various family processes that transactionally influence one another to impact youth’s sleep. Consequently, it is important to emphasize the reciprocal nature of the relationship between children’s sleep and parenting practices given the possibility that youth’s individual characteristics could similarly influence parents’ behavior. Correspondingly, youth sleep problems have been demonstrated to predict increased maternal negativity and decreased maternal sensitivity and closeness, highlighting the bidirectional association between youth sleep problems and parenting practices.14
Although research has linked general parenting behaviors, including behavioral control (i.e., structured nighttime routine), to youth sleep health, there has been scant attention to how emotion-related parenting practices may be related to sleep.15 Emotion socialization (ES) behaviors encompass the myriad ways parents teach their children about emotion identification, expression, and modulation.16 A large body of research has focused specifically on parental reactions to youth emotion. For example, parental nonsupportive reactions (i.e., dismissive, critical, punitive) to youth negative emotions (i.e., distress, sadness, anger) have been associated with less skillful emotion regulation, emotional overarousal, and heightened distress in youth,15,17 which could potentially manifest in sleep problems. Alternatively, emotion-related aspects of parenting, such as emotional responsiveness, warmth, and supportiveness have been shown to predict youths’ development of skillful regulation of emotions17 which, in turn, could protect against sleep problems.
Theoretically, and consistent with transactional and ecological models, parenting environments perceived as conflicted, unstable, and stressful result in vigilant states in youth that directly oppose sleep processes and can therefore disrupt sleep.5 More specifically, negative parenting practices can undermine youth’s ability to manage negative emotions and thereby affect their psychological wellbeing through greater emotional dysregulation and poor emotion-related coping,18 which may in turn lead to vigilant states known to disrupt sleep.19 Accordingly, harsh parenting (e.g., psychological control, hostility) has been previously linked to youth sleep problems.20 Additionally, mother-child relationships characterized by greater conflict and less closeness have been associated with greater sleep problems in children.14 Conversely, positive parenting practices (e.g., warmth, closeness, clear limit setting, monitoring) have been linked to more optimal sleep in children.14
Collectively, research findings support a contribution of parenting to youth sleep health and highlight the need to target parenting practices to improve youth sleep problems and associated emotional and behavioral difficulties. However, research is lacking on the type of parenting practices that most strongly predict youth’s sleep health. Further, the majority of research on parenting practices and children’s sleep has been exclusively conducted with infants and young children,5 which widens the research gap on the nature of the relations between parenting and youth’s sleep at other developmental stages. Importantly, growing evidence suggests youth sleep health is increasingly vulnerable to disruption around specific developmental periods (e.g., early adolescence),6 which warrants examination of familial factors that contribute to disrupted sleep in youth at different stages. Unfortunately, sensitive developmental periods for the relationship between parenting practices and youth sleep health are mostly unknown.
Scarce data on longitudinal models of parenting practices and youth’s sleep at different developmental stages limit the clinical applicability of research findings on how to offer parents interventions that are tailored to optimize sleep health in youth at various stages of development. The identification of key parenting practices that impact youth’s sleep health throughout development is integral to enhance interventions that address poor sleep and accompanying mental health difficulties in youth. Specifically, examining dynamics between positive (e.g., warmth, supportiveness) and negative (e.g., hostility, laxness) parenting, as well as ES practices and youth’s sleep health, may explain under which parenting conditions youth’s sleep health suffers or thrives across development. In turn, the literature on youth sleep warrants expansion on conceptual models, especially longitudinal designs, that can serve to inform interventions aiming to promote youths emotional and behavioral health by enhancing their sleep health. A thorough understanding of how constellations of parenting practices promote or stifle sleep health is not only uncharted research territory, but important to attempt to reduce the high prevalence of sleep problems in youth and thereby prevent psychosocial problems that ubiquitously coexist with disrupted sleep in youth.
The current longitudinal study examined the relationship between parenting and youth’s sleep problems. This study utilized a person-centered approach to identify profiles of parenting practices and ES strategies that are most predictive of sleep problems in youth. To explicate possible developmental differences and potentially discern sensitive periods, we investigated whether associations between distinct constellations of parenting practices and youth sleep problems differ across age groups. We predicted that positive and emotionally supportive parenting practices would predict lower levels of sleep problems in youth across all age groups. Conversely, we predicted that negative and emotionally unsupportive parenting practices would predict higher levels of sleep problems in youth across all age groups. Lastly, we explored predictors of parenting profile membership to examine the influence of family income, parent and youth sex, and youth internalizing and externalizing problems on profile membership probability.
Method
A sample of 292 parents of children between the ages of 3 and 14 from a larger study on the assessment of parenting were used for the current study. The parent study included a community sample of 564 parents who were recruited online through Amazon’s Mechanical Turk (MTurk) and completed electronic surveys at four waves throughout a 12-month period. Demographic information for the current study’s sample is presented in Table 1. Given the community sample, only 16% of children were reported to experience clinically significant internalizing and externalizing pathology. The current study examined data collected at the third (8-months) and fourth (12-month) waves as a relevant measure of ES was first incorporated at the third wave. Missing data were less than 1% for all study variables. Full maximum likelihood estimation techniques were utilized to include all available data.
Table 1.
Descriptive Statistics of the Parenting Profiles
| Descriptive Statistics of the Participants | |
|---|---|
| Demographic Characteristic | M (SD) or % N = 292 |
| Child Age | 8.4 (3.6, ) |
| Child Sex (% Female) | 50.3 |
| Parent Age | 36.51 (7.3) |
| Parent Sex (% Mothers) | 60.8 |
| Parent Race/Ethnicity | |
| White | 82 |
| Black | 8.9 |
| Latinx | 5.1 |
| Asian | 3 |
| Other | 1 |
| Family Structure | |
| Single | 16.8 |
| Cohabitating | 63.5 |
| Married | 17.9 |
| Family Income | |
| Under $30,000 | 21.7 |
| $30,000 – $49,000 | 28.7 |
| $50,000 – $69,000 | 19.5 |
| $70,000 – $99,000 | 16.8 |
| $100,000 or more | 13.3 |
| Parent Education | |
| Did not complete H.S | 0.6 |
| H.S or GED | 13.9 |
| Some College | 26.7 |
| College Degree | 41.8 |
| More than College Degree | 15.7 |
Note: H.S High School
Procedure
MTurk, a dominant crowdsourcing application in the social sciences, was utilized to recruit parents and obtain study data. Inclusion criteria included being a parent of a child between the ages 3 and 17, who resided in the United States. Additionally, a minimum of 95% task approval rate was required, a criterion that ensures a high-quality sample of users with better reputations (i.e., approval rating) due to a history of consistently passing attention checks at a high rate, responding in less socially desirable manners, and providing reliable responses to questionnaires similar to those of “traditional” samples. Prior research has demonstrated that obtaining data from parents through crowdsourcing methods is as reliable as obtaining data through more traditional data collection methods.21 Parents consented online prior to completing the survey following approved Institutional Review Board procedures. A 12-month study involving the completion of five surveys was listed on MTurk for which participants were compensated a total of $22 for completing surveys.
To ensure that parents’ responses were not random, ten attention check items were included in the survey. Participants were excluded from the current study for having more than one incorrect response on these items. In addition, participants were also excluded for failing to report the same demographic characteristics across study waves. The 53 participants excluded were not included in the total sample above.
Measures
Demographic Information.
Parents responded to demographic questions about themselves (e.g., education, age). their children (e.g., sex, age) and families (e.g., household income).
Youth Sleep Problems.
A shortened version of the Children’s Sleep Habits Questionnaire (CSHQ)22 was used to measure youth sleep problems. The CSHQ is a widely used parent-report measure of youth sleep behavior that includes items relating to key sleep domains that encompass clinical sleep complaints (e.g., bedtime behavior, sleep onset and duration). The CSHQ has been demonstrated to correlate with objective measurements of sleep functioning and has been shown to be both reliable and valid in community and clinical samples. Parents reported the frequency of sleep behavior for the most recent or “typical” week on a four-point Likert scale that included the following response options: usually (5–7 times per week), sometimes (2–4 times per week), rarely (0–1 time per week), and never (less than once a week). The shortened version of the CSHQ inquired about sleep latency (i.e., amount of time it takes to fall asleep), consistency of sleep timing, continuity of sleep (i.e., amount of sleep versus wakefulness during sleep period), sleep efficiency (i.e., ratio of total sleep time to amount of time spent in bed), and daytime sleepiness. Higher scores represented greater sleep problems in youth. Given our interest in examining levels of problems across various sleep dimensions, we utilized a Total Sleep Disturbances index to reflect overall sleep problems in youth. A total score above 14 was used as the clinical cut-off which corresponded to one SD above the mean, similar to the clinical sleep population mean used in the original CSHQ study. Cronbach’s alpha in the current sample averaged 0.70 across both waves.
Youth Internalizing and Externalizing Problems.
Parents completed the 19-item Brief Problem Monitor23 which comprises items from the Child Behavior Checklist and Youth Self-Report23 and examines both internalizing and externalizing pathology. Excellent internal consistency test re-test reliability, and validity of the BPM has been previously demonstrated.23 Internal consistency for subscales at the third and fourth waves ranged from .82 to .88.
Parenting Practices.
The Multidimensional Assessment of Parenting Scale (MAPS)21 is a self-report measure of parenting practices, whose 34 items were selected and subsequently adapted from well-established parenting scales. The Broadband Positive Parenting factor of the MAPS includes four narrowband subscales: Proactive Parenting, Positive Reinforcement, Warmth, and Supportiveness. The Broadband Negative Parenting factor includes three narrowband subscales: Hostility, Physical Control, and Lax Control. The MAPS has demonstrated strong reliability, and longitudinal examinations have provided support for its subscales’ validity.21 Cronbach’s alphas in the current sample were 0.93 and 0.88 for the Positive and Negative Parenting domains, respectively.
Emotion Socialization Strategies.
The Coping with Children’s Negative Emotions Scale (CCNES)24 is a self-report measure that includes 12 hypothetical emotionally evocative scenarios for youth in which caregivers rate how they would respond to their children’s negative emotions (e.g., distress, fear). The CCNES includes six ways in which parents can respond to their children’s negative emotions and these include (1) emotion-focused reactions, which represent parental responses to make the child feel better, (2) problem-focused reactions, which represent parental responses to help the child solve a problem that caused his/her distress, (3) expressive encouragement, which represents parental responses that validate children’s emotions while encouraging expression of negative affect, (4) distress reactions, which captures the distress experienced by parents when children express negative affect, (5) punitive reactions, which represent punitive parental responses to decrease exposure to children’s negative affect, and (6) minimization reactions, which represent parental responses that minimize or devalue the situation and children’s distress from it. The six subscales were grouped into the two broader domains of supportive (i.e., expressive encouragement, emotion-focused and problem-focused reactions) and unsupportive ES practices (i.e., distress, minimization, punitive reactions). The CCNES has previously demonstrated good internal and test-retest reliability as well as sensitivity to change over time.25 Cronbach’s alphas for the current sample were .0.95 and 0.90 for the supportive and unsupportive domains, respectively.
Data Analytic Plan
Latent Profile Analysis (LPA) was conducted to identify profiles of parenting practices and their association with indices of youth sleep health. LPA analyses allow variables to cluster that have similar indicator means and variances in order to identify group patterns. Specifically, the goal of LPA is to determine the most accurate number of profiles to describe the associations within the observed variables.26
Profile Enumeration.
In order to determine the optimal number of profiles, we utilized the Lo-Mendel-Ruben adjusted likelihood ratio test (LMR-A), the bootstrap likelihood ratio test (BLRT), the Bayesian Information Criterion (BIC), the Akaike Information Criteria (AIC), the consistent Akaike Information Criteria (CAIC), the sample size adjusted BIC (ssBIC), and entropy to select the best fitting model (see Table 2). Specifically, the LMR-A indicates statistically significant improvements (p-value < .05) in a model in comparison to the model with one fewer profile.27 Similarly, a statistically significant BLRT indicates superiority of a model when compared to the model with one fewer profile.27 The AIC, consistent AIC (cAIC), BIC, and sample size adjusted BIC (ssBIC) aid in determining model fit, with lower values on each index indicating better relative fit. Further, entropy determines the accuracy of classifying individuals into the profiles identified in each model, with values closer to 1 indicating more certainty in group division. Importantly, the determination of number of constellations or profiles of parenting practices should be theoretically-driven and informed.
Table 2.
LPA Model Fit Indices.
| Parsimony Criteria | LRT p Value | |||||||
|---|---|---|---|---|---|---|---|---|
| Profiles | LL | Entropy | AIC | BIC | ssBIC | CAIC | LMRa | BLRT |
| 1 | −1638.29 | -- | 3292.58 | 3321.99 | 2396.62 | 3329.99 | -- | -- |
| 2 | −1473.17 | .739 | 2980.35 | 3042.85 | 2988.94 | 3059.85 | .004 | .000 |
| 3 | −1407.99 | .810 | 2867.99 | 2963.58 | 2881.13 | 2989.58 | .139 | .000 |
| 4 | −1384.39 | .780 | 2838.79 | 2967.47 | 2856.48 | 3002.47 | .012 | .100 |
| 5 | −1363.62 | .779 | 2815.23 | 2977.01 | 2837.48 | 3021.02 | .021 | .150 |
Predicting Distal Outcomes.
When examining parenting profiles as predictors of youth sleep health, profile identification is often conducted through “hard classification,” that is, fixing individuals to a profile where they had the highest likelihood of membership. For the current study, we employed Vermunt’s three-step approach in Mplus.28 Specifically, once profiles were determined, cases were assigned to these profiles based on posterior probabilities. Following that, family, parent, and youth covariates were introduced as predictors of the categorical latent class variable without needing to hard-classify nor resulting in distortion of profiles. Finally, we used a three-step approach34 to examine the cross-sectional and longitudinal impact of latent parenting profiles on youth sleep problems. Specifically, youth sleep problems at baseline and at the 4-month wave (mean centered), and the stability of youth sleep problems across time were included at the latent class level so that estimates were unbiased by classification inaccuracy and without distorting class solution.
Results
Latent Profiles.
Latent profile analyses (LPA) were conducted using Mplus version 8.3. Parenting practices, parent ES strategies, and youth sleep problems were converted into z-scores. Every profile indicator was entered into the LPA models, which ranged from one to five profiles and were run with 200 random starts. Fit indices for the five profiles are presented in Table 2. The three-, four-, and five-profile models all exhibited appropriate entropy. However, the three-profile model had superior fit compared to other models for the bootstrapped LRT, BIC, and entropy and represented the model that is most theoretically robust and empirically defensible (see Figure 1 for complete profiles). The four and five-class models had the same three primary classes and introduced classes that did not meaningfully add to the interpretation of the results. Thus, the three-class model was selected for further analysis.
Figure 1.
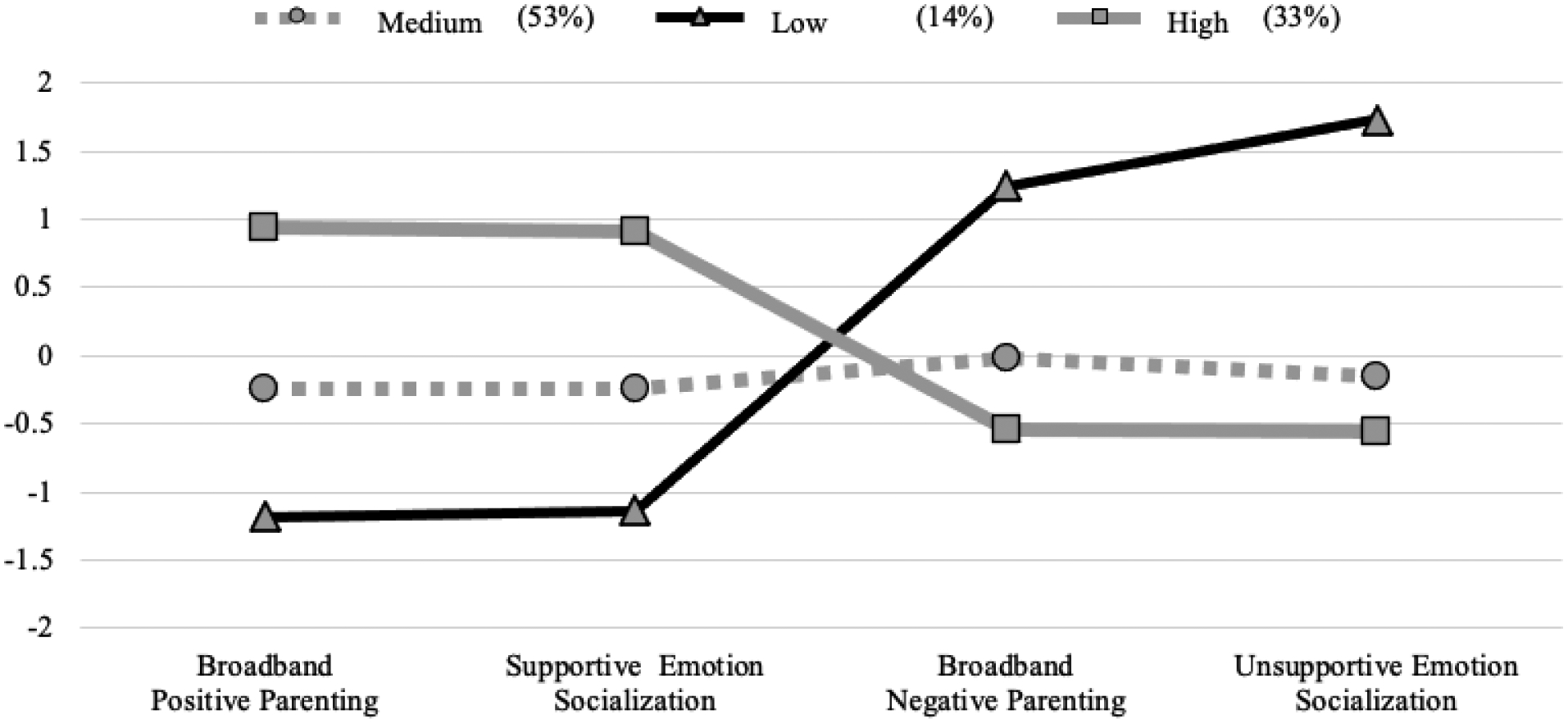
Z-Scored Parenting Practices and Parent Emotion Socialization Strategies within Three Latent Profiles.
The first parenting profile (33%), labeled as “High Support” was characterized as having the highest levels of positive parenting practices and supportive ES strategies paired with the lowest levels of negative parenting practices and unsupportive ES strategies. In contrast, the third parenting profile (14%), labeled as “Low Support” was characterized as having the lowest levels of positive parenting and supportive ES practices and highest levels of negative parenting and unsupportive ES practices. The second parenting profile (53%), labeled as “Medium Support” demonstrated moderate levels of positive and negative parenting practices as well as moderate levels of supportive and unsupportive ES strategies. More specifically, the Medium Support profile exhibited higher levels of negative parenting practices than the High Support profile (Cohen’s d = .67 to .71), but much lower than the Low Support profile (d = 1.66 to 3.05). Additionally, the difference in positive parenting between the Medium Support profile and both the High Support (d = −1.77) and Low Support (d = 1.36) was substantial.
Overall, LPA results supported three clearly delineated parenting profiles that longitudinally predict youth sleep problems. Following profile enumeration, we explored family (e.g., SES), parent (i.e., sex), and youth (i.e., age, sex, and problem behavior) predictors of parenting profile membership using multinomial logistic regression via Vermunt’s three-step approach28 in Mplus (see Table 3 for complete results).
Table 3.
Predictors of profile membership.
| Effect | Estimate | SE | OR | 95% CI |
|---|---|---|---|---|
| Medium vs. High | ||||
| Child Sex | −.164 | .340 | .849 | .436, 1.65 |
| Child Age | .104 | .050 | 1.11 | 1.01, 1.22 |
| Parent Sex | .596 | .596 | 1.82 | .845, 3.90 |
| Family Income | .068 | .068 | 1.07 | .956, 1.19 |
| Child Externalizing Problems | .286 | .286 | 1.33 | 1.00, 1.77 |
| Child Internalizing Problems | .063 | .063 | 1.07 | .856, 1.36 |
| Low vs. High | ||||
| Child Sex | .149 | .507 | 1.16 | .430, 3.13 |
| Child Age | .105 | .070 | 1.11 | .968, 1.28 |
| Parent Sex | 1.27 | .544 | 3.54 | 1.22, 10.3 |
| Family Income | .020 | .098 | 1.02 | .841, 1.23 |
| Child Externalizing Problems | .514 | .154 | 1.67 | 1.24, 2.26 |
| Child Internalizing Problems | .118 | .134 | 1.13 | .865, 1.46 |
Family income (a proxy for family SES), youth sex, and youth internalizing problems (e.g., anxiety, depression) were not associated with parenting profile probability (ps > .10). However, youth age was associated with parenting profile such that the odds of being in the Medium or Low Support profile, relative to the High Support profile, increased by 11% for every year youth got older. Specifically, the probability of a parent being in the High Support profile was approximately 45% for parents of young children (i.e., 3–8 years-old), but only 28% for parents of peri-pubertal youth (i.e., 9–14 years-old). Additionally, parent sex was associated with parenting profile such that fathers were more likely to be in the Low Support profile relative to mothers. Lastly, youth externalizing problems (e.g., defiance, aggression) was associated with parenting profile such that the odds of being in either the Medium or Low Support profiles, relative to the High Support profile, increased with higher levels of youth externalizing problems.
Youth Sleep Problems Outcomes.
Next, we used a three-step approach28 to examine the cross-sectional and longitudinal impact of latent parenting profiles on youth sleep problems. Wald’s chi-square tests of parameter equality results indicated significant cross-sectional, Wald χ2= 10.18(2), p = .006, and longitudinal, Wald χ2= 8.19(2), p = .017, differences in youth sleep problems. Longitudinally, the parents in the High Support profile reported that their children had the lowest levels of sleep problems (m = 10.74, 95% CI 10.12, 11.35), as compared to the Medium (m = 11.6, CI 11.09, 12.1) and Low Support parenting profiles (m = 13.31, CI 12.3, 14.3). A similar pattern of means emerged for cross-sectional associations. As expected, the Low Support parenting profile predicted the highest levels of sleep problems in youth. The differences in youth sleep problems between the High and Medium Support profiles was small (d = .29) whereas the youth sleep problems differences between the High Support and Low Support profiles was large (d = .88) – 50% of youth of parents in the Low Support parenting profile were classified as having clinically elevated sleep problems relative to 12.5% of youth of parents in the High Support parenting profile. Of note, 21.4% and 26.3% of youth were reported to have sleep disturbances above the clinical cutoff in wave 3 and 4, respectively.
Lastly, we explored if youth age moderated the association between parenting profile and youth sleep problems by estimating distal outcomes separately for two youth developmental stages (i.e., childhood: 3–8-years-old, peripuberty: 9–14-years-old). The association between parenting profile and youth sleep problems was significant for peripubertal youth, Wald χ2= 9.16(2), p = .010, but not for younger children, Wald χ2= 2.29(2), p = .318. Although the pattern of results was similar across developmental stages, the difference in sleep problems between the parenting profiles was most pronounced for peri-pubertal youth such that the Low Support parenting profile had its most detrimental impact on youth sleep health during peripuberty (see Figure 1). Intercorrelations among study variables are presented in Table 4.
Table 4.
Intercorrelations Between Study Variables
| M (SD) | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 8-Month Wave | ||||||||||||||
| 1. Sleep Problems | 11.6 (2.9) | 1 | ||||||||||||
| 2. Externalizing Problems | 1.84 (2.4) | .29** | 1 | |||||||||||
| 3. Internalizing Problems | 1.46 (2.1) | .34** | .41** | 1 | ||||||||||
| 4. Positive Parenting | 4.14 (.55) | −.29** | −.25** | −.21** | 1 | |||||||||
| 5. Negative Parenting | 1.83 (.47) | .29** | .46** | .27** | −.39** | 1 | ||||||||
| 6. Supportive ES | 5.21 (.93) | −.20** | −.19** | −.05 | .69** | −.36** | 1 | |||||||
| 7. Unsupportive ES | 2.39 (.68) | .26** | .32** | .18** | −.45** | .53** | −.42** | 1 | ||||||
| 12-Month Wave | ||||||||||||||
| 8. Sleep Problems | 11.87 (3.2) | .60** | .34** | .31** | .35** | .36** | −.19** | .28** | 1 | |||||
| 9. Externalizing | 1.82 (2.5) | .38** | .73** | .31** | −.29** | .46** | −.27** | .35** | .39** | 1 | ||||
| 10. Internalizing | 1.65 (2.2) | .31** | .38** | .78** | −.29** | .29** | −.15** | .28** | .34** | .43** | 1 | |||
| 11. Positive Parenting | 4.13 (.55) | −.29** | −.26** | −.18* | .80** | −.36** | .65** | −.42** | −.35** | −.23** | −.21** | 1 | ||
| 12. Negative Parenting | 1.83 (.48) | .27** | .48** | .22** | −.35** | .82* | −.38* | .49** | .38** | .54** | .32** | −.36** | 1 | |
| 13. Supportive ES | 5.21 (.94) | −.16** | −.26** | −.03 | .62** | −.34** | .81** | −.41** | −.22** | −.11** | −.22** | .68** | −.36** | 1 |
| 14. Unsupportive ES | 2.39 (.71) | .19** | .31** | .14* | −.37** | .42** | −.45** | .78** | .22** | .33** | .25** | −.42** | .52** | −.51** |
Note: Intercorrelations are Pearson correlations, which are Point-Biserial correlations.
p < .05.
p < .01. ES = Emotion Socialization
Discussion
The current study utilized a person-centered approach to identify profiles of parenting practices that differentially predict youth sleep problems. Specifically, we examined cross-sectional and longitudinal relations between distinct profiles of parenting practices and sleep problems in young children, school-age children, and peri-pubertal youth. Findings supported a three-profile model. Consistent with our hypothesis, we identified a profile of parenting that was cross-sectionally and longitudinally associated with the lowest levels of sleep problems in youth. Specifically, this profile, labeled as “High Support”, was characterized as having the highest levels of positive parenting practices and supportive ES strategies paired with the lowest levels of negative parenting practices and unsupportive ES strategies, relative to the other two parenting profiles. Conversely, we identified a profile of parenting that was cross-sectionally and longitudinally associated with the highest levels of sleep problems in youth, labeled as “Low Support”. This profile was characterized as having the lowest levels of positive parenting and supportive ES practices and highest levels of negative parenting and unsupportive ES practices (see Figure 1). Lastly, the most common parenting profile, labeled as “Medium Support”, was characterized as having moderate levels of positive and negative parenting practices. This parenting profile predicted higher levels of youth sleep problems than the High Support profile, but lower than the Low Support profile.
Findings demonstrating that the High Support and Low Support parenting profiles differentially predicted sleep problems expands the literature on children’s sleep by highlighting the influence of positive parent-youth interactions on youth sleep health. Evidently, positive parenting practices may likely protect youth against sleep problems otherwise associated with negative parenting practices and/or dysfunctional family dynamics. Importantly, our findings are consistent with previous research highlighting the benefit of parental warmth, structure, and monitoring on youth’s sleep’s health.29 Our findings also support previous theoretical propositions and empirical work by highlighting the role of maladjusted family relationships on disrupted sleep through possible increased vigilant states (e.g., concern, worry) and environmental threats (e.g., parent-youth conflict, parental nonsupportive reactions to youth distress) experienced by youth.19 Our results expand the scant longitudinal area of inquiry of parenting and youth sleep by underscoring the quality of parenting practices and parent-youth interactions as important intervention targets, which have been largely unexplored in the behavioral treatment of disturbed sleep in youth. Indeed, youth sleep interventions generally have not targeted the quality of parenting practices directly, but rather mostly involved parents by providing them with sleep education and/or encouraging parent-set bedtimes.29 Our results demonstrate a differential impact of distinct parenting profiles on youth sleep problems, highlighting the need to offer families parenting interventions that are tailored to promoting healthy sleep habits through reductions in parent-youth conflict and related improvements in youth physiological states needed for sleeping. Notably, children’s sleep health is embedded in the family milieu and parenting practices are merely one of the many family processes that ongoingly and bidirectionally relate to youth’s poor sleep.5 Further research is needed to conceptualize youth’s sleep health using a transactional framework to disentangle the mechanisms whereby children’s sleep-wake behaviors and parenting practices reciprocally influence one another.
Importantly, our moderation results demonstrated an increasingly detrimental effect of the Low Support profile on youth sleep health during peripuberty (9–14 years-old). In other words, the negative sequalae of negative and unsupportive parenting practices on youth disturbed sleep became more pronounced as youth got older and was only statistically significant for peripubertal youth. This is concerning given that biological and social changes lead to a normative increase in insufficient sleep, social jetlag (changes in sleep timing from weekdays to weekends), and other sleep related problems during the interval of time surrounding the onset of puberty.6 Our results suggest that, although addressing parenting practices in the context of child sleep interventions throughout development is critical, the peripuberty period might present as a crucial developmental time to modify suboptimal parenting practices in hopes of improving youth sleep. Undeniably, parents will diminish their supervision and involvement in regulating their children’s sleep-related behavior as youth grow older. However, parents continue to influence their children’s sleep habits (e.g., sleep-wake routines, social media use), which suggests that continued work in this area is important. Indeed, previous literature indicates that adolescents’ sleep health greatly benefits from parental monitoring and structure around sleep-wake behaviors.29 However, without proper tools and education at parents’ disposal, instilling enforcement measures surrounding sleep routines is likely to be an area of conflict within the family, which ironically can serve to worsen problems with sleep by impeding the necessary low-arousal emotional state needed for adequate sleep. In turn, the identification of parenting profiles that most likely relate to disturbed sleep in youth supports the goal of refining intervention efforts by allowing personalization of services through the emphasis on modifying maladaptive parenting practices that perpetuate sleep problems in youth, paying particular attention to dynamics of youth at developmental risk for disturbed sleep. Certainly, future research that integrates family functioning and youth’s sleep into models of child development is needed. To that aim, developmental models of sleep should incorporate findings on bidirectional links between shifts in the parent-youth relationship and youth sleep health across development as parenting practices could similarly be influenced by youth’s sleep and other individual characteristics, resulting in a transactional system of influence reinforced by both children’s and parents’ behaviors
Further, examinations of predictors of profile membership indicated that fathers were more likely to be in the Low Support profile. This finding reinforces the need to cast the net more broadly when it comes to measuring parenting practices in mothers and fathers, which could clarify different parent-youth dynamics that may occur based on the role or sex of the parent. Undoubtedly, given the high variability in household composition and family structure, future research is needed to ascertain the differential influence of multiple family relationships on youth’s sleep. Additionally, results demonstrated increased odds of being in the Medium and Low Support profiles in parents of youth with higher levels of externalizing problems. This finding is consistent with prior research suggesting transactional influences between children’s externalizing behavior and parenting quality31 and with recent data linking parent ES behaviors to youth conduct problems.32 Reciprocal influences between parenting practices and youth externalizing problems as well as established associations between externalizing behaviors and youth sleep problems further reinforce the potential of modifying parenting behaviors to not only promote adequate sleep, but also behavioral and emotional health in youth. Unexpectedly, youth internalizing problems were not associated with parenting profile probability, a surprising finding that may be related to reporter bias by parents given evidence of higher informant disagreement on youth internalizing pathology.33 Future work should include multiple informants to clarify reciprocal effects among parenting practices and youth psychopathology within the context of youth sleep functioning. Lastly, family income (proxy for SES) was not associated with parenting profile probability. Future research with larger samples should explore whether associations between parenting practices and youth sleep are moderated by SES and/or adversity.
It is important to interpret the current findings in light of the study’s limitations. First, a limitation includes lack of data on history of youth sleep disturbances as well as on medical conditions that may impact sleep, hampering our ability to draw specific conclusions on the directionality of the parenting practices-youth sleep problems relationship. This is important given links between neurodevelopmental disorders34 and sleep problems as well as sleep disorders (e.g., obstructive sleep apnea)34 and psychopathology. Future research should include such data to better inform models on youth’s sleep health within the family environment. Second, we obtained the study’s data through a single reporter, increasing the risk of shared method variance and possibly resulting in skewed reports of parenting practices and youth’s sleep due to social desirability biases and possible limited knowledge on youth’s sleep habits, particularly those of older children. Nevertheless, our findings are consistent with previous research demonstrating an association between parenting and youth sleep health using multiple informants and observational measurements of parenting.35,14 Future research should include reports by youth and additional caregivers. Obtaining information on adolescent’s perceptions of parenting practices might shed light on the consistency of parenting practices within the rearing environment. Although research suggests that parents and adolescents generally agree on their reports of parenting, there is evidence that adolescent report of negative parenting is more congruent with independent observations of parenting practices.36 As such, the adolescent perspective could more clearly illuminate potential dysfunctional parent-child transactional dynamics that interfere with youth’s sleep. Third, we measured sleep problems based on caregiver’s report on an abbreviated version of the CSHQ. The growth of the literature on youth sleep health warrants strong assessment of youth sleep health dimensions4 through objective methodology (e.g., actigraphy) in future investigations. Fourth, although the longitudinal nature of the study is a notable strength, the non-experimental design prevents us from making definitive causal conclusions due to potential intervening variables. Future research should examine whether the experimental modification of parenting practices results in reduced sleep problems in youth. Lastly, our sample did not exclusively include youth with clinically elevated sleep problems nor clinically significant borderline or clinical psychopathology. There is a continued need to examine the link between parenting practices on youth sleep health in clinical samples to further advance our understanding of children’s clinically disturbed sleep within the influence of family relationships.
Despite the study’s limitations, the findings from the present study serve as an important contribution to the literature by enhancing our understanding of youth’s sleep health within the family context. Undoubtedly, pediatric sleep problems pose a serious risk to the physical and mental health of youth. Advancing our conceptualization on how parenting behaviors and family functioning relate to youth sleep health promotes further understanding of factors that pervasively contribute to the epidemic of youth sleep problems. Such empirical evidence can inform how to durably modify sleep dysfunction and promote adaptive psychosocial outcomes in youth with sleep problems. Our findings suggest that including caregivers in interventions that aim to promote healthy sleep practices in children and adolescents is a necessity. Additionally, the impact of negative parenting on disrupted youth sleep health underscores the need to enhance caregiver wellbeing to mitigate the adverse sleep and mental health consequences associated with high levels of parenting stress and family conflict. Consideration of transactional dynamics between family and parent functioning and youth sleep health is imperative to further understand how to best promote youth sleep health across development.
Acknowledgments:
This research was supported by the Child and Adolescent Psychology Training and Research, Inc (CAPTR) and by NICHD F31HD082858. The first author is supported by F31HD101257.
Disclosure of funding received: National Institute of Child Health and Human Development (F31HD082858 and F31HD101257).
Footnotes
Disclosure Statement:
The authors have nothing to disclose. All authors declare that they have no conflicts of interest.
Portions of the data were previously presented at the 2019 Society for Research in Child Development Biennial Meeting in Baltimore, MD, and at the 2019 International Convention of Psychological Science in Paris, France.
References
- 1.Kelly RJ, El-Sheikh M. (2014). Reciprocal relations between children’s sleep and their adjustment over time. Dev Psychol. 2014; 50: 1137–1147. [DOI] [PubMed] [Google Scholar]
- 2.Dahl RE, El-Sheikh M. Considering sleep in a family context: Introduction to the special issue. J Fam Psychol. 2007; 21:1–3. [DOI] [PubMed] [Google Scholar]
- 3.Sadeh A, Raviv A, Gruber R. Sleep patterns and sleep disruptions in school-age children. Dev Psychol. 2000; 36: 291–301. [DOI] [PubMed] [Google Scholar]
- 4.Buysse DJ. Sleep health: can we define it? Does it matter? Sleep. 2014; 37:9–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.El‐Sheikh M, Kelly RJ. Family Functioning and Children’s Sleep. Child Dev Perspect. 2017; 11: 264–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McMakin DL, Alfano CA. Sleep and anxiety in late childhood and early adolescence. Curr Opin Psychiatr. 2015; 28:483–489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Roberts RE, Duong HT. (2014). The prospective association between sleep deprivation and depression among adolescents. Sleep. 2014; 37:239–244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wong MM, Brower KJ, Zucker RA. Sleep problems, suicidal ideation, and self-harm behaviors in adolescence. J Psychiatr Res. 2011; 45:505–511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shochat T, Cohen-Zion M, Tzischinsky O. Functional consequences of inadequate sleep in adolescents: a systematic review. Sleep Med Rev. 2014; 18:75–87. [DOI] [PubMed] [Google Scholar]
- 10.American Medical Association, American Academy of Sleep Medicine. Chicago, IL: American Medical Association, American Academy of Sleep Medicine; 2010. Resolution 503: Insufficient sleep in adolescents. [Google Scholar]
- 11.Meijer AM, Reitz E, Dekovic M. Parenting matters: a longitudinal study into parenting and adolescent sleep. J Sleep Res. 2016; 25:556–64. [DOI] [PubMed] [Google Scholar]
- 12.Gunn HE, O’Rourke F, Dahl RE, et al. Young adolescent sleep is associated with parental monitoring. Sleep Health. 2019; 5:58–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Meltzer LJ, Mindell JA. The relationship between child sleep disturbances and maternal sleep, mood, and parenting stress: a pilot study. J Fam Psychol. 2007; 21:67–73. [DOI] [PubMed] [Google Scholar]
- 14.Bell BG, Belsky J. Parents, parenting, and children’s sleep problems: Exploring reciprocal effects. Br J Dev Psychol. 2008; 26:579–593. [Google Scholar]
- 15.Eisenberg N, Cumberland A, Spinrad TL Parental Socialization of Emotion. Psychol Inq. 1998; 9:241–273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Eisenberg N, Spinrad TL, Eggum, ND. Emotion-related self-regulation and its relation to children’s maladjustment. Annu Rev Clin Psychol. 2010; 6:495–525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Thompson RA, Meyer S. Socialization of Emotion Regulation in the Family. In Gross JJ, ed. Handbook of Emotion Regulation. New York, NY: The Guilford Press; 2007; 249–268. [Google Scholar]
- 18.Sanders W, Zeman J, Poon J, et al. Child regulation of negative emotions and depressive symptoms: The moderating role of parental emotion socialization. J Child Fam Stud. 2015; 24:402–415. [Google Scholar]
- 19.Dahl RE. The regulation of sleep and arousal: Development and psychopathology. Dev Psychopathol. 1996; 8:123–139. [Google Scholar]
- 20.Kelly RJ, Marks BT, El-Sheikh M. Longitudinal relations between parent-child conflict and children’s adjustment: the role of children’s sleep. J Abnorm Child Psychol. 2014; 42:1175–1185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Parent J, Forehand R. The Multidimensional Assessment of Parenting Scale (MAPS): Development and psychometric properties. J Child Fam Stud. 2017; 26:2136–2151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Owens JA, Spirito A, McGuinn M. The Children’s Sleep Habits Questionnaire (CSHQ): Psychometric properties of a survey instrument for school-aged children. Sleep. 2000; 23:1043–1051. [PubMed] [Google Scholar]
- 23.Achenbach T, McConaughy S, Ivanova MY, Rescorla LA. Manual for the ASEBA Brief Problem Monitor (BPM). 2011; Burlington, VT: University of Vermont. [Google Scholar]
- 24.Fabes RA, Eisenberg N, Bernzweig J. The Coping with Children’s Negative Emotions Scales. (CCNES): Description and scoring. Tempe, AZ: Arizona State University. 1990. [Google Scholar]
- 25.Herbert SD, Harvey EA, Roberts JL, et al. A randomized controlled trial of a parent training and emotion socialization program for families of hyperactive preschool aged children. Behav Ther. 2013;44: 302–316. [DOI] [PubMed] [Google Scholar]
- 26.Roesch SC, Villodas M, Villodas F. Latent class/profile analysis in maltreatment research: A commentary on Nooner et al., Pears et al., and looking beyond. Child Abuse Negl. 2010; 34:155–160. [DOI] [PubMed] [Google Scholar]
- 27.Cloitre M, Garvert DW, Brewin CR, et al. Evidence for proposed ICD-11 PTSD and complex PTSD: a latent profile analysis. Eur Journal Psychotraumatol. 2013; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bakk Z, Tekle F, Vermunt J. Estimating the Association between Latent Class Membership and External Variables Using Bias-adjusted Three-step Approaches. Sociol Methodo. 2013; 43:272–311. [Google Scholar]
- 29.Randler C, Bilger S, & Díaz-Morales JF Associations among sleep, chronotype, parental monitoring, and pubertal development among German adolescents. J Psychol. 2009. 143: 09–520. [DOI] [PubMed] [Google Scholar]
- 30.Short MA, Gradisar M, Wright H, et al. Time for bed: parent-set bedtimes associated with improved sleep and daytime functioning in adolescents. Sleep. 2011; 34:797–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pearl AM, French BF, Dumas JE, et al. Bidirectional Effects of Parenting Quality and Child Externalizing Behavior in Predominantly Single Parent, Under-Resourced African American Families. J Child Fam Stud. 2014; 23:177–188. [Google Scholar]
- 32.Johnson AM, Hawes DJ, Eisenberg N, et al. Emotion socialization and child conduct problems: A comprehensive review and meta-analysis. Clin Psychol Rev, 2017;54: 65–80. [DOI] [PubMed] [Google Scholar]
- 33.Youngstrom E, Loeber R, Stouthamer-Loeber M. Patterns and correlates of agreement between parent, teacher, and male adolescent ratings of externalizing and internalizing problems. J Consult Clin Psychol. 2000; 68(6):1038–50. [DOI] [PubMed] [Google Scholar]
- 34.Beebe DW. Neurobehavioral morbidity associated with disordered breathing during sleep in children: a comprehensive review. Sleep. 2006; 29:1115–1134. [DOI] [PubMed] [Google Scholar]
- 35.Brand S, Gerber M, Beck J, Kalak N, Hatzinger M, Pühse U, Holsboer-Trachsler E. Perceived parenting styles differ between genders but not between elite athletes and controls. Adolesc Health Med Ther. 2011; 2:9–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Parent J, Forehand R, Dunbar JP, Watson KH, Reising MM, Seehuus M, Compas BE. Parent and adolescent reports of parenting when a parent has a history of depression: associations with observations of parenting. J Abnorm Child Psychol. 2014; 42(2):173–83. [DOI] [PMC free article] [PubMed] [Google Scholar]


