Abstract
Background
Structural racism is a complex system of inequities working in tandem to cause poor health for communities of color, especially for Black people. However, the multidimensional nature of structural racism is not captured by existing measures used by population health scholars to study health inequities. Multidimensional measures can be made using complex analytical techniques. Whether or not the multidimensional measure of structural racism provides more insight than the existing unidimensional measures is unknown.
Methods
We derived measures of Black-White residential segregation, inequities in education, employment, income, and homeownership, evaluated for 2,338 Public Use Microdata Areas (PUMAs) in the United States (US), and consolidated them into a multidimensional measure of structural racism using a latent class model. We compared the median COVID-19 vaccination rates observed across 54 New York City (NYC) PUMAs by levels (high/low) of structural racism and the multidimensional class using the Kruskal-Wallis test. This study was conducted in March 2021.
Findings
Our latent class model identified three structural racism classes in the US, all of which can be found in NYC. We observed intricate interactions between the five dimensions of structural racism of interest that cannot be simply classified as “high” (i.e., high on all dimensions of structural racism), “medium,” or “low.” Compared to Class A PUMAs with the median rate of two-dose completion of 6·9%, significantly lower rates were observed for Class B PUMAs (5·5%, p = 0·04) and Class C PUMAs (5·2%, p = 0·01). When the vaccination rates were evaluated based on each dimension of structural racism, significant differences were observed between PUMAs with high and low Black-White income inequity only (7·2% vs. 5·3%, p = 0·001).
Interpretation
Our analysis suggests that measuring structural racism as a multidimensional determinant of health provides additional insight into the mechanisms underlying population health inequity vis-à-vis using multiple unidimensional measures without capturing their joint effects.
Funding
This project is funded by the Robert J. Jones Urban Research and Outreach-Engagement Center, University of Minnesota. Additional support is provided by the Minnesota Population Center, which is funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (Grant P2C HD041023).
Keywords: Structural racism, measurement, latent class analysis, COVID-19, Health equity
Research in context.
Evidence before this study
Based on our peer-reviewed literature search conducted in 2020, we found that all existing measures of structural racism focus on a single dimension of structural racism (e.g., in education, employment, criminal justice involvement), except one study by Dougherty and colleagues (2020) that measures structural racism as a multidimensional determinant of health. Dougherty and colleagues’ approach leverages a confirmatory factor analysis to integrate several existing continuous-scale unidimensional measures of structural racism and uses a resulting factor score as an explanatory variable in regression analyses.
Added value of this study
We developed a multidimensional measure of structural racism (MMSR) by consolidating five unidimensional measures of structural racism (including Black-white residential segregation, inequities in education, employment, income, and homeownership), evaluated at the Public Use Microdata Area (PUMA), using a latent class model. We identified three PUMA classes, each representing a multidimensional structural racism profile. Using COVID-19 vaccination as a case study, we found a distinct gradient in vaccination rates by PUMA classes. When the vaccination rates were evaluated based on each unidimensional measure, differences by levels of structural racism were observed only for income inequity.
Implications of all the available evidence
Our research offers a new approach to measuring structural racism as a multidimensional determinant of health. Results from our case study suggest that evaluating population health patterns by unidimensional measures of structural racism may not capture the interaction between dimensions and their joint effects on health. Consequently, the need for a multidimensional measure of structural racism is warranted.
Alt-text: Unlabelled box
1. Introduction
The progress toward racial and health equities cannot be achieved if scholars and policymakers cannot measure the causes of the inequities, understanding their deleterious effects, and track changes over time [1]. Structural racism, defined as the macrolevel systems, social forces, institutions, ideologies, and processes that interact with one another to generate and reinforce inequities among racial and ethnic groups [2], are recognized by population health scholars as a fundamental cause of racial health inequities [3,4]. Operationalizing and measuring structural racism is an active area of research [1,5,14,[6], [7], [8], [9], [10], [11], [12], [13]]. In the past few decades, several indexes have been developed and applied to elucidate the relationship between structural racism and population health outcomes, particularly their effect among communities of color [1]. The brutal murder of George Floyd, Jr. by the knee of a Minneapolis police officer and the racial inequities in COVID-19 mortality have both shone a light on deeply rooted racial injustices and further motivate research that focuses on structural racism, not race, as a determinant of health. Yet, there is more work to be done to improve the measurement of structural racism. In fact, one of the most debated issues is the question of whether existing measures of structural racism embody what scholars aim to measure [15,16].
Structural racism, specifically anti-Black racism, is a system of oppression that corrupts the way in which Black, relative to White people, access resources and opportunities necessary for their health and well-being [17]. Evidence of the persistent inequities rooted in racist policies, practices, and cultural beliefs driven by White supremacy ideology to suppress and sustain racial hierarchy can be found in housing, education, employment, healthcare, political participation, and “public safety”, to name a few dimensions [18]. Empirically, each of these dimensions of structural racism (referred to as “unidimensional structural racism” henceforth) carries its deleterious effect on the health of Black people, with some literature stipulating potential health benefits for White people [[5], [6], [7],9,10,[12], [13], [14],19]. Because various dimensions of structural racism may share the same pathway (e.g., education inequity leads to employment inequity) or interact with one another (e.g., education inequity among residents in racially segregated neighborhoods) to generate joint effects on health, the way we measure structural racism must reflect this multidimensionality [15,16]. Currently, there is a dearth of literature on how to measure structural racism as a multidimensional determinant of health. In 2020, a pioneering study by Dougherty and colleagues proposed the use of a factor score from a confirmatory factor analysis that integrates several existing continuous-scale unidimensional measures of structural racism as an explanatory variable in regression analyses [11].
The objective of this article is to describe our effort to integrate categorical-scale unidimensional measures into one multidimensional measure of structural racism (MMSR) using a latent class model. Categorizing unidimensional structural racism into levels (e.g., high/low, quartiles) eases the interpretation of regression outputs compared with continuous measures and is the preferred strategy among scholars who study the health impacts of structural racism [5,6,9,10,12,14]. We demonstrated the utility of our latent-class-based MMSR by linking it to the COVID-19 vaccination tracker data from New York City (NYC). We assessed whether area-based vaccination patterns evaluated by unidimensional structural racism measures and the MMSR are inconsistent. If true, accounting for how various structural racism dimensions act jointly and using the MMSR to predict health inequities may be warranted.
2. Methods
2.1. Deriving a Multidimensional Measure of Structural Racism (MMSR)
The MMSR was designed to be used not only for regression analysis but also to track changes in structural racism over time. For these reasons, we aimed to include measures that 1) have been used and tested for their validity in previous research, 2) are easy to derive (e.g., do not need complicated models to calculate), and 3) can be derived and updated by researchers with publicly available data. From a list of existing unidimensional measures of racism [1], we selected five that can be derived and updated with the data from the American Community Survey (ACS), a population survey conducted annually by the US Census Bureau: the index of dissimilarity (for Black-White residential segregation), Black-White educational inequity, Black-White employment inequity, Black-White homeownership inequity, and the index of concentration at the extremes (for Black-White income inequity). The equations for these measures are available in the online supplement S1. For this pilot project, we used the 2019 ACS five-year estimates, extracted from the Integrated Public Use Microdata Series National Historical Geographic Information System (IPUMS NHGIS) database [20]. All unidimensional measures were dichotomized into high and low structural racism based on their sample median [5]. It is important to keep in mind that the five measures we selected for the current analysis do not represent all dimensions with which structural racism manifests. The inclusion of alternative measures to examine racial inequities in these five dimensions and/or measures of other dimensions of inequities can and should be tested in future research.
Previous literature measure structural racism at a state or county level, arguing that racist laws and policies that disadvantage people of color relative to their White peers (i.e., institutional racism) are designed and implemented at such levels [[5], [6], [7], [8],[11], [12], [13]]. While institutional racism is one component of structural racism, conflating the two concepts as the same rather than institutional racism as a building block of a large system of structural racism may lead to the inaccurate conclusion of the deleterious effect of structural racism on population health [21]. Riley (2018) argues that the units of measurement for structural racism must be theoretically meaningful yet capture the variation in race relations across geographic units [22]. Because states and counties (especially urban counties like New York County and Los Angeles County) span over large areas, state- and county-level structural racism may dilute the heterogeneity in racial inequities experienced by residents of the subunits of these geographic areas. To capture levels of racial inequities produced by structural racism, our study measured structural racism at the Public Use Microdata Area (PUMA) level. PUMAs are statistical areas that contain at least 100,000 residents and follow the boundaries of census tracts, single counties, or groups of counties [23]. Densely populated counties (e.g., New York County) consist of several PUMAs. In contrast, several counties with low numbers of residents are combined into one PUMA. PUMA-based measures may allow us to examine the heterogeneity of structural racism for large counties, especially those that consist of both urban and rural areas [24].
We used a latent class model to classify 2,338 PUMAs in the United States (US) with no missing data on the five unidimensional measures mentioned earlier into structural racism classes. This type of model can distinguish subpopulations (i.e., latent classes) that shared measure response patterns. The model estimated the probabilities of latent class membership for each PUMA based on its observed values of the unidimensional measures of structural racism and subsequently assigned the PUMA to the class with the highest posterior probability [25]. We specified our models with two to five latent classes (not exceeding the number of the unidimensional measures included) and selected the best-fitted model based on two fit statistics: Bayesian Information Criteria (BIC: the lower value indicates better model fit) and the standardized entropy (value from 0 to 1, with 0 indicates complete uncertainy of a latent class assignment and 1 indicates complete certainty) [25]. When these two fit statistics suggested models with a different number of latent classes, the model with fewer latent classes was selected for ease of interpretation. Details of our latent class model fitting can be found in the online supplement S2. The best-fitted model is referred to as the MMSR, with latent classes representing classes of PUMAs with different structural racism profiles. For sensitivity, we also fitted the latent class model with the tertile and quartile of the unidimensional measures of structural racism (see online supplement S3).
2.2. Linking the MMSR to the PUMA-based data from New York City
We leveraged the geocoded sociodemographic and health surveillance data from the NYC governmental agencies in this analysis. NYC is subdivided into 59 community districts, 55 of which share the exact boundaries with PUMAs delineated by the US Census Bureau. The four exceptions are Manhattan community districts 4 and 5 and Bronx community districts 1 and 2, which nest within PUMAs 3807 and 3710, respectively. Given the high level of comparability between community districts and PUMAs, we could readily merge the PUMA-based MMSR to the community-district-based data.
To understand the sociodemographic characteristics of PUMA classes, we merged the MMSR with the NYC Community District Profile. Details of the data collection protocols and rationale for specific data elements collected are published elsewhere [26]. We extracted the following variables from this dataset: community racial composition and percentages of residents aged 25 and older with college or advance degrees, residents of working-age (25–64 years), and those born outside of the US.
We also merged the MMSR with the NYC Department of Health and Mental Hygiene (NYC Health) COVID-19 vaccine tracker data.[27] This is the first public ZIP Code Tabulation Area (ZCTA)-level vaccination data in the US, but only all-race vaccination rates are available. We assigned the ZCTA-level data to the corresponding PUMAs using a ZCTA-PUMA relationship file (i.e., a crosswalk) available from the Baruch College Geoportal [28]. For our analysis, we intentionally used the earliest available data, which was released to the public on February 17, 2021. At that time, only the two-dose vaccines (Moderna and Pfizer-BioNTech) were available to a limited number of high-risk individuals and the NYC Health initiatives to ensure vaccine equity across various communities had not been in place yet. This methodology allows us to observe the effect of structural racism “in its prime” on the vaccination patterns.
2.3. Statistical analysis
We descriptively examined vaccination rates by structural racism levels for the five unidimensional measures and the MMSR classes with median and interquartile range (IQR). Median was chosen over mean because of the small number of PUMAs in NYC, and the distribution of the vaccination rates in our sample was skewed. We tested for significant differences with the Kruskal-Wallis test. PUMAs classified as having “low” structural racism were the reference group for the unidimensional measures. Because the latent class model may not identify a PUMA class where structural racism is low in all five dimensions of interest, we selected the PUMA class with the highest vaccination rates, assuming that this class experienced the least joint effect of structural racism, as a reference group for the significant test of difference in vaccination rates by the multidimensional classes.
The protocol for this study was reviewed and determined to be non-human subjects research by the University of Minnesota Internal Review Board. All analyses were conducted in R version 4.0.2. We used R package PoLCA to fit the latent class model [29]. This study adhered to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline [30].
2.4. Role of funding sources
All funders for this study have no involvement in the design, data analysis, interpretation of the study results, drafting the manuscript, or the decision to submit this paper for publication.
3. Results
3.1. PUMA Classes and Thier Characteristics
Our most parsimonious latent class model identified three PUMA classes in the US based on five unidimensional structural racism measures. However, this model has relatively low entropy (0.5), which indicates that the three classes are not highly distinguishable from one another. The entropy of the models with a higher number of PUMA classes improves slightly, but those models were less parsimonious, as indicated by higher BIC scores (see online supplement S2).
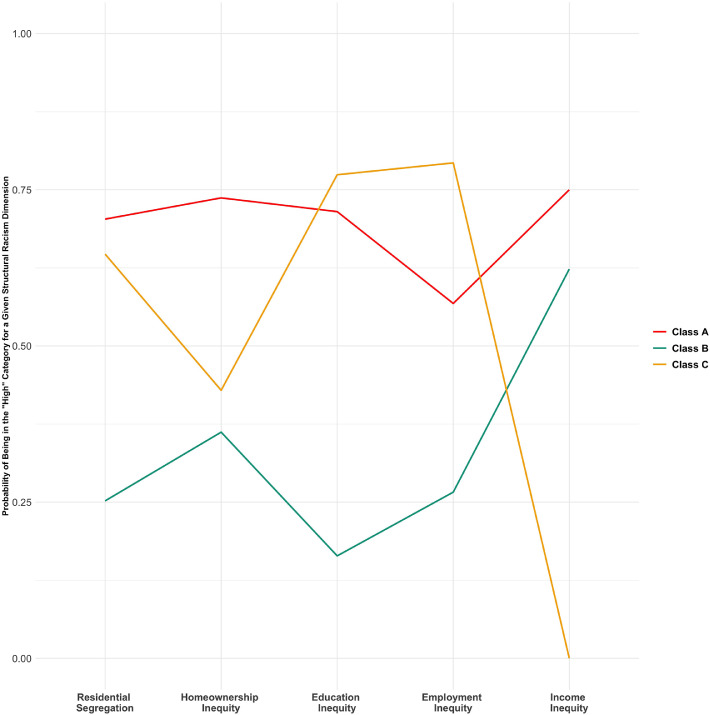
Fig. 1 shows the probability of being in the “high” category for each of the five unidimensional measures of structural racism for the three PUMA classes, conditioned on assigned class membership. Class A PUMAs are racially segregated, with high racial inequities in education, employment, homeownership, and income. Class B PUMAs are racially diverse, with low education, employment, and homeownership inequities and moderate income inequity between Black and White residents. Class C PUMAs are moderately segregated, with lower homeownership and income inequities and higher education and employment inequities than Class A. Out of the 2,338 PUMAs included in our analysis, 27·1% were assigned to Class A, 43·9% were assigned to Class B, and 29% were assigned to Class C (Table 1).
Fig. 1.
Multidimensional Structural Racism Profile by Latent Classes This figure shows the unique profiles of structural racism along five dimensions (residential segregation, homeownership, education, employment, and income inequities) for the three latent classes. The x-axis shows the dimensions and the y-axis shows the probability that a given class exhibits a level of Black-White inequity greater than the national median for the dimension in question.
Table 1.
Percentages of 2,338 PUMAs in the United States Within Each Latent Class With High Level of Structural Racism (Greater Than the National Median) for Each Dimension†.
| Dimension | Class A | Class B | Class C |
|---|---|---|---|
| Black-White Residential Segregation | 70·3 | 25·2 | 64·7 |
| Black-White Homeownership Inequity | 73·7 | 36·2 | 42·9 |
| Black-White Education Inequity | 71·5 | 16·4 | 77·4 |
| Black-White Employment Inequity | 56·8 | 26·6 | 79·3 |
| Black-White Income Inequity | 75·0 | 62·3 | 0·0 |
| Percentage of PUMA Class in the United States | 27·1 | 43·9 | 29·0 |
Latent class assignment is based on the Black-White structural racism measures calculated from the 2019 American Community Survey five-year estimates.
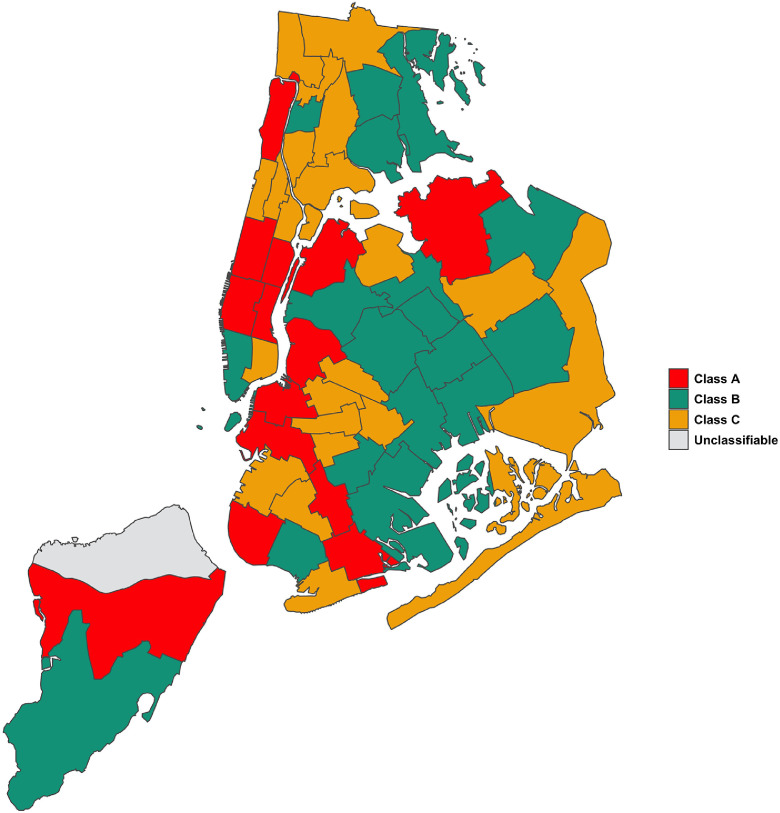
Fig. 2 displays the three PUMA classes in NYC. One Staten Island PUMA had a missing unidimensional structural measure, hence did not have the PUMA class assignment. Based on the Community District Profile data, residents of Class A PUMAs are mostly White (61%), working-age (60%), and have college or advanced degrees (50%) (Table 2). Class B PUMAs are racially integrated (15% Black, 25% White, 29% Latino, 11% Asian) and comprise a large percentage of foreign-born (42%). Compared to Class A, a smaller percentage of residents of Class B PUMAs are college-educated (p = 0·001) and of working age (p = 0·02). Residents in Class C PUMAs are mostly Black (27%) and Latino (25%).
Fig. 2.
Geographic Distribution of Multidimensional Structural Racism Classes in New York City.
Table 2.
Sociodemographic Characteristics of PUMA Classes in New York City.
| Class A (n = 14) | Class B (n = 18) | p-Value† | Class C (n = 22) | p-Value† | ||||
|---|---|---|---|---|---|---|---|---|
| Percent of Non-Hispanic Black residents, median (IQR) | 5·2 | (6·3) | 14·5 | (27·1) | 0·48 | 27·0 | (48·3) | 0·001 |
| Percent of Non-Hispanic White residents, median (IQR) | 61·2 | (23·8) | 25·0 | (42·3) | 0·005 | 12·0 | (21·5) | <0·001 |
| Percent of Hispanic/Latino residents, median (IQR) | 15·0 | (2·8) | 29·0 | (30·3) | 0·26 | 25·0 | (41·6) | 0·01 |
| Percent of Non-Hispanic Asian residents, median (IQR) | 12·0 | (7·0) | 10·5 | (23·8) | 1·00 | 5·5 | (14·8) | 0·055 |
| Percent of residents of other races, median (IQR) | 2·0 | (0·0) | 2·0 | (1·0) | 0·25 | 2·0 | (1·0) | 0·33 |
| Percent of residents of working age (25–64 years), median (IQR) | 60·0 | (5·8) | 56·0 | (3·0) | 0·02 | 55·0 | (3·8) | 0·001 |
| Percent of residents ages 25 and older with college or advance degree, median (IQR) | 50·0 | (33·3) | 33·5 | (12·5) | 0·001 | 35·0 | (16·0) | <0·001 |
| Percent of people born outside the US, median (IQR) | 27·5 | (19·3) | 42·0 | (15·5) | 0·09 | 34·0 | (12·0) | 0·236 |
P-values for significant differences by multidimensional of structural racism classes are based on the Kruskal-Wallis test with class A as a reference group.
3.2. COVID-19 Vaccination rates
Table 3 compares the median rates of COVID-19 vaccination across NYC PUMAs by levels and classes of structural racism. When PUMAs are grouped by their levels of Black-White residential segregation, education inequity, and employment inequity, no significant difference in vaccination rates was observed between those in the high and the low structural racism groups (p > 0.05 for all comparisons). PUMAs with high homeownership inequity had a higher rate of complete-dose (i.e., two doses of the two-dose series) vaccination (6·3%) than those with low homeownership inequity (5·1%, p = 0·04). PUMAs with high income inequity had higher rates of both partial and complete-dose vaccination than PUMAs in the low income inequity group (partial: 5·6% vs. 3·9%, p < 0·001; complete: 7·2% vs. 5·3%, p = 0·001). We observed a gradient in partial and complete-dose vaccination rates when PUMAs were examined based on the MMSR. That is, the highest rates were observed among Class A (5·6% partial; 6·9% complete; reference group), followed by Class B (4·0% partial, p = 0·009; 5·5% complete, p = 0·04), and were lowest among Class C PUMAs (3·8% partial, p = 0·002; 5.2% complete, p = 0·01).
Table 3.
Comparison of Median COVID-19 Vaccination Rates by Five Unidimensional Measures of Structural Racism and Multidimensional Structural Racism Classes
| Dimension | First Dose Only | P-Value | Two Doses | P-Value |
|---|---|---|---|---|
| Black-White Residential Segregation, median (IQR)† | ||||
| Low (n=16; reference group) | 3·8 (2·3) | 5·5 (1·8) | ||
| High (n=38) | 4·2 (2·3) | 0·350 | 5·8 (2·7) | 0·380 |
| Black-White Homeownership Inequity median (IQR)† | ||||
| Low (n=24; reference group) | 3·9 (2·1) | 5·1 (1·8) | ||
| High (n=30) | 4·7 (2·4) | 0·130 | 6·3 (2·2) | 0·040 |
| Black-White Education Inequity, median (IQR)† | ||||
| Low (n=22; reference group) | 4·0 (2·2) | 5·7 (2·7) | ||
| High (n=32) | 4·1 (2·6) | 0·870 | 5·7 (2·0) | 0·900 |
| Black-White Employment Inequity, median (IQR)† | ||||
| Low (n=24; reference group) | 4·1 (2·0) | 4·0 (2·6) | ||
| High (n=30) | 4·1 (2·0) | 0·850 | 5·8 (2·2) | 0·970 |
| Black-White Income Inequity, median (IQR)† | ||||
| Low (n=38; reference group) | 3·9 (1·8) | 5·3 (1·7) | ||
| High (n=16) | 5·6 (1·5) | <0·001 | 7·2 (2·7) | 0·001 |
| Multidimensional Structural Racism Class, median (IQR)‡ | ||||
| Class A (n=14; reference group) | 5·6 (1·7) | 6·9 (1·8) | ||
| Class B (n=18) | 4·0 (2·3) | 0·009 | 5·5 (2·0) | 0·040 |
| Class C (n=22) | 3·8 (1·9) | 0·002 | 5·2 (1·7) | 0·010 |
P-values for significant differences by unidimensional measures of structural racism are based on the Kruskal-Wallis test with “low” as a reference group.
P-values for significant differences by multidimensional measures of structural racism are based on the Kruskal-Wallis test with Class A as a reference group.
4. Discussion
The recent growth of literature that examines structural racism as a fundamental cause of health inequities signals a scholastic shift from passive documentation of racial inequities to active elucidation of what lies beneath the surface. To understand the complex linkages between structural racism and population health outcomes, scholars must develop theoretically rigorous measures of structural racism. Weak and/or inaccurate measurements of structural racism may lead to inappropriate conclusions of its health effects. In this article, we describe our effort to measure structural racism as a multidimensional determinant of health – consistent with its definition. We examined whether the MMSR – a latent-class-based multidimensional measure that requires a complex analytical technique to derive – provides better insight into population health trends than the easier-to-derive unidimensional measures.
Based on five unidimensional structural racism measures, our MMSR reveals three PUMA classes across the US. These classes, however, cannot be simply classified into “high” (i.e., high structural racism in all dimensions we examined), “medium,” or “low” structural racism profiles. While Class A PUMAs are highest (i.e., have the greatest likelihood of being in the high category) on Black-White residential segregation and inequities in income and homeownership, Class C PUMAs are highest on education and employment inequities among the three PUMA classes. Similarly, Class B PUMAs are lowest on Black-White residential segregation and inequities in education, employment, and homeownership inequities. Yet, its level of income inequity is higher than in Class C PUMAs. Such intricate interactions among the various dimensions of structural racism we chose for the MMSR may have been missed had we used the traditional approach of including each unidimensional structural racism measure as a fixed effect term in regression analyses. Because these unidimensional measures of structural racism are likely correlated, putting them together into a regression equation and including interaction terms (e.g., two, three, four, five-way terms) not only violate the model assumption [31] but also produce results that are difficult to interpret.
Linking the MMSR to the PUMA-level surveillance data from NYC provides some insight on the usefulness of the MMSR in population health studies. We found that the COVID-19 vaccination rates were highest among Class A, followed by Class B and Class C PUMAs. On the other hand, no significant differences were observed when COVID-19 vaccination rates were evaluated by the unidimensional measures of structural racism, except for income inequity (measured by the index of concentration at the extremes). Although these findings do not prove that the MMSR is associated with COVID-19 vaccination rates and that the unidimensional measures are not significant correlates, our findings of the significant difference by PUMA classes may incentivize a large majority of population health scholars to move forward to fit multivariate regression models. Given a common practice of identifying racial inequities first and then subsequently dissecting the root causes of those inequities, the use of unidimensional measures of structural racism may potentially lead scholars to inaccurate conclusions related to the relationship between structural racism and population health outcomes.
Several articles published during the COVID-19 pandemic report correlation between the proportion of Black residents in an areal unit (e.g., county) and the increased rates of infection, hospitalization, and mortality, and the lower rates of screening and vaccinations for COVID-19 [10,[32], [33], [34]]. While these findings have called policy attention to racial health inequities, relying solely on the presence of Black people as a proxy for structural racism may implicitly perpetuate the misconception that poor health outcomes among Black people are biological rather than socially constructed [35]. While the vaccination gradient by the PUMA classes in our study is likely correlated with the proportion of Black residents in the PUMA, the MMSR offers insight into potential root causes of population health inequities. Rather than attributing inequities to the presence of Black people in spaces, of which the only solution for improving population health is relocating Black people to non-Black neighborhoods, the use of MMSR in structural racism and health research can potentially point policymakers to specific inequities that need to be addressed with policy interventions and highlight the importance of addressing the whole system of structural racism rather than paying attention to specific dimensions of racial inequities to promote optimal population health equity.
Results reported in this article have several limitations that will be addressed in future efforts. First, the standardized entropy for our latent class model is relatively low (0.5); thus, the three PUMA classes identified by our latent class model are not clearly distinguishable from one another. Our future efforts will test whether adding more unidimensional measures of structural racism into the latent class model yields better class separation. Second, the vaccination data we used in this analysis were not race-specific. Given the inconsistencies of literature on the health benefits/harms from structural racism for White people, we were not able to characterize with confidence that the high vaccination rate observed in Class A PUMAs is attributable solely to the fraction of the PUMAs identifying as White and whether Black people living in that PUMA class have similar experience accessing the COVID-19 vaccine. Furthermore, we did not fit multivariate models to control for potential confounders in our analysis. Hence, we cannot explicitly conclude that the multidimensional structural racism class is associated with the COVID-19 vaccination patterns. This is because of the small number of PUMAs in NYC and the lack of individual-level data with PUMA geocoding. Given the increasing call for more race-specific health data, future studies should leverage new race-specific data with larger sample size and examine health outcomes by PUMA classes for Black and White people separately. For studies that will link the MMSR to other correlates, the Vermunt's “three-step” approach that accounts for class assignment error is recommended [36]. Lastly, because vaccination data used in our analysis was from a large US metropolitan area, our findings may not be generalizable to the population living in non-metropolitan areas or those living outside the US. Therefore, researchers with access to data from these areas are encouraged to replicate our study to examine our findings' validity in their locale of interest.
The complex and intersecting nature of structural racism requires innovative methodologies to elucidate its impact on population health. Our analysis sought to examine whether a multidimensional measure of structural racism provides an improved understanding of how structural racism is operating in communities in comparison to existing unidimensional measures of structural racism. Our findings suggest that measuring structural racism as a multidimensional determinant of health has the potential to offer critical insights into the underlying mechanisms of inequities in population health.
Contributors
TC designed and conducted all the analyses and drafted the original manuscript. He also had access and was responsible for the raw data associated with the study. DCV provided geospatial methodological expertise, reviewed and critically revised the final manuscript. RRH acquired the study funding, supervised the design of all the analyses, and reviewed and critically revised the final manuscript. All authors approved the final version of the manuscript for submission.
Declaration of Competing Interest
DCV reports a grant from the National Institutes of Health. All other authors report no declarations
Acknowledgments
Data Sharing Statement
Analyses described in this manuscript utilized publicly available datasets. American Community Survey data are available at https://www.nhgis.org. A ZCTA-PUMA crosswalk is available at https://www.baruch.cuny.edu/confluence/display/geoportal/NYC±Geographies. New York City Community District Profile data are available at https://communityprofiles.planning.nyc.gov. New York City COVID-19 vaccine data are available at https://www1.nyc.gov/site/doh/covid/covid-19-data-vaccines.page. TC had access and was responsible for the raw data associated with the study.
Funding
This project was funded by the Robert J. Jones Urban Research and Outreach-Engagement Center, University of Minnesota. Additional support was provided by the Minnesota Population Center, which is funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (Grant P2C HD041023). All funders have no involvement in the design, data analysis, interpretation of the study results, drafting the manuscript, or the decision to submit this paper for publication.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.eclinm.2021.101092.
Appendix. Supplementary materials
References
- 1.Groos M., Wallace M.E., Hardeman R.R., Theall K. Measuring inequity: a systematic review of methods used to quantify structural racism. J Health Dispar Res Pract. 2018;11(2):190–206. http://digitalscholarship.unlv.edu/jhdrp/http://digitalscholarship.unlv.edu/jhdrp Accessed August 18, 2019. [Google Scholar]
- 2.Powell J.A. Structural racism: building upon the insights of John Calmore. North Carol Law Rev. 2008;86(3):791–816. http://www.gnocdc.org/orleans/8/22/people.htm [Google Scholar]
- 3.Center for Disease Control and Prevention. Racism and Health. https://www.cdc.gov/healthequity/racism-disparities/index.html. Accessed April 9, 2019.
- 4.Phelan J.C., Link B.G. Is racism a fundamental cause of inequalities in health? Annu Rev Sociol. 2015;41:311–330. doi: 10.1146/annurev-soc-073014-112305. [DOI] [Google Scholar]
- 5.Lukachko A., Hatzenbuehler M.L., Keyes K.M. Structural racism and myocardial infarction in the United States. Soc Sci Med. 2014;103:42–50. doi: 10.1016/j.socscimed.2013.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wallace M., Crear-Perry J., Richardson L., Tarver M., Theall K. Separate and unequal: structural racism and infant mortality in the US. Heal Place. 2017;45(November 2016):140–144. doi: 10.1016/j.healthplace.2017.03.012. [DOI] [PubMed] [Google Scholar]
- 7.Wallace M.E., Mendola P., Liu D., Grantz K.L. Joint effects of structural racism and income inequality on small-for-Gestational-Age Birth. Am J Public Health. 2015;105(8):1681–1688. doi: 10.2105/AJPH.2015.302613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liu S.Y., Fiorentini C., Bailey Z., Huynh M., McVeigh K., Kaplan D. Structural racism and severe maternal morbidity in New York State. Clin Med Insights Women's Heal. 2019;12 doi: 10.1177/1179562x19854778. 1179562X1985477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bailey Z.D., Feldman J.M., Bassett M.T. How structural racism works — racist policies as a root cause of U . S . Racial Health Inequities. N Engl J Med. 2020:1–6. doi: 10.1056/NEJMms2025396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bin Tan S, P DeSouza, Raifman M. Structural racism and COVID-19 in the USA: a county-level empirical analysis. J Racial Ethn Heal Disparities. 2021 doi: 10.1007/s40615-020-00948-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dougherty G.B., Golden S.H., Gross A.L., Colantuoni E., Dean L.T. Measuring structural racism and its association with BMI. Am J Prev Med. 2020;000(000):1–8. doi: 10.1016/j.amepre.2020.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chambers B.D., Baer R.J., McLemore M.R., LL Jelliffe-Pawlowski. Using index of concentration at the extremes as indicators of structural racism to evaluate the Association with Preterm Birth and Infant Mortality—California, 2011–2012. J Urban Heal. 2018:1–12. doi: 10.1007/s11524-018-0272-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chambers B.D., Erausquin J.T., Tanner A.E., Nichols T.R., Brown-Jeffy S. Testing the association between traditional and novel indicators of county-level structural racism and birth outcomes among black and white women. J Racial Ethn Heal Disparities. 2018;5(5):966–977. doi: 10.1007/s40615-017-0444-z. [DOI] [PubMed] [Google Scholar]
- 14.Hardeman R.R., Chantarat T., Karbeah J. Police exposure as a determinant of structural racism: an exploration of the association between preterm birth in neighborhoods with high police exposure. Health Serv Res. 2020;55(S1) doi: 10.1111/1475-6773.13396. 50-50. [DOI] [Google Scholar]
- 15.Chantarat T. Structural racism as a system of racial inequities. New Approaches and Tools. 2019 https://iaphs.org/structural-racism-as-a-system-of-racial-inequities-new-approaches-and-tools/?fbclid=IwAR2cBYPm09gMGjJozbk80NRV0Kx3sKdr6mm031cLD-tCGftPCQKXYXcN384 Published 2020. Accessed March 31. [Google Scholar]
- 16.Riley A.R. Advancing the study of health inequality : fundamental causes as systems of exposure. SSM - Popul Heal. 2020;10 doi: 10.1016/j.ssmph.2020.100555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jones C.P. Levels of racism: a theoretic framework and a Gardener's Tale. Am J Public Health. 2000;90:1212–1215. doi: 10.1111/j.1467-8365.1979.tb00051.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Williams D.R., Lawrence J.A., Davis B.A. Racism and health: evidence and needed research. Annu Rev Public Heal. 2019;40:105–125. doi: 10.1146/annurev-publhealth. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liu S.Y., Fiorentini C., Bailey Z., Huynh M., McVeigh K., Kaplan D. Structural racism and severe maternal morbidity in New York State. Clin Med Insights Women's Heal. 2019;12(June) doi: 10.1177/1179562x19854778. 1179562X1985477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Manson S., Schroeder J., Van Riper D., Kugler T., Ruggles S. IPUMS National Historical Geographic Information System. Version. 2020 15.0 [Database] [Google Scholar]
- 21.Gee G.C., Hicken M.T. Structural racism: the rules and relations of inequity. Ethn Dis. 2021;31(Suppl):293–300. doi: 10.18865/ed.31.s1.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Riley A.R. Neighborhood disadvantage, residential segregation, and beyond-lessons for studying structural racism and health. J Racial Ethn Heal Disparities. 2018;5:357–365. doi: 10.1007/s40615-017-0378-5. [DOI] [PubMed] [Google Scholar]
- 23.US Census Bureau. Public Use Microdata Areas (PUMAs). https://www.census.gov/programs-surveys/geography/guidance/geo-areas/pumas.html. Accessed January 27, 2019.
- 24.Henning-Smith C.E., Hernandez A.M., Hardeman R.R., Ramirez M.R., Kozhimannil K.B. Rural counties with majority black or indigenous populations suffer the highest rates of premature death in The US. Health Aff. 2019;38(12):2019–2026. doi: 10.1377/hlthaff.2019.00847. [DOI] [PubMed] [Google Scholar]
- 25.Collins L.M., Lanza S.T.Latent class and latent transition analysis.; 2009. doi: 10.1002/0471264385.wei0226. [DOI]
- 26.New York City Deparmtne of Planning. New York City Community Profiles. https://communityprofiles.planning.nyc.gov/about. Accessed April 8, 2019.
- 27.New York City Department of Health and Mental Hygiene COVID-19: Data on Vaccines. 2019 https://www1.nyc.gov/site/doh/covid/covid-19-data-vaccines.page Accessed April 6. [Google Scholar]
- 28.NYC Geographies - Baruch Geoportal - Baruch College Confluence Service. https://www.baruch.cuny.edu/confluence/display/geoportal/NYC+Geographies. Accessed April 16, 2019.
- 29.Linzer D.A., Lewis J.B. poLCA: an R package for polytomous variable latent class analysis. J Stat Softw. 2011;42(10):1–18. doi: 10.4018/978-1-4666-2931-8.ch001. [DOI] [Google Scholar]
- 30.Von Elm E., Altman D.G., Egger M., Pocock S.J., Gøtzsche P.C., Vandenbroucke J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for Reporting Observational Studies. Lancet. 2007;370:1453–1457. doi: 10.1016/S0140-6736(07)61602-X. www.plosmedicine.org Accessed July 16, 2021. [DOI] [PubMed] [Google Scholar]
- 31.Barker L., Brown C. Logistic regression when binary predictor variables are highly correlated. Stat Med. 2001;20(9–10):1431–1442. doi: 10.1002/sim.680. [DOI] [PubMed] [Google Scholar]
- 32.Figueroa J.F., Wadhera R.K., Lee D., Yeh R.W., Sommers B.D. Community-level factors associated with racial and ethnic disparities in COVID-19 Rates in Massachusetts. Health Aff. 2020;39(11):1984–1992. doi: 10.1377/hlthaff.2020.01040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bloch M., Buchanan L., Holder J. The New York Times; 2019. See who has been Vaccinated so far in New York City.https://www.nytimes.com/interactive/2021/03/26/nyregion/nyc-vaccination-rates-map.html Published 2021Accessed April 12. [Google Scholar]
- 34.Kaufman H.W., Niles J.K., Nash D.B. Disparities in SARS-CoV-2 positivity rates. Assoc Race and Ethnicity. 2021 doi: 10.1089/pop.2020.0163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Smedley A., Smedley B.D. Race as Biology is fiction, racism as a social problem is real : anthropological and historical perspectives on the social construction of race. Am Psychol. 2005;60(1):16–26. doi: 10.1037/0003-066X.60.1.16. [DOI] [PubMed] [Google Scholar]
- 36.Vermunt J.K. Latent class modeling with covariates: two improved three-step approaches. Polit Anal. 2010;18(4):450–469. doi: 10.1093/pan/mpq025. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.