Abstract
Infection by severe respiratory syndrome coronavirus 2 (coronavirus disease 2019) has been the most important public health event of the last 100 years. The number of cases and deaths caused by this disease, its potential to rapidly spread and the search for a vaccine have been the center of discussion all over the world for over 1 year. In addition to the number of cases and all social, economic, and public health consequences of the pandemic, the variety of symptoms and clinical signs presented by infected patients has been subject of several studies and case reports. At the time of this writing, even with promising research, the clinical outcome of some patients is still unpredictable. The purpose of this article is to report an unusual case, the diagnostic process, and early treatment of this severe and atypical clinical picture. The patient is a young man diagnosed with coronavirus disease 2019 who sought our hospital in Southern Brazil reporting a history of pansinusitis progressing to a severe orbital cellulitis, requiring immediate surgical intervention.
Keywords: COVID-19, maxillofacial infection, orbital cellulitis, sinusitis
Coronavirus disease 2019 (COVID-19) is caused by severe respiratory syndrome coronavirus 2 (SARS-CoV-2), a new group of betacoronavirus.1 It predominantly affects the respiratory system and has caused unprecedented social impact throughout the world.1,2 Brazil, in May 2021, accounts for the third largest number of confirmed cases in and the second largest death toll in the world.
Reports have shown that person-to-person transmission is an important route of transmission, mainly by direct contact or through droplets suspended in the air by coughing or sneezing.1–3 The incubation period was determined as ranging from 1 to 14 days with an average of 5 to 6 days.2 Research has shown that virus particles may remain infectious on surfaces for about 5 to 9 days. Contamination may occur from touching surfaces and then bringing the virus to the eyes, mouth, or nose.4 Recent studies, however, have reported that contamination from surfaces is less frequent than initially thought, and that person-to-person transmission is the most important means of virus transmission. Social distancing, mask wearing, and hand antisepsis have been recommended, since contaminated individuals may present asymptomatic.
Vaccination has started in several countries, including Brazil, but at a slow pace, and its effect on the spread of COVID-19 may only be observed in a few months. As of May 2021, less than 4% of the world's population has been fully vaccinated.
Studies have shown that the most common symptoms at the onset of COVID-19 are fever, coughing, and fatigue. Other symptoms such as headache, dyspnea, disturbance of smell and/or taste are also frequent. Sputum, hemoptysis, diarrhea, lymphopenia, ground-glass opacity in chest x-rays, RNAemia, and acute respiratory distress syndrome have been described.1,3 The mortality is higher in patients over 70 years old and patients with associated comorbidities, both of which present a more weakened immune system to contain the progression of viral infection.1,2
The exponential number of infected people allowed for a significant variability in the symptomatology and clinical signs, especially in more severe cases. Aside from the aforementioned symptoms, literature reports some uncommon ophthalmological repercussions in patients infected with COVID-19, such as conjunctival congestion and secretion, blurred vision, dry eye, foreign body sensation, and pain.5 In addition, there are also reports of atypical conditions such as sinusitis, intracranial alterations, and orbital cellulitis, demanding early intervention.4
Facing the new conditions imposed by the COVID-19 pandemic, technology has evolved and influenced the response to new demands. Telemedicine is one of them.5 The use of this tool by health services increased quickly, because it permits interactive communication between patient and healthcare provider without person to person contact. It is especially useful for risk group patients and professionals.5 Other important use of technologies during the pandemic is three-dimensional printing of devices and equipment. Italian engineer Cristian Fracassi used a computer-aided design & computer-aided manufacturing system to develop and print mechanical respirator connections using three-dimensional printers. This new equipment helped Italian hospitals when respirators were scarce during the worst phase of the pandemic in that country in 2020.6
Although research has advanced regarding the treatment of COVID-19, there are still unanswered questions regarding clinical repercussions. The purpose of this work is to report the case of a healthy, young patient who developed a pansinusitis and severe orbital abscess while diagnosed with COVID-19.
CLINICAL REPORT
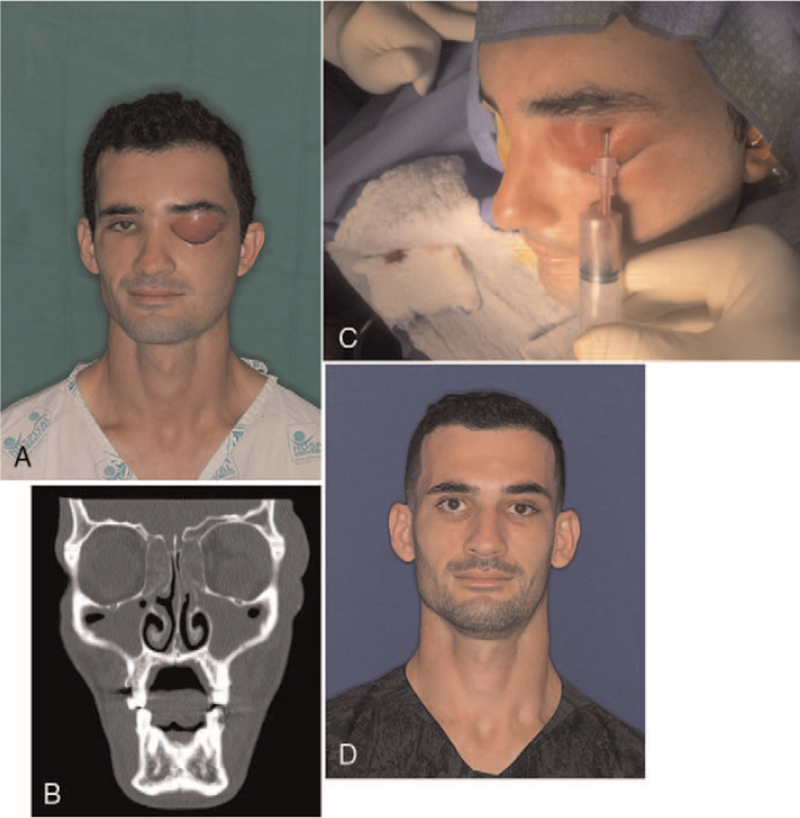
A 28-year-old male patient was admitted to the University Hospital in Londrina-PR/Brazil on October 18th, 2020, presenting a painful, progressive orbital swelling on the left side and a diagnosis of COVID-19 (Fig. 1A). Upon admission, the Emergency Medicine team started medication and a consult by the Oral and Maxillofacial Surgery team was requested.
FIGURE 1.
(A) Preoperative photo showing increased periorbital volume. (B) Computed tomography with bilateral sinus veiling of the maxillary, frontal and ethmoidal sinuses. (C) Aspiration of purulent secretion that was sent for analysis. (D) Thirty-day follow-up with significant clinical improvement.
Initially, a thorough anamnesis was performed, confirming the patient to be otherwise healthy, denying comorbidities, addictions, use of medications, or allergies. The patient told us that 13 days before he had felt unwell, with progressing fatigue followed by an absence of smell and taste. In the next 2 days, he developed a frontal headache associated with those other symptoms, and also the beginning of a left periorbital swelling and ipsilateral epiphora. Up to that moment, the patient had not sought medical attention and self-medicated with painkillers, assuming it was a case of ordinary sinusitis. However, after another day, the swelling around the eye progressed and his headache worsened. At that point, he sought an Emergency Department in his hometown and after carrying out some laboratory tests, the diagnosis of COVID-19 and concomitant sinusitis was confirmed, which caused the attending doctor to start a drug protocol for sinusitis (Levofloxacin, Dipyrone, and Prednisone). However, 4 days later, the patient noticed that although the symptoms commonly related to COVID were mild and gradually improving, the orbital infection worsened. He then returned to the first hospital and was transferred to our facility.
Upon evaluation, the patient was eupneic, responsive, oriented, afebrile, referring pain on palpation in the left periorbital region. We then noticed an increase in volume in the left frontal region as well as the periorbit, with significant firm edema on palpation, hyperemia, and associated local heat, but without evidence of drainage of purulent secretion or fistulae (Fig. 1B). Due to the significant swelling, his eyelid opening was compromised, making the complete eye exam impossible, however, after manual opening, we noticed secretion between the eyelids, a slight hypoglobe and proptosis of the left globe, movement restriction, but the visual acuity remained intact while the pupils are also reactive to light. Contralateral orbit was unaffected as well as any other areas of the head and neck, including the intraoral region; his oral health was good and no odontogenic infectious foci were observed. Then, the patient underwent a computed tomography (CT) examination of the skull, sinuses and jaw region, as well as the chest region, in view of his previous diagnosis of COVID (in turn, without signs of pulmonary involvement). This imaging examination revealed bilateral sinus veiling of the maxillary, frontal, and ethmoidal sinuses (Fig. 1C). In addition, purulent collection could be seen in the upper-superior compartment of the left globe, causing it to move inferiorly against the orbital floor.
After clinical examination and evaluation of the CT, the diagnosis of orbital cellulitis secondary to a pansinusitis related to COVID-19 was reached and we then decided to approach it early, in view of the urgency. The patient underwent surgery, under general anesthesia, for drainage of the left periorbit. Initially, an aspiration puncture (Fig. 2) was performed in the area of greatest edema, which revealed a significant presence of purulent secretion. This material was collected in a swab and sent for clinical analysis requesting microbiological culture of that material and COVID-19 detection. Then, a left supraorbital approach with a small incision and exploration of the orbital muscular planes was performed and after abundant irrigation with saline from that surgical access, a N°. 1 Pen Rose drain was installed and, finally, a dressing was made in the region. Immediately after the intervention, there was already a noticeable decrease in the periorbital volume.
FIGURE 2.
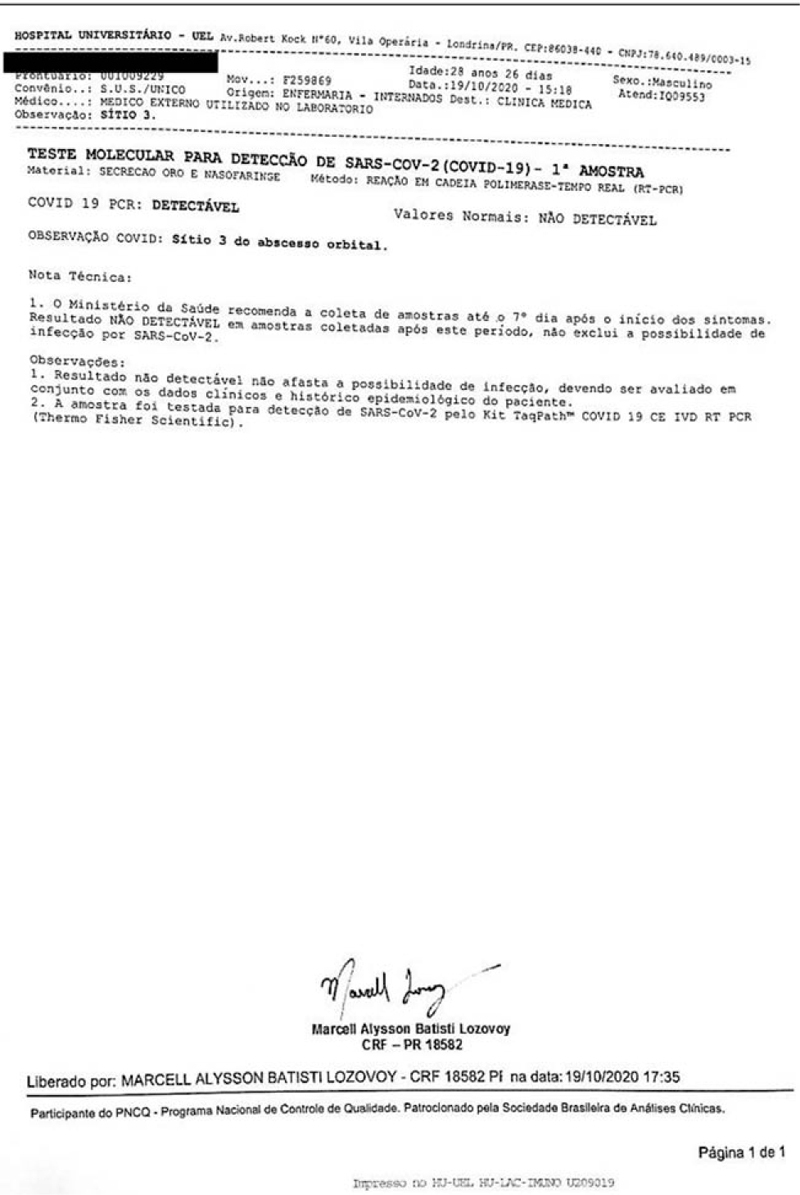
Culture result of swab test evidencing coronavirus detection in the collected secretion.
The patient remained under our care with intravenous antibiotic therapy (ceftriaxone 1 g q12 and clindamycin 600 q6), analgesics (sodium dipyrone 1 g q4 and morphine 4 mg q6), and general postoperative recommendations. After 7 days at our hospital, the patient was discharged to home with scheduled outpatient follow-ups. At that point, the analysis of the collected secretion was completed, coming out positive for COVID-19. He recovered uneventfully and in the 30-day postoperative follow-up, there was almost complete remission of orbital swelling, absence of pain, and reestablished eye function (Fig. 1D).
DISCUSSION
Acute COVID-19 infections are very similar to seasonal flu with the most common symptoms of fever, headache, shortness of breath, cough, muscle pain, and fatigue.7,8 However, it can also be associated with liver, cardiovascular, thromboembolic changes, and effects on the patient's immune response.9–11 In addition, although the literature is scarce, some ocular repercussions can be found in these patients, such as tearing and increased eyelid secretions.12 However, sinus disorders are not yet described as a typical symptom of a patient diagnosed with COVID-19.
The main imaging findings of COVID-19 on chest radiography consist of ground-glass opacities, associated or not with consolidation or septal thickening, predominantly peripheral, multilobar and bilateral, or even showing an inverted halo sign.13 When these imaging patterns are not present, chest CT scans can still be categorized as indeterminate, atypical, or negative for pneumonia. It is important to notice that some patients do not show radiological changes in the earlier stages of the disease, as in the case described here, where the patient did not show any changes in his chest CT.14
In the literature, it is evident that paranasal sinusitis is predominantly responsible for the spread of infection towards the orbit,15–17 but only 1% to 2% of all paranasal sinusitis lead to orbital involvement.18 Mills and Kartush19 in 1985 reported that the ethmoidal labyrinth was the region that most often served as a source of orbital inflammation because most abscesses appeared medially within the orbit. Unlike what was found in our report, where the infectious process was located in a supero-lateral position in the orbit, it is suggested that the path of propagation of such infection originated from the frontal sinus, which, in turn, met with a significant veiling, even though other sinuses (maxillary and ethmoidal) also had these characteristics.
According to Turbin et al4 in 2020, COVID 19 cases in their study had characteristics typically associated with acute or invasive sinus disease, both of which are strictly unilateral, which is contrary to our case, where all paranasal sinuses were affected and veiled on CT giving a more chronic aspect to the case.
Another study reported that chronic rhinosinusitis and atopy were more common in patients with prolonged viral spread (67%) compared to controls (11% and 25%, respectively). Multivariate analysis indicated that chronic rhinosinusitis was independently associated with prolonged SARS-CoV-2 RNA release in samples. If confirmed in prospective studies, this finding may have clinical implications for the duration of the quarantine due to the increased risk of contamination.20
Orbital cellulitis is an infection of the eyelid and periorbital soft tissues; usually, it does not involve the globe and generally the symptoms are eyelid erythema and edema, absence of visual impairment, pain to the eye movements, and proptosis.21 Byrne et al22 (2016) stated that if there is significant proptosis and suspected orbital compartment syndrome, a canthotomy and cantholysis can be performed to reduce intraorbital pressure and to minimize the risk of vision loss. It is then characterized as a medical emergency, because it can lead to blindness or other life-threatening complications if not treated promptly.21–23 Therefore, the clinical presentation of our patient demanded an early surgical intervention.
It is not clear whether SARS-CoV-2 itself is a contributing factor to the pathogenesis in these cases. However, the time of onset and the absence of previous symptoms of chronic sinus disease raises the possibility that congestion of the upper secondary airway by COVID-19 contributed to impaired mucociliary clearance, sinus obstruction, and secondary orbital bacterial infection. Health professionals involved in the care of COVID 19 cases should be aware of this unusual presentation.
Footnotes
The authors report no conflicts of interest.
REFERENCES
- 1.Rhotan AH, Byrareddy SN. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J Autoimmun 2020; 109:102433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ines S. A hundred days into the coronavirus disease (COVID-19) pandemic. Euro Surveill 2020; 25:2000550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Maffia F, Fontanari M, Vellone V, et al. Impact of COVID-19 on maxillofacial surgery practice: a worldwide survey. Int J Oral Maxillofac Surg 2020; 49:827–835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Turbin RE, Wawrzusin PJ, Sakla NM, et al. Orbital cellulitis, sinusitis and intracranial abnormalities in two adolescents with COVID- 19. Int J Orbital Disord Oculoplastic Lacrimal Surg 2020; 39:305–310. [DOI] [PubMed] [Google Scholar]
- 5.Chen L, Deng C, Chen X, et al. Ocular manifestations and clinical characteristics of 535 cases of COVID-19 in Wuhan, China: a cross-sectional study. Acta Ophthalmol 2020; 98:e951–e959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kleimann Z. 3D Printers Save Hospital with Valves. BBC News [Electronic article]. March 2021; Available at: BBC News Technology, Kleinman Z. Accessed March 16, 2021. [Google Scholar]
- 7.Yuen KS, Ye ZW, Fung SY, et al. SARS-CoV-2 and COVID-19: the most important research questions. Cell Biosci 2020; 10:40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Rettner R. How does the new coronavirus compare with the flu? Live Sci 2020. Available in: https://www.scientificamerican.com/article/how-does-the-new-coronavirus-compare-with-the-flu/. Accessed July 13, 2021. [Google Scholar]
- 9.Tian S, Xiong Y, Liu H, et al. Pathological study of the 2019 novel coronavirus disease (COVID-19) through postmortem core biopsies. Mod Pathol 2020; 33:1007–1014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Felsenstein S, Herbert JA, McNamara PS, et al. COVID-19: immunology and treatment options. Clin Immunol 2020; 215:108448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Becker RC. COVID-19 update: COVID-19-associated coagulopathy. J Thromb Thrombolysis 2020; 50:54–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wu P, Duan F, Luo C, et al. Characteristics of ocular findings of patients with coronavirus disease 2019 (COVID-19) in Hubei Province, China. JAMA Ophthalmol 2020; 138:575–578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Farias LPG, Strabelli DG, Fonseca EKUN, et al. Alterações tomográficas torácicas em pacientes sintomáticos respiratórios com a COVID-19. Radiol Bras 2020; 53:255–326.32904780 [Google Scholar]
- 14.Simpson S, Kay FU, Abbara S, et al. Radiological Society of North America Expert Consensus Statement on reporting chest CT findings related to COVID-19: endorsed by the Society of Thoracic Radiology, the American College of Radiology, and RSNA. J Thorac Imaging 2020; 35:219–227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Flood TP, Braude LS, Jampol LM, et al. Computed tomography in the management of orbital infections associated with dental disease. Br J Ophthalmol 1982; 66:269–274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Swift AC, Charlton G. Sinusitis and the acute orbit in children. J Laryngol Otol 1990; 104:213–216. [DOI] [PubMed] [Google Scholar]
- 17.Williams BJ, Harrison HC. Subperiosteal abscesses of the orbit due to sinusites in childhood. Aust N Z J Ophthamol 1991; 19:29–36. [DOI] [PubMed] [Google Scholar]
- 18.Jabor MA, Amedee RG. Orbital complications of sinusitis. J LA State Med Soc 1997; 149:105–108. [PubMed] [Google Scholar]
- 19.Mills RP, Kartush JM. Orbital wall thickness and the spread of infection from the paranasal sinuses. Clin Otolaryngol 1985; 10:209–216. [DOI] [PubMed] [Google Scholar]
- 20.Recalde-Zamacona B, Tomás-Velázquez A, Campo A, et al. Chronic rhinosinusitis is associated with prolonged SARS-CoV2 RNA shedding in upper respiratory tract samples: a case-control study. J Intern Med 2021; 289:921–925. [DOI] [PubMed] [Google Scholar]
- 21.Lee S, Yen MT. Management of preseptal and orbital cellulitis. Saudi J Ophthalmol 2011; 25:21–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Byrne N, Plonsker JH, Tan LA, et al. Orbital cellulitis with pansinusitis and subdural empyema. J Emerg Med 2016; 52:e41–e43. [DOI] [PubMed] [Google Scholar]
- 23.Mathew AV, Craig E, Al-Mahmoud RB, et al. Paediatric post-septal and pre- septal cellulitis: 10 years’ experience at a tertiary-level children's hospital. Br J Radiol 2014; 87:20130503. [DOI] [PMC free article] [PubMed] [Google Scholar]