Summary
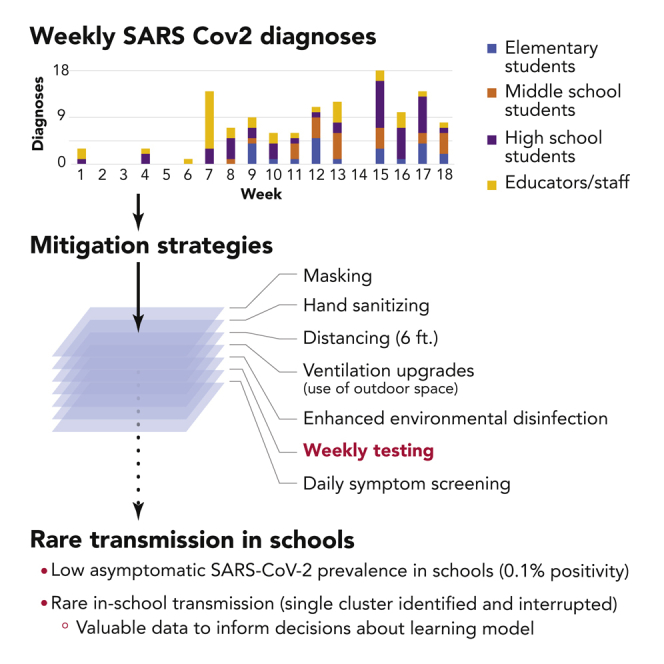
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) transmission in K–12 schools was rare during in 2020–2021; few studies included Centers for Disease Control and Prevention (CDC)-recommended screening of asymptomatic individuals. We conduct a prospective observational study of SARS-CoV-2 screening in a mid-sized suburban public school district to evaluate the incidence of asymptomatic coronavirus disease 2019 (COVID-19), document frequency of in-school transmission, and characterize barriers and facilitators to asymptomatic screening in schools. Staff and students undergo weekly pooled testing using home-collected saliva samples. Identification of >1 case in a school prompts investigation for in-school transmission and enhancement of safety strategies. With layered mitigation measures, in-school transmission even before student or staff vaccination is rare. Screening identifies a single cluster with in-school staff-to-staff transmission, informing decisions about in-person learning. The proportion of survey respondents self-reporting comfort with in-person learning before versus after implementation of screening increases. Costs exceed $260,000 for assays alone; staff and volunteers spend 135–145 h per week implementing screening.
Keywords: COVID-19, SARS-CoV-2, K-12 schools, asymptomatic SARS-CoV-2 screening, in-school SARS-CoV-2 transmission, prevention, mitigation
Graphical abstract
Highlights
-
•
In-school SARS-CoV-2 transmissions are rare with screening and safety measures
-
•
Comfort with in-person learning increases after screening program implementation
-
•
Educator workplace safety beyond in-classroom mitigation is a key priority
-
•
Benefits must be balanced against high financial and human resource requirements
Reports of rare SARS-CoV-2 transmission in K–12 schools are limited by lack of asymptomatic screening. Doron, Ingalls, et al. report that public-school screening for asymptomatic SARS-CoV-2 in 2020–2021 provides valuable data about in-school transmission risk and informs decisions about in-person learning, but human and financial resource requirements are high.
Introduction
The coronavirus disease 2019 (COVID-19) pandemic led to a global transition to remote learning in the spring of 2020. Many US schools persisted in this model in 2020–2021.1, 2, 3 By April 2021, the proportion of students attending school fully in person had increased but with substantial differences across racial and ethnic lines. Schools and families struggled to balance the challenges and inequities of remote learning against the risks of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection of in-person education.4 Where community rates are high, for example, in the absence of widespread vaccination, it is expected that some students and staff who enter school buildings will unknowingly be infected with COVID-19. A central question is whether they will transmit to others in the school setting. Data from both international and US settings in 2020–2021 suggested that where mitigation strategies, such as masking, distancing, and ventilation upgrades, are well implemented, in-school transmission of COVID-19 is rare.5, 6, 7, 8, 9 However, the lack of widespread SARS-CoV-2 testing of students and faculty and staff without symptoms (“screening”) precluded these reports from assessing the prevalence of asymptomatic infection, possibly placing educators and staff, students, and household members at risk.
The US government now provides financial and technical support for regular asymptomatic screening in K–12 schools, which is anticipated to continue into the 2021–2022 school year.10,11 Purported benefits of screening include revealing in-school transmission risk with mitigation measures in place, providing a snapshot of community COVID-19 prevalence, and reducing risk by identifying and isolating people with COVID-19 before onward transmission occurs.12 In the fall of 2020, we developed a consortium of 30 Massachusetts public-school districts (cities, towns, or groups of small towns), ranging in geographic and demographic characteristics, to implement and evaluate screening programs and collectively advocate for and negotiate lower screening costs.13 Many member districts were unfortunately unable to implement the program as they remained fully remote. Here, we report the results of a screening program in one well-resourced member district.
Results
Identification of COVID-19 through the screening program
A total of 921 staff were eligible for participation in the screening program, including 256 at the high school and 258 at the middle school and central office. Students eligible for screening included 1,403 at the high school and 1,000 at the middle school. Excluding holiday weeks (weeks 8, 9, and 14) and school closures, participation in screening varied by week from 61% to 77% of eligible high school students (mean [SD]: 66% [5.6%]), 70% to 81% of eligible middle school students (75% [4.0%]), and 73% to 83% (78% [2.8%]) of eligible staff. Common reasons for failure to submit a sample included absence from school on the day of kit distribution or collection or forgotten samples. The turnaround time from receipt of samples to results of a negative pool was approximately 48 h; time from consent to perform diagnostic testing to verification of diagnostic results was 2–4 h.
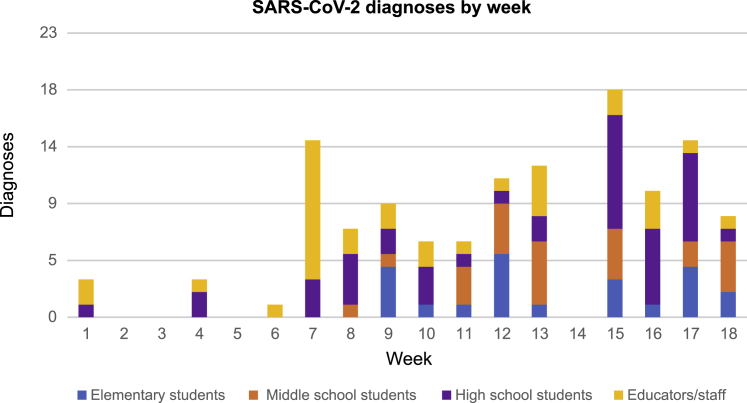
During the screening program period, rates of incident COVID-19 in the district’s municipality rose steadily from 5 to 32/100,000/day (Table 1). From weeks 1 to 18, 126 COVID-19 cases were identified among faculty and staff and students who were enrolled in any in-person learning model (Figure 1), representing 38 faculty and staff and 88 students. Of these 126 cases, 39 (14 staff and 25 students) were identified through the screening program and 87 (24 staff and 63 students) were identified through outside tests.
Table 1.
Results of a public K–12 school screening program
| Week | Staff (total n = 921) |
Students (total n = 2,403) |
Town COVID-19 metricsa |
Weighted staff city and town of residence metricsb |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Participated in screening: n | Positive results by screening: n (% of screened) | Positive results by outside testing: n | Participated in screening: n | Positive results by screening: n (% of screened) | Positive results by outside testing: n | 14-day average of daily cases/ 100K | Molecular test positivity (%) | 14-day average of daily cases/ 100K | Molecular test positivity (%) | |
| 1 | 1,005c | 0 (0) | 2 | 3,596c | 1 (0.03) | 0 | 2.2 | 0.09 | NA | NA |
| 2 | 0 | 0 | 2.4 | 0.08 | 5.4 | 0.8 | ||||
| 3 | 0 | 0 | 2.6 | 0.10 | 6.6 | 0.9 | ||||
| 4 | 363 | 0 (0) | 1 | 2 | 1.7 | 0.09 | 7.0 | 1.0 | ||
| 5 | 721 | 0 (0) | 0 | 0 | 3.4 | 0.17 | 8.4 | 1.2 | ||
| 6 | 739 | 1 (0.14) | 0 | 1,847 | 0 (0) | 0 | 5.8 | 0.26 | 11.0 | 1.4 |
| 7 | 687 | 5 (0.73) | 6 | 1,648 | 2 (0.12) | 1 | 5.3 | 0.23 | 14.8 | 1.7 |
| 8 | 584 | 2 (0.34) | 0 | 774 | 1 (0.13) | 4 | 13.7 | 0.58 | 20.4 | 2.2 |
| 9 | 602 | 2 (0.33) | 0 | 759 | 0 (0) | 7 | 19.5 | 0.78 | 23.8 | 2.4 |
| 10 | 737 | 0 (0) | 2 | 1,774 | 2 (0.11) | 2 | 19.5 | 0.88 | 25.4 | 2.8 |
| 11 | 749 | 0 (0) | 1 | 1,636 | 3 (0.18) | 2 | 19.7 | 0.98 | 34.4 | 3.7 |
| 12 | 763 | 0 (0) | 1 | 1,578 | 2 (0.13) | 8 | 20.9 | 1.05 | 43.8 | 4.2 |
| 13 | 735 | 0 (0) | 4 | 1,387 | 0 (0) | 8 | 21.6 | 1.26 | 43.3 | 4.4 |
| 14 | 0 | 0 (NA) | 0 | 0 | 0 (NA) | 0 | 18.8 | 1.58 | 40.7 | 4.6 |
| 15 | 727 | 1 (0.14) | 2 | 1,576 | 6 (0.38) | 10 | 19.5 | 2.34 | 43.2 | 5.5 |
| 16 | 673 | 1 (0.15) | 3 | 1,579 | 3 (0.19) | 4 | 24.5 | 2.11 | 55.5 | 5.7 |
| 17 | 722 | 1 (0.14) | 1 | 1,622 | 2 (0.12) | 11 | 25.0 | 1.61 | 53.9 | 4.8 |
| 18 | 733 | 1 (0.14) | 1 | 1585 | 3 (0.19) | 4 | 31.5 | 1.59 | 46.0 | 4.1 |
| Total | 10,050 | 14 (0.14) | 24 | 21,361 | 25 (0.12) | 63 | ||||
From Massachusetts Department of Public Health (DPH). Includes results from regular screening of two institutions of higher education.14
From Massachusetts DPH. Consistent with many districts across MA, 87% of school staff live in other towns. The weighted averages are calculated from weekly data for each town or city where staff members live, weighted by the number of staff from each city or town. These are data averaged over 2-week periods ending with the week listed, the format in which they reported by the state.
Baseline screening was offered to students at all grade levels (pre-K–12). Subsequent screening (weeks 6–18) was offered to middle and high school students (n = 2,403).
Figure 1.
Identification of SARS-CoV-2 through the screening program: SARS CoV-2 diagnoses during 18 weeks of in-person learning
This figure depicts the number of confirmed SARS-CoV-2 diagnoses among members of the school community. The horizontal axis shows week number. The vertical axis shows number of confirmed diagnoses. The bars are broken down into categories: elementary students (blue); middle school students (orange); high school students (purple); and educators and staff (yellow).
In week 6, screening identified 1 positive staff member in the high school main office. Three additional main office staff members were identified as close contacts; all sought individual testing during quarantine and tested positive. In week 7, 4 additional main office staff members not identified as close contacts had positive results from the weekly screening, as well as 1 staff member not based in the main office and 2 high school students. Based on these results, the high school was transitioned to remote learning for a period of 3 weeks (including a holiday, leading to 1.5 weeks of school missed) to allow for full investigation. Possible risk factors and opportunities for reinforcement of existing protocols were identified in three categories. First, review of heating, ventilation, and air conditioner (HVAC) systems, including assessment of airflow in the main office using smoke, suggested airflow impedance in the main office area that was attributed to plexiglass dividers with sidewalls; these structures were rearranged. Second, location mapping and staff interviews highlighted occasions of mask removal at distances <6’, primarily for eating and drinking; additional spaces for unmasking and eating and drinking were provided. Third, high-traffic areas (especially in two-way entry and egress areas) and shared offices were identified; one-way traffic flow and schedules for single office occupancy were established. Because no additional cases were identified in screening among staff at other schools or among middle school students, all other schools in the district continued in-person learning.
Identification of COVID-19 outside the screening program
In week 9, 3 cases were identified in one elementary school classroom, all through outside testing of close contacts. After evaluation by school and board of health officials, transmission was thought to have occurred outside of school. This single class moved to remote learning for 10 calendar days (including a professional development day, thus missing 1 full school week). Screening at the middle and high school and among elementary staff revealed few additional cases, and in-person learning continued at other sites. In week 15 (post-holiday), 9 students with SARS-CoV-2 were identified at the high school: 5 via the screening program and 4 via outside testing. The high school transitioned to remote learning for 10 calendar days (including 2 weekends, thus missing 1 full school week) to permit an investigation for the presence of in-school transmission (ultimately determined not to have occurred), and in-person learning remained in place at other schools.
Implementation and acceptability
Survey responses were received from 491 educators and staff and 658 families and caregivers, response rates of 53% and 12%–24%, respectively, assuming 1 to 2 responses per family. Prior to baseline testing, the proportion of educators and staff who reported feeling “mostly comfortable” or “very comfortable” was 12%; after baseline testing, 82% reported feeling “reassured” or “very reassured” (Table S1). Among families and caregivers, these proportions were 39% and 87%. Perceived benefits of the screening program for families and caregivers included outbreak prevention (91%), increased opportunity for in-person learning (88%), increased safety for educators and staff and their families (80%) and for students and their families (80%), and a reminder to follow safety protocols (46%). Perceived detriments of the screening program for families and caregivers included cost (35%), false sense of security (30%), stigma (6%), privacy (5%), burden to collect samples (4%), impact on family if student tests positive (4%), and impact of teachers needing to quarantine (4%); 47% reported no perceived detriments.
Assay costs averaged $10/individual screened/week, including both pooled screening and follow-up individual diagnostic testing; assay costs alone totaled >$260,000 for the 18-week period (excluding the baseline one-time screen). Community fundraising supported the monetary costs of the pilot screening program. Staff and volunteers from across the district participated in outreach and implementation of the screening program. The technology department developed and maintained a Google site for registering barcodes for each sample, requiring 4 h for initial development and 1 h/week for maintenance. Parent volunteers spent approximately 10 h/week for the first several weeks of the program to assemble saliva collection kits and collect and transport samples. Bus and van drivers, not driving on Wednesdays due to fully remote learning, spent a total of 54 h/week assembling test kits; on testing days, they also collected samples at individual schools and transported them to a central location for processing and shipping.
School nurses reinforced correct collection technique, prepared samples for shipping, maintained records of participation, and reviewed and addressed results. Fifteen school nurses each spent an average of 4 h per confirmed SARS-CoV-2 case (range, 1–6 h) to conduct contact tracing, provide education and support, and collaborate with the health department. The Director of Nursing also spent at least 20 h/week on result follow-up, management of positive cases, data entry, and program administration. Nursing, administration, and parent volunteer staff also dedicated additional evening and weekend hours consulting with other public-school districts implementing screening programs.
Discussion
This study reports the results of widespread, weekly asymptomatic SARS-CoV-2 screening among public-school K–12 students and staff. Our findings confirm and extend those from studies using primarily symptomatic testing: with mitigation measures, such as masking and distancing, that were used in many schools during the 2020–2021 school year, in-school transmission events were rare.5,7, 8, 9,12,15, 16, 17, 18, 19 Our results additionally demonstrate that rates of asymptomatic SARS-CoV-2 infection among students and staff were low, despite high community rates in the pre-vaccination era. Nevertheless, occasional in-school transmissions did occur; these were associated with breaks in mitigation protocols, consistent with data from Israel, Utah, Mississippi, Georgia, and Florida.20, 21, 22, 23, 24
There were several key lessons learned from these evaluations of COVID-19 risk in schools in 2020–2021, which will inform decision making for future school years. First, although the risk for severe illness from COVID-19 is relatively low in children, there was concern at the start of the school year that unrecognized or asymptomatic infection in students would be common, placing their unvaccinated household members at risk for infection.25,26 This concern led many schools across the United States to avoid in-person learning, which was associated with substantial non-COVID-19-related mental and physical health risks.4,27, 28, 29, 30, 31, 32, 33 Inequities that existed before the pandemic in education and health were exacerbated by school closures, particularly in Black, Latinx, and Indigenous communities and among children experiencing housing and food insecurity.4,34,35 Our findings provide reassurance that, even despite high community COVID-19 rates, asymptomatic infection was rare.
Second, educator health must be a key priority. Between 25% and 50% of educators have medical conditions or older age that place them at risk for COVID-19 complications or live with household members with a higher risk condition.36,37 Our results highlight unique issues for educator workplace safety that extend beyond the usually discussed in-classroom mitigation strategies, especially if educator vaccination is not widespread, including the need for well-ventilated, distanced places for eating and drinking, as well as shared workspace with adequate distancing between staff, consistent with SARS-CoV-2 outbreaks observed in other non-school low-risk settings, such as clusters of infection in hospital employees linked to eating and drinking in shared breakrooms.38,39
Third, in the pre-vaccination period, regular screening of asymptomatic students and staff for SARS-CoV-2 in the K–12 setting provided three additional benefits alongside other effective mitigation strategies. When community COVID-19 rates were high, it is likely that screening provided an added layer of protection by detecting infections before additional in-school transmission occurred and allowing investigation and improvement in potentially associated practices. Modeling (based both on wild-type and delta-variant virus) suggests that weekly screening would permit 5-day in-person education at the same total in-school COVID-19 risk as 2-day hybrid education without screening, particularly with high community COVID-19 rates.40,41,42 Additionally, screening programs provided data to inform responses to detected cases, e.g., allowing targeted closing of specific classrooms, offices, or buildings while the remaining facilities continued in-person learning and work. Last, consistent with a Rand report, screening made faculty, staff, parents, and students feel reassured about the safety of in-person education.11,43,44,45
Despite these benefits, there are disadvantages associated with screening. Some public-school screening programs have reported high rates of false-positive results, leading to unnecessary missed days of school.46 False-positive results may be minimized by screening only when community disease prevalence exceeds specific thresholds, prioritizing unvaccinated students and staff, and ensuring prompt access to confirmatory testing.47,48 The resources required to implement weekly screening in public schools are also substantial. This pilot program cost more than $260,000 in assay costs alone over 18 weeks. This program also required approximately 135–145 h per week of staff and volunteer time. Although point-of-care antigen tests may reduce assay costs, they also introduce additional operational considerations, such as staff time to process antigen cards and need for confirmatory testing.49,50 Screening was implemented successfully in this community only because the town had extensive financial resources, private funds, and parents and staff available to devote time to this initiative. The cost to implement weekly screening for all K–12 public school students in the United States has been estimated at $42.5 billion.51 Local, state, and national leaders must recognize that use of private funds is neither a sustainable nor an equitable approach; schools will need extensive state and federal support not only for assay cost but for all operational components of a screening program.
Efforts by Centers for Disease Control and Prevention (CDC) and US Department of Health and Human Services (HHS) to support K–12 school screening will address some of these financial burdens, and PCR test costs may decline over time, but implementation decisions should take into account whether these investments are “worth” the benefits they confer. In the study week with highest screen positivity (week 15: 0.3%), total cost for assays alone was $3,290/case detected by screening. A short-term analysis found that the cost of school screening could be offset by child-care costs saved from unplanned remote learning days; however, a comprehensive assessment of the cost-effectiveness of screening in K–12 schools will require data not yet available about the costs and clinical outcomes for students, staff, and families that result from COVID-19 infections, quarantine, and loss of in-person learning.42 Screening value may also differ between an elementary school (unvaccinated students, perhaps with lower transmission) and a high school (some vaccinated students, perhaps with higher transmission). It is also difficult to assign economic value to outcomes, such as reassurance for staff and families and the avoidance of a transition to remote learning. In our pilot, days of in-person school “lost” to quarantine after detection of asymptomatic cases were likely balanced by in-person days “gained” by maintaining a hybrid learning model throughout a statewide surge, during which many other districts in the state were fully remote.
The role that screening for SARS-CoV-2 in the pre-K–12 setting should play in the upcoming 2021–2022 school year is still unclear. Although vaccination is now available, vaccine uptake remains highly variable between communities, students younger than 12 are not yet eligible for vaccination, and the more contagious delta variant is spreading rapidly and causing vaccine breakthrough infections.52 At the same time, many schools are planning to remove mitigation measures, such as masking and distancing, for the upcoming school year.53 In settings with low vaccination rates and high transmission—or in the event that emerging viral variants efficiently evade immune responses from vaccines—together with loosened mitigation protocols, students and staff may continue to face substantial COVID-19 risks in schools, and screening could again provide both critical data and risk reduction. CDC suggests screening of unvaccinated teachers and staff regardless of community COVID-19 case rates and screening of unvaccinated students when incidence is at least 10/100,000 people/week.48 If screening is done at school, districts will need to plan for many of the implementation challenges that were identified in this study.
In summary, schools serve an essential function in society and require dedicated mitigation measures and resources to operate safely during the COVID-19 pandemic. The screening program we conducted during a period of high COVID-19 case rates before vaccination provided reassurance to students, families, and educators and detected one instance of in-school transmission to multiple members of a shared work area but at substantial financial and human resource cost. Planning for the upcoming school year should carefully consider local vaccination rates and case counts when evaluating how to most efficiently allocate limited resources to support safe in-person education.
Limitations of the study
This pilot evaluation was conducted in a single, suburban, primarily White, and affluent community. It was not intended to be widely generalizable but instead to identify key barriers and facilitators, some of which are likely even greater and require more planned support in less well-resourced settings.50,54, 55, 56 Additionally, it is unknown to what extent these benefits would have been seen had the testing program been implemented in the setting of full-time in-person school rather than a hybrid model.
STAR★Methods
Key resources table
| REAGENT or RESOURCE | SOURCE | IDENTIFIER |
|---|---|---|
| Critical commercial assays | ||
| Saliva Clear (Mirimus Laboratories) | Mirimus | https://www.salivaclear.com/ |
| Saliva Direct (Mirimus Laboratories) | Mirimus | https://www.mirimus.com/, https://ysph.yale.edu/salivadirect/ |
| Software and algorithms | ||
| Microsoft Excel | Microsoft Office | https://www.microsoft.com/en-us/microsoft-365/excel |
| Google Forms (for online survey) | https://www.google.com/forms/about/ | |
Resource availability
Lead contact
Further information and requests for resources should be directed to and will be fulfilled by the lead contact, Andrea Ciaranello (aciaranello@mgh.harvard.edu).
Materials availability
This study did not generate new unique reagents.
Experimental model and subject details
This public-school district is located in a suburban town; the population of 25,000- 30,000 is over 80% White, with a median household income of over $190,000.57 The district participates in a voluntary integration program that enrolls and transports students from the closest urban area. The district supports Pre-K to Grade 12 students in 1 preschool, 7 elementary schools (K-5), 1 middle school (6-8) and 1 high school (9-12). In fall 2020, families were offered the option to enroll students in a fully-remote curriculum (approximately 500 students) or a hybrid-learning curriculum (approximately 4000 students). Hybrid learning consisted of in-person learning 2 days per week and remote learning 2.5 days per week; students with high learning needs attended in-person 4 days per week, along with all students in Kindergarten and Grade 1, and later Grade 2. Safety measures were based on the CDC and state Department of Public Health (DPH) and Department of Education guidelines, and included mandatory masking (except during lunch and designated mask breaks), frequent hand sanitizing, 6 feet of distance separating students seated at their desks in most classrooms, ventilation upgrades as feasible based on age of individual buildings (MERV-13 filters in all buildings), use of outdoor space when possible, enhanced environmental disinfection (nightly disinfection of all surfaces, with high touch surfaces disinfected frequently throughout the day and use of electrostatic sprayers), and daily symptom screening.58,59
The school district independently implemented the screening program as a component of COVID-19 mitigation efforts. Parents and guardians provided consent for student testing. All educational and consent materials posted to the school district web site were translated into Spanish, French, Chinese and Korean. The study team later analyzed de-identified data that the district had originally collected for routine operational use. The Mass General Brigham IRB designated this study to be not human subjects research.
Method details
Screening approach
Baseline individual SARS-CoV-2 PCR screening was offered to all asymptomatic staff and students (at all grade levels) prior to the opening of hybrid learning. Weekly pooled PCR screening began three weeks later for all staff in the district and students in the middle and high schools. This testing frequency was chosen to balance case-finding with feasibility, based in part on mathematical models of university and K-12 testing and established university testing programs.40,60 Pooled testing is a cost-saving strategy that involves mixing multiple specimens together and processing them using a single diagnostic test, with a potential for modest decrease in sensitivity and substantial cost-savings compared to individual PCR.61 Positive pools are “deconvoluted” until a positive individual specimen or specimens are identified.62 An at-home saliva collection approach was selected due to its non-invasiveness and the ability for families to collect specimens at home without the involvement of school staff.
Participation in screening was not required but strongly encouraged. District staff conducted a series of four educational webinars for the entire school community. Additional information on logistics and rationale for screening was disseminated via emails and multiple social media, online, and print platforms. Saliva collection packages, including vials labeled with unique barcodes, collection straws, and instructions, were assembled and distributed to staff and students at school. Video instructions were available online. Students or staff who tested positive for SARS-CoV-2 within the previous 90 days were excluded from participation that week. Saliva samples (1 mL volume) were collected and registered at home, then returned to the schools for shipping to a commercial laboratory. Students with in-person learning scheduled on Monday/Thursday were screened on Mondays, enabling result-return and contact tracing over 48 h of remote learning, and students present Tuesday/Friday were screened on Tuesdays. During weeks of fully remote school or vacation, students and staff participated in screening by pickup up test kits and bringing specimens to centralized locations.
Laboratory procedures
Screening for SARS-CoV-2 was performed in a commercial laboratory using PCR directed at two targets in the nucleocapsid gene, N1 and N2 (Saliva Clear, New York State Department of Health-authorized, US FDA emergency use authorization (EUA) pending). Samples failing to demonstrate DNA on quality testing were not assayed. If a pool of 24 tests resulted as positive, pooled testing was repeated with sequentially fewer individual samples, until positive results were isolated to a pool of 2. Those two individuals were then contacted for consent to perform individual diagnostic testing in the same commercial laboratory using the originally provided specimen (Saliva Direct PCR, US FDA EUA), at which time US Department of Health and Human Services (HHS)-required demographic data were collected. No additional specimen was required for diagnostic testing. Individuals from positive pairs were instructed to isolate while awaiting diagnostic test results. Positive diagnostic SARS-CoV-2 test results were reported directly to the staff and parents/guardians of students, as well as local health officials and the director of nursing.
Result return and contact tracing
All individuals with a positive test result were required to isolate per CDC and state Department of Public Health (DPH) guidelines.63 Confirmed cases resulted in contact tracing performed by the health department linked to the address of each infected individual (to identify community contacts, as resources allowed) and the school nursing department (for in-school contacts), in accordance with DPH guidelines.63 Close contacts were instructed to quarantine and seek testing according to state guidelines (14 days regardless of testing through 12/2/20, with options for shorter quarantine periods following negative tests thereafter).43
Throughout the screening program, educators/staff and students were regularly reminded to stay out of school and seek outside diagnostic PCR testing if they developed symptoms consistent with COVID-19, even if they had recently participated in the pooled testing; some also sought outside testing after exposures or travel.58 People with positive outside tests were asked to communicate their results to school nurses immediately. Local health officials also transmitted results to the district for town residents. If > 1 case was identified in a single school over a 2-week period through screening or outside testing, an investigation was initiated to determine the presence or absence of in-school transmission. This included review for possible exposures in and outside of school and mapping of student and educator/staff movement patterns and locations of staff workstations; investigation and contact tracing was conducted by school nurses and local health officials and continued even if remote learning was implemented. Educators/staff and students also answered detailed questions regarding location and duration of mask breaks, eating, and drinking; shared objects and surfaces; and recall of any symptoms prior to detection of the cluster.
Survey
An online survey was sent to educators/staff and families/caregivers of students before baseline testing and before screening week 11 (supplemental information).64 Domains included: level of comfort with in-person schooling without baseline testing, degree of reassurance about school safety after results of baseline testing; change in comfort with in-person learning due to the screening program; and perceived benefits and detriments of weekly screening. Program staff tallied the number and type of personnel and number of hours spent by each to implement screening.
Quantification and statistical analysis
We calculated total case counts (Figure 1, Table 1, and Results sections: Identification of COVID-19 through the screening program and Identification of COVID-19 outside the screening program), descriptive statistics about screening particpation proportions among students and staff (Results section: Identification of COVID-19 through the screening program), positivity rates (Table 1, Results section: Identification of COVID-19 through the screening program), survey results as proportions of responses (Results section: Implementation and acceptability, Table S1), and resource use as sums of person-hours spent implementing the program and sums of assay costs (Results section: Implementation and acceptability). All sums, as well as dispersion and precision measures (mean, standard deviation for proportions participating weekly), were calculated in Excel.
Acknowledgments
The Wellesley Education Foundation provided financial and programmatic support for screening, including survey design, implementation, and analysis. We thank the students, families, faculty, and staff of Wellesley Public Schools; the Wellesley Education Foundation; the Safer Teachers, Safer Students Testing Collaborative; the Wellesley Board of Health; and the nursing staff and bus and van drivers of the Wellesley Public Schools. We also thank Alyssa Amick, Elena Jin, and Andrew Tang for assistance in manuscript and figure preparation.
Author contributions
Conceptualization, S.D., R.R.I., J.S.B., and A.C.; methodology, A.B., H.W.B., L.H.C., L.C., K.G., D.G., L.L., D.L., and M.T.; validation, S.D., R.R.I., A.B., L.C., and A.C.; formal analysis, A.B. and A.C.; investigation, A.B., J.S.B., H.W.B., L.H.C., L.C., K.G., D.G., L.L., D.L., and M.T.; resources, A.B., J.S.B., D.L., and M.T.; data curation, A.B. and A.C.; writing – original draft, S.D., R.R.I., and A.C.; writing – review and editing, all authors; visualization, A.B. and A.C.; supervision, S.D., R.R.I., and A.C.; funding acquisition, K.G. and D.L.
Declaration of interests
The authors declare no competing interests.
Published: October 27, 2021
Footnotes
Supplemental information can be found online at https://doi.org/10.1016/j.xcrm.2021.100452.
Supplemental information
Data and code availability
All data reported in this paper will be shared by the lead contact upon request. This paper does not report original code. Any additional information required to reanalyze the data reported in this paper is available from the lead contact upon request.
References
- 1.Education Week . 2020. School districts’ reopening plans: a snapshot.https://www.edweek.org/leadership/school-districts-reopening-plans-a-snapshot/2020/07 [Google Scholar]
- 2.Liesman S. 2020. Half of U.S. elementary and high school students will study virtually only this fall, study shows. CNBC.https://www.cnbc.com/2020/08/11/half-of-us-elementary-and-high-school-students-will-study-virtually-only-this-fall-study-shows.html [Google Scholar]
- 3.Belsha K. 2020. A nationwide divide: Hispanic and Black students more likely than white students to start the year online. Chalkbeat.https://www.chalkbeat.org/2020/9/11/21431146/hispanic-and-black-students-more-likely-than-white-students-to-start-the-school-year-online [Google Scholar]
- 4.Oster E., Jack R., Halloran C., Schoof J., McLeod D., Yang H., Roche J., Roche D. Disparities in learning mode access among K-12 students during the COVID-19 pandemic, by race/ethnicity, geography, and grade level - United States, September 2020-April 2021. MMWR Morb. Mortal. Wkly. Rep. 2021;70:953–958. doi: 10.15585/mmwr.mm7026e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Guthrie B.L., Seiler J., Tolentino L., Jiang W., Fischer M., Issema R., Fuller S., Green D., Tordoff D.M., Meisner J., et al. 2020. Summary of evidence related to schools during the COVID-19 pandemic.https://www.doh.wa.gov/Portals/1/Documents/1600/coronavirus/20201019-SchoolsSummary.pdf [Google Scholar]
- 6.Honein M.A., Barrios L.C., Brooks J.T. Data and policy to guide opening schools safely to limit the spread of SARS-CoV-2 infection. JAMA. 2021;325:823–824. doi: 10.1001/jama.2021.0374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.National Centre for Immunisation Research and Surveillance (NCIRS) 2020. COVID-19 transmission in educational settings in NSW Term 3.https://www.ncirs.org.au/sites/default/files/2020-10/COVID-19%20Transmission%20in%20educational%20settings%20in%20NSW%20Term%203%20report_0.pdf [Google Scholar]
- 8.Ismail S.A., Saliba V., Lopez Bernal J., Ramsay M.E., Ladhani S.N. SARS-CoV-2 infection and transmission in educational settings: a prospective, cross-sectional analysis of infection clusters and outbreaks in England. Lancet Infect. Dis. 2021;21:344–353. doi: 10.1016/S1473-3099(20)30882-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Larosa E., Djuric O., Cassinadri M., Cilloni S., Bisaccia E., Vicentini M., Venturelli F., Giorgi Rossi P., Pezzotti P., Bedeschi E., Reggio Emilia Covid-19 Working Group Secondary transmission of COVID-19 in preschool and school settings in northern Italy after their reopening in September 2020: a population-based study. Euro Surveill. 2020;25:2001911. doi: 10.2807/1560-7917.ES.2020.25.49.2001911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.HHS.gov . 2021. Biden administration to invest more than $12 billion to expand COVID-19 testing.https://www.hhs.gov/about/news/2021/03/17/biden-administration-invest-more-than-12-billion-expand-covid-19-testing.html [Google Scholar]
- 11.Massachusetts Department of Education . 2021. COVID-19 testing program.https://www.doe.mass.edu/covid19/testing/default.html [Google Scholar]
- 12.Gillespie D.L., Meyers L.A., Lachmann M., Redd S.C., Zenilman J.M. The experience of two independent schools with in-person learning during the COVID-19 pandemic. medRxiv. 2021 doi: 10.1101/2021.01.26.21250065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Safer Teachers, Safer Students Collaborative . 2021. Massachusetts K-12 asymptomatic COVID-19 screening dashboard.https://ma-k12testingcollaborative.org/ [Google Scholar]
- 14.Massachusetts Department of Education . 2021. Archive of COVID-19 weekly public health reports. Mass.gov.https://www.mass.gov/info-details/archive-of-covid-19-weekly-public-health-reports [Google Scholar]
- 15.Falk A., Brenda A., Falk P., Steffen S., Wallace Z., Høeg T.B. COVID-19 cases and transmission in 17 K–12 schools — Wood County, Wisconsin, August 31–November 29, 2020. Morb. Mortal Wkly. Rep. 2021;70:136–140. doi: 10.15585/mmwr.mm7004e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zimmerman K.O., Akinboyo I.C., Brookhart M.A., Boutzoukas A.E., McGann K.A., Smith M.J., Maradiaga Panayotti G., Armstrong S.C., Bristow H., Parker D., et al. ABC SCIENCE COLLABORATIVE Incidence and secondary transmission of SARS-CoV-2 infections in schools. Pediatrics. 2021;147 doi: 10.1542/peds.2020-048090. e2020048090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fricchione M.J., Seo J.Y., Arwady M.A. Data-driven reopening of urban public education through Chicago’s tracking of COVID-19 school transmission. J. Public Health Manag. Pract. 2021;27:229–232. doi: 10.1097/PHH.0000000000001334. [DOI] [PubMed] [Google Scholar]
- 18.NYC Department of Education . 2021. COVID-19: in-school testing program results.https://www.schools.nyc.gov/school-life/health-and-wellness/covid-information/covid-19-testing-for-students/covid-19-in-school-testing-program-results [Google Scholar]
- 19.Oster E., The School Superintendents Association. the National Association of Secondary School Principals. the National Association of Elementary School Principals . 2021. COVID-19 school response dashboard.https://covidschooldashboard.com/ [Google Scholar]
- 20.Stein-Zamir C., Abramson N., Shoob H., Libal E., Bitan M., Cardash T., Cayam R., Miskin I. A large COVID-19 outbreak in a high school 10 days after schools’ reopening, Israel, May 2020. Euro Surveill. 2020;25:2001352. doi: 10.2807/1560-7917.ES.2020.25.29.2001352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Taylor K. 2020. ‘Out of control’: when schools opened in a virus hot spot. The New York Times.https://www.nytimes.com/2020/10/18/us/coronavirus-schools-reopening-outbreak.html [Google Scholar]
- 22.Hobbs C.V., Martin L.M., Kim S.S., Kirmse B.M., Haynie L., McGraw S., Byers P., Taylor K.G., Patel M.M., Flannery B., CDC COVID-19 Response Team Factors associated with positive SARS-CoV-2 test results in outpatient health facilities and emergency departments among children and adolescents aged <18 years - Mississippi, September-November 2020. MMWR Morb. Mortal. Wkly. Rep. 2020;69:1925–1929. doi: 10.15585/mmwr.mm6950e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Doyle T., Kendrick K., Troelstrup T., Gumke M., Edwards J., Chapman S., Propper R., Rivkees S.A., Blackmore C. COVID-19 in primary and secondary school settings during the first semester of school reopening - Florida, August-December 2020. MMWR Morb. Mortal. Wkly. Rep. 2021;70:437–441. doi: 10.15585/mmwr.mm7012e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gold J.A.W., Gettings J.R., Kimball A., Franklin R., Rivera G., Morris E., Scott C., Marcet P.L., Hast M., Swanson M., et al. Georgia K–12 School COVID-19 Investigation Team Clusters of SARS-CoV-2 infection among elementary school educators and students in one school district - Georgia, December 2020-January 2021. MMWR Morb. Mortal. Wkly. Rep. 2021;70:289–292. doi: 10.15585/mmwr.mm7008e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.American Academy of Pediatrics . 2021. Children and COVID-19: state-level data report.https://services.aap.org/en/pages/2019-novel-coronavirus-covid-19-infections/children-and-covid-19-state-level-data-report/ [Google Scholar]
- 26.Fung H.F., Martinez L., Alarid-Escudero F., Saloman J.A., Studdert D.M., Andrews J.R., Goldhaber-Fiebert J.D. The household secondary attack rate of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2): a rapid review. Clin. Infect. Dis. 2021;73:S138–S145. doi: 10.1093/cid/ciaa1558. Stanford-CIDE Coronavirus Simulation Model (SC-COSMO) Modeling Group [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Masonbrink A.R., Hurley E. Advocating for children during the COVID-19 school closures. Pediatrics. 2020;146:e20201440. doi: 10.1542/peds.2020-1440. [DOI] [PubMed] [Google Scholar]
- 28.Pietrobelli A., Pecoraro L., Ferruzzi A., Heo M., Faith M., Zoller T., Antoniazzi F., Piacentini G., Fearnbach S.N., Heymsfield S.B. Effects of COVID-19 lockdown on lifestyle behaviors in children with obesity living in Verona, Italy: a longitudinal study. Obesity (Silver Spring) 2020;28:1382–1385. doi: 10.1002/oby.22861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Leeb R.T., Bitsko R.H., Radhakrishnan L., Martinez P., Njai R., Holland K.M. Mental health–related emergency department visits among children aged <18 years during the COVID-19 pandemic — United States, January 1–October 17, 2020. MMWR Morb. Mortal Wkly. Rep. 2020;69:1675–1680. doi: 10.15585/mmwr.mm6945a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Haripersad Y.V., Kannegiesser-Bailey M., Morton K., Skeldon S., Shipton N., Edwards K., Newton R., Newell A., Stevenson P.G., Martin A.C. Outbreak of anorexia nervosa admissions during the COVID-19 pandemic. Arch. Dis. Child. 2021;106:e15. doi: 10.1136/archdischild-2020-319868. [DOI] [PubMed] [Google Scholar]
- 31.Bignardi G., Dalmaijer E.S., Anwyl-Irvine A.L., Smith T.A., Siugzdaite R., Uh S., Astle D.E. Longitudinal increases in childhood depression symptoms during the COVID-19 lockdown. Arch. Dis. Child. 2020;106:791–797. doi: 10.1136/archdischild-2020-320372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Verlenden J.V., Pampati S., Rasberry C.N., Liddon N., Hertz M., Kilmer G., Viox M.H., Lee S., Cramer N.K., Barrios L.C., Ethier K.A. Association of children’s mode of school instruction with child and parent experiences and well-being during the COVID-19 pandemic - COVID experiences survey, United States, October 8-November 13, 2020. MMWR Morb. Mortal. Wkly. Rep. 2021;70:369–376. doi: 10.15585/mmwr.mm7011a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Burbio’s K-12 School Opening Tracker . 2021. Burbio.https://cai.burbio.com/school-opening-tracker/ [Google Scholar]
- 34.Harris B. 2020. Why Black families are choosing to keep their kids remote when schools reopen. The Hechinger Report.https://hechingerreport.org/why-black-families-are-choosing-to-keep-their-kids-remote-when-schools-reopen/ [Google Scholar]
- 35.Dorn E., Hancock B., Sarakatsannis J., Viruleg E. 2020. COVID-19 and student learning in the United States: the hurt could last a lifetime.https://ceros.mckinsey.com/coronavirus-promo-video-desktop [Google Scholar]
- 36.Claxton G., Levitt L., Kamal R., Neuman T., Kates J., Michaud J., Koma W., Rae M. 2020. How many teachers are at risk of serious illness if infected with coronavirus? KFF.https://www.kff.org/coronavirus-covid-19/issue-brief/how-many-teachers-are-at-risk-of-serious-illness-if-infected-with-coronavirus/ [Google Scholar]
- 37.Gaffney A.W., Himmelstein D., Woolhandler S. Risk for severe COVID-19 illness among teachers and adults living with school-aged children. Ann. Intern. Med. 2020;173:765–767. doi: 10.7326/M20-5413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Çelebi G., Pişkin N., Çelik Bekleviç A., Altunay Y., Salcı Keleş A., Tüz M.A., Altınsoy B., Hacıseyitoğlu D. Specific risk factors for SARS-CoV-2 transmission among health care workers in a university hospital. Am. J. Infect. Control. 2020;48:1225–1230. doi: 10.1016/j.ajic.2020.07.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Freyer F.J. 2020. Brigham and Women’s hospital completes investigation of coronavirus outbreak. The Boston Globe.https://www.bostonglobe.com/2020/10/19/metro/brigham-womens-hospital-completes-investigation-coronavirus-outbreak/?p1=Article_Inline_Text_Link [Google Scholar]
- 40.Bilinski A., Salomon J.A., Giardina J., Ciaranello A., Fitzpatrick M.C. Passing the test: a model-based analysis of safe school-reopening strategies. medRxiv. 2021 doi: 10.1101/2021.01.27.21250388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.McGee R.S., Homburger J.R., Williams H.E., Bergstrom C.T., Zhou A.Y. Model-driven mitigation measures for reopening schools during the COVID-19 pandemic. medRxiv. 2021 doi: 10.1101/2021.01.22.21250282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bilinski, A., Ciaranello, A., Fitzpatrick, M.C., Giardina, J., Shah, M., Salomon, J.A., and Kendall, E.A. SARS-CoV-2 testing strategies to contain school-associated transmission: model-based analysis of impact and cost of diagnostic testing, screening, and surveillance. medRxiv, doi: 10.1101/2021.05.12.21257131
- 43.CDC . 2020. Options to reduce quarantine for contacts of persons with SARS-CoV-2.https://www.cdc.gov/coronavirus/2019-ncov/more/scientific-brief-options-to-reduce-quarantine.html [PubMed] [Google Scholar]
- 44.Massachusetts Department of Education . 2021. Coronavirus/COVID: positive COVID-19 cases in schools.https://www.doe.mass.edu/covid19/positive-cases/ [Google Scholar]
- 45.Faherty L.J., Master B.K., Steiner E.D., Kaufman J.H., Predmore Z., Stelitano L., Leschitz J.T., Phillips B., Schwartz H.L., Wolfe R., RAND Corporation . 2021. COVID-19 testing in K–12 schools: insights from early adopters.https://www.rand.org/pubs/research_reports/RRA1103-1.html [Google Scholar]
- 46.Hoeg T.B., Gandhi M., Brown L. 2021. Perspective: widespread coronavirus surveillance testing at schools is a bad idea. Washington Post.https://www.washingtonpost.com/outlook/2021/04/19/schools-covid-testing-cost/ [Google Scholar]
- 47.CDC . 2021. COVID-19: interim public health recommendations for fully vaccinated people.https://www.cdc.gov/coronavirus/2019-ncov/vaccines/fully-vaccinated-guidance.html [Google Scholar]
- 48.CDC . 2021. Guidance for COVID-19 prevention in K-12 schools.https://www.cdc.gov/coronavirus/2019-ncov/community/schools-childcare/k-12-guidance.html [Google Scholar]
- 49.Pollock N.R., Berlin D., Smole S.C., Madoff L.C., Brown C., Henderson K., Larsen E., Hay J., Gabriel S., Gawande A.A., Lennon N.J. Implementation of SARS-CoV2 screening in K-12 schools using in-school pooled molecular testing and deconvolution by rapid antigen test. J. Clin. Microbiol. 2021;59:e0112321. doi: 10.1128/JCM.01123-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ciaranello A., Goehringer C., Nelson S.B., Ruark L.J., Pollock N.R. Lessons learned from implementation of SARS-CoV-2 screening in K-12 public schools in Massachusetts. Open Forum Infect. Dis. 2021;8:ofab287. doi: 10.1093/ofid/ofab287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.The Rockefeller Foundation . 2021. Taking back control: a resetting of Americas response to Covid 19.https://www.rockefellerfoundation.org/wp-content/uploads/2020/12/Taking-Back-Control-a-Resetting-of-Americas-Response-to-Covid-19.pdf [Google Scholar]
- 52.CDC . 2021. COVID data tracker.https://covid.cdc.gov/covid-data-tracker [Google Scholar]
- 53.Massachusetts Department of Education . 2021. Frequently Asked Questions, Week of May 17, 2021.https://www.doe.mass.edu/covid19/faq/2021-0517faq-installment.docx [Google Scholar]
- 54.COVID-19 Educational Testing . 2021. Everything you need to know about implementing COVID-19 pooled testing in your school.https://covidedtesting.com [Google Scholar]
- 55.Safer Teachers, Safer Students Collaborative . 2021. COVID-19 testing guidance for school committees: information and best practices for the efficient and effective implementation of COVID-19 testing in schools.https://ma-k12testingcollaborative.org/content/COVID-19%20Testing%20Guidance%20for%20School%20Committees%202.9.21.pdf [Google Scholar]
- 56.Open and Safe Schools . 2021. Open & Safe Schools.https://www.openandsafeschools.org [Google Scholar]
- 57.US Census Bureau . 2021. Census.gov.https://www.census.gov/en.html [Google Scholar]
- 58.Massachusetts Department of Education . 2020. Protocols for responding to COVID-19 scenarios in school, on the bus, or in community settings.https://www.doe.mass.edu/covid19/on-desktop/protocols/ [Google Scholar]
- 59.CDC . 2021. COVID-19: operational strategy for K-12 schools through phased mitigation.https://www.cdc.gov/coronavirus/2019-ncov/community/schools-childcare/operation-strategy.html [Google Scholar]
- 60.Paltiel A.D., Zheng A., Walensky R.P. Assessment of SARS-CoV-2 screening strategies to permit the safe reopening of college campuses in the United States. JAMA Netw. Open. 2020;3:e2016818. doi: 10.1001/jamanetworkopen.2020.16818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Mendoza R.P., Bi C., Cheng H.-T., Gabutan E., Pagaspas G.J., Khan N., Hoxie H., Hanna S., Holmes K., Gao N., et al. Implementation of a pooled surveillance testing program for asymptomatic SARS-CoV-2 infections in K-12 schools and universities. EClinicalMedicine. 2021;38:101028. doi: 10.1016/j.eclinm.2021.101028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Mutesa L., Ndishimye P., Butera Y., Souopgui J., Uwineza A., Rutayisire R., Ndoricimpaye E.L., Musoni E., Rujeni N., Nyatanyi T., et al. A pooled testing strategy for identifying SARS-CoV-2 at low prevalence. Nature. 2021;589:276–280. doi: 10.1038/s41586-020-2885-5. [DOI] [PubMed] [Google Scholar]
- 63.MA Department of Public Health . 2021. COVID-19 isolation and quarantine information. Mass.gov.https://www.mass.gov/info-details/covid-19-isolation-and-quarantine-information [Google Scholar]
- 64.Safer Teachers, Safer Students Collaborative . 2021. Safer teachers, safer students: back-to-school testing program summary.https://d0480129-a4ad-4b84-ac3a-932753c3acba.filesusr.com/ugd/a2eeb8_5882b833ad6d4168a7316ff70ac5a25b.pdf [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data reported in this paper will be shared by the lead contact upon request. This paper does not report original code. Any additional information required to reanalyze the data reported in this paper is available from the lead contact upon request.