Abstract
Objective
Reliable airway patency diagnosis in fetal tracheolaryngeal obstruction is crucial to select and plan ex utero intrapartum treatment (EXIT) surgery. We compared the clinical utility of magnetic resonance imaging (MRI) super-resolution reconstruction (SRR) of the trachea, which can mitigate unpredictable fetal motion effects, with standard 2-dimensional (2D) MRI for airway patency diagnosis and assessment of fetal neck mass anatomy.
Study Design
A single-center case series of 7 consecutive singleton pregnancies with complex upper airway obstruction (2013-2019).
Setting
A tertiary fetal medicine unit performing EXIT surgery.
Methods
MRI SRR of the trachea was performed involving rigid motion correction of acquired 2D MRI slices combined with robust outlier detection to reconstruct an isotropic high-resolution volume. SRR, 2D MRI, and paired data were blindly assessed by 3 radiologists in 3 experimental rounds.
Results
Airway patency was correctly diagnosed in 4 of 7 cases (57%) with 2D MRI as compared with 2 of 7 cases (29%) with SRR alone or paired 2D MRI and SRR. Radiologists were more confident (P = .026) in airway patency diagnosis when using 2D MRI than SRR. Anatomic clarity was higher with SRR (P = .027) or paired data (P = .041) in comparison with 2D MRI alone. Radiologists detected further anatomic details by using paired images versus 2D MRI alone (P < .001). Cognitive load, as assessed by the NASA Task Load Index, was increased with paired or SRR data in comparison with 2D MRI.
Conclusion
The addition of SRR to 2D MRI does not increase fetal airway patency diagnostic accuracy but does provide improved anatomic information, which may benefit surgical planning of EXIT procedures.
Keywords: fetal neck mass, CHAOS, magnetic resonance imaging, super-resolution reconstruction, trachea, EXIT
Fetal tracheolaryngeal obstruction is a life-threatening condition associated with substantial mortality of 80% to 100% if unrecognized before delivery. 1 Fetal airway compromise can occur due to extrinsic causes, such as complex neck masses, and intrinsic factors, such as congenital high airway obstruction (CHAOS). 1 A patent airway is necessary to complete the transition from fetal to neonatal life, but ex utero intrapartum treatment (EXIT) can be performed to treat or bypass the structural defect at birth. This modification of a caesarean section temporarily delivers only the fetal head through the maternal uterine incision while maintaining fetal oxygenation via placental circulation. This provides a crucial time window allowing the fetal airway to be secured by endotracheal intubation or tracheostomy.1,2 EXIT procedures have a significant rate of maternal complications, which includes hemorrhage due to deep maternal anesthesia for uterine relaxation and fetal risks such as hypoxic brain damage or death if the airway is not secured in a timely manner.3,4 Appropriate case selection and surgical planning are pivotal for optimizing outcome and depend on comprehensive preoperative imaging. 3 Ultrasound is the initial imaging method of choice due to its low cost and real-time capability. 5 However, the fetal airway is not always easily seen due to suboptimal fetal position.3,6-8 Therefore, magnetic resonance imaging (MRI) is often used in addition as it provides superior anatomic soft tissue visualization and definition due to multiplanar imaging with a larger field of view.3,4,6,9,10 MRI, however, is compromised by the effects of fast unpredictable fetal motion, which affects imaging quality and geometric integrity. 11 Some fetal magnetic resonance advances, such as ultrafast acquisition of thick 2-dimensional (2D) slices while maintaining a high signal-noise ratio, are still not enough to mitigate these challenges.6,11-14 Super-resolution reconstruction (SRR) is an example of postacquisition image processing based on rigid motion correction of 2D slices combined with robust outlier detection to reconstruct an isotropic high-resolution volume. It has been found to enhance anatomic evaluation of fetal brain structural anomalies.13-17 We investigated the clinical utility of SRR of the fetal trachea as compared with standard 2D MRI for airway patency diagnosis and anatomic assessment of fetal neck masses.
Methods
Participants
This study is based on 7 consecutive singleton pregnancies with fetal tracheal-laryngeal obstruction with antenatal MRI that were managed in the fetal surgical EXIT program at University College London Hospitals (2013-2019). All cases initially had ultrasonography, which identified fetuses with large neck masses (n = 6) or CHAOS syndrome (n = 1), with referral to our tertiary fetal medicine unit for further assessment and management. All MRI data were analyzed under the study entitled “Guided Instrumentation for Fetal Therapy and Surgery (GIFT-Surg): Fetal MRI to Improve Prenatal Diagnosis and Therapy for Fetal Abnormality” (Hampstead Research Ethics Committee, 15/LO/1488). Women provided written informed consent for fetal MRI research. All images were transferred with Caldicott Guardian approval from University College London Hospitals to collaborators at partner academic institutions (University College London, King’s College London, and Katholieke Universiteit Leuven) via the secure GIFT-Cloud platform, which ensures complete anonymization through XNAT technology. 18 Case outcome data were collected from neonatal records, including laryngoscopy at EXIT, postnatal magnetic resonance and x-ray imaging, and postmortem examination where performed.
Technical and Experiment Information
All MRI examinations were performed on a 1.5-T magnet (MAGNETOM Avanto; Siemens Healthcare). Women were placed in the supine or left lateral decubitus position. The gravid uterus was imaged in at least 3 orthogonal planes (axial, coronal, and sagittal) relative to the fetal body. The protocol consisted of T2-weighted fast acquisition spin echo sequences, typically HASTE (half-Fourier acquisition single-shot turbo spin echo), or gradient echo sequences, such as T1-weighted spoiled FLASH (fast low-angle shot) or T2-weighted TRUFI (true fast imaging with steady state–free precession). For HASTE sequences, the following parameters were applied: echo time (68-112 ms), repetition time (887-1460 ms), flip angle (90°), refocusing flip angle (80°-107°), slice thickness (2-4 mm), slice gap (0%-10% of slice thickness), field of view (260-360 mm × 195-315 mm), and voxel size (1-1.4 mm × 1-1.4 mm). For TRUFI the following parameters were applied: echo time (2.66 ms), repetition time (5.31 ms), flip angle (62°), slice thickness (4 mm), no gap, field of view (320 mm × 320 mm), and voxel size (1.4 mm × 1.4 mm). All patients were scanned in a normal specific absorption rate mode. Total acquisition time did not exceed 40 minutes.
A novel SRR algorithm was then applied to reconstruct an isotropic 3-dimensional volume of the trachea with native 2D MRI stacks. 15 At least 3 orthogonal T2-weighted image stacks, acquired in at least 3 orientations, were used for the algorithm in each case. A region of interest in 1 stack around the trachea was manually segmented and automatically propagated to the remaining stacks with rigid volume-to-volume registration. Afterward, robust SRR involving iterative motion correction and volumetric reconstruction steps was deployed, guided by the respective trachea masks. Iterative 3-dimensional reconstructions were estimated from motion-corrected slices through outlier-robust SRR methods to account for image artifacts as part of the motion correction step. Each SRR generation did not exceed 15 minutes.
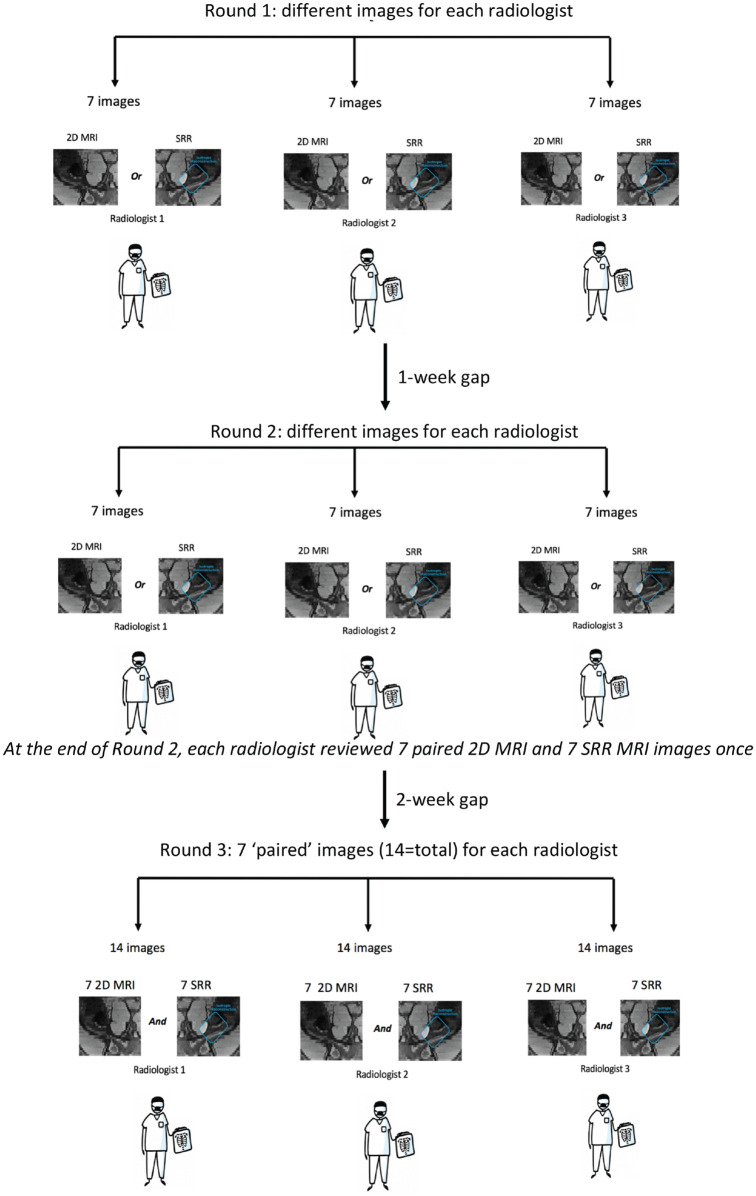
Experiments were separated into 3 rounds. The first 2 rounds involved a selection of individual SRR and 2D MRI scans, which were assessed by 3 senior pediatric radiologists (M.A., P.D.H., and T.G.) with specialist fetal MRI expertise who were blinded to case outcomes. The selection was randomly assigned such that each radiologist had a different set of independent SRR and 2D MRI scans in each of the first 2 rounds. Each radiologist read all the images by the end of the second round. In the third round, the radiologists each examined all the 2D MRI scans paired with their corresponding SRR images alongside. The first 2 rounds were separated by 1 week; 2 weeks after this, the third round was performed ( Figure 1 ).
Figure 1.
Flowchart of experimental design. 2D, 2-dimensional; MRI, magnetic resonance imaging; SRR, super-resolution reconstruction.
In every round, the assessment contained a set of clinical questions that had 3 themes: diagnosis and confidence of airway patency, anatomic clarity, and characteristics of mass and extent of head and neck involvement (Supplemental Table S1, available online). The time taken to answer these questions was measured. Airway patency was scored on a confidence scale of 0 to 5, ranging from no confidence at all to completely confident. Anatomic clarity was subjectively scored 0 to 4, where 0 = structure was not seen, 1 = poor depiction, 2 = suboptimal visualization, 3 = clear visualization of structure but reduced tissue contrast (image-based diagnosis feasible), and 4 = excellent depiction (optimal for diagnostic purposes).
The presence of various anatomic markers was evaluated, including description of the mass causing displacement, compression, and encasement of the trachea. Extent of neck, facial involvement, and intrathoracic extension was also rated. Further mass characteristics were assessed, such as cystic, septated, solid, and vascular. Radiologists were asked to evaluate SRR quality, which was dependent on the amount of fetal motion artifact remaining where 0 = substantial artifact/blur, 1 = little artifact/blur, and 2 = no artifact/blur. 2D MRI quality was not quantitatively examined, as there was no predefined marking that is comparable to our quality scoring for SRR. Radiologists additionally provided a subjective preference in the third round, to indicate whether 2D MRI, SRR images, both, or neither was more superior in answering the clinical questions. The NASA Task Load Index (TLX) 19 was performed at the end of each round to quantify user cognitive load of evaluating 2D MRI, SRR images, and those 2 modalities combined. The TLX is a subjective multidimensional tool that measures observed workload to assess a task. This has been used before in the context of new medical technology.20-23 It scores different task aspects on a graded scale from 0 to 20, including effort, frustration, and performance (Supplemental Table S2, available online).
Statistics
Statistical analysis was performed with Excel (Microsoft 365) and SPSS Statistics for Mac version 27 (IBM Corp). Kruskal-Wallis 1-way analysis of variance with correction for multiple comparisons was used to assess data among all imaging modalities. Results are documented as test statistic (degree of freedom) and the P value. For illustration of differences among modalities, a Bland-Altmann analysis was used, with the mean difference as a bias measure and the 2.5th and 97.5th percentiles as the 95% limits of agreement. Statistical significance was set <5%.
Results
Cases
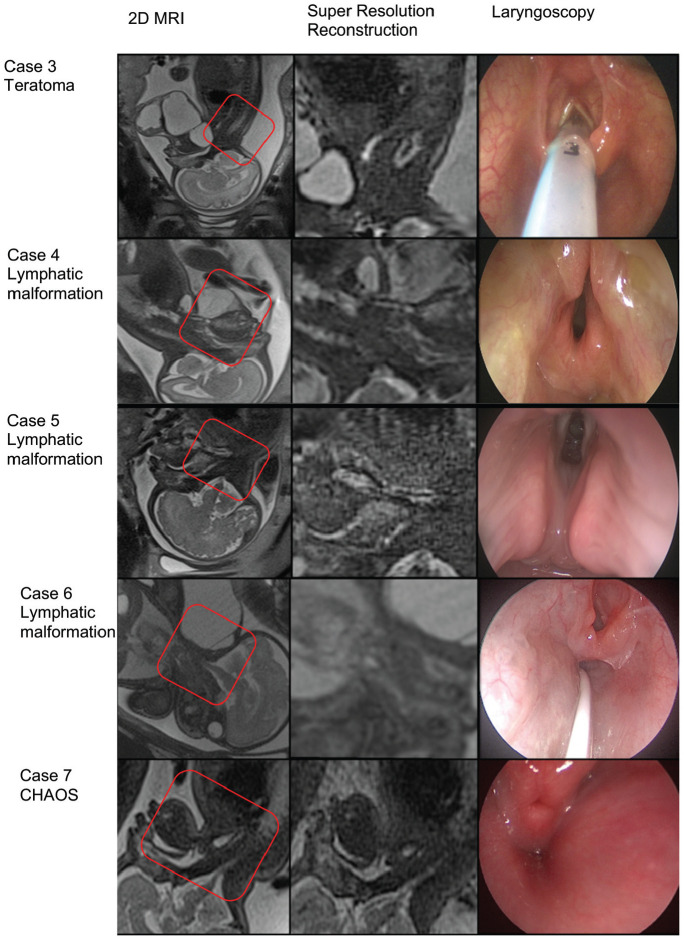
There were 7 cases of tracheal-laryngeal obstruction: 4 lymphatic malformations, 2 teratomas, and 1 CHAOS syndrome. All cases were diagnosed by ultrasound, with an average gestational age at MRI of 31 weeks + 4 days (SD, 1 + 1; range, 29 + 1 to 37 + 6). Average gestational age at delivery was 36 weeks + 3 days (SD, 2 + 2; range, 33 + 1 to 38 + 6). One case was not suitable for an EXIT procedure due to severe lung hypoplasia. The mother had an emergency caesarean section due to a pathologic cardiotocograph in her local hospital. Securing of the airway was impossible due to tracheal obstruction, and although a tracheostomy was performed, there was early neonatal death secondary to pulmonary hypoplasia. Six cases had an EXIT procedure, all of which had functional airways created by means of either a tracheostomy or endotracheal intubation. In 1 case there was an early neonatal death due to significant hemorrhage into a teratoma. There was additionally a left-sided pneumothorax that, despite airway security, resulted in poor response to ventilation causing grade 3 hypoxic ischemic encephalopathy. The fetus with CHAOS syndrome had a tracheostomy at EXIT, with a diagnosis of laryngeal atresia fully obstructing the airway at the subglottis. Further details of the cases are illustrated in Figure 2 and Table 1 .
Figure 2.
Example of 5 cases of tracheal-laryngeal obstruction. The box indicates the area on the 2-dimensional (2D) image (first column) that was reconstructed (middle column). CHAOS, congenital high airway obstruction; MRI, magnetic resonance imaging.
Table 1.
Characteristics and Outcomes of Fetuses.
| Characteristic | Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | Case 6 | Case 7 |
|---|---|---|---|---|---|---|---|
| Pregnancy | |||||||
| GA at MRI, wk + d | 29 + 6 | 29 + 4 | 31 + 1 | 30 + 5 | 37 + 2 | 32 + 3 | 31 + 6 |
| GA at delivery, wk + d | 37 + 5 | 34 + 2 | 36 + 6 | 37 + 3 | 38 + 2 | 34 + 1 | 33 + 4 |
| Tumor | |||||||
| Final diagnosis | Lymphatic malformation | Teratoma | Teratoma | Lymphatic malformation | Lymphatic malformation | Lymphatic Malformation | CHAOS |
| Lesion/obstruction size on MRI, mm | 55 × 35 | 145 × 110 | 45 × 36 | 83 × 42 × 46 | 80 × 60 × 76 | 88 × 122 × 87 | 7 × 5 |
| Delivery a | |||||||
| EXIT | No | Yes | Yes | Yes | Yes | Yes | Yes |
| Airway patent | No | No | Yes | Yes | Yes | Yes | No |
| Tracheostomy | No | Yes b | No | No | No | No | Yes |
| ET tube | No | No | Yes | Yes | Yes | Yes | No |
| Successful intubation | No | Yes | Yes | Yes | Yes | Yes | Yes |
| Outcome | Emergency caesarean section, cardiac arrest and neonatal death | Neonatal death due to significant hemorrhage into teratoma. Pulmonary hypoplasia, pneumothorax, and HIE grade 3 | Alive | Alive | Alive | Alive | Alive |
Abbreviations: CHAOS, congenital high airway obstruction; ET, endotracheal; EXIT, ex utero intrapartum treatment; GA, gestational age; HIE, hypoxic ischemic encephalopathy; MRI, magnetic resonance imaging.
Dark gray, no; light gray, yes.
ET tube placed directly into the trachea.
Super-resolution Reconstruction
An average of 8 stacks (SD, 2.5; range, 3-11) in at least 3 anatomic orientations were used for SRR. Average slice rejection was 1 (SD, 4; range, 0-15), indicating the degree of fetal motion in the acquired data. Of 7 SRR images, 3 (43%) scored >1 quality. Fewer than 5 stacks are typically insufficient for obtaining good SRR quality. 15 This is shown for cases 4 and 6 ( Table 2 ).
Table 2.
SRR Quality and Number of Stacks Used per Case.
| Case | Sequence for SRR | Slice rejection, mean ± SD (range) | No. of stacks for SRR | SRR quality a |
|---|---|---|---|---|
| 1 | T2 HASTE | 1 ± 1 (0-2) | 5 | 1.5 |
| 2 | T2 HASTE | 3 ± 4 (0-10) | 8 | 0.7 |
| 3 | T2 HASTE | 1 ± 1 (0-3) | 8 | 1.5 |
| 4 | T2 HASTE | 4 ± 3 (0-6) | 4 | 0 b |
| 5 | T2 HASTE | 3 ± 2 (0-7) | 9 | 0.3 |
| 6 | TRUFI | 0 ± 1 (0-1) | 3 | 0 b |
| 7 | T2 HASTE | 7 ± 4 (2-15) | 11 | 1.5 |
Abbreviations: SRR, super-resolution reconstruction; T2 HASTE, T2 half-Fourier acquisition single-shot turbo spin echo; TRUFI, true fast imaging with steady state–free precession.
Average obtained across 3 radiologists whereby 0 = lots of artifact/blur, 1 = little artifact/blur, and 2 = no artifact/blur.
Fewer than 5 stacks are typically insufficient for obtaining good SRR quality.
Diagnosis and Confidence of Airway Patency
With 2D MRI alone, airway patency was correctly diagnosed by each radiologist in 4 of 7 cases (57%). When provided with SRR images alone, however, radiologists were less often correct in their diagnosis (2 of 7 cases, 29%). The combination of 2D MRI with SRR imaging did not improve diagnostic accuracy above 2D MRI scans alone (2 of 7 cases, 29%). In 2 of 7 cases where 2D MRI yielded the correct diagnosis, the addition of SRR made some radiologists change their minds to an incorrect diagnosis ( Figure 3 ).
Figure 3.
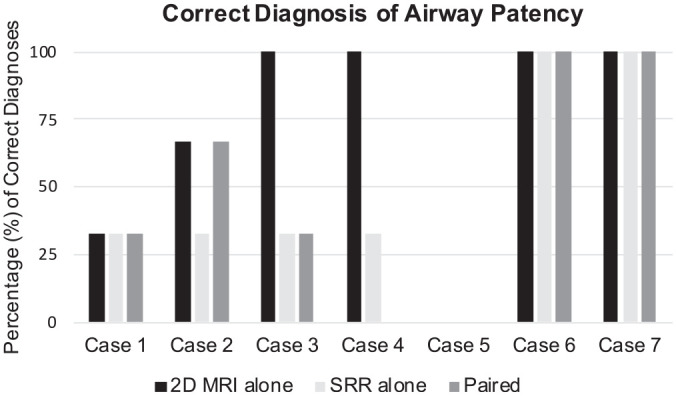
All 7 cases are on x-axis. Correct diagnosis of airway patency is expressed as percentage on y-axis. No radiologist correctly diagnosed outcome of airway patency for case 5. 2D, 2-dimensional; MRI, magnetic resonance imaging; SRR, super-resolution reconstruction.
Confidence Regarding Airway Patency
Radiologists were more confident (test statistic [5] = 12.737, P = .026) in assessing airway patency with 2D MRI alone (mean, 3.76; 95% CI, 3.22-4.30) in comparison with SRR images alone (2.81; 95% CI, 2.10-3.52; Figure 4 ). There was no significant improvement in airway patency confidence between paired data and 2D MRI and SRR data alone (Supplemental Figure S1, available online).
Figure 4.
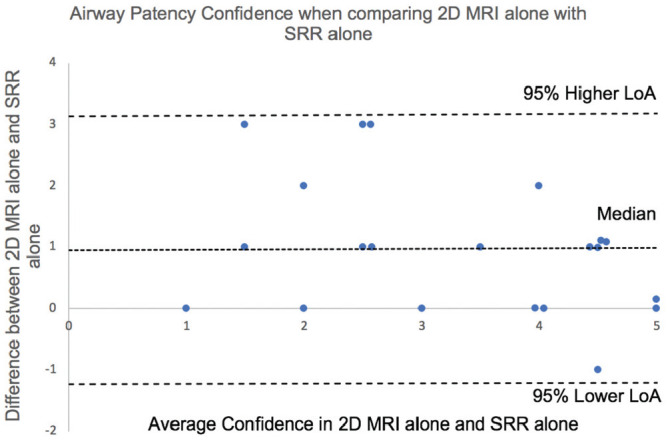
Bland-Altman plot illustrating differences in airway patency confidence of 3 radiologists using 2D MRI alone vs SRR imaging alone, whereby 0 on the y axis = equal confidence. 2D, 2-dimensional; LOA, limits of agreement; MRI, magnetic resonance imaging; SRR, super-resolution reconstruction.
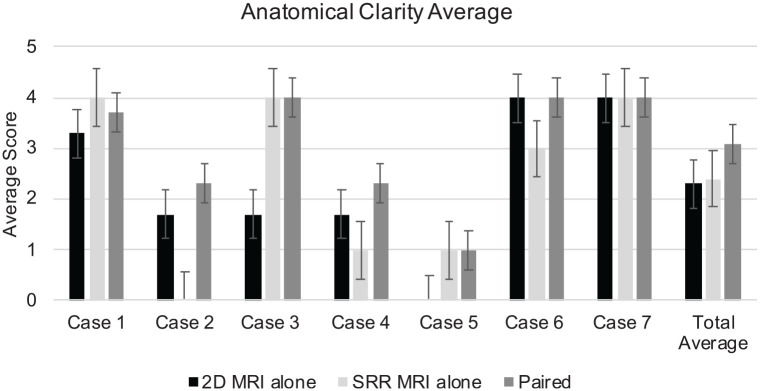
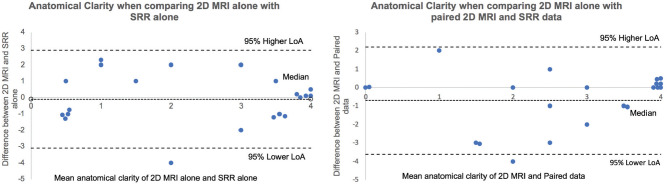
Anatomic Clarity
Subjective anatomic clarity was higher with paired data (mean, 3.05; 95% CI, 2.4-3.7; test statistic [3] = 8.251, P = .041) or SRR images alone (2.43; 95% CI, 1.67-3.18; test statistic [4] = 10.995, P = .027) in comparison with 2D MRI alone (2.33; 95% CI, 1.61-3.06; Figures 5 and 6 ).
Figure 5.
Anatomic clarity average of the 3 radiologists (y-axis). This is illustrated for each of the 7 cases of airway obstruction and the total average (x-axis). Values are presented as mean (95% CI). 2D, 2-dimensional; MRI, magnetic resonance imaging; SRR, super-resolution reconstruction.
Figure 6.
Bland-Altman plots illustrating anatomic clarity average differences with 2D MRI alone vs SRR alone (left) and 2D MRI vs paired imaging (right). 0 on the y-axis = equal confidence. 2D, 2-dimensional; LOA, limits of agreement; MRI, magnetic resonance imaging; SRR, super-resolution reconstruction.
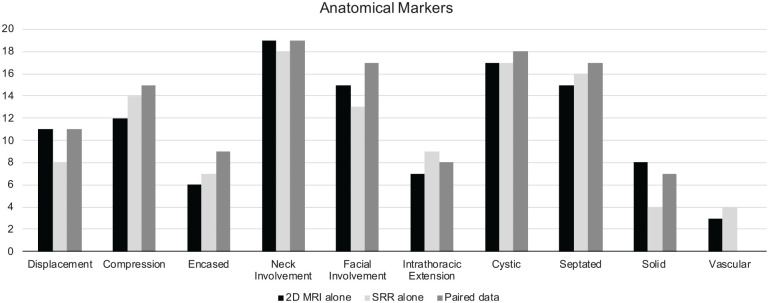
Characteristics of Mass and Extent of Head and Neck Involvement
Anatomic findings were significantly more likely to be detected with paired data (mean, 12.1; 95% CI, 7.71-16.5) than with 2D MRI alone (11.3; 95% CI, 7.56-15.04; test statistic [3] = 51.907, P < .001; Figure 7 ).
Figure 7.
Presence of various anatomic findings assessed by 3 radiologists using 2D MRI alone, SRR imaging alone, or in combination (paired data). 2D, 2-dimensional; MRI, magnetic resonance imaging; SRR, super-resolution reconstruction.
Time Taken to Answer Clinical Questions and Subjective Preference
The average time taken by radiologists to answer the clinical questions was not different between 2D MRI alone (mean, 306.71; 95% CI, 208.21-405.22) and paired data (314.43; 95% CI, 224.35-404.51). On average, 1.5% (4/273) of all clinical questions could not be answered with 2D MRI scans alone and 6.23% (17/273) SRR images alone. In contrast, all clinical questions could be answered by all radiologists using paired data. Additionally, the radiologists rated their preference toward using paired imaging (57% = 12/21) versus SRR (0%) or 2D MRI (38% = 8/21) images alone.
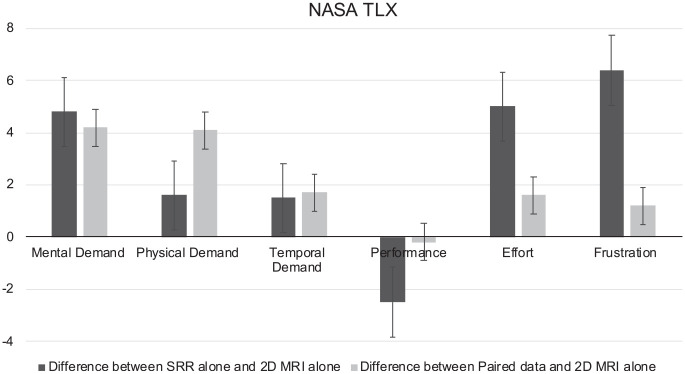
NASA TLX
The NASA TLX was used to determine radiologist cognitive load in answering the clinical questions. Mental, physical, temporal demand, effort, and frustration levels were all higher with SRR images alone or paired imaging in comparison with 2D MRI alone. Performance was lower with paired images and SRR data alone than with 2D MRI. This was improved by using paired imaging over SRR data alone. Physical demand was significantly increased with paired data (mean, 4.1; 95% CI, 2-6.2) than with SRR images alone (1.61; 95% CI, 0.23-3; test statistic [6] = 16.297, P = .012; Figure 8 ).
Figure 8.
NASA TLX indicating difference between SRR alone and 2D MRI alone and between paired data and 2D MRI alone (P = .012). Values are presented as mean (95% CI). 2D, 2-dimensional; MRI, magnetic resonance imaging; SRR, super-resolution reconstruction; TLX, Task Load Index.
Discussion
Main Findings
We compared the clinical utility of a novel SRR of the trachea with standard 2D MRI for diagnosis of airway patency and anatomic assessment of fetal neck masses. We found that airway patency was more likely to be correctly diagnosed with 2D MRI alone in comparison with SRR alone or paired data sets. However, anatomic clarity was significantly better with paired or SRR images alone than with 2D MRI scans alone. As SRR quality improved, airway patency confidence increased, as did anatomic clarity (Supplemental Figures S2 and S3, available online). Anatomic markers and mass characteristics were additionally detected significantly more with paired data in comparison with 2D MRI alone, with no increase in time taken to make a clinical assessment.
Interpretation
For anatomic marker analysis in the presence of fetal airway abnormalities, use of 2D MRI and SRR imaging in combination appears to provide optimum anatomic clarity while taking a similar amount of time as with 2D MRI alone. Although cognitive load is increased when SRR imaging is added, this may be a worthwhile compromise when considering the more comprehensive anatomic assessment of the fetal neck structures required for surgical planning of EXIT procedures. Reduced performance of paired imaging in terms of airway patency and confidence of diagnosis in comparison with 2D MRI alone may be explained by a natural learning curve that radiologists encounter when interpreting SRR images, given the different texture and visualization against the original MRI. Our study suggests the clinical potential of volumetric reconstruction in aiding anatomic clarity where original stacks are of good image quality. It can provide exquisite definition of fetal neck anatomy and potential involvement of the airway in the neck mass, which may facilitate surgical planning and improve perinatal outcome. A high-quality SRR crucially depends on precision of the established spatial correspondences among slices with at least 3 stacks in 3 orientations required for sufficient anatomic detail. 15 Nevertheless, the underlying rigid motion reconstruction model limits the ability to compensate for complex motion of tissue surrounding the trachea. This highlights the importance of optimizing 2D MRI data acquisition, as the quality of the reconstruction is reliant on this.
Case selection for an EXIT procedure is important given the significant maternal and fetal risks that exist with surgery.3,4 Choosing to perform EXIT should be balanced against the likelihood of fetal airway obstruction and poor neonatal prognosis. Planning an EXIT procedure is complex as it requires collective efforts of multiple disciplines, such as fetal medicine, anaesthetics, neonatology, pediatric anesthetics, otolaryngologic surgeons, and radiologists to manage the surgery and neonatal resusitation.5,9 Surgical planning is dependent on imaging findings, such as the level of obstruction in CHAOS, extent of the fetal neck mass, degree of tracheal compression, and displacement of the tracheoesophageal complex. 9 Our case series suggests that SRR may be useful alongside 2D MRI in 2 types of extrinsic tracheal compression, lymphangiomas and teratomas, and 1 intrinsic anomaly, CHAOS. Lymphangiomas are congenital malformations of the lymphatic system and may be cystic or solid with vascular composition, which disrupts tissue planes and can compress or encase the fetal airway. 6 Teratomas are cystic or solid and may contain calcifications.6,9 These tumors tend to be large, displacing essential structures such as the trachea and esophagus, hence compromising the fetal airway. 5 MRI use in neck tumors is advantageous due to its ability to provide superior soft tissue contrast, a larger field of view, and multiplanar imaging. 8 This is useful in delineating tissue characteristic differences and providing information on tracheal compression or distortion.6,9 CHAOS is a rare form of tracheal or laryngeal obstruction due to atresia or stenosis. MRI has been used to localize the level of obstruction in CHAOS, aiding determination of the likelihood of EXIT procedure success, as low tracheal obstruction has been associated with failed access of the fetal airway. 1 In our CHAOS case, 2D MRI and SRR helped define that the posterior communication of the obstruction was at the laryngeal level—detail that was not available on ultrasound examination.
Strengths and Limitations
Our SRR algorithm is limited, as a sufficiently small mask around the trachea is chosen to assume the approximate rigid motion in that area. This limits the region of interest, which might have affected the radiologists’ ability to identify its spatial location and assessment within the larger anatomic context. Super-resolved images may be improved in the future with a wider FOV or whole body SRR. 24 The small number of patients in our case series may have affected comparison between SRR and 2D MRI. However, complex neck masses and CHAOS are rare, and any single tertiary institution’s experience is likely to be small. There is a possibility of bias in the third round of interpretation by radiologists. Although it is separated by a 2-week interval, it is plausible that providers had image recall, which may have influenced their speed and preference for combined SRR and 2D MRI. It is additionally important to note that the involved radiologists had no prior background in interpretation of SRR MRI volumes of the fetal neck and airway. The inevitable learning curve associated with use of this novel technology may therefore have an impact on study results.
Conclusion
For fetal neck mass assessment, the addition of SRR to 2D MRI does not increase fetal airway patency diagnostic accuracy but does provide improved anatomic information. This may improve case selection for EXIT procedures and enhance surgical planning by ensuring that appropriate clinical teams and equipment are available. Additional validation with a larger data set is necessary to support the reconstruction fidelity, and SRR images should be considered supportive information and not a replacement of the original 2D MRI stacks.
Authorship Contributions
Nada Mufti, designed the study, analyzed the data, wrote the first draft, and corrected the final version of the manuscript; Michael Ebner, developed the super-resolution reconstruction algorithm and assisted in the experimental design; Premal Patel, refined the study design and randomization of data for experiments; Michael Aertsen, trained radiologist who carried out all 3 experimental rounds and helped in refining the study design and determining the field of view prior to commencement of the experiments; Trevor Gaunt, trained radiologist who carried out all 3 experimental rounds; Paul D. Humphries, trained radiologist who carried out all 3 experimental rounds; Fonteini Emmananouella Bredaki, assisted in the clinical care and data collection; Richard Hewitt, provided advice on otolaryngologic surgical content and laryngoscopy images; Colin Butler, provided advice on otolaryngologic surgical content and laryngoscopy images; Magdalena Sokolska, assisted in guidance and acquisition of the magnetic resonance imaging; Giles S. Kendall, provided advice on neonatal management content; David Atkinson, assisted in guidance and acquisition of the magnetic resonance imaging; Tom Vercauteren, supervised Michael Ebner; Sebastien Ourselin, supported and supervised this work since conception; Pranav P. Pandya, supported and supervised this work since conception; Jan Deprest, supported and supervised this work since conception; Andrew Melbourne, supported and supervised this work since conception; Anna L. David, supported and supervised this work since conception.
Disclosures
Competing interests: None.
Sponsorships: None.
Funding source: This work was supported by the Guided Instrumentation of Fetal Therapy and Surgery project, funded by the Wellcome Trust (203148/Z/16/Z, 203145Z/16/Z, WT101957) and Engineering and Physical Sciences Research Council (NS/A000049/1, NS/A000050/1, NS/A000027/1, EP/L016478/1). Sebastien Ourselin is the principal investigator on this grant, and Anna L. David, Jan Deprest, Tom Vercauteren, and Andrew Melbourne are coinvestigators. Nada Mufti is funded with support of the Wellcome/EPSRC Centre for Interventional and Surgical Sciences (203145Z/16/Z). Anna L. David is supported by the University College London Hospitals Biomedical Research Centre, National Institute for Health Research.
Supplemental Material
Supplemental material, sj-pdf-1-opn-10.1177_2473974X211055372 for Super-resolution Reconstruction MRI Application in Fetal Neck Masses and Congenital High Airway Obstruction Syndrome by Nada Mufti, Michael Ebner, Premal Patel, Michael Aertsen, Trevor Gaunt, Paul D. Humphries, Fonteini Emmananouella Bredaki, Richard Hewitt, Colin Butler, Magdalena Sokolska, Giles S. Kendall, David Atkinson, Tom Vercauteren, Sebastien Ourselin, Pranav P. Pandya, Jan Deprest, Andrew Melbourne and Anna L. David in OTO Open: The Official Open Access Journal of the American Academy of Otolaryngology-Head and Neck Surgery Foundation
Acknowledgments
We thank all the patients who participated in this research.
Footnotes
ORCID iDs: Nada Mufti  https://orcid.org/0000-0001-9839-8085
https://orcid.org/0000-0001-9839-8085
David Atkinson  https://orcid.org/0000-0003-1124-6666
https://orcid.org/0000-0003-1124-6666
Supplemental Material: Additional supporting information is available at http://journals.sagepub.com/doi/suppl/10.1177/2473974X18[article ID]
References
- 1. Courtier J, Poder L, Wang ZJ, Westphalen AC, Yeh BM, Coakley FV. Fetal tracheolaryngeal airway obstruction: prenatal evaluation by sonography and MRI. Pediatr Radiol. 2010;40(11):1800-1805. doi: 10.1007/s00247-010-1800-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Mychaliska GB, Bealer JF, Graf JL, Rosen MA, Adzick NS, Harrison MR. Operating on placental support: the ex utero intrapartum treatment procedure. J Pediatr Surg. 1997;32:227-231. [DOI] [PubMed] [Google Scholar]
- 3. Bulas D. Fetal magnetic resonance imaging as a complement to fetal ultrasonography. Ultrasound Q. 2007;23(1):3-22. [DOI] [PubMed] [Google Scholar]
- 4. Hubbard AM, Crombleholme TM, Adzick NS. Prenatal MRI evaluation of giant neck masses in preparation for the fetal exit procedure. Am J Perinatol. 1998;15:253-257. [DOI] [PubMed] [Google Scholar]
- 5. Werner H, Lopes dos Santos JR, Fontes R, et al. Virtual bronchoscopy for evaluating cervical tumors of the fetus. Ultrasound Obstet Gynecol. 2013;41(1):90-94. doi: 10.1002/uog.11162 [DOI] [PubMed] [Google Scholar]
- 6. Kathary N, Bulas DI, Newman KD, Schonberg RL. MRI Imaging of fetal neck masses with airway compromise: utility in delivery planning. Pediatr Radiol. 2001;31:727-731. [DOI] [PubMed] [Google Scholar]
- 7. Lazar DA, Olutoye OO, Moise KJ, Jr, et al. Ex-utero intrapartum treatment procedure for giant neck masses—fetal and maternal outcomes. J Pediatr Surg. 2011;46(5):817-822. doi: 10.1016/j.jpedsurg.2011.02.006 [DOI] [PubMed] [Google Scholar]
- 8. Ng TW, Xi Y, Schindel D, et al. Fetal head and neck masses: MRI prediction of significant morbidity. AJR Am J Roentgenol. 2019;212(1):215-221. doi: 10.2214/AJR.18.19753 [DOI] [PubMed] [Google Scholar]
- 9. Olutoye OO, Olutoye OA. EXIT procedure for fetal neck masses. Curr Opin Pediatr. 2012;24(3):386-393. doi: 10.1097/MOP.0b013e3283531b51 [DOI] [PubMed] [Google Scholar]
- 10. Stevens GH, Schoot BC, Smets MJW, et al. The ex utero intrapartum treatment (EXIT) procedure in fetal neck masses: a case report and review of the literature. Eur J Obstet Gynecol Reprod Biol. 2002;100:246-250. [DOI] [PubMed] [Google Scholar]
- 11. Gholipour A, Estroff JA, Barnewolt CE, et al. Fetal MRI: a technical update with educational aspirations. Concepts Magn Reson Part A Bridg Educ Res. 2014;43(6):237-266. doi: 10.1002/cmr.a [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Prayer D, Malinger G, Brugger PC, et al. ISUOG practice guidelines: performance of fetal magnetic resonance imaging. Ultrasound Obstet Gynecol. 2017;49(5):671-680. doi: 10.1002/uog.17412 [DOI] [PubMed] [Google Scholar]
- 13. Rousseau F, Glenn OA, Iordanova B, et al. Registration-based approach for reconstruction of high-resolution in utero fetal MR brain images. Acad Radiol. 2006;13(9):1072-1081. doi: 10.1016/j.acra.2006.05.003 [DOI] [PubMed] [Google Scholar]
- 14. Gholipour A, Estroff JA, Warfield SK. Robust super-resolution volume reconstruction from slice acquisitions: application to fetal brain MRI. IEEE Trans Med Imaging. 2010;29(10):1739-1758. doi: 10.1109/TMI.2010.2051680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ebner M, Wang G, Li W, et al. An automated framework for localization, segmentation and super-resolution reconstruction of fetal brain MRI. Neuroimage. 2020;206:116324. doi: 10.1016/j.neuroimage.2019.116324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ebner M, Patel PA, Atkinson D, et al. Super-resolution for upper abdominal MRI: acquisition and post-processing protocol optimization using brain MRI control data and expert reader validation. Magn Reson Med. 2019;82(5):1905-1919. doi: 10.1002/mrm.27852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kainz B, Steinberger M, Wein W, et al. Fast volume reconstruction from motion corrupted stacks of 2D slices. IEEE Trans Med Imaging. 2015;34(9):1901-1913. doi: 10.1109/TMI.2015.2415453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Doel T, Shakir DI, Pratt R, et al. GIFT-Cloud: a data sharing and collaboration platform for medical imaging research. Comput Methods Programs Biomed. 2017;139:181-190. doi: 10.1016/j.cmpb.2016.11.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Hart SG, Staveland LE. Development of NASA-TLX (task load index): results of empirical and theoretical research. Adv Psychol. 1988;52:139-183. doi: 10.1016/S0166-4115(08)62386-9 [DOI] [Google Scholar]
- 20. Yurko YY, Scerbo MW, Prabhu AS, Acker CE, Stefanidis D. Higher mental workload is associated with poorer laparoscopic performance as measured by the NASA-TLX tool. Simul Healthc. 2010;5(5):267-271. doi: 10.1097/SIH.0b013e3181e3f329 [DOI] [PubMed] [Google Scholar]
- 21. Ariza F, Kalra D, Potts HW. How do clinical information systems affect the cognitive demands of general practitioners? Usability study with a focus on cognitive workload. J Innov Health Inform. 2015;22(4):379-390. doi: 10.14236/jhi.v22i4.85 [DOI] [PubMed] [Google Scholar]
- 22. Bhandary S, Lipps J, Winfield SR, et al. NASA Task Load Index scale to evaluate the cognitive workload during cardiac anesthesia based simulation scenarios. Int J Anesthesiol Res. 2016;4(8):300-304. doi: 10.19070/2332-2780-1600063 [DOI] [Google Scholar]
- 23. McGrath H, Li P, Dorent R, et al. Manual segmentation versus semi-automated segmentation for quantifying vestibular schwannoma volume on MRI. Int J Comput Assist Radiol Surg. 2020;15(9):1445-1455. doi: 10.1007/s11548-020-02222-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Uus A, Zhang T, Jackson LH, et al. Deformable slice-to-volume registration for motion correction of fetal body and placenta MRI. IEEE Trans Med Imaging. 2020;39(9):2750-2759. doi: 10.1109/TMI.2020.2974844 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-opn-10.1177_2473974X211055372 for Super-resolution Reconstruction MRI Application in Fetal Neck Masses and Congenital High Airway Obstruction Syndrome by Nada Mufti, Michael Ebner, Premal Patel, Michael Aertsen, Trevor Gaunt, Paul D. Humphries, Fonteini Emmananouella Bredaki, Richard Hewitt, Colin Butler, Magdalena Sokolska, Giles S. Kendall, David Atkinson, Tom Vercauteren, Sebastien Ourselin, Pranav P. Pandya, Jan Deprest, Andrew Melbourne and Anna L. David in OTO Open: The Official Open Access Journal of the American Academy of Otolaryngology-Head and Neck Surgery Foundation