Abstract
Studies show decreased well-being during the COVID-19 pandemic, especially for healthcare providers from Asia. Less is known about the psychological responses of working during the pandemic on hospital-based registered nurses (RNs) in the United States (US). Therefore, the purpose of this paper is to report the well-being of U.S.-based hospital RNs working during the initial acute phase of COVID-19 and compare it with well-being among healthcare workers described in two global meta-analyses. We conducted a cross-sectional survey in May–June 2020 (N = 467). Well-being was measured using the following tools: Generalized Anxiety Disorder-7, Patient Health Questionnaire-2 for depressive symptoms, Impact of Events Scale-Revised for traumatic stress, and the Insomnia Severity Index. Compared with global rates from two meta-analyses, US-based RNs reported significantly more traumatic stress (54.6% vs. 11.4% and 21.5%; p < .001) and depressive symptoms (54.6% vs. 31.8% and 21.7%; p < .001). Rates of insomnia were also higher in U.S.-based RNs than in the meta-analysis that reported insomnia (32.4% vs 27.8%; p < .033). Rates of anxiety symptoms among US-based RNs did not differ from that reported in one meta-analysis (37.3% vs. 34.4%), while it was significantly higher in the other (37.3% vs. 22.1%; p < .001). Hospital-based RNs from the US exhibited over twice the rates of trauma and nearly double the rates of depressive symptoms than shown in reports from hospital workers globally during the acute phase of the COVID-19 pandemic. The lasting effects of this distress are unknown and warrant ongoing evaluation and solutions to better support emotional well-being and prevent burnout in the workplace.
Keywords: Nursing staff, Hospital, Stress, Psychological, Stress disorders, Traumatic, COVID-19
On March 11, 2020, the World Health Organization officially declared the outbreak of the novel coronavirus a global pandemic. Within days of the announcement, much of the world shut down their economies to only essential operations in an effort to reduce the threat of the SARS-CoV-2 virus. This rapidly spreading, highly contagious, and comparatively lethal coronavirus caused the now infamous disease known to the world as COVID-19. Emergence of COVID-19 dramatically increased workplace demands and stress among healthcare providers. These included extended work hours, inadequate staffing, and inadequate personal protective equipment (PPE) (Cohen & Rodgers, 2020; Emanuel et al., 2020; Livingston et al., 2020). According to Theorell (2020), p. 193), COVID-19 “is like a cruel experiment – a randomized trial for maximal worsening of the work environment.” Indeed, by June 2020, the International Council of Nurses (ICN) reported that more than 230,000 healthcare workers and more than 600 nurses had died from COVID-19. In October 2020 the ICN updated the number to 1500 (ICN, 2020).
Prior to the pandemic, there was already concern about clinician well-being and its relationship to patient outcomes. For example, the “Quadruple Aim,” put forth by Berwick et al. (2018), builds on the Institute for Healthcare Improvement's (2021) Triple Aim, which considers improving patient experience, improving population health, and reducing the per capita cost of care to optimize health system performance. Adding the component “care of care providers” bolsters the Triple Aim—hence, the Quadruple Aim. In addition, the National Academy of Medicine launched its Action Collaborative on Clinician Well-being in 2017 to raise awareness of issues surrounding anxiety, burnout, depression, stress, and suicide among clinicians and to promote interprofessional solutions to improve clinician well-being while improving patient outcomes. To summarize, clinician well-being was of high concern prior to COVID-19 (e.g., Mousavi et al., 2017); the pandemic has only exacerbated the conditions of an already stressed workforce (see Vizheh et al., 2020 for a systematic review).
Comprising the largest group of providers in hospitals, nurses have long been calling to improve their working conditions, including improving staffing and work environments to retain nurses and improve patient outcomes (Brom et al., 2021; Lasater et al., 2021). This has become more important now than ever (Schlak et al., 2021). COVID-19 has intensified the already highly strained nursing workforce as many have had their responsibilities increased, leading to working longer hours with limited staffing and personal protective resources (Arnetz et al., 2020; Benfante et al., 2020; Iheduru-Anderson, 2021; Jackson et al., 2020; Lapum et al., 2021; Leng et al., 2021; Lorente et al., 2021; Newby et al., 2020; Nie et al., 2020; Sagherian et al., 2020; Shaukat et al., 2020; Shechter et al., 2020; Vizheh et al., 2020). From the current literature, we know decreased mental well-being has been a major associated effect of working during the pandemic, particularly on nurses from Asia and China (e.g., Huang & Zhao, 2020; Lai et al., 2020). However, less is known about the effect of working during the pandemic on hospital-based nurses in the United States and how their well-being during the acute phase of the pandemic compares with that of others internationally.
Anticipating potentially severe impacts on frontline healthcare provider well-being, we launched the CHAMPS (Caring about Health for All, a study of the COVID-19 workforce) Registry to gather longitudinal data that will contribute to the understanding of the lasting effects of the pandemic on this workforce within the context of the United States. The aims of the present study are to 1) describe the emotional distress of hospital-based registered nurses enrolled in the CHAMPS study during the initial acute phase of COVID-19 in the United States (i.e., during the ‘shelter-in-place’ period), and 2) compare our (i.e., CHAMPS Registry) hospital-based registered nurses' emotional distress to rates reported among healthcare workers reported in two recent meta-analyses (Batra et al., 2020; Li et al., 2021) which comprised of 79,437 and 97,333 globally-based healthcare workers, respectively. Each meta-analysis included 65 studies (not mutually exclusive), and the data were collected primarily in Asian countries. Over half (N = 74) of the studies were conducted in China and about 45% of the healthcare workers sampled were nurses.
1. Methods
1.1. Participants and setting
The present study represents a cross-sectional examination of a baseline data subset from the CHAMPS Registry (ClinicalTrials.gov registration # NCT04370821). The design of the CHAMPS Registry is more thoroughly expounded upon in another source (Kaufmann et al., 2021). The National Institutes of Health issued a Certificate of Confidentiality (CC-OD-20-157) for this study dated April 21, 2020. Informed consent was obtained from each participant prior to enrolling in the study, which was approved by the authors' Institutional Review Board (IRBFY2020–213).
Participants were recruited using a snowballing strategy including outreach to alumni of the authors' university, news media, professional and trade organizations, social media, and outreach to facilities that treated COVID-19 patients. Registered nurses working throughout the U.S. and the U.S. territories (Puerto Rico, Guam, and the U.S. Virgin Islands) were eligible for the study. The primary sample described in this paper includes 467 hospital-based registered nurses (RNs) enrolled between May 5, 2020, and June 15, 2020. Data collection took place during the second half of the economic shutdown (i.e., the ‘shelter-in-place’ phase), which was experienced throughout the majority of the U.S. This period has been reported to be marked by shortages of PPE, overwhelmed critical care units, and deaths of healthcare providers (Bandyopadhyay et al., 2020; Keles et al., 2021). During this time COVID-19 infections doubled from 1,141,060 to 2,186,782 cases according to the Johns Hopkins Center for Systems Science and Engineering dashboard.
1.2. Measures
In addition to demographic information (i.e., race/ethnicity, age, gender-identity, marital status, education, hospital type, job role, type of work unit, living situation, region of U.S.), participants completed four validated instruments to measure emotional well-being at one point in time via the online Qualtrics platform. These instruments included: the Generalized Anxiety Disorder-7 for anxiety symptoms (GAD-7, Spitzer et al., 2006), the Patient Health Questionnaire-2 for depressive symptoms (PHQ-2, Kroenke et al., 2003; Arroll et al., 2010), the Impact of Events Scale-Revised for traumatic stress (IES-R, Creamer et al., 2003; Weiss & Marmar, 1997), and the Insomnia Severity Index (ISI) for sleep quality (Morin et al., 2011). We used categorical values of severity based on prior literature showing valid and reliable cut-offs for screening clinically significant symptoms as described below (e.g., Arroll et al., 2010; Kroenke et al., 2007).
GAD-7 scores range from 0 to 21. Scores of 0 to 4 suggest no to minimal anxiety, scores of 5 to 9 mild anxiety, scores of 10 to 14 moderate anxiety, and scores of 15 to 21 severe anxiety. Based on prior validation studies, we used a cut-off score of 10 to signify clinically significant symptoms of anxiety (e.g., Kroenke et al., 2007). The Cronbach's alpha coefficient for the GAD-7 in the present sample was equal to 0.92.
PHQ-2 scores range from 0 to 6 with higher scores meaning worse depression. Arroll et al. (2010) reported in their validation paper of the PHQ-2 that a score of 10 on the PHQ-9 (which typically denotes moderate depression) is most comparable to a score of 2 on the PHQ-2. Therefore, to make cross comparisons with the samples using the PHQ-9, we designated a score of 1 as “mild” depressive symptoms, 2 as “moderate” symptoms, and 3 as “severe” depressive symptoms, or equivalent to a score equal to above 15 on the PHQ-9. For the PHQ-2, because a score of 2 maps to a score of 10 according to the study by Arroll et al. (2010), and to be consistent with the Lai et al., 2020 study reporting similar outcomes for healthcare workers during the acute phase of COVID-19 in China (they used a cut-off of 10 for the PHQ-9), we applied the score of 2 to denote the presence of clinically significant symptoms of depression. Cronbach's alpha coefficient for the PHQ-2 in the present sample was equal to 0.83.
ISI scores range from 0 to 28, with higher scores meaning poor sleep quality. Categorically, scores of 0 to 7 represent no insomnia, scores 8 to14 represent subthreshold, scores 15 to 21 represent moderate insomnia, and scores 22 to 28 represent severe levels of insomnia (Morin et al., 2011). Again, to be consistent with the Lai et al., 2020 study conducted during the acute phase of COVID-19 in China, we considered poor sleep quality to be represented by a score ≥ 15 on the ISI. Cronbach's alpha coefficient for the ISI in the present sample was equal to 0.89.
Scores on the IES-R range from 0 to 88 with higher scores indicating more severe signs of traumatic stress and potential post-traumatic stress disorder (PTSD). Scores of 0–8 were considered “normal” or no traumatic stress, scores of 9–25 a “mild” degree traumatic stress, scores of 26–43 a “moderate” level of traumatic stress, and scores of 44–88 “severe” levels of traumatic stress (Lai et al., 2020; Zhang et al., 2020). Consistent with Lai et al.'s COVID-19 study of healthcare workers, clinically significant traumatic stress was considered a score over 25. The IES-R had a Cronbach's alpha coefficient of 0.94 in the present sample.
1.3. Data analysis
Data were exported from the Qualtrics platform into an SPSS datafile (v.25) for cleaning and analyses. We examined skewness, kurtosis, and the variable distributions by plotting histograms, box and whisker plots and Quantile-Quantile (Q-Q) plots to check for outliers and ascertain the degree of normality of the responses. Using the symptom cut-off scores described above, percentages with frequencies and 95% confidence intervals (CI) were calculated and presented in response to Aim 1: to report rates of distress in our sample of U.S. hospital-based RNs and Aim 2: to compare rates of distress among hospital-based RNs from the CHAMPS Registry to healthcare workers globally. To achieve Aim 2, we conducted z-tests for differences between two proportions to determine whether the variability in the symptom rates between the samples reached statistical significance. Our alpha for determining statistically significant differences was set at 0.05. Missing data constituted approximately 6% to 11% of the responses in the outcome variables (insomnia missing n = 29; traumatic stress missing n = 46; anxiety missing n = 49; depressive symptoms missing n = 51).
2. Results
The demographic characteristics of hospital-based RNs are described in Table 1 . The second column of this table shows comparisons of our sample to the National Workforce Survey data on variables available. The CHAMPS hospital-based RN sample identified mostly as female (92%) and white (91%); 69% were under the age of 45 years. Ninety-three percent served in direct patient care with 26% identifying their primary work as taking place on a COVID-19 designated unit and another 26% identifying their primary site as the intensive care unit (ICU). Compared to the characteristics of the meta-analyses, our sample comprised of a greater proportion of females (70% vs. 92%). However, they were relatively similar in age; data was available to calculate a weighted mean of 34.7 years for the Li/Scherer study. This compares with a mean (SD) of 38.1 (12.4) years for present study's CHAMPS hospital RNs. Additionally, the samples of the meta-analyses were primarily from Asian countries and included other health care workers with nurses comprising approximately 45% of their participants.
Table 1.
Demographic characteristics.
| Characteristic | N | (%) | 2020 National Workforce Survey (%) |
|---|---|---|---|
| Overall | 467 | (100) | |
| Gender | |||
| Male | 38 | (8.1) | (9.4) |
| Female | 429 | (91.9) | (90.5) |
| Gender non-conforming | 0 | (0) | (0.1) |
| Race / Ethnicity | |||
| White Non-Hispanic | 425 | (91.0) | (80.6) |
| Black/African American | 9 | (1.9) | (6.7) |
| Latinx/Hispanic | 9 | (1.9) | (5.6) |
| Asian/Pacific Islander | 9 | (1.9) | (7.6) |
| Multi-racial/Mixed identities | 8 | (1.7) | (2.1) |
| Other | 6 | (1.3) | (2.3) |
| Native American/Alaskan Native | 1 | (0.2) | (0.5) |
| Age (years) | |||
| 18–29 | 156 | (33.4) | (8.4) |
| 30–44 | 166 | (35.5) | (28.6) |
| 45–59 | 111 | (23.8) | (31.7) |
| 60 and over | 34 | (7.3) | (31.2) |
| Marital Status | |||
| Unmarried | 211 | (45.2) | |
| Married | 256 | (54.8) | |
| Education | |||
| Associates Degree/RN Diploma Program | 36 | (7.7) | (28.1) |
| Bachelors | 338 | (72.4) | (48.1) |
| Graduate Degree | 92 | (19.7) | (17.1) |
| Type of Hospital | |||
| Large / metropolitan | 240 | (51.4) | |
| Suburban / regional | 175 | (37.5) | |
| Rural / community-based | 52 | (11.1) | |
| Supervisory role | |||
| Yes | 55 | (11.8) | |
| No | 411 | (88.2) | |
| Direct Patient Care | |||
| Yes | 436 | (93.4) | (68.6) |
| No | 31 | (6.6) | (31.4) |
| Living Alone | |||
| Yes | 59 | (12.6) | |
| No | 408 | (87.4) | |
| Primary Work Unit | |||
| COVID designated | 117 | (25.8) | |
| Intensive Care Unit | 117 | (25.8) | |
| Emergency Department | 55 | (12.1) | |
| Other | 165 | (36.3) | |
| Region | |||
| Northeast | 351 | (75.3) | |
| South | 57 | (12.2) | |
| Midwest | 34 | (7.3) | |
| West | 24 | (5.2) | |
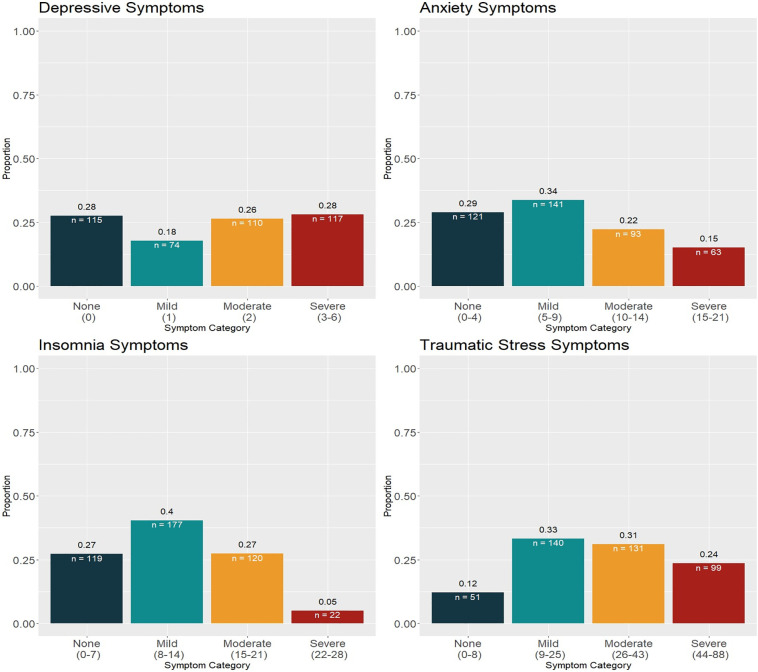
To answer our first study aim, we present the rates of each symptom category (anxiety, depression, insomnia, and traumatic stress) and the 95% confidence intervals (CIs) for the CHAMPS hospital-based RN sample in the upper portion of Table 2 . These rates are based on “moderate” degrees of symptom severity, as discussed in the measures section. A more nuanced break down of the experience of symptoms is shown in Fig. 1 (i.e., proportion of the sample scoring in the “no symptoms”, “mild”, “moderate”, and “severe” categories per established guidelines discussed in the measures section).
Table 2.
Prevalence of psychological symptoms.
| CHAMPS Hospital RNs (US) |
|||
|---|---|---|---|
| Psychological Outcome | N | Prevalence | 95% CI |
| Anxiety (GAD-7 ≥ 10) | 418 | 37.3% | (32.7%, 41.9%) |
| Depression (PHQ-2 ≥ 2) | 416 | 54.6% | (49.8%, 59.4%) |
| Insomnia (ISI ≥ 15) | 438 | 32.4% | (28.0%, 36.8%) |
| Traumatic Stress (IES-R ≥ 26) | 421 | 54.6% | (49.9%, 59.4%) |
| Batra et al. (Global) | |||
| Anxiety | 51,596 | 34.4% | (29.5%, 39.7%) |
| Depression | 53,164 | 31.8% | (26.8%, 37.2%) |
| Insomnia | 18,546 | 27.8% | (21.4%, 35.3%) |
| Traumatic Stress | 3676 | 11.4% | (3.6%, 30.9%) |
| Li-Scherer et al. (Global) | |||
| Anxiety | 97,333 | 22.1% | (18.2%, 26.3%) |
| Depression | 97,333 | 21.7% | (18.3%, 25.2%) |
| Insomnia | NA | NA | NA |
| Traumatic Stress | 97,333 | 21.5% | (10.5%, 34.9%) |
Fig. 1.
Proportions of hospital RN scoring in each symptom category for the PHQ-2 (depression), the GAD-7 (anxiety), the Insomnia Severity Index, and the IES-R (traumatic stress).
To answer our second study aim, we present the global prevalence rates of the symptoms captured in two recently published meta-analyses (Batra et al., 2020; Li et al., 2021) in the lower portions of Table 2. Using z-tests for differences between proportions, findings showed that compared to global rates reported in Batra et al. (2020) and Li et al. (2021), respectively, our sample of U.S. hospital-based RNs experienced significantly more traumatic stress (54.6% vs. 11.4%; z = 23.01; p < .001) and (54.6% vs. 21.5%; z = 16.47; p < .001). Rates of insomnia were also significantly higher in the CHAMPS hospital-based RN sample compared to the Batra meta-analysis (27.8% vs. 32.4%; z = 2.13; p < .033); the Li-Scherer review did not report on insomnia. Depressive symptoms were significantly more common in CHAMPS hospital-based RNs (54.6% vs. 31.8%; z = 9.92; p < .001) compared to the Batra et al. global rates and the rates reported by Li-Scherer et al. (54.6% vs. 21.7%; z = 16.19; p < .001). While rates of anxiety symptoms reported in CHAMPS hospital-based RNs (37.3%) did not differ from the 34.4% reported in the Batra et al. review (z = 1.25; p < .211), they were significantly higher than the 22.1% reported in the Li-Scherer et al. review (z = 7.48; p < .001).
3. Discussion
In summary, our data suggest that registered nurses working in U.S. hospitals were significantly more distressed on all well-being measures during the acute phase of the COVID-19 pandemic. Specifically, of particular concern are the high rates of severe depression found in our sample; 28% endorsed a 3 or above on the PHQ-2. This is 4 times greater than rates found in nurses working in China surveyed during a similar period of COVID-19 growth (Lai et al., 2020) and more than double the rates found in the general U.S. population during the same period (Ettman et al., 2020). Moreover, traumatic stress levels in U.S. nurses from the CHAMPS registry showed rates at nearly five times the level reported in the Batra et al. (2020) study and over twice the level reported in Li et al. (2021). Though our sample expressed higher levels of anxiety and insomnia symptoms as well, the differences were not as dramatic as seen with depression and traumatic stress.
Overall, although the reasons for such differences remain to be carefully evaluated, the higher psychosocial impact of the pandemic on nurses in the U.S. may include disparities in work environments among the types of healthcare workers being surveyed (i.e., the meta-analyses included physicians and other less hands-on workers vs. primarily direct care nurses). Or, perhaps the differences are partially due to the perceived failures of U.S. emergency response and mitigation strategies early in the pandemic. These failures could have also come in the form of acute changes in how management and organizational leaders were able to support nurses to provide optimal patient care while also attend to their own wellbeing. This could be explained, in part, by vast differences in the infrastructure and operations of the healthcare environments in the U.S. versus the other countries represented in the meta-analyses. It also may involve differences in the shelter-in-place policies experienced by healthcare workers throughout the world. Though U.S. policies that allowed only essential workers to operate in our economy were implemented to protect our citizens and the spread of the virus, this may have been responsible for worsening some of the distress levels our nurses demonstrated compared to healthcare workers on a more global level.
Furthermore, the possibility of culturally influenced responses cannot be excluded, especially considering the more recent experiences with pandemics such as SARS among Chinese healthcare workers. There are also considerable differences with respect to how mental health issues are viewed and expressed in Asian cultures (e.g., Chen et al., 2012). The social stigmas towards people with mental health disorders are even more severe in Asian countries than Western societies (Abdullah & Brown, 2011). In fact, those with mental illness are often considered dangerous and aggressive. Consequently, entire families may become socially devalued when one member experiences mental health problems according to a study by Lauber and Rössler (2007).
Indeed, the global rates of reported distress were surely heavily influenced by the experiences of healthcare workers in China. Of the 65 total studies reviewed in Batra et al., 23 were drawn from Chinese samples, while only 2 studies came out of the U.S. (2021)—neither of which were focused on the nursing workforce (Civantos et al., 2020 Shechter et al., 2020). This marks the importance of the present contribution. Interventions and treatment to address mental health concerns (Shanafelt et al., 2020) in the U.S. nursing workforce are needed to achieve best working conditions as advanced by the “Quadruple Aim” (Berwick et al., 2018).
3.1. Limitations
We interpret our findings with the following limitations in mind. Generalizability to all U.S. hospital-based RN must be made with caution given the snowballing sampling procedure. Compared to the National Workforce sample, CHAMPS nurses reported on here were more likely to be: a) younger, b) Bachelor's prepared, and c) working in direct patient care, some of which might have accounted for the high levels of distress experienced during the initial acute phase of the COVID-19 pandemic. As shown in Table 1, many of our participants came from the Northeast. We may have seen a different degree of distress in areas of the country that were not hit as hard during the earliest phase of the pandemic as some sections of the Northeast (e.g., New York). Unfortunately, our sample had few people of color, and we cannot assume that a sample containing a more diverse group in terms of ethnic and racial identity would have reported the same experiences as the primarily white-identifying workers in the CHAMPS Registry examined here. Ongoing efforts are underway to reach out to underrepresented sections of the country and individuals identifying as racial and ethnic minorities. Nonetheless, our findings are important in terms of capturing the experiences of nurses in the acute phase of the pandemic and with ongoing data collection for the CHAMPS Registry underway, we will be able to describe the patterns of their psychological stress in future studies.
3.2. Concluding remarks
By June of 2020 when these data were collected, more than 600 nurses had died from COVID-19. Fears of potential infection and spread to their loved ones are matters that should be addressed in wellness programs to be implemented for the nursing staff even now with vaccinations available. This workforce, many of whom are young and have many years ahead as healthcare providers, have been putting their lives on the line to care for the sick in ways they likely never imagined when their careers began. The stress is no longer acute; 18 months past the initial crisis phase of the pandemic, we must think about the mitigation strategies needed to save a workforce that has been under fire for a protracted length of time. Despite the presence of a vaccine, new more transmissible variants of the virus (e.g., Delta variant) COVID-19 patients are still being hospitalized at disturbing rates, especially among the unvaccinated. The present data from the CHAMPS Registry highlight that nurses working in the U.S. experienced a level of acute distress last year that far exceeded that of the general U.S. population (Ettman et al., 2020) and nurses practicing in China during the height of the pandemic (Lai et al., 2020). As put forth by the “Quadruple Aim,” caring for the care providers requires implementing new interventions to enhance the well-being of hospital RNs who continue to tirelessly provide essential healthcare services to their fellow citizens.
Funding sources
The CHAMPS (Caring about Health for All, a study of the COVID-19 workforce) Registry is supported by a grant from Travere Therapeutics, anonymous donors and internal funding from the Villanova University M. Louise Fitzpatrick College of Nursing.
CRediT authorship contribution statement
Janell L. Mensinger: Conceptualization, Writing – original draft, Formal analysis, Data curation, Methodology, Validation, Visualization, Supervision, Project administration. Heather Brom: Conceptualization, Writing – original draft. Donna S. Havens: Funding acquisition, Conceptualization, Writing – review & editing, Supervision. Alexander Costello: Data curation, Formal analysis, Visualization, Writing – review & editing. Christine D'Annunzio: Conceptualization, Writing – review & editing. Jennifer Dean Durning: Conceptualization, Writing – review & editing. Patricia K. Bradley: Conceptualization, Writing – review & editing. Linda Copel: Conceptualization, Writing – review & editing. Linda Maldonado: Conceptualization, Writing – review & editing. Suzanne Smeltzer: Conceptualization, Writing – review & editing. Jennifer Yost: Conceptualization, Writing – review & editing. Peter Kaufmann: Funding acquisition, Conceptualization, Writing – review & editing, Supervision.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
We thank Ms. Ann B. McKenzie MSN, RN for assistance in study recruitment and public relations efforts, Ms. Anita Burry, Sharon Roth-DeFulvio, BIS, MCSE for their information technology support, Ms. Sandi Schultz for administrative assistance, and Thomas Roscoe, BA, for his ongoing assistance with the database. The study could not be conducted without their dedicated contribution of time and effort.
References
- Abdullah T., Brown T.L. Mental illness stigma and ethnocultural beliefs, values, and norms: An integrative review. Clinical Psychology Review. 2011;31(6):934–948. doi: 10.1016/j.cpr.2011.05.003. [DOI] [PubMed] [Google Scholar]
- Arnetz J.E., Goetz C.M., Sudan S., Arble E., Janisse J., Arnetz B.B. Personal protective equipment and mental health symptoms among nurses during the COVID-19 pandemic. Journal of Occupational and Environmental Medicine. 2020;62(11):892–897. doi: 10.1097/JOM.0000000000001999. [DOI] [PubMed] [Google Scholar]
- Arroll B., Goodyear-Smith F., Crengle S., Gunn J., Kerse N., Fishman T., Falloon K., Hatcher S. Validation of PHQ-2 and PHQ-9 to screen for major depression in the primary care population. Annals of Family Medicine. 2010;8(4):348–353. doi: 10.1370/afm.1139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandyopadhyay S., Baticulon R.E., Kadhum M., Alser M., Ojuka D.K., Badereddin Y.…Khundkar R. Infection and mortality of healthcare workers worldwide from COVID-19: A systematic review. BMJ Global Health. 2020;5(12) doi: 10.1136/bmjgh-2020-003097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Batra K., Singh T.P., Sharma M., Batra R., Schvaneveldt N. Investigating the psychological impact of COVID-19 among healthcare workers: A meta-analysis. International Journal of Environmental Research and Public Health. 2020;17(23):9096. doi: 10.3390/ijerph17239096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benfante A., Di Tella M., Romeo A., Castelli L. Traumatic stress in healthcare workers during covid-19 pandemic: A review of the immediate impact. Frontiers in Psychology. 2020;11 doi: 10.3389/fpsyg.2020.569935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berwick D., Snair M., Nishtar S. Crossing the global health care quality chasm: A key component of universal health coverage. JAMA. 2018;320(13):1317–1318. doi: 10.1001/jama.2018.13696. [DOI] [PubMed] [Google Scholar]
- Brom H., Brooks Carthon J.M., Sloane D., McHugh M., Aiken L. Better nurse work environments associated with fewer readmissions and shorter length of stay among adults with ischemic stroke: A cross-sectional analysis of United States hospitals. Research in Nursing & Health. 2021;44(3):525–533. doi: 10.1002/nur.22121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Y.-Y., Chien-Chang Wu K., Yousuf S., Yip P.S.F. Suicide in Asia: Opportunities and challenges. Epidemiologic Reviews. 2012;34(1):129–144. doi: 10.1093/epirev/mxr025. [DOI] [PubMed] [Google Scholar]
- Civantos A.M., Byrnes Y., Chang C., Prasad A., Chorath K., Poonia S.K.…Rajasekaran K. Mental health among otolaryngology resident and attending physicians during the COVID-19 pandemic: National study. Head & Neck. 2020;42(7):1597–1609. doi: 10.1002/hed.26292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J., Rodgers Y. Contributing factors to personal protective equipment shortages during the COVID-19 pandemic. Preventive Medicine. 2020;141 doi: 10.1016/j.ypmed.2020.106263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creamer M., Bell R., Failla S. Psychometric properties of the impact of event scale - revised. Behavior Research and Therapy. 2003;41:1489–1496. doi: 10.1016/j.brat.2003.07.010. [DOI] [PubMed] [Google Scholar]
- Emanuel E.J., Persad G., Upshur R., Thome B., Parker M., Glickman A.…Phillips J.P. Fair allocation of scarce medical resources in the time of Covid-19. New England Journal of Medicine. 2020;382(21):2049–2055. doi: 10.1056/NEJMsb2005114. [DOI] [PubMed] [Google Scholar]
- Ettman C.K., Abdalla S.M., Cohen G.H., Sampson L., Vivier P.M., Galea S. Prevalence of depression symptoms in us adults before and during the COVID-19 pandemic. JAMA Network Open. 2020;3(9):e2019686. doi: 10.1001/jamanetworkopen.2020.19686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang Y., Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: A web-based cross-sectional survey. Psychiatry Research. 2020;288 doi: 10.1016/j.psychres.2020.112954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iheduru-Anderson K. Reflections on the lived experience of working with limited personal protective equipment during the COVID-19 crisis. Nursing Inquiry. 2021;28(1) doi: 10.1111/nin.12382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute for Healthcare Improvement IHI triple aim initiative. 2021. http://www.ihi.org/Engage/Initiatives/TripleAim/Pages/default.aspx
- International Council of Nurses ICN confirms 1,500 nurses have died from COVID-19 in 44 countries and estimates that healthcare worker COVID-19 fatalities worldwide could be more than 20,000. 2020, October 28. https://www.icn.ch/news/icn-confirms-1500-nurses-have-died-covid-19-44-countries-and-estimates-healthcare-worker-covid
- Jackson D., Bradbury-Jones C., Baptiste D., Gelling L., Morin K., Neville S., Smith G.D. Life in the pandemic: Some reflections on nursing in the context of COVID-19. Journal of Clinical Nursing. 2020;29(13–14):2041–2043. doi: 10.1111/jocn.15257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keles E., Bektemur G., Baydili K.N. COVID-19 deaths among nurses: A cross-sectional study. Occupational Medicine. 2021;kqab035:1–5. doi: 10.1093/occmed/kqab035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B. The patient health questionnaire-2: Validity of a two-item depression screener. Medical Care. 2003;41(11):1284–1292. doi: 10.1097/01.MLR.0000093487.78664.3C. [DOI] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B.W., Monahan P.O., Löwe B. Anxiety disorders in primary care: Prevalence, impairment, comorbidity, and detection. Annals of Internal Medicine. 2007;146(5):317–325. doi: 10.7326/0003-4819-146-5-200703060-00004. [DOI] [PubMed] [Google Scholar]
- Lai J., Ma S., Wang Y., Cai Z., Hu J., Wei N., Wu J., Du H., Chen T., Li R., Tan H., Kang L., Yao L., Huang M., Wang H., Wang G., Liu Z., Hu S. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Network Open. 2020;3(3) doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lapum J., Nguyen M., Fredericks S., Lai S., McShane J. “Goodbye … through a glass door”: Emotional experiences of working in COVID-19 acute care hospital environments. Canadian Journal of Nursing Research. 2021;53(1):5–15. doi: 10.1177/0844562120982420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lasater K.B., McHugh M., Rosenbaum P.R., Aiken L.H., Smith H., Reiter J.G.…Silber J.H. Valuing hospital investments in nursing: Multistate matched-cohort study of surgical patients. BMJ Quality & Safety. 2021;30(1):46–55. doi: 10.1136/bmjqs-2019-010534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lauber C., Rössler W. Stigma towards people with mental illness in developing countries in Asia. International Review of Psychiatry. 2007;19(2):157–178. doi: 10.1080/09540260701278903. [DOI] [PubMed] [Google Scholar]
- Leng M., Wei L., Shi X., Cao G., Wei Y., Xu H., Zhang X., Zhang W., Xing S., Wei H. Mental distress and influencing factors in nurses caring for patients with COVID-19. Nursing in Critical Care. 2021;26(2):94–101. doi: 10.1111/nicc.12528. [DOI] [PubMed] [Google Scholar]
- Li Y., Scherer N., Felix L., Kuper H. Prevalence of depression, anxiety and post-traumatic stress disorder in health care workers during the COVID-19 pandemic: A systematic review and meta-analysis. PLoS One. 2021;16(3) doi: 10.1371/journal.pone.0246454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Livingston E., Desai A., Berkwits M. Sourcing personal protective equipment during the COVID-19 pandemic. JAMA. 2020;323(19):1912–1914. doi: 10.1001/jama.2020.5317. [DOI] [PubMed] [Google Scholar]
- Lorente L., Vera M., Peiró T. Nurses´ stressors and psychological distress during the COVID-19 pandemic: The mediating role of coping and resilience. Journal of Advanced Nursing. 2021;77(3):1335–1344. doi: 10.1111/jan.14695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morin C.M., Belleville G., Bélanger L., Ivers H. The insomnia severity index: Psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. 2011;34(5):601–608. doi: 10.1093/sleep/34.5.601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mousavi S.V., Ramezani M., Salehi I., Hossein Khanzadeh A.A., Sheikholeslami F. The relationship between burnout dimensions and psychological symptoms (depression, anxiety and stress) among nurses. Journal of Holistic Nursing and Midwifery. 2017;27(2):37–43. doi: 10.18869/acadpub.hnmj.27.2.37. [DOI] [Google Scholar]
- Newby J.M., O’Moore K., Tang S., Christensen H., Faasse K. Acute mental health responses during the COVID-19 pandemic in Australia. PLoS One. 2020;15(7) doi: 10.1371/journal.pone.0236562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nie A., Su X., Zhang S., Guan W., Li J. Psychological impact of COVID-19 outbreak on frontline nurses: A cross-sectional survey study. Journal of Clinical Nursing. 2020;29(21−22):4217–4226. doi: 10.1111/jocn.15454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sagherian K., Steege L.M., Cobb S.J., Cho H. Insomnia, fatigue and psychosocial well-being during COVID-19 pandemic: A cross-sectional survey of hospital nursing staff in the United States. Journal of Clinical Nursing. 2020;00:1–14. doi: 10.1111/jocn.15566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schlak A.E., Aiken L.H., Chittams J., Poghosyan L., McHugh M. Leveraging the work environment to minimize the negative impact of nurse burnout on patient outcomes. International Journal of Environmental Research and Public Health. 2021;18(2):610. doi: 10.3390/ijerph18020610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shanafelt T., Ripp J., Trockel M. Understanding and addressing sources of anxiety among health care professionals during the COVID-19 pandemic. JAMA. 2020;323(21):2133–2134. doi: 10.1001/jama.2020.5893. [DOI] [PubMed] [Google Scholar]
- Shaukat N., Ali D.M., Razzak J. Physical and mental health impacts of COVID-19 on healthcare workers: A scoping review. International Journal of Emergency Medicine. 2020;13(1):40. doi: 10.1186/s12245-020-00299-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shechter A., Diaz F., Moise N., Anstey D.E., Ye S., Agarwal S.…Abdalla M. Psychological distress, coping behaviors, and preferences for support among New York healthcare workers during the COVID-19 pandemic. General Hospital Psychiatry. 2020;66:1–8. doi: 10.1016/j.genhosppsych.2020.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B.W., Lowe B. A brief measure for assessing generalized anxiety disorder. Archives of Inernal Medicine. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Theorell T. COVID-19 and working conditions in health care. Psychotherapy and Psychosomatics. 2020:193–194. doi: 10.1159/000507765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vizheh M., Qorbani M., Arzaghi S.M., Muhidin S., Javanmard Z., Esmaeili M. The mental health of healthcare workers in the COVID-19 pandemic: A systematic review. Journal of Diabetes & Metabolic Disorders. 2020;19(2):1967–1978. doi: 10.1007/s40200-020-00643-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss D.S., Marmar C.R. In: Assessing psychological trauma and PTSD. Wilson J., Keane T., editors. Guildford; 1997. The impact of event scale –revised; pp. 399–411. [Google Scholar]
- Zhang C., Yang L., Liu S., Su M., Zhang B., Ma S., Wang Y., Cai Z., Li R., Kang L., Liu Z., Du H., Zhang J. Survey of insomnia and related social psychological factors among medical staff involved in the 2019 novel coronavirus disease outbreak. Frontiers in Psychiatry. 2020;11:1–9. doi: 10.3389/fpsyt.2020.00306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaufmann P.K., Havens D.S., Mensinger J.L., Bradley P.K., Brom H.M.…CHAMPS Study Investigators The COVID-19 study of healthcare and support personnel (CHAMPS): Protocol for a longitudinal observational study. JMIR Research Protocols. 2021;10(10):e30757. doi: 10.2196/30757. [DOI] [PMC free article] [PubMed] [Google Scholar]