Abstract
Thrombotic complications are common in patients with severe COVID-19 pneumonia with important consequences on the diagnostic and therapeutic management. We report a consecutive series of five patients on long-term oral anticoagulation therapy who presented to our hospital for severe COVID-19 pneumonia associated with segmental acute pulmonary embolism despite adherence to therapy and with an adequate anticoagulant range at the time of the event. Four patients were receiving a direct oral anticoagulant (two with edoxaban, one with rivaroxaban and one with apixaban) and one patient a vitamin K antagonist. No significant thrombotic risk factors, active cancer, or detectable venous thromboembolism were present. In all cases, elevated d-dimer and fibrinogen levels with a parallel rise in markers of inflammation were documented. The combination of these findings seems to support the hypothesis that considers the local vascular damage determined by severe viral infection as the main trigger of thrombi detected in the lungs, rather than emboli from peripheral veins.
Keywords: Pulmonary embolism, Infectious diseases, Anticoagulant
Highlights
COVID-19 infection is associated with frequent thromboembolic events.
Systemic anticoagulant therapy appears to be generally useful.
Despite appropriate chronic anticoagulant therapy, segmental and subsegmental acute pulmonary embolism is documented.
In this specific clinical scenario, the embolic genesis of pulmonary embolism is uncertain and complex interactions between inflammation and coagulation play a major role.
Introduction
The COVID-19 does not involve only the respiratory tract, but has also major implications for the cardiovascular system [1]. Recently, accumulating data have shown an increased number of thromboembolic events among hospitalized patients which seems to suggest that coagulation function may be significantly impaired [2, 3] with important consequences on the diagnostic and therapeutic management of these patients [4]. Some studies pointed out that a dysregulated immune response, as seen during the inflammatory storm associated with COVID-19, could play a decisive role in endothelial dysfunction and thrombosis [5, 6], and microvascular permeability is crucial in viral infections. This condition is aggravated by hypoxia, which augments thrombosis by both increasing blood viscosity and hypoxia-inducible transcription factor-dependent signaling pathway [7].
Recently, clinical and autoptic studies reported a high rate of thrombotic complications in hospitalized patients, despite systematic prophylactic [8] or therapeutic anticoagulation [9, 10].
We report a consecutive series of five patients on long-term oral anticoagulation therapy who presented to our hospital for severe COVID-19 pneumonia associated with segmental pulmonary embolism (PE) despite a correct adherence to therapy and with adequate anticoagulant range at the time of the event. Our observations seem to reinforce the hypothesis of inflammatory-procoagulant pathogenesis undermining the clinical manifestations of COVID-19 which appear to be not fully protected by conventional anticoagulant treatment.
Case reports
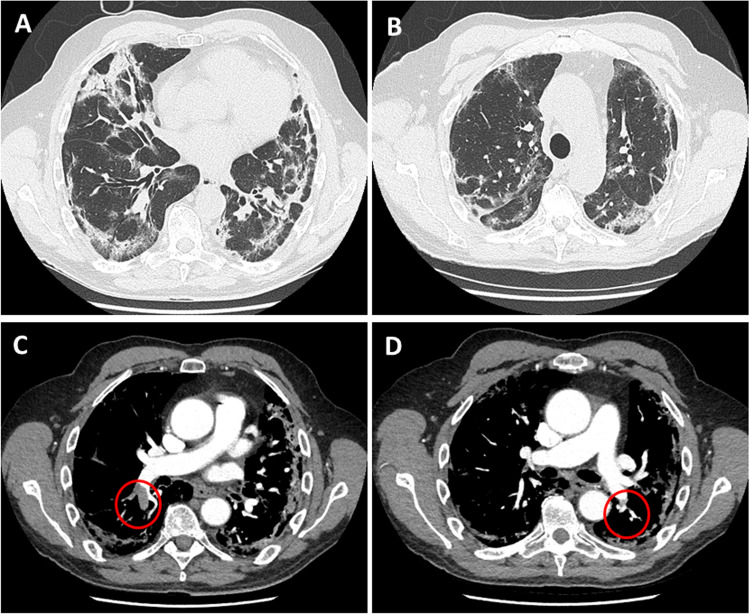
We analyzed demographic, clinical, radiological and laboratory characteristics of five consecutive patients on chronic anticoagulation therapy who presented in the emergency department (between March 1st and May 5th 2020) for severe COVID-19 pneumonia. Pneumonia was associated with acute PE diagnosed by means of CT pulmonary angiography (CTPA) at the time of admission (Fig. 1). According to our Institutional protocol, CTPA was performed in all subjects who met a Geneva score > 10 [11], and/or when the clinical suspicion of PE was very high, based on inadequate response to ventilation, or to high-flow oxygen therapy. CTPA was performed by a 64-row multidetector computed tomography scanner. The scan included the entire chest, with a cranio-caudal direction of scanning, and supine patient position. Standard CT scan settings were adopted: 120 kV tube voltage; 100–300 mA for tube current; 0.5 s of gantry rotation time; 64 × 0.6 mm detector collimation. Vessel attenuation was obtained by injecting 50–70 mL (volume calculated based on patient’s body weight) of non-ionic iodinated contrast media (iopamidol, Iopamiron 370 mg iodine/mL; Bracco, Milan, Italy) followed by a saline chaser of 25 mL through an antecubital vein at a flow rate of 3–4 mL/s, using a mechanical power injector. CT acquisition was timed by using bolus-tracking technique with a region-of-interest (ROI) placement in the pulmonary trunk. Once a threshold of 100 Hounsfield Units (HU) was reached, the scan automatically started after a delay of 5 s. Images were reconstructed with a thickness and increment of 1.25 mm. All CTPA scans were interpreted by two experienced radiologists and disagreements were resolved through discussion until consensus was reached.
Fig. 1.
Panel A and B Chest CT scan showing diffuse areas of consolidations and interlobular and intralobular septal thickenings involving both lung parenchymas. Panel C and D CT pulmonary angiography in axial view showing filling defects involving the inferior branch of the right pulmonary artery (open circles) and the posterior basal segmental branch of the left pulmonary artery (open circle)
SARS-CoV2 infection was confirmed by positive nasopharyngeal swab on real-time reverse transcriptase–polymerase chain reaction assay. Four of them were on chronic direct oral anticoagulants (DOAC) therapy (two patients were receiving edoxaban, one patient rivaroxaban, and one patient apixaban) and one was receiving a vitamin K antagonist (VKA). At admission, all patients claimed to diligently take the drugs, and at the same, time plasma samples were collected (an average of 15 h after the last dose intake). Appropriated DOAC plasma levels, and a prothrombin time, international normalized ratio (PT INR) > 2, with a time in therapeutic range (TTR) > 75% were confirmed by laboratory findings in all cases (Table 1). DOAC levels measurements (expressed as drug concentration-equivalent in ng/ml) were evaluated by using a specific anti FXa assay calibrated for apixaban, edoxaban, and rivaroxaban (Atellica COAG 360TM, Stago, France) [12]. At the time of admission, oral anticoagulant therapy was promptly replaced with a full dose (100UI/kg bid) of subcutaneous low-molecular-weight heparin up to one month of follow-up.
Table 1.
Demographic, clinical, radiological and laboratory findings
| Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | |
|---|---|---|---|---|---|
| Age (years) | 86 | 67 | 63 | 83 | 86 |
| Gender | M | M | M | F | F |
| Weight (Kg) | 68 | 65 | 72 | 49 | 60 |
| BMI > 30 | – | – | – | – | – |
| Hypertension | + | – | – | + | – |
| Diabetes | + | – | – | – | + |
| Heart failure | + | – | – | + | – |
| COPD | + | + | – | – | + |
| Active cancer | – | – | – | – | – |
| Chronic renal failure | + | – | – | – | – |
| Anticoagulant drug | Rivaroxaban | Edoxaban | Apixaban | Edoxaban | Warfarin |
| Anticoagulant dose | 15 mg day | 60 mg day | 5 mg BID | 30 mg day | |
| Plasma drug concentration ng/ml | 68 (LloD: 25) | 54 (LloD: 20) | 48 (LloD: 25) | 62 (LloD: 20) | |
| Indication to anticoagulation | AF | Previous PE | Previous PE | AF | AF |
| PE distribution | Segmental | Segmental | Subsegmental | Subsegmental | Subsegmental |
| ARDS severity at admission | Mild | Severe | Mild | Severe | Mild |
| PaO2/FIO2 ratio | 187 | 93 | 178 | 88 | 190 |
| PLT count x103 | 283 | 116 | 160 | 269 | 215 |
| CRP mg/l (nv: <5) | 70.5 | 82 | 33.2 | 321 | 27.3 |
| D-dimer µg/ml (nv: 0.5) | 3.99 | 18.4 | 7.2 | 0.27 | 1.7 |
| LDH U/l (nv: <248) | 234 | 786 | 214 | 447 | 358 |
| INR | 1.85 | 1.03 | 1.18 | 2.69 | 2.33 |
| APTT (nv: < 1.2) | 1.37 | 0.99 | 1.01 | 1.59 | 1.62 |
| TTr (nv: <1.2) | 1.10 | 1.3 | 1.60 | 1.2 | 0.9 |
| Fibrinogen ml/dl (nv: < 200) | 348 | 476 | 365 | 286 | 210 |
| Creatinine mg/dl (nv: < 1.18) | 1.28 | 1.09 | 0.86 | 0.74 | 0.6 |
| eGFR (mL/min) | 39.8 | 60.5 | 89 | 44.6 | 63.8 |
BMI body mass index, AF atrial fibrillation, PE pulmonary embolism, ARDS acute respiratory distress syndrome, PaO2 arterial partial pressure of oxygen, FIO2 fraction of inspired oxygen, PLT platelet, CRP C-reactive protein, LDH lactate dehydrogenase, INR international normalized ratio, APTT activated partial thromboplastin time, TTr thrombin time ratio, LloD lower limit of detection, eGFR estimated glomerular filtration rate
The chronic anticoagulant treatment had been previously prescribed as primary prevention of atrial fibrillation (AF)-related stroke in three patients and as secondary prevention of venous thromboembolism (VTE) in the remaining two patients. The dosages of DOACS were prescribed for each drug according to age, weight, and renal function as recommended by the international guidelines [13]. Two patients received anticoagulation after an episode of PE that was a consequence of a deep venous thrombosis (DVT) as a complication of a fracture of the lower limb. These episodes have occurred one year and six months before the present hospitalization. No other predisposing or genetic factors were reported. Demographic, comorbidities data, and main risk factors were recorded, as well as the main clinical features (ARDS severity by PaO2/FIO2 ratio, according to Berlin definition [14], PE type based on CTPA description, laboratory findings (including coagulation markers) and clinical outcomes. All the collected data are summarized in Table 1. All patients underwent lower extremities doppler ultrasonography but no sign of deep vein thrombosis (DVT) was detected. Transthoracic echocardiography showed no dilatation of right ventricular or pulmonary hypertension.
Discussion
Increased thromboembolic events among COVID-19 hospitalized patients have been largely reported [2, 3]. A French experience observed a frequency of PE twice higher than that found in a control period [15]. Additionally, clinical [16] and autopsy studies of patients who died of COVID-19 described a high incidence of deep venous thrombosis, with one-third of the patients who had a pulmonary embolism as the direct cause of death [17].
Approximately 1–2% of the western population is chronically treated with an oral anticoagulant [18], but, in the pre-COVID-19 era thrombotic events in patients on anticoagulation therapy were pretty uncommon [19]. In the PREFER Registry, among patients receiving chronic anticoagulation for AF (VKA in 48.7% of cases and a DOAC in 24.5%), the DVT recurrence was 3.9% with an overall incidence of PE of 1.3% [20]. Furthermore, only one recurrent episode of VTE (1.7 events per 100 patient-years) was documented in the more recent Dresden NOAC Registry [21]. However, COVID-19 infection is now considered an additional risk factor for DVT in hospitalized patients, but the rate of thrombotic recurrence in treated patients is unknown.
We report a series of five consecutive patients on chronic anticoagulant therapy who presented to our emergency department with severe COVID-19 pneumonia associated with acute PE. The peculiarity of this population is characterized by absence of major predisposing thrombotic risk factors: lack of detectable or recurrent history of VTE; no signs of active cancer or impairment of renal function; elevated D-dimer and fibrinogen levels with a parallel rise in markers of inflammation; localization of thrombus in the segmental and subsegmental branches of pulmonary arteries. Even if our observation is concerning a small sample of patients, these findings seem to support the hypothesis of a local vascular damage determined by viral infection in severe COVID-19 as the main trigger of thrombi detected in the lungs, rather than emboli from peripheral veins [22]. Recent morphologic studies may corroborate this pathological mechanism. In a series of autopsies of deceased COVID-19 patients [10, 23], pulmonary arteries at the hilum were free of thrombo-emboli, moreover, an elevated rate of platelet-fibrin thrombi in small arterial vessels (< 1 mm) was documented in the lung periphery, along with inflammatory infiltrate composed by macrophages in alveolar lumens and lymphocytes. This etiopathogenetic mechanism based on intense inflammatory-hypercoagulative status could explain the lack of protective effects of oral anticoagulant drugs (DOACS and VKA) despite their correct dose of administration and the evidence of adequate INR values and plasma levels. The latter were obtained by means of a validated specific anti FXa assay [12] and not via mass-spectrometry [24]. Consequently, we should cautiously consider the findings of DOACS concentration in this limited sample size.
In conclusion, recent observations suggest that COVID-19 infection promotes hypercoagulability. Our case series of severe interstitial pneumonia associated with acute PE in patients chronically treated with oral anticoagulant therapy underlines the role of complex interactions between inflammation and coagulation, representing a further challenge in the treatment of COVID-19 disease.
Author contributions
GDT designed the study; MD and IP contributed to data collection; all authors contributed to the interpretation of the data collected; GDT, MD and GBT wrote the draft of the manuscript; all the authors contributed to the final revision and accepted the manuscript.
Declarations
Conflict of interest
None of the authors has a conflict of interest to declare.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Guo T, Fan Y, Chen M, et al. Cardiovascular implications of fatal outcomes of patients with coronarovirus disease 2019 (COVID-19) JAMA Cardiol. 2020;5:811–818. doi: 10.1001/jamacardio.2020.1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bikdeli B, Madhavan MV, Jimenez D. COVID-19 and thrombotic or thromboembolic disease: implications for prevention, antithrombotic therapy, and follow-up. J Am Coll Cardiol. 2020;75:2950–2973. doi: 10.1016/j.jacc.2020.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Danzi GB, Loffi M, Galeazzi G, Gherbesi E. Acute pulmonary embolism and COVID-19 pneumonia: a random association? Eur Heart J. 2020;41:1858. doi: 10.1093/eurheartj/ehaa254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tang N, Bai H, Chen X, et al. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J Thromb Haemost. 2020;18:1094–1099. doi: 10.1111/jth.14817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schulz C, Engelmann B, Massberg S. Crossroads of coagulation and innate immunity: the case of deep vein thrombosis. J Thromb Haemost. 2013;11(Suppl 1):233–241. doi: 10.1111/jth.12261. [DOI] [PubMed] [Google Scholar]
- 6.Mezger M, Nording H, Sauter R, et al. Platelets and immune responses during thromboinflammation. Front Immunol. 2019;10:1731. doi: 10.3389/fimmu.2019.01731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Varga Z, Flammer AJ, Steiger P, et al. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;395:1417–1418. doi: 10.1016/S0140-6736(20)30937-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Klok FA, Kruip MJHA, van der Meer NJM, et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020;191:145–147. doi: 10.1016/j.thromres.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Llitjos JF, Leclerc M, Chochois C, et al. High incidence of venous thromboembolic events in anticoagulated severe COVID19 patients. Thromb Haemost. 2020;18:1743–1746. doi: 10.1111/jth.14869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lax SF, Skok K, Zechner P, et al. Pulmonary arterial thrombosis in COVID-19 with fatal outcome:results from a prospectiv, single-center, clinicopatholoogic case series. Ann Intern Med. 2020;173:350–361. doi: 10.7326/M20-2566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Klok FA, Mos ICM, Nijkeuter M, et al. Simplification of the revised Geneva score for assessing clinical probability of pulmonary embolism. Arch Intern Med. 2008;168:2131–2136. doi: 10.1001/archinte.168.19.2131. [DOI] [PubMed] [Google Scholar]
- 12.Gosselin RC, Adcock DM, Bates SM, et al. International council for standardization in hematology (ICSH). Recommendations for laboratory measurement of direct oral anticoagulants. J Thromb Haemost. 2018;118:437–450. doi: 10.1055/s-0038-1627480. [DOI] [PubMed] [Google Scholar]
- 13.Steffel TJ, Verhamme P, Tatjana S, Potpara TS, et al. The 2018 European Heart Rhythm Association Practical Guide on the use of non-vitamin K antagonist oral anticoagulants in patients with atrial fibrillation. Eur Heart J. 2018;39:1330–1393. doi: 10.1093/eurheartj/ehy136. [DOI] [PubMed] [Google Scholar]
- 14.Ranieri VM, Rubenfeld GD, Thompson BT, et al. Acute respiratory distress syndrome. JAMA. 2012;307:2526–2533. doi: 10.1001/jama.2012.5669. [DOI] [PubMed] [Google Scholar]
- 15.Poissy J, Goutay J, Caplan M, et al. Pulmonary embolism in COVID-19 patients: awareness of an invcreased prevalence. Circulation. 2020;142:184–186. doi: 10.1161/CIRCULATIONAHA.120.047430. [DOI] [PubMed] [Google Scholar]
- 16.Zhang L, Fenf X, Zhang D, et al. Deep vein thrombosis in hospitalized patients with coronavirus disease 2019 (COVID-19) in Wuhan, China: prevalence, risk factors, and outcome. Circulation. 2020;142:114–128. doi: 10.1161/CIRCULATIONAHA.120.046702. [DOI] [PubMed] [Google Scholar]
- 17.Fox SE, Akmatbekov A, Harbert JL, et al. Pulmonary and cardiac pathology in COVID-19: The first autopsy series from new orleans. Lancet Respir Med. 2020;8(7):681–686. doi: 10.1016/S2213-2600(20)30243-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Testa S, Paoletti O, Giorgi-Pierfranceschi M, Pan A. Switch from oral anticoagulants to parenteral heparin in SARS-CoV-2 hospitalized patients. Intern Emerg Med. 2020;15:751–753. doi: 10.1007/s11739-020-02331-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schulman S. How I treat recurrent venous thromboembolism in patients receiving anticoagulant therapy. Blood. 2017;129:3285–3293. doi: 10.1182/blood-2017-03-742304. [DOI] [PubMed] [Google Scholar]
- 20.Cohen AT, Gitt AK, Bauersachs R, et al. The management of acute venous thromboembolism in clinical practice. Results from the European PREFER in VTE Registry. J Thromb Haemost. 2017;117:1326–1337. doi: 10.1160/TH16-10-0793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Beyer-Westendorf J, Förster K, Pannach S, et al. Management, and outcome of rivaroxaban bleeding in daily care: results from the Dresden NOAC Registry. Blood. 2014;124:955–962. doi: 10.1182/blood-2014-03-563577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cattaneo M, Bertinato EM, Birocchi S, Brizio, et al. Pulmonary embolism or pulmonary thrombosis in COVID-19? Is the recommendation to ude high-dose heparin for thromboprophylaxis justified. J Thromb Haemost. 2020;120:1230–1232. doi: 10.1055/s-0040-1712097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wichmann D, Sperhake JP, Lütgehetmann M, et al. Autopsy findings and venous thromboembolism in patients with COVID-19: a prospective cohort study. Ann Intern Med. 2020 doi: 10.7326/M20-2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Douxfils J, Gosselin RC. Laboratory assessment of direct oral anticoagulants. Semin Thromb Hemost. 2017;43:277–290. doi: 10.1055/s-0036-1597296. [DOI] [PubMed] [Google Scholar]