Abstract
The objective of the current study was to complete a systematic review of the relationship between prenatal maternal stress due to potentially traumatic events (PTEs) and child temperament. Eligible studies through June 2020 were identified utilizing a search strategy in PubMed and PsycInfo. Included studies examined associations between prenatal maternal stress due to PTE and child temperament. Two independent coders extracted study characteristics and three coders assessed study quality. Of the 1,969 identified studies, 20 met full inclusion criteria. Studies were classified on two dimensions: (1) disaster-related stress, and (2) intimate partner violence during pregnancy. For disaster-related prenatal maternal stress, 75% (9 out of 12) of published reports found associations with increased child negative affectivity, 50% (5 out of 10) also noted associations with lower effortful control/regulation, and 38% (3 out of 8) found associations with lower positive affectivity. When considering prenatal intimate partner violence stress, 80% (4 out of 5) of published reports found associations with higher child negative affectivity, 67% (4 out of 6) found associations with lower effortful control/regulation, and 33% (1 out of 3) found associations with lower positive affectivity. Prenatal maternal stress due to PTEs may impact the offspring’s temperament, especially negative affectivity. Mitigating the effects of maternal stress in pregnancy is needed in order to prevent adverse outcomes on the infant’s socioemotional development.
Keywords: Systematic review, maternal stress, pregnancy, psychological trauma, temperament
The fetal programming hypothesis, as described in the Developmental Origins of Health and Disease (DOHaD) model, states that prenatal adversity can influence human behavior and mental health by shaping neurodevelopmental processes (D. J. P. Barker, 2007). Fetal programming theories suggest that prenatal adversity, in turn, is reflected in an expectant mother’s mental and physical health (Gluckman et al., 2008). Furthermore, DOHaD postulates that exposure to prenatal maternal stress might alter fetal neurodevelopment as reflected in an offspring’s temperament, specifically in reactivity and regulation (Van den Bergh et al., 2017). This relationship with temperament provides one possible mechanism for the established associations between prenatal maternal stress exposure and adverse child outcomes (Gartstein & Skinner, 2018). As a result, the risk for adverse emotional and behavioral outcomes can be increased even before birth.
Potentially traumatic events (PTEs) are life experiences which pose a significant threat to a person’s physical or psychological wellbeing (American Psychiatric Association, 2013). PTEs can be classified into individually experienced events and collectively experienced events (McFarlane & Norris, 2006). Individually experienced events include interpersonal violence, sudden bereavement, and life-threatening illness. In contrast, collectively experienced events include chronic threats (e.g., threat of terrorism), escalating threats (e.g., war and epidemics), and acute threats (e.g., natural disasters). PTEs can also be classified as chronic, escalating and acute threats according to the time-course of the events. Individually experienced events and interpersonal PTEs (e.g., intimate partner violence, physical assault, or sexual assault) have been shown to be more harmful in comparison to collectively experienced events or accidental exposures to PTEs (e.g., natural disaster or serious accident), war related trauma, and unexpected death of a love one (e.g., bereavement) and to have the highest risk to post-PTE psychopathology (Kessler et al., 2017; Schwerdtfeger & Goff, 2007).
Pregnant women are highly affected by the stress of PTEs (Levey et al., 2018). Among the most studied PTEs during pregnancy are natural and man-made disasters, intimate partner violence, and bereavement. Pregnant women exposed to trauma are twice as likely than nonpregnant women to die after the adverse exposure (Deshpande et al., 2017). Exposure to PTEs during pregnancy poses multiple threats to mental health. First, women exposed to intimate partner violence during pregnancy are at increased risk for depression, anxiety, perceived stress, alcohol or drug use, and post-traumatic stress disorders (PTSD; Kastello, Jacobsen, Gaffney, Kodadek, Bullock, et al., 2016; Kastello, Jacobsen, Gaffney, Kodadek, Sharps, et al., 2016; Murugan et al., 2020). Second, women who experienced a natural disaster during pregnancy report elevated depression and PTSD symptoms at two months postpartum (Harville et al., 2009). Some aspects of natural disasters, such as illness/injury, loss, or danger due to a hurricane, storm, flood or earthquake, may increase prenatal psychopathology. Pregnant women who experience traumatic war events, such as human and material losses, witnessing war events, and threat to life, also report higher PTSD and prenatal stress (Isosävi et al., 2017). To our knowledge, no studies have explored consequences of maternal bereavement (a core PTE) during pregnancy on maternal perinatal mental health. Studies examining PTEs may help us better understand the proximal mechanisms that may influence maternal mental health and aid targeted interventions. This approach is underutilized in the field.
Maternal adversity during pregnancy can lead to short and long-lasting outcomes in the offspring’s neurodevelopment. Women who were pregnant during the Tutsi genocide (Perroud et al., 2014) or the Holocaust (Yehuda et al., 2016) and their offspring had higher levels of PTSD and depression in comparison to non-exposed dyads. These authors suggested that children born from mothers exposed to a traumatic experience were at higher risk of adverse mental health outcomes (Perroud et al., 2014; Yehuda et al., 2016). Maternal stress has been associated with increased maternal glucocorticoid concentrations and subsequent increase in fetal exposure, glucocorticoid-sensitive brain regions, such as the amygdala and the hippocampus of the offspring, are the most affected (McGowan & Matthews, 2018). The amygdala plays a central role in threat and fear and defensive responses to external stimuli (LeDoux & Pine, 2016) and has an activating influence on the hypothalamic-adrenal (HPA) axis. The hippocampus, on the other hand, plays a major role in regulating the HPA axis and response to stress. In studies examining the developmental consequences of child adversity, the amygdala and hippocampus appear to be the brain regions the most affected (McLaughlin et al., 2019).
The current study focuses on the effect of prenatal stress due to PTEs on temperament, which is one of the core early indicators of socioemotional functioning in children (Pérez-Edgar, 2019). Temperament is an umbrella term for constitutionally-based characteristics associated with differences in reactivity and self-regulation (Rothbart et al., 2000). Within this conceptualization in psychobiological models, constitutional refers to the biological basis of temperament which include genetic, epigenetic, and specific microbiome mother-to-fetus transmission and programming (Gartstein & Skinner, 2018). According to Rothbart, Evans, and Ahadi (Rothbart et al., 2000), reactivity refers to excitability, responsibility, and arousability, while self-regulation refers to processes functioning to modulate this reactivity. Behavioral and parent-report measures suggest that temperament profiles are relatively stable (Beekman et al., 2015), and researchers often rely on a three-factor model of temperament including extraversion/surgency, negative affectivity, and regulation/effortful control evident across cultures (Rothbart et al., 2001). Merging the reactivity and regulation components, Thomas and Chess (Thomas & Chess, 1989) proposed three child temperament types: easy, difficult, and slow to warm up.
As noted above, temperament models suggest that multiple biological mechanisms contribute to observed socioemotional and behavioral profiles. Furthermore, temperament is modified over time via child maturation and experience. Traditionally, however, temperament traits are treated largely as genetically-based, such that the biological substrate is assumed to be set prior to birth (Rothbart & Bates, 2007). In this formulation, the environmental impact on the expression of temperament is thought to arise postnatally. However, recent work has captured more nuanced biological mechanisms of temperament, noting that prenatal stressors might activate a biological cascade effect during fetal development, generating epigenetic changes in temperament in utero (Ostlund et al., in press).
Prior research examining fetal programming of children’s temperament has focused on expectant mother’s stress, depression, anxiety, pregnancy-specific anxiety, and substance exposure (or combinations of these sources of stress) (Austin et al., 2005; Baibazarova et al., 2013; Davis et al., 2007; Haselbeck et al., 2017; Lin et al., 2018; Locke et al., 2016). Most of these studies have relied on a data-driven three-factor model of offspring temperament that includes Surgency/Positive Affectivity, Negative Affect, and Regulatory Capacity/Effortful Control. Positive Affectivity includes sociability, sensation seeking and activity. Negative Affectivity includes discomfort, fear, anger, sadness, low soothability. Regulation/Effortful Control includes processes, such as attention, which can modulate the expression of emotionality and reactivity. In general, researchers suggest that prenatal substance exposures and prenatal stress may heighten infant’s emotional reactivity and dampen regulation (Nolvi et al., 2016; Ostlund et al., in press, 2019; Werner et al., 2013).
Exploring specific PTEs during pregnancy may give an opportunity to understand their unique effects on child temperament, which has in turn been associated with psychopathology risk. Specifically, intimate partner violence as an individual experienced event and interpersonal PTE, natural disaster as a collectively experienced event or an accidental exposure PTE, and bereavement as an unexpected loss PTE were chosen for potential unique effects on temperament. In the case of natural disaster survivors, prenatal maternal stress offers an opportunity to explore the unique effects of wide-spread population level events on child development (King et al., 2012). This can be contrasted with the impact of intimate partner violence and unexpected loss, which while also a source of prenatal stress, do not typically occur at a population level (Chisholm et al., 2017).
Maternal traumatic stress increases or magnifies sensitivity to emotional distress (e.g., stress, anxiety, depression) during the perinatal period (Tung et al., 2020). Rather than differentiate the types of stressors, studies that focus on traumatic stress combine a list of exposures into a cumulative risk score, commonly as a count of negative life events (Austin et al., 2005; Baibazarova et al., 2013; Davis et al., 2007; Haselbeck et al., 2017). Nonetheless, this strategy hindered clarification of the specific mechanisms and the type, chronicity, or severity of the adversity that could help us better understand the processes underlying the intergenerational transmission of trauma and temperament. Building on the stress neurobiology literature, McLaughlin and colleagues characterized early childhood adversity into two groups: threat (e.g., violence in the community, intimate partner violence) and deprivation (e.g., support, socioeconomic status) (McLaughlin et al., 2014, 2019). According to this model, threat and deprivation have distinct influences on neural development. Controlling for co-occurring exposures (e.g., prenatal substance use) or possible consequences, such as maternal perinatal psychological distress, is needed to isolate potential effects on offspring.
While researchers have conceptualized and measured prenatal maternal stress and distress in a number of different ways, maternal depression during pregnancy has been the most common stressor studied. To date, there are two systematic reviews suggesting links between prenatal maternal anxiety and depression and an infant’s temperament reflected in increased negative reactivity or decreased self-regulation (Erickson et al., 2017; Korja et al., 2017). There are still multiple gaps in understanding the unique effects of other traumatic prenatal experiences, both acute, prolonged and chronic threats, may have on child temperament.
The overarching objective of the current study is to perform a comprehensive synthesis of the literature in order to provide a more precise determination of the associations between prenatal maternal stress due to PTEs, and its possible consequences on prenatal and early perinatal stress and distress, and subsequent child temperament. This systematic review encompasses all studies on prenatal maternal stress due to PTEs published through June 2020, including the specific onset of the stress exposure during gestation due to sudden events. Specific objectives of this review include (a) to examine the associations of prenatal maternal stress due to PTEs on children temperament; (b) to describe similarities and differences across studies of in the pattern of child temperament effects as a function of specific prenatal maternal stress due to unique PTEs, and (c) to identify methodological strengths and weaknesses among studies. Understanding prenatal origins of newborn temperament may also help to identifying mechanistic pathways by which prenatal adversity is transmitted from mother to child. This systematic review will help structure and appraise our knowledge on the prenatal origins of temperament, while also identifying specific targets for marking risk and intervening.
Methods
The research question was formulated according to the PECO format as follows: “Are mothers exposed to PTEs during pregnancy more likely to have children with altered temperament compared to mothers who are not exposed to such events?” This systematic review protocol was not registered previously in PROSPERO.
Definitional Criteria
Definition of exposure.
Potentially traumatic events (PTEs) are defined as “powerful and upsetting incidents that intrude into daily life”. They are usually experiences which are life threatening, or pose a significant threat to a person’s physical or psychological wellbeing” (American Psychiatric Association, 2013). PTEs include natural disasters, fire or explosion, serious transportation accident, physical assault, assault with a weapon, sexual assault, life threatening illness or injury, sudden violent death, severe human suffering, and sudden accidental death. For the purpose of this study, PTEs were limited to events that occurred during pregnancy to capture prenatal maternal stress and were categorized as individual experienced events and interpersonal (e.g., intimate partner violence, physical assault, or sexual assault), collectively experienced or accidental exposures (e.g., natural disaster or serious accident), and unexpected death of a love one (e.g., bereavement).
Definition of outcome.
The definition of temperament in the current systematic review is “individual differences that can be seen early in life, shaping our reaction to events in the social and physical environment, and the environment’s reaction to us. Temperament includes the child’s dispositions toward emotionality, activity and orienting, along with their attention based effortful control” (Rothbart, 2019). Child temperament includes an individual’s affect and behavior, regularity of biological functioning, response to new stimuli, adaptability to new situations, intensity of reaction, and quality of mood (Thomas & Chess, 1989). According to Thomas and Chess (1989) proposed temperament styles, the difficult child has irregular sleep and feeding schedules, is slow to accept new people and situations, and responds to frustration with tantrums (Thomas & Chess, 1989).
Search Strategy
This systematic review was performed according to the standard reporting recommendations by PRISMA (Moher et al., 2015). Searches were conducted in PubMed and PsycINFO between (April 2020 and June 2020) for published studies. A librarian suggested the text word fields searched. Relevant database specific subject heading and text word fields were searched. The search included the three concept strings related to: 1) stress, 2) pregnancy, and 3) temperament. For the first string, searches included “stress”, “adversity, “adverse event”, “adverse life event”, “anxiety”, “depression”. For the second string, searches included “pregnancy”, “prenatal”, and “antenatal”. For the third string, searches included “temperament”, “surgency”, “reactivity”, “regulation”, “effortful control”. Synonymous terms were combined with the Boolean operator “OR”, and then these three strings were combined using the Boolean operator “AND”. As recommended by a research librarian, truncation symbols were used in searches when appropriate (i.e., pregnan*, prenatal*). A systematic database search from 1980 up to June 2020 was performed. The search was limited to English and Spanish language articles.
Study Inclusion and Exclusion Criteria
Inclusion criteria for the systematic review were: (1) exposure: PTE experiences (sexual abuse, interpersonal partner violence, war, bereavement, and natural and man-made disasters) experienced by the mother during pregnancy and, if included, the possible consequences on prenatal maternal distress: maternal depression, trauma, and/or distress; (2) outcome: offspring’s temperament assessed prior to the age of 12 years; (3) the full-text article was available and written in English or Spanish. We excluded review articles, editorials, commentaries, and animal studies. An upper limit of 12 years was selected in light of the multiple changes in social relationships, biological maturation, and cognitive development seen in early adolescence (Vijayakumar et al., 2018). We excluded studies where the stress exposure was not restricted to pregnancy. Although negative life events during pregnancy are extremely stressful, we excluded them because they may fail to detect the effects of specific traumatic events.
Data Screening, Extraction and Analysis
Articles that were related to prenatal PTEs, and its possible consequences of prenatal and early perinatal stress and distress, and their effects on child temperament were extracted. A protocol was developed so that each sample of participants was presented in the systematic review. First, if a study presented more than one predictor (e.g., PTSD and depression) or outcome (e.g., effortful control and negative affect), each result was presented and entered into the tables separately. Second, if more than one time point of exposure or child outcomes were provided, each indicator was presented and entered into the tables.
After duplicate citations were removed, the remaining articles was assessed for eligibility by three independent reviewers (NR-S, IO-Q, MS-G). Studies meeting inclusion criteria were coded using a detailed coding system for recording sample, design and measurement. Sample characteristics were prenatal stress factor (PTEs, and PTSD or depression), time of assessment during pregnancy, child gender, family socioeconomic status, and mean age of the children at the time of assessment. The design and measurement characteristics included: study designs (case-control, cross-sectional, or cohort studies), temperament dimensions (negative affect, positive affect, or effortful control/regulation), or type of temperament (easy, difficult, or slow to warm-up), and sample size. Potential covariates accounted for included: medical risk (e.g., maternal age of pregnancy), socio-demographic risk (e.g., low income, low education, single parent, child age and sex, number of children, and gestational age), and behavior risk (e.g., smoking and alcohol use during pregnancy, and postnatal depression).
Finally, an assessment of study quality was conducted based on a quality assessment tool adapted from previous published meta-analyses and systematic reviews (Accortt et al., 2015; Madigan et al., 2018) (see Table 1). This tool considers elements of study quality recommended by the Cochrane collaboration group (Downes et al., 2016). Data extraction was conducted by first author (NR-S) and co-authors (IO-Q, MS-G). Two independent coders extracted study characteristics and three independent coders performed the quality assessment. Consensus was achieved among three data extractors and reported accordingly. Two experts (KP-E, CB) then reviewed and revised data extraction results.
Table 1.
Study Quality Criteria Evaluations
| 1. Defined Sample | Study has a defined eligibility and exclusion criteria for their sample; and time period (dates) and location (s) of recruitment and assessment.
|
0= No 1= Yes |
| 2. Demographic Information | Does the study report complete demographic data for parents and children included in the study? 0= No demographic information specified 1= data for only child or parent (eg., child gender, birthweight, gestational age, infant’s age). At least two indicators. 2= demographic data for child and parent |
0 = Not specified 1 = specified for parent or child 2 = specified for parent and child |
| 3. Representative Sample | Is the sample representative of a defined population? (i.e. was everyone included who should be and is this sample generalizable) E.g. only selecting mothers of children with disabilities = 0. 1 = Cohorts recruited from the general population or from multi-site (eg. cities or clinics) studies or large databases. 0 = Single site clinical studies (eg., one clinic or hospital) |
0= No 1= Yes |
| 4. Valid Instrument (Trauma/Stress) | Does the study use a validated instrument for the assessment of potentially traumatic event or stress? 0 = Non-validated (made up by researcher) 1 = Validated measure (eg., BDI, EPDS) |
0 = Non-validated 1 = Validated |
| 5. Valid Instrument (Child Temperament) | Does the study use a validated instrument for the assessment of child outcome? 0 = Non-validated (made up by researcher) 1 = Validated measure (eg., IBQ, ECBQ) |
0 = Non-validated 1 = Validated |
| 6. Subjective vs objective measures (Trauma/stress) | Does the study use different reporters or multiple methods to measure potentially traumatic events and stress? 0 = Maternal self-report (eg., EPDS) 1 = Objective measure = physician or clinical evaluation, cortisol levels or biological data. 2 = Multiple methods = self-report and biological data or clinical/physician diagnosis. |
0 = Self-report 1 = Objective measure 2 = Multiple methods |
| 7. Subjective vs objective measures (Child Temperament) | Does the study use different reporters or methods to measure child outcome? 0= Maternal report (IBQ, ECBQ) 1= Objective measure = observation protocol or cortisol 2= Multiple methods = self-report and biological data/multiple informants/observation protocol (Lab-TAB) |
0 = Maternal report 1 = Objective measure 2 = Multiple methods (e.g. two reporters, maternal report and observational data) |
| 8. Confounding Variables | Were confounding variables taken into account in the analysis? (Consider exclusion criteria, covariates and control in statistical analyses)
E.g. In modeling or regression did they control or adjust for confounding factors? |
0 = No control 1 = Limiting the sample, treating key variable as effect modifier or statistically controlling for three or more key variables from at least two categories out of three (eg. medical, sociodemographic, and behavior). 2 = Control for at least one variable from each category and a total of four or more variables. |
Results
Studies Selected
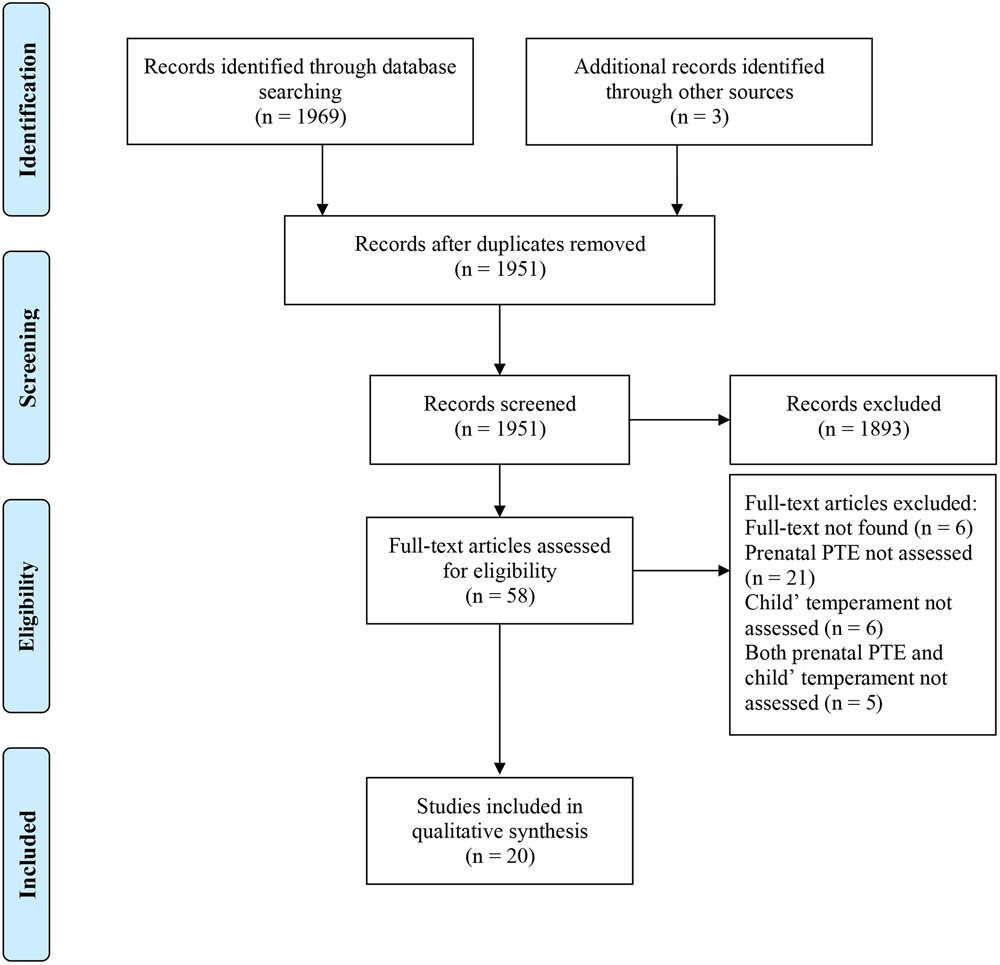
The PRISMA flow diagram detailing the search strategy is presented in Figure 1 (Moher et al., 2009). Our search of two databases yielded 1,969 articles. Upon review of the titles and abstracts, 58 articles were identified as potentially meeting study inclusion criteria. Three additional articles were identified through backward citation (Laplante et al., 2016; McLean et al., 2019; Tees et al., 2010). After review of full text articles, 20 studies met full inclusion criteria.
Figure 1.
PRISMA flow diagram
Study Characteristics and Quality
Study quality is reported in Table 2. Sample sizes ranged from 82 to 12,151 mother-child dyads (Med = 299). At the outcome assessment, child age averaged ranged from 2 to 24 months (mean: 8 months). Studies were found from multiple nations and territories, as labeled in the original study, including the United States (n = 12), Australia (n = 3), Israel (Gaza) (n = 3), England (n = 1), and Canada (n = 1). A detailed study quality is reported in Table 3. For study quality, the mean score across all studies was 6 (SD = 1.30; range 4 – 8). Included studies were classified on two dimensions: (1) collectively experienced event or accidental related exposure (natural and man-made disasters), and (2) individual experienced event and interpersonal exposure (intimate partner violence). Studies related to unexpected loss (bereavement) were not identified in the search.
Table 2.
Study quality criteria and characteristics
| Criteria | N (%) | |
|---|---|---|
| 1. Defined Sample | Yes | 11 (55%) |
| No | 9 (45%) | |
| 2. Demographic Information | Specified for Parent and Child | 8 (40%) |
| Specified for Parent or Child | 9 (45%) | |
| Not Specified | 3 (15%) | |
| 3. Representative Sample | Yes | 15 (75%) |
| No | 5 (25%) | |
| 4. Valid Instrument (Trauma/Stress) | Validated | 16 (80%) |
| Non-Validated | 4 (20%) | |
| 5. Valid Instrument (Child temperament) | Validated | 19 (95%) |
| Non-Validated | 1 (5%) | |
| 6. Subjective vs Objective Measure (Trauma/Stress) | Multiple Methods | 1 (5%) |
| Objective Measure | 2 (10%) | |
| Self-report | 17 (85%) | |
| 7. Subjective vs Objective Measure (Child temperament) | Multiple Methods | 2 (10%) |
| Objective Measure | 0 | |
| Maternal Report | 18 (90%) | |
| 8. Confounding Variables | Adequate control | 7 (35%) |
| Limited control | 12 (60%) | |
| No control | 1 (5%) |
Table 3.
Study Quality
| Defined sample |
Demograph ics |
Representativ e Sample |
Valid scale (trauma / stress) |
Valid scale (temperamen t) |
Subjective vs objective measure (trauma / stress) |
Subjective vs objective measure (temperament) |
Confounders’ Variables |
Total | |
|---|---|---|---|---|---|---|---|---|---|
| Ahlfs-Dunn (2014) | 0 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 5 |
| Barker (2013) | 1 | 0 | 1 | 1 | 1 | 0 | 0 | 1 | 5 |
| Brand (2006) | 0 | 0 | 0 | 1 | 1 | 2 | 0 | 1 | 5 |
| Burke (2008) | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 1 | 6 |
| Buthmann (2019) | 1 | 2 | 1 | 1 | 1 | 0 | 0 | 2 | 8 |
| Diab (2018) | 0 | 2 | 1 | 1 | 1 | 0 | 0 | 1 | 6 |
| Gibson (2015) | 1 | 1 | 1 | 1 | 1 | 0 | 2 | 1 | 8 |
| Isosavi (2017) | 0 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 5 |
| Laplante (2015) | 1 | 0 | 1 | 1 | 1 | 0 | 0 | 1 | 5 |
| Martinez-Torteya (2018) | 0 | 1 | 1 | 1 | 1 | 0 | 2 | 2 | 8 |
| McLean (2019) | 1 | 2 | 1 | 1 | 1 | 0 | 0 | 1 | 7 |
| McMahon (2011) | 1 | 2 | 1 | 0 | 0 | 0 | 0 | 1 | 5 |
| Miller-Graff (2019) | 0 | 1 | 0 | 1 | 1 | 0 | 0 | 1 | 4 |
| Nomura (2019) | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 2 | 7 |
| Pehne (2018) | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 4 |
| Quinlivan (2005) | 0 | 2 | 0 | 0 | 1 | 1 | 0 | 2 | 6 |
| Simcock (2017) | 1 | 2 | 0 | 1 | 1 | 0 | 0 | 1 | 6 |
| Tees (2010) | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 2 | 7 |
| Vanska (2019) | 0 | 2 | 1 | 1 | 1 | 0 | 0 | 0 | 5 |
| Zhang (2018) | 1 | 2 | 1 | 1 | 1 | 0 | 0 | 2 | 8 |
12 published studies examined disaster-related prenatal maternal stress and temperament (Table 4). Most studies (n = 8) were related to natural disasters (Buthmann et al., 2019; Laplante et al., 2016; McLean et al., 2019; Nomura et al., 2019; Pehme et al., 2018; Simcock et al., 2017; Tees et al., 2010; Zhang et al., 2018), including the Queensland Floods in Australia, the Quebec Ice Storm in Canada, and Superstorm Sandy and Hurricane Katrina in the United States. Man-made disasters included the World Trade Center collapse on 9/11 (Brand et al., 2006) in New York City and the Gaza War (2008-2009 and 2014) in Israel (Diab et al., 2018; Isosävi et al., 2017; Vänskä et al., 2019). Eight published findings examining prenatal intimate partner violence and temperament were identified from 20 studies (see Table 5) (Ahlfs-Dunn & Huth-Bocks, 2014; E. D. Barker, 2013; Burke et al., 2008; Gibson et al., 2015; Martinez-Torteya et al., 2018; McMahon et al., 2011; Miller-Graff & Scheid, 2020; Quinlivan & Evans, 2005).
Table 4.
Studies examining prenatal maternal stress due to disasters and child temperament
| Reference | Sample Country |
Methods | Prenatal stress Exposure Measure |
Confoun ders |
Outcome Measure |
Outcome | Quality | ||
|---|---|---|---|---|---|---|---|---|---|
| Negative affectivity |
Surgency/Posi tive affectivity |
Effortful control/ Regulation |
|||||||
| Brand (2006) |
*n = 98 USA |
Prospective Cohort Study Exposed PTSD: n= 47 Not exposed to PTSD: n= 55 |
PCL (Blanchard et al., 1996) Pregnancy (Sept. 11, 2002) 9/11 World Trade Center One week postnatally Maternal salivary cortisol (morning and night) |
Medical | IBQ (Rothbart, 1981) 9 months |
PTSD and infant’s distress to novelty (r = 0.450, p < 0.01). Maternal morning cortisol and infant distress to novelty (r = −0.274, p < 0.05). |
5 | ||
| Buthmann (2019) | n = 380 USA |
Prospective Cohort Study Prenatal: n= 169 Postnatal: n= 175 Preconception: n = 36 |
Storm32 (King & Laplante, 2005) Pregnancy (2nd trimester) Superstorm Sandy EPDS (Murray & Carothers, 1990) IES-R (Weiss & Marmar, 1996) |
Medical Sociodemographic Behavior |
IBQ-R (Gartstein & Rothbart, 2003) 6 months |
ns Prenatal depression and infants’ negative affectivity (r = 0.18, p <0.01). Prenatal subjective distress and infant’s negative affectivity (r = 0.11, p < 0.05). |
ns ns ns |
ns Prenatal depression and infant’s regulation (r = −0.15, p < 0.01) ns |
8 |
| Diab (2018) | n = 511 Israel (Gaza) |
Prospective Cohort Study | War trauma (Qouta et al., 2005) Pregnancy (2nd trimester) War of Gaza HTQ (Mollica et al., 1992) EPDS (Cox et al., 1987) |
Medical Sociodemographic |
IBQ-R (Gartstein & Rothbart, 2003) 4 months |
ns ns ns |
ns ns ns |
ns ns ns |
6 |
| Isosävi (2017) | n = 511 Israel (Gaza) |
Prospective Cohort Study | War trauma (Qouta et al., 2005) Pregnancy (2nd trimester) War of Gaza HTQ (Mollica et al., 1992) EPDS (Cox et al., 1987) |
Medical Sociodemographic |
IBQ-R (Gartstein & Rothbart, 2003) 4 months |
ns (In mothers with low levels of war trauma, high childhood emotional abuse was associated with higher negative affectivity (β = −0.21, p = 0.002). ns (Prenatal hypervigilance and infant’s sadness (r = −0.10, p < 0.05) ns |
ns ns ns |
5 | |
| Laplante (2016) | n = 121 Canada |
Retrospective Cohort Study/Cross-sectional | Storm32 (King & Laplante, 2005) Pregnancy Quebec Ice Storm IES-R (Weiss & Marmar, 1996) |
Medical Sociodemographic Behavior |
ICQ (Bates et al., 1979) 6 months |
ns Prenatal subjective distress and infants’ difficulty/fussy (r = 0.24, p < 0.01). |
ns ns |
ns Prenatal subjective distress and infant’s needs attention (r = 0.31, p < 0.001). |
5 |
| McLean (2019) | n = 104 Australia |
Prospective Cohort Study | QFOSS (Brock et al., 2014) Pregnancy Queensland floods IES-R (Weiss & Marmar, 1996) PDI (Brunet et al., 2001) EPDS (Cox et al., 1987) (6 months postpartum) |
Medical Behavior |
STST (Prior et al., 1989) 16 months |
ns Maternal subjective distress and toddler’s negative reactivity (r = 0.23, p < 0.05). ns Perinatal depression at 6 months and toddler’s negative reactivity (r = 0.28, p < 0.05). |
ns ns Peritraumatic distress and toddler’s persistence (r = −0.23, p < 0.05). ns |
7 | |
| Nomura (2019) | n = 310 USA |
Prospective Cohort Study Exposed: n=110 Not exposed: n=200 (pregnant before Sandy) |
Pregnancy during Superstorm Sandy EPDS (Murray & Carothers, 1990) |
Medical Sociodemographic Behavior |
IBQ-R (Gartstein & Rothbart, 2003) 6 months |
Infants exposed prenatally to Superstorm Sandy and to maternal depression had greater sadness (M = 3.74, p = 0.05) and greater distress (M = 4.50, p = 0.03) than those exposed to Superstorm Sandy (without depression). Prenatal depression and infant’s sadness (b = 0.05, p < 0.001) and distress (b = 0.25, p < 0.05) and less recovering from distress (b= −0.031, p < 0.01). |
Infants exposed prenatally to Superstorm Sandy and to maternal depression had greater activity (M = 4.87, p = 0.02) and greater approach (M = 6.03, p = 0.05) than those exposed to Superstorm Sandy (without depression). Prenatal depression and infant’s less smiling and laughter (b = −0.043, p < 0.01) and less high pleasure seeking (b = −0.20, p = 0.05). |
ns Prenatal depression and less infant’s soothability (b = −0.030, p < 0.01) and cuddliness (b= −0.034, p < 0.01). |
7 |
| Pehme (2018) | n = 95 USA |
Prospective Cohort Study Exposed: n=43 Not exposed: n=52 (44 gave birth before Sandy and 8 became pregnant after Sandy) |
Pregnancy during Superstorm Sandy (2nd trimester) EPDS (Cox et al., 1987) (6 months postpartum) |
Medical Sociodemographic Behavior |
IBQ-R (Gartstein & Rothbart, 2003) 12 months |
ns | Infants whose mothers were exposed (M = 5.59) compared to those who were not exposed in utero to Sandy (M = 6.12) had lower Smiling/Laughter scores, t(93) = 2.96, p = 0.004. ns |
ns | 4 |
| Simcock (2017) |
*n = 121 Australia |
Prospective Cohort Study Exposed: n= 38 Not exposed: n= 88 (not pregnant during floods) |
QFOSS (Brock et al., 2014): 7 months after disaster Queensland floods PDI (Brunet et al., 2001) IES-R (Weiss & Marmar, 1996) 12 months after floods |
Medical Sociodemographic Behavior |
STSI (Sanson et al., 1987) 6 months |
ns ns Maternal subjective distress and higher irritability (r = 0.27, p < 0.01). |
ns Peritraumatic distress and higher activity-reactivity (r = 0.21, p < 0.01). ns |
ns ns ns |
6 |
| Tees (2010) |
*n = 288 USA |
Prospective Cohort Study Prenatal (exposed): n=68 Preconception (not exposed): n= 216 |
EDS (Norris et al., 1999) Pregnancy Hurricane Katrina: 2 months postpartum PTSD Checklist (DeSalvo et al., 2007) EPDS (Cox et al., 1987) |
Medical Sociodemographic Behavior |
EITQ (Medoff-Cooper et al., 1993) 2 months TTS (Fullard et al., 1984) 12 months |
Flooding in the house and 3 difficult temperament among those pregnant during the storm (OR = 11.25). Perinatal PTSD increased odds of difficult temperament at 12 months (OR = 2.27). Perinatal depression increased odds of difficult temperament at 12 months (OR = 3.16). |
7 | ||
| Vänskä (2019) | n = 502 Israel (Gaza) |
Prospective Cohort Study | HTQ (Mollica et al., 1992) Pregnancy (1st trimester) 2014 War of Gaza |
Medical | IBQ-R (Gartstein & Rothbart, 2003) 6–7 months |
ns | ns | ns | 5 |
| Zhang (2018) | n = 318 USA |
Prospective Cohort Study Exposed: n=183 Not exposed: n=135 (pregnant before or after Sandy) |
Pregnancy during Superstorm Sandy (2nd trimester) |
Medical Sociodemographic Behavior |
IBQ-R (Gartstein & Rothbart, 2003) 6 months 12 months ECBQ (Putnam et al., 2006) 18 months 24 months |
At 6 months, children exposed to Sandy in-utero were rated higher on Fearfulness, and Perceptual Sensitivity as compared to no-exposed. Fearfulness decreased overtime. |
At 6 months, children exposed to Sandy in-utero were rated higher on High-Intensity Pleasure, and Approach as compared to no-exposed. Approach and High-Intensity Pleasure decreased overtime. |
At 6 months, children exposed to Sandy in-utero were rated lower on Cuddliness and Duration of Orientation as compared to no-exposed. | 8 |
Notes:
It is not clear from which groups participants were excluded. Questionnaires’ abbreviations. Depression: EPDS: Edinburgh Postnatal Depression Scale; PTE: Objective hardship: EDS: Exposure to Disaster Scale, QFOSS: Queensland flood objective stress scale, Storm32: Objective stress due to a storm; Subjective distress: IES-R: Impact of Event Scale-Revised; Peritraumatic Distress: PDI: Peritraumatic Distress Inventory; PTSD: PCL: PTSD checklist; Temperament: CITS: Carey Infant Temperament Scale, ECBQ: Early Childhood Behavior Questionnaire, EITQ: Early Infancy Temperament Questionnaire, IBQ: Infant Behavior Questionnaire, IBQ-R: Infant Behavior Questionnaire-Revised, ICQ: Infant Characteristics Questionnaire, STS: Short Temperament Scale, STSI: Short Temperament Scale for Infants, STST: Short Temperament Scale for Toddlers, TTS: Toddler Temperament Scale; Trauma: HTQ: Harvard Trauma Questionnaire.
Table 5.
Studies examining prenatal intimate partner violence (IPV) and child temperament
| Outcome Results | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Reference | Sample Country |
Methods | Prenatal stress Exposure |
Confoun ders |
Outcome Measure |
Negative affectivity |
Surgency/Posi tive affectivity |
Effortful control/ Regulation |
Quality |
| Ahlfs-Dunn (2014) |
*n = 120 USA |
Prospective Cohort Study Presence (exposed): n = 90 Absence (not exposed): n = 25 |
CTS-2 (Straus et al., 1996) Pregnancy (3rd trimester) PCL-C (Blanchard et al., 1996) |
Behavior | CFSI (McDonough et al., 1998) 3 months |
ns, Prenatal IPV and infant’s regulatory difficulties was moderated by prenatal PTSD avoidance symptoms ( = 0.39, p < 0.05). | 5 | ||
| Barker (2013) | n = 12151 UK |
Prospective Cohort Study | DIS (dependent interpersonal stress) Pregnancy (12 – 18 wk) (2nd trimester) EPDS (Cox et al., 1987) (32 wk prenatal) |
Sociodemographic Behavior |
CIT (Carey & McDevitt, 1978) 24 months CIT (Carey & McDevitt, 1978) 48 months |
Prenatal DIS and child’s dysregulation at 2 years (r = 0.08, p < 0.05) and child’ dysregulation at 4 years (r = 0.10, p < 0.05). Children of mothers who experienced prenatal DIS and chronic depression (r = 0.20, p < 0.05) showed continuity in dysregulation. |
5 | ||
| Burke (2008) | n = 4141 USA |
Prospective Cohort Study | IPV Interview After giving birth |
Medical Sociodemographic |
EAS (Buss & Plomin, 1984) 12 months |
Infants of mothers who had experienced psychological IPV during pregnancy reported difficult temperaments ( = 0.13, p < 0.001). | 6 | ||
| Gibson (2015) | n = 592 USA |
Prospective Cohort Study | CTS-2 (Straus et al., 1996) Pregnancy (2nd or 3rd trimester) CES-D (Radloff, 1977) (6 months postpartum) |
Medical Sociodemographic |
CIT (Carey & McDevitt, 1978) 6 months 12 months |
Once controlling for confounders, prenatal IPV was associated with poorer infant’s temperament (B = −2.925, p < 0.01). Perinatal depression mediated the association between prenatal IPV and poorer infant temperament (B = −2.130, p < 0.01). |
8 | ||
| Martinez-Torteya (2018) | n = 99 USA |
Cross-sectional with retrospective report | CTS-2 (Straus et al., 1996) Pregnancy |
Medical Sociodemographic Behavior |
Cortisol (infant) IBQ (Rothbart, 1981) 12 months |
ns ns, (For infants with Met allele, more physical IPV predicted less orienting (b = −0.29, p = 0.009). |
8 | ||
| McMahon (2011) | n = 3961 USA |
Prospective Cohort Study | IPV questions about pregnancy After baby’s birth |
Medical Sociodemographic |
Temperament questions 15 months |
Prenatal emotional IPV significantly affected toddler’s more difficult temperament (OR = 0.15, p < 0.001). | 5 | ||
| Miller-Graff (2020) | n = 82 USA |
Prospective Cohort Study Not exposed: n = 18 |
CTS-2 (Straus et al., 1996) Pregnancy CES-D (Radloff, 1977) |
Behavior | IBQ-R-VS (Putnam et al., 2014) 4 months |
ns, once adjusted for confounders ns |
Once adjusted for confounders, prenatal IPV was associated with infant’s positive affectivity (ß= −1.27, p < 0.001). ns |
ns, Once adjusted for confounders, prenatal IPV was associated with infant’s regulatory capacity (ß = −1.10, p < 0.001). ns |
4 |
| Quinlivan (2005) | n = 117 Australia |
Prospective Cohort Study Exposed: n = 33 Not exposed: n = 84 |
Interviews Pregnancy |
Medical Sociodemographic Behavior |
STS (Prior et al., 1989) 6 months |
Adolescent mothers who had been exposed to IPV had infants with more irritability than the non-abused (p < 0.01). | ns | ns | 6 |
Notes:
It is not clear from which groups participants were excluded. Questionnaires’ abbreviations. Depression: CES-D: Center for Epidemiological Studies Depression Scale, EPDS: Edinburgh Postnatal Depression Scale; PTE: Intimate Partner Violence: CTS-2: Conflict Tactics Scale 2, DIS: Dependent Interpersonal Stress; PTSD: PCL-C: PTSD checklist; Temperament: CFSI: Cry- Feed-Sleep Interview, CIT: Carey Infant Temperament Scale, IBQ: Infant Behavior Questionnaire, IBQ-R-VS: Infant Behavior Questionnaire-Revised: Very Short Form, EAS: Emotionality, Activity, Sociability Inventory, STS: Short Temperament Scale;
Studies Methodologies
Most studies were prospective cohort designs (n = 18), except for one retrospective cohort design (Laplante et al., 2016) and one cross-sectional study (Martinez-Torteya et al., 2018). To measure infant or child temperament, most studies administered maternal self-reported questionnaires (n = 19), such as the Infant Behavior Questionnaire (IBQ) (Rothbart, 1981). Very few studies included biological measures (n = 1) or multiple reporters (n = 1) (Gibson et al., 2015; Martinez-Torteya et al., 2018). To measure maternal stress, many studies measured maternal depression (n = 10) or maternal PTSD (n = 5) with self-reported questionnaires, such as the Edinburgh Postnatal Depression Scale (EDPS) (Murray & Carothers, 1990) or PTSD Checklist (PCL-C) (Blanchard et al., 1996). Only one study collected maternal biological measures during pregnancy (n = 1) (Brand et al., 2006). Furthermore, few studies assessed maternal subjective distress (n = 4) (Buthmann et al., 2019; Laplante et al., 2016; McLean et al., 2019; Simcock et al., 2017). To assess prenatal exposure to disasters, most studies included self-reported questionnaires to understand objective hardships due to disasters (n = 7), such as Storm32 (King & Laplante, 2005) or war checklist (Qouta et al., 2005). To assess prenatal exposure to intimate partner violence, most studies administered self-reported measures (n = 5), such as the Conflict Tactics Scale (CTS2) (Straus et al., 1996).
Of the 12 disaster reports, most were prospective cohort studies (n = 11). Of these 12 reports, five studies did not identify at least a not exposed group (Diab et al., 2018; Isosävi et al., 2017; Laplante et al., 2016; McLean et al., 2019; Vänskä et al., 2019). Five included adequate postnatal control for known temperamental risk factors (Buthmann et al., 2019; Nomura et al., 2019; Pehme et al., 2018; Tees et al., 2010; Zhang et al., 2018). For example, Zhang and colleagues (Zhang et al., 2018) controlled for seven medical (i.e., GDM/preeclampsia), socio-demographic (i.e., maternal education and infant’s sex) and behavioral factors (i.e., substance use and trauma) and excluded women with HIV infection, maternal psychosis, maternal age< 15 years, life-threatening maternal medical complications, and congenital or chromosomal abnormalities in the fetus. Furthermore, temperament was assessed longitudinally at 6, 12, 18 and 24 months with the IBQ-R (Gartstein & Rothbart, 2003) and ECBQ (Putnam et al., 2006).
Of the eight reports using intimate partner violence as an exposure, most were prospective cohort studies (n = 7). Only two studies identified unexposed groups of mothers for comparison (Ahlfs-Dunn & Huth-Bocks, 2014; Quinlivan & Evans, 2005). Of eight reports, two included adequate postnatal covariates for known temperamental risk factors, such as postnatal intimate partner violence and postnatal depression (Martinez-Torteya et al., 2018; Quinlivan & Evans, 2005). For example, Quinlivan & Evans (Quinlivan & Evans, 2005) controlled for 10 socio-demographic (i.e., social class, and homelessness) and behavioral factors (i.e., breastfeeding, and postnatal depression).
Timing of Exposures and Outcomes
Baseline assessments were conducted in most studies during second trimester (n = 6). In regard to natural disasters, most studies assessed prenatal consequences in the second trimester (n = 5), while others waited five to seven months after the disaster to collect data (Buthmann et al., 2019; Diab et al., 2018; Isosävi et al., 2017; Pehme et al., 2018; Zhang et al., 2018). In regard to intimate partner violence, most assessments were conducted during second or third trimester (n = 3) (Ahlfs-Dunn & Huth-Bocks, 2014; E. D. Barker, 2013) or after giving birth (n = 2) (Burke et al., 2008; McMahon et al., 2011).
In studies that explored associations between prenatal disaster stress and temperament, children’s assessment varied from 4 months to 24 months postnatally. In most reports (n = 10), temperament was only measured once. In the studies using exposure to intimate partner violence, the timing of temperament assessment varied from 4 months to 48 months postnatally. In most studies, temperament was measured at one time point (n = 6). Most studies used maternal self-reported measures of their child’s temperament and only two studies utilized multiple methods of assessments (Gibson et al., 2015; Martinez-Torteya et al., 2018). One report included measures that had not been independently validated (McMahon et al., 2011).
Summary of Findings: Prenatal Disaster Stress and Child Temperament.
Not all studies assessed each temperament dimension: all evaluated negative affect (or an indicator), while only 10 looked at effortful control/regulation and eight considered positive affectivity. When combining all possible prenatal disaster stress exposures (maternal depression or PTSD, objective hardships due to disasters, and subjective distress), 75% (9 out of 12) of published reports noted associations with higher negative affectivity, 50% (5 out of 10) noted associations with decreased effortful control/regulation, and 38% (3 out of 8) noted some associations with positive affectivity.
Negative affectivity.
In the 7 studies that explore prenatal depression or perinatal PTSD symptoms, 5 studies suggested positive associations with children’s negative affectivity (Brand et al., 2006; Buthmann et al., 2019; McLean et al., 2019; Nomura et al., 2019; Tees et al., 2010). In the 4 studies where subjective distress was included, 4 studies found positive associations (Buthmann et al., 2019; Laplante et al., 2016; McLean et al., 2019; Simcock et al., 2017). When objective hardships due to the disaster experience were considered in 10 of the studies, only 4 studies showed associations with negative affectivity (Isosävi et al., 2017; Nomura et al., 2019; Tees et al., 2010; Zhang et al., 2018).
Positive affectivity.
In the 4 studies that explores prenatal depression or perinatal PTSD, only one study suggested a negative association with children’ positive affectivity (Miller-Graff & Scheid, 2020). No associations between subjective distress and positive affectivity were found out of 3 studies. When objective hardships due to the disaster experience were considered, associations were inconsistent in most studies. At least 3 out of 7 suggested some type of association between those infants prenatally exposed to the disaster in comparison to those not exposed (Nomura et al., 2019; Pehme et al., 2018; Zhang et al., 2018).
Effortful control/regulation.
Only two studies suggested negative associations between prenatal depression or perinatal PTSD and effortful control/regulation in the five studies that evaluated this relationship (Buthmann et al., 2019; Nomura et al., 2019). In four studies that included subjective distress, only one study suggested a negative association with effortful control (Laplante et al., 2016). In nine studies that considered objective hardships due to the disaster experience, associations were not found in most studies, with only one showing negative association between those infants prenatally exposed to the disaster in comparison to those not exposed (Zhang et al., 2018).
Summary of Findings: Prenatal Intimate Partner Violence and Child Temperament.
Not all studies assessed each temperamental dimension: studies looked at indicators of negative affect, positive affectivity, and effortful control. When considering both maternal prenatal psychological symptoms and objective intimate partner experience, 80% (4 out of 5) of published reports noted associations with higher negative affectivity, 67% (4 out of 6) found associations with lower effortful control/regulation, and 33% (1 out of 3) noted associations with lower positive affectivity.
Negative affectivity.
In a study that explored prenatal depression as a consequence of prenatal intimate partner violence exposure, no association was found between prenatal depression and toddler negative affectivity (Miller-Graff & Scheid, 2020). However, in a different study perinatal depression at 6 month postpartum mediated the association between prenatal intimate partner violence and poorer infant’s temperament (Gibson et al., 2015). Prenatal intimate partner violence showed associations with difficult temperament or irritability (n = 4 out of 5) (Burke et al., 2008; Gibson et al., 2015; McMahon et al., 2011; Quinlivan & Evans, 2005).
Positive affectivity.
In a study that explored prenatal depression as a consequence of prenatal intimate partner violence exposure, no association was found between prenatal depression and infant’s positive affectivity (Miller-Graff & Scheid, 2020). Only one study (1 out of 2) suggested a negative association between prenatal intimate partner violence and infant’s positive affectivity (Miller-Graff & Scheid, 2020).
Effortful control/regulation.
Only one study suggested a positive association between prenatal chronic depression and prenatal intimate partner violence and child’s dysregulation (n = 1 out of 1) (E. D. Barker, 2013). When objective experience was considered, four studies suggested associations with indicators of child’s effortful control/regulatory capacity (n = 4 out of 5) (Ahlfs-Dunn & Huth-Bocks, 2014; E. D. Barker, 2013; Martinez-Torteya et al., 2018; Miller-Graff & Cheng, 2017).
Discussion
This systematic review presented a descriptive assessment of the relatively small number of published reports that have examined the associations between unique prenatal PTE’s and children’s temperament. The three-factor model of temperament including extraversion/surgency, negative affectivity, and regulation/effortful control has been among the most studies formulation of temperament (Buthmann et al., 2019; Diab et al., 2018; Isosävi et al., 2017; Miller-Graff & Scheid, 2020; Nomura et al., 2019; Pehme et al., 2018; Vänskä et al., 2019). Not surprisingly, most researchers selected this model in their respective studies. Results suggest that clear patterns emerged showing that prenatal PTE’s were associated most strongly with indicators of increased negative affectivity and decreased effortful control/regulation (Erickson et al., 2017; Korja et al., 2017). Specifically, 75% (n = 9 out of 12) of published reports found significant associations between any prenatal disaster-related stress and child temperament, and 67% (n = 6 out of 9) of published results found significant associations between prenatal intimate partner violence stress and child temperament. The majority of studies used validated self-report measures to evaluate PTEs and mother’s perceptions of their child’s temperament. As covariates, short screening tools to evaluate levels of perinatal depression or PTSD and cutoff scores for identifying clinically significant symptoms were included. However, very few studies used a confirmed clinical diagnosis as a measure.
To our knowledge, this is the first systematic review that explores the associations between prenatal PTEs and children’ temperament. We used a systematic method (i.e. PRISMA guidelines) (Moher et al., 2015) and covered a fairly long time period (1980 – 2020). Although the search engine considered studies from 1980 – 2020, the first published reports in this area were evident in 2005. Given that, it is notable that 20 studies met inclusion criteria. We included retrospective assessments (n = 1) of prenatal exposure to any PTE. We also added studies that combined maternal perinatal mental health (i.e., depression, and PTSD) as secondary variables or as covariates. We found that the evidence favors broad associations between potentially traumatic events during pregnancy and patterns of child temperament. In more specific terms, exposure to prenatal disaster and prenatal intimate partner violence were more closely associated with higher negative affect in the child.
The effects of prenatal stress on offspring temperament due to a disaster were unique to the developmental window observed. At two months of age, infants exposed in utero to a natural disaster and PTSD and depression had increased odds of having an infant with three characteristics of difficult temperament (Tees et al., 2010). At four months of age, we found no associations with any temperament dimensions, with the exception of prenatal hypervigilance and infant sadness (Diab et al., 2018; Isosävi et al., 2017). At six months, infant exposure to prenatal depression due to a natural disaster was associated with increase negative affectivity, decreased effortful control and less positive affect (Buthmann et al., 2019; Nomura et al., 2019; Simcock et al., 2017; Zhang et al., 2018), but prenatal trauma was not associated with any of these temperamental traits (Vänskä et al., 2019). At twelve months of age, infants exposed in utero to a natural disaster and PTSD had three characteristics of difficult temperament and lower Smiling and Laughter scores (Pehme et al., 2018; Tees et al., 2010). At 16 months, prenatal depression due to a natural disaster was associated with toddler’s negative reactivity but not persistence, while peritraumatic distress was associated with toddler’s persistence, but not negative reactivity (McLean et al., 2019). Of course, a more comprehensive longitudinal study capturing temperament in the same children across the time windows would be needed to fully test any developmentally-related outcomes.
The effects of prenatal stress due to intimate partner violence on offspring temperament were also unique to child development. At three months of age, infants exposed to prenatal intimate partner violence was associated with infant’s regulatory difficulties (Ahlfs-Dunn & Huth-Bocks, 2014). At four months of age, infants’ prenatal intimate partner violence was associated with lower positive affectivity and regulatory capacity, but not with negative affectivity (Miller-Graff & Scheid, 2019). At six months of age, infants exposed to intimate partner violence were more irritable than those non-exposed (Quinlivan & Evans, 2005). However, temperament trajectories associated with prenatal intimate partner violence are not clear. Due to this, disentangling the biological dimensions of prenatal aspects from the social-contextual are complex.
Studies about prenatal disaster-related stress and temperament had the most controls in the designs. Most studies about natural disaster-stress included some type of control (prenatal exposure or unexposed group), while studies about war-related stress did not include controls to explore differential effects on offspring temperament. Multiple methods of assessing prenatal maternal stress (i.e., self-report and biological data) noted differential associations (Brand et al., 2006). In terms of child outcome, studies with at least two time points suggested that longitudinal changes in offspring temperament due to disaster-related prenatal stress are characterized by pattern of changes in temperament (Tees et al., 2010; Zhang et al., 2018). Unfortunately, none of these studies provided multiple-informant or observational methods to assess child temperament which again could reduce the maternal report bias and provide more fruitful data.
Studies regarding prenatal intimate partner violence and temperament had fewer controls in the designs. Lack of control group in most studies prevented us from examining differences in temperament outcomes among exposed and nonexposed groups. Results suggest associations with negative affectivity even when controlling with a nonexposed group (Burke et al., 2008; Quinlivan & Evans, 2005). Unlike disaster-related studies, two studies had multiple methods to assess child temperament (Gibson et al., 2015; Martinez-Torteya et al., 2018). The addition of observational assessment, particularly when coupled with longitudinal measures of child temperament, will allow for multidimensional assessment of long-term impacts. For example, the child maltreatment and neglect literature (Blaisdell et al., 2019) suggests that early experiences may have long-term implications for biological regulatory mechanisms. For example, blunted HPA-axis responses often follow early hyperreactivity, providing a mechanistic understanding of observed changes in emotional reactivity and regulation (Reilly & Gunnar, 2019).
Although both prenatal disaster-related stress and prenatal intimate partner violence are PTEs, vulnerabilities to these exposures during pregnancy varies substantially. On the one hand, intimate partner violence is an interpersonal exposure and an individually experienced event with chronic and prolonged stress. A history of childhood sexual or physical abuse was associated with threefold increase of experiencing intimate partner violence during pregnancy (Gartland et al., 2016). In this case, women with a history of childhood abuse may be at high risk of revictimization in adulthood. Pointing to a precise day where the stressor occurs in this case is problematic. Moreover, women who reported intimate partner violence are more likely to report maternal depression, thoughts of self-harm, and smoking (Dahlen et al., 2018). Due to this constellation of effects, these pregnant women are more likely to be admitted for preterm labor (Dahlen et al., 2018). Prematurity is a major risk factor for adverse neurodevelopmental outcomes. In comparison, there is little evidence to support the effects of disaster on premature birth (Harville et al., 2010). On the other hand, disasters, by definition, are collectively experienced events, accidental exposures, and acute stressors (McFarlane & Norris, 2006). Although natural disasters are promising quasi-experimental designs where we can point the day it happened, post-disaster stressors have lingering effects. Furthermore, the magnitude of the effects varies as a function of unique issues experienced by the women (i.e., education and socioeconomic status), and characteristics of the environment (i.e., disaster preparedness and community support).
As noted above, human studies do not allow us to fully understand the unique effects of PTE on childhood outcomes. Animal studies provide a valuable opportunity to control both the timing and severity of prenatal stress exposure and to better understand its mechanisms and specific impact. Even among the adequately controlled studies, many scored lower in methodological quality due to few control variables and exclusion criteria, lack of multiple methods to assess temperament (e.g., two reporters, maternal report, and observational data), and only relying on maternal self-report measures to assess her PTE or psychological symptoms. Additionally, the timing of PTE assessment or mental health screening differed between studies. As such, we lack a robust and replicated evidence base to note how the specific timing of an event, and the impact on the mother, can systematically shape child temperament. Thus, the available data are suggestive of broader patterns of socioemotional functioning. In addition, the pattern and specific instruments of assessment differed with the category of PTE examined. We observed that in prenatal intimate partner violence stress, some studies assessed the experience after the baby’s birth, while in prenatal disaster related stress exposure was assessed at five to seven months after the disaster. As a systematic error, recall bias can decrease or increase the strength of associations.
Strengths, limitations, and research directions
One of the main strengths of this systematic review is that it builds on the methodological quality and characteristics of the individual research designs. Studies included women from varied and diverse countries, including the United States, England, Canada, Israel (Gaza), and Australia. Mothers were from many ethnicities and races (Buthmann et al., 2019; Martinez-Torteya et al., 2018; Miller-Graff & Scheid, 2020; Nomura et al., 2019; Zhang et al., 2018) and sociodemographic backgrounds (Martinez-Torteya et al., 2018; Miller-Graff & Scheid, 2020; Nomura et al., 2019; Quinlivan & Evans, 2005; Tees et al., 2010).
However, most studies were self-contained and specific to one specific pool of recruited participants. Multisite studies were scarce. The types of PTEs examined were also limited. Despite predicted relations that would have been of interest, we found no studies exploring the effects of prenatal bereavement, systemic violence, or pandemics on child temperament. With respect to our approach to the study, limitations include the fact that we did not register the protocol prospectively and studies were from only two databases.
Several additional steps would be needed in order to better understand the relations noted here. Distinguishing types of maternal adversity following the framework from McLaughlin and colleagues to separate threat and deprivation exposures during pregnancy is necessary (McLaughlin et al., 2014). Among the intimate partner violence studies, few divided prenatal intimate partner violence exposures into emotional intimate partner violence and physical intimate partner violence. Among the disaster studies, findings used the cumulative risk score or a general exposure metric, which hindered our ability to examine the type (e.g., food deprivation vs fear of death), chronicity (during and/or after the disaster), or severity of the adversity.
Furthermore, a meta-analysis could compare perinatal mood and PTEs to explore their unique effects on child temperament. However, there would be an imbalance in the evidence base as most studies have focused on prenatal depression and anxiety as unique sources of adverse prenatal and postnatal exposure with community samples (Madigan et al., 2018). Well-designed randomized control trials, carefully noting the timing, type, and severity of exposure could be used to assess the impact on child outcomes as well as explore if a psychological intervention targeting the maternal stress response can reduce the evident negative effects on child socioemotional functioning.
Conclusions
In conclusion, there is evidence supporting the associations between prenatal PTE and child temperament, particularly increased levels of negative affectivity, and decreased levels of effortful control/regulation. This evidence arises mostly from prospective cohort studies relying on self-reported measures. PTEs, such as disasters and intimate partner violence, may increase maternal distress during pregnancy, which in turn has an impact on the fetal development of the offspring, including brain structures associated with HPA axis activity. These relations are also noted in neural development. For example, high negative affect is associated with alterations in amygdala activity and connectivity (Kann et al., 2017). Thus, the review shows that exposure to stress during the prenatal period can result in changes in early indicators for socio-emotional development, such as temperament. Future work can build on these largely observational studies to examine potential mechanisms and points of intervention or prevention.
Funding sources:
The project described was supported by the National Institutes of Health: Awards Number HCTRECD R25MD007607 and R21MD013652 from the National Institute on Minority Health and Health Disparities. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Minority Health and Health Disparities or the National Institutes of Health. The authors have no conflicts of interest relevant to this article to disclose.
Footnotes
Financial Disclosures: The authors have no conflict of interest to disclose.
Ethic statement: This manuscript in not published elsewhere.
References
- Accortt EE, Cheadle ACD, & Dunkel Schetter C (2015). Prenatal Depression and Adverse Birth Outcomes: An Updated Systematic Review. Maternal and Child Health Journal, 19(6), 1306–1337. 10.1007/s10995-014-1637-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahlfs-Dunn SM, & Huth-Bocks AC (2014). Intimate partner violence and infant socioemotional development: the moderating effects of maternal trauma symptoms. Infant Mental Health Journal, 35(4), 322–335. http://10.0.3.234/imhj.21453 [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association, (APA). (2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed.). American Psychiatric Association. [Google Scholar]
- Austin M-P, Hadzi-Pavlovic D, Leader L, Saint K, & Parker G (2005). Maternal trait anxiety, depression and life event stress in pregnancy: relationships with infant temperament. Early Human Development, 81(2), 183–190. 10.1016/j.earlhumdev.2004.07.001 [DOI] [PubMed] [Google Scholar]
- Baibazarova E, van de Beek C, Cohen-Kettenis PT, Buitelaar J, Shelton KH, & van Goozen SHM (2013). Influence of prenatal maternal stress, maternal plasma cortisol and cortisol in the amniotic fluid on birth outcomes and child temperament at 3 months. Psychoneuroendocrinology, 38(6), 907–915. 10.1016/j.psyneuen.2012.09.015 [DOI] [PubMed] [Google Scholar]
- Barker DJP (2007). The origins of the developmental origins theory. Journal of Internal Medicine, 261(5), 412–417. 10.1111/j.1365-2796.2007.01809.x [DOI] [PubMed] [Google Scholar]
- Barker ED (2013). The duration and timing of maternal depression as a moderator of the relationship between dependent interpersonal stress, contextual risk and early child dysregulation. Psychological Medicine, 43(8), 1587–1596. 10.1017/S0033291712002450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beekman C, Neiderhiser JM, Buss KA, Loken E, Moore GA, Leve LD, Ganiban JM, Shaw DS, & Reiss D (2015). The Development of Early Profiles of Temperament: Characterization, Continuity, and Etiology. Child Development, 86(6), 1794–1811. 10.1111/cdev.12417 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blaisdell KN, Imhof AM, & Fisher PA (2019). Early adversity, child neglect, and stress neurobiology: From observations of impact to empirical evaluations of mechanisms. International Journal of Developmental Neuroscience, 78(1), 139–146. 10.1016/j.ijdevneu.2019.06.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanchard EB, Jones-Alexander J, Buckley TC, & Forneris CA (1996). Psychometric properties of the PTSD checklist (PCL). Behaviour Research and Therapy, 34(8), 669–673. 10.1016/0005-7967(96)00033-2 [DOI] [PubMed] [Google Scholar]
- Brand SR, Engel SM, Canfield RL, & Yehuda R (2006). The effect of maternal PTSD following in utero trauma exposure on behavior and temperament in the 9-month-old infant. Annals of the New York Academy of Sciences, 1071, 454–458. 10.1196/annals.1364.041 [DOI] [PubMed] [Google Scholar]
- Burke JG, Lee LC, & O’Campo P (2008). An exploration of maternal intimate partner violence experiences and infant general health and temperament. Maternal and Child Health Journal, 12(2), 172–179. 10.1007/s10995-007-0218-z [DOI] [PubMed] [Google Scholar]
- Buthmann J, Ham J, Davey K, Finik J, Dana K, Pehme P, Zhang W, Glover V, & Nomura Y (2019). Infant Temperament: Repercussions of Superstorm Sandy-Related Maternal Stress. Child Psychiatry & Human Development, 50(1), 150–162. 10.1007/s10578-018-0828-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chisholm CA, Bullock L, & Ferguson JE (2017). Intimate partner violence and pregnancy: epidemiology and impact. American Journal of Obstetrics and Gynecology, 217(2), 141–144. 10.1016/j.ajog.2017.05.042 [DOI] [PubMed] [Google Scholar]
- Dahlen HG, Munoz AM, Schmied V, & Thornton C (2018). The relationship between intimate partner violence reported at the first antenatal booking visit and obstetric and perinatal outcomes in an ethnically diverse group of Australian pregnant women: a population-based study over 10 years. BMJ Open, 8(4), e019566. 10.1136/bmjopen-2017-019566 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis EP, Glynn LM, Schetter CD, Hobel C, Chicz-Demet A, & Sandman CA (2007). Prenatal exposure to maternal depression and cortisol influences infant temperament. Journal of the American Academy of Child and Adolescent Psychiatry, 46(6), 737–746. 10.1097/chi.0b013e318047b775 [DOI] [PubMed] [Google Scholar]
- Deshpande NA, Kucirka LM, Smith RN, & Oxford CM (2017). Pregnant trauma victims experience nearly 2-fold higher mortality compared to their nonpregnant counterparts. American Journal of Obstetrics and Gynecology, 217(5), 590.e1–590.e9. 10.1016/j.ajog.2017.08.004 [DOI] [PubMed] [Google Scholar]
- Diab SY, Isosävi S, Qouta SR, Kuittinen S, & Punamäki R-L (2018). The protective role of maternal post-traumatic growth and cognitive trauma processing in Palestinian mothers and infants: a longitudinal study. Lancet, 391, S39–S39. http://10.0.3.248/S0140-6736(18)30405-7 [DOI] [PubMed] [Google Scholar]
- Downes MJ, Brennan ML, Williams HC, & Dean RS (2016). Development of a critical appraisal tool to assess the quality of cross-sectional studies (AXIS). BMJ Open, 6(12), e011458. 10.1136/bmjopen-2016-011458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erickson NL, Gartstein MA, & Dotson JAW (2017). Review of Prenatal Maternal Mental Health and the Development of Infant Temperament. JOGNN - Journal of Obstetric, Gynecologic, and Neonatal Nursing, 46(4), 588–600. 10.1016/j.jogn.2017.03.008 [DOI] [PubMed] [Google Scholar]
- Gartland D, Woolhouse H, Giallo R, McDonald E, Hegarty K, Mensah F, Herrman H, & Brown SJ (2016). Vulnerability to intimate partner violence and poor mental health in the first 4-year postpartum among mothers reporting childhood abuse: an Australian pregnancy cohort study. Archives of Women’s Mental Health, 19(6), 1091–1100. 10.1007/s00737-016-0659-8 [DOI] [PubMed] [Google Scholar]
- Gartstein MA, & Rothbart MK (2003). Studying infant temperament via the Revised Infant Behavior Questionnaire. Infant Behavior and Development, 26(1), 64–86. 10.1016/S0163-6383(02)00169-8 [DOI] [Google Scholar]
- Gartstein MA, & Skinner MK (2018). Prenatal influences on temperament development: The role of environmental epigenetics. Development and Psychopathology, 30(4), 1269–1303. 10.1017/s0954579417001730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibson C, Callands TA, Magriples U, Divney A, & Kershaw T (2015). Intimate partner violence, power, and equity among adolescent parents: Relation to child outcomes and parenting. Maternal and Child Health Journal, 19(1), 188–195. 10.1007/s10995-014-1509-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gluckman PD, Hanson MA, Cooper C, & Thornburg KL (2008). Effect of In Utero and Early-Life Conditions on Adult Health and Disease. New England Journal of Medicine, 359(1), 61–73. 10.1056/NEJMra0708473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harville EW, Xiong X, & Buekens P (2010). Disasters and Perinatal Health: A Systematic Review. Obstetrical & Gynecological Survey, 65(11), 713–728. 10.1097/OGX.0b013e31820eddbe [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harville EW, Xiong X, Pridjian G, Elkind-Hirsch K, & Buekens P (2009). Postpartum mental health after Hurricane Katrina: A cohort study. BMC Pregnancy and Childbirth, 9, 1–8. 10.1186/1471-2393-9-21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haselbeck C, Niederberger U, Kulle A, Wache K, Brauner E, Gutermuth M, Holterhus P-M, Gerber W-D, & Siniatchkin M (2017). Prenatal maternal distress seems to be associated with the infant’s temperament and motor development: An explorative study. Journal of Neural Transmission, 124(7), 881–890. 10.1007/s00702-017-1712-0 [DOI] [PubMed] [Google Scholar]
- Isosävi S, Diab SY, Kangaslampi S, Qouta S, Kankaanpää S, Puura K, & Punamäki R-L (2017). Maternal trauma affects prenatal mental health and infant stress regulation among palestinian dyads. Infant Mental Health Journal, 38(5), 617–633. 10.1002/imhj.21658 [DOI] [PubMed] [Google Scholar]
- Kann SJ, O’Rawe JF, Huang AS, Klein DN, & Leung H-C (2017). Preschool negative emotionality predicts activity and connectivity of the fusiform face area and amygdala in later childhood. Social Cognitive and Affective Neuroscience, 12(9), 1511–1519. 10.1093/scan/nsx079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kastello JC, Jacobsen KH, Gaffney KF, Kodadek MP, Bullock LC, & Sharps PW (2016). Posttraumatic stress disorder among low-income women exposed to perinatal intimate partner violence: Posttraumatic stress disorder among women exposed to partner violence. Archives of Women’s Mental Health, 19(3), 521–528. 10.1007/s00737-015-0594-0 [DOI] [PubMed] [Google Scholar]
- Kastello JC, Jacobsen KH, Gaffney KF, Kodadek MP, Sharps PW, & Bullock LC (2016). Predictors of Depression Symptoms Among Low-Income Women Exposed to Perinatal Intimate Partner Violence (IPV). Community Mental Health Journal, 52(6), 683–690. 10.1007/s10597-015-9977-y [DOI] [PubMed] [Google Scholar]
- Kessler RC, Aguilar-Gaxiola S, Alonso J, Benjet C, Bromet EJ, Cardoso G, Degenhardt L, de Girolamo G, Dinolova RV, Ferry F, Florescu S, Gureje O, Haro JM, Huang Y, Karam EG, Kawakami N, Lee S, Lepine J-P, Levinson D, … Koenen KC (2017). Trauma and PTSD in the WHO World Mental Health Surveys. European Journal of Psychotraumatology, 8(sup5), 1353383. 10.1080/20008198.2017.1353383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- King S, Dancause K, Turcotte-Tremblay AM, Veru F, & Laplante DP (2012). Using Natural Disasters to Study the Effects of Prenatal Maternal Stress on Child Health and Development. Birth Defects Research Part C - Embryo Today: Reviews, 96(4), 273–288. 10.1002/bdrc.21026 [DOI] [PubMed] [Google Scholar]
- King S, & Laplante DP (2005). The effects of prenatal maternal stress on children’s cognitive development: Project Ice Storm. Stress: The International Journal on the Biology of Stress, 8(1), 35–45. 10.1080/10253890500108391 [DOI] [PubMed] [Google Scholar]
- Korja R, Nolvi S, Grant KA, & McMahon C (2017). The Relations Between Maternal Prenatal Anxiety or Stress and Child’s Early Negative Reactivity or Self-Regulation: A Systematic Review. Child Psychiatry & Human Development, 48(6), 851–869. 10.1007/s10578-017-0709-0 [DOI] [PubMed] [Google Scholar]
- Laplante DP, Brunet A, & King S (2016). The effects of maternal stress and illness during pregnancy on infant temperament: Project Ice Storm. Pediatric Research, 79(1), 107–113. 10.1038/pr.2015.177 [DOI] [PubMed] [Google Scholar]
- LeDoux JE, & Pine DS (2016). Using neuroscience to help understand fear and anxiety: A two-system framework. American Journal of Psychiatry, 173(11), 1083–1093. 10.1176/appi.ajp.2016.16030353 [DOI] [PubMed] [Google Scholar]
- Levey EJ, Gelaye B, Koenen K, Zhong Q-Y, Basu A, Rondon MB, Sanchez S, Henderson DC, & Williams MA (2018). Trauma exposure and post-traumatic stress disorder in a cohort of pregnant Peruvian women. Archives of Women’s Mental Health, 21(2), 193–202. 10.1007/s00737-017-0776-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin B, Ostlund BD, Conradt E, Lagasse LL, & Lester BM (2018). Testing the programming of temperament and psychopathology in two independent samples of children with prenatal substance exposure. Development and Psychopathology, 30(3), 1023–1040. 10.1017/S0954579418000391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Locke RL, Lagasse LL, Seifer R, Lester BM, Shankaran S, Bada HS, & Bauer CR (2016). Effects of prenatal substance exposure on infant temperament vary by context. Development and Psychopathology, 28(2), 309–326. 10.1017/S0954579415000504 [DOI] [PubMed] [Google Scholar]
- Madigan S, Oatley H, Racine N, Fearon RMP, Schumacher L, Akbari E, Cooke JE, & Tarabulsy GM (2018). A Meta-Analysis of Maternal Prenatal Depression and Anxiety on Child Socioemotional Development. Journal of the American Academy of Child and Adolescent Psychiatry, 57(9), 645. 10.1016/j.jaac.2018.06.012 [DOI] [PubMed] [Google Scholar]
- Martinez-Torteya C, Figge CJ, Gilchrist MA, Muzik M, King AP, & Sorenson M (2018). Prenatal intimate partner violence exposure predicts infant biobehavioral regulation: Moderation by the brain-derived neurotrophic factor (BDNF) gene. Development and Psychopathology, 30(3), 1009–1021. 10.1017/S0954579418000329 [DOI] [PubMed] [Google Scholar]
- McFarlane AC, & Norris FH (2006). Definitions and Concepts in Disaster Research. In Norris FH, Galea S, Friedman MJ, & Watson PJ (Eds.), Methods for Disaster Mental Health Research (pp. 3–19). Guilford Press. [Google Scholar]
- McGowan PO, & Matthews SG (2018). Prenatal stress, glucocorticoids, and developmental programming of the stress response. Endocrinology, 159(1), 69–82. 10.1210/en.2017-00896 [DOI] [PubMed] [Google Scholar]
- McLaughlin KA, Sheridan MA, & Lambert HK (2014). Childhood adversity and neural development: Deprivation and threat as distinct dimensions of early experience. Neuroscience & Biobehavioral Reviews, 47, 578–591. 10.1016/j.neubiorev.2014.10.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, Weissman D, & Bitrán D (2019). Childhood Adversity and Neural Development: A Systematic Review. Annual Review of Developmental Psychology, 1(1), 277–312. 10.1146/annurev-devpsych-121318-084950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLean MA, Cobham VE, Simcock G, Kildea S, & King S (2019). Toddler Temperament Mediates the Effect of Prenatal Maternal Stress on Childhood Anxiety Symptomatology: The QF2011 Queensland Flood Study. International Journal of Environmental Research and Public Health, 16(11). 10.3390/ijerph16111998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMahon S, Huang C-C, Boxer P, & Postmus JL (2011). The impact of emotional and physical violence during pregnancy on maternal and child health at one year post-partum. Children and Youth Services Review, 33(11), 2103–2111. 10.1016/j.childyouth.2011.06.001 [DOI] [Google Scholar]
- Miller-Graff L, & Cheng P (2017). Consequences of violence across the lifespan: Mental health and sleep quality in pregnant women. Psychological Trauma: Theory, Research, Practice, and Policy, 9(5), 587–595. 10.1037/tra0000252 [DOI] [PubMed] [Google Scholar]
- Miller-Graff L, & Scheid CR (2019). Breastfeeding continuation at 6 weeks postpartum remediates the negative effects of prenatal intimate partner violence on infant temperament. Development and Psychopathology. 10.1017/S0954579419000245 [DOI] [PubMed] [Google Scholar]
- Miller-Graff L, & Scheid CR (2020). Breastfeeding continuation at 6 weeks postpartum remediates the negative effects of prenatal intimate partner violence on infant temperament. Development and Psychopathology, 32(2), 503–510. 10.1017/S0954579419000245 [DOI] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, & Altman DG (2009). Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Medicine, 6(7), e1000097. 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA, Estarli M, Barrera ESA, Martínez-Rodríguez R, Baladia E, Agüero SD, Camacho S, Buhring K, Herrero-López A, Gil-González DM, Altman DG, Booth A, … Whitlock E (2015). Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Systematic Review, 4(1), 148–160. 10.1186/2046-4053-4-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray L, & Carothers AD (1990). The Validation of the Edinburgh Post-natal Depression Scale on a Community Sample. British Journal of Psychiatry, 157(2), 288–290. 10.1192/bjp.157.2.288 [DOI] [PubMed] [Google Scholar]
- Murugan V, Holzer KJ, Termos M, & Vaughn M (2020). Intimate partner violence among pregnant women reporting to the emergency department: findings from a nationwide sample. BMJ Sexual & Reproductive Health, bmjsrh-2020-200761. 10.1136/bmjsrh-2020-200761 [DOI] [PubMed] [Google Scholar]
- Nolvi S, Karlsson L, Bridgett DJ, Korja R, Huizink AC, Kataja E-L, & Karlsson H (2016). Maternal prenatal stress and infant emotional reactivity six months postpartum. Journal of Affective Disorders, 199, 163–170. 10.1016/j.jad.2016.04.020 [DOI] [PubMed] [Google Scholar]
- Nomura Y, Davey K, Pehme PM, Finik J, Glover V, Zhang W, Huang Y, Buthmann J, Dana K, Yoshida S, Tsuchiya KJ, Li XB, & Ham J (2019). Influence of in utero exposure to maternal depression and natural disaster-related stress on infant temperament at 6 months: The children of Superstorm Sandy. Infant Mental Health Journal, 40(2), 204–216. 10.1002/imhj.21766 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ostlund BD, Pérez-Edgar K, Shisler S, Terrell S, Godleski S, Shuetze P, & Das Eiden R. (n.d.). Prenatal substance exposure and maternal hostility from pregnancy to toddlerhood: Associations with temperament profiles at 16-months of age. Development & Psychopathology. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ostlund BD, Vlisides-Henry RD, Crowell SE, Raby KL, Terrell S, Brown MA, Tinajero R, Shakiba N, Monk C, Shakib JH, Buchi KF, & Conradt E (2019). Intergenerational transmission of emotion dysregulation: Part II. Developmental origins of newborn neurobehavior. Development and Psychopathology, 31(3), 833–846. 10.1017/S0954579419000440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pehme PM, Zhang W, Finik J, Pritchett A, Buthmann J, Dana K, Hao K, & Nomura Y (2018). Placental MAOA expression mediates prenatal stress effects on temperament in 12-month-olds. Infant & Child Development, 27(4), 1. 10.1002/icd.2094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pérez-Edgar K (2019). Through the Looking Glass: Temperament and Emotion as Separate and Interwoven Constructs. In Handbook of Emotional Development (pp. 139–168). Springer International Publishing. 10.1007/978-3-030-17332-6_7 [DOI] [Google Scholar]
- Perroud N, Rutembesa E, Paoloni-Giacobino A, Mutabaruka J, Mutesa L, Stenz L, Malafosse A, & Karege F (2014). The Tutsi genocide and transgenerational transmission of maternal stress: Epigenetics and biology of the HPA axis. World Journal of Biological Psychiatry, 15(4), 334–345. 10.3109/15622975.2013.866693 [DOI] [PubMed] [Google Scholar]
- Putnam SP, Gartstein MA, & Rothbart MK (2006). Measurement of fine-grained aspects of toddler temperament: The Early Childhood Behavior Questionnaire. Infant Behavior and Development, 29(3), 386–401. 10.1016/j.infbeh.2006.01.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qouta S, Punamäki R-L, & El Sarraj E (2005). Mother-Child Expression of Psychological Distress in War Trauma. Clinical Child Psychology and Psychiatry, 10(2), 135–156. 10.1177/1359104505051208 [DOI] [Google Scholar]
- Quinlivan JA, & Evans SF (2005). Impact of domestic violence and drug abuse in pregnancy on maternal attachment and infant temperament in teenage mothers in the setting of best clinical practice. Archives of Women’s Mental Health, 8(3), 191–199. 10.1007/s00737-005-0079-7 [DOI] [PubMed] [Google Scholar]
- Reilly EB, & Gunnar MR (2019). Neglect, HPA axis reactivity, and development. International Journal of Developmental Neuroscience, 78(1), 100–108. 10.1016/j.ijdevneu.2019.07.010 [DOI] [PubMed] [Google Scholar]
- Rothbart MK (1981). Measurement of Temperament in Infancy. Child Development, 52(2), 569. 10.2307/1129176 [DOI] [Google Scholar]
- Rothbart MK (2019). Early Temperament and Psychosocial Development. In Tremblay RE, Boivin M, & RDeV P (Eds.), Encyclopedia on Early Childhood Development [Online] (2nd rev. e). http://www.child-encyclopedia.com/temperament/according-experts/early-temperament-and-psychosocial-development [Google Scholar]
- Rothbart MK, Ahadi SA, Hershey KL, & Fisher P (2001). Investigations of Temperament at Three to Seven Years: The Children’s Behavior Questionnaire. Child Development, 72(5), 1394–1408. 10.1111/1467-8624.00355 [DOI] [PubMed] [Google Scholar]
- Rothbart MK, & Bates JE (2007). Temperament. In Handbook of Child Psychology. John Wiley & Sons, Inc. 10.1002/9780470147658.chpsy0303 [DOI] [Google Scholar]
- Rothbart MK, Evans DE, & Ahadi SA (2000). Temperament and personality: Origins and outcomes. Journal of Personality and Social Psychology, 78(1), 122–135. 10.1037/0022-3514.78.1.122 [DOI] [PubMed] [Google Scholar]
- Schwerdtfeger KL, & Goff BSN (2007). Intergenerational transmission of trauma: Exploring mother–infant prenatal attachment. Journal of Traumatic Stress, 20(1), 39–51. 10.1002/jts.20179 [DOI] [PubMed] [Google Scholar]
- Simcock G, Elgbeili G, Laplante DP, Kildea S, Cobham V, Stapleton H, Austin M-P, Brunet A, & King S (2017). The Effects of Prenatal Maternal Stress on Early Temperament. Journal of Developmental & Behavioral Pediatrics, 38(5), 310–321. 10.1097/DBP.0000000000000444 [DOI] [PubMed] [Google Scholar]
- Straus MA, Hamby SL, Boney-McCoy S, & Sugarman DB (1996). The Revised Conflict Tactics Scales (CTS2). Journal of Family Issues, 17(3), 283–316. 10.1177/019251396017003001 [DOI] [Google Scholar]
- Tees MT, Harville EW, Xiong X, Buekens P, Pridjian G, & Elkind-Hirsch K (2010). Hurricane Katrina-related maternal stress, maternal mental health, and early infant temperament. Maternal and Child Health Journal, 14(4), 511–518. 10.1007/s10995-009-0486-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas A, & Chess S (1989). Temperament and personality. In Kohnstamm GA, & Bates JE, & Rothbart MK (Eds.), Temperament in childhood (pp. 249–261). John Wiley & Sons. [Google Scholar]
- Tung I, Keenan K, Stepp SD, & Hipwell AE (2020). The moderating effects of traumatic stress on vulnerability to emotional distress during pregnancy. Development and Psychopathology, 32(2), 673–686. 10.1017/S0954579419000531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van den Bergh BRH, van den Heuvel MI, Lahti M, Braeken M, de Rooij SR, Entringer S, Hoyer D, Roseboom T, Räikkönen K, King S, & Schwab M (2017). Prenatal developmental origins of behavior and mental health: The influence of maternal stress in pregnancy. Neuroscience and Biobehavioral Reviews, April. 10.1016/j.neubiorev.2017.07.003 [DOI] [PubMed] [Google Scholar]
- Vänskä M, Diab SY, Perko K, Quota SR, Albarqouni NMA, Myöhänen A, Punamäki R-L, & Manduca P (2019). Toxic environment of war: Maternal prenatal heavy metal load predicts infant emotional development. Infant Behavior & Development, 55, 1–9. 10.1016/j.infbeh.2019.01.002 [DOI] [PubMed] [Google Scholar]
- Vijayakumar N, Op de Macks Z, Shirtcliff EA, & Pfeifer JH (2018). Puberty and the human brain: Insights into adolescent development. Neuroscience & Biobehavioral Reviews, 92, 417–436. 10.1016/j.neubiorev.2018.06.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Werner E, Zhao Y, Evans L, Kinsella M, Kurzius L, Altincatal A, McDonough L, & Monk C (2013). Higher maternal prenatal cortisol and younger age predict greater infant reactivity to novelty at 4 months: an observation-based study. Developmental Psychobiology, 55(7), 707–718. 10.1002/dev.21066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yehuda R, Daskalakis NP, Bierer LM, Bader HN, Klengel T, Holsboer F, & Binder EB (2016). Holocaust Exposure Induced Intergenerational Effects on FKBP5 Methylation. Biological Psychiatry, 80(5), 372–380. 10.1016/j.biopsych.2015.08.005 [DOI] [PubMed] [Google Scholar]
- Zhang W, Rajendran K, Ham J, Finik J, Buthmann J, Davey K, Pehme PM, Dana K, Pritchett A, Laws H, & Nomura Y (2018). Prenatal exposure to disaster-related traumatic stress and developmental trajectories of temperament in early childhood: Superstorm Sandy pregnancy study. Journal of Affective Disorders, 234, 335–345. 10.1016/j.jad.2018.02.067 [DOI] [PMC free article] [PubMed] [Google Scholar]