Abstract
Background
Childhood vaccination is one of the most effective ways to prevent serious illnesses and deaths in children. However, worldwide, many children do not receive all recommended vaccinations, for several potential reasons. Vaccines might be unavailable, or parents may experience difficulties in accessing vaccination services; for instance, because of poor quality health services, distance from a health facility, or lack of money. Some parents may not accept available vaccines and vaccination services.
Our understanding of what influences parents’ views and practices around childhood vaccination, and why some parents may not accept vaccines for their children, is still limited.
This synthesis links to Cochrane Reviews of the effectiveness of interventions to improve coverage or uptake of childhood vaccination.
Objectives
‐ Explore parents’ and informal caregivers’ views and practices regarding routine childhood vaccination, and the factors influencing acceptance, hesitancy, or nonacceptance of routine childhood vaccination.
‐ Develop a conceptual understanding of what and how different factors reduce parental acceptance of routine childhood vaccination.
‐ Explore how the findings of this review can enhance our understanding of the related Cochrane Reviews of intervention effectiveness.
Search methods
We searched MEDLINE, Embase, CINAHL, and three other databases for eligible studies from 1974 to June 2020.
Selection criteria
We included studies that: utilised qualitative methods for data collection and analysis; focused on parents’ or caregivers’ views, practices, acceptance, hesitancy, or refusal of routine vaccination for children aged up to six years; and were from any setting globally where childhood vaccination is provided.
Data collection and analysis
We used a pre‐specified sampling frame to sample from eligible studies, aiming to capture studies that were conceptually rich, relevant to the review's phenomenon of interest, from diverse geographical settings, and from a range of income‐level settings. We extracted contextual and methodological data from each sampled study. We used a meta‐ethnographic approach to analyse and synthesise the evidence. We assessed methodological limitations using a list of criteria used in previous Cochrane Reviews and originally based on the Critical Appraisal Skills Programme quality assessment tool for qualitative studies. We used the GRADE‐CERQual (Confidence in the Evidence from Reviews of Qualitative research) approach to assess our confidence in each finding. We integrated the findings of this review with those from relevant Cochrane Reviews of intervention effectiveness. We did this by mapping whether the underlying theories or components of trial interventions included in those reviews related to or targeted the overarching factors influencing parental views and practices regarding routine childhood vaccination identified by this review.
Main results
We included 145 studies in the review and sampled 27 of these for our analysis. Six studies were conducted in Africa, seven in the Americas, four in South‐East Asia, nine in Europe, and one in the Western Pacific. Studies included urban and rural settings, and high‐, middle‐, and low‐income settings.
Many complex factors were found to influence parents’ vaccination views and practices, which we divided into four themes.
Firstly, parents’ vaccination ideas and practices may be influenced by their broader ideas and practices surrounding health and illness generally, and specifically with regards to their children, and their perceptions of the role of vaccination within this context. Secondly, many parents’ vaccination ideas and practices were influenced by the vaccination ideas and practices of the people they mix with socially. At the same time, shared vaccination ideas and practices helped some parents establish social relationships, which in turn strengthened their views and practices around vaccination. Thirdly, parents' vaccination ideas and practices may be influenced by wider political issues and concerns, and particularly their trust (or distrust) in those associated with vaccination programmes. Finally, parents' vaccination ideas and practices may be influenced by their access to and experiences of vaccination services and their frontline healthcare workers.
We developed two concepts for understanding possible pathways to reduced acceptance of childhood vaccination.
The first concept, ‘neoliberal logic’, suggests that many parents, particularly from high‐income countries, understood health and healthcare decisions as matters of individual risk, choice, and responsibility. Some parents experienced this understanding as in conflict with vaccination programmes, which emphasise generalised risk and population health. This perceived conflict led some parents to be less accepting of vaccination for their children.
The second concept, ‘social exclusion’, suggests that some parents, particularly from low‐ and middle‐income countries, were less accepting of childhood vaccination due to their experiences of social exclusion. Social exclusion may damage trustful relationships between government and the public, generate feelings of isolation and resentment, and give rise to demotivation in the face of public services that are poor quality and difficult to access. These factors in turn led some parents who were socially excluded to distrust vaccination, to refuse vaccination as a form of resistance or a way to bring about change, or to avoid vaccination due to the time, costs, and distress it creates.
Many of the overarching factors our review identified as influencing parents' vaccination views and practices were underrepresented in the interventions tested in the four related Cochrane Reviews of intervention effectiveness.
Authors' conclusions
Our review has revealed that parents’ views and practices regarding childhood vaccination are complex and dynamic social processes that reflect multiple webs of influence, meaning, and logic. We have provided a theorised understanding of the social processes contributing to vaccination acceptance (or not), thereby complementing but also extending more individualistic models of vaccination acceptance. Successful development of interventions to promote acceptance and uptake of childhood vaccination will require an understanding of, and then tailoring to, the specific factors influencing vaccination views and practices of the group(s) in the target setting. The themes and concepts developed through our review could serve as a basis for gaining this understanding, and subsequent development of interventions that are potentially more aligned with the norms, expectations, and concerns of target users.
Plain language summary
What factors influence parents’ views and practices around routine childhood vaccines?
Review aim
This Cochrane synthesis of qualitative evidence aimed to explore the factors that influence parents’ views and practices around routine childhood vaccines. To do this, we searched for and analysed qualitative studies of parents’ views, experiences, and practices.
This synthesis complements other Cochrane Reviews assessing the effect of strategies to improve the uptake of childhood vaccination.
Key messages
Many factors influence parents’ vaccination views and practices, including those related to individual perceptions, social relationships, and the wider context in which parents live. When parents make decisions about vaccination for their children, they are often communicating not just what they think about vaccines, but also who they are, what they value, and with whom they identify.
What was studied in this synthesis?
Childhood vaccination is one of the most effective ways to prevent serious illnesses and deaths in children. However, worldwide, many children do not receive all recommended vaccinations. There are several potential reasons for this. Vaccines might be unavailable, or parents may experience difficulties in accessing vaccination services. Some parents may not accept available vaccines and vaccination services.
Our understanding of what influences parents’ views and practices around childhood vaccination, and why some parents may not accept vaccines for their children is still limited. Qualitative research explores how people perceive and experience the world around them, and is therefore well‐placed for examining these issues.
What are the main findings of the review?
We included 27 studies in our analysis. Studies were conducted in Africa, the Americas, South‐East Asia, Europe, and the Western Pacific, and included urban and rural settings, as well as high‐, middle‐, and low‐income settings.
Many complex factors were found to influence parents’ vaccination views and practices, which we divided into four themes.
Firstly, parents’ vaccination ideas and practices may be influenced by their broader ideas and practices surrounding health and illness generally, and specifically with regards to their children, and their perceptions of the role of vaccination within this context. Secondly, many parents’ vaccination ideas and practices were influenced by the vaccination ideas and practices of the people they mix with socially. At the same time, shared vaccination ideas and practices helped some parents establish social relationships, which in turned strengthened their views and practices around vaccination. Thirdly, parent’s vaccination ideas and practices may be influenced by wider political issues and concerns, and particularly their trust (or distrust) in those associated with vaccination programmes. Finally, parent’s vaccination ideas and practices may be influenced by their access to and experiences of vaccination services and their frontline healthcare workers.
We developed two concepts for understanding possible pathways to reduced acceptance of childhood vaccination.
The first concept, ‘neoliberal logic’, suggests that many parents, particularly from high‐income countries, understood health and healthcare decisions as matters of individual risk, choice, and responsibility. Some parents experienced this understanding as in conflict with vaccination programmes, which emphasise generalised risk and population health. This perceived conflict led some parents to be less accepting of vaccination for their children.
The second concept, ‘social exclusion’, suggests that some parents, particularly from low‐ and middle‐income countries, were less accepting of childhood vaccination due to their experiences of social exclusion. Social exclusion may damage trustful relationships between government and the public, generate feelings of isolation and resentment, and give rise to demotivation in the face of public services that are poor quality and difficult to access. These factors in turn led some parents who were socially excluded to distrust vaccination, to refuse vaccination as a form of resistance or a way to bring about change, or to avoid vaccination due to the time, costs, and distress it creates.
How up‐to‐date is this review?
We searched for studies published before 3 June 2020.
Summary of findings
Summary of findings 1. Summary of qualitative findings (SoQF) table.
| Summary of review findings | Studies contributing to the review finding | GRADE‐CERQual assessment of confidence in the evidence | Explanation of GRADE‐CERQual assessment |
|
Theme 1: ideas and practices surrounding (child) health and illness | |||
| Finding 1: religious beliefs. Some parents were less accepting of childhood vaccination due to the religious beliefs they held, and the view that illness, including in children, can only be prevented by divine providence. These parents expressed religious objections to vaccination. | Renne 2010; Reich 2016 | Low confidence | Finding downgraded because of serious concerns about adequacy, moderate concerns about relevance (partial relevance), and minor concerns about methodological limitations |
| Finding 2: the ‘fragile’ infant. An understanding of infants and their immune systems as fragile and still in a state of development was common amongst parents across diverse settings, contexts, and population groups. Numerous parents characterised infants and young children as weak and vulnerable, and in need of protection against multiple social, biological, or spiritual threats. This perception was associated with both reduced and increased acceptance of childhood vaccination. | Bisht 2000; Brownlie 2005; Poltorak 2005; Millimouno 2006; Casiday 2007; Leach 2007; Brunson 2013; McKnight 2014; Giles‐Vernick 2016; Reich 2016; Smith 2017; Limaye 2020 | High confidence | |
| Finding 3: primacy of ‘nature’ and ‘the natural’. Some parents, predominantly from HICs, were less accepting of childhood vaccination due to their understanding of health and illness as holistic or naturalistic. This understanding conceives many biomedical interventions, including vaccination, as unnatural intrusions that are unnecessary or harmful. Various parents who held this view also engaged in certain ‘natural’ health‐promoting activities or “salutogenic parenting”, which for them further negated the need for vaccination. | Rogers 1995; Brownlie 2005; Poltorak 2005; Casiday 2007; Dube 2016; Reich 2016; Barbieri 2017; Ward 2017; Peretti‐Watel 2019 | High confidence | |
| Finding 4: individualised health, immunity, and vaccine‐response trajectories. Many parents, predominantly from HICs, held a view that children possess unique bodies and immune systems, and therefore individual vaccine needs and vulnerabilities. As such, these parents frequently assessed the risks and benefits of vaccines as they pertain to their specific child, rather than in general. If the risks were seen to outweigh the benefits for their particular child, then these parents tended to be less accepting of childhood vaccination. |
Rogers 1995; Brownlie 2005; Poltorak 2005; Casiday 2007; Brunson 2013; Dube 2016; Reich 2016; Sobo 2016; Barbieri 2017; Smith 2017 |
High confidence | |
| Finding 5: claiming parental expertise. Many parents from HICs held a view of themselves as experts of their child, possessing the best understanding of their child’s health strengths and vulnerabilities. They in turn considered themselves best placed to judge their child’s vaccination needs and risks. |
Petts 2004; Poltorak 2005; Casiday 2007; Brunson 2013; Johnson 2014; Reich 2016; Sobo 2016; Ward 2017; Carrion 2018; Peretti‐Watel 2019 |
Moderate confidence | Finding downgraded because of moderate concerns about coherence (contradictory data), and minor concerns about relevance (partial relevance) and methodological limitations |
| Finding 6: personal choice and responsibility. Many parents, predominantly from HICs, perceived healthcare decision‐making, including vaccination, to be a matter of personal responsibility and choice. In cases where the risks of a vaccine or vaccination in general were thought to outweigh the benefits for their particular child, then these values of personal responsibility and choice were often prioritised over collective responsibility. These parents in turn tended to be less accepting of vaccination for their children. | Rogers 1995; Petts 2004; Brownlie 2005; Poltorak 2005; Casiday 2007; Brunson 2013; Johnson 2014; Reich 2016; Sobo 2016; Barbieri 2017; Ward 2017; Carrion 2018 | High confidence | |
|
Theme 2: social communities and networks | |||
| Finding 7: social networks shape vaccination ideas and practices. Parents' vaccination views and practices, across diverse settings, contexts, and population groups, were influenced by the vaccination views and experiences of their social networks. These networks included relatives, peers, neighbours, and additional significant others in the community. However, the views and practices of other parents, and particularly other mothers, were especially influential. | Petts 2004; Brownlie 2005; Poltorak 2005; Millimouno 2006; Casiday 2007; Leach 2007; Ruijs 2012; Brunson 2013; Varghese 2013; Johnson 2014; Dube 2016; Giles‐Vernick 2016; Sobo 2016; Barbieri 2017; Ward 2017; Peretti‐Watel 2019 | High confidence | |
| Finding 8: vaccination ideas and practices shape social networks. Parents' vaccination views and practices also shaped their social networks. Shared vaccination ideas and practices were a powerful force in building social relations and ties. While this phenomenon occurred amongst parents across the spectrum of vaccination attitudes, it may be particularly significant for parents who are less accepting of vaccination. In these cases, parents may be afforded access to various types of social resources, in turn potentially reinforcing both their group affiliation and vaccination views and practices. | Poltorak 2005; Millimouno 2006; Leach 2007; Ward 2017; Reich 2016 | Moderate confidence | Finding downgraded because of moderate concerns about adequacy and about coherence (ambiguous data), and minor concerns about relevance (partial relevance) and methodological limitations |
|
Theme 3: political events, relations and processes | |||
| Finding 9: distrust in the institutions or systems implicated with vaccination. Some parents were less accepting of vaccination due to a lack of, or breakdown in, trust in the institutions or systems implicated with vaccination ‐ most particularly government, the pharmaceutical industry, and science. The reasons for this distrust were complex and contextually situated, embedded in political events, relations, and processes within specific times and places. | Rogers 1995; Petts 2004; Brownlie 2005; Poltorak 2005; Casiday 2007; Leach 2007; Chaturvedi 2009; Renne 2010; Varghese 2013; Hussain 2015; Dube 2016; Giles‐Vernick 2016; Reich 2016; Smith 2017; Ward 2017; Carrion 2018; Peretti‐Watel 2019 | Moderate confidence | Finding downgraded due to moderate concerns about coherence (contradictory data), and minor concerns about methodological limitations |
| Finding 10: generalised decline in trust of authority and expert systems. For some parents, distrust of the institutions or systems implicated with vaccination may be part and parcel of a more generalised contemporary trend of decreasing trust in authorities and expert systems. | Brownlie 2005; Poltorak 2005; Casiday 2007; Ward 2017 | Low confidence | Finding downgraded because of serious concerns about relevance (partial relevance), moderate concerns about coherence (contradictory data) and adequacy, and minor concerns about methodological limitations |
| Finding 11: agendas and interests underpinning the expert systems implicated with vaccination. For some parents, distrust of the institutions or systems implicated with vaccination was linked to their concerns about the agendas or interests embedded in these systems. Many of these parents were particularly concerned about the economic interests of these systems, and especially the economic interests of the pharmaceutical industry, which they perceived to be negatively influencing vaccination programmes. | Rogers 1995; Petts 2004; Poltorak 2005; Casiday 2007; Varghese 2013; Dube 2016; Giles‐Vernick 2016; Reich 2016; Ward 2017; Carrion 2018; Peretti‐Watel 2019 |
Moderate confidence |
Finding downgraded because of moderate concerns about relevance (partial relevance), and minor concerns about methodological limitations |
| Finding 12: current and past controversies. Some parents' distrust of the institutions or systems implicated with vaccination was linked to particular ‘scandals’ or ‘controversies’ related to vaccination specifically or health‐related issues more broadly. The occurrence of such scandals, and the manner in which they were perceived to have been handled, caused some parents to feel misled by authorities and to question their legitimacy in protecting the public’s health. | Petts 2004; Brownlie 2005; Poltorak 2005; Casiday 2007; Renne 2010; Hussain 2015 |
Low confidence |
Finding downgraded because of serious concerns about relevance (partial relevance) and coherence (contradictory and ambiguous data), and minor concerns about methodological limitations |
| Finding 13: marginalisation, inadequate public services, and priority misalignment. Some parents' distrust in the institutions or systems implicated with vaccination was linked to their experiences of marginalisation, inadequate public services, or misalignment between their own priorities and those of the state. These experiences undermined trustful and benevolent state‐citizen relations, leading many parents to distrust government and government‐sponsored programs, including vaccination. | Chaturvedi 2009; Renne 2010; Hussain 2015; Smith 2017 |
Moderate confidence |
Finding downgraded because of serious concerns about relevance (partial relevance), and minor concerns about coherence (contradictory data) and methodological limitations |
|
Theme 4: access‐supply‐demand interactions | |||
| Finding 14: socio‐economic challenges in accessing vaccination services. Parents living in resource‐limited settings frequently face numerous socioeconomic challenges to accessing vaccination services, including practical questions of geography and transport, childcare constraints, and family economics and household work pressures. As a result of these challenges, some of these parents were less accepting of vaccination due to the time, effort, and opportunity costs that accessing vaccination involved. | Millimouno 2006; Leach 2007; Dugas 2009; McKnight 2014; Giles‐Vernick 2016; Smith 2017 |
High confidence |
|
| Finding 15: undesirable features of vaccination services and delivery logistics. Some parents were less accepting of vaccination due to undesirable features of vaccination services and delivery logistics. These features, common to vaccination services within resource‐limited settings, included resource constraints that affect vaccine supply and costs and health facility waiting times, and constraining organisational procedures. | Millimouno 2006; Leach 2007; Dugas 2009; McKnight 2014; Giles‐Vernick 2016 |
Moderate confidence |
Finding downgraded because of moderate concerns about relevance (partial relevance), and minor concerns about methodological limitations |
| Finding 16: vaccination as a social event. Vaccination may be a social event where people gather and interact with each other. Some parents found this to a positive experience, whereby they received affirmation about themselves and their children. This potentially motivated attendance at childhood vaccination services. For other parents, the social nature of vaccination services was a negative experience, whereby they felt judged by, disapproved of by, or alienated from others. This potentially demotivated attendance of childhood vaccination services. | Millimouno 2006; Leach 2007 | Low confidence | Finding downgraded because of serious concerns about relevance (partial relevance) and adequacy, and minor concerns about methodological limitations |
| Finding 17: interactions with frontline healthcare workers. Parents' vaccination views and practices, across diverse settings, contexts and population groups, were mediated by the face‐to‐face interactions or personal relations they had with frontline healthcare workers. Some parents were less accepting of vaccination due to mistreatment from healthcare workers, and when they felt the vaccination information provided to them was simplistic and unbalanced. In contrast, some parents were more accepting of vaccination due to positively‐received engagements with healthcare workers, whereby they felt supported, listened to and respected, and whereby healthcare workers shared balanced information and personal stories about themselves as parents. | Brownlie 2005; Poltorak 2005; Millimouno 2006; Casiday 2007; Leach 2007; Dugas 2009; McKnight 2014; Hussain 2015; Dube 2016; Giles‐Vernick 2016; Reich 2016; Sobo 2016; Smith 2017; Ward 2017; Peretti‐Watel 2019; Limaye 2020 |
High confidence |
|
|
Third‐order concepts | |||
| Finding 18: neoliberal logic. Many parents, predominantly from HICs, held a worldview informed by neoliberal discourses. These discourses understand health as individualised, and health‐related risks and decisions as matters of individual choice and responsibility. Furthermore, these discourses suggest that being a ‘good’ and responsible person in the world means consistently assessing one’s own, individual health‐related risks, seeking and questioning evidence about such risks, proactively avoiding and managing such risks, and understanding that one is singularly accountable for the outcomes that ensue. Some parents experienced this worldview as in conflict with vaccination promotion messages, which tend to be informed by other types of discourses. The discourses underpinning vaccination promotion messages frequently emphasise generalised risk and safety statistics, claim that ‘doctor knows best’, ask people to trust authorities and follow what they promote, and advocate for social responsibility and the health of the community. Parents’ perceived tension between the discourses informing their own worldview and those of vaccination promotion messages led some to resist these messages and be less accepting of vaccination. |
Rogers 1995; Petts 2004; Brownlie 2005; Poltorak 2005; Casiday 2007; Brunson 2013; Johnson 2014; Dube 2016; Reich 2016; Sobo 2016; Barbieri 2017; Smith 2017; Ward 2017; Carrion 2018; Peretti‐Watel 2019 |
Moderate confidence |
Finding downgraded because of moderate concerns about coherence (ambiguous data), and minor concerns about methdological limitations |
| Finding 19: social exclusion. Some parents, predominantly from LMICs, were less accepting of childhood vaccination due to their experiences of social exclusion. Social exclusion may involve economic disadvantage, residential segregation, a lack of political representation or power, discrimination and unequal protection of rights, and a myriad of socioeconomic barriers to good quality public services, including vaccination. Social exclusion weakened trustful government‐citizen relations, generated feelings of alienation from, and resentment towards, the state and others, and gave rise to frustration and demotivation in the face of structural challenges. These factors in turn led some parents who are socially excluded to distrust vaccination, to refuse vaccination as a form of resistance or a mechanism to bring about change, or to avoid vaccination due to the time, effort, (opportunity) costs and distress it creates. |
Millimouno 2006; Leach 2007; Chaturvedi 2009; Dugas 2009 Renne 2010; McKnight 2014 Hussain 2015; Giles‐Vernick 2016; Smith 2017 |
Moderate confidence |
Finding downgraded because of moderate concerns about both relevance (partial relevance) and coherence (ambiguous data) |
Background
Vaccination is considered one of the most effective public health interventions for reducing infant and child morbidity and mortality globally (CDC 1999; WHO 2018a). Vaccination programmes have led to the global eradication of smallpox, and large reductions in disability and death from polio, measles, tetanus, rubella, and diphtheria (CDC 1999; Andre 2008). To be successful, vaccination programmes depend on high levels of vaccination uptake. Not only does this provide direct protection for vaccinated individuals, it also induces indirect protection for the overall community ('herd immunity') by slowing transmission of disease (Fine 2011). This in turn decreases the risk of infection amongst those who remain susceptible in the community, and helps prevent disease outbreaks.
In 2016, over 19 million children did not receive the full series of basic vaccinations globally, which resulted in numerous vaccine‐preventable disease outbreaks and child deaths (Feldstein 2017). While low‐ and middle‐income countries (LMICs) bear the largest proportion of under‐vaccinated or non‐vaccinated children (Feldstein 2017), high‐income countries (HICs) are also affected by suboptimal vaccination. National coverage rates in LMICs and many HICs remain below aspirational targets, and have shown only modest progress toward meeting those targets, despite concerted efforts to improve vaccination uptake (Corben 2016; de Figueiredo 2016). National vaccination estimates also mask subnational and subgroup variations, and the low vaccination coverage rates in certain populations (Omer 2009; Scheifele 2014; Hill 2015; Hull 2017).
The reasons for suboptimal childhood vaccination coverage are commonly categorised into ‘supply‐side’ and ‘demand‐side’ issues (Lewin 2011), although the distinction between these terms is not well‐defined in the immunisation literature (Hickler 2017). ‘Supply‐side’ factors tend to relate to the provision of vaccines and vaccination services, including, for example, availability and accessibility of effective vaccines, adequate health systems to support their delivery, and health personnel to administer the vaccines (Lewin 2011; WHO 2013a; WHO 2018a). Several studies, in both HICs and LMICs, have found 'supply‐side' factors to be significant reasons for children not being up‐to‐date with their vaccinations (Rainey 2011; Machingaidze 2013a; Pearce 2015; Nadeau 2016). Studies have also found that interventions that target 'supply‐side' barriers – such as integrating vaccination with other services (Oyo‐Ita 2016), or reducing missed opportunities for vaccination (Jaca 2018) – are effective in improving childhood vaccination coverage.
'Demand‐side' factors generally relate to the recipients of vaccines and vaccination services, including factors such as service‐users' knowledge, understanding, attitudes, beliefs, intentions, decision‐making and behaviours (Lewin 2011; Hickler 2017). In research and policy, more attention has traditionally been placed on 'supply‐side' issues, to the neglect of more 'demand‐related' issues (Hickler 2015; Suk 2015). However, this is changing, with an increased global focus on the demand side of vaccination in recent years (see below: 'Why is it important to do this synthesis?'). Various studies and some reviews have revealed that a growing number of parents are questioning vaccines, seeking alternative vaccination schedules, and deciding to delay or refuse vaccination for their children, both in high‐ and low‐income settings (Larson 2014; Dube 2015; Corben 2016). Yet we currently lack a comprehensive understanding of what, and how, different factors influence parental views and practices regarding routine childhood vaccination, and why some parents may be less accepting of vaccination for their children (Corben 2016; WHO 2018a). Qualitative research can contribute to this understanding and help inform policy and practice, including the development of more relevant, acceptable, and effective interventions to promote public acceptance and uptake of childhood vaccination.
Description of the topic
There is debate in the literature regarding how we should name the fact that some people decide not to vaccinate. Various concepts and definitions have been used, sometimes interchangeably, including: nonacceptance, refusal, hesitancy, confidence, trust, demand, uptake. However, there is agreement in the literature that traditional understandings of individuals and groups as either ‘anti‐’ or ‘pro‐’ vaccines are inadequate. Rather, vaccination views and practices are thought to exist along a continuum, from nonacceptance of all vaccines to active support of all immunisation recommendations (Feemster 2013; Larson 2014; NVAC 2015). Vaccine hesitancy is seen to fall in the middle of this continuum. The World Health Organization (WHO) defines vaccine‐hesitant individuals as: "a heterogeneous group who hold varying degrees of indecision about specific vaccines or vaccination in general. Vaccine hesitant individuals may accept all vaccines but remain concerned about vaccines, some may refuse or delay some vaccines, but accept others; some individuals may refuse all vaccines" (WHO 2014).
There is also agreement in the literature that vaccination views and practices are complex, and influenced by multiple factors that may vary by time, place, and vaccines (Dube 2013; Larson 2014; MacDonald 2015; Corben 2016). Several contrasting theoretical frameworks have been proposed in an attempt to understand these influencing factors. The WHO developed the 'Three C' framework, including axes of confidence (trust in effectiveness and safety of vaccines and the systems that deliver them), complacency (low perceived risk of vaccine‐preventable diseases), and convenience (affordability and access) (WHO 2013b; MacDonald 2015). Betsch and colleagues added two additional items to this framework (calculating and collective responsibility), to encompass cost‐benefit reasoning and concerns for the protection of others (Betsch 2015; Betsch 2018). The ‘C frameworks’ seek to identify the psychological determinants of vaccine acceptance, hesitancy, and refusal, drawing on psychological models of decision‐making behaviour, such as the health belief model (HBM) and the theory of planned behaviour (TPB). In contrast, Peretti‐Watel and colleagues have reformulated the ‘C frameworks’ to incorporate the major structural features of contemporary societies (Peretti‐Watel 2015). Their model conceptualises vaccine hesitancy as a two‐dimensional decision‐making process, that depends on people’s level of commitment to modern society’s risk culture, or “healthism”, and their trust in the authority of healthcare providers and mainstream medicine.
Alternative approaches have drawn on adaptations of ecological models of health behaviour to identify the multiple and interrelated levels of influence impacting on vaccine acceptance, hesitancy, or nonacceptance (Sturm 2005; Callreus 2010; WHO 2013b; Larson 2014). For example, the WHO has developed a 'Vaccine Hesitancy Determinants Matrix', which categorises factors under three domains: contextual influences, including sociocultural and health systems factors; individual and group influences, including those arising from personal perceptions of a vaccine; and vaccine‐ or vaccination‐specific issues, including individual assessments of risks and benefits and the effects of the mode of administration (WHO 2013b; MacDonald 2015).
There is, therefore, no agreed framework for understanding the factors influencing vaccination views and practices. In addition, while current models have provided important insights into what factors potentially influence vaccine acceptance, hesitancy, or nonacceptance, few provide a comprehensive and theoretical understanding of how these factors operate and interact (Cooper 2019). In addition, few existing models are based on empirical qualitative evidence. For example, the WHO’s 'Three C' framework was developed by reviewing existing conceptual models for grouping vaccine hesitancy determinants, and by taking into consideration model complexity, understandability, global applicability, breadth of factors considered, and potential usefulness in informing the development of vaccine hesitancy indicators and survey questions (MacDonald 2015). Similarly, the WHO’s 'Vaccine Hesitancy Determinants Matrix' was derived from determinants identified in a commissioned systematic (quantitative) review of determinants, the collective experience and insights of members of the WHO's Strategic Advisory Group of Experts on Immunisation (SAGE) working group on vaccine hesitancy, and consultation with experts working in the field (Larson 2014; MacDonald 2015). The commissioned systematic review of determinants concluded that "[f]uture consideration of qualitative studies in all regions would help…enhance understanding around decision‐making processes and the ways in which explanatory factors come together to influence vaccination behavior" (Larson 2014).
The research question we aimed to address in this review is: what factors influence parental views and practices regarding routine childhood vaccination, and how do those factors exert influence? In addition to identifying what factors might be most relevant, we also sought to build theory about how different factors come together to reduce acceptance of routine childhood vaccination. This might contribute to the development or refinement of conceptual models of vaccination acceptance, built on a broader evidence‐base and more theoretical in nature.
In this review, we focus on factors that may ‘enhance’ or ‘reduce’ acceptance of vaccination as a way of capturing the continuous, as opposed to categorical nature, of vaccination views and practices. If a study reported factors associated with a specific vaccination stance (e.g. delayed vaccination, nonacceptance, hesitancy, etc.), this was captured by the review findings. We also focused specifically on studies that reported on the views of parents and informal caregivers, and not those of other relevant stakeholders. This is because our intention was to understand the influencing factors considered important by, and meaningful to, vaccine target users themselves. If they reported that others had an influence on their vaccination views and practices, this was captured by the review findings.
Why is it important to do this synthesis?
Currently, there is a large global focus on the demand side of vaccination. Various international working groups have been established to investigate this topic: a working group on vaccine hesitancy within the WHO's SAGE was formed in 2012 (Schuster 2015); a working group on vaccine confidence was established in the National Vaccine Advisory Committee (NVAC) in the USA in 2013 (NVAC 2015); and an informal working group on vaccine demand was initiated in 2015, under the leadership of the United Nations International Children's Emergency Fund (UNICEF) and in collaboration with the WHO (Hickler 2017). In addition, in 2018, the WHO's SAGE indicated that "[d]emand‐related issues like vaccine hesitancy are complex, and subject to multiple influences. The need is pressing to better understand the drivers of and barriers to vaccination uptake and to build national capacities to develop and implement tailored strategies to promote demand for immunisation services" (WHO 2018a). A year later, in 2019, the WHO also identified vaccine hesitancy as one of the ten main threats to global health in 2019 (WHO 2019). This increased focus on the demand side of vaccination is the consequence of several factors, including settings with low or stagnated rates of vaccination (de Figueiredo 2016; Hull 2017); recent global outbreaks of largely eliminated vaccine‐preventable diseases, such as measles, which have been linked to under‐vaccination (Dabbagh 2018; Larson 2018a); concerns about the rise of vaccine hesitancy (Hickler 2015; Lane 2018); more vaccines becoming available; and more diseases becoming the focus of eradication campaigns (WHO 2013a). The COVID‐19 pandemic, and current global roll‐out of COVID‐19 vaccination programmes, has further heightened international concerns about, and focus on, vaccine hesitancy and refusal (NASEM 2021; WHO 2021).
To support decision‐making within vaccination programmes regarding effective strategies to increase and sustain public uptake of childhood vaccination, it is important to understand which factors enhance and reduce acceptance of vaccination. In particular, understanding parents' and informal caregivers' reasons for their vaccination views and practices could help inform the development of interventions to promote acceptance and uptake of vaccines that are better aligned with the norms, views, expectations, and potential concerns of target users, thereby potentially enhancing their acceptability and effectiveness. As stressed by Larson and colleagues, "emphasis should be placed on listening to the concerns and understanding the perceptions of the public to inform risk communication and to incorporate public perspectives in planning vaccine policies and programmes" (Larson 2011).
Qualitative research is well‐placed for exploring complex perceptions, practices, and decision‐making, and for understanding how different factors influence these. Data arising from qualitative studies can help answer questions regarding what people think about vaccines, their practices around vaccination, their vaccination decision‐making processes, and the reasons for these views, practices, and decisions. A better understanding of these issues, and their impact in different settings, can help identify what factors influence parental vaccination decision‐making, and how they do so. This, in turn, can help us think through which interventions may be most appropriate for enhancing vaccination acceptance and uptake, and why.
Various reviews have focused on the demand side of childhood vaccination (see Table 2 for a summary of these reviews). Many of these reviews are dated, limited in geographical scope (i.e. include studies only from HICs), focused on specific vaccines or broader populations than children, and are not ‘systematic’ in their approach. In addition, few existing reviews include qualitative studies, and amongst those that do, in most cases, the results were synthesised quantitatively or in a narrative summary. Carrying out an up‐to‐date qualitative review that systematically explores the factors influencing parental views and practices regarding routine childhood vaccination, from the perspective of parents and informal caregivers and across a variety of regions and vaccines, will provide a single point of access for synthesised qualitative evidence on childhood vaccination acceptance to inform immunisation policy and strategies.
1. Summary of related published reviews focused on the demand side of childhood vaccination.
|
Author/ date |
Title | Focus | Methodology |
| Dube 2018 | Underlying factors impacting vaccine hesitancy in high‐income countries: a review of qualitative studies | Focuses on the determinants of parents’ attitudes and behaviours towards childhood vaccination. Only includes studies from HICs | Qualitative |
| Larson 2018b | Measuring trust in vaccination: a systematic review | Focuses specifically on the issue of trust and how different dimensions of trust interact to influence vaccine acceptance, hesitancy and refusal. Considers vaccines for both children and adolescents | Mixed methods, includes both quantitative and qualitative studies |
| Ames 2017b | Parents’ and informal caregivers’ views and experiences of communication about routine childhood vaccination: a synthesis of qualitative evidence | Focuses specifically on views and experiences of communication interventions about childhood vaccinations | Qualitative |
| Karafillakis 2017 | The benefit of the doubt or doubts over benefits? A systematic literature review of perceived risks of vaccines in European populations | Focuses on perceptions of the benefits and risks of vaccines. Only includes studies from Europe and considers vaccines for all age groups | Mixed methods, includes both quantitative and qualitative studies |
| Carlsen 2016 | The swine flu vaccine, public attitudes, and researcher interpretations: a systematic review of qualitative research | Focuses on attitudes towards a vaccine given in response to a pandemic and also considers all age groups | Qualitative |
| Corben 2016 | To close the childhood immunisation gap, we need a richer understanding of parents’ decision‐making | A narrative review focusing on factors influencing parents’ vaccination decision‐making and interventions to increase vaccination uptake | Mixed methods, includes both quantitative and qualitative studies |
| Tauil 2016 | Factors associated with incomplete or delayed vaccination across countries: a systematic review | Focuses on the factors influencing adherence to routine childhood immunisation schedule. Considers both demand‐ and supply‐related factors | Quantitative |
| Larson 2014 | Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: a systematic review of published literature, 2007‐2012 |
Focuses on the factors affecting vaccine hesitancy and its determinants | Quantitative |
| Williams 2014 | What are the factors that contribute to parental vaccine‐hesitancy and what can we do about it? | Focuses on the barriers to vaccination reported by vaccine‐hesitant parents and the current evidence on strategies to address parental vaccine hesitancy. Considers vaccines for both children and adolescents | Quantitative |
| Yaqub 2014 | Attitudes to vaccination: a critical review | Focuses on vaccination attitudes among the public and healthcare professionals. Only includes studies from Europe and considers vaccines for all age groups | Mixed methods, includes both quantitative and qualitative studies |
| Dube 2013 | Vaccine hesitancy: an overview | A narrative review providing an overview of the phenomenon of vaccine hesitancy and the possible causes of its increase, and the determinants of individual vaccination decision‐making. Only includes studies from HICs | Unclear as it includes multiple studies and reviews and does not specify the methods for each |
| Favin 2012 | Why children are not vaccinated: a review of the grey literature | A review of grey literature focusing on the reasons for childhood incomplete or non‐vaccination. Considers both demand‐ and supply‐related factors | Mixed methods, includes both quantitative and qualitative studies |
| Rainey 2011 | Reasons related to non‐vaccination and under‐vaccination of children in LMICs: findings from a systematic review of the published literature, 1999–2009 | Focuses on the factors related to the under‐vaccination and non‐vaccination of children. Considers both demand‐ and supply‐ related factors and only includes studies from LMICs | Mixed methods, includes both quantitative and qualitative studies |
| Brown 2010 | Factors underlying parental decisions about combination childhood vaccinations including MMR: a systematic review | Focuses on the factors influencing vaccination decisions. Only includes studies from HICs and considers only combination MMR vaccines | Mixed methods, includes both quantitative and qualitative studies |
| Falagas 2008 | Factors associated with suboptimal compliance to vaccinations in children in developed countries: a systematic review | Focuses on the factors associated with suboptimal childhood vaccination compliance. Only includes studies from HICs | Quantitative |
| Jackson 2008 | A systematic review of decision support needs of parents making child health decisions | Focuses on all parental decision‐making about child health, not just vaccination | Mixed methods, includes both quantitative and qualitative studies |
| Nagaraj 2006 | Does qualitative synthesis of anecdotal evidence with that from scientific research help in understanding public health issues: a review of low MMR uptake | Focuses on professional and parental factors underlying uptake of MMR only, and only includes studies from HICs | Qualitative, includes technical and non‐technical anecdotal literature |
| Mills 2005 | Systematic review of qualitative studies exploring parental beliefs and attitudes toward childhood vaccination identifies common barriers to vaccination | Focuses on parental beliefs and attitudes toward childhood vaccination and associated barriers to paediatric immunisations. Only includes studies from HICs | Qualitative |
| Sturm 2005 | Parental beliefs and decision making about child and adolescent immunisation: from polio to sexually transmitted infections | A narrative review focusing on the influence of parental attitudes and beliefs on vaccine decision‐making. Only includes studies from HICs and considers vaccines for children and adolescents |
Mixed methods, includes both quantitative and qualitative studies |
| Roberts 2002 | Factors affecting uptake of childhood immunisation: a Bayesian synthesis of qualitative and quantitative evidence | Focuses on the factors that affect the uptake of recommended childhood immunisations. Only includes studies from HICs | Mixed |
HICs: high‐income countries; LMICs: low‐ and middle‐income countries; MMR: measles, mumps, and rubella
How this synthesis links to evidence about intervention effectiveness
The findings of this qualitative evidence synthesis complement those of a Cochrane qualitative evidence synthesis on perceptions and experiences of communication about routine childhood vaccination (Ames 2017b). As the review authors explain, communication is one of many interacting factors that may influence parents' and informal caregivers' decisions to take their children for vaccination, and communication alone will therefore not address all aspects of vaccine acceptance, hesitancy, or refusal. Therefore, our review builds upon the Ames 2017b review by identifying the range of factors (in addition to vaccination communication and information) that may influence parental views and practices regarding routine childhood vaccination, and by explaining how these factors potentially operate to impact on vaccination acceptance.
This qualitative evidence synthesis also supplements existing Cochrane Reviews of the effectiveness of different interventions for improving childhood vaccination coverage and uptake (Saeterdal 2014; Oyo‐Ita 2016; Jacobson‐Vann 2018; Kaufman 2018). It may provide partial explanations for the heterogeneity of results across these Cochrane Reviews, as well as contribute to the development of more relevant, acceptable, and effective interventions in the future.
The results from this synthesis may improve our understanding of the reasons for enhanced or reduced acceptance of childhood vaccination from the perspective of parents and informal caregivers. These results can be used to generate hypotheses about why and how certain interventions to improve vaccine uptake might be more effective than others, for whom, and in which contexts, for subsequent subgroup analyses in future reviews of intervention effectiveness.
Finally, this review provides insights from qualitative review data, which could be used in the development or refinement of conceptual models explaining the demand side of vaccination, so that these models are informed by a larger evidence base and are potentially more theoretically grounded.
Objectives
Explore parents’ and informal caregivers’ views and practices regarding routine childhood vaccination, and the factors influencing acceptance, hesitancy, or nonacceptance of routine childhood vaccination.
Develop a conceptual understanding of what and how different factors reduce parental acceptance of routine childhood vaccination.
Explore how the findings of this review can enhance our understanding of the related Cochrane Reviews of intervention effectiveness (Saeterdal 2014; Oyo‐Ita 2016; Jacobson‐Vann 2018; Kaufman 2018).
Methods
Criteria for considering studies for this synthesis
Types of studies
We included primary studies that used qualitative study designs such as ethnography, phenomenology, case studies, grounded theory studies, and qualitative process evaluations. We included studies that used both qualitative methods for data collection (e.g. focus group discussions, individual interviews, observation, diaries, document analysis, and open‐ended survey questions), and qualitative methods for data analysis (e.g. thematic analysis, framework analysis, grounded theory). We excluded studies that collected data using qualitative methods but did not analyse the data using qualitative analysis methods (e.g. open‐ended survey questions where the response data were analysed using descriptive statistics only). We included mixed methods studies where it was possible to extract the data that were collected and analysed using qualitative methods. We included studies regardless of whether or not they were linked to an intervention. We did not exclude any studies based on our assessment of methodological limitations, but utilised this information to assess our confidence in the synthesised findings.
Topic of interest
The topic of interest of this synthesis was the range of factors which influence parental views and practices regarding routine childhood vaccination from the perspective of parents and informal caregivers.
Types of participants
We included studies that reported on views, practices, or factors influencing acceptance, hesitancy, or nonacceptance regarding routine childhood vaccination, as given by parents or informal caregivers. By ‘informal caregiver’, we mean anyone who is directly involved in caring for the child or making the decision to vaccinate the child, or who has the responsibility to take the child for vaccination (Ames 2017b). We also included studies if they reported on the views, practices, or factors influencing acceptance, hesitancy or nonacceptance regarding routine childhood vaccination as given by prospective parents (e.g. pregnant women, their partners, or both). We excluded studies if they only reported what healthcare providers, policymakers, programme administrators and managers, or other immunisation stakeholders said about the vaccination views, practices, acceptance, hesitancy, or nonacceptance of parents and informal caregivers or the factors influencing these.
Types of interventions
We included studies about parents’ or informal caregivers’ vaccination views, practices, acceptance, hesitancy, or nonacceptance regarding routine childhood vaccination, irrespective of the vaccination setting or mode of delivery. Vaccination settings and modes of delivery included, for example, vaccination provided at healthcare facilities or fixed outreach sites, or by mobile health teams in communities (Machingaidze 2013b).
By ‘routine’ childhood vaccination, we mean WHO‐recommended routine vaccines for children under six years of age as part of the Expanded Programme on Immunisation (EPI). This included the following vaccines or combinations of vaccines (WHO 2018b).
Bacillus Calmette‐Guérin (BCG).
Hepatitis B.
-
Polio:
Oral poliovirus vaccine (OPV);
Inactivated polio vaccine (IPV).
Diphtheria, tetanus, pertussis (whooping cough) (DTaP)
Haemophilus influenzae type b (Hib).
Pneumococcal conjugate vaccines (PCV).
Rotavirus.
Measles.
Mumps.
Rubella.
Measles, mumps, and rubella (MMR).
Japanese encephalitis.
Yellow fever.
Tick‐borne encephalitis.
Typhoid.
Cholera.
Meningococcal.
Hepatitis A.
Seasonal influenza.
We excluded the following vaccines because children under six years of age do not routinely receive them as part of the EPI.
Human papillomavirus (HPV).
Rabies.
Haemagglutinin type 1 and neuraminidase type 1 (H1N1), and other epidemic vaccinations.
We excluded studies on hypothetical vaccines, future vaccines, or vaccination trials. We also excluded studies if it was not possible to separate out the data on views of routine childhood vaccination from views of vaccination in other age groups (e.g. adolescents, adults) or views on vaccination in general.
Setting
We included studies from any setting globally where childhood vaccination is provided. These settings could include healthcare facilities, fixed outreach sites, or mobile health teams in communities.
Search methods for identification of studies
Electronic searches
We searched PDQ‐Evidence (pdq-evidence.org) for related reviews, as well as the following electronic databases for eligible studies from 1974 to 3 June 2020.
PDQ‐Evidence, Epistemonikos Foundation
MEDLINE and Epub Ahead of Print, In‐Process & Other Non‐Indexed Citations and Daily 1946 to June 02, 2020, Ovid
Embase 1974 to 2020 June 02, Ovid
CINAHL (Cumulative Index to Nursing and Allied Health Literature)1980‐present, EbscoHost
Web of Science Core Collection (Clarivate Analytics).
APA PsycInfo 1806 to May Week 4 2020
We chose these databases as we anticipated that they would yield the highest number of results based on preliminary, exploratory searches. We developed search strategies for each database, using guidelines developed by the Cochrane Qualitative & Implementation Methods Group for searching for qualitative evidence (Harris 2018). We did not apply any limits on language or geographic location. We searched all databases from 1974 to capture parents’ and informal caregivers’ views and practices regarding routine childhood vaccination since the introduction of the WHO’s EPI. We included a methodological filter for qualitative studies. Search strategies for all databases are given in Appendix 1.
Searching other resources
In addition to database searching, we handsearched references of all included studies and key references (i.e. relevant systematic reviews).
Data collection, management, and synthesis
Selection of studies
We collated records identified from different sources into one database and removed duplicates. Two independent review authors then used Covidence (www.covidence.org/) to assess each record for eligibility (SC, BS, ES). At this stage, we discarded abstracts that were clearly irrelevant to the topic of this review and abstracts published in languages other than English, French or German (see 'Language translation' for more details). At this stage, we also decided to exclude dissertations, because of the very high numbers of dissertation abstracts identified and the difficulties we experienced in accessing their full texts. We retrieved the full texts of all abstracts identified as potentially relevant. Two independent review authors (SC, BS, ES) then used Covidence to assess each full‐text article for inclusion, according to predefined criteria. For both the title/abstract and full‐text screening, review authors resolved disagreements through discussion or, when required, by seeking a third review author’s opinion. Where appropriate, we contacted the study authors for further information.
Language translation
Only articles published in languages spoken by the review authors were selected for inclusion. This meant that only articles in French, English, and German were included. The resources needed and difficulties associated with translating papers reporting qualitative research in the context of a qualitative evidence synthesis are common issues across synthesis approaches. However, these issues are arguably particularly challenging with more interpretive (as opposed to aggregative) synthesis approaches. In these cases, an in‐depth and nuanced understanding of the meaning of complex conceptual data is essential (France 2014; Noyes 2018). To ensure analytical rigour, we therefore decided to exclude studies published in languages not spoken by the review authors.
Sampling of studies
In contrast to reviews of intervention effectiveness, the inclusion of large numbers of primary studies in qualitative evidence syntheses can impair the quality of the analysis (Ames 2019a). Large volumes of data may hinder a detailed and in‐depth engagement with the data and make it difficult to move from a descriptive or aggregative analysis to a more interpretive analysis. Moreover, unlike reviews of intervention effectiveness, which aim to be exhaustive in order to achieve statistical generalisability, syntheses of qualitative studies aim for depth of understanding and conceptual generalisability (Hannes 2013).
Numerous studies met our inclusion criteria – 145 studies, described in 176 full texts (173 articles and 3 books) – and we considered this number too large to analyse adequately and undertake an interpretive meta‐ethnography. Therefore, we purposefully sampled a selection of studies to be included in the synthesis (Suri 2011), using 3 sampling criteria in the following order: ‘conceptual richness’, ‘relevance’, and ‘geographical spread’. Our sampling approach draws on the guidance provided by Cochrane Effective Practice and Organisation of Care (EPOC 2017), and the sampling approach developed and used for a related review on perceptions and experiences of communication about routine childhood vaccination (Ames 2019a).
There is growing recognition that meta‐ethnography requires conceptually‐rich studies, since more descriptive findings usually have too little depth to allow an interpretive synthesis (Britten 2012; France 2014; France 2019). Various meta‐ethnographies have found that studies that lacked interpretation beyond basic description limited the analysis (Atkins 2008; Garside 2008; Campbell 2011), while another meta‐ethnography found that the synthesised findings remained the same when only conceptually‐rich papers were included in the analysis (Malpass 2009). Therefore, we decided to use ‘conceptual richness’ as our primary sampling criterion, to ensure that those studies included in the analysis were conceptually rich enough to enable translation and explanation of concepts which go beyond the settings of individual studies.
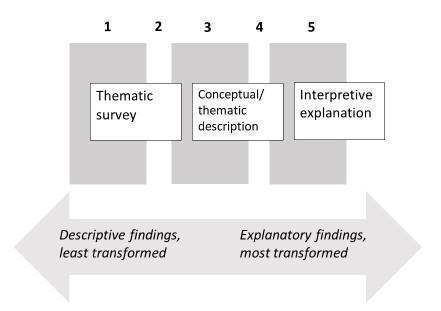
While there is a tool to assess the data richness of qualitative studies (Ames 2019a), to our knowledge, there is no existing tool to assess the conceptual richness of qualitative studies. Therefore, we developed our own assessment scale by drawing on the typology of the type and nature of qualitative findings developed by Sandelowski 2007. This typology conceives qualitative findings as being located along a continuous spectrum based on the degree of abstraction of analysis and interpretation of the data, or what is referred to as the extent of ‘data transformation’. At one end of the spectrum are more descriptive findings; that is, findings that describe patterns in the data. At the other end of the spectrum are interpretive or explanatory findings. These transformed findings have a high level of abstraction and provide theoretical interpretations or explanations of the patterns in the data.
We created a simple 1 to 5 scale for categorising studies on this spectrum of data transformation (Figure 1). Employing the terms used by the original authors of the typology, we defined our scores as follows.
1.
Conceptual richness 5‐point scale (adapted from the typology of qualitative findings developed by Sandelowski 2007)
A score of 1: thematic survey: concepts or themes may be used to label, present, or organise portions of data. These concepts or themes may be developed in situ (i.e. invented by the researcher from the data collected in a study) or from theoretical or empirical literature outside the study.
A score of 3: conceptual/thematic description: findings that explore and interpret patterns of association in portions of data or link these patterns to key theoretical concepts. In contrast to thematic surveys in which in situ or imported concepts or themes are used to label or order portions of data, in conceptual/thematic descriptions, concepts or themes are used to interpretively reframe portions of data.
A score of 5: interpretive explanation: interpretive or explanatory findings that provide theoretical interpretations or explanations of the patterns in the data. In contrast to findings that consist of conceptual/thematic descriptions of segments of data representing one or more elements of an experience, interpretive explanations offer a coherent model, single thesis, or line of argument which provides integrated explanations of phenomena or events.
Using this conceptual‐richness scale, two reviewers (SC, BS) independently scored 25 studies. Comparison of their assessments revealed a fair degree of consensus. Therefore, one reviewer (SC) performed the assessment on the remaining eligible studies, which was subsequently checked by a second reviewer (BS). We sampled all studies that scored a 3 or higher on the scale, which comprised 30 studies from 56 articles.
Meta‐ethnography requires studies that are not only conceptually rich, but which are also likely to make an important contribution to the synthesis (Noblit 1988; Campbell 2011). Thus, a study may be conceptually rich, but very little of the data may relate to the question of interest of the synthesis. For example, a study which focuses on parents’ experiences of promoting infant health and development may be conceptually rich, but the data in relation to vaccination specifically may be conceptually thin. Similar to Ames and colleagues (Ames 2019a), we therefore employed a second sampling criterion of ‘relevance’ to assess the studies that had already been sampled. We did this by re‐examining the studies that scored 3 or higher on the conceptual‐richness scale to assess their relevance with regards to the phenomenon of interest of the synthesis. Here, we asked the question: ‘Is the study conceptually rich in relation to the question of interest of the synthesis?’, and employed a simple ‘yes/no’ approach to answer this question. Through this process, we removed three studies from our pool of sampled studies, as most of their data and focus were outside of the scope of the synthesis. This resulted in 27 studies from 53 articles sampled.
Finally, and similar to Ames and colleagues again (Ames 2019a), we considered the geographic distribution of the sampled studies. Our review sought to develop a global understanding of the factors influencing parental views and practices regarding routine childhood vaccination, including similarities and differences across different settings. Moreover, as the majority of existing reviews on the demand side of childhood vaccination have been limited to studies from HICs (see Table 2), we felt it was important to ensure our review comprised a more representative geographical spread of findings. Therefore, we extracted information on the WHO region and income level (HIC or LMIC) of all included studies and considered the geographic representation of sampled studies. We agreed that the regional and income‐level distribution of sampled studies was adequate, and as such made the decision to not undertake any further sampling. Therefore, we sampled and included a total of 27 studies from 53 articles in the analysis.
Data extraction
We extracted contextual and methodological data for each sampled study using a form designed specifically for this review. We used this form to extract the following information (where available): study author; date of publication; country of study; high‐income country/low‐ and middle‐income country; WHO region; participant details, including total number of participants, participant group (first‐time parent/informal caregiver, older parent/informal caregiver, etc.), gender, socioeconomic status; type of vaccine; objectives or aim; study design, including overarching methodological approach, guiding theoretical or conceptual framework, data collection and analysis methods; other contextual details (any key political, historical, and cultural factors of potential relevance).
Assessment of methodological limitations in the included studies
Our inclusion criteria specified that included studies needed to use both qualitative data collection and analysis methods. This constituted a basic quality threshold, as we excluded studies that used qualitative methods to collect data but not to analyse these data. In addition, two review authors (SC, BS) independently assessed methodological limitations for each study using criteria employed in previous Cochrane Reviews (Ames 2017b; Munabi‐Babigumira 2017; Ames 2019b; Karimi‐Shahanjarini 2019; Houghton 2020). These criteria were originally based on the Critical Appraisal Skills Programme (CASP) tool (CASP 2018), but they have since gone through several iterations. For instance, we did not include questions about the appropriateness of qualitative methodology or the specific research design used, as these were already covered in our inclusion criteria. We resolved disagreements through discussion between the two review authors or through consultation with a third review author (ES). The adapted tool includes the following eight questions, which we used to assess methodological limitations.
Are the setting(s) and context described adequately?
Is the sampling strategy described, and is this appropriate?
Is the data collection strategy described and justified?
Is the data analysis described, and is this appropriate?
Are the claims made/findings supported by sufficient evidence?
Is there evidence of reflexivity?
Does the study demonstrate sensitivity to ethical concerns?
Any other concerns?
We conducted a pilot on three sampled studies to assess the feasibility of using this tool and to ensure integrity of the assessment. We did not use our quality assessments to exclude studies, but rather to judge the relative contribution of each study to the development of explanations and relationships and as part of the assessment of how much confidence we have in each finding (see below). Our assessments for each study are reported in the Methodological limitations table in Appendix 2.
Data management, analysis, and synthesis
We used a meta‐ethnographic approach, drawing on the analytical steps outlined originally by Noblit and Hare (Noblit 1988), and the eMERGe meta‐ethnography reporting guidance (France 2019). Meta‐ethnography is an interpretive, rather than aggregative, qualitative synthesis approach which is well‐suited to producing new concepts or theories (France 2014; Noyes 2018). As the central aim of this synthesis was to derive a new conceptual understanding of the factors influencing parental views and practices regarding routine childhood vaccination, we decided that a meta‐ethnographic approach was the most appropriate synthesis method. Meta‐ethnography involves induction and interpretation to translate and synthesise conceptual data identified within included studies into higher‐order interpretations. The analysis is built up study by study, in a manner that both preserves the context of the primary data within individual studies, and facilitates an understanding of how concepts in different studies are related to each other (France 2019).
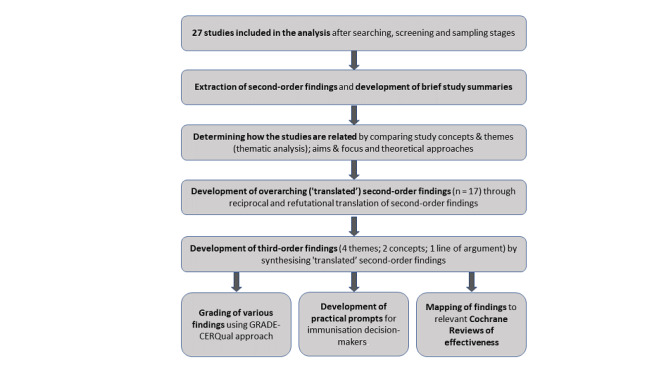
Our analysis comprised various stages, which we describe separately and in detail below (see Figure 2 for a flow diagram of the analysis phases). In practice, however, the different stages and processes of the analysis were blurred and iterative, unfolding in a manner that “cannot be reduced to mechanistic tasks" (Britten 2002). The final findings of our synthesis were the outcome of acombination of deep immersion in the data, detailed reading and prior knowledge of theory, team discussion and compromise, as well as rigour, reflection, and creativity. Ultimately, these processes continued until we reached an understanding of our phenomenon of interest, an understanding which is inevitably incomplete but one with which we were satisfied.
2.
Flow diagram to illustrate analysis phases
Stage 1: extraction of study author interpretations (second‐order findings) and development of brief study summaries
The first stage of the analysis involved undertaking a close reading and rereading of all studies to identify and extract study author interpretations (second‐order findings), as well as a selection of corresponding participant quotes (first‐order findings) for illustrative purposes. During this stage, we also developed a brief, structured summary for each study, capturing the study aims and context, the theory or theories used to explain findings or link concepts, and the study's line of argument. Data extraction for each paper, as well as the structured study summaries, was conducted by one review author (SC), checked by a second author (BS or ES), and followed by discussion and resolution of any queries.
Key issues and considerations
When undertaking the data extraction, we understood research participants’ quotes as reflecting first‐order findings, and study authors’ interpretations as second‐order findings (Britten 2002). However, we recognised that this distinction is blurred, as study authors select and interpret participant quotes to demonstrate second‐order findings (Schutz 1971).
We extracted concepts, themes, and the study's line of argument as second‐order findings. Here, we understood concepts as having some analytic or conceptual power, in contrast to themes which are more descriptive and comprise data simply organised and presented without much transformation or evidence of second‐order conceptualisation by the researcher (Britten 2012). When extracting concepts, we also extracted (where available) the theory or theories underpinning their meaning. Drawing on more recent definitions provided by Noblit (Noblit 2016; Noblit 2019), we understood a line of argument to be an overarching explanation, interpretation, or ‘storyline’ of a phenomenon. Therefore, while themes and concepts may describe or explain segments of data, a line of argument provides a broader theory or single thesis which links and potentially integrates different concepts and themes (see Figure 3).
We tried as much as possible to use the study authors’ own words or a close paraphrase, with little re‐interpretation, when extracting second‐order findings.
Data extraction occurred across the full texts, as second‐order findings were often reported and developed throughout the articles and books.
Many studies were reported in several articles or books included in the review. We therefore performed data extraction for each individual article or book first, and then amalgamated these extractions into a single Word document for each study, removing duplicate findings.
3.
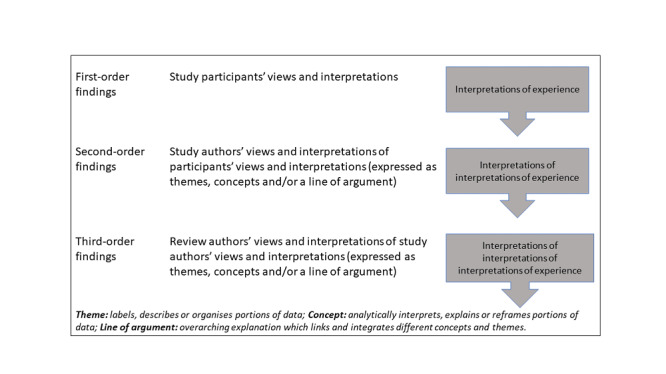
Types and definitions of qualitative research findings (drawing on Noblit 1988; Britten 2002; Malpass 2009; Sandelowski 2007)
Stage 2: determining how the studies are related
The next stage in the analysis involved comparing and contrasting the primary studies to decide how they were related and, therefore, how they could be synthesised. One author (SC) led this process, with discussion and input from two other authors (BS, ES). Here, we compared three aspects of the studies: the meaning of their key concepts or themes, their central aim or focus, and their theoretical approaches (Noblit 1988).
Comparing the meaning of study concepts and themes
To compare how studies related in terms of their concepts and themes, we created a list of the second‐order findings, including a summary of their meaning, for each study. Although there was an immediately obvious similarity between study concepts and themes, we felt that the numerous second‐order findings necessitated some preliminary form of organising to enable adequate comparison. We therefore performed a basic thematic analysis at this point, following a process similar to others (Pound 2005; Atkins 2008), to group the concepts and themes inductively within and between studies into categories of shared meaning. Through this process, we developed seven broad thematic categories of meaning.
Comparing study aim/focus and theoretical approaches of studies
We compared the central aim, as well as the theoretical approaches, of studies by reading the structured summaries we had previously developed for each study, returning to the original articles where necessary. The commonalities in study aims were clearly evident, which was unsurprising, given the relatively tightly focused aim and research question of our review, and associated search and sampling strategies (France 2019).
The relationship between the studies’ theoretical approaches was less obvious. Using the structured summaries, we made a list of the main theory or theories that studies used to explain, describe, or predict findings or link concepts, so we could examine them more closely. There were many similar, but also diverse, theories across the studies. However, on investigation, we considered them to be mutually commensurate in their politics and underpinning epistemological assumptions (Bevan 2007). Our assessment was both enabled and informed by many of the review authors’ understanding and prior knowledge of the theories employed by studies.
Outcome of the comparisons
From these comparisons, we concluded that the general conceptual coherence between studies, their similarities in topic and focus, and their epistemological compatibility meant that, in general, the studies were reciprocally related. While no study was a complete refutation of another, our comparisons did reveal various specific findings within and between studies that were incongruent, inconsistent, or in opposition. For example, in some studies, the concept of ‘infant fragility’ was found to enhance vaccination acceptance, whereas in other studies, it was found to reduce vaccination acceptance. We therefore conducted both a ‘reciprocal’ and a ‘refutational’ translation (see 'Stage 3') for the similar and the disconfirming findings, respectively (France 2019).
Stage 3: development of overarching (‘translated’) second‐order findings
The next stage of the analysis comprised the translation of the studies into each other to produce overarching or 'translated' second‐order concepts and themes. This entailed comparing the second‐order concepts and themes across the studies so as to ‘match’ those describing a similar idea, albeit with a different label (reciprocal translation), and to identify and explain deviant cases (refutational translation). One review author (SC) led the process of translation, with discussion, input, and verification from two other authors (BS, ES) in the early stages, and from all review authors in the later stages.
We began the translation process by grouping the studies according to income group (HIC or LMIC), and then, as others have done (Atkins 2008; Malpass 2009; Campbell 2011), by the date of publication within each of the income groups. Using this grouping, we then approached the reciprocal translations in a way similar to that of Campbell 2011. We systematically compared the second‐order findings from study 1 with study 2, and then the synthesis of these studies with study 3, and so on. We conducted our comparisons within the seven thematic categories we had developed through our thematic analysis in stage 2. We followed this process chronologically for studies within each income group until all the studies had been translated into each other. Once we had a list of translated findings for each income group, we then translated the findings from the two income groups into each other.
For the refutational translations, we juxtaposed apparent incongruencies, inconsistencies, and oppositions to “take into account the implied relationship between them” (Noblit 2019). That is, we explored whether they might be explained by differences in participants, settings, or study design, or whether the differences pointed to other potential variations in the phenomenon of interest (Booth 2013; France 2019).
The translation processes culminated in the identification of 17 translated second‐order findings, each with several related subconcepts or subthemes. Each second‐order finding represents a specific factor influencing parental views and practices regarding childhood vaccination. We created a list of all second‐order findings, and accompanied each with a brief narrative summary.
Key issues and considerations
We needed to make decisions about the order in which to translate the studies. Through our thematic analysis in the previous stage, we had observed several similar second‐order findings amongst the studies in HICs and amongst those in LMICs, or what felt like a conceptual coherence within (and less between) these two country income groups. It therefore made sense to us to arrange the studies, firstly, according to income group (HIC or LMIC). Grouping the studies in this way enhanced our understanding of this particular contextual issue, although this grouping may also have limited our analysis in other ways (see ‘Limitations of the review’). The studies in our review spanned over 20 years and, therefore, like Atkins 2008, we were interested in ascertaining the potential impact that any changes over time in vaccination policy, programmes, and/or research may have on the findings. Therefore, and in a similar way to others (Atkins 2008; Malpass 2009; Campbell 2011), after grouping the studies by income group, we then arranged the studies by date of publication within each of the income groups. However, similar to Atkins 2008, we found it difficult to discern the potential impact of any changes over time in vaccination policy, programmes, and/or research. Our decision to organise and synthesise the studies chronologically within income groups therefore appears to have had little impact on the analysis and findings.
We used the seven thematic categories we had developed in stage 2 as the basis of the translation. However, these initial categories were gradually reconfigured, merged, added to, or removed as the processes unfolded.
When labelling the reciprocally translated second‐order findings, sometimes we used the terminology from one study which adequately incorporated the ideas of others (e.g. the concept of “salutogenic parenting”). At other times, we created a new label which we felt appropriately encompassed the meaning of the related concepts (e.g. the concept of the “fragile infant”). We drew on Noblit and Hare’s criteria for assessing the adequacy of metaphors (economy, cogency, range, apparency, credibility) (Noblit 1988), when considering how to name our translated second‐order findings.
Whilst conceptually distinct, the reciprocal and refutational translations were not performed separately but were integrated in a back and forth process and as part of our unfolding analysis and interpretations.
Stage 4: development of third‐order findings
The final stage of the analysis comprised synthesising the translated second‐order findings to create higher‐level findings, also referred to as ‘third‐order’ findings (Britten 2002) (see Figure 3). One review author (SC) led the synthesis process, with discussion, input, and verification from two other authors (BS, ES) in the early stages, and from all review authors in the later stages.
Key processes undertaken
This stage comprised various back and forth processes:
We repeatedly read and compared the lists and summaries of the translated second‐order findings, frequently returning to the original study articles and books to clarify meanings.
We drew many visual diagrams and mind‐maps to aid our interpretations of the translated second‐order findings and their potential inter‐relationships.
We revisited the overarching line of argument of each study (Noblit 2019), as captured in our structured study summaries. These helped us to gain a fuller understanding of context, and provided a way of checking whether our emerging interpretations were capturing the collective voice of the studies.
We used our refutation translations to test our emerging interpretations, and to integrate and contextualise them further (Finfgeld‐Connett 2014).
We examined the various theories used by the studies included in the review more closely. In some cases, we also obtained the original theoretical sources cited by study authors to refamiliarise ourselves with the relevant theory.
We also examined the various conceptual or theoretical models developed or used by the studies included in the review, as well as those developed in the existing literature external to the studies included in the review (see 'Description of the topic'). Here, three models proved useful and informed our thinking: the three‐layered analytical framework developed by Leach 2007 (study included in the review); the two‐dimensional vaccine hesitancy model developed by Peretti‐Watel 2015 (paper external to the studies included in the review); and the three‐dimensional ‘Vaccine Hesitancy Determinants Matrix’ developed by the WHO 2013b (paper external to the studies included in the review). While these models informed our interpretations, none were able to fully ‘hold’ or account for all of our translated second‐order findings.
Through these different processes, we developed various third‐order findings: four themes; two concepts; and one overarching line of argument.
Four themes: the seven original thematic categories (from stage 2) were refined and reconceptualised into four third‐order themes. Taken together, these themes provide an organising framework for the seventeen translated second‐order findings (from stage 3). Each theme represents a category of factors influencing parental views and practices around childhood vaccination (see Figure 4).
4.
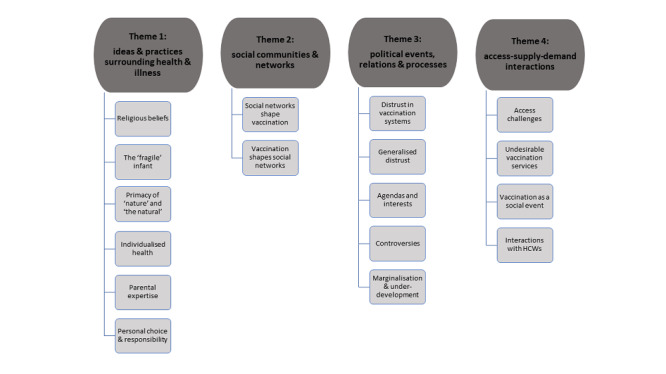
Second‐order findings organised by the third‐order themes
Two concepts: the 17 translated second‐order findings were also reinterpreted and conceptually integrated to produce two third‐order concepts which we labelled as: ‘neoliberal logic’ and ‘social exclusion’. Each concept encapsulates a potential pathway to reduced acceptance of childhood vaccination. These third‐order concepts were the product of a combination of the 17 translated second‐order findings, as well as theory and conceptual models imported from existing literature, identified in the included studies, and originally developed by the review authors (Colvin 2018) (see Figure 5).
5.
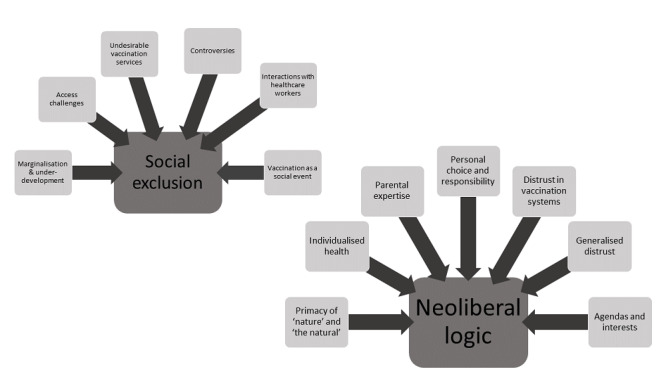
Second‐order findings that contributed to each third‐order concept
One overarching line of argument: finally, we also integrated all of the findings to develop one overarching line of argument. This provides a conceptual and more overarching explanation for how one might conceptualise parental views and practices regarding childhood vaccination. It resembles a reinterpretation of meaning across studies, and represents more than an aggregative descriptive account (Barnett‐Page 2009) (see Figure 6).
6.
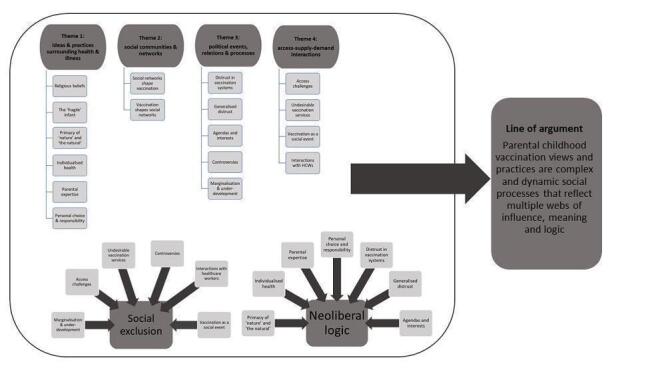
All second‐ and third‐order findings and their relationships
Key issues and considerations
Throughout the synthesis process, we were mindful of the importance of remaining grounded in the context and meaning of the primary study data (Noyes 2018). Our structured summaries of each study were particularly useful in this regard, helping us preserve the meaning of concepts and their interrelationships within specific studies as the analysis unfolded. Throughout the analysis process, we frequently returned to these structured study summaries and also the full texts of studies for clarification and further elucidation of concepts and themes.
Most studies genuinely and appropriately incorporated the theory or theories they indicated using, most likely due to our sampling of only conceptually‐rich studies for the analysis. That said, there were a few studies that mentioned using a particular theory, yet its actual incorporation in the analysis appeared limited. In such cases, the findings from these studies were mainly used to confirm, rather than further develop, our emerging interpretations. Therefore, while all studies contributed to the analysis and synthesis, some studies played a more confirmatory role.
Many of the review authors had considerable prior knowledge of the different theories employed by the studies, which facilitated our analysis. At the same time, however, this also meant that the boundaries between our own reading of the theories and how they related to the study findings, and those of the study authors, were not always easy to separate.
During our discussions, we made a conscious effort to consider potential alternative interpretations or explanations, which was facilitated by the constitution of the review team and inclusion of review authors from diverse academic disciplines.
Implications for practice
Once we had finalised our review findings, we examined each finding to identify factors that could influence the design and implementation of interventions to promote childhood vaccination acceptance or uptake. Based on this, we developed prompts for future policy‐ and decision‐makers (see Appendix 3: 'Moving from review findings to implications for practice'). These prompts are presented in the 'Implications for practice' section. These prompts are not intended to be recommendations, but are phrased as questions to help policy‐ and decision‐makers consider the implications of the review findings within their context.
Assessment of confidence in the synthesis findings
We used the GRADE‐CERQual (Confidence in the Evidence from Reviews of Qualitative research) approach to summarise our confidence in various review findings (Lewin 2018). These included 19 review findings in total: the 17 second‐order findings (study author interpretations) and the two third‐order concepts (review author interpretations). GRADE‐CERQual assesses confidence in the evidence, based on the following four key components.
Methodological limitations of included studies: the extent to which there are concerns about the design or conduct of the primary studies that contributed evidence to an individual review finding.
Coherence of the review finding: an assessment of how clear and cogent the fit is between the data from the primary studies and a review finding that synthesises those data. By cogent, we mean well‐supported or compelling.
Adequacy of the data contributing to a review finding: an overall determination of the degree of richness and quantity of data supporting a review finding.
Relevance of the included studies to the review question: the extent to which the body of evidence from the primary studies supporting a review finding is applicable to the context (perspective or population, phenomenon of interest, setting) specified in the review question.
After assessing each of the four components, we made a judgement about the overall confidence in the evidence supporting the review finding. We judged confidence as high, moderate, low, or very low. The final assessment was based on consensus among the review authors. All findings started as high confidence and were then graded down if there were important concerns regarding any of the CERQual components. Two review authors (SC, BS) led the GRADE‐CERQual assessments of the second‐order findings, and all review authors conducted the assessments of the findings for the third‐order concepts. Few GRADE‐CERQual assessments have been conducted on conceptual findings. Therefore, in our ‘Evidence profiles’, we include a greater than usual amount of detail on how we reached our assessments of the third‐order concepts.
Summary of qualitative findings tables and evidence profiles
To facilitate understanding and use of the review findings, we present them in a summary of qualitative findings (SoQF) table (see Table 1). The table displays a structured summary of each review finding and references to the studies contributing data to each finding. It also provides our assessment of confidence in the evidence, as well as an explanation of this assessment, based on the GRADE‐CERQual approach (Lewin 2018). All review findings that were assessed using GRADE‐CERQual are reported in the SoQF table regardless of their associated level of confidence.
We present detailed descriptions of our confidence assessment in the evidence profiles (Appendix 4).
Integrating the review findings with the Cochrane intervention reviews
We identified existing Cochrane Reviews of intervention effectiveness focused on interventions to improve coverage or uptake of vaccination (Saeterdal 2014; Oyo‐Ita 2016; Jacobson‐Vann 2018; Kaufman 2018). As part of our data synthesis, we explored how we could integrate the findings from these related reviews with those of our review. Here, we used a matrix‐model approach similar to Candy 2011 and Ames 2017b. Two authors (SC, BS) used a matrix‐model approach to create a comparative table that explored whether the underlying theories or components of the interventions included in the related Cochrane Reviews of intervention effectiveness reflected or targeted the factors influencing parental views and practices regarding routine childhood vaccination identified by our review.
To create the matrix, we first reviewed our four overarching themes of factors influencing parental views and practices around childhood vaccination, and devised questions which reflected their central idea or meaning. Theme four ('Access‐supply‐demand interactions') contained various core ideas and so, for this theme, we created various questions to reflect this.
Have parents’ broader health beliefs and practices been considered, and the meanings, concerns, or questions about vaccination these may give rise to?
Have the social networks and groups (e.g. social, cultural, religious, geographical) with which parents are affiliated been considered and potentially included?
Have parents’ perceptions of the authorities associated with vaccination programmes (e.g. government, healthcare workers, medical researchers, the pharmaceutical industry, global health agencies, or other relevant stakeholders) been considered? Has an attempt been made to address parents’ potential distrust of these authorities?
Has an attempt been made to address the social or economic challenges parents face in accessing vaccination services?
Has an attempt been made to address features of vaccination services that parents might find undesirable or inconvenient?
Have parents’ experiences of the social nature of vaccination services, as a place where people gather and interact, been considered?
Has an attempt been made to ensure positive interactions between healthcare workers and parents, including ensuring healthcare workers are supportive, willing to have non‐judgemental discussions with parents about their questions and concerns regarding vaccination, and provide information that parents perceive as impartial, balanced, and unbiased?
Secondly, we created a table listing these seven questions. We then assessed whether the underlying theories or components of the interventions included in the related Cochrane Reviews of intervention effectiveness reflected or targetted the influencing factors. We did this by creating a summary of the underlying theories or components of each intervention, and then applying the seven questions to each intervention. Each question could be answered as yes, no, partially, or not reported/unclear, to indicate whether the influencing factor was reflected in the underlying theories or components of the intervention. We listed all of the studies from the related Cochrane Reviews of intervention effectiveness in our matrix table, and added our assessment for each of the seven questions.
After removing duplicates, there were a total of 54 interventions from the related effectiveness reviews. As the scope of Jacobson‐Vann 2018 was broader than childhood vaccination, we only assessed trials from that review which focused on interventions for childhood vaccination. We gathered information about the interventions only from the publications included in the related Cochrane Reviews of intervention effectiveness; we did not search for additional information in related publications or from study authors.
Results
Results of the search
We found 145 studies that met our inclusion criteria (Figure 7). We sampled 27 of these studies for inclusion in the analysis. All of the sampled studies were published between 1995 and 2020.
7.
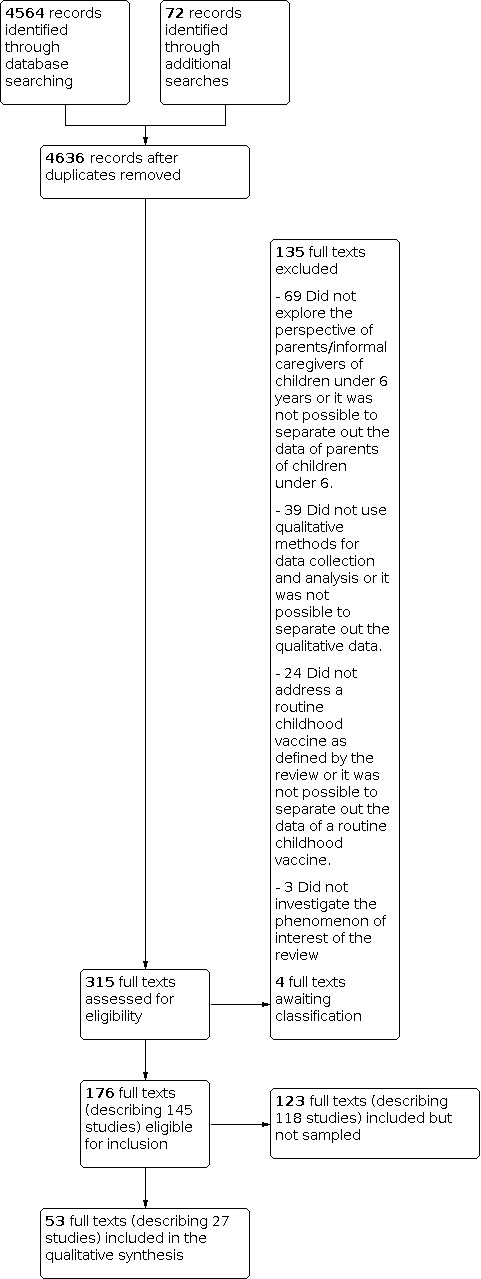
Study flow diagram
Description of the studies
In this section, we describe the studies that we included and sampled. For a more detailed description of these studies, as well as the studies that were included but not sampled, see the Characteristics of included studies.
Setting
Eleven studies were based in low‐ and middle‐income countries (LMICs): Brazil (n = 1) (Barbieri 2017), India (n = 4) (Bisht 2000; Chaturvedi 2009; Varghese 2013; Hussain 2015), Burkina Faso (n = 1) (Dugas 2009), Central African Republic and Burkina Faso (n = 1) (Giles‐Vernick 2016), Gambia (n = 1) (Leach 2007), Guinea (n = 1) (Millimouno 2006), Ethiopia (n = 1) (McKnight 2014), Nigeria (n = 1) (Renne 2010).
Sixteen studies took place in high income countries (HICs): Australia (n = 1) (Ward 2017), USA (n = 5) (Brunson 2013; Reich 2016; Sobo 2016; Carrion 2018; Limaye 2020), Canada (n = 1) (Dube 2016), United Kingdom (UK, n = 7) (Rogers 1995; Petts 2004; Brownlie 2005; Poltorak 2005; Casiday 2007; Johnson 2014; Smith 2017), France (n = 1) (Peretti‐Watel 2019), Netherlands (n = 1) (Ruijs 2012). These assignments are based on the World Bank’s classification of income level as of June 2019.
In terms of WHO regions, six studies were conducted in Africa (Millimouno 2006; Leach 2007; Dugas 2009; Renne 2010; McKnight 2014; Giles‐Vernick 2016), seven in the Americas (Brunson 2013; Dube 2016; Reich 2016; Sobo 2016; Barbieri 2017; Carrion 2018; Limaye 2020), four in South‐East Asia (Bisht 2000; Chaturvedi 2009; Varghese 2013; Hussain 2015), nine in Europe (Rogers 1995; Petts 2004; Brownlie 2005; Poltorak 2005; Casiday 2007; Ruijs 2012; Johnson 2014; Smith 2017; Peretti‐Watel 2019), one in the Western Pacific (Ward 2017), and none in the Eastern Mediterranean.
Six studies, all undertaken in the UK, focused exclusively on the MMR vaccine (Petts 2004; Brownlie 2005; Poltorak 2005; Casiday 2007; Johnson 2014; Smith 2017). Three studies focused exclusively on polio vaccines: two of these were undertaken in India (Chaturvedi 2009; Hussain 2015), and one in Nigeria (Renne 2010). The rest of the studies (n = 18) focused on all childhood vaccines or childhood vaccination in general.
Respondents
In all of the studies, authors sought the perspectives of parents and informal caregivers, such as grandmothers, although it was not possible to distinguish between the viewpoints of these groups during the analysis.
Twelve studies explored the perspectives of mothers only (Rogers 1995; Bisht 2000; Petts 2004; Poltorak 2005; Leach 2007; Varghese 2013; Johnson 2014; McKnight 2014; Dube 2016; Smith 2017; Carrion 2018; Limaye 2020).
Two studies reported focusing on parents from specific minority groups: one study in the Netherlands explored the perspectives of orthodox Protestant parents from various villages in the ‘Dutch bible belt’ (Ruijs 2012), and one study in the UK examined the perspectives of site‐dwelling Gypsy, Roma, and Traveller parents in South East England (Smith 2017).
Nine studies reported including parents from diverse socioeconomic groups: five of these studies were conducted in Europe (Petts 2004; Brownlie 2005; Poltorak 2005; Casiday 2007; Peretti‐Watel 2019); three in the Americas (Brunson 2013; Carrion 2018; Limaye 2020), and one in South East Asia (Hussain 2015). Six studies reported including parents exclusively from higher socioeconomic groups: two of these studies were conducted in Europe (Rogers 1995; Johnson 2014), three in the Americas (Reich 2016; Sobo 2016; Barbieri 2017), and one in the Western Pacific (Ward 2017). One study (conducted in Ethiopia) reported that the majority of parents were peasants who lived just above subsistence level (McKnight 2014). Eleven studies did not report on the socioeconomic status of the participants: five of these studies were conducted in Africa (Millimouno 2006; Leach 2007; Dugas 2009; Renne 2010; Giles‐Vernick 2016); three in South East Asia (Bisht 2000; Chaturvedi 2009; Varghese 2013); two in Europe (Ruijs 2012; Smith 2017); and one in the Americas (Dube 2016).
Five studies only included parents who did not vaccinate their child(ren) according to the national EPI recommended schedule (e.g. refused vaccination, partially vaccinated, delayed some or all vaccinations), including two studies conducted in the USA (Reich 2016; Carrion 2018), one study in Ethiopia (McKnight 2014), one study in the UK (Rogers 1995), and one study in Australia (Ward 2017). One study, undertaken in the UK, only included parents with concerns about immunisation (Brownlie 2005).
Methodology
Thirteen studies employed a long‐term ethnographic approach (sometimes spanning many years), including the use of multiple data collection strategies and various types of observational and participatory methods (e.g. simultaneous use of formal individual or group interviews, informal discussions, and participant and/or nonparticipant observations amongst the people and settings of interest) (Bisht 2000; Poltorak 2005; Millimouno 2006; Leach 2007; Chaturvedi 2009; Dugas 2009; Renne 2010; Varghese 2013; McKnight 2014; Hussain 2015; Giles‐Vernick 2016; Reich 2016; Sobo 2016).
Nine studies only conducted in‐depth, individual interviews (Rogers 1995; Ruijs 2012; Brunson 2013; Dube 2016; Barbieri 2017; Ward 2017; Carrion 2018; Peretti‐Watel 2019; Limaye 2020).
Four studies only conducted focus group discussions (Petts 2004; Brownlie 2005; Johnson 2014; Smith 2017), and one study conducted both individual interviews and focus group discussions (Casiday 2007).
All studies employed interpretive analytical approaches and drew on a range of critical social theories, particularly from the fields of sociology and anthropology. These included, inter alia, critical theory on risk, trust, and uncertainty; idioms of distress and practices around health, disease, and therapy; science and technology; knowledge, power, and discourse; governmentality; subjectivity; social capital; and a range of other actor‐ and practice‐oriented social theories. Whilst studies utilised diverse critical social theories, there was a collective compatibility regarding their underpinning politics and epistemologies (Bevan 2007).
Methodological limitations of the studies
The findings from the majority of studies were supported by plentiful, conceptually‐rich data (i.e. depth, detail, and breadth of evidence). Most of the studies also provided detailed descriptions of the setting(s), and the broader socioeconomic and political contexts in which the research was conducted. This extensive reporting of data and context may be attributable, at least in part, to the fact that many of the studies were described in multiple sources: the 27 sampled studies were reported in a total of 53 full texts, including three books. Moreover, many of the articles were also published in social science journals, which are frequently less stringent with word limits in comparison to health research journals.
Across most of the studies, however, there was generally poor reporting of the methods employed, a relatively common characteristic of sociological and anthropological research (Green 2004). In particular, most studies provided little or no detail of both the sampling strategies employed and data analysis methods. Evidence of reflexivity and sensitivity to ethical concerns were also limited in the majority of studies. Thus, the methodological limitations of most studies primarily related to poor or inadequate reporting, which made it challenging for us to assess the appropriateness of the research methods utilised. Details of the assessments of methodological limitations for individual studies can be found in Appendix 2.
Confidence in the review findings
We used the GRADE‐CERQual approach to grade our confidence in 19 review findings. We graded seven as high confidence, eight as moderate confidence, and four as low confidence.
Our main concerns were connected to the methodological limitations of the studies and the relevance of the data. Common methodological limitations included limited evidence of researcher reflexivity and sensitivity to ethical considerations, as well as poor reporting of sampling and data analysis methods. The data were often assessed as being only partially relevant, mainly because the studies contributing to the finding came from specific countries (e.g. only HICs); or included a subset of the population of interest (e.g. only parents who do not accept vaccination according to the recommended schedule); or focused on specific vaccines (e.g. only MMR or only polio vaccines). We downgraded some findings due to concerns about coherence, usually because of some ambiguous data. Many of the review findings were interpretive or explanatory in nature, and as such, were often complex and comprised multiple aspects. In cases where there was strong evidence for some aspects of the review finding, but insufficient data to support other aspects, we downgraded the review finding due to concerns about coherence. Our explanation of the GRADE‐CERQual assessment for each review finding is shown in the evidence profiles (Appendix 4).
Review findings
We present summaries of the findings and our assessments of confidence in these findings in the Table 1. We present detailed descriptions of our confidence assessments in the evidence profiles (Appendix 4). The different types of findings we developed, and their relationships, are graphically depicted in Figure 3, Figure 4, Figure 5, and Figure 6.
1. Themes
In the following themes, we have synthesised the views and interpretations of the study authors regarding the factors influencing parental views and practices around routine childhood vaccination, and have used direct study participant and study author quotes to contextualise and illustrate meaning.
Theme 1: ideas and practices surrounding (child) health and illness
Parents' ideas and practices regarding routine childhood vaccination may be influenced by their broader ideas and practices surrounding health and illness generally, and specifically with regards to their children, and their perceptions of the role of vaccination within this context. That is, the way parents think about vaccination may be shaped by their conceptions of child health specifically, influences on it, and strategies to protect it and prevent illness. As suggested by the authors of various studies (Bisht 2000; Millimouno 2006; Leach 2007; Giles‐Vernick 2016), what appears to matter with regards to acceptance of vaccination (or not), is whether parents’ own ideas about child health (and associated therapeutic traditions) fit with their own ideas about vaccines and what they can do. In other words, parents may accept vaccination even if they hold views about health and vaccination that fail to match or even contradict biomedical understandings of health, disease, and immunity. At the same time, parents may reject vaccination even if they hold 'correct' biomedical views about health and vaccination. What seems important regarding vaccination acceptance (or not), is whether parents' subjective beliefs about vaccines are compatible (or incompatible) with their subjective beliefs about health and illness.
Six specific second‐order findings emerged within this broader theme as implicated in vaccination views and practices: 1) religious beliefs; 2) the ‘fragile’ infant; 3) primacy of ‘nature’ and ‘the natural’; 4) individualised health, immunity, and vaccine‐response trajectories; 5) claiming parental expertise; and 6) personal choice and responsibility.
Finding 1: religious beliefs. Some parents were less accepting of childhood vaccination due to the religious beliefs they held, and the view that illness, including in children, can only be prevented by divine providence. These parents expressed religious objections to vaccination (low confidence).
Two studies, one in the Netherlands (Ruijs 2012), and one in Nigeria (Renne 2010), revealed that some parents were less accepting of childhood vaccination due to the religious beliefs they held. For example, many orthodox Protestant parents in a study in the Netherlands held the view that illness, including in children, can only be prevented by divine providence, and as such, expressed religious objections to vaccination: “Whether I have my children vaccinated or not does not matter to me because I don’t believe in it. I believe that if God wants to spare my children from an accident, then He will spare them from it” (Ruijs 2012, the Netherlands, participant quote). Similarly, while many Muslim parents in a study in Northern Nigeria accepted vaccination for their children, others viewed vaccination as unnecessary or even possibly dangerous (Renne 2010). As suggested by the author of this study, this view was underpinned by these parents’ understanding of prayer as the only sufficient and real protection against disease, which they believed to ultimately come from God: “If God wishes, the one who had immunisation will be sick but the one who didn’t have immunisation will be in good health” (Renne 2010, Nigeria, participant quote).
Finding 2: the ‘fragile’ infant. An understanding of infants and their immune systems as fragile and still in a state of development was common amongst parents across diverse settings, contexts, and population groups. Numerous parents characterised infants and young children as weak and vulnerable, and in need of protection against multiple social, biological, or spiritual threats. This perception was associated with both reduced and increased acceptance of childhood vaccination (high confidence).
An understanding of infants and their immune systems as fragile and still in a state of development was ubiquitous amongst parents across diverse settings, contexts, and population groups (Bisht 2000; Brownlie 2005; Poltorak 2005; Millimouno 2006; Casiday 2007; Leach 2007; Brunson 2013; McKnight 2014; Giles‐Vernick 2016; Reich 2016; Smith 2017; Limaye 2020). Numerous parents characterised infants and young children as weak and vulnerable, and in need of protection against multiple social, biological, and spiritual threats. However, the studies revealed refutational findings in the way this common understanding of infancy impacted upon vaccination, reducing acceptance in some studies and increasing acceptance in other studies. We interpreted this refutation as related to differences in study settings and associated potential sociocultural variations in how vaccines, and what they do, are commonly understood.
Various studies from the USA and United Kingdom revealed that some parents were less accepting of childhood vaccination due to the perception they had of infancy as precarious (Brownlie 2005; Poltorak 2005; Casiday 2007; Brunson 2013; Reich 2016; Smith 2017; Limaye 2020). This perception gave rise to several specific concerns about vaccination. Some of these parents were concerned about unnecessary pain and suffering they perceived vaccination would cause (Brownlie 2005; Smith 2017): “It was just the fact that you don’t want to inflict pain on this wee helpless baby” (Brownlie 2005, UK, participant quote). Other parents’ concerns centred on what they saw as the overwhelming effects of vaccination, which they feared an infant is too weak to withstand (Brownlie 2005; Poltorak 2005; Casiday 2007; Brunson 2013; Reich 2016; Smith 2017; Limaye 2020). Many parents pointed to the side effects or adverse reactions that sometimes occur with vaccination as evidence of this overwhelming effect (Reich 2016; Smith 2017). In certain instances, this view underpinned parents’ decision to delay or postpone vaccination for when their child was older and their immune system supposedly stronger: “I’ll revisit [vaccination] with him when he gets older… his body will be bigger, his immune system will be stronger then” (Brunson 2013, USA, participant quote).
Many parents who were concerned about the overwhelming effects of vaccination on infants were particularly uneasy about the combined vaccines, such as the triple MMR vaccination, or vaccination schedules requiring multiple vaccines simultaneously (Brownlie 2005; Poltorak 2005; Casiday 2007; Reich 2016; Smith 2017). They queried whether infants have the capacity to handle combined or multiple vaccines, commonly describing these as “excessive” (Poltorak 2005, UK, participant quote), “too much at one go” (Brownlie 2005, UK, participant quote), an “unnecessary overload into such a young body” (Smith 2017, UK, participant quote), or as one parent recounted her reaction to her doctor’s suggestion that her baby be given six vaccines in one day: “I was like, ‘my child is eighteen pounds and you’re gonna give her six shots today?’ I said, ‘No. No. We’re not doing that’” (Reich 2016, USA, participant quote). These concerns underpinned some parents’ decision to develop their own, more evenly spaced‐out immunisation schedules or to seek out separate injections, not necessarily available as part of state‐funded, routine immunisation programmes (Brownlie 2005; Poltorak 2005; Casiday 2007; Reich 2016; Smith 2017).
In contrast, the findings from studies in multiple African countries (Gambia, Guinea, Central African Republic, Burkina Faso, and Ethiopia) (Millimouno 2006; Leach 2007; McKnight 2014; Giles‐Vernick 2016), and a study in India (Bisht 2000), suggest that the common understanding of the fragility of infants contributed to enhancing many parents’ acceptance of vaccination. Various authors of these studies stated that, in many West African (Millimouno 2006; Leach 2007), and South Asian countries (Bisht 2000), there is a common belief that injections, including vaccines, are powerful substances which go directly into the blood and play multiple positive roles: preventative, strength‐building, and curative. This perception is clearly conveyed by one parent’s description that, “Vaccines build up the strength, like Ravita's [her daughter] cough was cured after she was given the injection [vaccine]” (Bisht 2000, India, participant quote). Further, the authors of these studies suggest that many parents in various West African and South Asian countries also frequently understand the side effects or adverse reactions that sometimes occur with vaccination as signs of the effectiveness of vaccines in the body (Bisht 2000; Millimouno 2006; McKnight 2014). As this quote from a parent in Guinea aptly illustrates, “The reactions felt by the infant after vaccination are normal. They show that this is eliminating the illnesses found in the body” (Leach 2007, Gambia, participant quote).
Many parents in these studies in Africa and India therefore had understandings of vaccines that did not neatly align with biomedical notions of immunity and vaccination. Yet their acceptance of vaccination appeared to relate to the congruency between their own understanding of vaccination and what it does, and their own understanding of infants and what they need. As such, many parents in these settings strongly accepted vaccination, and incorporated it amongst the range of other practices they employed for protecting and promoting child strength and well‐being (Bisht 2000; Millimouno 2006; Leach 2007; Giles‐Vernick 2016). This is evident in the following description given by a parent from Guinea: “He received his first vaccination the day after his birth. To protect him against wind and illness, his father bought him clothes as a means of protection, and we tied a string to his right hand to stop him getting thin, because he was very fat. When a child is born we tie this string, made with Koranic writing, because when certain people praise the baby, he can start to have health problems” (Leach 2007, Guinea, participant quote).
Finding 3: primacy of ‘nature’ and ‘the natural’. Some parents, predominantly from HICs, were less accepting of childhood vaccination due to their understanding of health and illness as holistic or naturalistic. This understanding conceives many biomedical interventions, including vaccination, as unnatural intrusions that are unnecessary or harmful. Various parents who held this view also engaged in certain ‘natural’ health‐promoting activities or “salutogenic parenting”, which for them further negated the need for vaccination (high confidence).
Some parents were less accepting of childhood vaccination due to their understandings of health and illness, variably labelled by study authors as “holistic” (Casiday 2007; Ward 2017), “natural” (Barbieri 2017), “naturalistic” (Poltorak 2005; Brownlie 2005; Reich 2016; Peretti‐Watel 2019), “homeopathic” (Rogers 1995), or “alternative” (Dube 2016). As described by the authors of these studies, this understanding of health and illness posits that the body generally and the immune system more specifically are ‘naturally’ robust and balanced. From this perspective, many biomedical interventions, including vaccination, are seen as unnatural or artificial intrusions, ultimately compromising the body’s natural equilibrium and innate capabilities to prevent or cure diseases. Therefore, people who hold this view often have a strong preference for ‘natural’ health interventions over what they see as chemical or technologically‐mediated health interventions. Some study authors suggested that this view of health and illness is potentially more pervasive amongst parents from higher socioeconomic groups (Rogers 1995; Barbieri 2017; Peretti‐Watel 2019), although the findings from other studies suggest that these views may occur across socioeconomic divides within HICs (Casiday 2007; Brownlie 2005).
Parents holding this view of health and illness expressed a variety of interrelated concerns about vaccination. Some concerns centred around what was seen as the ‘artificial immunity’ granted by vaccines. Natural immunity – that is, immunity from diseases – was viewed by many of these parents as essential for the development of a child’s immune system, and also superior to the immunity conferred by vaccines (Rogers 1995; Brownlie 2005; Dube 2016; Reich 2016; Peretti‐Watel 2019): “To develop the immune system you need to have certain diseases and afterwards, you’re stronger and you develop antibodies” (Dube 2016, Canada, participant quote). Some parents suggested that vaccines could also harm the immune system, or undermine the body’s natural immune capabilities (Poltorak 2005; Dube 2016; Reich 2016; Carrion 2018). Other concerns related to what were perceived as the chemicals, preservatives, and adjuvants within vaccines, and the potentially toxic and harmful effect of these (Brownlie 2005; Poltorak 2005; Dube 2016; Reich 2016; Peretti‐Watel 2019): “Aluminum, mercury, I don’t want to pollute my child’s body with that… I think the body reacts better to diseases if it is clean” (Peretti‐Watel 2019, France, participant quote). As implied by this parent and suggested by various study authors (Poltorak 2005; Reich 2016; Peretti‐Watel 2019), many parents who were worried about the toxicity of vaccines were particularly apprehensive about those containing aluminium or mercury.
An additional trepidation expressed by parents concerned what was seen as the ‘unnatural’ way injectable vaccines enter the body, a mode of absorption which was described as different to the route that viruses or bacteria antigens enter the body (Rogers 1995; Dube 2016; Reich 2016; Ward 2017): “If you inject something into the blood stream it doesn't go through the normal sort of defense mechanisms of the body” (Rogers 1995, UK, participant quote). Some study authors found that this concern underpinned parents’ rejection of injectable vaccines, but acceptance of oral vaccines (Reich 2016; Ward 2017).
Many parents who expressed a ‘holistic’ view of health and illness also described engaging in a range of ‘natural’ health‐promoting and immune‐boosting activities (Rogers 1995; Reich 2016), or what study authors referred to as “salutogenic parenting” (Ward 2017), or “labour‐intensive parenting practices” (Peretti‐Watel 2019). These activities included, for example, reducing exposure to environmental chemicals and toxins (e.g. living ‘off the grid’; eating organic or home‐grown food, or both; avoiding plastics and cleaning products in the home), pursuing ‘alternative’ schooling, natural births, long‐term breastfeeding, and using complementary and alternative medicine (CAM). In addition to enhancing the natural immunity of their children and protecting them from illness, some parents believed these activities also negated or reduced the need for vaccination (Rogers 1995; Reich 2016; Ward 2017; Peretti‐Watel 2019). These beliefs are aptly depicted in the following comment made by a parent from Australia: “I grow vegetables and I have chickens I mean, I feed my children organic food, I cook everything from scratch. I don't give them processed food. We have no chemicals in the house. We don't drink fluoridated water, we drink rainwater which has been filtered. So why would I then go and put all those chemicals in my child?” (Ward 2017, Australia, participant quote).
Finding 4: individualised health, immunity, and vaccine‐response trajectories. Many parents, predominantly from HICs, held a view that children possess unique bodies and immune systems, and therefore, individual vaccine needs and vulnerabilities. As such, these parents frequently assessed the risks and benefits of vaccines as they pertain to their specific child, rather than in general. If the risks were seen to outweigh the benefits for their particular child, then these parents tended to be less accepting of childhood vaccination (high confidence).
Studies from various HICs (USA, Canada, United Kingdom) found that numerous parents are of the view that children possess unique bodies and immune systems, and thus also individual vaccine needs and vulnerabilities (Rogers 1995; Brownlie 2005; Poltorak 2005; Casiday 2007; Brunson 2013; Dube 2016; Reich 2016; Sobo 2016; Smith 2017). This finding also emerged in one study conducted in an LMIC: this belief was found to be commonplace amongst parents from middle and higher socioeconomic groups in a study conducted in São Paulo, Brazil (Barbieri 2017). This idea of the individuality or particularity of each child meant that, for many parents, the risks and benefits of vaccination are not set values that can be meaningfully captured by population‐level data or generalised risk calculations. As proposed by this parent, and capturing the views of many other parents, “I think statistics are a bit meaningless from a ‘I want to protect my baby point of view’” (Brownlie 2005, UK, participant quote). Rather, children were thought to possess unique vaccine needs and vulnerabilities that vary depending on their particular composition and socio‐familial circumstances. Consequently, and as articulated by the authors of one study, for many parents, vaccination benefits, risks, and safety tend to be situated within the individual, with these notions framed “not in general”, but “for my child” (Poltorak 2005).
Thus, when deciding whether to vaccinate their child (or not), many parents “individualised” or “particularised” (Poltorak 2005) the risks and benefits of vaccination for their individual child. This approach to vaccination was pertinently revealed in parents’ accounts of their vaccination decision‐making processes. Here, many parents described a meticulous process of considering the various strengths and weaknesses of their child which may make them more (or less) vulnerable to disease or to vaccination adverse effects (Rogers 1995; Poltorak 2005; Casiday 2007; Brunson 2013; Reich 2016; Smith 2017). Several characteristics were commonly considered in this regard, including a child’s current and past health status, their socio‐familial living circumstances, and the family’s health history and potential genetic predispositions. For example, when evaluating the appropriateness of a specific vaccine or vaccines in general, many parents described assessing their child’s health status, often taking into account aspects related to their birth, feeding and sleeping patterns, dietary intolerances, allergies, and current or past illnesses (Rogers 1995; Casiday 2007; Reich 2016; Smith 2017). These factors were considered important for determining whether their child might be less resilient or of an especially weak constitution. For many parents, this additional fragility was perceived to reduce their capacity to handle vaccines and to increase their susceptibility to adverse vaccination outcomes. This underpinned some parents’ decision to avoid or delay vaccination until their child’s constitution had strengthened or a period of particular susceptibility had passed: “When he was small ‐ he was really small, he got pneumonia. Because he’d had pneumonia I didn’t want to give him the needle” (Smith 2017, UK, participant quote).
Another factor commonly considered by many parents when making a vaccination decision for their child was the health history and potential genetic predispositions of their family (Brownlie 2005; Poltorak 2005; Reich 2016). A history of family conditions, such as allergies, digestive disorders, cancer, autism, and various other neurological or autoimmune problems, was identified by many parents as making vaccination particularly risky for their child: “I think if my husband’s family didn’t have this thing, my daughter’s uncle who we think has Crohn’s, if that wasn’t there then I’d be ‘fine, I’ll put her in for it’” (Brownlie 2005, UK, participant quote).
An additional consideration for many parents was their socio‐familial living circumstances (Poltorak 2005; Casiday 2007; Brunson 2013; Reich 2016; Smith 2017). For example, some parents considered whether they intended to send their child to nursery school, or whether, as a family, they plan to travel overseas a lot in the future – scenarios which they felt would enhance their child’s risk of contracting a vaccine‐preventable disease and thus increase their need for vaccination (Casiday 2007; Brunson 2013; Reich 2016; Smith 2017).
Many parents were also of the view that a healthy living environment potentially reduces a child’s need for vaccination (Poltorak 2005). Those parents who held a ‘holistic’ understanding of health and illness (see above, "‘Primacy of ‘nature’ and ‘the natural’’), were particularly confident that the lifestyle their family leads mitigates disease risk and renders vaccination unnecessary for their child. This belief is illuminated by this parent’s explanation for why she decided not to vaccinate her daughter: “We also are very conscious about how she eats and how, you know, that she eats mostly organic food… I made all of her food at home the first—when she started solids—and so we try to keep her immune system strong in that sense as well” (Reich 2016, USA, participant quote).
Many parents considered these different factors related to their child, their family, and their living circumstances simultaneously. The following narrative by one parent clearly captures the type of thought processes many parents conveyed in this regard: “My child suffers with severe eczema… therefore I did not want her to have MMR when her eczema is still so bad, and make it worse. My first child has always caught chest infections from colds plus doesn’t eat a varied diet. He is not particularly robust. We have a strong family history of very bad hay fever, eczema, asthma and food allergies” (Poltorak 2005, UK, participant quote).
Depending on the individual risk‐benefit assessment made, parents may reject all vaccines, or design what the authors of one study described as a more “personalised approach to vaccination” (Poltorak 2005). That is, they may develop delayed, slow, or alternative vaccine schedules for their child, choosing to have some vaccines which they consider beneficial and safe, against the illnesses which they believe require protection, at a time when they consider to be most appropriate (Poltorak 2005; Reich 2016). Ultimately, they may seek to tailor the recommended vaccination schedule according to what they perceive as their child’s specific vaccination needs and vulnerabilities.
As these needs and vulnerabilities potentially change, so too do many parents’ risk assessments and associated vaccination decisions. As suggested by various study authors, parents’ individualised risk assessments are often not static or fixed, but change as personal, familial, or environmental factors change (Rogers 1995; Poltorak 2005; Brunson 2013; Dube 2016; Reich 2016; Sobo 2016). Many parents explicitly highlighted the nonfinality of their vaccination decisions, and how they would reconsider their decision if and when circumstances change. As one parent put it, “I never am settling for what I’ve decided upon thus far… It’s not a decision that it’s just very black and white and once it’s made it’s made, it’s very fluid…” (Brunson 2013, USA, participant quote).
Finding 5: claiming parental expertise. Many parents from HICs held a view of themselves as experts of their child, possessing the best understanding of their child’s health strengths and vulnerabilities. They in turn considered themselves best placed to judge their child’s vaccination needs and risks (moderate confidence).
Studies from various HICs (USA, Australia, United Kingdom, France) found that another common perception amongst parents is a view of themselves as experts of their children (Petts 2004; Poltorak 2005; Casiday 2007; Brunson 2013; Johnson 2014; Reich 2016; Sobo 2016; Ward 2017; Carrion 2018; Peretti‐Watel 2019). That is, many parents felt that they know their own children better than anyone else and have the best understanding of their children’s unique health strengths and vulnerabilities. One study author explicitly ascribed this view of parental expertise to two main factors: a sense of instinct or experiential intuition that parents perceive to come from being a parent, and the widespread information‐seeking activities that many parents described undertaking (Reich 2016). Other studies corroborated this study author’s view on the reasons for this perception of parental expertise (Petts 2004; Poltorak 2005; Casiday 2007; Brunson 2013; Johnson 2014; Sobo 2016; Ward 2017; Carrion 2018; Peretti‐Watel 2019).
In terms of the first factor, numerous parents spoke about the “gut feeling” or “instinct” (Johnson 2014, UK, participant quote), “intuition” (Reich 2016, USA, participant quote), or “mommy gut” (Carrion 2018, USA, participant quote), that they have about their own children. Some study authors referred to this type of knowledge as “experiential expertise” (Poltorak 2005), or as “maternal epistemology” (Carrion 2018), which they defined as the knowledge which is gained and maintained from the daily observations and interactions of parents with their children, and which provides them with a sense of intimate knowledge about their children. This sense that parents have of themselves was encapsulated in the widespread remarks made by parents that “you know best” (Reich 2016, USA, participant quote), and “just go and follow your instincts in the end” (Johnson 2014, UK, participant quote), or as one parent articulated categorically, “It’s really gonna come down to your gut. You know what you know about your child, and weighing the risks and benefits in your own mind… you’re the only person who knows what you know” (Carrion 2018, USA, participant quote).
The second factor underpinning parents' sense of themselves as experts of their children was the extensive information‐seeking activities that many described undertaking around health‐related issues, including vaccination (Petts 2004; Poltorak 2005; Casiday 2007; Brunson 2013; Reich 2016; Sobo 2016; Ward 2017; Carrion 2018). Numerous parents reported investing tremendous amounts of energy into “doing their research” (Carrion 2018, USA, participant quote), “reading widely” (Ward 2017, Australia, participant quote), and “gathering as much information as we could” (Reich 2016, USA, participant quote), to proactively inform themselves about vaccination. As one parent put it: “It was a long, drawn out process. I mean we went back and forth… we made worksheets and we read books and went to workshops and brought back information” (Brunson 2013, USA, participant quote). Like this parent, numerous parents highlighted consulting many and varied forms of information from different sources so they could obtain multiple perspectives (Petts 2004; Casiday 2007; Brunson 2013; Sobo 2016; Peretti‐Watel 2019). Several parents also described questioning and being critical of all the sources of vaccination information they consulted, and particularly the internet and social media (Petts 2004; Casiday 2007; Ward 2017; Peretti‐Watel 2019). Indeed, the internet and social media were portrayed by some parents as “sensationalism”, creating “hype”, and “blowing risks out of proportion” (Petts 2004, UK, participant quotes). Many parents explained that these sources need to be viewed with considerable caution as “anybody could put anything on the Internet” (Casiday 2007, UK, participant quote).
Therefore, and as suggested by various study authors, many parents engaged “reflexively rather than passively” with regards to vaccination information (Peretti‐Watel 2019), or as the authors of another study put it, “[w]hile the media are identified as important sources of information, there is no evidence to suggest that parents passively receive and act upon such risk messages” (Petts 2004). Some parents even recounted in detail the strategies they undertook to filter and critically appraise the information they consulted (Ward 2017; Peretti‐Watel 2019). One parent from a study in France typifies the type of narrative many parents provided regarding the processes they undertake to assess the validity of information: “The internet I cross‐check and I make sure that info A is not a copy‐paste of info B and vice versa… because often if I’ve seen it on many sites… if you look it’s the same original info that’s spread, that people pick up from one another… and I try to have several really different sources” (Peretti‐Watel 2019, France, participant quote).
The studies revealed inconsistent (refutational) findings around how parents experience this process of seeking information about vaccination and consulting multiple (sometimes conflicting) sources of information. Some studies found that it created anxiety and confusion for many parents (Poltorak 2005; Casiday 2007; Ward 2017). In contrast, one study found that parents highly enjoyed their information‐seeking activities and actually celebrated the varied perspectives they came across, or what the study authors referred to as “valorised multivocality” (Sobo 2016). This study found that these parents purposively sought out diverse or conflicting opinions, and were suspect of anyone who held one‐sided views. We did not identify any obvious methodological or theoretical explanations for these different findings. We interpreted it to mean that parents' experiences of seeking information about vaccination and consulting numerous sources of information vary.
However, what did appear to be common amongst parents across these studies was the value and importance placed on seeking widespread information about vaccination, even if it may cause anxiety or confusion. Many parents understood educating yourself about health‐related issues, including vaccination, as a sign of good parenting and evidence of one’s commitment to one’s children (Brunson 2013; Reich 2016; Sobo 2016; Ward 2017; Carrion 2018). This emerged most pertinently in the vaccination advice so many parents reported giving (or would give) to other parents, where it was very common for parents to make remarks such as: “I would say… just do your research” (Ward 2017, Australia, participant quote), and that “[m]y only piece of advice would be just to do as much reading and research” (Reich 2016, USA, participant quote), or as one parent explained, “I think as long as you research, and you are making an informed decision, then whatever decision you’re making is the right one whether you vaccinate or not” (Carrion 2018, USA, participant quote). As noted by the author of this study, for this parent, like many others, a ‘right’ vaccination decision was determined by the process used to produce it (rather than the outcome), and whether it was underpinned by a thorough process of information seeking (Carrion 2018).
Finding 6: personal choice and responsibility. Many parents, predominantly from HICs, perceived healthcare decision‐making, including vaccination, to be a matter of personal responsibility and choice. In cases where the risks of a vaccine or vaccination in general were thought to outweigh the benefits for their particular child, then these values of personal responsibility and choice were often prioritised over collective responsibility. These parents in turn tended to be less accepting of vaccination for their children (high confidence).
Another common perception amongst parents in various HICs (USA, United Kingdom, Australia) was that health‐related decisions, including those pertaining to vaccination, are matters of personal choice (Rogers 1995; Petts 2004; Brownlie 2005; Poltorak 2005; Casiday 2007; Brunson 2013; Johnson 2014; Reich 2016; Sobo 2016; Ward 2017; Carrion 2018). This finding also emerged in one study conducted in an LMIC: this perception was found to be commonplace amongst parents from middle and higher socioeconomic groups in a study conducted in São Paulo, Brazil (Barbieri 2017). Parents’ accounts about vaccination in these studies were replete with discourses relating to personal choice and the right to choose. As one parent unambiguously stated with regards to the advice she would give to a friend about vaccination, “I would tell her… to really know that it is her baby and it’s her choice. It is not her doctor’s choice, it is not her mom’s choice, it’s not her neighbour’s choice, and it is not her school’s choice (Carrion 2018, USA, participant quote).
As suggested by the authors of one study (Poltorak 2005), and supported by the findings of other studies (Petts 2004; Brownlie 2005; Casiday 2007; Johnson 2014; Reich 2016), the importance attributed to personal choice in vaccination decision‐making was closely linked, and in some cases predicated upon, a strong sense of personal responsibility that many parents expressed with regards to their child. Numerous parents saw themselves as personally responsible for their children’s health and healthcare decision‐making, holding themselves individually accountable for their health outcomes (Rogers 1995; Poltorak 2005; Casiday 2007; Johnson 2014). The sense of self‐blame many parents conveyed with regards to making the wrong health‐related choices for their children was palpable. Vaccination choices were no exception, as manifest in recurring statements such as: “I couldn’t forgive myself if my child became autistic” (Poltorak 2005, UK, participant quote), “ultimately I would be responsible” (Reich 2016, USA, participant quote), “you could only blame yourself really” (Petts 2004, UK, participant quote), or as one parent lamented, “[a]lthough it might be a very, very small percentage risk, it’s your child and if it gets that, you have to deal with that for the rest of your life, I mean would you ever forgive yourself? To feel that you were responsible and that you could have prevented that” (Brownlie 2005, UK, participant quote).
Making the right health‐related choices and taking responsibility thus materialised in the studies as a sign of good parenting and a moral imperative for countless parents. Many studies found that this strong sense of personal responsibility around vaccination decisions also took precedence over societal considerations for many parents (Petts 2004; Poltorak 2005; Casiday 2007; Reich 2016). That is, while most parents understood claims of social or collective responsibility with regards to vaccination, for many, this was of lesser importance than their sense of individual responsibility to protect their own child. When justifying their vaccination decisions, many parents stated unequivocally how “[i]t’s solely, I just want what’s best for my children” (Reich 2016, USA, participant quote), or “I am not prepared to risk my child’s health” (Poltorak 2005, UK, participant quote), or as one parent confessed, “I did think about benefits to other children but it was very much secondary to what was best for Molly” (Petts 2004, UK, participant quote).
Theme 2: social communities and networks
For many parents, their vaccination ideas and practices, and the social networks in which they are embedded, exist in a potentially mutually reinforcing relationship, both shaping and being shaped by each other (Leach 2007).
Finding 7: social networks shape vaccination ideas and practices. Parents vaccination views and practices, across diverse settings, contexts, and population groups, were influenced by the vaccination views and experiences of their social networks. These networks included relatives, peers, neighbours, and additional significant others in the community. However, the views and practices of other parents, and particularly other mothers, were especially influential (high confidence).
Studies across diverse countries, contexts, and populations demonstrated how parents’ views and practices regarding routine childhood vaccination were shaped by the vaccination views and practices of the social networks in which they reside (Petts 2004; Brownlie 2005; Poltorak 2005; Millimouno 2006; Casiday 2007; Leach 2007; Ruijs 2012; Brunson 2013; Varghese 2013; Dube 2016; Giles‐Vernick 2016; Sobo 2016; Barbieri 2017; Ward 2017; Peretti‐Watel 2019). Even parents in the studies that talked about vaccination as a matter of individual responsibility and choice revealed in their narratives the social situatedness of both this conceptualisation and their vaccination decisions. As the authors of one study suggested (Leach 2007), and supported by other authors (Peretti‐Watel 2019), “a sense of individual responsibility does not suggest that people are simply thinking and acting as atomised individuals; rather, it goes along with the forging of social relations and forms of community”.
The studies revealed that when parents make decisions about vaccination, together with other issues regarding child health and health care, they do so as members of societies and communities. Health and health care are topical issues that frequently generate much discussion in social settings: parents interact and talk with members of their community, they share their personal opinions and experiences, they exchange advice, and they learn from each other (Leach 2007). While community members include relatives, peers, neighbours, and other significant members of the community, across numerous studies, other parents emerged as particularly influential.
Several parents described the interactions they have with other parents as especially valuable and helpful (Petts 2004; Poltorak 2005; Johnson 2014; Dube 2016). Numerous parents spoke about how “I talk a lot to other mothers” (Poltorak 2005, UK, participant quote), and “[i]t is the experiences of my friends, my close friends that also have children” (Dube 2016, Canada, participant quote), or as one mother succinctly put it, “certainly people do talk to health professionals… but I think most people talk to other mums” (Petts 2004, UK, participant quote). As reflected in these excerpts, many parents also suggested the gendered nature of the sociality of vaccination decision‐making. That is, in many settings, mothers were revealed to be the primary vaccination decision‐maker for their children, and therefore the interactions between particularly female relatives, peers, neighbours, and community members emerged as especially strong in shaping vaccination decisions (Petts 2004; Poltorak 2005; Millimouno 2006; Leach 2007; Peretti‐Watel 2019).
Various studies revealed how, in many social situations and communities, vaccination is a valued and legitimate social practice, or what study authors referred to as the “social normalisation of vaccination” (Petts 2004), or a “culture of immunisation” (Barbieri 2017). Consequently, vaccination for many parents in these situations may be an automatic or habitual practice that generates little deliberation. Several parents revealed this element of routinisation in relation to childhood vaccination; a sense that this is just what all parents do (Brownlie 2005; Brunson 2013; Varghese 2013; Johnson 2014; Giles‐Vernick 2016; Sobo 2016; Barbieri 2017). Many described their acceptance of vaccination from an ‘everyone does it’ point of view, as exemplified by this parent's explanation: “I think what it still boils down to that’s just what’s expected of you … it’s a society thing isn’t it? This is when your child has these things so you do it” (Johnson 2014, UK, participant quote). Many other parents shared this parent’s view, providing similar accounts of how “[i]t’s the first time I’ve thought about it (Barbieri 2017, Brazil, participant quote), or that “I hadn’t really given it huge amount of thought” (Brownlie 2005, UK, participant quote), and that it was a foregone conclusion to “just turn up and get it done” (Petts 2004, UK, participant quote). For other parents, a ‘culture of vaccination’ made it a practice that was difficult to evade, as it would entail potential stigmatisation and condemnation from others (Brownlie 2005; Millimouno 2006; Casiday 2007; Leach 2007; Varghese 2013; Giles‐Vernick 2016; Peretti‐Watel 2019). This was starkly illustrated in a study from Burkina Faso, where a parent provided an impassioned description of the social pressures of vaccination: “When they tell you to come out [to vaccinate your child] one day and everybody comes out… you can’t refuse!” (Giles‐Vernick 2016, Burkina Faso, participant quote).
However, in other situations and communities, vaccination hesitancy or nonacceptance is a socially desirable stance; a norm imbued with high social value. In these situations, various parents explained how their decision not to vaccinate their children was just following that tradition (Ruijs 2012; Brunson 2013; Sobo 2016; Ward 2017). One parent clearly articulated this view when she explained why she had delayed vaccinations for her two sons who were born in Santa Cruz, California: “Santa Cruz is very much a hippie area… So very much I was indoctrinated into the hippie ways when my kids were born… and there’s no other way to be in Santa Cruz… if you tried to bottle feed in public in Santa Cruz you would get the filthiest looks on the planet” (Ward 2017, Australia, participant quote).
Similarly, parents in one study highlighted how they started questioning vaccination when they found themselves in a new social group or setting in which nonacceptance of vaccination was highly valued (Ward 2017). The authors of this study found that this change in sentiment facilitated these parents’ integration and sense of belonging within their new social circumstances. Many parents also described the difficulties they faced going against the social norm of vaccination nonacceptance. They spoke about the blame and ostracism they had experienced (or would experience) if they vaccinated their child in such settings. This view is clearly reflected in the following statement from a parent in India: “Nobody here is too keen about injections. It is difficult for me to take initiative… I am in favour of this [vaccination]. But if I decide alone and take the child for vaccination and after that if the child develops even a cold, all blame will be on me” (Varghese 2013, India, participant quote).
Therefore, the social networks in which parents resided constituted a powerful force, influencing the vaccination views they held and the actions they were willing or unwilling to take. Various study authors attempted to explain how and why this is the case, similarly suggesting that it may relate to the manner in which views about vaccination – whichever stance is taken – form an integral part of parents’ identification processes (Brunson 2013; Sobo 2016; Ward 2017). That is, and as articulated by the authors of one study, the practice of vaccination is “an act of identification ‐ of opting in ‐ of proclaiming ‘I belong’ and ‘I share your values’” (Sobo 2016). In other words, through their vaccination views and practices, parents proclaim their affiliation or social communion with particular communities and associated in‐group norms and values. These authors go on to suggest how, in circumstances when nonacceptance of vaccination or vaccination hesitancy is a social norm, the “opting out” of vaccination can be understood as a “positively prosocial act” of accepting or “opting in” to the values, identities, and lifestyles of a particular community. Conformity to the norms, values, and lifestyles of a social group can be very rewarding for individuals, whereas noncompliance can have negative consequences. As one study shows, drawing on sociologist Pierre Bourdieu’s concept of capital (Bourdieu 1977; Bourdieu 1984), vaccination and nonvaccination, like many other social practices (eating, food, school choices, birth practices, etc.) are ascribed high value or ‘symbolic capital’ within different communities and settings (Ward 2017). Enactment of practices with high symbolic capital promoted social inclusion for parents and a sense of belonging. However, enacting practices of low value or ‘symbolic capital’ strained social relations and contributed to social exclusion and ostracism for many parents.
Finding 8: vaccination ideas and practices shape social networks. Parents' vaccination views and practices also shaped their social networks. Shared vaccination ideas and practices were a powerful force in building social relations and ties. While this phenomenon occurred amongst parents across the spectrum of vaccination attitudes, it may be particularly significant for parents who are less accepting of vaccination. In these cases, parents may be afforded access to various types of social resources, in turn potentially reinforcing both their group affiliation and their vaccination views and practices (moderate confidence).
Various studies demonstrated how, at the same time that parents’ social networks influenced their vaccination ideas and practices, through these ideas and practices social networks were also being forged, consolidated, or reinforced (Poltorak 2005; Millimouno 2006; Leach 2007; Reich 2016; Ward 2017 ). In other words, and as articulated by the authors of one study, vaccination views and practices were also implicated in the making of different types of kinships and collectivities (Leach 2007).
Through shared vaccination ideas and practices, parents were able to forge new social relations, or to affirm or strengthen existing ones. For example, authors of one study in the United Kingdom found that the sharing of similar views around the MMR vaccination provided a “common camaraderie among mothers”, the “fomenting of relationships with other mothers”, and the “affirming of a new and growing identity as mother” (Poltorak 2005). Similar conclusions were drawn from authors of studies in the USA (Reich 2016), Australia (Ward 2017), Gambia (Leach 2007), and Guinea (Millimouno 2006), where they found that collective mobilisation around vaccine choices and potential dilemmas enabled parents to develop a sense of community amongst themselves, or as the authors of one study put it, to “reinforce kin and friendship ties” and “contribute to and reinforce a valued local community of mothers” (Leach 2007).
This building of communities through shared vaccination ideas and practices was found to occur amongst parents across the spectrum of vaccination attitudes ‐ those who accepted vaccination, those who were hesitant towards vaccination, and those who refused vaccination (Poltorak 2005; Millimouno 2006; Leach 2007). However, two studies suggested that this phenomenon, and its consequences, are particularly significant for parents who are less accepting of vaccination (Reich 2016; Ward 2017). In these cases, the social networks parents acquire through their vaccination ideas and practices frequently provide various types of resources or ‘social capital’ for these parents. For example, they may be afforded with validation for their vaccination choices, further information and support, and acceptance from ‘like‐minded’ others who are often similarly on the fringe of mainstream society (Reich 2016; Ward 2017). As one vaccine‐hesistant parent described, “I feel like in certain circles, I'm kind of an oddball. I try to surround myself with people that are like‐minded because then you feel—it makes you feel more relaxed or like you fit in a little bit more” (Reich 2016, USA, participant quote). Similarly, another parent who had refused vaccination for her children explained how she had developed a “community of other mothers” who all had similar views about vaccination, and how “I guess I’m surrounded by a cohort of people now who are very similar, so I guess we support each other in that way” (Ward 2017, Australia, participant quote). As suggested by the authors of these two studies, this social capital may serve as a buffer against the disapproval parents who are less accepting of vaccination frequently receive from more mainstream society regarding their vaccination choices. At the same time, through such processes, both parents’ affiliations with particular social networks and their vaccination views and practices are potentially further maintained and mutually reinforced (Reich 2016; Ward 2017).
Theme 3: political events, relations, and processes
Parents' ideas and practices regarding childhood vaccination may be influenced by, and sometimes enmeshed with, wider political issues and concerns. As aptly summed up by the authors of one study, “[v]accination is at one and the same time a microtechnological and macro‐political experience” (Leach 2007). These macro‐political issues may range from broader state structures and governmental processes, to global institutions and relations, to ethnic or religious interactions, to economic orders, to the political economy of science. Parental vaccination views and practices are sometimes a means to oppose these wider political processes, relations, and orders.
Finding 9: distrust in the institutions or systems implicated with vaccination. Some parents were less accepting of vaccination due to a lack of, or breakdown in, trust in the institutions or systems implicated with vaccination ‐ most particularly, government, the pharmaceutical industry, and science. The reasons for this distrust were complex and contextually situated, embedded in political events, relations, and processes within specific times and places (moderate confidence).
The notion of distrust emerged across numerous studies as a particularly pervasive concept for understanding the role that wider political concerns play in shaping some parents' ideas and practices regarding childhood vaccination (Rogers 1995; Petts 2004; Brownlie 2005; Poltorak 2005; Casiday 2007; Leach 2007; Chaturvedi 2009; Renne 2010; Varghese 2013; Hussain 2015; Dube 2016; Giles‐Vernick 2016; Reich 2016; Smith 2017; Ward 2017; Carrion 2018; Peretti‐Watel 2019). That is, a lack of, or breakdown in, trust in the institutions or systems implicated with vaccination ‐ most particularly, government, the pharmaceutical industry, and science ‐ materialised strongly in parents’ vaccination discourses. We found that the reasons for such distrust were complex and varied, but could usefully be divided into four main subthemes: 1) generalised decline in trust of authority and expert systems; 2) agendas and interests underpinning the expert systems implicated with vaccination; 3) current and past controversies; and 4) marginalisation, inadequate public services, and priority misalignment.
The authors of one study, however, provide a divergent perspective (Leach 2007). These authors question whether distrust is a helpful or appropriate concept for understanding the political dimensions of vaccination acceptance. They are critical of the vague and highly generalised ways in which the term is frequently used, which they suggest conceals the intricacies of particular political events, relations, and processes of which a so‐called breakdown in trust is a part. More than these issues, however, they argue that the concept of distrust, even when disaggregated and contextualised, may actually obscure more than it reveals. As they explain, “[in] our analyses of vaccination practices…the notion of trust rarely proved helpful. When we used it, on reflection, it is rather as our informants did: as a convenient shorthand to express a more complex, embedded set of meanings that it was perhaps not the moment to articulate in full” (Leach 2007).
Taking heed of their critique, in our description of the political issues at play, we have therefore attempted to move away from what these authors refer to as the “shorthand, universalising qualities” of the concept of distrust, to explaining why trusting relations between parents and institutions in all their “rich diversity and texture” might break down (Leach 2007). Various concepts that these authors propose as alternatives to 'trust' are incorporated in other sections of this review (see, for example, ‘Finding 16: vaccination as a social event’ and ‘Finding 17: interactions with frontline healthcare workers’).
Finding 10: generalised decline in trust of authority and expert systems. For some parents, distrust of the institutions or systems implicated with vaccination may be part and parcel of a more generalised contemporary trend of decreasing trust in authorities and expert systems (low confidence).
Various studies (from the United Kingdom and Australia) attributed some parents' distrust in the institutions or systems implicated with vaccination to a more generalised decline in trust in authorities and expert systems (Brownlie 2005; Casiday 2007; Ward 2017). Various parents in these studies, whether explicitly or by implication, assigned their nonacceptance of, or hesitancy towards, vaccination to their more general feelings of distrust towards government and what it promotes. This was clearly reflected in comments made by parents, such as “I don’t trust like I used to”, and “all governments have lost credibility nobody believes them anymore” (Brownlie 2005, UK, participant quote), or in the words of one parent, “[i]ntrinsically we don't trust them [Government]. Whoever they are, whatever party, there's always a suspicion” (Casiday 2007, UK, participant quote).
One study, however, explicitly refuted this finding (Poltorak 2005). The authors of this study rejected the notion of a deepening decline of trust more generally, suggesting that it is a simplistic and misleading linear interpretation of history that presumes, naively, that trust existed previously, and is only breaking down more recently. The data from their study suggested that levels of distrust in authorities, and associated impact on vaccination, ebb and flow dynamically over time and in relation to specific social and political contexts of the day.
Finding 11: agendas and interests underpinning the expert systems implicated with vaccination. For some parents, distrust of the institutions or systems implicated with vaccination was linked to their concerns about the agendas or interests embedded in these systems. Many of these parents were particularly concerned about the economic interests of these systems, and especially the economic interests of the pharmaceutical industry, which they perceived to be negatively influencing vaccination programmes (moderate confidence).
Studies in various countries (Australia, USA, United Kingdom, Canada, France, India, Central African Republic) found that many parents had concerns about the socio‐political agendas or interests embedded in vaccination programmes. Many of these parents were particularly concerned with what they perceived as the financial interests underpinning vaccination programmes, which in turn led them to question the motivations of those promoting vaccination (Rogers 1995; Petts 2004; Poltorak 2005; Casiday 2007; Varghese 2013; Dube 2016; Giles‐Vernick 2016; Reich 2016; Ward 2017; Carrion 2018; Peretti‐Watel 2019).
For example, parents in various studies in Britain mentioned the targeted payment scheme, introduced in the country in the 1990s, whereby doctors were paid according to the percentage of their patients who were fully immunised (Rogers 1995; Petts 2004; Poltorak 2005; Casiday 2007; Carrion 2018). Many parents described how this scheme caused them to question the advice and information provided by healthcare providers, as they felt their impartiality could be compromised by such incentives: “What I was really concerned about was that they were in no position to have an unbiased view because they are paid a lump sum and they have to get a percentage of children vaccinated… She couldn’t possibly be objective about it” (Rogers 1995, UK, participant quote).
For many parents, most particularly those from HICs, their concerns about the economic interests of the expert systems promoting vaccination specifically centred on the pharmaceutical industry (Dube 2016; Reich 2016; Ward 2017; Carrion 2018). Countless parents in these countries perceived the pharmaceutical industry and its profit motive to be a major force behind vaccination programmes: “Some of the reasons for my reticence toward vaccination come from the fact that vaccines are produced by drug companies that have yes, interest in health but, above all, commercial interests” (Dube 2016, Canada, participant quote). Many parents perceived these commercial interests of pharmaceutical companies to be tainting vaccination systems, including biasing the systems of research, the intentions of health professionals, and the procedures of government. For example, several parents were suspicious of vaccination research, suggesting that studies on vaccines are frequently funded by pharmaceutical companies which are likely to skew or conceal results about risks and inefficacies (Reich 2016; Ward 2017). Illustrating these concerns, one parent explained, “It’s biased because it was paid‐for studies. They’ll take the numbers and twist them” (Reich 2016, USA, participant quote). Various parents also perceived the profit motives of pharmaceutical companies to be tainting the intentions of health professionals (Reich 2016; Ward 2017; Carrion 2018). For example, they alluded to pharmaceutical companies paying doctors to promote vaccines at conferences or subsidising their medical training which, according to this parent and others, ultimately means that “[d]octors just do what they’re told by the pharmaceutical companies” (Carrion 2018, USA, participant quote). Finally, some parents thought that pharmaceutical companies also cast a shadow over the procedures of government, or as one parent put it, “I feel like the pharmaceutical company is getting…a huge say in…how the government chooses to go with those things” (Ward 2017, Australia, participant quote).
Finding 12: current and past controversies. Some parents' distrust of the institutions or systems implicated with vaccination was linked to particular ‘scandals’ or ‘controversies’ related to vaccination specifically or health‐related issues more broadly. The occurrence of such scandals, and the manner in which they were perceived to have been handled, caused some parents to feel misled by authorities and to question their legitimacy in protecting the public’s health (low confidence).
Some parents’ mistrust in the institutions implicated in vaccination may be linked to particular ‘scandals’ or ‘controversies’ related to vaccination specifically or health‐related issues more broadly. The occurrence of such scandals, and the manner in which they are perceived to have been handled, may cause people to feel misled by government or biomedicine, or both, and to question the legitimacy of these institutions in protecting the public’s health (Petts 2004; Brownlie 2005; Casiday 2007). Moreover, and as described by various study authors (Brownlie 2005; Renne 2010; Hussain 2015), health‐related controversies and how they are interpreted do not take place in a vacuum but occur within particular political contexts and historical moments, and are therefore also shaped by these. Health‐related scandals may therefore produce or exacerbate suspicion of government and scientific institutions, suspicions which may spill over into views and practices regarding vaccination. These issues were demonstrated in various studies in different countries (Britain, India and Nigeria) with diverse political contexts (Petts 2004; Brownlie 2005; Casiday 2007; Renne 2010; Hussain 2015).
For example, several parents in Britain explicitly mentioned various current and past health‐related controversies as contributing to their hesitancy towards vaccination (Petts 2004; Brownlie 2005; Casiday 2007). One commonly‐cited event was the Wakefield measles, mumps, and rubella (MMR) controversy, which involved the publication of a now‐retracted research paper in The Lancet in 1998 which linked the combined MMR vaccine to colitis and autism spectrum disorders. Many parents spoke about this controversy, and specially about what they perceived as the British government’s mishandling of it, including what they saw as a defensive and heavy‐handed approach taken (Casiday 2007), how the issue was politicised by some Members of Parliament (Brownlie 2005; Casiday 2007), and the fact that the Prime Minister at the time refused to say whether his son had received the MMR vaccine (Petts 2004; Brownlie 2005; Casiday 2007). According to the authors of all these studies, the view that the British government had mismanaged the controversy seriously undermined many parents' confidence in governmental pronouncements that the MMR vaccine was safe, both at the time of the controversy and for some time afterwards (Petts 2004; Brownlie 2005; Casiday 2007).
Many parents in Britain described the MMR vaccine controversy as just one of various health‐related controversies which they felt had been mismanaged by government and which contributed to their distrust of government. Parents cited, for example, the bovine spongiform encephalopathy (BSE) controversy, and the debates over genetically‐modified foods, as other incidents where they felt the government had lied to the public and pushed a dubious or hidden agenda (Petts 2004; Brownlie 2005; Casiday 2007). The effect of these controversies was aptly summed up by one parent who concluded, “Because of their history of government mismanagement of public health issues in this country I think a lot of people are very, very suspicious when the government says 'oh there's nothing to worry about, don't you worry” (Casiday 2007, UK, participant quote).
One study in Britain refuted these findings, with very few parents in this study mentioning these types of controversies as influencing their trust in the government and vaccination, and several parents even actively denying any link when asked directly (Poltorak 2005). The authors of this study themselves reported surprise at this finding, given the findings from other studies in the country. They interpreted this refutation as potentially related to the fact that trust (or a lack thereof) in government may be less relevant than the issue of parents’ personal confidence in their own decision‐making processes. That is, the value of personal choice and responsibility for some parents in Britain almost implicitly assumes, and takes into account, governmental fallibility. As the study authors note, “[p]eople’s contemporary anxieties about state‐led technocracies reflect the emergence of individuated perspectives and political philosophies surrounding health, lifestyle and choice that are rooted far more deeply than are a few instances of government reputational damage” (Poltorak 2005).
Other pertinent examples of the role health scandals may play in fuelling mistrust in authorities and, in turn, vaccination, are the controversial Trovan clinical drug trial and state boycott of the polio vaccine that both took place in Northern Nigeria. As outlined in a study conducted in Northern Nigeria which explored parents’ perceptions of the Polio Eradication Initiative, the Trovan controversy involved a Pfizer‐organised clinical trial of the antibiotic Trovan in Kano State in the north during the 1996 cerebrospinal meningitis epidemic in the country (Renne 2010). Several children died during the trial, and a lawsuit was filed against Pfizer for failing to fully inform participants of the risks, for ‘low‐dosing the control drug’, and for withholding the fact that approved treatment for meningitis was available. The study found that this incident, and what the author describes as the government’s failure to properly oversee it, was mentioned by numerous parents. Many of these parents attributed their suspicions of polio immunisation to this incident, which for them, served as evidence that both Western pharmaceutical companies and local government cannot be trusted. Many parents in this study also spoke about the 2003/2004 polio vaccine boycott, whereby various political and religious leaders questioned the safety of the oral polio vaccine, which led to the boycott of polio immunisation campaigns in five states in Northern Nigeria. According to the author of this study, although the ban was eventually lifted, its impact lingered within communities, who continued to question the safety of polio immunisation and the agendas of vaccination programmes more generally (Renne 2010).
The Trovan trial and polio vaccine boycott, and the impact they had on parents’ vaccination acceptance, need to be understood within the broader milieu in which they occurred. The Renne 2010 study showed in detail how Nigeria has a long and painful history of (medical) colonialism, North‐South religious and political tensions, as well as more recent postcolonial inequalities and top‐down global public health initiatives. As suggested by the study author, parents’ perceptions of these controversies and associated suspicions of vaccination are therefore embedded in these much wider relationships between global institutions, Nigerian federal and state institutions, and their citizens (Renne 2010).
A final example of how particular health‐related controversies can produce and exacerbate mistrust in authorities, and the associated impact on vaccination views and practices, is the "Family Planning Program" of the 1970s in India. A study in India revealed how distrust of the government and resistance to polio vaccination amongst some Muslims was linked, at least in part, to historical fears pertaining to the controversial "Family Planning Program" of the 1970s which promoted sterilisation as a means of population control (Hussain 2015). Various Muslim parents in this study believed that Muslims were specifically targeted for sterilisation during the program, and that polio vaccination was a continuation of this agenda. This is clearly illustrated by one Muslim parent’s characterisation of the Family Planning Program and polio immunisation: “Before they had done forced sterilisation, now the government is not doing this, but doing this through the polio program so that there can be no future generations…. That same program is repeating. It is happening in another guise. In another life” (Hussain 2015, India, participant quote). Like the abovementioned study in Nigeria, this study also revealed how perceptions of this controversy, and the impact it had on parents’ vaccination acceptance, were embroiled in the intricacies of a much wider political economy of ethnic, religious, and class relations and identities in India, both historical and contemporary (see 'Finding 13: marginalisation, inadequate public services, and priority misalignment’ below for further details in this regard).
Finding 13: marginalisation, inadequate public services, and priority misalignment. Some parents' distrust in the institutions or systems implicated with vaccination was linked to their experiences of marginalisation, inadequate public services, or misalignment between their own priorities and those of the state. These experiences undermined trustful and benevolent state‐citizen relations, leading many parents to distrust government and government‐sponsored programs, including vaccination (moderate confidence).
Various studies revealed how some parents’ mistrust in the institutions implicated in vaccination, and their associated reduced acceptance of vaccination, are related to their experiences of marginalisation (Chaturvedi 2009; Renne 2010; Hussain 2015; Smith 2017), or experiences of deficiencies in basic infrastructure and functioning public services (Chaturvedi 2009; Renne 2010; Hussain 2015), or the neglect or sidelining of issues and concerns that they themselves prioritise (Chaturvedi 2009; Renne 2010; Hussain 2015). Through all these experiences, people may lose confidence that those in power have their best interests at heart, increasingly questioning the real intentions of their actions and what they promote. Vaccination, often a major state‐run and freely‐available public health intervention, provides a fertile ground for such resentment to play out. These issues were demonstrated in studies amongst Gypsies, Roma, and Travellers in Britain (Smith 2017), Muslim communities in India (Chaturvedi 2009; Hussain 2015), and in Nigeria (Renne 2010).
For example, two studies in India explored the reasons for resistance to the polio eradication initiatives in the Uttar Pradesh state in the late 2000s (Chaturvedi 2009; Hussain 2015). Both studies found that, while resistance occurred within all sectors of society, it was disproportionately higher amongst the poorest Muslim communities. One study suggested that this was linked to the historically‐rooted social marginalisation many Muslims have experienced in India (Hussain 2015). According to these authors, the legacy of colonialism, the Partition, and the rise of Hindu nationalism in the 1990s have rendered Muslims a sociological minority within Indian society and the victims of ethnic violence and socio‐political exclusion. Moreover, segregated, Muslim‐majority slums have suffered significant underdevelopment, characterised by weak basic public services, including healthcare services. The study authors found that this contributed to a sense of ‘otherness’ amongst many Muslims in India, widespread anger, and a deep‐seated mistrust of government and government‐sponsored programs, including vaccination (Hussain 2015).
Numerous Muslim parents in both studies expressed dissatisfaction with the lack of basic services afforded to them (Chaturvedi 2009; Hussain 2015). Many questioned the benefits of the polio vaccination programme when, in their view, very little else had been provided for their advantage. Some conveyed resentment at what they perceived as the government’s failure to provide basic infrastructure, while compelling them to vaccinate. Many also expressed anger at what they perceived as a misalignment of their own priorities and those of the government. That is, some saw polio vaccination as the “government’s need… not mine” (Chaturvedi 2009, India, participant quote), ultimately taking priority over what they perceived as their more pressing needs, such as food, basic sanitation, employment, and other diseases, such as diarrhoeal illnesses and malaria. As one parent in Jeevangarh shouted, clearly expressing her frustration, “We have malaria here...I tell them not to come to my door... we are in so much misery... the children have diarrhea and you are forcing them to take this other medicine… If the child is sick make the child feel better first!” (Hussain 2015, India, participant quote).
Similar findings were revealed in a study from Northern Nigeria (Renne 2010). This study showed how, during the 1990s, many Northern Nigerian states experienced a deterioration of public infrastructure due to a complex set of factors: political instability and neoliberal reforms emphasising a rolling‐back of the state and cost‐recovery for basic services. The author of the study argues that this has, in turn, undermined the benevolence of state‐citizen relations and fostered much public distrust of government. Many parents in this study mentioned distrust of the government as a major reason for rejecting the Polio Eradication Initiative. More specifically, they expressed suspicions of the motives of government, promoting a vaccine ostensibly offered for their benefit, when other services were notably neglected and underserviced. Several parents were also distrustful of the polio vaccine, which was given for free and vigorously promoted, when other vaccines and healthcare services often incurred costs and more effort to obtain: “We are looking for medicine in the hospital to give to our children and we can’t get it but this one [polio vaccine], they are following us to our houses to give it. I don’t trust this polio vaccine” (Renne 2010, Nigeria, participant quote). Many parents were also angered by the focus on polio, when, for them, other diseases, such as malaria, measles, and meningitis, were seen to pose much bigger threats to the lives of their children. As indicated by the study author, since the polio immunisation programme was not driven by their principal priorities and concerns, many parents experienced it as a top‐down initiative that therefore couldn’t be trusted (Renne 2010).
The studies in both India (Chaturvedi 2009; Hussain 2015), and Nigeria (Renne 2010), revealed that nonacceptance of vaccination could be used as a mechanism for some parents to have their principal concerns and priorities addressed. For example, various parents in India agreed to vaccinate their children only if roads were built and other medical services provided (Chaturvedi 2009). Similarly, the study in Nigeria reported that several parents had told healthcare workers that their acceptance of the polio vaccination for their children would be dependent on the government simultaneously providing them with other basic primary healthcare services (Renne 2010). According to the study author, these demands were met with the implementation of Immunisation Plus Days in 2006 and 2007, a broader‐based public health initiative that provided polio vaccines together with other services such as vitamin A drops, deworming medicines, and drugs and bednets to protect against malaria. Many parents in the study expressed considerable support for this initiative, and an associated change in their views about polio vaccination, as clearly illuminated by this parent’s comment: “Really, it is a good thing they are doing… I will agree for the polio people to do polio for my child because I need the bednet” (Renne 2010, Nigeria, participant quote). In fact, the study found that, in a reversal of earlier rejection of vaccination, some parents actually took their children to receive multiple doses of the polio vaccine at different sites so they could get additional bednets. Demand was so great that vaccine supplies eventually ran out.
Theme 4: access‐supply‐demand interactions
Parents' ideas and practices regarding childhood vaccination may be influenced by their access to and experiences of vaccination delivery institutions and their frontline healthcare workers. That is, there is a complex interplay between access‐supply and demand dimensions of vaccination or what the authors of one study termed “unfolding supply‐demand dynamics” (Millimouno 2006). Across the studies, we identified four particular subthemes with regards to these dynamics: 1) socioeconomic challenges in accessing vaccination services; 2) undesirable features of vaccination services and delivery logistics; 3) vaccination as a social event; and 4) interactions with frontline healthcare workers.
Finding 14: socioeconomic challenges in accessing vaccination services. Parents living in resource‐limited settings frequently face numerous socioeconomic challenges to accessing vaccination services, including practical questions of geography and transport, childcare constraints, and family economics and household work pressures. As a result of these challenges, some of these parents were less accepting of vaccination due to the time, effort, and opportunity costs that accessing vaccination involved (high confidence).
Studies within resource‐limited settings revealed how livelihood struggles can pose significant barriers to accessing vaccination services. Whilst parents in these contexts may hold a general belief in the value of vaccination for their children, socioeconomic challenges may reduce their acceptance of vaccination (Millimouno 2006; Leach 2007; Dugas 2009; McKnight 2014; Giles‐Vernick 2016; Smith 2017). These challenges may include practical questions of geography and transport, childcare constraints, and family economics and household work pressures. For example, parents in studies from multiple African countries (Gambia, Guinea, Ethiopia, Central African Republic, and Burkina Faso) spoke about the long distances they have to travel (up to 40 km in some localities), often by foot, to reach the nearest site where vaccination is provided (Millimouno 2006; Leach 2007; Dugas 2009; Giles‐Vernick 2016). Similar findings emerged in a study amongst site‐dwelling Gypsy, Roma, and Traveller parents in Britain (Smith 2017). These parents frequently reside in geographically‐ and socially‐isolated locations, often poorly served by public transport and other services, which hindered their ability to access immunisation services. Many parents also highlighted the difficulties they experience finding someone to care for their other children or family members who cannot be left at home alone while they make the trip to the clinic (Millimouno 2006; Leach 2007; McKnight 2014). Parents emphasised how taking their child for vaccination requires arranging for someone to look after these other family members or enduring the additional burden of bringing them along.
At the same time, many parents in these settings in Africa and Britain spoke at length about the constant, daily juggling of economic activities and domestic tasks that they have to undertake so as to keep their households afloat (Millimouno 2006; Leach 2007; McKnight 2014; Giles‐Vernick 2016; Smith 2017). As described by the authors of all these studies, vaccination constitutes one of the many basic priorities for these parents, and therefore needs to be fitted into an often already demanding daily schedule. They suggest that the day‐to‐day demands of living ultimately make taking time out for vaccinating a challenge for many of these parents, frequently resulting in a trade‐off with another activity that is of central importance for their survival. This balancing act was clearly captured by one parent from Bangui, Central African Republic, who explained, “My children haven’t gotten all of their vaccinations… I have to work every day at the market… If I don’t go to the market, my family won’t have any money. I know that I had to bring my children to receive their vaccinations. But I couldn’t do it” (Giles‐Vernick 2016, Central African Republic, participant quote). Numerous parents provided analogous accounts to this one, similarly attributing their avoidance or delay in vaccinating their children to the time, effort, and opportunity costs that vaccination involved for them.
Finding 15: undesirable features of vaccination services and delivery logistics. Some parents were less accepting of vaccination due to undesirable features of vaccination services and delivery logistics. These features, common to vaccination services within resource‐limited settings, included resource constraints that affect vaccine supply and costs, and health facility waiting times, and constraining organisational procedures (moderate confidence).
Studies in resource‐limited settings also revealed that some parents were less accepting of childhood vaccination due to the undesirable features of vaccination services and delivery logistics, even if they held a general belief in the value of vaccination for their children (Millimouno 2006; Leach 2007; Dugas 2009; McKnight 2014; Giles‐Vernick 2016). Common undesirable features revealed by these studies included resource constraints that affect vaccine supply (Millimouno 2006; Leach 2007; McKnight 2014; Giles‐Vernick 2016), and organisational procedures that impact vaccination delivery (Leach 2007; Dugas 2009; McKnight 2014).
Healthcare facilities within resource‐limited settings are often plagued by financial constraints, resulting in poor health infrastructure, such as a lack of cold chain equipment, overcrowded facilities and long waiting times, vaccine shortages and stock‐outs, and informal charging for vaccination. All of these systemic issues may impact on parents’ views and practices regarding routine childhood vaccination (Millimouno 2006; Leach 2007; McKnight 2014; Giles‐Vernick 2016). For example, it can be particularly frustrating for parents who have overcome the access challenges they face in getting to the clinic, only to find that there are no vaccines available. Many parents suggested that this could lead to their future nonattendance (Millimouno 2006; Leach 2007; McKnight 2014). Moreover, according to various study authors, the financial constraints faced by many health facilities within low‐resource settings has resulted in some of these facilities charging, albeit informally, for vaccination services that are officially free to parents (Millimouno 2006; Leach 2007; Dugas 2009; Giles‐Vernick 2016). The authors explained that, while this practice may be formally denounced, various facilities have found that this the only way to ensure a regular supply of vaccines (Leach 2007), and stable incomes for healthcare workers within contexts of irregular payment of meagre salaries (Dugas 2009). These studies revealed that, for many parents, especially those from the poorest families, these costs may be unaffordable and impede vaccination, as communicated by this parent from Kissidougou, Guinea: “I did not have the means to follow vaccination for my child ‐ for each vaccine one needs to hand over a sum of money. It is for lack of money that my child does not follow vaccination… It is not refusal” (Leach 2007, Guinea, participant quote).
In addition to resource constraints that affect vaccination delivery, the organisational procedures parents must follow in order to obtain vaccination may be perceived as undesirable, and constitute an additional deterrent to vaccination for some parents. In particular, studies in Guinea (Leach 2007), Burkina Faso (Dugas 2009), and Ethiopia (McKnight 2014), found that many parents experienced the requirement that they have their vaccination booklet available at each vaccination session constraining and a potential hindrance to vaccination. As these studies showed, the vaccination booklet is meant to be a reference document that parents and healthcare workers can consult to keep track of a child’s vaccination status. However, many parents found it very difficult to keep the booklet safe and in a usable state. Yet, according to various parents in these studies, if they attend vaccination services without their child’s vaccination booklet or with a booklet in a poor condition, they may be refused vaccination (Leach 2007; Dugas 2009; McKnight 2014). Many parents also spoke about the sense of shame they experience if they lose their vaccination booklet or if they have to present it in a poor condition. Ultimately, parents may forego vaccination to prevent such refusal or shame (Dugas 2009).
Finding 16: vaccination as a social event. Vaccination may be a social event where people gather and interact with each other. Some parents found this to be a positive experience, whereby they received affirmation about themselves and their children. This potentially motivated attendance at childhood vaccination services. For other parents, the social nature of vaccination services was a negative experience, whereby they felt judged by, disapproved of by, or alienated from others. This potentially demotivated attendance atchildhood vaccination services (low confidence).
Studies conducted in Gambia and Guinea revealed how vaccination services are social settings: places where people gather and interact with each other (Millimouno 2006; Leach 2007). According to the authors of these studies, this ‘socialness’ of vaccination services can be a source of enjoyment and a valued social event for some. However, for others, it can be a place of worry and alienation. Both studies found that, in urban and peri‐urban settings in their respective countries, vaccination attendance at the clinic on the designated day is commonly a social occasion, an event where mothers and their children are ‘on show’ to others and where their status is often publicly displayed. As these studies revealed, this can be a very positive experience for some, with vaccination attendance serving as an occasion to show pride in one’s wealth and baby. For example, a young mother in peri‐urban Gambia recounted how, “I would find something suitable for my baby, I would also dress beautifully, put on matching shoes, take my bag and go to the clinic. As an adolescent, I loved to draw attention, and I did it (Leach 2007, Gambia, participant quote). Both studies revealed how experiences of vaccination services as a positive social event can be a powerful motivator for attendance of vaccination services.
However, as noted by the authors of both studies (Millimouno 2006; Leach 2007), the socialness of vaccination services also places mothers and their children open to scrutiny, which for some can be a source of fear and marginalisation. Both studies found that poorer and less integrated mothers (such as immigrants or sex workers), and mothers with a thin or unwell baby, often fear the unwanted attention on themselves or their baby that vaccination attendance may potentially bring. Some of these mothers therefore avoided or delayed vaccination for their child in order to eschew judgement and disapproval from others. Both these studies also found that infant health facilities have become highly feminised spaces, attended by pregnant and postnatal women who are often accompanied by their mothers, female neighbours, and other female kin. According to the authors of both studies, this has resulted in many fathers feeling uncomfortable in these spaces, sometimes even delaying vaccination until the child’s mother or a female relative was available to take the child to the clinic.
Finding 17: interactions with frontline healthcare workers. Parents' vaccination views and practices, across diverse settings, contexts, and population groups, were mediated by the face‐to‐face interactions or personal relations they have with frontline healthcare workers. Some parents were less accepting of vaccination due to mistreatment from healthcare workers, and when they felt the vaccination information provided to them was simplistic and unbalanced. In contrast, some parents were more accepting of vaccination due to positively‐received engagements with healthcare workers, whereby they felt supported, listened to, and respected and whereby healthcare workers shared balanced information and personal stories about themselves as parents (high confidence).
Many parents experience vaccines and vaccination services through the face‐to‐face encounters they have with frontline healthcare workers. As demonstrated by various studies, these engagements can therefore play an important role in shaping how many parents assess expert claims about immunisation and think about vaccination (Brownlie 2005; Poltorak 2005; Millimouno 2006; Casiday 2007; Leach 2007; Dugas 2009; McKnight 2014; Hussain 2015; Dube 2016; Giles‐Vernick 2016; Reich 2016; Sobo 2016; Smith 2017; Ward 2017; Peretti‐Watel 2019; Limaye 2020).
For some parents, the engagements they have with frontline healthcare workers are coloured by the broader, more macro‐level distrust they may have in the expert systems implicated in vaccination (see ‘Theme 3: political events, relations, and processes’) (Brownlie 2005; Chaturvedi 2009; Giles‐Vernick 2016; Smith 2017; Peretti‐Watel 2019). As explained by the authors of one study, frontline workers may be seen as representatives of, or “access points” to, these more remote expert systems, and thus parents may distrust healthcare workers and what they promote by implication (Ward 2017). However, what emerged across many studies was the influence of the quality of the actual face‐to‐face interactions or personal relations parents have with frontline healthcare workers (Brownlie 2005; Poltorak 2005; Millimouno 2006; Casiday 2007; Leach 2007; McKnight 2014; Hussain 2015; Dube 2016; Reich 2016; Sobo 2016; Smith 2017; Ward 2017; Peretti‐Watel 2019; Limaye 2020).
Various studies, across diverse contexts and populations, demonstrated how some parents were less accepting of childhood vaccination due to their experiences of mistreatment or poor communication from frontline healthcare workers (Poltorak 2005; Millimouno 2006; Casiday 2007; Leach 2007; Dugas 2009; McKnight 2014; Hussain 2015; Dube 2016; Reich 2016; Sobo 2016; Smith 2017; Ward 2017). For example, several parents from various African countries (Ethiopia, Guinea, Gambia, and Burkina Faso) reported that parents who miss vaccinations, come late, or have lost, forgotten, or failed to keep their vaccination booklet in a good condition are often blamed and condemned by healthcare workers and subjected to embarrassing, humiliating, or neglectful treatment (Millimouno 2006; Leach 2007; Dugas 2009; McKnight 2014). For instance, parents described how healthcare workers commonly labelled parents as ‘defaulters’, shouted at or insulted them in front of other parents, sent them to the back of the queue, or ignored them. Lots of parents feared this mistreatment, or what the authors of one study conceptualised as “symbolic violence” (McKnight 2014), and as a consequence, decided to forgo subsequent vaccination sessions if they had missed previously scheduled vaccinations, could not locate their vaccination booklet, or their booklet was in a poor condition (Millimouno 2006; Leach 2007; McKnight 2014). As one parent painfully exclaimed, “The reason why we don’t take our children is the workers at the health centre don’t admit us if we have missed the date of the appointment. They insult us for being late. So we fear to go there for vaccination because they offended us” (McKnight 2014, Ethiopia, participant quote). Various study authors suggested that healthcare workers treat parents in this way because they erroneously attribute non‐ or delayed‐vaccination to ignorance or child neglect, failing to appreciate the socioeconomic struggles many parents face in negotiating clinic attendance (Millimouno 2006; Leach 2007; McKnight 2014).
Mistreatment from healthcare workers, and how this can negatively impact on parents' vaccination acceptance, was similarly revealed in studies from HICs, including in the United Kingdom (Poltorak 2005; Casiday 2007; Smith 2017), and Australia (Ward 2017). Parents in these studies described incidences with healthcare workers where they had raised their concerns, asked questions, or expressed their opinions about vaccination, and had in turn been “patronised or intimidated” (Poltorak 2005, UK participant quote), or responded to in ways they experienced as “disrespectful” (Ward 2017, Australia, participant quote), “rude and dismissive”, “condescending”, and “disempowering” (Ward 2017, Australia, participant quotes). Other parents in these studies spoke about being “pressured” or “emotionally manipulated” into vaccinating their children by healthcare workers (Casiday 2007, UK, participant quotes). Many of these parents explicitly stated how this type of treatment led them to distrust their healthcare worker and the vaccination advice or information they provided, as clearly conveyed by this parent: “My GP… she was so rude and dismissive… each interaction like that erodes my trust further” (Ward 2017, Australia, participant quote).
Many parents’ descriptions of the negative interactions they have had with healthcare workers centred specifically on the way in which information about vaccination is communicated. Parents from a range of countries (USA, Canada, the United Kingdom, Australia, and India) expressed frustration at what they perceived as the simplistic and unbalanced vaccination information provided to them by healthcare workers (Casiday 2007; Hussain 2015; Dube 2016; Reich 2016; Sobo 2016; Smith 2017; Ward 2017). Many parents indicated that healthcare providers only talk about the benefits of vaccination, remaining silent or defensive about the potential risks or side effects of vaccination: “They don’t tell you the side effects of having these vaccines they don’t tell you this side of it” (Smith 2017, UK, participant quote). Many of these parents explained that this made them distrustful of their healthcare worker and sceptical of the vaccination advice or information they provide (Casiday 2007; Hussain 2015; Reich 2016; Sobo 2016; Ward 2017).
Various studies, across diverse settings and populations, also demonstrated how affirming interactions and forms of communication with frontline healthcare workers can enhance parents’ acceptance of vaccination for their children (Brownlie 2005; Poltorak 2005; Casiday 2007; Leach 2007; Ward 2017; Peretti‐Watel 2019; Limaye 2020). Numerous parents described the positive influence of healthcare workers who were supportive and empathetic, who listened to their concerns and genuinely engaged with their questions, who respected views that they did not necessarily share, and who provided balanced and nuanced information about vaccination. Parents highlighted how these types of engagements built their trust in their healthcare worker and the vaccination recommendations he or she provided: “I really trust [my son’s] doctor. I really like her… Like, she listens to me” (Limaye 2020, USA, participant quote).
Many parents spoke specifically about the value of healthcare workers' sharing personal stories or information about themselves as parents (Brownlie 2005; Poltorak 2005; Casiday 2007; Leach 2007; Peretti‐Watel 2019). These more personally‐focused interactions may enhance relations of familiarity and, in turn, parents’ faith in healthcare workers and what they say (Brownlie 2005). As this parent implied, “I think I would have confidence in my own GP if he were to say ‘well I have had all my children vaccinated’. If the health professional were to say ‘I would have no hesitation to have my own children vaccinated’ well then, I would trust their decision” (Brownlie 2005, UK, participant quote). More personally‐focused interactions may also allow parents to more easily voice and discuss their particular concerns about their children and vaccination (Poltorak 2005).
2. Third‐order concepts
In the following two concepts, we present the views and interpretations of the review authors regarding potential pathways to reduced acceptance of childhood vaccination.
Finding 18: neoliberal logic. Many parents, predominantly from HICs, held a worldview informed by neoliberal discourses. These discourses understand health as individualised, and health‐related risks and decisions as matters of individual choice and responsibility. Furthermore, these discourses suggest that being a ‘good’ and responsible person in the world means consistently assessing one’s own individual health‐related risks, seeking and questioning evidence about such risks, proactively avoiding and managing such risks, and understanding that one is singularly accountable for the outcomes that ensue. Some parents experienced this worldview as in conflict with vaccination promotion messages, which tend to be informed by other types of discourses. The discourses underpinning vaccination promotion messages frequently emphasise generalised risk and safety statistics, claim that ‘doctor knows best’, ask people to trust authorities and follow what they promote, and advocate for social responsibility and the health of the community. Parents’ perceived tension between the discourses informing their own worldview and those of vaccination promotion messages led some to resist these messages and be less accepting of vaccination (moderate confidence).
One potential pathway to reduced acceptance of childhood vaccination can be captured by the concept of ‘neoliberal logic’. This concept encapsulates the interconnected and frequently coexisting ideas held by many parents, which come together to create a particular logic of care regarding vaccination. This logic of care was common amongst parents across socioeconomic divides in HICs. It also emerged amongst parents from middle‐ and higher‐ socioeconomic groups in Brazil (Barbieri 2017). This logic can be characterised as follows. With a view of their child’s health as individualised and inevitably fragile, parents attempt to separate out the risks of disease and the potential benefits of vaccines as they pertain to their specific child. With a view of themselves as experts of their children and a skepticism of the expert systems implicated with vaccination, parents perceive themselves as best placed to conduct this risk‐benefit calculus for their child. With a strong conviction that they are singularly responsible for their child’s health, they see this risk assessment as a moral obligation and the vaccination decision taken as ultimately a matter of personal choice.
This particular logic of care is not an ‘individual’ belief held by a select few. Rather, it is deeply rooted in, and reflects, trends in thinking that have become ubiquitous within contemporary, industrialised societies. Within these contexts, the ideas of individual responsibility and personal choice have become dominant values in recent decades. This is related to the processes of individualisation and a rollback of the state to a political agenda stressing citizens’ own rights and responsibilities. Drawing on the works of sociologists Ulrich Beck and Anthony Giddens (Giddens 1990; Giddens 1991; Beck 1992), many study authors highlight how we are currently living within a ‘risk society’ era (Rogers 1995; Petts 2004; Poltorak 2005; Casiday 2007; Brunson 2013; Sobo 2016). In this era, risks have intensified in magnitude and become increasingly global: international disease outbreaks, nuclear war, environmental pollution, global warming, accidents, terrorism, and so forth. The nature and scope of contemporary risks make them more difficult than in the past to calculate and control, creating a climate of increased vulnerability. At the same time, central institutions and systems (government, industry, science) are increasingly viewed as partly responsible for, and unable to control, the types of risks thrown up by the processes of modernisation. Distrust and suspicion of these institutions have therefore become pervasive features of contemporary social life.
Within this context, there has been an intensification of concern with assessing, avoiding, and managing risk, processes which have become increasingly individualised and understood as matters of personal responsibility and choice. Drawing on the thinking of French philosopher Michel Foucault (Foucault 1977; Foucault 1989; Foucault 1991), various study authors highlighted how people are increasingly required to become ‘responsibilised’ citizens who self‐govern their lives, remain actively aware of dangers and opportunities, and who recognise that they themselves are accountable for their own well‐being (Petts 2004; Ward 2017). Ultimately, making decisions in terms of individual choice and responsibility has become a moral imperative and has infiltrated many domains of life.
Health and healthcare are no exception in this regard, where individual responsibility for one’s own health (or that of one’s children) has become a major societal value. Using the theory of “healthism”, originally coined by Robert Crawford (Crawford 1980; Crawford 2004), various study authors demonstrate how people are encouraged to empower themselves to become “active” (Sobo 2016), and “enterprising and entrepreneurial” (Peretti‐Watel 2019), healthcare consumers who undertake “self‐initiated health promoting behavior” (Rogers 1995). Within this neoliberal logic, health has also become a moral imperative and an essential aspect of self‐worth, whereby a ‘failure’ to look after one’s health or to make ‘good’ healthcare choices is seen as a moral transgression (Reich 2016; Ward 2017). The ‘holistic’ or ‘natural’ health movement is a product, at least in part, of this heightened preoccupation with personal health and the individual lifestyle modifications thought to promote or maintain it (Crawford 1980; Crawford 2004).
This ideology of ‘healthism’ dovetails with, and is reinforced, by a contemporary public health paradigm that strongly promotes the values of ‘patient choice’, ‘patient empowerment’, ‘self‐management’, and ‘shared decision‐making’ in health and healthcare practices. As suggested by several study authors, health promotion policy and practice consistently urge people to be independent and self‐efficacious, to educate themselves on health‐related issues and to fully participate in making decisions to optimise their own (and their families’) health and well‐being (Rogers 1995; Poltorak 2005; Brunson 2013; Reich 2016; Sobo 2016; Ward 2017).
Views regarding childhood vaccination for many parents in HICs therefore need to be understood within this context and the forms of neoliberal subjectivity it has produced. These kinds of vaccination views, informed by neoliberal discourses, were common amongst parents across the spectrum of vaccination attitudes in HICs: those who accepted vaccination, those who were hesitant towards vaccination, and those who refused vaccination. However, for certain parents, these views were experienced as in conflict with vaccination promotion messages. Some of these parents were particularly uneasy with the population‐level risk‐benefit statistics that vaccination promotion discourses provide, which they felt disregarded their child’s individual vaccination needs and vulnerabilities. Other parents resented the emphasis such discourses placed on community obligation and the health of the ‘herd’, when being a good parent is associated with taking personal responsibility for what’s best for one’s own child. Other parents resented the claim of ‘doctor knows best’ underpinning vaccination promotion messages, when they considered themselves to have the best knowledge of their child’s strengths and vulnerabilities. Many of these parents had an inherent distrust for health authorities, and therefore objected to vaccination promotion messages asking them to be ‘a blind follower of the state’ and to ‘uncritically trust’ what health authorities promote. Some parents also pointed to and resented the inconsistencies between these messages and other health promotion discourses which advocate for independent, reflexive decision‐making and personal choice.
Therefore, the source of conflict certain parents perceived between vaccination promotion messages and their views about health and healthcare informed by neoliberal discourses varied. However, what appeared common for these parents, and what potentially separated them from other parents who accepted vaccination, was that this experienced tension was absolute and unacceptable. This, in turn, may have led them to resist vaccination promotion messages and be less accepting of vaccination.
Finding 19: social exclusion. Some parents, predominantly from LMICs, were less accepting of childhood vaccination due to their experiences of social exclusion. Social exclusion may involve economic disadvantage, residential segregation, a lack of political representation or power, discrimination and unequal protection of rights, and a myriad of socioeconomic barriers to good quality public services, including vaccination. Social exclusion weakened trustful government‐citizen relations, generated feelings of alienation from, and resentment towards, the state and others, and gave rise to frustration and demotivation in the face of structural challenges. These factors, in turn, led some parents who are socially excluded to distrust vaccination, to refuse vaccination as a form of resistance or a mechanism to bring about change, or to avoid vaccination due to the time, effort, (opportunity) costs, and distress it creates (moderate confidence).
Another potential pathway to reduced acceptance of childhood vaccination may be captured by the concept of ‘social exclusion’. Here we define social exclusion as a state in which individuals, communities, or areas are unable to participate fully in the economic, social, political, and cultural life of society, as well as the process leading to and sustaining such a state (United Nations 2016). Studies included in this review revealed how social exclusion may entail various different dimensions: poverty and inequality, including deficiencies in and poor access to basic infrastructure and functioning vaccination and other public services; residential segregation; a lack of political representation or power; discrimination; and unequal respect for and protection of rights. All of these different dimensions of social exclusion may lead parents to be less accepting of vaccination through varying mechanisms of effect. Experiences of social exclusion may rupture trustful government‐citizenry relations, in turn leading excluded communities to lose confidence that those in power have their best interests at heart. They may become increasingly sceptical of initiatives ostensibly offered for their advantage, when they are disadvantaged in so many other aspects of their lives. In such cases, parents may be less accepting of vaccination for their children because they do not trust the safety of vaccines, the motivations of those delivering them, or the real benefits of vaccination programmes.
Experiences of social exclusion may also generate a climate of alienation from, and anger towards, the state and others in society. Socially‐excluded communities may, in turn, resent having to take part in ‘public good’ initiatives when they feel estranged from the public in whose interests they must cooperate, and disenfranchised by the authorities asking for their participation. They may begrudge being asked to vaccinate when what they consider to be their principal concerns are neglected. In such cases, childhood vaccination may be rejected by parents as a form of resistance to authorities, or what one study author – following political scientist James Scott (Scott 1985) – calls a “weapon of the weak” (Renne 2010). That is, it may provide socially‐excluded parents with a degree of agency within contexts where they are fundamentally disempowered. For some, and as suggested by various study authors, nonacceptance of vaccination may actually be used more overtly as a mechanism to bring about change, a “bargaining point” (Chaturvedi 2009), or “negotiating tool” (Hussain 2015), to have their principal concerns and priorities addressed. While this might be considered “dangerous development”, as suggested by the authors of one study (Hussain 2015), it is arguably also a strategic and potentially desperate response to oppressive contexts where lives and livelihoods are fundamentally threatened.
Experiences of social exclusion, particularly when social exclusion includes poverty and inequality, may also produce substantial frustration and demotivation around vaccination. The studies included in this review revealed how economically‐disadvantaged communities frequently face major structural barriers to accessing vaccination services, whether due to long distances needed to travel to access vaccination, childcare constraints, competing livelihood activities and domestic tasks (Millimouno 2006; Leach 2007; Dugas 2009; McKnight 2014; Giles‐Vernick 2016; Smith 2017). Many studies also found that, if these economic struggles and situational constraints are overcome, parents are then frequently met with suboptimal vaccination services, including vaccine shortages and stock‐outs, overcrowded facilities, long waiting times, informal charges, and mistreatment from healthcare workers (Millimouno 2006; Leach 2007; Dugas 2009; McKnight 2014; Giles‐Vernick 2016). In such cases, and as suggested by various study authors (Millimouno 2006; Leach 2007; McKnight 2014), parents’ acceptance of vaccination may be reduced, albeit more passively, due to the extensive time, effort, (opportunity) costs, and distress that vaccination entails for them.
3. Overarching line of argument
In the following line of argument, we present the views and interpretations of the review authors regarding how one might conceptualise, more broadly, parental views and practices regarding childhood vaccination.
The overarching line of argument emerging from the analysis of the data is as follows: parents’ views and practices regarding childhood vaccination can be conceptualised as complex and dynamic social processes that reflect multiple webs of influence, meaning, and logic. That is, parents’ vaccination decisions usually comprise an ongoing engagement that is contingent on unfolding personal and social circumstances. Such decisions usually emerge through interacting and relating, rather than through a deliberative calculus at a single moment in time. As such, vaccination views ‐ whatever position is taken ‐ may be best understood as a ‘process’, rather than an a priori or fixed ‘stance’. The procedural nature of vaccination views also means that parents' vaccination views and practices change or can potentially change.
Moreover, parents’ vaccination views and practices are influenced by multiple forces and carry a variety of meanings: social, political, structural, moral, as well as biological. Through their vaccination choices, parents are often reflecting their experiences of, and the meanings they attach to, broader relations, entities, and processes ‐ big and small, past and present, directly and indirectly related to vaccination. These include, for example, parents’ engagements with other parents, peers and community members, with healthcare institutions and their providers, with the state, with science and medicine, with global institutions and programmes, with former colonial powers. Sometimes, parents’ vaccination views and practices are more explicitly commenting on and even challenging the nature of these relations, entities, and processes. Therefore, through their vaccination decisions, parents are often communicating not just what they think about vaccines, but also who they are, what they value, and with whom they identify.
As such, reduced vaccination acceptance is often not about ‘ignorance’ or ‘misinformation’. Rather, it forms an integral part of the wider social milieu in which parents live. Nor is reduced vaccination acceptance necessarily about irrational forms of thinking. The wider social milieu in which parents live frequently contains features that make vaccination hesitancy or nonacceptance not only possible, but seem entirely logical ‐ whether in the neoliberal world of more affluent parents or the disadvantaged world of more socially‐excluded parents. While the logic may not conform to the logic of vaccination programmes, it makes sense within the political, moral, structural, and conceptual landscapes of those worlds. Ultimately, recognising these logics on their own terms could provide avenues for more effectively and sensitively bridging the goals of immunisation programmes with those of parents who decide against vaccination for their children.
Results of integrating the review findings with the Cochrane intervention reviews
The results of our comparison of the findings from our qualitative evidence synthesis and the findings from the related Cochrane Reviews of intervention effectiveness are presented in the matrix in Figure 8. The matrix provides a summary of how the overarching factors our review identified as influencing parents’ vaccination views and practices are (or not) reflected in the underlying theories or components of the interventions in the studies included in the related Cochrane Reviews of intervention effectiveness (Saeterdal 2014; Oyo‐Ita 2016; Jacobson‐Vann 2018; Kaufman 2018).
8.
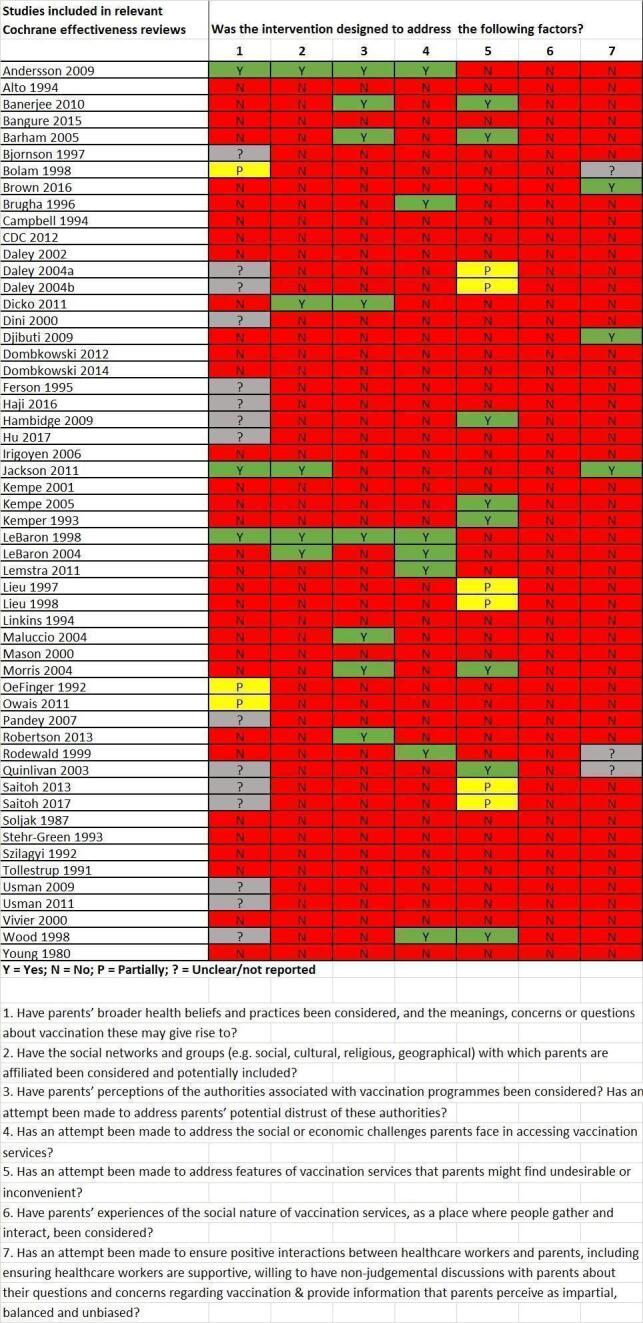
Matrix model applying key findings from the qualitative synthesis to studies included in the Cochrane Reviews of interventions
The following are links to the references of the studies included in the relevant Cochrane effectiveness reviews: Young 1980; Soljak 1987; Tollestrup 1991; Oeffinger 1992; Szilagyi 1992; Kemper 1993; Stehr‐Green 1993; Alto 1994; Campbell 1994; Linkins 1994; Ferson 1995; Brugha 1996; Bjornson 1997; Lieu 1997; Bolam 1998; LeBaron 1998; Lieu 1998; Wood 1998; Rodewald 1999; Dini 2000; Mason 2000; Vivier 2000; Kempe 2001; Daley 2002; Quinlivan 2003; Daley 2004a; Daley 2004b; LeBaron 2004; Maluccio 2004; Morris 2004; Barham 2005; Kempe 2005; Irigoyen 2006; Pandey 2007; Andersson 2009; Djibuti 2009; Hambidge 2009; Usman 2009; Banerjee 2010; Dicko 2011; Jackson 2011; Lemstra 2011; Owais 2011; Usman 2011; CDC 2012; Dombkowski 2012; Robertson 2013; Saitoh 2013; Dombkowski 2014; Bangure 2015; Brown 2016; Haji 2016; Hu 2017; Saitoh 2017.
In summary:
the factor most commonly targeted amongst the interventions was features of vaccination services that parents might find undesirable or inconvenient, with 14 (26%) of interventions reflecting or partially reflecting this influencing factor.
eight interventions (15%) addressed the issue of trust/distrust of authorities associated with vaccination programmes. Seven of these focused specifically on providing a range of basic services or goods along with vaccination, which the findings from our review suggested could help alleviate distrust in vaccination programmes and those delivering them.
Seven interventions (13%) targetted the social or economic challenges parents face in accessing vaccination services, followed by six interventions (11%) which considered or partially considered parents’ broader health beliefs and practices, and the concerns or questions about vaccination these may give rise to.
Only five interventions (9%) considered the social networks and groups with which parents are affiliated, and only three interventions (5%) considered the interactions and forms of communication between healthcare workers and parents. Our review findings on the influence of social networks (finding 7) and healthcare workers (finding 17) on parents' vaccination acceptance were both assessed as having high confidence.
None of the interventions appeared to consider parents’ experiences of the social nature of vaccination services.
Interventions with multiple components were more likely to include more elements that could be mapped onto the findings of our review than those with single components.
For various interventions, it was unclear whether the intervention failed to reflect or target an influencing factor, or alternatively, whether the researchers conducting the intervention studies did not report an influencing factor. In these cases, we may have gained greater clarity about the intervention if we had searched for additional information in related publications or from study authors, rather than relying solely on the information provided in the publications included in the related Cochrane Reviews of intervention effectiveness.
Review author reflexivity
Throughout the review process, none of us held a neutral position regarding vaccination. At the outset of the review, we all believed that childhood vaccination is an important individual and public health intervention. We all fully accepted childhood vaccination according to the recommended schedules. This was based on our shared view that vaccines are mostly safe and beneficial for individuals, and that most individuals can each absorb minimal risk to safeguard those in our communities who are most vulnerable. One member of the team had the experience of unintentionally delayed and incomplete vaccination for her children, which provided her with a more nuanced experience of parental decision‐making about childhood vaccinations. In addition, we all held the view that individuals have a right to make their own healthcare decisions, including about vaccination. Moreover, we believed that it is important for people to have easy access to balanced and transparent information about vaccination, including about adverse effects, evidence gaps, and uncertainties. We recognised that there are many potential tensions between public health, community obligation, and individual choice, tensions which we tried to hold and grapple with throughout the review process.
While the review did not change any of our views about vaccination, we have all been required to engage seriously with the complex logics underpinning parents’ vaccination views and practices that may differ from our own. Through this process, many of us have recognised parts of ourselves in these views and practices, and have in turn gained a more nuanced and less judgmental understanding of diverse perspectives.
Much of the research on the demand side of vaccination focuses on understanding what parents think, feel, and do regarding vaccines. While we as a review team shared this interest, we also wished to provide a critical and contextualised understanding of these views, emotions, and practices. This motivation informed, at least in part, our choice of a meta‐ethnographic analysis approach and associated decision to use 'conceptual richness' as our primary sampling strategy. These decisions inevitably also shaped the interpretive process and synthesis of the findings. Before undertaking the review, many of us had considerable prior knowledge of existing conceptual frameworks on the demand side of vaccination, as well as many of the social theories employed by the studies included in the review. We anticipated that these former understandings could both enhance and negatively impact upon the interpretive process and synthesis of the findings. We therefore employed various strategies to mitigate this potentially negative impact, and to mitigate other ways in which we might inappropriately skew the interpretation of the data and our own review findings. The team regularly discussed progress and preliminary findings, with the aims of identifying assumptions in the data synthesis, clarifying procedures and choices, and documenting various challenges faced in the review process. These discussions were greatly enhanced by our having a multidisciplinary review team, which enabled both the exploration of multiple perspectives and productive contestation. Our review team comprised authors with disciplinary backgrounds in sociology (SC), anthropology (BS, AS, CC), psychology (NL, SC), health systems (NL, CW), vaccinology (CW), and epidemiology (BS, ES, CC, CW). During our team discussions, we also tried to remain mindful of our presuppositions and, as a team, to support each other to question our own viewpoints. We also used refutational analysis techniques (‘disconfirming analyses’) as an integral part of the data analysis. We identified various incongruencies, inconsistencies, and refutations in the data, which we explored and accounted for in our synthesis of the findings. This process deepened our interpretations and further enhanced the reflexive stance of the review team.
A final strategy we used to try operationalise a reflexive stance was to write ourselves explicitly into the text of the review findings; for example, by commonly making statements such as “we interpreted this to mean”, or “we did not identify”, or “we have attempted to move away from”. Through this approach, we hoped to make the interactions between the studies and our own views and positions more visible, and to provide review findings that ultimately reflect a “view from somewhere” (Harraway 1988) rather than “a view from nowhere” (Nagel 1986).
Discussion
Summary of the main findings
For a summary of the main findings, see the Plain Language Summary.
Comparison with other reviews and implications for the field
The findings of our qualitative evidence synthesis have various commonalities with the findings from a related Cochrane qualitative evidence synthesis on perceptions and experiences of communication about routine childhood vaccination (Ames 2017b). Ames and colleagues also highlighted the importance of frontline healthcare workers in influencing parents' vaccination intentions. For example, like our review, Ames and colleagues found that parents want healthcare workers to answer their questions, provide impartial and balanced information (about both the benefits and risks of vaccination), and be caring, sensitive, and receptive to their concerns. The Ames 2017b review similarly revealed the positive impact of the presence of these factors on parents' vaccination views and practices, but also the negative impact when these factors are absent. Ames and colleagues also revealed the importance of trust/distrust in the context of vaccination. For example, the review found: that parental attitudes towards vaccination influenced which vaccination information sources they trusted; that parents who trusted their health workers also trusted the information they provided; and that some parents distrusted information sources linked to the government. Our review supports and extends these findings by revealing how, in addition to influencing views about information sources, parents' trust or distrust in healthcare workers, government, and other forms of authority also impacts upon their views and practices about vaccination. Ames and colleagues indicated that communication is one of many interacting factors that may influence parents' and informal caregivers' decisions to take their children for vaccination, and communication alone will therefore not address all aspects of vaccine acceptance, hesitancy, or refusal. Our review provides insights into what these other aspects may be.
The findings from our review also have commonalities with findings from other qualitative and mixed‐methods reviews focused on the demand side of childhood vaccination (Mills 2005; Brown 2010; Larson 2014; Dube 2018), although none of these reviews had the same focus or scope as our review. Two of these were qualitative reviews that synthesised beliefs, attitudes, and practices toward childhood vaccination in high‐income contexts specifically (Mills 2005; Dube 2018). Two were mixed‐methods reviews that focused on the factors influencing decision‐making regarding combination childhood vaccination in high‐income contexts specifically (Brown 2010), and the factors affecting vaccine hesitancy and its determinants globally (Larson 2014).
As with our findings, all four of these reviews found that childhood vaccination views and practices are complex social processes influenced by multiple factors ‐ sociocultural, political, economic, historical, ideological, psychological, moral as well as biological (Mills 2005; Brown 2010; Larson 2014; Dube 2018). Therefore, these reviews, like ours, challenge common understandings of vaccination hesitancy or nonacceptance as individual phenomena resulting primarily from ‘ignorance’ or irrational forms of thinking (i.e. ‘knowledge‐deficit’ approaches).
Many of the factors we identified as influencing parental vaccination views and practices were also identified in these reviews. For example, all four reviews highlighted the significant role of trust or distrust in government, biomedicine, and pharmaceutical companies, and how a lack of or decline in trust in these entities can contribute to reduced acceptance of childhood vaccination amongst parents (Mills 2005; Brown 2010; Larson 2014; Dube 2018). Our review reflects this finding, but also elaborates on it by demonstrating the complex and contextually‐situated nature of this distrust, and how the absence or decline of trust may be linked to political events, relations, and processes within specific times and places.
Moreover, parents’ relationship and interactions with healthcare workers were also identified as important factors shaping parents’ vaccination views and practices in three of these reviews (Mills 2005; Brown 2010; Dube 2018). As in our review, these reviews found that the manner in which healthcare workers treat parents – and specifically whether parents feel respected, supported, and listened to (or not) by healthcare workers – can influence what parents think and do regarding vaccination for their children. The interplay between access‐supply and demand dimensions of vaccination were also highlighted in three reviews (Mills 2005; Brown 2010; Larson 2014). As in our review, these reviews showed how practical barriers to accessing vaccination and challenges around vaccine supply can reduce parents’ acceptance of vaccination for their children. Similarly to our review, two reviews also identified social networks and norms, as well as parents’ broader ideas and practices surrounding health and illness, as additional important factors influencing parental vaccination views and practices (Larson 2014; Dube 2018).
Two reviews found that many parents hold perspectives similar to what our review conceptualised as a ‘neoliberal logic’ (Brown 2010; Dube 2018). In their mixed‐methods review, Brown 2010 found that lower vaccine uptake was associated significantly with parents who valued the right to choose whether to vaccinate, who engaged in personal research on vaccination, and who had a preference for ‘naturally‐acquired’ immunity. Relatedly, in their qualitative review, Dube 2018 found that parents who expressed hesitancy towards or who refused vaccination for their children commonly expressed strong feelings of personal responsibility to their children and highlighted the importance of personal choice. These parents often also placed considerable emphasis on ‘healthy, natural lifestyles’, and conveyed resentment over the pressures they felt to risk their own child’s safety for public health benefits. Both reviews also found that, when making decisions about vaccination for their children, many parents prioritised individual risk assessments over generalised or population‐level statistics of risks and benefits. Our own review reflects these findings, but also enhances them by trying to bring them together theoretically through our concept of a ‘neoliberal logic’. There is a persepctive in some health literature that the neoliberal values of individual responsibility and choice are more common amongst higher socioeconomic groups (e.g. Lindbladh 2003). The findings from our review does not support this perspective, but rather suggests that, at least in HICs, neoliberal values and views may be held by parents across the socioeconomic spectrum.
Many reviews focused on the demand side of childhood vaccination included studies only from HICs (see Table 2 for a summary of these reviews). Our review addresses this gap by incorporating, and comparing the findings of, studies from both HICs and LMICs. We identified both differences and commonalities in the findings between these study groups. One of the main differences relates to potential sociocultural variations in ideas and practices surrounding health and illness, and associated perceptions of the role of vaccination. For example, we suggested that a ‘neoliberal logic’ of health may be more applicable to parents in HICs as a potential pathway to reduced acceptance of childhood vaccination. However, one study conducted in Brazil included in our review (Barbieri 2017), found this type of logic to be very common amongst parents from middle and higher socioeconomic groups. More research is needed to determine the relevance of this finding amongst parents from middle and higher socioeconomic groups in other LMICs. Another main difference our review found between findings from HIC and LMIC studies was the role of access challenges and suboptimal vaccination services and delivery logistics. These issues, common in many resource‐limited settings, emerged as impacting negatively on vaccination acceptance amongst parents in many LMICs. However, access challenges were found to be an important issue impacting upon vaccination acceptance amongst Gypsy, Roma, and Traveller parents in one study in Britain included in this review (Smith 2017). More research is therefore needed to determine the relevance of this issue amongst parents from other minority or marginalised groups in HICs.
There were, however, also many commonalities that emerged in the studies from HICs and LMICs. The mutually‐reinforcing relationship between parents’ vaccination ideas and practices and the social networks in which they are embedded was found in both HIC and LMIC studies. Moreover, a pertinent finding that emerged across study groups was the impact of distrust in the institutions or systems implicated with vaccination on vaccination acceptance. Similarly, the interactions parents have with frontline healthcare workers, and how these can positively and negatively influence vaccination acceptance, was another common finding between studies in HICs and LMICs. At the same time, our four third‐order themes and overarching line of argument were able to 'hold' and account for the findings from both HIC and LMIC studies.
Ultimately, the specific configurations of influencing factors, and the particular conditions, relations, and dynamics in which they are rooted, may differ between HIC and LMIC (and potentially other) contexts. Yet we would argue that the broader categories of influencing factors developed and applied in this review, and our overarching conceptualisation of vaccination, are potentially applicable across country income divides.
The findings from our review support and also enhance various existing conceptual and theoretical models of the demand side of vaccination. Our concept of ‘neoliberal logic’ aligns with, and provides empirical support for, the theoretical framework of vaccine hesitancy proposed by Peretti‐Watel and colleagues (Peretti‐Watel 2015). This framework conceptualises vaccine hesitancy as a two‐dimensional decision‐making process that depends on people’s level of commitment to modern society’s risk culture, or “healthism”, and their trust in the authority of healthcare providers and mainstream medicine. Our review’s concept of ‘social exclusion’ provides possible insights into how this framework might be expanded to incorporate other major structural features of contemporary societies, thereby enhancing its potential generalisability.
The four third‐order themes of our review also align with, and provide empirical support for, existing socio‐ecological conceptual models of vaccination acceptance, including the WHO’s ‘Vaccine Hesitancy Determinants Matrix’ (Sturm 2005; Callreus 2010; WHO 2013b; Larson 2014). These models understand vaccination decision‐making as shaped by interrelated factors operating at multiple levels (e.g. intrapersonal, interpersonal, institutional, community). Our review identifies several factors which may be important at different levels of influence. Our review also provides insights into how these factors might function and interact to influence vaccination views and practices. In particular, through our third‐order concepts of ‘neoliberal logic’ and ‘social exclusion’, our review provides a theorised understanding of two potential mechanisms or pathways through which different factors, at different levels, might interact to reduce vaccination acceptance.
These mechanisms or pathways may also supplement the core theoretical constructs of the various ‘C frameworks’. The 'C frameworks' draw on psychological models (e.g. the Health Belief Model and Theory of Planned Behaviour, amongst many others) to understand the psychological processes underpinning vaccination decision‐making (WHO 2013b; Betsch 2015; MacDonald 2015; Betsch 2018). While the constructs of these frameworks have been recognised as highly relevant, these frameworks have also been criticised for prioritising individual processes over more social processes (Larson 2014; Corben 2016; Dube 2018). Informed by critical social theories, the two third‐order concepts developed in this review (‘neoliberal logic’ and ‘social exclusion’) provide insights into potential social processes or mechanisms underpinning vaccination decision‐making. Therefore, these could potentially be used to complement and extend the core psychological constructs of the ‘C frameworks’.
In terms of the four related published Cochrane Reviews of intervention effectiveness, as revealed in the matrix in Figure 8, many of the overarching factors our review identified as influencing parents' vaccination views and practices were underrepresented in the interventions tested in the studies. In particular, relatively few interventions considered or targeted parents’ broader health beliefs and practices, the social networks and groups with which parents are affiliated, and the interactions and forms of communication between healthcare workers and parents. No interventions appeared to consider parents’ experiences of the social nature of vaccination services. Moreover, seven of the eight interventions that addressed the issue of trust/distrust in vaccination focused specifically on providing a range of basic services or goods along with vaccination. Our review found that inadequate public services or goods may be just one of the many complex reasons for parents' distrust of vaccination. Future trials should consider incorporating interventions that target a wider array of factors influencing parents' vaccination views and practices. Specifically, there is a need for more interventions which target parents’ broader health beliefs and practices, the social networks and groups with which parents are affiliated, the interactions and forms of communication between healthcare workers and parents, and the context‐specific factors potentially contributing to parents' distrust in vaccination.
Overall completeness and applicability of the evidence
The studies included in this review encompassed diverse countries and socioeconomic settings. The sampling approach we used (see 'Sampling of studies' above) was geared towards including only conceptually‐rich studies, and as such, the evidence of this review has a relatively high degree of depth, detail, and breadth. Moreover, nearly half (n = 13) of the studies used a long‐term ethnographic approach (sometimes spanning many years), including various types of observational and participatory methods. This may have enabled researchers to develop an in‐depth understanding of parents’ unarticulated thoughts and actual practices, in addition to what they explicitly said. These insights may have further enhanced the completeness of the findings. It is possible, however, that our inclusion of studies published only in English, German, or French led to the omission of findings from cultural contexts where these languages are not the norm. Similarly, our use of a purposeful sampling approach may have led to the omission of findings relevant to particular populations, settings, and experiences. For example, our sampling approach resulted in all eligible studies from the WHO Eastern Mediterranean region being excluded from the analysis.
All of the studies we included explored parental views and practices regarding routine childhood vaccination. Yet a large majority of studies focused their analyses and findings on those views and practices associated with reduced acceptance (e.g. hesitancy or nonacceptance) of routine childhood vaccination. In addition, many studies only included parents who were hesitant towards or nonaccepting of routine childhood vaccination. This focus of the included studies is thus reflected in the findings of our review, which tend to concentrate on the factors associated with reduced acceptance of routine childhood vaccination. Factors that reduce and those that enhance vaccination are not necessarily binary categories that can be populated by their opposites. A greater focus specifically on the factors that enhance acceptance of routine childhood vaccination would add important insights into how acceptance might be sustained over time.
While most of the studies targetted parents, the majority were conducted with mothers or female caregivers only. When fathers or male caregivers were included, the researchers generally did not distinguish between mothers' and fathers’ perspectives, nor did they explore any potential gender‐based differences in their analysis. Thus, we are uncertain whether fathers have the same perspectives and practices regarding childhood vaccination.
Our review excluded studies that focused on hypothetical vaccines, future vaccines, and vaccines given in response to an outbreak situation, as we were interested in gaining a general understanding of parents’ views and practices towards routine childhood vaccination. It is therefore unclear whether the findings of this review can be appropriately applied to nonroutine vaccines, such as those given in an outbreak. Moreover, some included studies focused on specific vaccines: six studies (all from the UK) focused exclusively on the MMR vaccine, and three studies (in India and Nigeria) focused exclusively on the polio vaccine. These vaccines in these settings have a particularly controversial history, including the publication of a now‐retracted research paper linking the combined MMR vaccine to colitis and autism spectrum disorders (Godlee 2011), which was well known to the British public, and the historical, widespread social resistance to, and boycott of, the polio vaccine in India and Nigeria, respectively (Larson 2011). Many of the findings of this review rely heavily on findings from these studies. It is possible that parents’ views and practices regarding childhood vaccination were different in settings where these controversies occurred, compared to settings where they did not.
Limitations of the review
All of the studies included (and sampled) in our review were published in English, although various German and French studies were included at the full‐text screening stage. The scarcity of studies identified from non‐anglophone countries may be partly attributble to the fact that we did not include regional databases as part of our search strategy (e.g. the Latin American and Caribbean Health Science Information database, LILACS; Biblioteca Regional de Medicina, BIREME; African Index Medicus). We also made the decision to only include studies published in languages spoken by the review authors, which meant that only articles in French, English, and German were eligible for inclusion. This decision was based on our use of a meta‐ethnographic approach, an interpretative synthesis methodology that depends upon an in‐depth and nuanced understanding of the meanings of complex conceptual data (see ‘Language translation’ for more details). Ultimately, the absence of studies from non‐anglophone countries means that we may have missed important findings of studies from cultural contexts where English is not the norm, a key limitation of our review.
The volume of data included in the analysis meant that it was feasible for only one review author (SC) to lead the data analysis processes, albeit with regular discussion with, input, and verification from other review authors. We recognise that these processes are inherently interpretive: more than one review author undertaking these processes independently may have produced different interpretations and enhanced the exploration of alternative explanations. The volume of data also meant that, in the early stages of the analysis, we organised the data into preliminary broad themes which served as the basis for the translations. While this initial grouping was pragmatic, it may have constrained the emergence of new categories and interpretations during the subsequent translation and synthesis stages. Finally, based on our initial sense of a commonality in findings amongst studies in HICs and amongst those in LMICs, our analysis involved grouping the studies according to country income level. While this approach helped preserve one important aspect of context during the translation and synthesis processes, it may have also impacted on the overall interpretations of the synthesis.
Authors' conclusions
Implications for practice
Below are a set of questions and prompts that may help policy‐ and decision‐makers when planning and implementing strategies to promote childhood vaccination acceptance or uptake. The questions and prompts are based on the findings of this review (see Appendix 3). They also align with implications identified in a linked review on perceptions and experiences of communication about routine childhood vaccination (Ames 2017b).
When applying these questions and prompts, please consider the following points.
The studies in our review took place in settings or amongst populations that may differ from your own. Not all factors will therefore necessarily be applicable. Similarly, our review suggests that parents may accept some vaccines for some diseases, but not others. Successful development and implementation of interventions will require an understanding of, and then a tailoring to, the target setting and the target vaccine and disease.
There are a wide range of interventions relevant to increasing childhood vaccination uptake. The questions and prompts below are not geared towards any specific strategy; they can be used to inform all strategies or help inform decisions regarding which types of strategies might be most important.
Finally, the questions and prompts were informed by our position that adherence to the currently recommended vaccines is an important public health measure. Our perspective also recognises the importance of supporting an individual’s right to make their own decision about vaccination, including having access to evidence‐based information about vaccination, such as side effects, evidence gaps, and uncertainties. This perspective may not be shared in all settings. It is therefore important to consider what the vaccination values, aims, and policies are in your setting, and how these may potentially diverge from the perspective provided here.
In sum, these questions and prompts should be regarded as guidance to help stakeholders think about how best to design and deliver strategies to promote vaccination acceptance or uptake that are tailored to the specific needs, priorities, and values of their own context.
1. Have you considered the broader beliefs and practices that parents in your target setting have about health and illness, and the role they perceive vaccination to play within these?
For instance, might parents hold various religious beliefs, or naturalistic views about health and illness, that may reduce acceptance of vaccination? Or might parents hold certain beliefs about infants and their immune systems that might increase or decrease acceptance of vaccination? Might parents have an individualistic view of health and the risks and benefits of vaccines? Might they perceive personal responsibility and choice regarding health and healthcare decision‐making as more important than collective responsibility? Might parents experience these views as in conflict with vaccination promotion messages, and therefore be less accepting of vaccination? What other health beliefs might parents have, and what specific meanings, fears, or reservations about vaccination do these give rise to?
Have you considered how the intervention(s) could be tailored to the specific health beliefs and practices of parents in your target setting ‐ for instance, by providing vaccination communication that acknowledges these beliefs and practices, and attempts to address the concerns, questions, and tensions they may give rise to?
2. Have you taken into account the social networks and groups in which parents in your target setting reside or with which they are affiliated?
What are the different groups (for example, social, cultural, religious, and geographical) that parents in your target setting belong to or inhabit? What are the common vaccination views and practices within these groups? For instance, is vaccination generally supported, or alternatively might non‐vaccination be a social norm, within these groups?
Have you considered whether the intervention(s) could incorporate the social groups in which parents in your target setting belong, such as involving influential individuals within these groups (e.g. key opinion leaders) in the design, planning, and/or delivery of the intervention(s)?
3. Have you considered how parents in your target setting perceive the authorities associated with vaccination programmes?
Might parents feel distrustful towards any of the authorities associated with vaccination programmes ‐ for instance, government, healthcare workers, medical researchers, the pharmaceutical industry, global health agencies, or other relevant stakeholders?
If so, have you considered the specific reasons for this distrust? For instance, might they perceive them to be driven by motives other than the best interests of their child, such as financial gain? Might parents be aware of or have experienced ‘scandals’ in the past related to vaccination or other health‐related issues that have made them distrustful of authorities? Might parents be distrustful of authorities because their other concerns and priorities (e.g. food, sanitation, housing, income, employment, and general healthcare) are not being met, and might nonacceptance of vaccination be a form of resistance or a mechanism to have their other concerns and priorities addressed?
Have you considered whether the intervention(s) could be tailored to address the specific reasons for parents’ distrust, such as dialogue‐based approaches inviting open discussion about the reasons for distrust and how services could be reorganised in ways that might increase trust? Or could the interventions developed incorporate broader development goals by providing a wider range of basic services or goods along with vaccination? Alternatively, have you considered collaborating with groups or individuals that are known to be a trusted source amongst parents (e.g. non‐governmental organisations, local opinion leaders, etc.), potentially involving them in the design, planning, and/or delivery of the intervention(s)?
4. Have you considered the social or economic challenges parents in your target setting may face in accessing vaccination services?
For instance, do parents need to travel long distances to get to vaccination services? Might parents have demanding daily schedules that make it difficult to take time out for vaccination? What other struggles may parents face in negotiating vaccination services for their children?
Have you considered whether the intervention(s) could target the specific barriers parents face in accessing vaccination ‐ for instance, through the provision of vaccination outreach or mobile vaccination teams that bring vaccination closer to where parents live?
5. Have you considered whether there are features of vaccination services in your target setting that parents might find undesirable or inconvenient?
For instance, might vaccination involve (formal or informal) costs for parents? Or might parents experience long waiting times for vaccination? Or are regular vaccine stock‐outs an issue in your healthcare facility? Or might there be procedures that parents need to follow in order to obtain vaccination (e.g. those pertaining to the vaccination booklet) that they might find constraining or complicated to follow?
Have you considered whether the intervention(s) could be tailored to address the specific features of vaccination services that might diminish parents’ acceptance of vaccination or trust in vaccination programmes, or both, in your target setting? For instance, if vaccine stock‐outs are a regular feature of your health facility, can you identify what the underlying reasons for stock‐outs are and how these problems could be addressed? Could the logistical procedures parents need to follow for vaccination be potentially redesigned, so they are more responsive to parents' needs and circumstances? Could the physical environment at your health facility be reorganised to facilitate more efficient vaccination delivery? Could aspects of vaccination programmes (e.g. healthcare worker incentives for vaccination) that foster parents' distrust be rethought and potentially restructured?
6. Have you considered the ‘social’ nature of vaccination services, and how this might be experienced by parents?
For instance, might some parents experience attendance of vaccination services as a positive social event, one whereby they receive affirmation about themselves and their children? Alternatively, might some parents (e.g. poorer women, immigrants, fathers) feel judged or alienated by others when attending vaccination services?
Have you considered whether the intervention(s) could draw upon and promote the positive social aspects of vaccination services? At the same time, could the delivery of vaccination be rethought and potentially restructured so that less integrated parents might feel less judged or alienated when attending vaccination services?
7. Have you considered how parents in your target setting feel about the interactions they have with healthcare workers?
For instance, do they feel supported or mistreated by healthcare workers? Do they feel they can have open, respectful discussions with healthcare workers in a caring, sensitive, and non‐judgemental way? Do they feel they can ask healthcare workers questions and receive clear and respectful answers? Do parents perceive the vaccination information they receive from healthcare workers as impartial, balanced, independent, and transparent?
Have you considered intervention(s) that specifically target healthcare workers ‐ for instance, by making them aware of the influence their interactions with parents may have, providing them with training in communication skills or increased supervision and support, or adapting the types of vaccination information healthcare workers have access to and provide to parents? (See Ames 2017b for further guidance on tailoring vaccination information for parents.)
Implications for future research
We have developed these implications for research based on the overview of studies included in this review and our GRADE‐CERQual assessments of the review findings.
There is a need for better reporting of methods in qualitative studies, including those from more sociological and anthropological health research traditions. In particular, future qualitative studies should provide more detailed and transparent reporting of sampling methods and data analysis. These studies should also pay more attention to, and provide evidence for, the researchers’ roles in the study and their prior assumptions and standpoints, and how these may have impacted on the process and findings of the study (i.e. researcher reflexivity).
Qualitative research about parental views and practices regarding routine childhood vaccination needs to include a broader spectrum of contexts and population groups. In particular, more studies are needed in the regions of South America, the Middle East, and Eastern Europe. Moreover, more studies with parents from higher socioeconomic groups in LMICs and amongst minority or more marginalised groups in HICs would be beneficial. For example, the findings from a study included in this review amongst parents from higher socioeconomic groups in Brazil revealed that these parents may hold neoliberal values and views similar to those held by parents in HICs. It would be useful for studies in other LMICs to explore this issue further. Similarly, the findings from one study included in this review amongst Gypsy, Roma, and Traveller parents in Britain revealed that socioeconomic challenges in accessing vaccination services may reduce these parents' acceptance of vaccination in a similar way to many parents in LMICs. It would be useful for studies to determine the relevance of this issue amongst parents from other marginalised or minority groups in HICs.
Future studies should also consider the perceptions of fathers, to help give us a better understanding of their viewpoints and how gender identities, roles, and relations might influence ideas and practices regarding childhood vaccination. This understanding would facilitate further development of conceptual and theoretical models in this area. Finally, more qualitative research is needed on the drivers of childhood vaccination acceptance and active demand (as opposed to hesitancy and refusal), which could provide important insights into how vaccination acceptance uptake might be sustained over time.
Future quantitative studies on vaccination acceptance, hesitancy, or nonacceptance that examine levels of influence beyond individual factors (i.e. to also incorporate community or contextual factors) would be worthwhile. Future trials should consider incorporating interventions that target a broader array of factors influencing parents' vaccination views and practices, with consideration of the factors identified in this review. Specifically, there is a need for more interventions which target parents’ broader health beliefs and practices, the social networks and groups with which parents are affiliated, the interactions and forms of communication between healthcare workers and parents, and the context‐specific factors potentially contributing to parents' distrust in vaccination.
In future updates of this review, we will consider how studies from non‐anglophone countries might be better represented; for example, by broadening the scope of regional databases searched, employing an alternative (potentially more aggregative) qualitative synthesis approach, or adding review authors who speak additional languages so that studies published in a wider range of languages can potentially be included. Moreover, for findings which were downgraded in the GRADE‐CERQual assessments, in future updates of this review, we will consider whether any studies that were included but not sampled could contribute data to enhance confidence.
History
Protocol first published: Issue 2, 2019
Acknowledgements
When preparing this review, we used EPOC’s Protocol and Review Template for Qualitative Evidence Synthesis (Glenton 2020a). We also used EPOC’s plain language summary template (Glenton 2020b).
SC, BS, ES, NL, and CW are supported by the South African Medical Research Council, and BS is also supported by the University of the Western Cape, South Africa.
We would like to thank the following editors and peer referees who provided comments to improve the review: Claire Glenton, Anjali Sharma, Heather Ames, and Andrew Booth. We would also like to thank Marit Johansen for help with developing the search strategies, Elizabeth Paulsen for her logistical support, and Faith Armitage for copy‐editing the review.
The Norwegian Satellite of Cochrane Effective Practice and Organisation of Care (EPOC) receives funding from the Norwegian Agency for Development Cooperation (Norad), via the Norwegian Institute of Public Health, to support review authors in the production of their reviews.
This Cochrane Review is associated with the Research, Evidence and Development Initiative (READ‐It). READ‐It (project number 300342‐104) is funded by UK aid from the UK government; however, the views expressed do not necessarily reflect the UK government’s official policies.
Appendices
Appendix 1. Search strategies
PDQ‐Evidence, Epistemonikos Foundation (searched 03 June 2020)
Limited to Publication type: Systematic Review
Title/Abstract: "anti vaccine" OR anti‐vaccine OR antivaccine OR "anti vaccines" OR anti‐vaccines OR antivaccines OR "anti vaccination" OR anti‐vaccination OR antivaccination
OR
Title/Abstract: (vaccine OR vaccines OR vaccination OR immunization OR immunization) AND (attitude OR attitudes OR perspective OR perspectives OR perception OR perceptions OR belief OR beliefs OR concern OR concerns OR view OR views OR acceptance OR acceptability OR hesitant OR hesitancy OR refusal OR resistance OR rejection OR deny OR denier OR deniers OR denial)
CINAHL 1980‐present, EbscoHost (searched 03 June 2020)
| # | Query | Results |
| S41 | S33 OR S39 Limiters ‐ Exclude MEDLINE records | 1,073 |
| S40 | S33 OR S39 | 2,647 |
| S39 | S32 AND S38 | 994 |
| S38 | S34 OR S35 OR S36 OR S37 | 372,829 |
| S37 | TI ( (qualitative or group W0 discussion* or focus W0 group* or themes) ) OR AB ( (qualitative or group W0 discussion* or focus W0 group* or themes) ) | 195,328 |
| S36 | (MH "Focus Groups") | 49,802 |
| S35 | (MH "Interviews") | 168,731 |
| S34 | (MH "Qualitative Studies+") | 166,852 |
| S33 | S30 AND S31 | 2,503 |
| S32 | S30 AND S31 | 6,585 |
| S31 | S6 OR S27 | 11,419 |
| S30 | S28 OR S29 | 929,651 |
| S29 | TI ( child* or infant* or infancy or newborn* or new W0 born* or neonat* or neo W0 nat* or postnatal* or post W0 natal* or baby* or babies or toddler* ) OR AB ( child* or infant* or infancy or newborn* or new W0 born* or neonat* or neo W0 nat* or postnatal* or post W0 natal* or baby* or babies or toddler* ) | 665,185 |
| S28 | (MH "Child") OR (MH "Child, Preschool") OR (MH "Infant") OR (MH "Infant, Newborn") | 684,396 |
| S27 | S12 AND S26 | 8,110 |
| S26 | S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25 | 315,434 |
| S25 | TI ( (parent* or mother* or father* or informal W0 caregiver*) ) OR AB ( (parent* or mother* or father* or informal W0 caregiver*) ) | 228,133 |
| S24 | (MH "Mothers") | 31,940 |
| S23 | (MH "Fathers") | 6,820 |
| S22 | (MH "Parents") | 45,472 |
| S21 | (MH "Parenting") | 19,579 |
| S20 | (MH "Parental Behavior") | 2,369 |
| S19 | (MH "Parental Attitudes") | 14,116 |
| S18 | (MH "Caregiver Attitudes") | 1,581 |
| S17 | (MH "Health Beliefs") | 15,308 |
| S16 | (MH "Attitude to Health") | 44,065 |
| S15 | (MH "Attitude to Medical Treatment") | 843 |
| S14 | (MH "Treatment Refusal") | 5,423 |
| S13 | (MH "Refusal to Participate") | 249 |
| S12 | S7 OR S8 OR S9 OR S10 OR S11 | 78,683 |
| S11 | TI ( (vaccin* or immunis* or immuniz*) ) OR AB ( (vaccin* or immunis* or immuniz*) ) | 58,760 |
| S10 | (MH "Vaccination Coverage") | 419 |
| S9 | (MH "Vaccines+") | 47,503 |
| S8 | (MH "Immunization Programs") | 5,827 |
| S7 | (MH "Immunization") | 25,051 |
| S6 | S1 OR S2 OR S3 OR S4 OR S5 | 5,695 |
| S5 | TI ( (vaccin* or immunis* or immuniz*) N2 (attitude* or perspective* or perception* or belief* or concern* or view or views or accept* or hesita* or refus* or reject* or abstain* or declin* or resist* or object* or deny* or denier* or denial* or decision* or behavior* or behaviour*) ) OR AB ( (vaccin* or immunis* or immuniz*) N2 (attitude* or perspective* or perception* or belief* or concern* or view or views or accept* or hesita* or refus* or reject* or abstain* or declin* or resist* or object* or deny* or denier* or denial* or decision* or behavior* or behaviour*) ) | 4,338 |
| S4 | TI ( vaccin* or immunis* or immuniz* ) AND TI ( attitude* or perspective* or perception* or belief* or concern* or view or views or accept* or hesita* or refus* or reject* or abstain* or declin* or resist* or object* or deny* or denier* or denial* or decision* or behavior* or behaviour* ) | 2,900 |
| S3 | TI ( (anti W0 vaccin* or antivaccin*) ) OR AB ( (anti W0 vaccin* or antivaccin*) ) | 210 |
| S2 | (MH "Anti‐Vaccination Movement") | 82 |
| S1 | (MH "Attitude to Vaccines") | 507 |
MEDLINE and Epub Ahead of Print, In‐Process & Other Non‐Indexed Citations and Daily 1946 to June 02, 2020, Ovid (searched 03 June 2020)
| # | Searches | Results |
| 1 | Vaccination Refusal/ | 316 |
| 2 | Anti Vaccination Movement/ | 69 |
| 3 | (anti vaccin* or antivaccin*).ti,ab,kf. | 658 |
| 4 | or/1‐3 | 980 |
| 5 | exp Vaccines/ | 226948 |
| 6 | Vaccination/ | 80791 |
| 7 | Mass Vaccination/ | 3008 |
| 8 | Immunization/ | 50518 |
| 9 | Immunization Programs/ | 10721 |
| 10 | or/5‐9 | 289042 |
| 11 | "Patient Acceptance of Health Care"/ | 46279 |
| 12 | Refusal to Participate/ | 617 |
| 13 | Treatment Refusal/ | 11795 |
| 14 | Health Knowledge, Attitudes, Practice/ | 110420 |
| 15 | Attitude to Health/ | 83226 |
| 16 | or/11‐15 | 234096 |
| 17 | 10 and 16 | 7696 |
| 18 | ((vaccin* or immunis* or immuniz*) and (attitude* or perspective* or perception* or belief* or concern* or view or views or accept* or hesita* or refus* or reject* or abstain* or declin* or resist* or object* or deny* or denier* or denial* or decision*)).ti. | 7024 |
| 19 | ((vaccin* or immunis* or immuniz*) adj2 (attitude* or perspective* or perception* or belief* or concern* or view or views or accept* or hesita* or refus* or reject* or abstain* or declin* or resist* or object* or deny* or denier* or denial* or decision*)).ab. | 7240 |
| 20 | ((vaccin* or immunis* or immuniz*) adj2 (attitude* or perspective* or perception* or belief* or concern* or view or views or accept* or hesita* or refus* or reject* or abstain* or declin* or resist* or object* or deny* or denier* or denial* or decision*)).kf. | 619 |
| 21 | ((vaccination or immunisation or immunization) adj (behavior? or behaviour?)).ti,ab,kf. | 288 |
| 22 | or/18‐21 | 12381 |
| 23 | exp Vaccines/ | 226948 |
| 24 | Vaccination/ | 80791 |
| 25 | Mass Vaccination/ | 3008 |
| 26 | Vaccination Coverage/ | 1029 |
| 27 | Immunization/ | 50518 |
| 28 | Immunization Programs/ | 10721 |
| 29 | (vaccin* or immunis* or immuniz*).ti,ab,kf. | 391173 |
| 30 | or/23‐29 | 459912 |
| 31 | Child/ | 1677091 |
| 32 | Child,Preschool/ | 912085 |
| 33 | Infant/ | 786913 |
| 34 | Infant, Newborn/ | 600946 |
| 35 | (child* or infant* or infancy or newborn* or new born* or neonat* or neo nat* or postnatal* or post natal* or baby* or babies or toddler*).ti,ab,kf. | 2051244 |
| 36 | or/31‐35 | 3154084 |
| 37 | Parents/ | 63122 |
| 38 | Mothers/ | 43198 |
| 39 | Fathers/ | 8980 |
| 40 | Parenting/ | 16530 |
| 41 | Parental Consent/ | 3242 |
| 42 | (parent* or mother* or father* or informal caregiver*).ti,ab,kf. | 613789 |
| 43 | or/37‐42 | 639707 |
| 44 | 30 and 36 and 43 | 13603 |
| 45 | 17 or 22 or 44 | 27204 |
| 46 | limit 45 to "qualitative (maximizes specificity)" | 1098 |
| 47 | 45 and (Qualitative Research/ or Interviews as Topic/) | 825 |
| 48 | 45 and (qualitative or group discussion? or focus group? or themes).ti,ab,kf. | 1361 |
| 49 | or/46‐48 | 1753 |
| 50 | 4 or 49 | 2670 |
| 51 | limit 50 to yr=1974‐current | 2612 |
Embase 1974 to 2020 June 02, Ovid (searched 03 June 2020)
| # | Searches | Results |
| 1 | vaccination refusal/ | 397 |
| 2 | anti‐vaccination movement/ | 158 |
| 3 | (anti vaccin* or antivaccin*).ti,ab,kw. | 721 |
| 4 | or/1‐3 | 1150 |
| 5 | exp vaccine/ | 325735 |
| 6 | vaccination/ | 138488 |
| 7 | immunization/ | 93367 |
| 8 | mass immunization/ | 3473 |
| 9 | or/5‐8 | 414102 |
| 10 | exp patient attitude/ | 399250 |
| 11 | attitude to health/ | 110938 |
| 12 | or/10‐11 | 497073 |
| 13 | 9 and 12 | 9246 |
| 14 | ((vaccin* or immunis* or immuniz*) and (attitude* or perspective* or perception* or belief* or concern* or view or views or accept* or hesita* or refus* or reject* or abstain* or declin* or resist* or object* or deny* or denier* or denial* or decision*)).ti. | 7901 |
| 15 | ((vaccin* or immunis* or immuniz*) adj2 (attitude* or perspective* or perception* or belief* or concern* or view or views or accept* or hesita* or refus* or reject* or abstain* or declin* or resist* or object* or deny* or denier* or denial* or decision*)).ab. | 9481 |
| 16 | ((vaccin* or immunis* or immuniz*) adj2 (attitude* or perspective* or perception* or belief* or concern* or view or views or accept* or hesita* or refus* or reject* or abstain* or declin* or resist* or object* or deny* or denier* or denial* or decision*)).kw. | 717 |
| 17 | ((vaccination or immunisation or immunization) adj (behavior? or behaviour?)).ti,ab,kw. | 315 |
| 18 | or/14‐17 | 15146 |
| 19 | exp vaccine/ | 325735 |
| 20 | vaccination/ | 138488 |
| 21 | vaccination coverage/ | 1866 |
| 22 | immunization/ | 93367 |
| 23 | mass immunization/ | 3473 |
| 24 | (vaccin* or immunis* or immuniz*).ti,ab,kw. | 445783 |
| 25 | or/19‐24 | 552320 |
| 26 | childhood/ | 72218 |
| 27 | child/ | 1697781 |
| 28 | preschool child/ | 540559 |
| 29 | school child/ | 360760 |
| 30 | infant/ | 587255 |
| 31 | newborn/ | 523571 |
| 32 | baby/ | 14184 |
| 33 | toddler/ | 4690 |
| 34 | (child* or infant* or infancy or newborn* or new born* or neonat* or neo nat* or postnatal* or post natal* or baby* or babies or toddler*).ti,ab,kw. | 2457267 |
| 35 | or/26‐34 | 3368973 |
| 36 | parent/ | 91822 |
| 37 | father/ | 22746 |
| 38 | mother/ | 84893 |
| 39 | child parent relation/ | 51471 |
| 40 | parental consent/ | 4229 |
| 41 | parental behavior/ | 10895 |
| 42 | (parent* or mother* or father* or informal caregiver*).ti,ab,kw. | 771314 |
| 43 | or/36‐42 | 806952 |
| 44 | 25 and 35 and 43 | 17139 |
| 45 | 4 or 13 or 18 or 44 | 35862 |
| 46 | limit 45 to "qualitative (maximizes specificity)" | 1114 |
| 47 | 45 and (qualitative research/ or exp interview/) | 1913 |
| 48 | 45 and (qualitative or group discussion? or focus group? or themes).ti,ab,kw. | 1606 |
| 49 | or/46‐48 | 2747 |
| 50 | limit 49 to yr=1974‐current | 2736 |
| 51 | limit 50 to embase | 1601 |
APA PsycInfo 1806 to May Week 4 2020 (searched 03 June 2020)
| # | Searches | Results |
| 1 | (anti vaccin* or antivaccin*).ti,ab,id. | 97 |
| 2 | immunization/ | 4575 |
| 3 | (vaccin* or immunis* or immuniz*).ti,ab,id. | 8803 |
| 4 | or/2‐3 | 8908 |
| 5 | (child* or infant* or infancy or newborn* or new born* or neonat* or neo nat* or postnatal* or post natal* or baby* or babies or toddler*).ti,ab,id. | 785148 |
| 6 | ("100" or "120" or "140" or "160" or "180").ag. | 537971 |
| 7 | or/5‐6 | 919469 |
| 8 | parental attitudes/ | 17434 |
| 9 | treatment refusal/ | 770 |
| 10 | health attitudes/ | 10234 |
| 11 | risk perception/ | 6463 |
| 12 | parenting/ | 10065 |
| 13 | parents/ | 39623 |
| 14 | mothers/ | 37142 |
| 15 | fathers/ | 10359 |
| 16 | (parent* or mother* or father* or informal caregiver*).ti,ab,id. | 363801 |
| 17 | or/8‐16 | 382577 |
| 18 | 4 and 7 and 17 | 1465 |
| 19 | ((vaccin* or immunis* or immuniz*) and (attitude* or perspective* or perception* or belief* or concern* or view or views or accept* or hesita* or refus* or reject* or abstain* or declin* or resist* or object* or deny* or denier* or denial* or decision*)).ti,ab,id. | 4384 |
| 20 | ((vaccination or immunisation or immunization) adj (behavior? or behaviour?)).ti,ab,id. | 91 |
| 21 | or/19‐20 | 4396 |
| 22 | 18 or 21 | 4926 |
| 23 | limit 22 to "qualitative (maximizes specificity)" | 403 |
| 24 | 22 and (qualitative research/ or interviews/ or interviewing/ or questioning/) | 20 |
| 25 | 22 and (qualitative or group discussion? or focus group? or themes).ti,ab,id. | 499 |
| 26 | or/23‐25 | 514 |
| 27 | 1 or 26 | 601 |
| 28 | limit 27 to yr=1974‐current | 598 |
Appendix 2. Methodological limitations of sampled studiesa,b
| Study ID | 1. Are the setting(s) and context described adequately? | 2. Is the sampling strategy described, and is this appropriate? | 3. Is the data collection strategy described and justified? | 4. Is the data analysis described, and is this appropriate? |
5. Are the claims made/ findings supported by sufficient evidence? |
6. Is there evidence of reflexivity? | 7. Does the study demonstrate sensitivity to ethical concerns? | 8. Any other concerns? |
| Barbieri 2017 | Yes | Yes | Yes | Yes | Yes | No | Yes | |
| Bisht 2000 | No | No | No | No | Yes | No | No | |
| Brownlie 2005 | No | Yes | No | Yes | Yes | No | Yes | Yes |
| Brunson 2013 | Yes | Yes | Yes | Yes | Yes | No | No | |
| Carrion 2018 | No | Yes | Yes | Yes | Yes | Yes | No | |
| Casiday 2007 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |
| Chaturvedi 2009 | No | No | Yes | Yes | Yes | Yes | No | |
| Dube 2016 | No | Yes | Yes | Yes | Yes | No | No | |
| Dugas 2009 | Yes | No | Yes | No | Yes | No | No | |
| Giles‐Vernick 2016 | Yes | Yes | No | No | Yes | No | No | |
| Hussain 2015 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |
| Johnson 2014 | Yes | No | Yes | Yes | Yes | No | Yes | Yes |
| Leach 2007 | Yes | No | No | No | Yes | No | No | |
| Limaye 2020 | Yes | Yes | Yes | Yes | No | No | Yes | |
| McKnight 2014 | Yes | Yes | Yes | No | Yes | No | No | |
| Millimouno 2006 | Yes | No | Yes | No | Yes | No | Yes | |
| Peretti‐Watel 2019 | Yes | No | Yes | Yes | Yes | No | No | |
| Petts 2004 | Yes | Yes | Yes | No | Yes | No | No | |
| Poltorak 2005 | Yes | Yes | Yes | No | Yes | Yes | No | |
| Reich 2016 | Yes | Yes | Yes | No | Yes | Yes | Yes | |
| Renne 2010 | Yes | No | No | No | Yes | Yes | No | |
| Rogers 1995 | Yes | Yes | No | No | Yes | No | No | |
| Ruijs 2012 | Yes | Yes | Yes | Yes | Yes | Yes | No | |
| Smith 2017 | Yes | No | Yes | Yes | Yes | No | Yes | |
| Sobo 2016 | Yes | Yes | Yes | Yes | Yes | Yes | No | |
| Varghese 2013 | Yes | Yes | Yes | Yes | No | No | Yes | |
| Ward 2017 | Yes | No | Yes | Yes | Yes | Yes | No | Yes |
| aBased on a list of criteria used in previous Cochrane Reviews and originally based on the Critical Appraisal Skills Programme (CASP) quality assessment tool for qualitative studies (CASP 2018) bComprises a summarised version, excluding detailed notes for each question | ||||||||
Appendix 3. Moving from review findings to implications for practice
| Review finding | Implication for practice |
| Theme 1: ideas and practices surrounding (child) health and illness |
1. Have you considered the broader beliefs and practices parents in your target setting have about health and illness, and the role they perceive vaccination to play within these? |
|
Finding 1: religious beliefs. Some parents were less accepting of childhood vaccination due to the religious beliefs they held, and the view that illness, including in children, can only be prevented by divine providence. These parents expressed religious objections to vaccination. Finding 3: primacy of ‘nature’ and ‘the natural’. Some parents, predominantly from HICs, were less accepting of childhood vaccination due to their understanding of health and illness as holistic or naturalistic. This understanding conceives many biomedical interventions, including vaccination, as unnatural intrusions that are unnecessary or harmful. Various parents who held this view also engaged in certain ‘natural’ health promoting activities or “salutogenic parenting” which for them further negated the need for vaccination. |
• For instance, might parents hold various religious beliefs, or naturalistic views about health and illness, that may reduce acceptance of vaccination? |
| Finding 2: the ‘fragile’ infant. An understanding of infants and their immune systems as fragile and still in a state of development was common amongst parents across diverse settings, contexts, and population groups. Numerous parents characterised infants and young children as weak and vulnerable, and in need of protection against multiple social, biological, or spiritual threats. This perception was associated with both reduced and increased acceptance of childhood vaccination | • Or might parents hold certain beliefs about infants and their immune systems that might increase or decrease acceptance of vaccination? |
|
Finding 4: individualised health, immunity and vaccine‐response trajectories. Many parents, predominantly from HICs, held a view that children possess unique bodies and immune systems and therefore individual vaccine needs and vulnerabilities. As such, these parents frequently assessed the risks and benefits of vaccines as they pertain to their specific child, rather than in general. If the risks were seen to outweigh the benefits for their particular child, then these parents tended to be less accepting of childhood vaccination. Finding 5: claiming parental expertise. Many parents from HICs held a view of themselves as experts of their child, possessing the best understanding of their child’s health strengths and vulnerabilities. They in turn considered themselves best placed to judge their child’s vaccination needs and risks. Finding 6: personal choice and responsibility. Many parents, predominantly from HICs, perceived healthcare decision‐making, including vaccination, to be a matter of personal responsibility and choice. In cases where the risks of a vaccine or vaccination in general were thought to outweigh the benefits for their particular child, then these values of personal responsibility and choice were often prioritised over collective responsibility. These parents in turn tended to be less accepting of vaccination for their children. Finding 18: neoliberal logic. Many parents, predominantly from HICs, held a worldview informed by neoliberal discourses. These discourses understand health as individualised, and health‐related risks and decisions as matters of individual choice and responsibility. Furthermore, these discourses suggest that being a ‘good’ and responsible person in the world means consistently assessing one’s own, individual health‐related risks, seeking and questioning evidence about such risks, proactively avoiding and managing such risks, and understanding that one is singularly accountable for the outcomes that ensue. Some parents experienced this worldview as in conflict with vaccination promotion messages, which tend to be informed by other types of discourses. The discourses underpinning vaccination promotion messages frequently emphasise generalised risk and safety statistics, claim that ‘doctor knows best’, ask people to trust authorities and follow what they promote, and advocate for social responsibility and the health of the community. Parents’ perceived tension between the discourses informing their own worldview and those of vaccination promotion messages led some to resist these messages and be less accepting of vaccination. |
• Might parents have an individualistic view of health and the risks and benefits of vaccines? Might they perceive personal responsibility and choice regarding health and healthcare decision‐making as more important than collective responsibility? Might parents experience these views as in conflict with vaccination promotion messages and in turn be less accepting of vaccination? |
| • What other health beliefs might parents have, and what specific meanings, fears, or reservations about vaccination do these give rise to? • Have you considered how the intervention(s) could be tailored to the specific health beliefs and practices of parents in your target setting; for instance, by providing vaccination communication that acknowledges these beliefs and practices and attempts to address the concerns, questions, and tensions they may give rise to? |
|
| Theme 2: social communities and networks |
2. Have you taken into account the social networks and groups with which parents in your target setting reside or are affiliated? |
|
Finding 7: social networks shape vaccination ideas and practices. Parents' vaccination views and practices, across diverse settings, contexts, and population groups, were influenced by the vaccination views and experiences of their social networks. These networks included relatives, peers, neighbours and additional significant others in the community. However, the views and practices of other parents, and particularly other mothers, were especially influential. Finding 8: vaccination ideas and practices shape social networks. Parents' vaccination views and practices also shaped their social networks. Shared vaccination ideas and practices were a powerful force in building social relations and ties. While this phenomenon occurred amongst parents across the spectrum of vaccination attitudes, it may be particularly significant for parents who are less accepting of vaccination. In these cases, parents may be afforded access to various types of social resources, in turn potentially reinforcing both their group affiliation and vaccination views and practices. |
• What are the different groups ‐ for example, social, cultural, religious, geographical ‐ that parents in your target setting belong to or inhabit? What are the common vaccination views and practices within these groups? For instance, is vaccination generally supported, or alternatively, might non‐vaccination be a social norm, within these groups? • Have you considered whether the intervention(s) could incorporate the social groups in which parents in your target setting belong, such as involving influential individuals within these groups (e.g. key opinion leaders) in the design, planning, and/or delivery of the intervention(s)? |
| Theme 3: political events, relations and processes |
3. Have you considered how parents in your target setting perceive the authorities associated with vaccination programmes? |
|
Finding 9: distrust in the institutions or systems implicated with vaccination. Some parents were less accepting of vaccination due to a lack of, or breakdown in, trust in the institutions or systems implicated with vaccination ‐ most particularly, government, the pharmaceutical industry, and science. The reasons for this distrust were complex and contextually situated, embedded in political events, relations, and processes within specific times and places. Finding 10: generalised decline in trust of authority and expert systems. For some parents, distrust of the institutions or systems implicated with vaccination may be part and parcel of a more generalised contemporary trend of decreasing trust in authorities and expert systems. |
• Might parents feel distrustful towards any of the authorities associated with vaccination programmes; for instance, government, healthcare workers, medical researchers, the pharmaceutical industry, global health agencies, or other relevant stakeholders? If so, have you considered the specific reasons for this distrust? |
| Finding 11: agendas and interests underpinning the expert systems implicated with vaccination. For some parents, distrust of the institutions or systems implicated with vaccination was linked to their concerns about the agendas or interests embedded in these systems. Many of these parents were particularly concerned about the economic interests of these systems, and especially the economic interests of the pharmaceutical industry, which they perceived to be negatively influencing vaccination programmes. | • For instance, might they perceive them to be driven by motives other than the best interests of their child, such as financial gain? |
|
Finding 12: current and past controversies. Some parents' distrust of the institutions or systems implicated with vaccination was linked to particular ‘scandals’ or ‘controversies’ related to vaccination specifically or health‐related issues more broadly. The occurrence of such scandals, and the manner in which they were perceived to have been handled, caused some parents to feel misled by authorities and to question their legitimacy in protecting the public’s health. |
• Might parents be aware of or have experienced ‘scandals’ in the past, related to vaccination or other health‐related issues, that have made them distrustful of authorities? |
|
Finding 13: marginalisation, inadequate public services, and priority misalignment. Some parents' distrust in the institutions or systems implicated with vaccination was linked to their experiences of marginalisation, inadequate public services, or misalignment between their own priorities and those of the state. These experiences undermined trustful and benevolent state‐citizen relations, leading many parents to distrust government and government‐sponsored programs, including vaccination. Finding 19: social exclusion. Some parents, predominantly from LMICs, were less accepting of childhood vaccination due to their experiences of social exclusion. Social exclusion may involve economic disadvantage, residential segregation, a lack of political representation or power, discrimination and unequal protection of rights, and a myriad of socioeconomic barriers to good quality public services, including vaccination. Social exclusion weakened trustful government‐citizen relations, generated feelings of alienation from, and resentment towards, the state and others, and gave rise to frustration and demotivation in the face of structural challenges. These factors in turn led some parents who are socially excluded to distrust vaccination, to refuse vaccination as a form of resistance or a mechanism to bring about change, or to avoid vaccination due to the time, effort, (opportunity) costs and distress it creates. |
• Might parents be distrustful of authorities because their other concerns and priorities (e.g. food, sanitation, housing, income, employment, general health care) are not being met, and might nonacceptance of vaccination be a form of resistance or a mechanism to have their other concerns and priorities addressed? |
| • Have you considered whether the intervention(s) could be tailored to address the specific reasons for parents’ distrust, such as dialogue‐based approaches inviting open discussion about the reasons for distrust and how services could be reorganised in ways that might increase trust? • Or could the interventions developed incorporate broader development goals by providing a wider range of basic services or goods along with vaccination? • Alternatively, have you considered collaborating with groups or individuals that are known to be a trusted source amongst parents (e.g. non‐governmental organisations, local opinion leaders, etc.), potentially involving them in the design, planning, or delivery of the intervention(s)? |
|
| Theme 4: access‐supply‐demand interactions |
|
|
Finding 14: socio‐economic challenges in accessing vaccination services. Parents living in resource‐limited settings frequently face numerous socioeconomic challenges to accessing vaccination services, including practical questions of geography and transport, childcare constraints, and family economics and household work pressures. As a result of these challenges, some of these parents were less accepting of vaccination due to the time, effort, and opportunity costs accessing vaccination involved. Finding 19: social exclusion (see above for details). |
4. Have you considered the social or economic challenges parents in your target setting may face in accessing vaccination services? • For instance, do parents need to travel long distances to get to vaccination services? Might parents have demanding daily schedules that make it difficult to take time out for vaccination? What other struggles may parents face in negotiating vaccination services for their children? • Have you considered whether the intervention(s) could target the specific barriers parents face in accessing vaccination; for instance, through the provision of vaccination outreach or mobile vaccination teams that bring vaccination closer to where parents live? |
|
Finding 15: undesirable features of vaccination services and delivery logistics. Some parents were less accepting of vaccination due to undesirable features of vaccination services and delivery logistics. These features, common to vaccination services within resource‐limited settings, included resource constraints that affect vaccine supply and costs and health facility waiting times, and constraining organisational procedures. Finding 19: social exclusion (see above for details). |
5. Have you considered whether there are features of vaccination services in your target setting that parents might find undesirable or inconvenient? • For instance, might vaccination involve (formal or informal) costs for parents? Or might parents experience long waiting times for vaccination? Or are regular vaccine stock‐outs an issue in your healthcare facility? Or might there be procedures that parents need to follow in order to obtain vaccination (e.g. those pertaining to the vaccination booklet) that they might find constraining or complicated to follow? • Have you considered whether the intervention(s) could be tailored to address the specific features of vaccination services that might diminish parents’ acceptance of vaccination or trust in vaccination programmes, or both, in your target setting? For instance, if vaccine stock‐outs are a regular feature of your health facility, can you identify what the underlying reasons for stock‐outs are and how these problems could be addressed? Could the logistical procedures parents need to follow for vaccination be potentially redesigned, so they are more responsive to parents' needs and circumstances? Could the physical environment at your health facility be reorganised to facilitate more efficient vaccination delivery? Could aspects of vaccination programmes (e.g. healthcare worker incentives for vaccination) that foster parents' distrust be rethought and potentially restructured? |
| Finding 16: vaccination as a social event. Vaccination may be a social event where people gather and interact with each other. Some parents found this to a positive experience, whereby they received positive affirmation about themselves and their children. This potentially motivated attendance of childhood vaccination appointments. For other parents, the social nature of vaccination services was a negative experience, whereby they experienced judgement, disapproval, and alienation from others. This potentially demotivated attendance of childhood vaccination appointments. |
6. Have you considered the ‘social’ nature of vaccination services, and how this might be experienced by parents? • For instance, might some parents experience clinic attendance as a positive social event, one whereby they receive positive affirmation about themselves and their children? Alternatively, might some parents (e.g. poorer women, immigrants, fathers) feel judged or alienated by others when attending vaccination services? • Have you considered whether the intervention(s) could draw upon and promote the positive social nature of vaccination services? At the same time, could the delivery of vaccination be rethought and potentially restructured so that less integrated parents might feel less judged or alienated when attending? |
|
Finding 17: interactions with frontline healthcare workers. Parents' vaccination views and practices, across diverse settings, contexts and population groups, were mediated by the face‐to‐face interactions or personal relations they have with frontline healthcare workers. Some parents were less accepting of vaccination due to mistreatment from healthcare workers, and when they felt the vaccination information provided to them was simplistic and unbalanced. In contrast, some parents were more accepting of vaccination due to positively‐received engagements with healthcare workers, whereby they felt supported, listened to, and respected, and whereby healthcare workers shared balanced information and personal stories about themselves as parents. Finding 19: social exclusion (see above for details). |
7. Have you considered how parents in your target setting feel about the interactions they have with healthcare workers? • For instance, do they feel supported or mistreated by healthcare workers? Do they feel they can have open, respectful discussions with healthcare workers in a caring, sensitive, and non‐judgemental way? Do they feel they can ask healthcare workers questions and receive clear and respectful answers? • Do parents perceive the vaccination information they receive from healthcare workers as impartial, balanced, independent, and transparent? • Have you considered intervention(s) that specifically target healthcare workers; for instance, by making them aware of the influence their interactions with parents may have, providing them with training in communication skills or increased supervision and support, or adapting the types of vaccination information healthcare workers have access to and provide to parents? (See Ames 2017b for further guidance on tailoring vaccination information for parents.) |
Appendix 4. Evidence Profiles
| Finding 1: religious beliefs. Some parents were less accepting of childhood vaccination due to the religious beliefs they held, and the view that illness, including in children, can only be prevented by divine providence. These parents expressed religious objections to vaccination. | |
| Assessment for each GRADE‐CERQual component | |
| Methodological limitations | Minor concerns regarding methodological limitations because of poor reporting of sampling and data collection in both studies, and poor reporting of data analysis in one study. |
| Coherence | No or very minor concerns |
| Relevance | Moderate concerns because both studies were only partially relevant (1 study focused only on polio vaccination and 1 study focused on a specific group of parents ‐ orthodox Protestants) |
| Adequacy | Serious concerns because only 2 studies, both with relatively limited and thin data contributing to this finding. |
| Overall GRADE‐CERQual assessment and explanation | |
| Low confidence | Finding downgraded because of serious concerns about adequacy, moderate concerns about relevance (partial relevance), and minor concerns about methodological limitations |
| Contributing studies | |
| Renne 2010; Reich 2016 | |
| Finding 2: the ‘fragile’ infant. An understanding of infants and their immune systems as fragile and still in a state of development was common amongst parents across diverse settings, contexts, and population groups. Numerous parents characterised infants and young children as weak and vulnerable, and in need of protection against multiple social, biological, or spiritual threats. This perception was associated with both reduced and increased acceptance of childhood vaccination. | |
| Assessment for each GRADE‐CERQual component | |
| Methodological limitations | Minor concerns regarding methodological limitations because of poor reporting of sampling, data collection and data analysis in some studies, and limited evidence of reflexivity in some studies |
| Coherence | No or very minor concerns (the finding reflects the complexity and variation of the data, and is well supported by details in the underlying studies) |
| Relevance | No or very minor concerns regarding relevance (studies include a wide range of participants, countries, settings, and vaccines) |
| Adequacy | No or very minor concerns regarding adequacy (12 studies contributing a large amount of rich data) |
| Overall GRADE‐CERQual assessment and explanation | |
| High confidence | |
| Contributing studies | |
| Bisht 2000; Brownlie 2005; Poltorak 2005; Millimouno 2006; Casiday 2007; Leach 2007; Brunson 2013; McKnight 2014; Giles‐Vernick 2016; Reich 2016; Smith 2017; Limaye 2020 | |
| Finding 3: primacy of ‘nature’ and ‘the natural’. Some parents, predominantly from HICs, were less accepting of childhood vaccination due to their understanding of health and illness as holistic or naturalistic. This understanding conceives many biomedical interventions, including vaccination, as unnatural intrusions that are unnecessary or harmful. Various parents who held this view also engaged in certain ‘natural’ health‐promoting activities or “salutogenic parenting”, which for them further negated the need for vaccination. | |
| Assessment for each GRADE‐CERQual component | |
| Methodological limitations | Minor concerns due to lack of reporting of data analysis methods used in some studies and limited evidence of sensitivity to ethical concerns or reflexivity in many studies |
| Coherence | Minor concerns because there are insufficient data to support one aspect of the review finding (the notion of 'salutogenic parenting') (ambiguous data) |
| Relevance | Minor concerns because 4 studies only included parents who were hesitant towards or nonaccepting of vaccination, 4 studies only included parents from higher socioeconomic groups, and 3 studies focused only on MMR vaccination (partial relevance) |
| Adequacy | No or very minor concerns (9 studies contributing a large amount of rich data) |
| Overall GRADE‐CERQual assessment and explanation | |
| High confidence | |
| Contributing studies | |
| Rogers 1995; Brownlie 2005; Poltorak 2005; Casiday 2007; Dube 2016; Reich 2016; Barbieri 2017; Ward 2017; Peretti‐Watel 2019 | |
| Finding 4: individualised health, immunity and vaccine‐response trajectories. Many parents, predominantly from HICs, held a view that children possess unique bodies and immune systems and therefore individual vaccine needs and vulnerabilities. As such, these parents frequently assessed the risks and benefits of vaccines as they pertain to their specific child, rather than in general. If the risks were seen to outweigh the benefits for their particular child, then these parents tended to be less accepting of childhood vaccination. | |
| Assessment for each GRADE‐CERQual component | |
| Methodological limitations | Minor concerns due to poor reporting of data analysis and limited evidence of sensitivity to ethical concerns or reflexivity in many of the studies |
| Coherence | No or very minor concerns (the finding reflects the complexity and variation of the data, and is well supported by details in the underlying studies) |
| Relevance | Minor concerns because 4 studies focused only on MMR vaccination, 3 studies only included parents who were hesitant towards or nonaccepting of vaccination, and 4 studies only included parents from higher socioeconomic groups (partial relevance) |
| Adequacy | No or very minor concerns (10 studies contributing a large amount of rich data) |
| Overall GRADE‐CERQual assessment and explanation | |
| High confidence | |
| Contributing studies | |
| Rogers 1995; Brownlie 2005; Poltorak 2005; Casiday 2007; Brunson 2013; Dube 2016; Reich 2016; Sobo 2016; Barbieri 2017; Smith 2017 | |
| Finding 5: claiming parental expertise. Many parents from HICs held a view of themselves as experts of their child, possessing the best understanding of their child’s health strengths and vulnerabilities. They in turn considered themselves best placed to judge their child’s vaccination needs and risks. | |
| Assessment for each GRADE‐CERQual component | |
| Methodological limitations | Minor concerns due to limited evidence of sensitivity to ethical concerns and reflexivity in many studies |
| Coherence | Moderate concerns because although generally the case, the data were a bit more varied; for example, in some studies, parents did not consider themselves to be experts of their child, and other studies showed that some parents considered others (such as doctors, peers) to be experts of their children and also well‐positioned to judge their children's needs (contradictory data) |
| Relevance | Minor concerns because 4 studies focused only on MMR vaccination, 3 studies only included parents who were hesitant towards or nonaccepting of vaccination, and 4 studies only included parents from higher socioeconomic groups (partial relevance) |
| Adequacy | No or very minor concerns (10 studies contributing a large amount of rich data) |
| Overall GRADE‐CERQual assessment and explanation | |
| Moderate confidence | Finding downgraded because of moderate concerns about coherence (contradictory data), and minor concerns about relevance (partial relevance) and methodological limitations |
| Contributing studies | |
| Petts 2004; Poltorak 2005; Casiday 2007; Brunson 2013; Johnson 2014; Reich 2016; Sobo 2016; Ward 2017; Carrion 2018; Peretti‐Watel 2019 | |
| Finding 6: personal choice and responsibility. Many parents, predominantly from HICs, perceived healthcare decision‐making, including vaccination, to be a matter of personal responsibility and choice. In cases where the risks of a vaccine or vaccination in general were thought to outweigh the benefits for their particular child, then these values of personal responsibility and choice were often prioritised over collective responsibility. These parents in turn tended to be less accepting of vaccination for their children. | |
| Assessment for each GRADE‐CERQual component | |
| Methodological limitations | Minor concerns due to poor reporting of data analysis methods in many studies and limited evidence of sensitivity to ethical concerns or reflexivity in some studies |
| Coherence | Minor concerns because one aspect of the review finding (personal responsibility and choice prioritised over collective responsibility) was not explored in much detail by the studies. It is therefore unclear how adequately the data support this aspect of the finding (ambiguous data). |
| Relevance | Minor concerns because 5 studies focused only on MMR vaccination, 5 studies only included parents who were hesitant towards or nonaccepting of vaccination, and 6 studies only included parents from higher socioeconomic groups (partial relevance) |
| Adequacy | No or very minor concerns (12 studies contributing a large amount of rich data) |
| Overall GRADE‐CERQual assessment and explanation | |
| High confidence | |
| Contributing studies | |
| Rogers 1995; Petts 2004; Brownlie 2005; Poltorak 2005; Casiday 2007; Brunson 2013; Johnson 2014; Reich 2016; Sobo 2016; Barbieri 2017; Ward 2017; Carrion 2018 | |
| Finding 7: social networks shape vaccination ideas and practices. Parents' vaccination views and practices, across diverse settings, contexts, and population groups, were influenced by the vaccination views and experiences of their social networks. These networks included relatives, peers, neighbours, and additional significant others in the community. However, the views and practices of other parents, and particularly other mothers, were especially influential. | |
| Assessment for each GRADE‐CERQual component | |
| Methodological limitations | Minor concerns due to poor reporting of sampling, and limited demonstration of reflexivity and sensitivity to ethical concerns in many of the studies |
| Coherence | Minor concerns due to some contradictory data (e.g. some parents resisted and went against the views and practices of their social networks) |
| Relevance | No or very minor concerns regarding relevance (studies include a wide range of participants, countries, settings, and vaccines) |
| Adequacy | No or very minor concerns (16 studies contributing a large amount of rich data) |
| Overall GRADE‐CERQual assessment and explanation | |
| High confidence | |
| Contributing studies | |
| Petts 2004; Brownlie 2005; Poltorak 2005; Millimouno 2006; Casiday 2007; Leach 2007; Ruijs 2012; Brunson 2013; Varghese 2013; Johnson 2014; Dube 2016; Giles‐Vernick 2016; Sobo 2016; Barbieri 2017; Ward 2017; Peretti‐Watel 2019 | |
| Finding 8: vaccination ideas and practices shape social networks. Parents' vaccination views and practices also shaped their social networks. Shared vaccination ideas and practices were a powerful force in building social relations and ties. While this phenomenon occurred amongst parents across the spectrum of vaccination attitudes, it may be particularly significant for parents who are less accepting of vaccination. In these cases, parents may be afforded access to various types of social resources, in turn potentially reinforcing both their group affiliation and vaccination views and practices. | |
| Assessment for each GRADE‐CERQual component | |
| Methodological limitations | Minor concerns due to limited demonstration of reflexivity and sensitivity to ethical concerns in many of the studies |
| Coherence | Moderate concerns because only 2 studies provided support for part of the finding (phenomenon, and associated consequences, being particularly significant for parents who are less accepting of vaccination) (ambiguous data) |
| Relevance | Minor concerns because 1 study focused only on MMR vaccine and 2 studies only included parents from higher socioeconomic status (SES) groups and who were hesitant towards or nonaccepting of vaccination (partial relevance) |
| Adequacy | Moderate concerns because together the studies contributed relatively limited and thin data to this particular finding |
| Overall GRADE‐CERQual assessment and explanation | |
| Moderate confidence | Finding downgraded because of moderate concerns about adequacy and coherence (ambiguous data), and minor concerns about relevance (partial relevance) and methodological limitations |
| Contributing studies | |
| Poltorak 2005; Millimouno 2006; Leach 2007; Reich 2016; Ward 2017 | |
| Finding 9: distrust in the institutions or systems implicated with vaccination. Some parents were less accepting of vaccination due to a lack of, or breakdown in, trust in the institutions or systems implicated with vaccination ‐ most particularly, government, the pharmaceutical industry, and science. The reasons for this distrust were complex and contextually situated, embedded in political events, relations, and processes within specific times and places. | |
| Assessment for each GRADE‐CERQual component | |
| Methodological limitations | Minor concerns due to poor reporting of sampling, data analysis, and data collection in most studies, as well as limited evidence of sensitivity to ethical concerns or reflexivity in many studies |
| Coherence | Moderate concerns because there were contradictory data that did not fit the interpretation in this finding (e.g. one study refuted the explanatory potential of the concept of 'distrust', suggesting that there are other possible concepts that have been marginalised and subsumed under the notion of trust/distrust) |
| Relevance | No or very minor concerns (studies include a wide range of participants, countries, settings, and vaccines) |
| Adequacy | No or very minor concerns (17 studies contributing a large amount of rich data) |
| Overall GRADE‐CERQual assessment and explanation | |
| Moderate confidence | Finding downgraded due to moderate concerns about coherence (contradictory data) and minor concerns about methodological limitations |
| Contributing studies | |
| Rogers 1995; Petts 2004; Brownlie 2005; Poltorak 2005; Casiday 2007; Leach 2007; Chaturvedi 2009; Renne 2010; Varghese 2013; Hussain 2015; Dube 2016; Giles‐Vernick 2016; Reich 2016; Smith 2017; Ward 2017; Carrion 2018; Peretti‐Watel 2019 | |
| Finding 10: generalised decline in trust of authority and expert systems. For some parents, distrust of the institutions or systems implicated with vaccination may be part and parcel of a more generalised contemporary trend of decreasing trust in authorities and expert systems. | |
| Assessment for each GRADE‐CERQual component | |
| Methodological limitations | Minor concerns due to poor reporting of sampling and data collection methods, as well as limited evidence of reflexivity and sensitivity to ethical concerns in most of the studies |
| Coherence | Moderate concerns because there were contradictory data that did not fit the interpretation in this finding (e.g. one study refuted the idea of a generalised contemporary trend towards decreasing trust in authorities and expert systems, suggesting this is an erroneous and oversimplified interpretation) |
| Relevance | Serious concerns because all studies were conducted in HICs (partial relevance); 3 studies focused only on MMR vaccination (partial relevance); and 2 studies only included parents from higher SES groups (partial relevance) |
| Adequacy | Moderate concerns because together the studies contributed relatively limited and thin data to this particular finding |
| Overall GRADE‐CERQual assessment and explanation | |
| Low confidence | Finding downgraded because of serious concerns about relevance (partial relevance), moderate concerns about coherence (contradictory data) and adequacy, and minor concerns about methodological limitations |
| Contributing studies | |
| Brownlie 2005; Poltorak 2005; Casiday 2007; Ward 2017 | |
| Finding 11: agendas and interests underpinning the expert systems implicated with vaccination. For some parents, distrust of the institutions or systems implicated with vaccination was linked to their concerns about the agendas or interests embedded in these systems. Many of these parents were particularly concerned about the economic interests of these systems, and especially the economic interests of the pharmaceutical industry, which they perceived to be negatively influencing vaccination programmes. | |
| Assessment for each GRADE‐CERQual component | |
| Methodological limitations | Minor concerns due to poor reporting of data analysis methods, and limited evidence of reflexivity and sensitivity to ethical concerns in many of the studies |
| Coherence | No or very minor concerns (the finding reflects the variation and complexity of the data, and is well supported by details in the underlying studies) |
| Relevance | Moderate concerns because 9 studies were conducted in HICs (partial relevance); 3 studies focused only on MMR vaccination (partial relevance); and 4 studies only included parents who were hesitant towards or nonaccepting of vaccination (partial relevance) |
| Adequacy | No or very minor concerns (11 studies contributing a large amount of rich data) |
| Overall GRADE‐CERQual assessment and explanation | |
| Moderate confidence | Finding downgraded because of moderate concerns about relevance (partial relevance) and minor concerns about methodological limitations |
| Contributing studies | |
| Rogers 1995; Petts 2004; Poltorak 2005; Casiday 2007; Varghese 2013; Dube 2016; Giles‐Vernick 2016; Reich 2016; Ward 2017; Carrion 2018; Peretti‐Watel 2019 | |
| Finding 12: current and past controversies. Some parents' distrust of the institutions or systems implicated with vaccination was linked to particular ‘scandals’ or ‘controversies’ related to vaccination specifically or health‐related issues more broadly. The occurrence of such scandals, and the manner in which they were perceived to have been handled, caused some parents to feel misled by authorities and to question their legitimacy in protecting the public’s health. | |
| Assessment for each GRADE‐CERQual component | |
| Methodological limitations | Minor concerns due to poor reporting of data analysis and limited evidence of sensitivity to ethical concerns in many of the studies |
| Coherence | Serious concerns because there were some contradictory data that did not fit the interpretation of this finding (one study found that various well‐known ‘controversies’ did not affect parents’ trust in authorities and did not have an associated influence on their vaccination acceptance)(contradictory data), and for some aspects of the finding, it was hard to tell the level of support from the underlying data because the issue (e.g. the handling of the controversy) was mentioned in passing and not explored in detail by many of the studies (ambiguous data) |
| Relevance | Serious concerns because all studies focused on a specific vaccine: 4 studies focused only on MMR vaccination, and 2 studies focused only on polio vaccination (partial relevance) |
| Adequacy | No or very minor concerns (6 studies contributing a large amount of rich data) |
| Overall GRADE‐CERQual assessment and explanation | |
| Low confidence | Finding downgraded because of serious concerns about relevance (partial relevance) and coherence (contradictory and ambiguous data), and minor concerns about methodological limitations (partial relevance). |
| Contributing studies | |
| Petts 2004; Brownlie 2005; Poltorak 2005; Casiday 2007; Renne 2010; Hussain 2015 | |
| Finding 13: marginalisation, inadequate public services, and priority misalignment. Some parents' distrust in the institutions or systems implicated with vaccination was linked to their experiences of marginalisation, inadequate public services, or misalignment between their own priorities and those of the state. These experiences undermined trustful and benevolent state‐citizen relations, leading many parents to distrust government and government‐sponsored programs, including vaccination. | |
| Assessment for each GRADE‐CERQual component | |
| Methodological limitations | Minor concerns due to poor reporting of sampling and limited evidence of sensitivity to ethical concerns in many of the studies |
| Coherence | Minor concerns due to some contradictory data (some data showed how experiences of social exclusion, inadequate public services, and priority misalignment did not undermine state‐citizen relations) |
| Relevance | Serious concerns because 3 studies were conducted in LMICs (partial relevance); and all studies focused on a specific vaccine: 1 study focused only on MMR vaccination (partial relevance) and 3 studies focused only on polio vaccination (partial relevance) |
| Adequacy | No or very minor concerns (4 studies contributing a large amount of rich data) |
| Overall GRADE‐CERQual assessment and explanation | |
| Moderate confidence | Finding downgraded because of serious concerns about relevance (partial relevance), and minor concerns about coherence (contradictory data) and methodological limitations |
| Contributing studies | |
| Chaturvedi 2009; Renne 2010; Hussain 2015; Smith 2017 | |
| Finding 14: socio‐economic challenges in accessing vaccination services. Parents living in resource‐limited settings frequently face numerous socioeconomic challenges to accessing vaccination services, including practical questions of geography and transport, childcare constraints, and family economics and household work pressures. As a result of these challenges, some of these parents were less accepting of vaccination due to the time, effort, and opportunity costs that accessing vaccination involved. | |
| Assessment for each GRADE‐CERQual component | |
| Methodological limitations | Minor concerns due to poor reporting of data analysis methods, and limited evidence of reflexivity and sensitivity to ethical concerns in most studies |
| Coherence | No or minor concerns (the finding reflects the variation and complexity of the data, and is well supported by details in the underlying studies) |
| Relevance | Minor concerns because 5 of the 6 studies were conducted in Africa, yet 1 study was conducted in Britain |
| Adequacy | No or very minor concerns (6 studies contributing a large amount of data) |
| Overall GRADE‐CERQual assessment and explanation | |
| High confidence | |
| Contributing studies | |
| Millimouno 2006; Leach 2007; Dugas 2009; McKnight 2014; Giles‐Vernick 2016; Smith 2017 | |
| Finding 15: undesirable features of vaccination services and delivery logistics. Some parents were less accepting of vaccination due to undesirable features of vaccination services and delivery logistics. These features, common to vaccination services within resource‐limited settings, included resource constraints that affect vaccine supply and costs and health facility waiting times, and constraining organisational procedures. | |
| Assessment for each GRADE‐CERQual component | |
| Methodological limitations | Minor concerns due to poor reporting of data analysis methods, and limited evidence of reflexivity and sensitivity to ethical concerns in most studies |
| Coherence | No or minor concerns (the finding reflects the variation and complexity of the data, and is well supported by details in the underlying studies) |
| Relevance | Moderate concerns because all studies were conducted in Africa |
| Adequacy | No or very minor concerns (5 studies contributing a large amount of data) |
| Overall GRADE‐CERQual assessment and explanation | |
| Moderate confidence | Finding downgraded because of moderate concerns about relevance (partial relevance) and minor concerns about methodological limitations |
| Contributing studies | |
| Millimouno 2006; Leach 2007; Dugas 2009; McKnight 2014; Giles‐Vernick 2016 | |
| Finding 16: vaccination as a social event.Vaccination may be a social event where people gather and interact with each other. Some parents found this to a positive experience, whereby they received affirmation about themselves and their children. This potentially motivated attendance of childhood vaccination services. For other parents, the social nature of vaccination services was a negative experience, whereby they felt judged, disapproved of, or alienated from others. This potentially demotivated attendance of childhood vaccination services. | |
| Assessment for each GRADE‐CERQual component | |
| Methodological limitations | Minor concerns due to poor reporting of sampling and data analysis in both studies, as well as limited evidence of reflexivity in both studies |
| Coherence | No or minor concerns (the finding reflects the variation and complexity of the data, and is well supported by details in the underlying studies) |
| Relevance | Serious concerns because both studies were conducted in LMICs in Africa (partial relevance) |
| Adequacy | Serious concerns because only 2 studies contributed to the review finding, both with relatively limited data contributing to this finding |
| Overall GRADE‐CERQual assessment and explanation | |
| Low confidence | Finding downgraded because of serious concerns about relevance (partial relevance) and adequacy, and minor concerns about methodological limitations |
| Contributing studies | |
| Millimouno 2006; Leach 2007 | |
| Finding 17: interactions with frontline healthcare workers. Parents' vaccination views and practices, across diverse settings, contexts, and population groups, were mediated by the face‐to‐face interactions or personal relations they have with frontline healthcare workers. Some parents were less accepting of vaccination due to mistreatment from healthcare workers, and when they felt the vaccination information provided to them was simplistic and unbalanced. In contrast, some parents were more accepting of vaccination due to positively‐received engagements with healthcare workers, whereby they felt supported, listened to, and respected and whereby healthcare workers shared balanced information and personal stories about themselves as parents. | |
| Assessment for each GRADE‐CERQual component | |
| Methodological limitations | Minor concerns due to poor reporting of sampling and data analysis in most studies, as well as limited evidence of sensitivity to ethical concerns or reflexivity in many studies |
| Coherence | Minor concerns because there were insufficient data to support some aspects of the review finding (e.g. the sharing of balanced information and personal stories) (ambiguous data) |
| Relevance | No or very minor concerns (studies include a wide range of participants, countries, settings, and vaccines) |
| Adequacy | No or very minor concerns (16 studies contributing a large amount of rich data) |
| Overall GRADE‐CERQual assessment and explanation | |
| High confidence | |
| Contributing studies | |
| Brownlie 2005; Poltorak 2005; Millimouno 2006; Casiday 2007; Leach 2007; Dugas 2009; McKnight 2014; Hussain 2015; Dube 2016; Giles‐Vernick 2016; Reich 2016; Sobo 2016; Smith 2017; Ward 2017; Peretti‐Watel 2019; Limaye 2020 | |
| Finding 18: neoliberal logic. Many parents, predominantly from HICs, held a worldview informed by neoliberal discourses. These discourses understand health as individualised, and health‐related risks and decisions as matters of individual choice and responsibility. Furthermore, these discourses suggest that being a ‘good’ and responsible person in the world means consistently assessing one’s own, individual health‐related risks, seeking and questioning evidence about such risks, proactively avoiding and managing such risks, and understanding that one is singularly accountable for the outcomes that ensue. Some parents experienced this worldview as in conflict with vaccination promotion messages, which tend to be informed by other types of discourses. The discourses underpinning vaccination promotion messages frequently emphasise generalised risk and safety statistics, claim that ‘doctor knows best’, ask people to trust authorities and follow what they promote, and advocate for social responsibility and the health of the community. Parents’ perceived tension between the discourses informing their own worldview and those of vaccination promotion messages led some to resist these messages and be less accepting of vaccination. | |
| Assessment for each GRADE‐CERQual component | |
| Methodological limitations | Minor concerns due to limited evidence of sensitivity to ethical concerns or reflexivity in many of the studies |
| Coherence | Moderate concerns: for some aspects of the finding, there was less support from the underlying data (e.g. proactively avoiding and managing risks), or it was hard to tell the level of support from the underlying data because the issue (e.g. parents’ experienced conflict) was mentioned in passing and not explored in detail by many of the studies (ambiguous data). However, the theory of neoliberalism is well established and its various components and tensions well‐mapped out in existing literature. This therefore slightly increased our confidence. We also explored alternative explanations and found that the data supports various alternative theoretical interpretations (e.g. psychological theories on risk beliefs and appraisal and utility calculation). However, we did not identify any theory that contradicted or refuted our interpretation: all plausible alternatives we explored complemented our interpretation, albeit providing a different perspective or paradigm in which to interpret the findings. We therefore did not judge these plausible (compatible) alternatives to pose a serious threat to coherence. However, and in sum, this is a conceptually transformed finding that has moved somewhat away from the underlying data and the primary focus of the studies, and various inferences have been made. We therefore do have moderate concerns regarding its coherence. |
| Relevance | No or very minor concerns (studies include a wide range of participants, settings, and vaccines within HICs) |
| Adequacy | No or very minor concerns (15 studies, together contributing a large amount of rich data) |
| Overall GRADE‐CERQual assessment and explanation | |
| Moderate confidence | Finding downgraded because of moderate concerns about coherence (ambiguous data) and minor concerns about methdological limitations |
| Contributing studies | |
| Rogers 1995; Petts 2004; Brownlie 2005; Poltorak 2005; Casiday 2007; Brunson 2013; Johnson 2014; Dube 2016; Reich 2016; Sobo 2016; Barbieri 2017; Smith 2017; Ward 2017; Carrion 2018; Peretti‐Watel 2019 | |
| Finding 19: social exclusion. Some parents, predominantly from LMICs, were less accepting of childhood vaccination due to their experiences of social exclusion. Social exclusion may involve economic disadvantage, residential segregation, a lack of political representation or power, discrimination and unequal protection of rights, and a myriad of socioeconomic barriers to good quality public services, including vaccination. Social exclusion weakened trustful government‐citizen relations, generated feelings of alienation from, and resentment towards, the state and others and gave rise to frustration and demotivation in the face of structural challenges. These factors in turn led some parents who are socially excluded to distrust vaccination, to refuse vaccination as a form of resistance or a mechanism to bring about change, or to avoid vaccination due to the time, effort, (opportunity) costs and distress it creates. | |
| Assessment for each GRADE‐CERQual component | |
| Methodological limitations | Minor concerns due to poor reporting on sampling and data analysis methods, as well as limited evidence of sensitivity to ethical concerns or reflexivity in many of the studies |
| Coherence | Moderate concerns: for some aspects of the finding, it was hard to tell the level of support from the underlying data because the issue (e.g. the specific mechanisms of effect of social exclusion) was mentioned in passing and not explored in detail by many of the studies (ambiguous data). We also explored alternative explanations and found that the data supports various alternative theoretical interpretations (e.g. management theories of “exit” and “voice”; psychological theories of self‐efficacy; sociological theories of structural violence; social theories of trust) (plausible alternatives). However, we did not identify any theory that contradicted or refuted our interpretation; all plausible alternatives explored complemented our interpretation, albeit provided a different perspective or paradigm in which to interpret the findings. We therefore did not judge these plausible (compatible) alternatives to pose a serious threat to coherence. However, and in sum, this is a conceptually transformed finding that has moved somewhat away from the underlying data and the primary focus of the studies, and various inferences have been made. We therefore do have moderate concerns regarding its coherence. |
| Relevance | Moderate concerns because 6 (of the 9) studies were conducted in Africa (partial relevance), and 4 studies focused on specific vaccines:3 on polio and 1 on MMR vaccination (partial relevance) |
| Adequacy | No or very minor concerns (9 studies, together contributing a large amount of rich data) |
| Overall GRADE‐CERQual assessment and explanation | |
| Moderate confidence | Finding downgraded because of moderate concerns about both relevance (partial relevance) and coherence (ambiguous data) |
| Contributing studies | |
| Millimouno 2006; Leach 2007; Chaturvedi 2009; Dugas 2009; Renne 2010; McKnight 2014; Hussain 2015; Giles‐Vernick 2016; Smith 2017 | |
Footnotes
MMR: measles, mumps, and rubella; SES: socioeconomic status
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Abakar 2018.
| Study characteristics | ||
| WHO region | Africa | |
| Country classification by income level | LMIC | |
| Study aim | Understand the factors that caregivers consider, explicitly or implicitly, when deciding whether or not to vaccinate their child | |
| Study setting | Chad; primary caregivers (mothers with at least one child under 5 years old), within rural, mobile pastoralist communities | |
| Notes | ||
Aharon 2017.
| Study characteristics | ||
| WHO region | Europe | |
| Country classification by income level | HIC | |
| Study aim | To identify the main reasons why parents decided not to vaccinate their children according to the official recommendations | |
| Study setting | Israel; parents residing in the second largest urban city in Israel who refused to vaccinate their children and who had at least one 2‐year‐old child | |
| Notes | ||
Ames 2017a.
| Study characteristics | ||
| WHO region | Africa | |
| Country classification by income level | LMIC | |
| Study aim | Explore stakeholders' views, experiences, and preferences for childhood vaccination communication | |
| Study setting | Cameroon; parents with children aged 12 months or younger attending health clinics for a vaccination session in urban and rural areas of the Central and North‐West regions of Cameroon | |
| Notes | ||
Attwell 2019.
| Study characteristics | ||
| WHO region | Western Pacific | |
| Country classification by income level | HIC | |
| Study aim | 1) Evaluate the ‘I Immunise’ campaign; 2) explore how selective vaccinators understand themselves in relation to ‘the system’ that sought their vaccination, and how ‘the system’ might respond to the parents’ concerns | |
| Study setting | Parents self‐identifying as living an alternative lifestyle, having a child aged five or under, and either having refused a vaccine in the past, or keeping quiet socially about being fully vaccinated. All parents lived in Fremantle and were part of the ‘I Immunise’ campaign, a pro‐immunisation social marketing campaign conducted as part of the Immunisation Alliance of Western Australia (IAWA), a not‐for‐profit health promotion charity dedicated to advocating the importance of vaccination. | |
| Notes | ||
Austin 2001.
| Study characteristics | ||
| WHO region | Europe | |
| Country classification by income level | HIC | |
| Study aim | Understand parents’ experiences of deciding to have their child immunised or not | |
| Study setting | UK; parents of children aged between 7 and 9 months, and aged 18 months, who had recently been immunised and were routinely seen in developmental clinics | |
| Notes | ||
Austvoll‐Dahlgren 2010.
| Study characteristics | ||
| WHO region | Europe | |
| Country classification by income level | HIC | |
| Study aim | Identify parents’ decision‐making processes in relation to childhood vaccinations, including barriers and facilitators to searching for information. | |
| Study setting | Norway; parents attending counselling at one of three maternal and child health centres in a major Norwegian city who had made a decision about childhood vaccinations within the previous 3 months | |
| Notes | ||
Babirye 2011.
| Study characteristics | ||
| WHO region | Africa | |
| Country classification by income level | LMIC | |
| Study aim | Understand influences on immunisation behaviour using the attitude‐social influence‐self efficacy model | |
| Study setting | Uganda; mothers and fathers with children younger than five years residing in the Nakawa and Makindye divisions of Kampala | |
| Notes | ||
Barbieri 2017.
| Study characteristics | ||
| WHO region | America | |
| Country classification by income level | LMIC | |
| Study aim | Explore parents’ experiences in the process of choosing whether to vaccinate their children (or not), the influences permeating such decisions, and the feelings associated with these experiences. | |
| Study setting | Brazil; couples (n = 15) both with at least a university degree and belonging to the upper‐ and upper‐middle classes and living in the city of São Paulo | |
| Notes | Data describing this study were also collected from Barbieri 2015 | |
Benin 2006.
| Study characteristics | ||
| WHO region | America | |
| Country classification by income level | HIC | |
| Study aim | Investigate decision‐making about vaccinations for infants | |
| Study setting | USA; mothers 1 to 3 days postpartum and again at 3 to 6 months. All mothers were English‐speaking who delivered at the Yale‐New Haven Hospital (New Haven, Connecticut) or who delivered at home in the care of 1 of 2 midwifery practices in Connecticut | |
| Notes | ||
Berhanel 2000.
| Study characteristics | ||
| WHO region | Africa | |
| Country classification by income level | LMIC | |
| Study aim | Identify the socio‐cultural and service‐related factors that affect acceptance and coverage of immunisation services in Ethiopia | |
| Study setting | Ethiopia; mothers of children under the age of five years living in the Southern Nations and Nationalities People’s Region (SNNPR) | |
| Notes | ||
Berry 2018.
| Study characteristics | ||
| WHO region | Western Pacific | |
| Country classification by income level | HIC | |
| Study aim | Explore parents’ communication needs to inform the development of a clinical communication support intervention | |
| Study setting | Australia; parents of at least one child under five years old or expecting a first child, from two major cities (Sydney and Melbourne) or a rural town north of Sydney (Lismore). Within these areas, higher prevalence of under‐vaccination is recorded. All parents had at least some questions about routine childhood vaccinations. | |
| Notes | ||
Biezen 2018.
| Study characteristics | ||
| WHO region | Western Pacific | |
| Country classification by income level | HIC | |
| Study aim | Understand the views, attitudes, and practices of parents on their knowledge and acceptance of influenza vaccination in children under five years old. | |
| Study setting | Australia; parents from Melbourne | |
| Notes | ||
Bisht 2000.
| Study characteristics | ||
| WHO region | South‐East Asia | |
| Country classification by income level | LMIC | |
| Study aim | Understand community perceptions of protection, prevention, and immunity in the specific context of measles, and child health in general. | |
| Study setting | India; mothers with children between the ages of 0 to 2 years from four selected districts in diverse parts of Inda: Pauri Garhwal and Kanpur Dehat in Uttar Pradesh, Surat in Gujarat, and Thiruvananthapuram in Kerala | |
| Notes | ||
Bond 1998.
| Study characteristics | ||
| WHO region | Western Pacific | |
| Country classification by income level | HIC | |
| Study aim | Explore the similarities and differences between complete immunisers, incomplete immunisers, and non‐immunisers in terms of their perceptions of risk and susceptibility to disease and risks of immunisation. | |
| Study setting | Australia; first time and experienced mothers of infants who were completely immunised (for age), incompletely immunised (behind the recommended immunisation schedule), partially immunised (parents chose or advised not to have a specific immunisation) or had had no immunisations, identified by maternal and child health nurses in five Melbourne metropolitan councils (Banyule, Darebin, Hume, Moreland, Yarra). | |
| Notes | ||
Braka 2012.
| Study characteristics | ||
| WHO region | Africa | |
| Country classification by income level | LMIC | |
| Study aim | Identify community sources of information on immunisation, vaccine safety, and adverse events following immunisation; determine caretakers’ knowledge of immunisation; identify community concerns or fears about immunisation and adverse events following immunisation and their influence on caretakers’ decisions to vaccinate | |
| Study setting | Uganda; caretakers, with children aged 5 years or younger, who were very or somewhat concerned about vaccine safety in two districts ‐ Kampala and Mbarara (1 urban and 1 rural) | |
| Notes | ||
Brown 2012.
| Study characteristics | ||
| WHO region | Europe | |
| Country classification by income level | HIC | |
| Study aim | Obtain a picture of factors underlying parents’ decision‐making about the first dose of MMR (MMR1) | |
| Study setting | UK; mothers planning to accept, postpone, or decline the first MMR dose (MMR1) for their 11‐ to 36‐month‐old children registered with NHS Ealing. | |
| Notes | ||
Brownlie 2005.
| Study characteristics | ||
| WHO region | Europe | |
| Country classification by income level | HIC | |
| Study aim | Explore parental attitudes towards MMR and immunisation generally from a sociological perspective | |
| Study setting | UK; secondary analysis of two qualitative data sets on parental views of the MMR vaccination carried out for the Health Education Board for Scotland in 1999 and 2001 in the context of growing concern about the impact on immunisation take‐up rates following the publication of a report in The Lancet that highlighted a putative link between MMR, autism, and inflammatory bowel disease. The 1999 study included parents stratified by deprivation category (DEPCAT) and by whether they were at a pre‐ or post‐MMR invitation stage; the 2001 study included parents from 3 health board areas, different socioeconomic areas, with varying degrees of concern about immunisation and who had children aged between 2 and 6 months, or 7 and 18 months. | |
| Notes | Data describing this study were also collected from Brownlie 2011. | |
Brunson 2013.
| Study characteristics | ||
| WHO region | America | |
| Country classification by income level | HIC | |
| Study aim | Develop an understanding of the general process parents go through when making decisions about their children’s vaccinations | |
| Study setting | USA; USA‐born parents living in King County, Washington who had children ≤ 18 months of age; 20 mothers and 5 couples. Purposeful sample of parents who made all types of vaccination decisions and who were also diverse in terms of age, education, and income | |
| Notes | Data describing this study were also collected from Brunson 2015 and Brunson 2017. | |
Burghouts 2017.
| Study characteristics | ||
| WHO region | America | |
| Country classification by income level | LMIC | |
| Study aim | Gain insight into reasons for vaccine acceptance or rejection among Warao Amerindians in Venezuela | |
| Study setting | Venezuela; vaccine‐accepting and vaccine‐declining primary caregivers of children aged between 6 weeks and 6 months residing in Orinoco Delta (a rural watery area) in Northeastern Venezuela. | |
| Notes | ||
Bystrom 2014.
| Study characteristics | ||
| WHO region | Europe | |
| Country classification by income level | HIC | |
| Study aim | Explore facilitators and barriers to MMR vaccination among parents living in anthroposophic communities | |
| Study setting | Sweden; parents living in an anthroposophic community near Stockholm | |
| Notes | ||
Carrion 2018.
| Study characteristics | ||
| WHO region | America | |
| Country classification by income level | HIC | |
| Study aim | Explore the sense‐making context in which mothers describe being motivated to think about and ultimately make decisions about vaccine refusal | |
| Study setting | USA; mothers who had given birth or adopted within the last two years and who had refused one or more recommended vaccines. Included mothers from the Eastern Time Zone of the United States, the Central Time Zone, the Pacific Time Zone (including Arizona), and the Mountain Time Zone | |
| Notes | Data describing this study were also collected from Carrion 2018b. | |
Casiday 2007.
| Study characteristics | ||
| WHO region | Europe | |
| Country classification by income level | HIC | |
| Study aim | Explore risk conceptualisation, trust, and decision‐making in the case of MMR vaccination | |
| Study setting | UK; 87 parents of young children (77 mothers and 10 fathers), in and around Cambridge and Durham. Participants were purposively selected to include a broad range of educational qualifications, socioeconomic backgrounds, and immunisation decisions. | |
| Notes | Data describing this study were also collected from Casiday 2005 and Casiday 2006. | |
Castroviejo 2019.
| Study characteristics | ||
| WHO region | Europe | |
| Country classification by income level | HIC | |
| Study aim | Explore reasons for childhood vaccination hesitancy or refusal | |
| Study setting | Belgium; parents having at least one child under 6 years old, and attending nurseries or pre‐schools (in both low‐ and high‐income settings) in Brussels | |
| Notes | ||
Chantler 2006.
| Study characteristics | ||
| WHO region | Europe | |
| Country classification by income level | HIC | |
| Study aim | Explore parents' understanding of pneumococcal disease and their views of the introduction of this vaccine | |
| Study setting | UK; parents with children under 2 years of age recruited from six surgeries representing geographically and socioeconomically diverse areas of Oxfordshire | |
| Notes | ||
Chaturvedi 2009.
| Study characteristics | ||
| WHO region | South‐East Asia | |
| Country classification by income level | LMIC | |
| Study aim | Gain an insight into the phenomenon of social resistance/reluctance and rumours against pulse polio campaign | |
| Study setting | India; parents with children under five years of age, including Muslims and Hindus from rural and urban areas in two highly polio endemic districts of western Uttar Pradesh (North India): Moradabad and JP Nagar | |
| Notes | ||
Closser 2016.
| Study characteristics | ||
| WHO region | Africa, South‐East Asia, and Eastern Mediterranean | |
| Country classification by income level | LMIC | |
| Study aim | Assess the impact of the Global Polio Eradication Initiative (GPEI) on local health systems, including its impact on polio vaccine acceptance and refusal | |
| Study setting | Ethnographic case studies, including with community members, ground‐level staff, and district and national leadership; and participant observation of polio eradication activities in seven diverse contexts: Rautahat, Nepal; Purba Champaran, Bihar, India; Nizamabad, Andhra Pradesh, India; Karachi, Pakistan; South Omo, SNNP, Ethiopia; Kumbotso LGA, Kano, Nigeria; Rubavu, Rwanda; Camucuio, Namibe, Angola | |
| Notes | ||
Cockcroft 2014.
| Study characteristics | ||
| WHO region | Africa | |
| Country classification by income level | LMIC | |
| Study aim | Examine factors related to measles vaccination and parental reasons for non‐vaccination | |
| Study setting | Nigeria; mothers or caregivers of children aged less than four years old residining in Cross River or Bauchi states of Nigeria | |
| Notes | ||
Condon 2002.
| Study characteristics | ||
| WHO region | Europe | |
| Country classification by income level | HIC | |
| Study aim | Explore the attitudes of ethnic minority parents to preschool immunisations, particularly first MMR (measles, mumps, and rubella) vaccination | |
| Study setting | UK; Pakistani, Somali, and Afro‐Caribbean mothers of infants aged 16 months to 3 years living in Bristol | |
| Notes | ||
Coreil 1994.
| Study characteristics | ||
| WHO region | America | |
| Country classification by income level | LMIC | |
| Study aim | Explore maternal perceptions of the barriers and incentives to immunisation | |
| Study setting | Haiti; mothers of children 12 to 23 months of age enrolled in a community health program in the town of Mirebalais in the Central Highlands | |
| Notes | ||
Cotter 2003.
| Study characteristics | ||
| WHO region | Europe | |
| Country classification by income level | HIC | |
| Study aim | Determine the knowledge, attitudes, and practices of parents and health professionals to early childhood vaccines | |
| Study setting | Ireland; mothers from 'mother and toddler' groups and hospitals providing obstetric services in Cork and Kerry | |
| Notes | ||
Cuesta 2020.
| Study characteristics | ||
| WHO region | Africa | |
| Country classification by income level | LMIC | |
| Study aim | Understand the reasons for recurrent measles outbreaks | |
| Study setting | Republic of Guinea; caregivers whose children were of target age for the measles mass vaccination campaigns (MVCs) in April 2017 in two communes of Conakry (Matoto and Matam). Communes were selected for their differences in urbanisation levels and for being the most affected by the previous two measles epidemics. | |
| Notes | ||
Cullen 2005.
| Study characteristics | ||
| WHO region | Europe | |
| Country classification by income level | HIC | |
| Study aim | Explore the experience of five parents from different families who had chosen not to have their children vaccinated against childhood diseases. | |
| Study setting | UK; parents of children who had not received any vaccinations by the age of four years attending GPs in Portsmouth, Hampshire | |
| Notes | ||
Cutts 1990.
| Study characteristics | ||
| WHO region | Africa | |
| Country classification by income level | LMIC | |
| Study aim | Evaluate the immunisation system in Conakry, Guinea | |
| Study setting | Guinea; parents from 12 dispersed neighbourhoods in the town of Conakry, Guinea | |
| Notes | ||
Delkhosh 2014.
| Study characteristics | ||
| WHO region | Eastern Mediterranean | |
| Country classification by income level | LMIC | |
| Study aim | Determine the immunisation concerns of mothers | |
| Study setting | Iran; mothers who had at least one 0‐ to 24‐month‐old child and who were referred to the vaccination section of health centers affiliated with Tehran University of Medical Sciences (Tehran, Iran) in south Tehran for their child’s vaccination. | |
| Notes | ||
deRose 2018.
| Study characteristics | ||
| WHO region | America | |
| Country classification by income level | HIC | |
| Study aim | Explore the issues Latino immigrants experience when vaccinating their children in the health care system in the USA | |
| Study setting | USA; Latino immigrants who had sought immunisations for their foreign‐born children during their first five years in the United States. Parents recruited from local clinics and churches that serve the Latino population in a Midwestern city in the USA. | |
| Notes | ||
Downs 2008.
| Study characteristics | ||
| WHO region | America | |
| Country classification by income level | HIC | |
| Study aim | Identify parents’ patterns of beliefs regarding vaccinations | |
| Study setting | USA; parents with a child between 18 and 23 months of age from three cities identified as providing diversity in race, background, and vaccination attitudes: Kansas City (Missouri), Philadelphia (Pennsylvania), and Eugene (Oregon). | |
| Notes | ||
Dube 2016.
| Study characteristics | ||
| WHO region | America | |
| Country classification by income level | HIC | |
| Study aim | Understand how and why mothers in Quebec (Canada) decide to have their newborn vaccinated or not, with a particular focus on vaccine‐hesitant mothers | |
| Study setting | Canada; 56 pregnant mothers living in different areas of Quebec | |
| Notes | ||
Dugas 2009.
| Study characteristics | ||
| WHO region | Africa | |
| Country classification by income level | LMIC | |
| Study aim | Understand, from an anthropological point of view, the logic behind the parental decision‐making process regarding the vaccination or non‐vaccination of children | |
| Study setting | Burkina Faso; mothers, fathers, grandmothers, or grandfathers from four ethnic groups (the Marka, Bwaba, Mossi, and Peulh) in the Health district of Nouna, North‐west of Burkina Faso | |
| Notes | ||
Eng 1991.
| Study characteristics | ||
| WHO region | Africa | |
| Country classification by income level | LMIC | |
| Study aim | Investigate the lack of acceptance of childhood immunisation | |
| Study setting | Togo; mothers or caretakers from nine different villages | |
| Notes | ||
Enkel 2018.
| Study characteristics | ||
| WHO region | Western Pacific | |
| Country classification by income level | HIC | |
| Study aim | Identify the behaviours, knowledge, and attitudes of ‘hesitant complier’ parents | |
| Study setting | Australia; vaccinating parents of children ( < 5 years) who were identified as being hesitant in Perth, Western Australia | |
| Notes | ||
Evans 2001.
| Study characteristics | ||
| WHO region | Europe | |
| Country classification by income level | HIC | |
| Study aim | Investigate what influences parents’ decisions on whether to accept or refuse the primary MMR immunisation and the impact of the Wakefield controversy over its safety | |
| Study setting | UK; parents, whose youngest child was between 14 months and 3 years old from six localities in Avon and Gloucestershire. Parents comprised those who had accepted MMR for their youngest child (‘immunisers’) and those who had refused MMR (‘non‐immunisers’). | |
| Notes | ||
Evers 2000.
| Study characteristics | ||
| WHO region | America | |
| Country classification by income level | HIC | |
| Study aim | Gain insight into parents’ knowledge and attitudes regarding childhood immunisation | |
| Study setting | USA; African‐American mothers and grandmothers of children who had received or needed to receive immunisation and who were attending a paediatric clinic in Louisiana, New Orleans | |
| Notes | ||
Fadda 2015.
| Study characteristics | ||
| WHO region | Europe | |
| Country classification by income level | HIC | |
| Study aim | Understand what drives parents’ vaccination decision‐making for their children, giving special attention to vaccination literacy and psychological empowerment in such a context | |
| Study setting | Switzerland; mothers or fathers of children less than one year old living in Canton of Ticino (Italian‐speaking Switzerland) | |
| Notes | ||
Fadda 2016.
| Study characteristics | ||
| WHO region | Europe | |
| Country classification by income level | HIC | |
| Study aim | Gain insights from parents residing in a low measles, mumps, rubella (MMR) uptake area on what constitutes feelings of empowerment in the decision they have to make on their child’s MMR vaccination. | |
| Study setting | Italy; mothers and fathers of children for whom the MMR vaccination decision was still pending. Recruited during their vaccination appointment for the first or second dose of the diphtheria, tetanus, and pertussis (DTaP) vaccination at vaccination centres and hospitals in the Province of Trento, Italy (diphtheria and tetanus vaccinations are mandatory in Italy) |
|
| Notes | ||
Figueiredo 2011.
| Study characteristics | ||
| WHO region | America | |
| Country classification by income level | LMIC | |
| Study aim | Describe the experience of families in the immunisation of children under two years | |
| Study setting | Brazil; families having a child under two years old living in the coverage area of the selected health units which have a large number of children who access medical care and a high demand for vaccination. Families comprised a mother or caregiver who stayed at home with the child most of the time. | |
| Notes | ||
Fleming 2019.
| Study characteristics | ||
| WHO region | Africa | |
| Country classification by income level | LMIC | |
| Study aim | Document community perceptions of maternal immunisation, using tetanus vaccine as an example, and identify factors perceived to be important to successfully introducing other maternal vaccines, such as influenza vaccine | |
| Study setting | Malawi; pregnant and recently pregnant women and their family members from one district in each of the three regions of Malawi: Rumphi (Northern Region), Dowa (Central Region), and Zomba (Southern Region). Chosen districts represented a mix of rural, peri‐urban, and urban populations. | |
| Notes | ||
Fowler 2007.
| Study characteristics | ||
| WHO region | Europe | |
| Country classification by income level | LMIC | |
| Study aim | Identify concerns about immunisations and strategies to address these concerns | |
| Study setting | Kazakhstan and Uzbekistan (two Central Asian countries in economic transition); mothers and grandmothers who make healthcare decisions for one or more children aged 0 to 6 years from four regions in each country (two urban and two rural oblasts from Kazakhstan and one urban and three rural oblasts from Uzbekistan) | |
| Notes | ||
Fredrickson 2004.
| Study characteristics | ||
| WHO region | America | |
| Country classification by income level | HIC | |
| Study aim | Estimate the frequency of and reasons for immunisation refusal | |
| Study setting | USA; parents of young children of immunisation age from six cities (Albuquerque, New Mexico; Cleveland, Ohio; Shreveport, Louisiana; Rochester, New York; Santa Fe, New Mexico; and Wichita, Kansas). Cities were chosen for their geographic representation, and ethnic and socioeconomic diversity. | |
| Notes | ||
Gardner 2010a.
| Study characteristics | ||
| WHO region | Europe | |
| Country classification by income level | HIC | |
| Study aim | Extract underlying beliefs towards measles, mumps, and rubella (MMR) vaccination from UK parents’ views towards potential motivational and organisational interventions to boost MMR vaccination | |
| Study setting | UK; London‐based parents from parent‐and‐toddler groups based in five different Primary Care Trust areas, each of which at the time of the study reported MMR uptake levels below the 95% rate required for herd immunity and the 2007/08 UK average: Greenwich; Westminster; Sutton and Merton; Brent; and Camden. Majority of parents were white and educated to degree level or above. | |
| Notes | ||
Geelen 2016.
| Study characteristics | ||
| WHO region | Europe | |
| Country classification by income level | HIC | |
| Study aim | Explore parental vaccination practices and relationships between professionals and parents | |
| Study setting | Netherlands; parents with divergent socioeconomic backgrounds and age groups, one or more children, and different views on vaccination recruited from and observed at different child welfare centres. | |
| Notes | ||
George 2016.
| Study characteristics | ||
| WHO region | South‐East Asia | |
| Country classification by income level | LMIC | |
| Study aim | Explore factors that influence the decision of parents as well as pediatricians on whether their children should be vaccinated with a particular vaccine | |
| Study setting | India; parents of children who were eligible for rotavirus vaccination across eight Indian cities | |
| Notes | ||
Giles‐Vernick 2016.
| Study characteristics | ||
| WHO region | Africa | |
| Country classification by income level | LMIC | |
| Study aim | Explore different kinds of incertitude (ambiguity, uncertainty, ignorance) about infancy, hepatitis B vaccine (HBV), health protection, and vaccination | |
| Study setting | Central African Republic and Burkina Faso; parents of children between 12 and 59 months from Bangui, Central African Republic (CAR) and the Cascades region of southwestern Burkina Faso | |
| Notes | ||
Glanz 2013.
| Study characteristics | ||
| WHO region | America | |
| Country classification by income level | HIC | |
| Study aim | Describe parental vaccine decision‐making behaviors and characterise trust in physician advice among parents with varying childhood vaccination behaviors | |
| Study setting | USA; vaccine‐hesitant parents of children aged < 4 years who were members of Kaiser Permanente Colorado health plan | |
| Notes | ||
Gorman 2019.
| Study characteristics | ||
| WHO region | Europe | |
| Country classification by income level | HIC | |
| Study aim | Explore Polish migrant mothers' views on the childhood vaccination programme with a specific focus on influenza and human papillomavirus (HPV) vaccination | |
| Study setting | Scotland; Polish parents and grandparents who were regular attenders of a mother and toddlers’ group in Edinburgh | |
| Notes | ||
Guillaume 2004.
| Study characteristics | ||
| WHO region | Europe | |
| Country classification by income level | HIC | |
| Study aim | Examine the measles, mumps, and rubella (MMR) vaccination scare, its impact on parents of young children, and its effect on their need for information | |
| Study setting | UK; parents of children under the age of five attending community‐based childcare organisations (nursery schools and toddler groups) in Sheffield | |
| Notes | ||
Gullion 2008.
| Study characteristics | ||
| WHO region | America | |
| Country classification by income level | HIC | |
| Study aim | Explore the attitudes and beliefs of parents who consciously choose not to vaccinate their children and the ways in which these parents process information on the pros and cons of vaccines | |
| Study setting | USA; parents in the North Texas area who consciously chose to forgo vaccination for their children | |
| Notes | ||
Gust 2008.
| Study characteristics | ||
| WHO region | America | |
| Country classification by income level | HIC | |
| Study aim | Obtain detailed information from 'Worried’ and ‘Fencesitter’ mothers about their attitudes and beliefs regarding vaccines and their interactions with their child’s main health care provider; solicit comments on draft educational materials that were developed specifically for the study | |
| Study setting | USA; mothers having at least one child < 6 years of age and who were identified as 'Worried’ and ‘Fencesitter’ regarding vaccination from 3 cities; Atlanta, Georgia; La Crosse, Wisconsin; and Los Angeles, California | |
| Notes | ||
Handy 2017.
| Study characteristics | ||
| WHO region | Africa, USA, Europe | |
| Country classification by income level | LMIC and HIC | |
| Study aim | Explore the knowledge and attitudes regarding vaccines and vaccine‐preventable diseases among caregivers and immunisation providers, and examine how access to information impacts reported vaccine acceptance | |
| Study setting | Botswana, Dominican Republic (DR), Greece; caregivers of children younger than five years. In Botswana and the DR, caregivers were recruited from clinics in low‐, middle‐, and high‐income neighborhoods across urban, peri‐urban, and rural communities with a range of sociodemographic characteristics and immunisation rates. In Greece, caregivers were recruited from kindergarten networks in communities of low‐, middle‐, and high‐income neighborhoods. | |
| Notes | ||
Harjaningrum 2013.
| Study characteristics | ||
| WHO region | South‐East Asia | |
| Country classification by income level | LMIC | |
| Study aim | Knowledge, perceptions, and attitudes of mothers and healthcare providers toward pneumococcal conjugate vaccine | |
| Study setting | Indonesia; mothers having at least one child aged 0 to 5 years old recruited from several health care facilities in Bandung, West Java | |
| Notes | ||
Harmsen 2012.
| Study characteristics | ||
| WHO region | Europe | |
| Country classification by income level | HIC | |
| Study aim | Gain insight into parents’ experience at an anthroposophical child welfare center (CWC), the factors that influence their vaccination decision‐making and their need for information | |
| Study setting | Netherlands; parents who visit an anthroposophical child welfare center | |
| Notes | ||
Harmsen 2013.
| Study characteristics | ||
| WHO region | Europe | |
| Country classification by income level | HIC | |
| Study aim | Explore the reasons for childhood vaccination refusal in order to design public information and interventions that will help parents make decisions that best serve their children and the wider community | |
| Study setting | Netherlands; Dutch parents with at least one child aged 0 to 4 years for whom they refused all or part of the vaccinations within the National Immunization Program identified from Praeventis, the vaccination database in the Netherlands | |
| Notes | ||
Harmsen 2015.
| Study characteristics | ||
| WHO region | Europe | |
| Country classification by income level | HIC | |
| Study aim | Explore factors that influence vaccination decision‐making among parents with different ethnic backgrounds | |
| Study setting | Netherlands; mothers of Moroccan, Turkish, and other ethnic backgrounds with at least one child aged 0 to 4 years, who had lived in the Netherlands for at least one year and was currently living in Utrecht | |
| Notes | ||
Harrington 1999.
| Study characteristics | ||
| WHO region | Europe | |
| Country classification by income level | HIC | |
| Study aim | Explore mothers' response to the addition of Haemophilus influenzae type b (Hib) vaccine to the primary schedule | |
| Study setting | Ireland; mothers of babies aged 1 to 2 years in Dublin | |
| Notes | Data describing this study were also collected from Harrington 2000 and Robson 2000 | |
Hatokova 2018.
| Study characteristics | ||
| WHO region | Europe | |
| Country classification by income level | HIC | |
| Study aim | Investigate the issues and heuristics that play a role in parental decision‐making on children’s vaccinations | |
| Study setting | Slovakia; mothers of children under the age of 5 from a range of income groups living in the capital Bratislava or a neighbouring municipality | |
| Notes | ||
Helman 2004.
| Study characteristics | ||
| WHO region | Africa | |
| Country classification by income level | LMIC | |
| Study aim | Examine perceptions of childhood illnesses, the role of immunisation in preventing them, and the reasons for the low uptake of immunisations in the area. | |
| Study setting | South Africa; caretakers of children aged under 5 years brought to a community health centre in Mhlakulo, a rural community in Transkei, Eastern Cape | |
| Notes | ||
Henderson 2008.
| Study characteristics | ||
| WHO region | Europe | |
| Country classification by income level | HIC | |
| Study aim | Assess reasons for low uptake of immunisation amongst orthodox Jewish families | |
| Study setting | UK; mothers with children aged between 2 and 3 years living in the orthodox Jewish community in North East London | |
| Notes | ||
Hilton 2006.
| Study characteristics | ||
| WHO region | Europe | |
| Country classification by income level | HIC | |
| Study aim | Explore parents’ understandings of the diseases included in the current UK Childhood Immunization Programme (CIP), and the role of first‐ and second‐hand experiences of these diseases in assessments of their severity | |
| Study setting | UK; parents of children aged 6 years and below from areas with high and low MMR uptake rates and from high‐ and low‐income areas in Scotland | |
| Notes | Data describing this study were also collected from Hilton 2007a and Hilton 2007b | |
Houseman 1997.
| Study characteristics | ||
| WHO region | America | |
| Country classification by income level | HIC | |
| Study aim | Understand mothers' views regarding immunisations and the barriers they face in getting their children immunised | |
| Study setting | USA; African‐American and white mothers of children who received immunisation services from the public or private sector in the city of Norfolk | |
| Notes | ||
Hussain 2015.
| Study characteristics | ||
| WHO region | South‐East Asia | |
| Country classification by income level | LMIC | |
| Study aim | Explore social factors associated with resistance to the polio eradication program during the summer months of 2009 | |
| Study setting | India; parents with vaccine‐eligible children who interacted with the polio eradication program in the City of Aligarh in Uttar Pradesh, India. Included mothers (n = 37) and fathers (n = 43) from a range of socioeconomic statuses | |
| Notes | Data describing this study were also collected from Hussain 2012 | |
Jackson 2017a.
| Study characteristics | ||
| WHO region | Europe | |
| Country classification by income level | HIC | |
| Study aim | Examine existing knowledge of, and attitudes towards, group B meningococcal disease and serogroup B meningococcal (MenB) vaccine among parents of young children | |
| Study setting | UK; parents of children under 2 years of age in London and Yorkshire and with a mix of socioeconomic backgrounds | |
| Notes | ||
Jama 2018.
| Study characteristics | ||
| WHO region | Europe | |
| Country classification by income level | HIC | |
| Study aim | Explore the factors influencing the decision of Somali parents on whether or not to vaccinate their children with the measles, mumps, and rubella (MMR) vaccine | |
| Study setting | Sweden; Somali mothers of at least one child aged 18 months to 5 years, living in the Rinkeby and Tensta districts of Stockholm | |
| Notes | ||
Jamal 2020.
| Study characteristics | ||
| WHO region | South‐East Asia | |
| Country classification by income level | LMIC | |
| Study aim | Examine community perspectives on routine childhood immunisation (RI) for children 0 to 23 months of age | |
| Study setting | Pakistan; female caregivers of children < 2 years living in the rural under‐resourced district of Tando Muhammad Khan of Pakistan’s Sindh province | |
| Notes | ||
Johnson 2014.
| Study characteristics | ||
| WHO region | Europe | |
| Country classification by income level | HIC | |
| Study aim | Explore mothers’ engagement with advice around the combined measles, mumps, and rubella (MMR) vaccine | |
| Study setting | UK; well‐educated mothers of preschool children between the ages of 12 and 18 months in North England | |
| Notes | ||
Kagone 2018.
| Study characteristics | ||
| WHO region | Africa | |
| Country classification by income level | LMIC | |
| Study aim | Understand perceptions of mothers and health workers regarding the vaccination program; identify factors that influence immunisation coverage; make recommendations on how to improve the vaccination program | |
| Study setting | Burkina Faso; mothers of children less than three years of age from the rural Nouna Health District in north‐western Burkina Faso. Mothers represented the five major ethnic groups residing in the area (Dafing, Bwaba, Mossi, Peulh, and Samo). | |
| Notes | ||
Keane 1993.
| Study characteristics | ||
| WHO region | America | |
| Country classification by income level | HIC | |
| Study aim | Explore parents' perceptions of disease severity of childhood illnesses and vaccine efficacy for childhood vaccines, as well as the prioritisation of the tasks of parenthood | |
| Study setting | USA; parents/guardians of infants aged 18 to 24 months living in inner‐city Baltimore | |
| Notes | ||
Khowaja 2012.
| Study characteristics | ||
| WHO region | Eastern Mediterranean | |
| Country classification by income level | LMIC | |
| Study aim | Assess parents' knowledge and perceptions surrounding polio and polio vaccination, self‐reported participation in polio supplementary immunisation activities (SIAs), and reasons for non‐participation | |
| Study setting | Pakistan; parents of children aged < 5 years of Pashtun ethnicity (a high‐risk group) living in Karachi who refused to vaccinate their children | |
| Notes | ||
King 2017.
| Study characteristics | ||
| WHO region | Western Pacific | |
| Country classification by income level | HIC | |
| Study aim | Explore the impact of the suspension of influenza vaccine for children under 5 years of age (April 2010) on parental knowledge, attitudes, trust, information needs, and intent related to influenza vaccination and broader immunisation programs | |
| Study setting | Australia; parents of children attending childcare centres in Sydney. Centres were selected to include parents from a range of socioeconomic backgrounds. | |
| Notes | ||
Kishore 2003.
| Study characteristics | ||
| WHO region | South‐East Asia | |
| Country classification by income level | LMIC | |
| Study aim | Determine the reasons for continued occurrence of wild polio cases in certain districts of western Uttar Pradesh | |
| Study setting | India; parents of children with confirmed wild polio isolation in 10 villages from the 5 high‐risk districts of western Uttar Pradesh | |
| Notes | ||
Krishnendhu 2019.
| Study characteristics | ||
| WHO region | South‐East Asia | |
| Country classification by income level | LMIC | |
| Study aim | Analyse the drivers and barriers for acceptance of the measles‐rubella (MR) vaccination | |
| Study setting | India; parents of vaccinated and unvaccinated children in the field area of a primary health center (PHC) which reported a low coverage (62%) during the initial phase of the MR vaccination campaign | |
| Notes | ||
Kurup 2017.
| Study characteristics | ||
| WHO region | Western Pacific | |
| Country classification by income level | HIC | |
| Study aim | Explore the views, concerns, and needs of parents regarding their child’s vaccination | |
| Study setting | Singapore; parents of children 0 to 18 months undergoing routine vaccination in a clinic in Singapore | |
| Notes | ||
Lannon 1995.
| Study characteristics | ||
| WHO region | America | |
| Country classification by income level | HIC | |
| Study aim | Understand the factors that impede poor parents' utilisation of healthcare services for their children and use this to refine interventions to improve immunisation rates | |
| Study setting | USA; mothers whose children received care at health departments in five rural and urban North Carolina counties. Mothers were all uninsured or were receiving Medicaid. | |
| Notes | ||
Leach 2007.
| Study characteristics | ||
| WHO region | Africa | |
| Country classification by income level | LMIC | |
| Study aim | Explore how parents’ own perspectives and experiences, embedded in broader cultural and political processes, shape immunisation demand, supply, and interfaces with providers | |
| Study setting | Gambia; mothers with child(ren) aged under two years of age from two sites in Gambia: the settlement of Sukuta in the rapidly expanding peri‐urban fringe of the capital Banjul in the Western Division, and in the rural village of Marikunda in the Upper River Division | |
| Notes | Data describing this study were also collected from Cassell 2006 | |
Leask 2006a.
| Study characteristics | ||
| WHO region | Western Pacific | |
| Country classification by income level | HIC | |
| Study aim | Explore how parents respond to competing media messages about vaccine safety | |
| Study setting | Australia; mothers of infants recruited from waiting rooms of child wellness clinics in four demographically varied but predominantly middle‐class areas across metropolitan Sydney | |
| Notes | ||
Lewendon 2002.
| Study characteristics | ||
| WHO region | Europe | |
| Country classification by income level | HIC | |
| Study aim | Identify local factors contributing to poor immunisation uptake | |
| Study setting | UK; parents of children who had been either fully immunised or partly/unimmunised in areas of low uptake in South Devon, a rural, relatively affluent area. Recruited from the attendees at local Child Health Clinics | |
| Notes | ||
Limaye 2020.
| Study characteristics | ||
| WHO region | America | |
| Country classification by income level | HIC | |
| Study aim | Explore pregnant women’s trust in obstetric providers and how power plays a role in a mother’s decision‐making process for childhood vaccines | |
| Study setting | USA; 40 first‐time pregnant women from four obstetric‐gynaecology practices in Georgia and Colorado, located in both urban and suburban settings (19 from Colorado and 21 from Georgia). Women purposively sampled to include those with a diverse range of vaccination attitudes, races/ethnicities, urbanicity, and socioeconomic statuses | |
| Notes | ||
Lugg 2015.
| Study characteristics | ||
| WHO region | Europe | |
| Country classification by income level | HIC | |
| Study aim | Explore parents’ beliefs about gastroenteritis (GE) and their attitudes towards vaccinating their children | |
| Study setting | UK; parents of children who had recently experienced an episode of GE in England and Wales | |
| Notes | ||
Lupton 2011.
| Study characteristics | ||
| WHO region | Western Pacific | |
| Country classification by income level | HIC | |
| Study aim | Explore mothers’ concepts and experiences related to promoting their infants’ health and development | |
| Study setting | Australia; women from various socioeconomic backgrounds living in Sydney with at least one child aged five years or younger | |
| Notes | ||
Mansuri 2003.
| Study characteristics | ||
| WHO region | Eastern Mediterranean | |
| Country classification by income level | LMIC | |
| Study aim | Assess the immunisation services available through expanded program of immunisations (EPI) and national immunisation days (NIDs), and to determine the reasons for incomplete immunization | |
| Study setting | Pakistan; mothers and fathers from urban squatter settlements of mixed ethnicity in all five districts of Karachi | |
| Notes | ||
Manthiram 2014.
| Study characteristics | ||
| WHO region | South‐East Asia | |
| Country classification by income level | LMIC | |
| Study aim | Assess immunisation rates of routine and optional vaccines, and examine parental attitudes toward vaccines in Pallavapuram, Tamil Nadu | |
| Study setting | India; parents with children between 18 and 36 months of age recruited from the waiting room of a private clinic in Pallavapuram, an urban area located in Kanchipuram district in the state of Tamil Nadu | |
| Notes | ||
Marshall 1999.
| Study characteristics | ||
| WHO region | Western Pacific | |
| Country classification by income level | HIC | |
| Study aim | Investigate the factors that influence parental decision‐making for childhood immunisation, and whether parents’ experiences were better conceptualised in terms of static, subjective, expected utility models or in terms of a more dynamic process | |
| Study setting | Australia; predominantly middle‐class mothers ‐ both immunisers and non‐immunisers ‐ with at least one pre‐school age child from Melbourne, Victoria | |
| Notes | ||
McCormick 1997.
| Study characteristics | ||
| WHO region | America | |
| Country classification by income level | HIC | |
| Study aim | Explore perceived parental barriers to childhood immunisation delivery | |
| Study setting | USA; white, African‐American, Hispanic, and urban and rural parents of children five years old and younger | |
| Notes | ||
McKnight 2014.
| Study characteristics | ||
| WHO region | Africa | |
| Country classification by income level | LMIC | |
| Study aim | Explore vaccination barriers and facilitators from mothers’ perspectives. | |
| Study setting | Ethiopia; 83 mothers who had not vaccinated their eligible child from Jimma Zone. The majority of mothers were peasants who lived just above a subsistence level. | |
| Notes | ||
McMurray 2004.
| Study characteristics | ||
| WHO region | Europe | |
| Country classification by income level | HIC | |
| Study aim | Explore parents’ accounts of decision‐making relating to the MMR vaccine controversy, and identify uptake determinants and education needs | |
| Study setting | UK; parents of children aged between four and five years of age recruited from five general practices in the Leeds area. Practices were purposely sampled to allow for diversity in the size, location, and level of deprivation in the populations served. | |
| Notes | ||
McNeil 2019.
| Study characteristics | ||
| WHO region | America | |
| Country classification by income level | HIC | |
| Study aim | Understand maternal vaccination decision‐making for children | |
| Study setting | Canada; mothers participating in an ongoing longitudinal pregnancy cohort study in Calgary, Alberta, interviewed at 24 months postpartum | |
| Notes | ||
Mendel‐Van Alstyne 2018.
| Study characteristics | ||
| WHO region | America | |
| Country classification by income level | HIC | |
| Study aim | Learn how mothers who are hesitant about vaccination characterise confidence in health‐related products for young children, including the recommended vaccines; gain insights into what influences vaccine confidence beliefs; and assess whether short education materials affect parental confidence in childhood vaccinations. | |
| Study setting | USA; mothers of children five years of age or less who are hesitant about vaccines, from a range of socioeconomic backgrounds, living in the Philadelphia area and the San Francisco/Oakland area | |
| Notes | ||
Miller 2008.
| Study characteristics | ||
| WHO region | America | |
| Country classification by income level | HIC | |
| Study aim | Gain insight into parents’ information needs regarding childhood immunisation in order to improve and optimise information shared by health professionals | |
| Study setting | Canada; mothers responsible for decisions about immunising their infant in the previous year from local rural communities south of Calgary, Alberta, within the boundaries of the Calgary Health Region | |
| Notes | ||
Millimouno 2006.
| Study characteristics | ||
| WHO region | Africa | |
| Country classification by income level | LMIC | |
| Study aim | Explore how vaccine supply‐demand dynamics are shaped by cultural and political processes | |
| Study setting | Guinea; parents or carers (usually the mother) of children under two years of age from rural villages and urban locations in two administrative divisions: Kissidougou and Dinguiraye | |
| Notes | Data describing this study were also collected from Leach 2007 and Leach 2008 | |
Mixer 2007.
| Study characteristics | ||
| WHO region | Europe | |
| Country classification by income level | HIC | |
| Study aim | Investigate whether a relationship exists between ethnicity and uptake of the first dose of mumps, measles, and rubella (MMR1) vaccination, and to identify important factors influencing parental decisions about vaccination | |
| Study setting | UK; mixed methods study with mothers of young children from Asian, Afro‐Caribbean and white backgrounds in Brent, northwest London | |
| Notes | ||
Mossey 2019.
| Study characteristics | ||
| WHO region | America | |
| Country classification by income level | HIC | |
| Study aim | Understand parents’ and nurses’ experiences of decision‐making about childhood immunisation, specifically measles, mumps, and rubella or diphtheria, tetanus, and acellular pertussis | |
| Study setting | Canada; parents of children under the age of five residing in a small urban centre in northeast Ontario | |
| Notes | ||
New 1991.
| Study characteristics | ||
| WHO region | Europe | |
| Country classification by income level | HIC | |
| Study aim | Examine the immunisation experiences, and influencing factors, of mothers | |
| Study setting | UK; mothers with diverse immunisation attitudes within two District Health Authorities (DHAs) in the North West of England: Lancaster and Salford | |
| Notes | ||
Niederhauser 2007.
| Study characteristics | ||
| WHO region | America | |
| Country classification by income level | HIC | |
| Study aim | Explore the barriers to immunisations in parents whose children are not fully immunised by age 2 | |
| Study setting | USA; parents with children 2 to 4 years of age who were not fully immunised at age 24 months from different islands (Oahu, Kauai, Maui, Hawaii) | |
| Notes | ||
Opel 2012.
| Study characteristics | ||
| WHO region | America | |
| Country classification by income level | HIC | |
| Study aim | Determine the feasibility of using direct observation of provider–parent immunisation discussions, and characterise provider communication practices with vaccine‐hesitant parents | |
| Study setting | USA; videotaped immunisation discussions between paediatric providers and vaccine‐hesitant parents during health supervision visits involving children 2 to 15 months old in the Seattle area, Washington, USA | |
| Notes | ||
Pal 2014.
| Study characteristics | ||
| WHO region | Western Pacific | |
| Country classification by income level | HIC | |
| Study aim | Explore attitudes, values, experiences, knowledge, behaviour, and perceived barriers regarding childhood immunisation | |
| Study setting | New Zealand; New Zealand Asian parents of children under the age of five years living in Auckland | |
| Notes | ||
Paterson 2018a.
| Study characteristics | ||
| WHO region | Europe | |
| Country classification by income level | HIC | |
| Study aim | Gain an in‐depth understanding of parents’ experience and views of vaccinating their four‐ to six‐year‐old child against influenza at school and at the general practice (GP) | |
| Study setting | UK; parents of children in Reception and Year 1 in four randomly selected schools in Bury, Leicestershire, and Surrey, England | |
| Notes | ||
Payne 2011.
| Study characteristics | ||
| WHO region | America | |
| Country classification by income level | HIC | |
| Study aim | Assess paediatrician and maternal perspectives on rotavirus vaccines and the detection of porcine circovirus (PCV) | |
| Study setting | USA; non‐vaccine‐hesitant mothers of children between 6 months and 4 years of age living in Seattle, WA; Cincinnati, OH; and Rochester, NY | |
| Notes | ||
Peretti‐Watel 2019.
| Study characteristics | ||
| WHO region | Europe | |
| Country classification by income level | HIC | |
| Study aim | Gain an in‐depth insight into parents’ vaccination decision‐making processes | |
| Study setting | France; parents (23 mothers; 2 fathers) of nursery school pupils aged 3 to 5 years old from a large city in Southeastern France. Parents purposively sampled from two contrasting socioeconomic sites: one public school located in a poor suburb characterised by high rates of unemployment, single‐parent families, and migrants; the second a private school located downtown, in a wealthier area. | |
| Notes | ||
Petts 2004.
| Study characteristics | ||
| WHO region | Europe | |
| Country classification by income level | HIC | |
| Study aim | Identify and understand individuals’ risk ‘literacy’ and its impact upon information requirements in relation to MMR and the MMR vaccination | |
| Study setting | UK; 64 women who had recently given birth to, or were expecting, their first child, and parents (mothers and fathers) with children aged 2 to 5 years from the West Midlands area, centred on Birmingham and Nuneaton. Purposive sampling to include parents from a diversity of ethnicities and socioeconomic statuses. | |
| Notes | Data describing this study were also collected from Petts 2005. | |
Pihl 2017.
| Study characteristics | ||
| WHO region | Europe | |
| Country classification by income level | HIC | |
| Study aim | Explore how parents in Denmark make a decision about whether to allow their child to receive a Bacille Calmette Guerin vaccine at birth for the purpose of achieving non‐specific effects on the immune system | |
| Study setting | Denmark; expectant mothers and fathers participating in antenatal classes at Kolding Hospital, Kolding. Socioeconomic background of the participants ranged from no education to a college education, and from no work to working as a managing director. | |
| Notes | ||
Poltorak 2005.
| Study characteristics | ||
| WHO region | Europe | |
| Country classification by income level | HIC | |
| Study aim | Explore how mothers in Brighton are thinking and deciding about MMR for their infants. | |
| Study setting | UK; mothers of child(ren) under three years of age from two economically contrasting areas (Whitehawk and Fiveways/Preston Park) of the City of Brighton and Hove, East Sussex. Mothers had a variety of social, demographic, educational, and occupational backgrounds, and had made a variety of vaccination decisions for their children. | |
| Notes | Data describing this study were also collected from Poltorak 2004 and Leach 2007 | |
Reich 2016.
| Study characteristics | ||
| WHO region | America | |
| Country classification by income level | HIC | |
| Study aim | Explore questions regarding vaccine resistance and choice | |
| Study setting | USA; 34 parents (5 fathers; 29 mothers) who have chosen either to refuse recommended vaccines for their children or consent to vaccines on a schedule other than that recommended by federal advisory bodies, state law, and physician organisations. Parents from different regions of the state of Colorado, including Denver, Colorado Springs, and Boulder, and the outlying suburbs around these cities. All but one parent was white. Parents who worked for wages tended to work in elite careers or to have jobs with high levels of flexibility. There were also large numbers of parents who did not work for wages. | |
| Notes | Data describing this study were also collected from Reich 2014, Reich 2016b, Reich 2018a, and Reich 2018b | |
Renne 2010.
| Study characteristics | ||
| WHO region | Africa | |
| Country classification by income level | LMIC | |
| Study aim | Explore parents’ perceptions of the Polio Eradication Initiative as it was conducted from 1988 to mid‐2009 | |
| Study setting | Nigeria; parents who did and did not have their children vaccinated for polio from the town of Zaria, in the northern Kaduna State | |
| Notes | Data describing this study were also collected from Renne 2006 | |
Rogers 1995.
| Study characteristics | ||
| WHO region | Europe | |
| Country classification by income level | HIC | |
| Study aim | Gain an understanding of non‐compliance with childhood immunisation | |
| Study setting | UK; 19 mothers who were opposed to immunisation mainly from a middle‐class, professional background, with a high level of occupations requiring graduate or postgraduate qualifications | |
| Notes | Data describing this study were also collected from Rogers 1995b | |
Romijnders 2019.
| Study characteristics | ||
| WHO region | Europe | |
| Country classification by income level | HIC | |
| Study aim | Explore factors related to informed decision‐making about childhood vaccination among acceptors, refusers, and partial acceptors | |
| Study setting | Netherlands; parents with children two years old from three large municipalities in the Netherlands. Parents included those from diverse socio‐economic backgrounds and those who were vaccine acceptors, refusers, and partial acceptors. | |
| Notes | ||
Ruijs 2012.
| Study characteristics | ||
| WHO region | Europe | |
| Country classification by income level | HIC | |
| Study aim | Gain insight into how orthodox Protestant parents (a specific religious minority in the Netherlands) decide to vaccinate or not vaccinate their children | |
| Study setting | The Netherlands; both vaccinating and nonvaccinating orthodox Protestant parents (from various orthodox Protestant denominations) who recently had to decide whether to vaccinate their young children or not (21 mothers, 3 fathers, and 3 couples) from various villages in the ‘Dutch bible belt’. | |
| Notes | ||
Saada 2015.
| Study characteristics | ||
| WHO region | America | |
| Country classification by income level | HIC | |
| Study aim | Gain a better understanding of the rationale underpinning parents' choices to adopt alternative vaccination schedules for their children | |
| Study setting | USA; parents of children 12 to 36 months of age who were members of Kaiser Permanente in Northern California (KPNC), a nonprofit health maintenance organisation serving privately‐ and publicly‐insured individuals. | |
| Notes | ||
Schwarz 2009.
| Study characteristics | ||
| WHO region | Africa | |
| Country classification by income level | LMIC | |
| Study aim | Explore attitudes of mothers towards childhood vaccinations and reasons for non‐attendance at and non‐adherence to mother–child clinics (MCCs) | |
| Study setting | Gabon; mothers with children less than five years attending EPI clinics in Lambaréné, the main centre of the Moyen Ogouée region | |
| Notes | ||
Sensarma 2015.
| Study characteristics | ||
| WHO region | South‐East Asia | |
| Country classification by income level | LMIC | |
| Study aim | Explore the barriers to immunisation of children with HIV‐infected mothers, as perceived by their caregivers and local healthcare service providers | |
| Study setting | India; caregivers of children (one to five years of age) born to HIV‐infected mothers from the metropolitan areas of Kolkata | |
| Notes | ||
Shefer 1998.
| Study characteristics | ||
| WHO region | America | |
| Country classification by income level | HIC | |
| Study aim | Gain a better understanding of how parents using resources from the Special Supplemental Nutrition Program for Women, Infants and Children view immunisation, and the effect of racial background on these views | |
| Study setting | USA; mothers whose children (between 6 and 24 months of age) receive services from the Special Supplemental Nutrition Program for Women, Infants and Children in Milwaukee, Wisconsin. Included Asian, white, African‐American and Hispanic mothers | |
| Notes | ||
Shui 2005.
| Study characteristics | ||
| WHO region | America | |
| Country classification by income level | HIC | |
| Study aim | Examine the vaccine safety concerns of African‐American mothers who, despite concerns, have their children immunised | |
| Study setting | USA; Atlanta‐area African‐American mothers who were very concerned about vaccine safety but whose children were fully vaccinated | |
| Notes | ||
Sjogren 2017.
| Study characteristics | ||
| WHO region | Europe | |
| Country classification by income level | HIC | |
| Study aim | Describe parental conceptions of rotavirus infection and vaccination during its implementation as part of the child immunisation program | |
| Study setting | Sweden; parents of children aged four to six weeks from five child healthcare centers in different socioeconomic areas in the center of Stockholm County. All parents had been offered, but not yet received, the first dose of the rotavirus vaccine. | |
| Notes | ||
Smith 2017.
| Study characteristics | ||
| WHO region | Europe | |
| Country classification by income level | HIC | |
| Study aim | Explore Gypsies, Roma, and Travellers (GRT) mothers’ decisions with regards to MMR immunisation and the factors underpinning those decisions | |
| Study setting | UK; 16 site‐dwelling Gypsies, Roma, and Travellers (GRT) mothers in Kent, South‐East England | |
| Notes | Data describing this study were also collected from Newton 2017 | |
Sobo 2016.
| Study characteristics | ||
| WHO region | America | |
| Country classification by income level | HIC | |
| Study aim | Learn about paediatric vaccine decision‐making amongst parents | |
| Study setting | USA; 53 English‐speaking parents (mothers and fathers) with at least one child kindergarten age or younger from San Diego, California. Participants had above average household incomes and were relatively well educated. | |
| Notes | Data describing this study were also collected from Sobo 2016b and Sobo 2016c. | |
Stamidis 2019.
| Study characteristics | ||
| WHO region | Africa | |
| Country classification by income level | LMIC | |
| Study aim | Explore the strategies, successes, and contribution between 2012 and 2017 of the CORE Group Polio Project (CGPP), a community‐centered polio eradication initiative using community volunteers (CVs) | |
| Study setting | Ethiopia; mothers and fathers with at least one child under five years of age from the CGPP‐implementation pastoralist areas in the 85 border woreda (administrative districts) of Benishangul‐Gumuz; Gambella; Oromia; Southern Nations, Nationalities, and Peoples’ Region; and Somali regions. | |
| Notes | ||
Swaney 2018.
| Study characteristics | ||
| WHO region | Western Pacific | |
| Country classification by income level | HIC | |
| Study aim | Explore reasons for vaccine‐hesitancy amongst parents from higher socioeconomic groups | |
| Study setting | Australia; vaccine‐hesitant parents from higher socioeconomic groups in Perth, Western Australia | |
| Notes | ||
Sychareun 2019.
| Study characteristics | ||
| WHO region | Western Pacific | |
| Country classification by income level | LMIC | |
| Study aim | Describe the knowledge, attitudes, and practices of mothers regarding their children’s immunisation status; and identify individual and health system determinants of access to immunisation | |
| Study setting | Lao People’s Democratic Republic; mothers with at least one child aged 12 to 23 months of age from five rural villages within the Sangthong District, Vientiane Capital City | |
| Notes | ||
Syiroj 2019.
| Study characteristics | ||
| WHO region | South‐East Asia | |
| Country classification by income level | LMIC | |
| Study aim | Explore parents’ reasons for incomplete childhood immunisation | |
| Study setting | Indonesia; primary carers of partially and unimmunised children (aged less than five years) from two Puskesmas (community health centres) in Kota Tangerang Selatan, a city in Banten Province, Indonesia | |
| Notes | ||
Tabana 2016.
| Study characteristics | ||
| WHO region | Africa | |
| Country classification by income level | LMIC | |
| Study aim | Assess the acceptability and acceptance of three vaccine injections at a single immunisation visit by caregivers and vaccinators | |
| Study setting | South Africa; caregivers with infants aged between six weeks and six months recruited from public and private primary healthcare facilities offering EPI services in rural and urban areas in the Western Cape (WC) and KwaZulu‐Natal (KZN) provinces | |
| Notes | ||
Tadesse 2009.
| Study characteristics | ||
| WHO region | Africa | |
| Country classification by income level | LMIC | |
| Study aim | Explore factors associated with childhood immunisation | |
| Study setting | Ethiopia; mothers or immediate caretakers with children between 9 and 23 months of age who had not completed the recommended child immunisation schedule and who were permanent residents in the Wonago district, Gedeo zone, Southern Nations, Nationalities and People’s Regional State (SNNPR), Ethiopia | |
| Notes | ||
Tadesse 2017.
| Study characteristics | ||
| WHO region | Africa | |
| Country classification by income level | LMIC | |
| Study aim | Explore the various factors and misperceptions of routine childhood immunisation service uptake and provide recommendations to mitigate them | |
| Study setting | Ethiopia; caretakers of children aged 12 to 23 months from nine regional states and two city administrations in Ethiopia | |
| Notes | ||
Tarrant 2003.
| Study characteristics | ||
| WHO region | America | |
| Country classification by income level | HIC | |
| Study aim | Examine mothers' perceptions of childhood immunisations and the factors that influence uptake | |
| Study setting | Canada; mothers of young children in two First Nations communities in the Sioux Lookout Zone | |
| Notes | Data describing this study were also collected from Tarrant 2003. | |
Tarrant 2008.
| Study characteristics | ||
| WHO region | Western Pacific | |
| Country classification by income level | HIC | |
| Study aim | Explore perceptions of childhood immunisations in a highly immunised population | |
| Study setting | Hong Kong; parents with a child between six months and three years of age recruited while attending a paediatric referral clinic at a university teaching hospital on Hong Kong Island. This area has high vaccination coverage. | |
| Notes | ||
Tickner 2007.
| Study characteristics | ||
| WHO region | Europe | |
| Country classification by income level | HIC | |
| Study aim | Explore parental decision‐making about the DTaP/IPV/Hib ‘five‐in‐one’ vaccine | |
| Study setting | UK; parents of babies aged between 4 and 13 weeks old from a range of socioeconomic backgrounds and a diverse range of views towards immunisation. Parents recruited from four general practices in southern England | |
| Notes | ||
Tickner 2010.
| Study characteristics | ||
| WHO region | Europe | |
| Country classification by income level | HIC | |
| Study aim | Explore parents’ views about pre‐school immunisation | |
| Study setting | UK; parents of children aged two to five years of age recruited from nine playgroups and pre‐schools in three locations (Southampton; Romsey; Windsor) in southern England | |
| Notes | ||
Tomlinson 2013.
| Study characteristics | ||
| WHO region | Europe | |
| Country classification by income level | HIC | |
| Study aim | Explore the health beliefs of Somali women resident in the UK in order to assist healthcare providers to deliver services in a manner sensitive to Somali culture | |
| Study setting | UK; mothers with at least one child under five years old who were born in Somalia, but were resident in the UK. Recruited from third‐sector organisations providing services to Somali women in Birmingham | |
| Notes | ||
Topuzoglu 2007.
| Study characteristics | ||
| WHO region | Europe | |
| Country classification by income level | LMIC | |
| Study aim | Understand the behaviours of mothers concerning the immunisation of their children, the decision‐making process, the perceived barriers, and the enabling factors to access the services. | |
| Study setting | Turkey; mothers with children younger than five years residing in Umraniye, a suburban district of Istanbul, which is composed of a socioeconomically disadvantaged population with mostly a traditional family structure | |
| Notes | ||
Vandenberg 2015.
| Study characteristics | ||
| WHO region | America | |
| Country classification by income level | HIC | |
| Study aim | Compare and contrast the understanding and decision‐making process of non‐immunising mothers and health professionals’ perceptions of these mothers’ understanding and decision‐making process | |
| Study setting | Canada; mothers from both rural and urban settings in southern Alberta with children under the age of six years who had not been immunised with routine recommended childhood immunisations according to the Alberta immunisation schedule | |
| Notes | ||
Varghese 2013.
| Study characteristics | ||
| WHO region | South‐East Asia | |
| Country classification by income level | LMIC | |
| Study aim | Examine norms regarding immunisation within communities | |
| Study setting | India; mothers of children under five years old who attended an anganwadi centre (government‐run free preschool and nutrition centre) in two Indian states: Kerala and Tamil | |
| Notes | ||
Wang 2015.
| Study characteristics | ||
| WHO region | America | |
| Country classification by income level | HIC | |
| Study aim | Examine how attitudes and beliefs of parents who self‐report as pro‐vaccine are developed and contribute to immunisation decisions | |
| Study setting | USA; parents with young children (18 months to 6 years of age) from upper‐middle‐class neighborhoods in Philadelphia | |
| Notes | ||
Ward 2017.
| Study characteristics | ||
| WHO region | Western Pacific | |
| Country classification by income level | HIC | |
| Study aim | Understand the various factors that led parents not to (or to selectively) vaccinate their children | |
| Study setting | 29 parents (25 = mothers) from the cities of Adelaide, South Australia (n = 20) and Fremantle, West Australia (n = 9) who had made an explicit, personal choice not to vaccinate, partially vaccinate or delay some vaccinations for their children and who had a child aged five years or younger. Over half of the parents held a university qualification and had middle‐ to higher‐than‐average incomes. | |
| Notes | Data describing this study were also collected from Attwell 2017, Attwell 2018a, Attwell 2018b, Attwell 2018c and Ward 2018 | |
White 1995.
| Study characteristics | ||
| WHO region | Western Pacific | |
| Country classification by income level | HIC | |
| Study aim | Explore parents' knowledge, experiences, and concerns regarding childhood immunisation | |
| Study setting | New Zealand; primary caregivers of at least one preschool child from all major socioeconomic and cultural groups in Auckland | |
| Notes | ||
Widayanti 2020.
| Study characteristics | ||
| WHO region | South‐East Asia | |
| Country classification by income level | LMIC | |
| Study aim | Explore mothers’ experiences in immunising their children through Posyandu, an outreach programme for improving mothers’ and children’s health, including immunisation | |
| Study setting | Indonesia; mothers with a child or children aged under three years who attended the Posyandu programme in East Nusa Tenggara, and West Sumatera, two provinces located outside Java Island | |
| Notes | ||
Wilson 2000.
| Study characteristics | ||
| WHO region | America | |
| Country classification by income level | HIC | |
| Study aim | Assess parental perceptions of their decision‐making regarding children’s vaccinations, and describe parents’ evaluation of immunisation services provided by rural clinics and offices | |
| Study setting | USA; mothers of children younger than three years of age with fewer than the recommended number of immunisations from rural Missouri | |
| Notes | ||
Wilson 2008.
| Study characteristics | ||
| WHO region | America | |
| Country classification by income level | HIC | |
| Study aim | Examine parental decision‐making concerning paediatric vaccination | |
| Study setting | Canada; parents who fully vaccinated and those who did not in Toronto | |
| Notes | ||
Zamir 2017.
| Study characteristics | ||
| WHO region | Europe | |
| Country classification by income level | HIC | |
| Study aim | Study attitudes and knowledge on vaccinations amongst mothers in communities with low immunisation coverage | |
| Study setting | Israel; mothers with at least one child under six years of age from one of five Jewish ultra‐Orthodox communities in the Jerusalem district that had low immunisation coverage (three Jerusalem neighborhoods and two municipalities near Jerusalem) | |
| Notes | ||
Zewdie 2016.
| Study characteristics | ||
| WHO region | Africa | |
| Country classification by income level | LMIC | |
| Study aim | Explore the reasons behind defaulting from the immunisation program | |
| Study setting | Ethiopia; mothers of children aged 6 to 11 months that defaulted from vaccination from two districts of Hadiya zone in the Southern Nations, Nationalities, and Peoples’ Region of Ethiopia | |
| Notes | ||
DTaP/IPV/Hib: diphtheria, tetanus, whooping cough, polio, and Haemophilus influenzae type B; EPI: Expanded Programme of Immunisation; HBV: hepatitis B vaccine; HICs: high‐income countries; HPV: human papillomavirus; LMICs: low‐ and middle‐income countries; MMR: measles, mumps, and rubella; NHS: National Health Service (UK).
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Adams 2007 | Did not address a routine childhood vaccine as defined by the review |
| Adams 2015 | Did not investigate the views, experiences, or decision‐making regarding routine childhood vaccination or the factors influencing acceptance, hesitancy, or nonacceptance of routine childhood vaccination arising from parents’ and informal caregivers’ accounts |
| Adams 2016 | Not possible to separate out the qualitative data |
| Akmatov 2009 | Did not use qualitative methods for data collection and analysis |
| Bastien 1995 | Not possible to separate out the data of parents of children under six years |
| Bedford 2017 | Not possible to separate out the data of parents of children under six years |
| Bell 2019 | Not possible to separate out the data of parents of children under six years |
| Berezin 2016 | Did not use qualitative methods for data collection and analysis |
| Bhat‐Schelbert 2012 | Not possible to separate out the data of parents of children under six years |
| Blaisdell 2016 | Not possible to separate out the data of parents of children under six years |
| Blum 2014 | Not possible to separate out the data of parents of children under six years |
| Blume 2017 | Did not use qualitative methods for data collection and analysis |
| Boas 2016 | Did not address a routine childhood vaccine as defined by the review |
| Brooke 1999 | Not possible to separate out the data of parents of children under six years |
| Brown 2017 | Did not address a routine childhood vaccine as defined by the review |
| Canavati 2011 | Not possible to separate out the data of parents of children under six years |
| Cassell 2006 | Did not use qualitative methods for data collection and analysis |
| Cawkwell 2016 | Did not use qualitative methods for data collection and analysis |
| Chung 2017 | Did not use qualitative methods for data collection and analysis |
| Cohen 2000 | Did not use qualitative methods for data collection and analysis |
| Conis 2014 | Did not use qualitative methods for data collection and analysis |
| Das 2000 | Not possible to separate out the data of parents of children under six years |
| Das 2003 | Did not use qualitative methods for data collection and analysis |
| Deas 2019 | Not possible to separate out the data of parents of children under six years |
| Demolis 2018 | Not possible to separate out the data of parents of children under six years |
| Elverdam 2011 | Did not investigate the views, experiences, and decision‐making regarding routine childhood vaccination, or the factors influencing acceptance, hesitancy, or nonacceptance of routine childhood vaccination arising from parents’ and informal caregivers’ accounts |
| Feldman‐Savelsberg 2000 | Did not address a routine childhood vaccine as defined by the review |
| Feldman‐Savelsberg 2005 | Did not address a routine childhood vaccine as defined by the review |
| Fourn 2009 | Not possible to separate out the data of parents of children under six years |
| Gardner 2010b | Not possible to separate out the data of parents of children under six years |
| Gazmararian 2010 | Not possible to separate out the data of parents of children under six years |
| Gesser‐Edelsburg 2016 | Not possible to separate out the data of parents of children under six years |
| Ghinai 2013 | Did not explore the perspective of parents or informal caregivers of children under six years |
| Godoy‐Ramirez 2019 | Not possible to separate out the data of parents of children under six years |
| Gottlieb 2016 | Did not address a routine childhood vaccine as defined by the review |
| Gross 2015 | Not possible to separate out the data of parents of children under six years |
| Habib 2017 | Not possible to separate out the data of parents of children under six years |
| Helle 2001 | Did not address a routine childhood vaccine as defined by the review |
| Helps 2019 | Not possible to separate out the data of parents of children under six years |
| Hilton 2007b | Not possible to separate out the data of parents of children under six years |
| Hobson‐West 2003 | Did not explore the perspective of parents or informal caregivers of children under six years |
| Hobson‐West 2004 | Did not use qualitative methods for data collection and analysis |
| Hobson‐West 2007 | Not possible to separate out the data of parents of children under six years |
| Holler 2012 | Did not use qualitative methods for data collection and analysis |
| Holte 2012 | Did not use qualitative methods for data collection and analysis |
| Ishita 2000 | Did not address a routine childhood vaccine as defined by the review |
| Jackson 2017b | Not possible to separate out the data of parents of children under six years |
| Jalloh 2019 | Not possible to separate out the data of parents of children under six years |
| Jegede 2007 | Did not explore the perspective of parents or informal caregivers of children under six years |
| Johnson 2013 | Did not use qualitative methods for data collection and analysis |
| Judith 1983 | Not possible to separate out the qualitative data |
| Kennedy 2008 | Not possible to separate out the data of parents of children under six years |
| Kennedy 2014 | Not possible to separate out the data of parents of children under six years |
| Keshet 2018 | Not possible to separate out the data for routine childhood vaccine |
| Kitta 2012 | Not possible to separate out the data of parents of children under six years |
| Kofoed 1992 | Not possible to separate out the data of parents of children under six years |
| Kowal 2015 | Not possible to separate out the data for routine childhood vaccine |
| Krishnamoorthy 2019 | Not possible to separate out the data of parents of children under six years |
| Kulig 2002 | Not possible to separate out the data of parents of children under six years |
| Largent 2012 | Did not use qualitative methods for data collection and analysis |
| Larson 2018 | Did not address a routine childhood vaccine as defined by the review |
| Lasseter 2020 | Not possible to separate out the data of parents of children under six years |
| Lawrence 2014 | Did not use qualitative methods for data collection and analysis |
| Leask 2006b | Not possible to separate out the data of parents of children under six years |
| Lee 2011 | Did not use qualitative methods for data collection and analysis |
| Lester 2000 | Did not explore the perspective of parents or informal caregivers of children under six years |
| Letley 2018 | Not possible to separate out the qualitative data |
| Lind 2014 | Did not address a routine childhood vaccine as defined by the review |
| Lind 2015 | Not possible to separate out the data of parents of children under six years |
| Lindegger 2007 | Did not address a routine childhood vaccine as defined by the review |
| Logullo 2008 | Did not use qualitative methods for data collection and analysis |
| Luthy 2012 | Did not use qualitative methods for data collection and analysis |
| Luthy 2013 | Not possible to separate out the data of parents of children under six years |
| Machekanyanga 2017 | Not possible to separate out the data of parents of children under six years |
| Mack 1999 | Not possible to separate out the qualitative data |
| Maryam 2007 | Did not use qualitative methods for data collection and analysis |
| Maya 2016 | Did not explore the perspective of parents or informal caregivers of children under six years |
| McCoy 2019 | Not possible to separate out the data of parents of children under six years |
| McDonald 2019 | Not possible to separate out the data of parents of children under six |
| McGranahan 2016 | Did not address a routine childhood vaccine as defined by the review |
| McHale 2016 | Not possible to separate out the data of parents of children under six years |
| McIntosh 2016 | Did not use qualitative methods for data collection and analysis |
| Moulsdale 2017 | Not possible to separate out the data of parents of children under six years |
| Murakami 2014 | Not possible to separate out the data of parents of children under six years |
| Namuigi 2005 | Did not use qualitative methods for data collection and analysis |
| Navin 2016 | Did not use qualitative methods for data collection and analysis |
| Newton 2006 | Did not use qualitative methods for data collection and analysis |
| Nichter 1995 | Not possible to separate out the qualitative data |
| Nuwaha 2000 | Did not explore the perspective of parents or informal caregivers of children under six years |
| Offit 2011 | Did not use qualitative methods for data collection and analysis |
| Oku 2017 | Did not investigate the views, experiences, or decision‐making regarding routine childhood vaccination or the factors influencing acceptance, hesitancy, or nonacceptance of routine childhood vaccination arising from parents’ and informal caregivers’ accounts |
| Omotara 2012 | Not possible to separate out the data of parents of children under six years |
| Onnela 2016 | Did not use qualitative methods for data collection and analysis |
| Oude 2016 | Not possible to separate out the data of parents of children under six years |
| Patel 2007 | Not possible to separate out the data of parents of children under six years |
| Paterson 2018b | Not possible to separate out the data of parents of children under six years |
| Peprah 2016 | Not possible to separate out the data of parents of children under six years |
| Plumridge 2008 | Did not explore the perspective of parents or informal caregivers of children under six years |
| Pool 2008 | Did not address a routine childhood vaccine as defined by the review |
| Pugliese‐Garcia 2018 | Not possible to separate out the data for routine childhood vaccine |
| Raithatha 2003 | Not possible to separate out the data of parents of children under six years |
| Renu 2000 | Did not explore the perspective of parents or informal caregivers of children under six years |
| Roberta 2012 | Not possible to separate out the data of parents of children under six years |
| Rodrigues 2014 | Not possible to separate out the data of parents of children under six years |
| Rodriguez 2016 | Did not explore the perspective of parents or informal caregivers of children under six years |
| Rozbroj 2020 | Not possible to separate out the data of parents of children under six years |
| Rumetta 2020 | Not possible to separate out the data of parents of children under six years |
| Sampson 2011 | Not possible to separate out the data of parents of children under six years |
| Schaetti 2012 | Did not use qualitative methods for data collection and analysis |
| Schoeppe 2017 | Not possible to separate out the data of parents of children under six years |
| Senier 2008 | Not possible to separate out the data of parents of children under six years |
| Serquina‐Ramiro 2001 | Did not use qualitative methods for data collection and analysis |
| Shahbari 2020 | Not possible to separate out the data for routine childhood vaccine |
| Sherlock 2013 | Did not address a routine childhood vaccine as defined by the review |
| Sobo 2015 | Did not explore the perspective of parents or informal caregivers of children under six years |
| Sporton 2001 | Not possible to separate out the data of parents of children under six years |
| Streefland 1999a | Not possible to separate out the qualitative data |
| Streefland 1999b | Not possible to separate out the qualitative data |
| Streefland 2001 | Not possible to separate out the qualitative data |
| Swaney 2019 | Not possible to separate out the data of parents of children under six years |
| Taylor 2010 | Did not use qualitative methods for data collection and analysis |
| Taylor 2015 | Did not use qualitative methods for data collection and analysis |
| Thorpe 2021 | Not possible to separate out the data of parents of children under six years |
| Uddin 2014 | Did not address a routine childhood vaccine as defined by the review |
| Valido 2018 | Did not address a routine childhood vaccine as defined by the review |
| Varma 2008 | Did not explore the perspective of parents or informal caregivers of children under six years |
| Velan 2016 | Did not use qualitative methods for data collection and analysis |
| Visser 2016 | Did not address a routine childhood vaccine as defined by the review |
| Wahed 2013 | Not possible to separate out the data for routine childhood vaccine |
| Wang 2014 | Not possible to separate out the data of parents of children under six years |
| Watson 2007 | Not possible to separate out the data of parents of children under six years |
| Whyte 2011 | Did not use qualitative methods for data collection and analysis |
| Wilson 2019 | Did not address a routine childhood vaccine as defined by the review |
| Winslade 2017 | Did not address a routine childhood vaccine as defined by the review |
| You 2007 | Not possible to separate out the data of parents of children under six years |
Characteristics of studies awaiting classification [ordered by study ID]
Chowdhury 1999.
| Notes | Unable to access the full text |
Closser 2010.
| Notes | Unable to access the full text |
Kennell 2014.
| Notes | Unable to access the full text |
Rogers 1994.
| Notes | Unable to access the full text |
Differences between protocol and review
Cornelia Betsch was a co‐author on this review protocol. We appreciate her contributions to the conceptualisation of the protocol design.
Once all eligible studies had been identified and we were more familiar with the evidence, it became clear that vaccination views and practices exist along a continuum. As such, we found that focusing on categorical terms such as ‘acceptance’, ‘hesitancy’, or ‘nonacceptance’, and the factors influencing these, was unhelpful and misleading. Therefore, focusing on vaccination views and practices more broadly, and the factors that may ‘enhance’ or ‘reduce’ acceptance of vaccination was more aligned with the emerging evidence. To reflect this, we therefore slightly amended our review title, topic of interest, and two of the objectives:
The protocol title was: 'Factors that influence parents’ and informal caregivers’ acceptance of routine childhood vaccination: a qualitative evidence synthesis'. The title of our review is: 'Factors that influence parents' and informal caregivers' views and practices regarding routine childhood vaccination: a qualitative evidence synthesis.'
-
The first two objectives listed in the protocol were:
Identify, appraise, and synthesise qualitative studies exploring: parents’ and informal caregivers’ views, experiences, or decision‐making regarding routine childhood vaccination; or the factors influencing acceptance of routine childhood vaccination arising from parents’ and informal caregivers’ accounts.
Develop a conceptual understanding of what and how different factors influence parental acceptance of routine childhood vaccination.
-
The first two objectives listed in the review are:
Explore parents’ and informal caregivers’ views and practices regarding routine childhood vaccination and the factors influencing acceptance, hesitancy, or nonacceptance of routine childhood vaccination.
Develop a conceptual understanding of what and how different factors reduce parental acceptance of routine childhood vaccination.
The topic of interest in the protocol was: the factors which influence the acceptance of routine childhood vaccination from the perspective of parents and informal caregivers. The topic of interest for the review is: the factors which influence parental views and practices regarding routine childhood vaccination from the perspective of parents and informal caregivers.
Contributions of authors
SC and CW conceived the review topic. SC designed the review and led the review process and write‐up.
SC, BS, ES, and NL conducted title/abstract and full‐text screening.
All review authors (SC, BS, ES, AS, CC, NL, CW) together devised the sampling frame for the review.
SC led the data management, analysis, and synthesis processes, with discussion, input and verification from BS and ES in the early stages, and from all review authors (BS, ES, AS, CC, NL, CW) in the later stages of the analysis.
SC and BS conducted the assessment of methodological limitations of the sampled studies and developed the implications for practice.
SC and BS led the GRADE‐CERQual assessments of the second‐order findings with verification from all other review authors (ES, AS, CC, NL, CW). All review authors (SC, BS, ES, AS, CC, NL, CW) together conducted the GRADE‐CERQual assessments of the third‐order findings.
SC wrote the manuscript, with input and revisions from all review authors (BS, ES, AS, CC, NL, CW).
Sources of support
Internal sources
South African Medical Research Council (SC, BS, ES, NL, CW), South Africa
University of the Western Cape (BS), South Africa
External sources
-
Foreign, Commonwealth and Development Office, UK
Project number 300342‐104
Declarations of interest
Sara Cooper: none known.
Bey‐Marrié Schmidt: none known.
Evanson Z Sambala: none known.
Alison Swartz: none known.
Christopher J Colvin: none known.
Natalie Leon: none known.
Charles S Wiysonge: none known.
New
References
References to studies included in this review
Abakar 2018 {published data only}
- Abakar MF, Seli D, Lechthaler F, Schelling E, Tran N, Zinsstag J, et al. Vaccine hesitancy among mobile pastoralists in Chad: a qualitative study. International Journal for Equity in Health 2018;17(1):167. [DOI] [PMC free article] [PubMed] [Google Scholar]
Aharon 2017 {published data only}
- Aharon A, Nehama H, Rishpon S, Bron-Epel O. Autonomy and control among parents who do not comply with recommended pediatric vaccinations: a qualitative case study. Journal of Community and Public Health Nursing 2017;3(1):152. [Google Scholar]
Ames 2017a {published data only}
- Ames H, Njang DM, Glenton C, Fretheim A, Kaufman J, Hill S, et al. Stakeholder perceptions of communication about vaccination in two regions of Cameroon: a qualitative case study. PLoS One 2017;12(8):e0183721. [DOI] [PMC free article] [PubMed] [Google Scholar]
Attwell 2019 {published data only}
- Attwell K. The politics of picking: selective vaccinators and population-level policy. SSM - Population Health 2019;7:100342. [DOI] [PMC free article] [PubMed] [Google Scholar]
Austin 2001 {published data only}
- Austin H. Parents' perceptions of information on immunisations. Journal of Child Health Care 2001;5(2):54-9. [DOI] [PubMed] [Google Scholar]
Austvoll‐Dahlgren 2010 {published data only}
- Austvoll-Dahlgren A, Helseth S. What informs parents' decision-making about childhood vaccinations? Journal of Advanced Nursing 2010;66(11):2421-30. [DOI] [PubMed] [Google Scholar]
Babirye 2011 {published data only}
- Babirye JN, Rutebemberwa E, Kiguli J, Wamani H, Nuwaha F, Engebretsen IM. More support for mothers: a qualitative study on factors affecting immunisation behaviour in Kampala, Uganda. BMC Public Health 2011;11:723. [DOI] [PMC free article] [PubMed] [Google Scholar]
Barbieri 2017 {published data only}
- Barbieri CL, Couto MT, Aith FM. Culture versus the law in the decision not to vaccinate children: meanings assigned by middle-class couples in Sao Paulo, Brazil. Cadernos de Saude Publica 2017;33(2):e00173315. [DOI] [PubMed] [Google Scholar]
- Barbieri CL, Couto MT. Decision-making on childhood vaccination by highly educated parents. Revista de Saude Publica 2015;49(18):1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Benin 2006 {published data only}
- Benin AL, Wisler-Scher DJ, Colson E, Shapiro ED, Holmboe ES. Qualitative analysis of mothers' decision-making about vaccines for infants: the importance of trust. Pediatrics 2006;117(5):1532-41. [DOI] [PubMed] [Google Scholar]
Berhanel 2000 {published data only}
- Berhanel Y, Bekele A, Tesfaye F. Immunization (EPI) in Ethiopia: acceptance, coverage, and sustainability. Ethiopian Medical Journal 2000;38 Suppl 1:1-60. [PubMed] [Google Scholar]
Berry 2018 {published data only}
- Berry NJ, Danchin M, Trevena L, Witteman HO, Kinnersley P, Snelling T, et al. Sharing knowledge about immunisation (SKAI): an exploration of parents' communication needs to inform development of a clinical communication support intervention. Vaccine 2018;36(44):6480-90. [DOI] [PubMed] [Google Scholar]
Biezen 2018 {published data only}
- Biezen R, Grando D, Mazza D, Brijnath B. Why do we not want to recommend influenza vaccination to young children? A qualitative study of Australian parents and primary care providers. Vaccine 2018;36(6):859-65. [DOI] [PubMed] [Google Scholar]
Bisht 2000 {published data only}
- Bisht S, Coutinho L. When cure is better than prevention: immunity and preventive care of measles. Economic and Political Weekly 2000;35(8/9):697-708. [Google Scholar]
Bond 1998 {published data only}
- Bond L, Nolan T, Pattison P, Carlin J. Vaccine preventable diseases and immunisations: a qualitative study of mothers' perceptions of severity, susceptibility, benefits and barriers. Australian & New Zealand Journal of Public Health 1998;22(4):441-6. [DOI] [PubMed] [Google Scholar]
Braka 2012 {published data only}
- Braka F, Asiimwe D, Soud F, Lewis RF, Makumbi I, Gust D. A qualitative analysis of vaccine safety perceptions and concerns among caretakers in Uganda. Maternal & Child Health Journal 2012;16(5):1045-52. [DOI] [PubMed] [Google Scholar]
Brown 2012 {published data only}
- Brown KF, Long SJ, Ramsay M, Hudson MJ, Green J, Vincent CA, et al. UK parents' decision-making about measles-mumps-rubella (MMR) vaccine 10 years after the MMR-autism controversy: a qualitative analysis. Vaccine 2012;30(10):1855-64. [DOI] [PubMed] [Google Scholar]
Brownlie 2005 {published data only}
- Brownlie J, Howson A. ‘Leaps of Faith’ and MMR: an empirical study of trust. Sociology 2005;39(2):221-39. [Google Scholar]
- Brownlie J, Sheach Leith LM. Social bundles: thinking through the infant body. Childhood 2011;18(2):196-210. [Google Scholar]
Brunson 2013 {published data only}
- Brunson EK, Sobo E. Framing childhood vaccination in the United States: getting past polarization in the public discourse. Human Organization 2017;76(1):38-47. [Google Scholar]
- Brunson EK. How parents make decisions about their children's vaccinations. Vaccine 2013;31(46):5466-70. [DOI] [PubMed] [Google Scholar]
- Brunson EK. Identifying parents who are amenable to pro-vaccination conversations. Global Pediatric Health 2015;2:2333794X15616332. [DOI] [PMC free article] [PubMed] [Google Scholar]
Burghouts 2017 {published data only}
- Burghouts J, Del Nogal B, Uriepero A, Hermans PW, Waard JH, Verhagen LM. Childhood vaccine acceptance and refusal among Warao Amerindian caregivers in Venezuela: a qualitative approach. PloS One 2017;12(1):e0170227. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bystrom 2014 {published data only}
- Bystrom E, Lindstrand A, Likhite N, Butler R, Emmelin M. Parental attitudes and decision-making regarding MMR vaccination in an anthroposophic community in Sweden: a qualitative study. Vaccine 2014;32(50):6752-7. [DOI] [PubMed] [Google Scholar]
Carrion 2018 {published data only}
- Carrion ML. "You need to do your research": vaccines, contestable science, and maternal epistemology. Public Understanding of Science 2018;27(3):310-24. [DOI] [PubMed] [Google Scholar]
- Carrion ML. An ounce of prevention: identifying cues to (in)action for maternal vaccine refusal. Qualitative Health Research 2018b;28(14):2183-94. [DOI] [PubMed] [Google Scholar]
Casiday 2007 {published data only}
- Casiday RE. Children's health and the social theory of risk: insights from the British measles, mumps and rubella (MMR) controversy. Social Science & Medicine 2007;65(5):1059-70. [DOI] [PubMed] [Google Scholar]
- Casiday RE. Risk and trust in vaccine decision making. Durham Anthropology Journal 2005;13(1):1-10. [Google Scholar]
- Casiday RE. Uncertainty, decision-making and trust: lessons from the MMR controversy. Community Practitioner 2006;79(11):354-7. [PubMed] [Google Scholar]
Castroviejo 2019 {published data only}
- Castroviejo FI, Jourdain S, Kacenelenbogen N, Smeesters PR. Parental perspective about paediatric vaccination: a focus group study in Brussels. Revue Medicale de Bruxelles 2019;40(1):5-17. [Google Scholar]
Chantler 2006 {published data only}
- Chantler T, Newton S, Lees A, Diggle L, Mayon-White R, Pollard AJ, et al. Parental views on the introduction of an infant pneumococcal vaccine. Community Practitioner 2006;79(7):213-6. [PubMed] [Google Scholar]
Chaturvedi 2009 {published data only}
- Chaturvedi S, Dasgupta R, Adhish V, Ganguly KK, Rai S, Sushant L, et al. Deconstructing social resistance to pulse polio campaign in two North Indian districts. Indian Pediatrics 2009;46(11):963-74. [PubMed] [Google Scholar]
Closser 2016 {published data only}
- Closser S, Rosenthal A, Maes K, Justice J, Cox K, Omidian PA, et al. The global context of vaccine refusal: insights from a systematic comparative ethnography of the Global Polio Eradication Initiative. Medical Anthropology Quarterly 2016;30(3):321-41. [DOI] [PubMed] [Google Scholar]
Cockcroft 2014 {published data only}
- Cockcroft A, Usman MU, Nyamucherera OF, Emori H, Duke B, Umar NA, et al. Why children are not vaccinated against measles: a cross-sectional study in two Nigerian States. Archives of Public Health 2014;72(1):48. [DOI] [PMC free article] [PubMed] [Google Scholar]
Condon 2002 {published data only}
- Condon L. Maternal attitudes to preschool immunisations among ethnic minority groups. Health Education Journal 2002;61(2):180-9. [Google Scholar]
Coreil 1994 {published data only}
- Coreil J, Augustin A, Halsey NA, Holt E. Social and psychological costs of preventive child health services in Haiti. Social Science & Medicine 1994;38(2):231-8. [DOI] [PubMed] [Google Scholar]
Cotter 2003 {published data only}
- Cotter S, Ryan F, Hegarty H, McCabe TJ, Keane E. Immunisation: the views of parents and health professionals in Ireland. Euro Surveillance 2003;8(6):145-50. [DOI] [PubMed] [Google Scholar]
Cuesta 2020 {published data only}
- Cuesta JG, Whitehouse K, Kaba S, Nanan-N’Zethc K, Habac B, Bachy C, et al. 'When you welcome well, you vaccinate well': a qualitative study on improving vaccination coverage in urban settings in Conakry, Republic of Guinea. International Health 2020 Jan 13 [Epub ahead of print]. [DOI: ] [DOI] [PMC free article] [PubMed]
Cullen 2005 {published data only}
- Cullen J. Why parents choose not to vaccinate their children against childhood diseases. Professional Nurse 2005;20(5):31-3. [PubMed] [Google Scholar]
Cutts 1990 {published data only}
- Cutts FT, Glik DC, Gordon A, Parker K, Diallo S, Haba F, et al. Application of multiple methods to study the immunization programme in an urban area of Guinea. Bulletin of the World Health Organization 1990;68(6):769-76. [PMC free article] [PubMed] [Google Scholar]
Delkhosh 2014 {published data only}
- Delkhosh M, Negarandeh R, Ghasemi E, Rostami H. Maternal concerns about immunization over 0-24 month children: a qualitative research. Issues in Comprehensive Pediatric Nursing 2014;37(4):235-49. [DOI] [PubMed] [Google Scholar]
deRose 2018 {published data only}
- deRose BS. The Latino immigrants’ experience in obtaining required childhood vaccinations. Journal of Transcultural Nursing 2018;29(4):363-8. [DOI] [PubMed] [Google Scholar]
Downs 2008 {published data only}
- Downs JS, Bruin WB, Fischhoff B. Parents' vaccination comprehension and decisions. Vaccine 2008;26(12):1595-607. [DOI] [PubMed] [Google Scholar]
Dube 2016 {published data only}
- Dube E, Vivion M, Sauvageau C, Gagneur A, Gagnon R, Guay M. "Nature does things well, why should we interfere?": vaccine hesitancy among mothers. Qualitative Health Research 2016;26(3):411-25. [DOI] [PubMed] [Google Scholar]
Dugas 2009 {published data only}
- Dugas M, Dube E, Kouyate B, Sanou A, Bibeau G. Portrait of a lengthy vaccination trajectory in Burkina Faso: from cultural acceptance of vaccines to actual immunization. BMC International Health & Human Rights 2009;9 Suppl 1:S9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Eng 1991 {published data only}
- Eng E, Naimoli J, Naimoli G, Parker KA, Lowenthal N. The acceptability of childhood immunization to Togolese mothers: a sociobehavioral perspective. Health Education Quarterly 1991;18(1):97-110. [DOI] [PubMed] [Google Scholar]
Enkel 2018 {published data only}
- Enkel SL, Attwell K, Snelling TL, Christian HE. 'Hesitant compliers': qualitative analysis of concerned fully-vaccinating parents. Vaccine 2018;36(44):6459-63. [DOI] [PubMed] [Google Scholar]
Evans 2001 {published data only}
- Evans M, Stoddart H, Condon L, Freeman E, Grizzell M, Mullen R. Parents' perspectives on the MMR immunisation: a focus group study. British Journal of General Practice 2001;51(472):904-10. [PMC free article] [PubMed] [Google Scholar]
Evers 2000 {published data only}
- Evers DB. Insights on immunizations from caregivers of children receiving Medicaid-funded services. Journal of the Society of Pediatric Nurses 2000;5(4):157-66. [DOI] [PubMed] [Google Scholar]
Fadda 2015 {published data only}
- Fadda M, Depping MK, Schulz PJ. Addressing issues of vaccination literacy and psychological empowerment in the measles-mumps-rubella (MMR) vaccination decision-making: a qualitative study. BMC Public Health 2015;15:836. [DOI] [PMC free article] [PubMed] [Google Scholar]
Fadda 2016 {published data only}
- Fadda M, Galimberti E, Carraro V, Schulz PJ. What are parents' perspectives on psychological empowerment in the MMR vaccination decision? A focus group study. BMJ Open 2016;6(4):e010773. [DOI] [PMC free article] [PubMed] [Google Scholar]
Figueiredo 2011 {published data only}
- Figueiredo GA, Pina JC, Tonete VL, Lima RG, Mello DF. Experiences of families in the immunization of Brazilian children under two years old. Revista Latino-Americana de Enfermagem (RLAE) 2011;19(3):598-605. [Google Scholar]
Fleming 2019 {published data only}
- Fleming JA, Munthali A, Ngwira B, Kadzandira J, Jamili-Phiri M, Ortiz JR, et al. Maternal immunization in Malawi: a mixed methods study of community perceptions, programmatic considerations, and recommendations for future planning. Vaccine 2019;37(32):4568-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
Fowler 2007 {published data only}
- Fowler GL, Kennedy A, Leidel L, Kohl KS, Khromava A, Bizhanova G, et al. Vaccine safety perceptions and experience with adverse events following immunization in Kazakhstan and Uzbekistan: a summary of key informant interviews and focus groups. Vaccine 2007;25(18):3536-43. [DOI] [PubMed] [Google Scholar]
Fredrickson 2004 {published data only}
- Fredrickson DD, Davis TC, Arnould CL, Kennen EM, Hurniston SG, Cross JT, et al. Childhood immunization refusal: provider and parent perceptions. Family Medicine 2004;36(6):431-9. [PubMed] [Google Scholar]
Gardner 2010a {published data only}
- Gardner B, McAteer J, Davies A, Michie S. Views towards compulsory MMR vaccination in the UK. Archives of Disease in Childhood 2010;95(8):658-9. [DOI] [PubMed] [Google Scholar]
Geelen 2016 {published data only}
- Geelen E, Van Vliet H, Hoogh P, Horstman K. Taming the fear of voice: dilemmas in maintaining a high vaccination rate in the Netherlands. Social Science & Medicine 2016;153:12-9. [DOI] [PubMed] [Google Scholar]
George 2016 {published data only}
- George MS, Negandhi P, Farooqui HH, Sharma A, Zodpey S. How do parents and pediatricians arrive at the decision to immunize their children in the private sector? Insights from a qualitative study on rotavirus vaccination across select Indian cities. Human Vaccines & Immunotherapeutics 2016;12(12):3139-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
Giles‐Vernick 2016 {published data only}
- Giles-Vernick T, Traore A, Bainilago L. Incertitude, hepatitis B, and infant vaccination in West and Central Africa. Medical Anthropology Quarterly 2016;30(2):203-21. [DOI] [PubMed] [Google Scholar]
Glanz 2013 {published data only}
- Glanz JM, Wagner NM, Narwaney KJ, Shoup JA, McClure DL, McCormick EV, et al. A mixed methods study of parental vaccine decision making and parent-provider trust. Academic Pediatrics 2013;13(5):481-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gorman 2019 {published data only}
- Gorman DR, Bielecki K, Willocks LJ, Pollock KG. A qualitative study of vaccination behaviour amongst female Polish migrants in Edinburgh, Scotland. Vaccine 2019;37(20):2741-7. [DOI] [PubMed] [Google Scholar]
Guillaume 2004 {published data only}
- Guillaume LR, Bath PA. The impact of health scares on parents' information needs and preferred information sources: a case study of the MMR vaccine scare. Health Informatics Journal 2004;10(1):5-22. [Google Scholar]
Gullion 2008 {published data only}
- Gullion JS, Henry L, Gullion G. Deciding to opt out of childhood vaccination mandates. Public Health Nursing 2008;25(5):401-8. [DOI] [PubMed] [Google Scholar]
Gust 2008 {published data only}
- Gust DA, Kennedy A, Wolfe S, Sheedy K, Nguyen C, Campbell S. Developing tailored immunization materials for concerned mothers. Health Education Research 2008;23(3):499-511. [DOI] [PubMed] [Google Scholar]
Handy 2017 {published data only}
- Handy LK, Maroudi S, Powell M, Nfila B, Moser C, Japa I, et al. The impact of access to immunization information on vaccine acceptance in three countries. PLoS One 2017;12(8):e0180759. [DOI] [PMC free article] [PubMed] [Google Scholar]
Harjaningrum 2013 {published data only}
- Harjaningrum AT, Kartasasmita C, Orne-Gliemann J, Jutand MA, Goujon N, Koeck JL. A qualitative study on knowledge, perceptions, and attitudes of mothers and health care providers toward pneumococcal conjugate vaccine in Bandung, West Java, Indonesia. Vaccine 2013;31(11):1516-22. [DOI] [PubMed] [Google Scholar]
Harmsen 2012 {published data only}
- Harmsen IA, Ruiter RA, Paulussen TG, Mollema L, Kok G, Melker HE. Factors that influence vaccination decision-making by parents who visit an anthroposophical child welfare center: a focus group study. Advances in Preventive Medicine 2012;2012:175694. [DOI] [PMC free article] [PubMed] [Google Scholar]
Harmsen 2013 {published data only}
- Harmsen IA, Mollema L, Ruiter RA, Paulussen TG, Melker HE, Kok G. Why parents refuse childhood vaccination: a qualitative study using online focus groups. BMC Public Health 2013;13:1183. [DOI] [PMC free article] [PubMed] [Google Scholar]
Harmsen 2015 {published data only}
- Harmsen IA, Bos H, Ruiter RA, Paulussen TG, Kok G, Melker HE, et al. Vaccination decision-making of immigrant parents in the Netherlands: a focus group study. BMC Public Health 2015;15:1229. [DOI] [PMC free article] [PubMed] [Google Scholar]
Harrington 1999 {published data only}
- Harrington PM, Woodman C, Shannon WF. Low immunisation uptake: is the process the problem? Journal of Epidemiology and Community Health 2000;54(5):394-400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrington PM, Woodman C, Shannon WF. Vaccine, yes; injection, no: maternal responses to the introduction of Haemophilus influenzae type b (Hib) vaccine. British Journal of General Practice 1999;49(448):901-2. [PMC free article] [PubMed] [Google Scholar]
- Robson J. Mothers' attitudes to vaccination. AIMS Journal 2000;12(1):17. [Google Scholar]
Hatokova 2018 {published data only}
- Hatokova M, Masaryk R, Tunyiova M. How Slovak mothers view child vaccination: focus group analysis. Ceskoslovenska Psychologie: Casopis Pro Psychologickou Teorii a Praxi 2018;62(2):101-18. [Google Scholar]
Helman 2004 {published data only}
- Helman CG, Yogeswaran P. Perceptions of childhood immunisations in rural Transkei - a qualitative study. South African Medical Journal. Suid-Afrikaanse Tydskrif Vir Geneeskunde 2004;94(10):835-8. [PubMed] [Google Scholar]
Henderson 2008 {published data only}
- Henderson L, Millett C, Thorogood N. Perceptions of childhood immunization in a minority community: qualitative study. Journal of the Royal Society of Medicine 2008;101(5):244-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hilton 2006 {published data only}
- Hilton S, Hunt K, Petticrew M. Gaps in parental understandings and experiences of vaccine-preventable diseases: a qualitative study. Child: Care, Health & Development 2007;33(2):170-9. [DOI] [PubMed] [Google Scholar]
- Hilton S, Petticrew M, Hunt K. 'Combined vaccines are like a sudden onslaught to the body's immune system': parental concerns about vaccine 'overload' and 'immune-vulnerability'. Vaccine 2006;24(20):4321-7. [DOI] [PubMed] [Google Scholar]
- Hilton S, Petticrew M, Hunt K. Parents' champions vs. vested interests: who do parents believe about MMR? A qualitative study. BMC Public Health 2007b;7(42). [DOI: 10.1186/1471-2458-7-42] [DOI] [PMC free article] [PubMed] [Google Scholar]
Houseman 1997 {published data only}
- Houseman C, Butterfoss FD, Morrow AL, Rosenthal J. Focus groups among public, military, and private sector mothers: insights to improve the immunization process. Public Health Nursing 1997;14(4):235-43. [DOI] [PubMed] [Google Scholar]
Hussain 2015 {published data only}
- Hussain RS, McGarvey ST, Fruzzetti LM. Partition and poliomyelitis: an investigation of the polio disparity affecting Muslims during India's eradication program. PLoS One 2015;10(3):e0115628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hussain RS, McGarvey ST, Shahab T, Fruzzetti LM. Fatigue and fear with shifting polio eradication strategies in India: a study of social resistance to vaccination. PLoS One 2012;7(9):e46274. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jackson 2017a {published data only}
- Jackson C, Yarwood J, Saliba V, Bedford H. UK parents' attitudes towards meningococcal group B (MenB) vaccination: a qualitative analysis. BMJ Open 2017;7(4):e012851. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jama 2018 {published data only}
- Jama A, Ali M, Lindstrand A, Butler R, Kulane A. Perspectives on the measles, mumps and rubella vaccination among Somali mothers in Stockholm. International Journal of Environmental Research & Public Health 2018;15(11):01. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jamal 2020 {published data only}
- Jamal D, Zaidi S, Husain S, Orr DW, Riaz A, Farrukhi AA, et al. Low vaccination in rural Sindh, Pakistan: a case of refusal, ignorance or access? Vaccine 2020;38(30):4747-54. [DOI] [PubMed] [Google Scholar]
Johnson 2014 {published data only}
- Johnson S, Capdevila R. ‘That’s just what’s expected of you … so you do it’: mothers' discussions around choice and the MMR vaccination. Psychology & Health 2014;29(8):861-76. [DOI] [PubMed] [Google Scholar]
Kagone 2018 {published data only}
- Kagone M, Ye M, Nebie E, Sie A, Muller O, Beiersmann C. Community perception regarding childhood vaccinations and its implications for effectiveness: a qualitative study in rural Burkina Faso. BMC Public Health 2018;18(1):324. [DOI] [PMC free article] [PubMed] [Google Scholar]
Keane 1993 {published data only}
- Keane V, Stanton B, Horton L, Aronson R, Galbraith J, Hughart N. Perceptions of vaccine efficacy, illness, and health among inner-city parents. Clinical Pediatrics 1993;32(1):2-7. [DOI] [PubMed] [Google Scholar]
Khowaja 2012 {published data only}
- Khowaja AR, Khan SA, Nizam N, Omer SB, Zaidi A. Parental perceptions surrounding polio and self-reported non-participation in polio supplementary immunization activities in Karachi, Pakistan: a mixed methods study. Bulletin of the World Health Organization 2012;90(11):822-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
King 2017 {published data only}
- King C, Leask J. The impact of a vaccine scare on parental views, trust and information needs: a qualitative study in Sydney, Australia. BMC Public Health 2017;17(1):106. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kishore 2003 {published data only}
- Kishore J, Pagare D, Malhotra R, Singh MM. Qualitative study of wild polio cases in high risk districts of Uttar Pradesh, India. National Medical Journal of India 2003;16(3):131-4. [PubMed] [Google Scholar]
Krishnendhu 2019 {published data only}
- Krishnendhu VK, George LS. Drivers and barriers for measles rubella vaccination campaign: a qualitative study. Journal of Family Medicine and Primary Care 2019;8(3):881-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kurup 2017 {published data only}
- Kurup L, He HG, Wang X, Wang W, Shorey S. A descriptive qualitative study of perceptions of parents on their child's vaccination. Journal of Clinical Nursing 2017;26(23-24):4857-67. [DOI] [PubMed] [Google Scholar]
Lannon 1995 {published data only}
- Lannon C, Brack V, Stuart J, Caplow M, McNeill A, Bordley WC, et al. What mothers say about why poor children fall behind on immunizations. A summary of focus groups in North Carolina. Archives of Pediatrics & Adolescent Medicine 1995;149(10):1070-5. [DOI] [PubMed] [Google Scholar]
Leach 2007 {published data only}
- Cassell JA, Leach M, Fairhead JR, Mary S, Mercer CH. The social shaping of childhood vaccination practice in rural and urban Gambia. Health Policy and Planning 2006;21(5):373-91. [DOI] [PubMed] [Google Scholar]
- Leach M, Fairhead J. Vaccine Anxieties: Global Science, Child Health and Society. London (UK): Earthscan, 2007. [Google Scholar]
Leask 2006a {published data only}
- Leask J, Chapman S, Hawe P, Burgess M. What maintains parental support for vaccination when challenged by anti-vaccination messages? A qualitative study. Vaccine 2006;24(49-50):7238-45. [DOI] [PubMed] [Google Scholar]
Lewendon 2002 {published data only}
- Lewendon GJ, Maconachie M. Why are children not being immunised? Barriers to immunisation uptake in South Devon. Health Education Journal 2002;61(3):212-20. [Google Scholar]
Limaye 2020 {published data only}
- Limaye RJ, Malik F, Frew PM, Randall LA, Ellingson MK, O'Leary ST, et al. Patient decision making related to maternal and childhood vaccines: exploring the role of trust in providers through a relational theory of power approach. Health Education & Behavior 2020;47(3):449-56. [DOI] [PubMed] [Google Scholar]
Lugg 2015 {published data only}
- Lugg FV, Butler CC, Evans MR, Wood F, Francis NA. Parental views on childhood vaccination against viral gastroenteritis: a qualitative interview study. Family Practice 2015;32(4):456-61. [DOI] [PubMed] [Google Scholar]
Lupton 2011 {published data only}
- Lupton DA. ‘The best thing for the baby’: mothers’ concepts and experiences related to promoting their infants’ health and development. Health, Risk & Society 2011;13(7/8):637-51. [Google Scholar]
Mansuri 2003 {published data only}
- Mansuri FA, Baig LA. Assessment of immunization service in perspective of both the recipients and the providers: a reflection from focus group discussions. Journal of Ayub Medical College 2003;15(1):14-8. [PubMed] [Google Scholar]
Manthiram 2014 {published data only}
- Manthiram K, Blood EA , Kuppuswamy V, Martins Y, Narayan A, Burmeister K, et al. Predictors of optional immunization uptake in an urban south Indian population. Vaccine 2014;32(27):3417-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
Marshall 1999 {published data only}
- Marshall S, Swerissen H. A qualitative analysis of parental decision making for childhood immunisation. Australian & New Zealand Journal of Public Health 1999;23(5):543-5. [DOI] [PubMed] [Google Scholar]
McCormick 1997 {published data only}
- McCormick LK, Bartholomew LK, Lewis MJ, Brown MW, Hanson IC. Parental perceptions of barriers to childhood immunization: results of focus groups conducted in an urban population. Health Education Research 1997;12(3):355-62. [DOI] [PubMed] [Google Scholar]
McKnight 2014 {published data only}
- McKnight J, Holt DB. Designing the Expanded Programme on Immunisation (EPI) as a service: prioritising patients over administrative logic. Global Public Health 2014;9(10):1152-66. [DOI] [PubMed] [Google Scholar]
McMurray 2004 {published data only}
- McMurray R, Cheater FM, Weighall A, Nelson C, Schweiger M, Mukherjee S. Managing controversy through consultation: a qualitative study of communication and trust around MMR vaccination decisions. British Journal of General Practice 2004;54(504):520-5. [PMC free article] [PubMed] [Google Scholar]
McNeil 2019 {published data only}
- McNeil DA, Mueller M, MacDonald S, McDonald S, Saini V, Kellner JD, et al. Maternal perceptions of childhood vaccination: explanations of reasons for and against vaccination. BMC Public Health 2019;19(1):49. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mendel‐Van Alstyne 2018 {published data only}
- Mendel-Van Alstyne JA, Nowak GJ, Aikin AL. What is 'confidence' and what could affect it?: a qualitative study of mothers who are hesitant about vaccines. Vaccine 2018;36(44):6464-72. [DOI] [PubMed] [Google Scholar]
Miller 2008 {published data only}
- Miller NK, Verhoef M, Cardwell K. Rural parents' perspectives about information on child immunization. Rural & Remote Health 2008;8(2):863. [PubMed] [Google Scholar]
Millimouno 2006 {published data only}
- Leach M, Fairhead J. Vaccine Anxieties: Global Science, Child Health and Society. London (UK): Earthscan, 2007. [Google Scholar]
- Leach MA, Fairhead JR, Millimouno D, Diallo AA. New therapeutic landscapes in Africa: parental categories and practices in seeking infant health in the Republic of Guinea. Social Science & Medicine 2008;66(10):2157-67. [DOI] [PubMed] [Google Scholar]
- Millimouno D, Diallo AA, Fairhead J, Leach M. The social dynamics of infant immunisation in Africa: perspectives from the Republic of Guinea; 2006. Available at https://opendocs.ids.ac.uk/opendocs/bitstream/handle/20.500.12413/4062/Wp262.pdf?sequence=1&isAllowed=y.
Mixer 2007 {published data only}
- Mixer RE, Jamrozik K, Newsom D. Ethnicity as a correlate of the uptake of the first dose of mumps, measles and rubella vaccine. Journal of Epidemiology & Community Health 2007;61(9):797-801. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mossey 2019 {published data only}
- Mossey S, Hosman S, Montgomery P, McCauley K. Parents' experiences and nurses' perceptions of decision-making about childhood immunization. Canadian Journal of Nursing Research = Revue Canadienne de Recherche en Sciences Infirmieres 2019;Apr 30:844562119847343. [DOI] [PubMed] [Google Scholar]
New 1991 {published data only}
- New SJ, Senior ML. "I don't believe in needles": qualitative aspects of a study into the uptake of infant immunisation in two English health authorities. Social Science & Medicine 1991;33(4):509-18. [DOI] [PubMed] [Google Scholar]
Niederhauser 2007 {published data only}
- Niederhauser VP, Markowitz M. Barriers to immunizations: multiethnic parents of under- and unimmunized children speak. Journal of the American Academy of Nurse Practitioners 2007;19(1):15-23. [DOI] [PubMed] [Google Scholar]
Opel 2012 {published data only}
- Opel DJ, Robinson JD, Heritage J, Korfiatis C, Taylor JA, Mangione-Smith R. Characterizing providers' immunization communication practices during health supervision visits with vaccine-hesitant parents: a pilot study. Vaccine 2012;30(7):1269-75. [DOI] [PubMed] [Google Scholar]
Pal 2014 {published data only}
- Pal M, Goodyear-Smith F, Exeter D. Factors contributing to high immunisation coverage among New Zealand Asians. Journal of Primary Health Care 2014;6(4):304-11. [PubMed] [Google Scholar]
Paterson 2018a {published data only}
- Paterson P, Schulz W, Utley M, Larson HJ. Parents' experience and views of vaccinating their child against influenza at primary school and at the general practice. International Journal of Environmental Research & Public Health 2018;15(4):28. [DOI] [PMC free article] [PubMed] [Google Scholar]
Payne 2011 {published data only}
- Payne DC, Humiston S, Opel D, Kennedy A, Wikswo M, Downing K, et al. A multi-center, qualitative assessment of pediatrician and maternal perspectives on rotavirus vaccines and the detection of Porcine circovirus. BMC Pediatrics 2011;11:83. [DOI] [PMC free article] [PubMed] [Google Scholar]
Peretti‐Watel 2019 {published data only}
- Peretti-Watel P, Ward JK, Vergelys C, Bocquier A, Raude J, Verger P. 'I Think I Made The Right Decision ... I Hope I'm Not Wrong'. Vaccine hesitancy, commitment and trust among parents of young children. Sociology of Health & Illness 2019;41(6):1192-206. [DOI] [PubMed] [Google Scholar]
Petts 2004 {published data only}
- Petts J, Niemeyer S. Health risk communication and amplification: learning from the MMR vaccination controversy. Health, Risk & Society 2004;6(1):7-23. [Google Scholar]
- Petts J. Health, responsibility, and choice: contrasting negotiations of air pollution and immunisation information. Environment and Planning A: Economy and Space 2005;37(5):791-804. [Google Scholar]
Pihl 2017 {published data only}
- Pihl GT, Johannessen H, Ammentorp J, Jensen JS, Kofoed PE. "Lay epidemiology": an important factor in Danish parents' decision of whether to allow their child to receive a BCG vaccination. A qualitative exploration of parental perspectives. BMC Pediatrics 2017;17(1):194. [DOI] [PMC free article] [PubMed] [Google Scholar]
Poltorak 2005 {published data only}
- Leach M, Fairhead J. Vaccine Anxieties: Global Science, Child Health and Society. London (UK): Earthscan, 2007. [Google Scholar]
- Poltorak M, Leach M, Fairhead J, Cassell J. 'MMR talk' and vaccination choices: an ethnographic study in Brighton. Social Science & Medicine 2005;61(3):709-19. [DOI] [PubMed] [Google Scholar]
- Poltorak M, Leach M, Fairhead J. MMR “choices” in Brighton: understanding public engagement with vaccination science and delivery; 2004. Available at https://opendocs.ids.ac.uk/opendocs/handle/20.500.12413/4115.
Reich 2016 {published data only}
- Reich J. Calling the Shots: Why Parents Reject Vaccines. New York (NY): New York University Press, 2016a. [Google Scholar]
- Reich JA. “I Have to Write a Statement of Moral Conviction. Can Anyone Help?”: parents’ strategies for managing compulsory vaccination laws. Sociological Perspectives 2018a;61(2):222-39. [Google Scholar]
- Reich JA. "We are fierce, independent thinkers and intelligent": social capital and stigma management among mothers who refuse vaccines. Social Science & Medicine 2018b;30:30. [DOI] [PubMed] [Google Scholar]
- Reich JA. Neoliberal mothering and vaccine refusal: imagined gated communities and the privilege of choice. Gender & Society 2014;28(5):679-704. [Google Scholar]
- Reich JA. Of natural bodies and antibodies: parents' vaccine refusal and the dichotomies of natural and artificial. Social Science & Medicine 2016b;157:103-10. [DOI] [PubMed] [Google Scholar]
Renne 2010 {published data only}
- Renne EP. Perspectives on polio and immunization in Northern Nigeria. Social Science & Medicine 2006;63(7):1857-69. [DOI] [PubMed] [Google Scholar]
- Renne EP. The Politics of Polio in Northern Nigeria. Bloomington (IN): Indiana University Press, 2010. [Google Scholar]
Rogers 1995 {published data only}
- Rogers A, Pilgrim D. Paper One. Immunisation and its discontents: an examination of dissent from the UK mass childhood immunisation programme. Health Care Analysis 1995b;3(2):99-107. [DOI] [PubMed] [Google Scholar]
- Rogers A, Pilgrim D. The risk of resistance: perspectives in the mass childhood immunization (MCI) programme. In: Gabe J, editors(s). Medicine, Health and Risk. Sociological Approaches. Oxford (UK): Blackwell, 1995a. [Google Scholar]
Romijnders 2019 {published data only}
- Romijnders KA, Van Seventer SL, Scheltema M, Van Osch L, Vries H, Mollema L. A deliberate choice? Exploring factors related to informed decision-making about childhood vaccination among acceptors, refusers, and partial acceptors. Vaccine 2019;37(37):5637-44. [DOI] [PubMed] [Google Scholar]
Ruijs 2012 {published data only}
- Ruijs WL, Hautvast JL, Van Ijzendoorn G, Van Ansem WJ, Van der Velden K, Hulscher ME. How orthodox Protestant parents decide on the vaccination of their children: a qualitative study. BMC Public Health 2012;12:408. [DOI] [PMC free article] [PubMed] [Google Scholar]
Saada 2015 {published data only}
- Saada A, Lieu TA, Morain SR, Zikmund-Fisher BJ, Wittenberg E. Parents' choices and rationales for alternative vaccination schedules: a qualitative study. Clinical Pediatrics 2015;54(3):236-43. [DOI] [PubMed] [Google Scholar]
Schwarz 2009 {published data only}
- Schwarz NG, Gysels M, Pell C, Gabor J, Schlie M, Issifou S, et al. Reasons for non-adherence to vaccination at mother and child care clinics (MCCs) in Lambarene, Gabon. Vaccine 2009;27(39):5371-5. [DOI] [PubMed] [Google Scholar]
Sensarma 2015 {published data only}
- Sensarma P, Bhandari S, Kutty VR. Barriers to immunization among children of HIV-infected mothers in Kolkata, India: a qualitative study. Asia-Pacific Journal of Public Health 2015;27(2):NP1362-71. [DOI] [PubMed] [Google Scholar]
Shefer 1998 {published data only}
- Shefer A, Mezoff J, Caspari D, Bolton M, Herrick P. What mothers in the Women, Infants, and Children (WIC) program feel about WIC and immunization linkage activities. A summary of focus groups in Wisconsin. Archives of Pediatrics & Adolescent Medicine 1998;152(1):65-70. [DOI] [PubMed] [Google Scholar]
Shui 2005 {published data only}
- Shui I, Kennedy A, Wooten K, Schwartz B, Gust D. Factors influencing African-American mothers' concerns about immunization safety: a summary of focus group findings. Journal of the National Medical Association 2005;97(5):657-66. [PMC free article] [PubMed] [Google Scholar]
Sjogren 2017 {published data only}
- Sjogren E, Ask LS, Ortqvist A, Asp M. Parental conceptions of the rotavirus vaccine during implementation in Stockholm: a phenomenographic study. Journal of Child Health Care 2017;21(4):476-87. [DOI] [PubMed] [Google Scholar]
Smith 2017 {published data only}
- Newton P, Smith DM. Factors influencing uptake of measles, mumps and rubella (MMR) immunization in site-dwelling Gypsy, Roma and Traveller (G&T) communities: a qualitative study of G&T parents' beliefs and experiences. Child: Care, Health & Development 2017;43(4):504-10. [DOI] [PubMed] [Google Scholar]
- Smith D, Newton P. Structural barriers to measles, mumps and rubella (MMR) immunisation uptake in Gypsy, Roma and Traveller communities in the United Kingdom. Critical Public Health 2017;27(2):238-47. [Google Scholar]
Sobo 2016 {published data only}
- Sobo EJ, Huhn A, Sannwald A, Thurman L. Information curation among vaccine cautious parents: Web 2.0, pinterest thinking, and pediatric vaccination choice. Medical Anthropology 2016a;35(6):529-46. [DOI] [PubMed] [Google Scholar]
- Sobo EJ. Theorizing (vaccine) refusal: through the looking glass. Cultural Anthropology 2016b;31(3):342-50. [Google Scholar]
- Sobo EJ. What is herd immunity, and how does it relate to pediatric vaccination uptake? US parent perspectives. Social Science & Medicine 2016c;165:187-95. [DOI] [PubMed] [Google Scholar]
Stamidis 2019 {published data only}
- Stamidis KV, Bologna L, Bisrat F, Tadesse T, Tessema F, Kang E. Trust, communication, and community networks: how the CORE Group Polio project community volunteers led the fight against polio in Ethiopia's most at-risk areas. American Journal of Tropical Medicine and Hygiene 2019;101(4 Suppl):59-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
Swaney 2018 {published data only}
- Swaney SE, Burns S. Exploring reasons for vaccine-hesitancy among higher-SES parents in Perth, Western Australia. Health Promotion Journal of Australia 2018;09:09. [DOI] [PubMed] [Google Scholar]
Sychareun 2019 {published data only}
- Sychareun V, Rowlands L, Vilay P, Durham J, Morgan A. The determinants of vaccination in a semi-rural area of Vientiane City, Lao People's Democratic Republic: a qualitative study. Health Research Policy & Systems 2019;17(1):2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Syiroj 2019 {published data only}
- Syiroj ATR, Pardosi JF, Heywood AE. Exploring parents' reasons for incomplete childhood immunisation in Indonesia. Vaccine 2019;37(43):6486-93. [DOI] [PubMed] [Google Scholar]
Tabana 2016 {published data only}
- Tabana H, Dudley LD, Knight S, Cameron N, Mahomed H, Goliath C, et al. The acceptability of three vaccine injections given to infants during a single clinic visit in South Africa. BMC Public Health 2016;16:749. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tadesse 2009 {published data only}
- Tadesse H, Deribew A, Woldie M. Explorative assessment of factors affecting child immunization in Wonago district, Gedeo zone, South Ethiopia. Archives of Medical Science 2009;5(2):233-40. [Google Scholar]
Tadesse 2017 {published data only}
- Tadesse T, Getachew K, Assefa T, Ababu Y, Simireta T, Birhanu Z, et al. Factors and misperceptions of routine childhood immunization service uptake in Ethiopia: findings from a nationwide qualitative study. Pan African Medical Journal 2017;28:290. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tarrant 2003 {published data only}
- Tarrant M, Gregory D. Exploring childhood immunization uptake with First Nations mothers in north-western Ontario, Canada. Journal of Advanced Nursing 2003;41(1):63-72. [DOI] [PubMed] [Google Scholar]
- Tarrant M, Gregory D. Mothers' perceptions of childhood immunizations in First Nations communities of the Sioux Lookout Zone. Canadian Journal of Public Health. Revue Canadienne de Sante Publique 2001;92(1):42-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tarrant 2008 {published data only}
- Tarrant M, Thomson N. Secrets to success: a qualitative study of perceptions of childhood immunisations in a highly immunised population. Journal of Paediatrics & Child Health 2008;44(10):541-7. [DOI] [PubMed] [Google Scholar]
Tickner 2007 {published data only}
- Tickner S, Leman PJ, Woodcock A. 'It's just the normal thing to do': exploring parental decision-making about the 'five-in-one' vaccine. Vaccine 2007;25(42):7399-409. [DOI] [PubMed] [Google Scholar]
Tickner 2010 {published data only}
- Tickner S, Leman PJ, Woodcock A. Parents' views about pre-school immunization: an interview study in southern England. Child: Care, Health & Development 2010;36(2):190-7. [DOI] [PubMed] [Google Scholar]
Tomlinson 2013 {published data only}
- Tomlinson N, Redwood S. Health beliefs about pre-school immunisation. Diversity and Equality in Health and Care 2013;10(2):101-13. [Google Scholar]
Topuzoglu 2007 {published data only}
- Topuzoglu A, Ay P, Hidiroglu S, Gurbuz Y. The barriers against childhood immunizations: a qualitative research among socio-economically disadvantaged mothers. European Journal of Public Health 2007;17(4):348-52. [DOI] [PubMed] [Google Scholar]
Vandenberg 2015 {published data only}
- Vandenberg SY, Kulig JC. Immunization rejection in southern Alberta: a comparison of the perspectives of mothers and health professionals. Canadian Journal of Nursing Research 2015;47(2):81-96. [DOI] [PubMed] [Google Scholar]
Varghese 2013 {published data only}
- Varghese J, Raman KV, Ramanathan M. The interactions of ethical notions and moral values of immediate stakeholders of immunisation services in two Indian states: a qualitative study. BMJ Open 2013;3(3):01. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wang 2015 {published data only}
- Wang E, Baras Y, Buttenheim AM. "Everybody just wants to do what's best for their child": understanding how pro-vaccine parents can support a culture of vaccine hesitancy. Vaccine 2015;33(48):6703-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ward 2017 {published data only}
- Attwell K, Leask J, Meyer SB, Rokkas P, Ward P. Vaccine rejecting parents' engagement with expert systems that inform vaccination programs. Journal of Bioethical Inquiry 2017;14(1):65-76. [DOI] [PubMed] [Google Scholar]
- Attwell K, Meyer SB, Ward PR. The social basis of vaccine questioning and refusal: a qualitative study employing Bourdieu's concepts of 'capitals' and 'habitus'. International Journal of Environmental Research & Public Health 2018a;15(5):22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Attwell K, Smith DT, Ward PR. 'The unhealthy other': how vaccine rejecting parents construct the vaccinating mainstream. Vaccine 2018b;36(12):1621-6. [DOI] [PubMed] [Google Scholar]
- Attwell K, Ward PR, Meyer SB, Rokkas PJ, Leask J. "Do-it-yourself": vaccine rejection and complementary and alternative medicine (CAM). Social Science & Medicine 2018c;196:106-14. [DOI] [PubMed] [Google Scholar]
- Ward PR, Attwell K, Meyer SB, Rokkas P, Leask J. Risk, responsibility and negative responses: a qualitative study of parental trust in childhood vaccinations. Journal of Risk Research 2018;21(9):1117-30. [Google Scholar]
- Ward PR, Attwell K, Meyer SB, Rokkas P, Leask J. Understanding the perceived logic of care by vaccine-hesitant and vaccine-refusing parents: a qualitative study in Australia. PLoS One 2017;12(10):e0185955. [DOI] [PMC free article] [PubMed] [Google Scholar]
White 1995 {published data only}
- White GE, Thomson AN. 'As every good mother should.' Childhood immunization in New Zealand: a qualitative study. Health & Social Care in the Community 1995;3(2):73-82. [Google Scholar]
Widayanti 2020 {published data only}
- Widayanti AW, Norris P, Green JA, Heydon S. Is expanding service through an outreach programme enough to improve immunisation uptake? A qualitative study in Indonesia. Global Public Health 2020;15(8):1168-81. [DOI] [PubMed] [Google Scholar]
Wilson 2000 {published data only}
- Wilson T. Factors influencing the immunization status of children in a rural setting. Journal of Pediatric Health Care 2000;14(3):117-21. [DOI] [PubMed] [Google Scholar]
Wilson 2008 {published data only}
- Wilson K, Barakat M, Vohra S, Ritvo P, Boon H. Parental views on pediatric vaccination: the impact of competing advocacy coalitions. Public Understanding of Science 2008;17(2):231-43. [DOI] [PubMed] [Google Scholar]
Zamir 2017 {published data only}
- Zamir CS, Israeli A. Knowledge, attitudes and perceptions about routine childhood vaccinations among Jewish ultra-orthodox mothers residing in communities with low vaccination coverage in the Jerusalem District. Maternal & Child Health Journal 2017;21(5):1010-7. [DOI] [PubMed] [Google Scholar]
Zewdie 2016 {published data only}
- Zewdie A, Letebo M, Mekonnen T. Reasons for defaulting from childhood immunization program: a qualitative study from Hadiya zone, Southern Ethiopia. BMC Public Health 2016;16(1):1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies excluded from this review
Adams 2007 {published data only}
- Adams IF. The ethnographic evaluation of Michigan's high-risk hepatitis B vaccination program. NAPA Bulletin 2007;27(1):81-92. [Google Scholar]
Adams 2015 {published data only}
- Adams J, Bateman B, Becker F, Cresswell T, Flynn D, McNaughton R, et al. Effectiveness and acceptability of parental financial incentives and quasi-mandatory schemes for increasing uptake of vaccinations in preschool children: systematic review, qualitative study and discrete choice experiment. Health Technology Assessment (Winchester, England) 2015;19(94):1-176. [DOI] [PMC free article] [PubMed] [Google Scholar]
Adams 2016 {published data only}
- Adams J, McNaughton RJ, Wigham S, Flynn D, Ternent L, Shucksmith J. Acceptability of parental financial incentives and quasi-mandatory interventions for preschool vaccinations: triangulation of findings from three linked studies. PLoS One 2016;11(6):e0156843. [DOI] [PMC free article] [PubMed] [Google Scholar]
Akmatov 2009 {published data only}
- Akmatov MK, Mikolajczyk RT, Kretzschmar M, Kramer A. Attitudes and beliefs of parents about childhood vaccinations in post-soviet countries: the example of Kyrgyzstan. Pediatric Infectious Disease Journal 2009;28(7):637-40. [DOI] [PubMed] [Google Scholar]
Bastien 1995 {published data only}
- Bastien JW. Cross cultural communication of tetanus vaccinations in Bolivia. Social Science & Medicine 1995;41(1):77. [DOI] [PubMed] [Google Scholar]
Bedford 2017 {published data only}
- Bedford J, Chitnis K, Webber N, Dixon P, Limwame K, Elessawi R, et al. Community engagement in Liberia: routine immunization post-Ebola. Journal of Health Communication 2017;22(Suppl 1):81-90. [DOI] [PubMed] [Google Scholar]
Bell 2019 {published data only}
- Bell S, Edelstein M, Zatonski M, Ramsay M, Mounier-Jack S. 'I don't think anybody explained to me how it works': qualitative study exploring vaccination and primary health service access and uptake amongst Polish and Romanian communities in England. BMJ Open 2019;9(7):e028228. [DOI] [PMC free article] [PubMed] [Google Scholar]
Berezin 2016 {published data only}
- Berezin M, Eads A. Risk is for the rich? Childhood vaccination resistance and a Culture of Health. Social Science & Medicine 2016;165:233-45. [DOI] [PubMed] [Google Scholar]
Bhat‐Schelbert 2012 {published data only}
- Bhat-Schelbert K, Lin CJ, Matambanadzo A, Hannibal K, Nowalk MP, Zimmerman RK. Barriers to and facilitators of child influenza vaccine - perspectives from parents, teens, marketing and healthcare professionals. Vaccine 2012;30(14):2448-52. [DOI] [PubMed] [Google Scholar]
Blaisdell 2016 {published data only}
- Blaisdell LL, Gutheil C, Hootsmans N, Han Paul KJ. Unknown risks. Medical Decision Making 2016;36(4):479-89. [DOI] [PubMed] [Google Scholar]
Blum 2014 {published data only}
- Blum LS, Dentz H, Chingoli F, Chilima B, Warne T, Lee C, et al. Formative investigation of acceptability of typhoid vaccine during a typhoid fever outbreak in Neno District, Malawi. American Journal of Tropical Medicine & Hygiene 2014;91(4):729-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
Blume 2017 {published data only}
- Blume S. How Vaccines Became Controversial. London (UK): Reaktion, 2017. [Google Scholar]
Boas 2016 {published data only}
- Boas H, Rosenthal A, Davidovitch N. Between individualism and social solidarity in vaccination policy: the case of the 2013 OPV campaign in Israel. Israel Journal of Health Policy Research 2016;5:64. [DOI] [PMC free article] [PubMed] [Google Scholar]
Brooke 1999 {published data only}
- Brooke D, Omeri A. Beliefs about childhood immunisation among Lebanese Muslim immigrants in Australia. Journal of Transcultural Nursing 1999;10(3):229-36. [DOI] [PubMed] [Google Scholar]
Brown 2017 {published data only}
- Brown T, Goldman SN, Acosta F, Garrett AM, Lee JY, Persell SD, et al. Understanding black patients' refusal of pneumococcal vaccination. Journal of Racial & Ethnic Health Disparities 2017;4(1):1-8. [DOI] [PubMed] [Google Scholar]
Canavati 2011 {published data only}
- Canavati S, Plugge E, Suwanjatuporn S, Sombatrungjaroen S, Nosten F. Barriers to immunization among children of migrant workers from Myanmar living in Tak province, Thailand. Bulletin of the World Health Organization 2011;89(7):528-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cassell 2006 {published data only}
- Cassell JA, Leach M, Poltorak MS, Mercer CH, Iversen A, Fairhead JR. Is the cultural context of MMR rejection a key to an effective public health discourse? Public Health 2006;120(9):783-94. [DOI] [PubMed] [Google Scholar]
Cawkwell 2016 {published data only}
- Cawkwell PB, Oshinsky D. Storytelling in the context of vaccine refusal: a strategy to improve communication and immunisation. Medical Humanities 2016;42(1):31-5. [DOI] [PubMed] [Google Scholar]
Chung 2017 {published data only}
- Chung Y, Schamel J, Fisher A, Frew PM. Influences on immunization decision-making among US parents of young children. Maternal & Child Health Journal 2017;21(12):2178-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cohen 2000 {published data only}
- Cohen LL, Manimala R, Blount RL. Easier said than done: what parents say they do and what they do during children's immunizations. Children's Health Care 2000;29(2):79-86. [Google Scholar]
Conis 2014 {published data only}
- Conis E. Vaccine Nation. Chicago (IL): University of Chicago Press, 2014. [Google Scholar]
Das 2000 {published data only}
- Das V, Das RK, Lester C. Disease control and immunisation: a sociological enquiry. Economic and Political Weekly 2000;35(8/9):625-32. [Google Scholar]
Das 2003 {published data only}
- Das J, Das S. Trust, learning, and vaccination: a case study of a North Indian village. Social Science & Medicine 2003;57(1):97-112. [DOI] [PubMed] [Google Scholar]
Deas 2019 {published data only}
- Deas J, Bean SJ, Sokolovska I, Fautin C. Childhood vaccine attitudes and information sources among Oregon parents and guardians. Health Promotion Practice 2019;20(4):529-38. [DOI] [PubMed] [Google Scholar]
Demolis 2018 {published data only}
- Demolis R, Botao C, Heyerdahl LW, Gessner BD, Cavailler P, Sinai C, et al. A rapid qualitative assessment of oral cholera vaccine anticipated acceptability in a context of resistance towards cholera intervention in Nampula, Mozambique. Vaccine 2018;36(44):6497-505. [DOI] [PMC free article] [PubMed] [Google Scholar]
Elverdam 2011 {published data only}
- Elverdam B. ‘It is only a pinprick’ – (or is it?) – childhood vaccinations in general practice as ‘matter out of place’. Anthropology & Medicine 2011;18(3):339-50. [DOI] [PubMed] [Google Scholar]
Feldman‐Savelsberg 2000 {published data only}
- Feldman-Savelsberg P, Ndonko FT, Schmidt-Ehry B. Sterilizing vaccines or the politics of the womb: retrospective study of a rumor in Cameroon. Medical Anthropology Quarterly 2000;14(2):159-79. [DOI] [PubMed] [Google Scholar]
Feldman‐Savelsberg 2005 {published data only}
- Feldman-Savelsberg P, Ndonko FT, Yang S, Fine GA, Campion-Vincent V, Heath C. How rumor begets rumor: collective memory, ethnic conflict, and reproductive rumors in Cameroon. In: Fine GA, Campion-Vincent V, Heath C, editors(s). Rumor Mills: The Social Impact of Rumor and Legend. New York (NY): Routledge, 2005:141–158. [Google Scholar]
Fourn 2009 {published data only}
- Fourn L, Haddad S, Fournier P, Gansey R. Determinants of parents' reticence toward vaccination in urban areas in Benin (West Africa). BMC International Health & Human Rights 2009;9 Suppl 1:S14. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gardner 2010b {published data only}
- Gardner B, Davies A, McAteer J, Michie S. Beliefs underlying UK parents' views towards MMR promotion interventions: a qualitative study. Psychology Health & Medicine 2010;15(2):220-30. [DOI] [PubMed] [Google Scholar]
Gazmararian 2010 {published data only}
- Gazmararian JA, Orenstein W, Prill M, Hitzhusen HB, Coleman MS, Pazol K, et al. Maternal knowledge and attitudes toward influenza vaccination: a focus group study in metropolitan Atlanta. Clinical Pediatrics 2010;49(11):1018-25. [DOI] [PubMed] [Google Scholar]
Gesser‐Edelsburg 2016 {published data only}
- Gesser-Edelsburg A, Shir-Raz Y, Green MS. Why do parents who usually vaccinate their children hesitate or refuse? General good vs. individual risk. Journal of Risk Research 2016;19(4):405-24. [Google Scholar]
Ghinai 2013 {published data only}
- Ghinai I, Willott C, Dadari I, Larson HJ. Listening to the rumours: what the northern Nigeria polio vaccine boycott can tell us ten years on. Global Public Health 2013;8(10):1138-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
Godoy‐Ramirez 2019 {published data only}
- Godoy-Ramirez K, Bystrom E, Lindstrand A, Butler R, Ascher H, Kulane A. Exploring childhood immunization among undocumented migrants in Sweden - following qualitative study and the World Health Organizations Guide to Tailoring Immunization Programmes (TIP). Public Health 2019;171:97-105. [DOI] [PubMed] [Google Scholar]
Gottlieb 2016 {published data only}
- Gottlieb SD. Vaccine resistances reconsidered: vaccine skeptics and the Jenny McCarthy effect. BioSocieties 2016;11(2):152-74. [Google Scholar]
Gross 2015 {published data only}
- Gross K, Hartmann K, Zemp E, Merten S. 'I know it has worked for millions of years': the role of the 'natural' in parental reasoning against child immunization in a qualitative study in Switzerland. BMC Public Health 2015;15:373. [DOI] [PMC free article] [PubMed] [Google Scholar]
Habib 2017 {published data only}
- Habib MA, Soofi SB, Ali N, Hussain I, Tabassum F, Suhag Z, et al. Knowledge and perceptions of polio and polio immunization in polio high-risk areas of Pakistan. Journal of Public Health Policy 2017;38(1):16-36. [DOI] [PubMed] [Google Scholar]
Helle 2001 {published data only}
- Helle S. Infusions of health: the popularity of vaccinations among Bissa in Burkina Faso. Anthropology and Medicine 2001;8(2/3):163-75. [Google Scholar]
Helps 2019 {published data only}
- Helps C, Leask J, Barclay L, Carter S. Understanding non-vaccinating parents' views to inform and improve clinical encounters: a qualitative study in an Australian community. BMJ Open 2019;9(5):e026299. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hilton 2007b {published data only}
- Hilton S, Hunt K, Petticrew M. MMR: marginalised, misrepresented and rejected? Autism: a focus group study. Archives of Disease in Childhood 2007;92(4):322-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hobson‐West 2003 {published data only}
- Hobson-West P. Understanding vaccination resistance: moving beyond risk. Health, Risk & Society 2003;5(3):273-83. [Google Scholar]
Hobson‐West 2004 {published data only}
- Hobson-West P. The construction of lay resistance to vaccination. In: Shaw I, Kauppinen K, editors(s). Constructions of Health and Illness. London (UK): Routledge, 2004:89-106. [Google Scholar]
Hobson‐West 2007 {published data only}
- Hobson-West P. 'Trusting blindly can be the biggest risk of all': organised resistance to childhood vaccination in the UK. Sociology of Health & Illness 2007;29(2):198-215. [DOI] [PubMed] [Google Scholar]
Holler 2012 {published data only}
- Holler K, Scalzo A. "I've heard some things that scare me". Responding with empathy to parents' fears of vaccinations. Missouri Medicine 2012;109(1):10-3, 16. [PMC free article] [PubMed] [Google Scholar]
Holte 2012 {published data only}
- Holte JH, Mæstad O, Jani JV. The decision to vaccinate a child: an economic perspective from southern Malawi. Social Science & Medicine 2012;75(2):384. [DOI] [PubMed] [Google Scholar]
Ishita 2000 {published data only}
- Ishita G, Lester C. Normalcy and crisis in time of cholera: an ethnography of cholera in Calcutta. Economic and Political Weekly 2000;35(8/9):684-96. [Google Scholar]
Jackson 2017b {published data only}
- Jackson C, Bedford H, Cheater FM, Condon L, Emslie C, Ireland L, et al. Needles, jabs and jags: a qualitative exploration of barriers and facilitators to child and adult immunisation uptake among Gypsies, Travellers and Roma. BMC Public Health 2017;17(1):254. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jalloh 2019 {published data only}
- Jalloh MF, Bennett SD, Alam D, Kouta P, Lourenco D, Alamgir M, et al. Rapid behavioral assessment of barriers and opportunities to improve vaccination coverage among displaced Rohingyas in Bangladesh. Vaccine 2019;37(6):833-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jegede 2007 {published data only}
- Jegede AS. What led to the Nigerian boycott of the polio vaccination campaign? PLoS Medicine 2007;4(3):e73. [DOI] [PMC free article] [PubMed] [Google Scholar]
Johnson 2013 {published data only}
- Johnson AM. Antivaccinationism: parental viewpoint. In: Chatterjee A, editors(s). Vaccinophobia and Vaccine Controversies of the 21st Century. New York (NY): Springer, 2013:129-46. [Google Scholar]
Judith 1983 {published data only}
- Judith E. Low immunization coverage in Yaounde, Cameroon: finding the problems. Medical Anthropology 1983;7(2):9-18. [Google Scholar]
Kennedy 2008 {published data only}
- Kennedy AM, Gust DA. Measles outbreak associated with a church congregation: a study of immunization attitudes of congregation members. Public Health Reports 2008;123(2):126-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kennedy 2014 {published data only}
- Kennedy C, Gray BC, Hogg R. 'Just that little bit of doubt': Scottish parents', teenage girls' and health professionals' views of the MMR, H1N1 and HPV vaccines. International Journal of Behavioral Medicine 2014;21(1):3-10. [DOI] [PubMed] [Google Scholar]
Keshet 2018 {published data only}
- Keshet Y, Popper-Giveon A. The undisciplined patient in neoliberal society: conscious, informed and intuitive health behaviours. Health, Risk and Society 2018;20(3-4):182-99. [Google Scholar]
Kitta 2012 {published data only}
- Kitta A. Vaccinations and Public Concern in History: Legend, Rumor, and Risk Perception. New York (NY): Routledge Taylor & Francis Group, 2012. [Google Scholar]
Kofoed 1992 {published data only}
- Kofoed PE, Zeitlyn S, Rahman AK, Gomes M, Nielsen B. Reasons for low tetanus immunization coverage in a hospital: a focus group investigation. Acta Paediatrica 1992;81(8):632. [DOI] [PubMed] [Google Scholar]
Kowal 2015 {published data only}
- Kowal SP, Jardine CG, Bubela TM. "If they tell me to get it, I'll get it. If they don't...": immunization decision-making processes of immigrant mothers. Canadian Journal of Public Health. Revue Canadienne de Sante Publique 2015;106(4):e230-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Krishnamoorthy 2019 {published data only}
- Krishnamoorthy Y, Sivaranjini K, Gokul S, Gilbert M, Sonali S, Vishwanath N. Factors related to vaccine hesitancy during the implementation of Measles-Rubella campaign 2017 in rural Puducherry: a mixed-method study. Journal of Family Medicine and Primary Care 2019;8(12):3962-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kulig 2002 {published data only}
- Kulig JC, Meyer CJ, Hill SA, Handley CE, Lichtenberger SM, Mycks SL. Refusals and delay of immunization within Southwest Alberta. Canadian Journal of Public Health 2002;93(2):109-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
Largent 2012 {published data only}
- Largent MA. Vaccine: The Debate in Modern America. Baltimore (MD): Johns Hopkins University Press, 2012. [Google Scholar]
Larson 2018 {published data only}
- Larson WA, McCloskey L, Mwale M, Mwananyanda L, Murray K, Herman AR, et al. "When you are injected, the baby is protected:" assessing the acceptability of a maternal Tdap vaccine based on mothers' knowledge, attitudes, and beliefs of pertussis and vaccinations in Lusaka, Zambia. Vaccine 2018;36(21):3048-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lasseter 2020 {published data only}
- Lasseter G, Al-Janabi H, Trotter CL, Carroll FE, Christensen H. Understanding the role of peace of mind in childhood vaccination: a qualitative study with members of the general public. Vaccine 2020;38(10):2424-32. [DOI] [PubMed] [Google Scholar]
Lawrence 2014 {published data only}
- Lawrence HY, Hausman BL, Dannenberg CJ. Reframing medicine's publics: the local as a public of vaccine refusal. Journal of Medical Humanities 2014;35(2):111-29. [DOI] [PubMed] [Google Scholar]
Leask 2006b {published data only}
- Leask J, Sheikh-Mohammed M, Macintyre CR, Leask A, Wood NJ. Community perceptions about infectious disease risk posed by new arrivals: a qualitative study. Medical Journal of Australia 2006;185(11-12):591-3. [DOI] [PubMed] [Google Scholar]
Lee 2011 {published data only}
- Lee E, Turner J, Bate J. Parental opinions on childhood varicella and the varicella vaccine: a UK multicentre qualitative interview study. Archives of Disease in Childhood 2011;96(9):901. [DOI] [PubMed] [Google Scholar]
Lester 2000 {published data only}
- Lester C, Niharika B. Social production of blame: case study of OPV-related deaths in West Bengal. Economic and Political Weekly 2000;35(8/9):709-17. [Google Scholar]
Letley 2018 {published data only}
- Letley L, Rew V, Ahmed R, Habersaat KB, Paterson P, Chantler T, et al. Tailoring immunisation programmes: using behavioural insights to identify barriers and enablers to childhood immunisations in a Jewish community in London, UK. Vaccine 2018;36(31):4687-92. [DOI] [PubMed] [Google Scholar]
Lind 2014 {published data only}
- Lind C, Russell ML, MacDonald J, Collins R, Frank CJ, Davis AE. School-based influenza vaccination: parents' perspectives. PLoS One 2014;9(3):e93490. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lind 2015 {published data only}
- Lind C, Russell ML, Collins R, MacDonald J, Frank CJ, Davis AE. How rural and urban parents describe convenience in the context of school-based influenza vaccination: a qualitative study. BMC Health Services Research 2015;15:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lindegger 2007 {published data only}
- Lindegger G, Quayle M, Ndlovu M. Local knowledge and experiences of vaccination: implications for HIV-preventive vaccine trials in South Africa. Health Education & Behavior 2007;34(1):108-23. [DOI] [PubMed] [Google Scholar]
Logullo 2008 {published data only}
- Logullo P, Barbosa de Carvalho H, Saconi R, Massad E. Factors affecting compliance with the measles vaccination schedule in a Brazilian city. Sao Paulo Medical Journal 2008;126(3):166-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
Luthy 2012 {published data only}
- Luthy KE, Beckstrand RL, Callister LC, Cahoon S. Reasons parents exempt children from receiving immunizations. Journal of School Nursing 2012;28(2):153-60. [DOI] [PubMed] [Google Scholar]
Luthy 2013 {published data only}
- Luthy KE, Beckstrand RL, Asay W, Hewett C. Vaccinating parents experience vaccine anxiety too. Journal of the American Association of Nurse Practitioners 2013;25(12):667-73. [DOI] [PubMed] [Google Scholar]
Machekanyanga 2017 {published data only}
- Machekanyanga Z, Ndiaye S, Gerede R, Chindedza K, Chigodo C, Shibeshi ME, et al. Qualitative assessment of vaccination hesitancy among members of the Apostolic Church of Zimbabwe: a case study. Journal of Religion & Health 2017;56(5):1683-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mack 1999 {published data only}
- Mack RW, Darden PM. Children's immunizations: the gap between parents and providers. Health Marketing Quarterly 1999;16(4):7-14. [DOI] [PubMed] [Google Scholar]
Maryam 2007 {published data only}
- Maryam Y. Polio vaccines - "No thank you!" barriers to polio eradication in northern Nigeria. African Affairs 2007;106(423):185-204. [Google Scholar]
Maya 2016 {published data only}
- Maya JG. Public misunderstanding of science? Reframing the problem of vaccine hesitancy. Perspectives on Science 2016;24(5):552-81. [Google Scholar]
McCoy 2019 {published data only}
- McCoy JD, Painter JE, Jacobsen KH. Perceptions of vaccination within a Christian homeschooling community in Pennsylvania. Vaccine 2019;37(38):5770-6. [DOI] [PubMed] [Google Scholar]
McDonald 2019 {published data only}
- McDonald P, Limaye RJ, Omer SB, Buttenheim AM, Mohanty S, Klein NP, et al. Exploring California's new law eliminating personal belief exemptions to childhood vaccines and vaccine decision-making among homeschooling mothers in California. Vaccine 2019;37(5):742-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
McGranahan 2016 {published data only}
- McGranahan C. Theorizing refusal: an introduction. Cultural Anthropology 2016;31(3):319-25. [Google Scholar]
McHale 2016 {published data only}
- McHale P, Keenan A, Ghebrehewet S. Reasons for measles cases not being vaccinated with MMR: investigation into parents' and carers' views following a large measles outbreak. Epidemiology and Infection 2016;144(4):870-5. [DOI] [PubMed] [Google Scholar]
McIntosh 2016 {published data only}
- McIntosh ED, Janda J, Ehrich JH, Pettoello-Mantovani M, Somekh E. Vaccine hesitancy and refusal. Journal of Pediatrics 2016;175:248-249.e1. [DOI] [PubMed] [Google Scholar]
Moulsdale 2017 {published data only}
- Moulsdale P. Parents' perceptions of influenza and why they accept or decline the nasal vaccine for their child. Nursing Children & Young People 2017;29(3):28-33. [DOI] [PubMed] [Google Scholar]
Murakami 2014 {published data only}
- Murakami H, Kobayashi M, Hachiya M, Khan ZS, Hassan SQ, Sakurada S. Refusal of oral polio vaccine in northwestern Pakistan: a qualitative and quantitative study. Vaccine 2014;32(12):1382-7. [DOI] [PubMed] [Google Scholar]
Namuigi 2005 {published data only}
- Namuigi P, Phuanukoonnon S. Barriers to measles immunization: the beliefs and attitudes of caregivers in Goroka, Eastern Highlands Province, Papua New Guinea. Papua New Guinea Medical Journal 2005;48(3-4):183-7. [PubMed] [Google Scholar]
Navin 2016 {published data only}
- Navin M. Values and Vaccine Refusal: Hard Questions in Ethics, Epistemology, and Health Care. New York (NY): Routledge, 2016. [Google Scholar]
Newton 2006 {published data only}
- Newton S, Chantler T, Diggle L, Yu L, McCarthy N, Moxon R, et al. Parental acceptability of a pneumococcal conjugate vaccine in the UK childhood immunisation schedule. Primary Health Care 2006;16(8):34-9. [Google Scholar]
Nichter 1995 {published data only}
- Nichter M. Vaccinations in the Third World: a consideration of community demand. Social Science & Medicine 1995;41(5):617-32. [DOI] [PubMed] [Google Scholar]
Nuwaha 2000 {published data only}
- Nuwaha F, Mulindwa G, Kabwongyera E, Barenzi J. Causes of low attendance at national immunization days for polio eradication in Bushenyi district, Uganda. Tropical Medicine & International Health 2000;5(5):364-9. [DOI] [PubMed] [Google Scholar]
Offit 2011 {published data only}
- Offit PA. Deadly Choices: How the Anti-Vaccine Movement Threatens Us All. New York (NY): Basic Books, 2011. [Google Scholar]
Oku 2017 {published data only}
- Oku A, Oyo-Ita A, Glenton C, Fretheim A, Ames H, Muloliwa A, et al. Perceptions and experiences of childhood vaccination communication strategies among caregivers and health workers in Nigeria: a qualitative study. PLoS One 2017;12(11):e0186733. [DOI] [PMC free article] [PubMed] [Google Scholar]
Omotara 2012 {published data only}
- Omotara BF, Okujagu T. Assessment of knowledge, attitude and practice of stakeholders towards immunization in Borno State, Nigeria: a qualitative approach. Journal of Community Medicine & Health Education for Health 2012;2(9):181. [Google Scholar]
Onnela 2016 {published data only}
- Onnela JP, Landon BE, Kahn AL, Ahmed D, Verma H, O'Malley AJ, et al. Polio vaccine hesitancy in the networks and neighborhoods of Malegaon, India. Social Science & Medicine 2016;153:99-106. [DOI] [PubMed] [Google Scholar]
Oude 2016 {published data only}
- Oude EA, Carbonnel F, Lognos B, Million E, Vallart M, Gagnon S, et al. Understanding parents' vaccination decisions to better help their decisions: a phenomenological qualitative study with French parents [Comprendre la decision vaccinale des parents pour mieux accompagner leurs choix: etude qualitative phenomenologique aupres des parents français]. Canadian Journal of Public Health. Revue Canadienne de Sante Publique 2016;106(8):e527-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
Patel 2007 {published data only}
- Patel MM, Janssen AP, Tardif RR, Herring M, Parashar UD. A qualitative assessment of factors influencing acceptance of a new rotavirus vaccine among health care providers and consumers. BMC Pediatrics 2007;7(32):5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Paterson 2018b {published data only}
- Paterson P, Chantler T, Larson HJ. Reasons for non-vaccination: parental vaccine hesitancy and the childhood influenza vaccination school pilot programme in England. Vaccine 2018;36(36):5397-401. [DOI] [PubMed] [Google Scholar]
Peprah 2016 {published data only}
- Peprah D, Palmer JJ, Rubin GJ, Abubakar A, Costa A, Martin S, et al. Perceptions of oral cholera vaccine and reasons for full, partial and non-acceptance during a humanitarian crisis in South Sudan. Vaccine 2016;34(33):3823-7. [DOI] [PubMed] [Google Scholar]
Plumridge 2008 {published data only}
- Plumridge E, Goodyear-Smith FA, Ross J. Parents and nurses during the immunization of children--where is the power? A conversation analysis. Family Practice 2008;25(1):14-9. [DOI] [PubMed] [Google Scholar]
Pool 2008 {published data only}
- Pool R, Mushi A, Schellenberg JA, Mrisho M, Alonso P, Montgomery C, et al. The acceptability of intermittent preventive treatment of malaria in infants (IPTi) delivered through the expanded programme of immunization in southern Tanzania. Malaria Journal 2008;7:213. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pugliese‐Garcia 2018 {published data only}
- Pugliese-Garcia M, Heyerdahl LW, Mwamba C, Nkwemu S, Chilengi R, Demolis R, et al. Factors influencing vaccine acceptance and hesitancy in three informal settlements in Lusaka, Zambia. Vaccine 2018;36(37):5617-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
Raithatha 2003 {published data only}
- Raithatha N, Holland R, Gerrard S, Harvey I. A qualitative investigation of vaccine risk perception amongst parents who immunize their children: a matter of public health concern. Journal of Public Health Medicine 2003;25(2):161-4. [DOI] [PubMed] [Google Scholar]
Renu 2000 {published data only}
- Renu A. Global-local dialectic in medico-administrative practice: case study of poliomyelitis. Economic and Political Weekly 2000;35(8/9):676-83. [Google Scholar]
Roberta 2012 {published data only}
- Roberta R. When 'to choose' is 'to care': informed dissent and the case of paediatric vaccinations. Suomen Antropologi – Journal of the Finnish Anthropological Society 2012;37(3):8-23. [Google Scholar]
Rodrigues 2014 {published data only}
- Rodrigues AD, Lorenzini E, da Silva FE. Mothers' knowledge regarding the vaccination program and factors which lead to delays in infant vaccination. Cogitare Enfermagem 2014;19(1):179-92. [Google Scholar]
Rodriguez 2016 {published data only}
- Rodriguez NJ. Vaccine-hesitant justifications: "Too Many, Too Soon," narrative persuasion, and the conflation of expertise. Global Qualitative Nursing Research 2016;3:2333393616663304. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rozbroj 2020 {published data only}
- Rozbroj T, Lyons A, Lucke J. Vaccine-hesitant and vaccine-refusing parents' reflections on the way parenthood changed their attitudes to vaccination. Journal of Community Health 2020;45(1):63-72. [DOI] [PubMed] [Google Scholar]
Rumetta 2020 {published data only}
- Rumetta J, Abdul-Hadi H, Lee Y. A qualitative study on parents' reasons and recommendations for childhood vaccination refusal in Malaysia. Journal of Infection and Public Health 2020;13(2):199-203. [DOI] [PubMed] [Google Scholar]
Sampson 2011 {published data only}
- Sampson R, Wong L, Macvicar R. Parental reasons for non-uptake of influenza vaccination in young at-risk groups: a qualitative study. British Journal of General Practice 2011;61(588):e386-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
Schaetti 2012 {published data only}
- Schaetti C, Ali SM, Hutubessy R, Khatib AM, Chaignat C, Weiss MG. Social and cultural determinants of oral cholera vaccine uptake in Zanzibar. Human Vaccines & Immunotherapeutics 2012;8(9):1223-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Schoeppe 2017 {published data only}
- Schoeppe J, Cheadle A, Melton M, Faubion T, Miller C, Matthys J, et al. The immunity community: a community engagement strategy for reducing vaccine hesitancy. Health Promotion Practice 2017;18(5):654-61. [DOI] [PubMed] [Google Scholar]
Senier 2008 {published data only}
- Senier L. "It's your most precious thing": worst-case thinking, trust, and parental decision making about vaccinations. Sociological Inquiry 2008;78(2):207-29. [Google Scholar]
Serquina‐Ramiro 2001 {published data only}
- Serquina-Ramiro L, Kasniyah N, Inthusoma T, Higginbotham N, Streiner D, Nichter M, et al. Measles immunization acceptance in Southeast Asia: past patterns and future challenges. Southeast Asian Journal of Tropical Medicine & Public Health 2001;32(4):791-804. [PubMed] [Google Scholar]
Shahbari 2020 {published data only}
- Shahbari NA, Gesser-Edelsburg A, Mesch GS. Perceived trust in the health system among mothers and nurses and its relationship to the issue of vaccinations among the Arab population of Israel: a qualitative research study. Vaccine 2020;38(1):29-38. [DOI] [PubMed] [Google Scholar]
Sherlock 2013 {published data only}
- Sherlock M, Cardoso M, Lélis A, Lopes M, Pereira M. Reasons for non-compliance of mothers to immunization schedule of children exposed to HIV. Revista da Rede de Enfermagem do Nordeste 2013;14(2):341-53. [Google Scholar]
Sobo 2015 {published data only}
- Sobo EJ. Social cultivation of vaccine refusal and delay among Waldorf (Steiner) school parents. Medical Anthropology Quarterly 2015;29(3):381-99. [DOI] [PubMed] [Google Scholar]
Sporton 2001 {published data only}
- Sporton RK, Francis SA. Choosing not to immunize: are parents making informed decisions? Family Practice 2001;18(2):181-8. [DOI] [PubMed] [Google Scholar]
Streefland 1999a {published data only}
- Streefland PH, Chowdhury AM, Ramos-Jimenez P. Quality of vaccination services and social demand for vaccinations in Africa and Asia. Bulletin of the World Health Organization 1999;77(9):722-30. [PMC free article] [PubMed] [Google Scholar]
Streefland 1999b {published data only}
- Streefland P, Chowdhury AM, Ramos-Jimenez P. Patterns of vaccination acceptance. Social Science & Medicine 1999;49(12):1705-16. [DOI] [PubMed] [Google Scholar]
Streefland 2001 {published data only}
- Streefland PH. Public doubts about vaccination safety and resistance against vaccination. Health Policy 2001;55(3):159-72. [DOI] [PubMed] [Google Scholar]
Swaney 2019 {published data only}
- Swaney SE, Burns S. Exploring reasons for vaccine-hesitancy among higher-SES parents in Perth, Western Australia. Health promotion journal of Australia 2019;30(2):143-52. [DOI] [PubMed] [Google Scholar]
Taylor 2010 {published data only}
- Taylor S, Shimp L. Using data to guide action in polio health communications: experience from the Polio Eradication Initiative (PEI). Journal of Health Communication 2010;15 Suppl 1:48-65. [DOI] [PubMed] [Google Scholar]
Taylor 2015 {published data only}
- Taylor S. Culture and behaviour in mass health interventions: lessons from the global polio eradication initiative. Critical Public Health 2015;25(2):192. [Google Scholar]
Thorpe 2021 {published data only}
- Thorpe M, Taylor J, Cole R. Parents' use of information accessed through social media to make immunisation decisions for their young children. Health Promotion Journal of Australia 2021;32(2):189-196. [DOI] [PubMed] [Google Scholar]
Uddin 2014 {published data only}
- Uddin MJ, Wahed T, Saha NC, Kaukab SS, Khan IA, Khan AI, et al. Coverage and acceptability of cholera vaccine among high-risk population of urban Dhaka, Bangladesh. Vaccine 2014;32(43):5690-5. [DOI] [PubMed] [Google Scholar]
Valido 2018 {published data only}
- Valido EM, Laksanawati IS, Utarini A. Acceptability of the dengue vaccination among parents in urban poor communities of Quezon City, Philippines before and after vaccine suspension. BMC Research Notes 2018;11(1):661. [DOI] [PMC free article] [PubMed] [Google Scholar]
Varma 2008 {published data only}
- Varma GR, Kusuma YS. Immunization coverage in tribal and rural areas of Visakhapatnam district of Andhra Pradesh, India. Journal of Public Health 2008;16(6):389-97. [Google Scholar]
Velan 2016 {published data only}
- Velan B. Vaccine hesitancy as self-determination: an Israeli perspective. Israel Journal of Health Policy Research 2016;5:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
Visser 2016 {published data only}
- Visser O, Hautvast JL, Van der Velden K, Hulscher ME. Intention to accept pertussis vaccination for cocooning: a qualitative study of the determinants. PLoS One 2016;11(6):e0155861. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wahed 2013 {published data only}
- Wahed T, Kaukab SS, Saha NC, Khan IA, Khanam F, Chowdhury F, et al. Knowledge of, attitudes toward, and preventive practices relating to cholera and oral cholera vaccine among urban high-risk groups: findings of a cross-sectional study in Dhaka, Bangladesh. BMC Public Health 2013;13:242. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wang 2014 {published data only}
- Wang LD, Lam WW, Wu JT, Liao Q, Fielding R. Chinese immigrant parents' vaccination decision making for children: a qualitative analysis. BMC Public Health 2014;14:133. [DOI] [PMC free article] [PubMed] [Google Scholar]
Watson 2007 {published data only}
- Watson PB, Yarwood J, Chenery K. Meningococcal B: tell me everything you know and everything you don't know. New Zealanders' decision-making regarding an immunisation programme. New Zealand Medical Journal 2007;120(1263):U2751. [PubMed] [Google Scholar]
Whyte 2011 {published data only}
- Whyte MD, Whyte Iv J, Cormier E, Eccles DW. Factors influencing parental decision making when parents choose to deviate from the standard pediatric immunization schedule. Journal of Community Health Nursing 2011;28(4):204-14. [DOI] [PubMed] [Google Scholar]
Wilson 2019 {published data only}
- Wilson R, Paterson P, Larson HJ. Strategies to improve maternal vaccination acceptance. BMC Public Health 2019;19(1):342. [DOI] [PMC free article] [PubMed] [Google Scholar]
Winslade 2017 {published data only}
- Winslade CG, Heffernan CM, Atchison CJ. Experiences and perspectives of mothers of the pertussis vaccination programme in London. Public Health 2017;146:10-14. [DOI] [PubMed] [Google Scholar]
You 2007 {published data only}
- You X, Kobayashi Y, Yang J, Zhu X, Liang X. Qualitative study of knowledge and behaviours related to tetanus toxoid immunization among women of childbearing age in rural China. Public Health 2007;121(3):227-30. [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
Chowdhury 1999 {published data only}
- Chowdhury M, Aziz A, Bhuiya A. The 'Near Miracle' Revisited: Social Science Perspectives of the Immunization Programme in Bangladesh. Amsterdam (the Netherlands): Het Spinhuis, 1999. [Google Scholar]
Closser 2010 {published data only}
- Closser S. Chasing Polio in Pakistan: Why the World’s Largest Public Health Initiative May Fail. Nashville (TN): Vanderbilt University Press, 2010. [Google Scholar]
Kennell 2014 {published data only}
- Kennell JL. Vaccination programs and the sensibilisation of an Aja community in Benin. In: Rhine K, Janzen J, Adams G, Aldersey H, editors(s). Medical Anthropology in Global Africa. Lawrence (KS): University of Kansas, Department of Anthropology, 2014:27-33. [Google Scholar]
Rogers 1994 {published data only}
- Rogers A, Pilgrim D. Rational non-compliance with childhood immunisation: personal accounts of parents and primary health care professionals. In: Uptake of lmmunisation: Issues for Health Educators. London (UK): Health Education Authority, 1994. [Google Scholar]
Additional references
Alto 1994
- Alto WA, Fury D, Condo A, Doran M, Aduddell M. Improving the immunization coverage of children less than 7 years old in a family practice residency. Journal of the American Board of Family Practice 1994;7(6):472-7. [PubMed] [Google Scholar]
Ames 2017b
- Ames HM, Glenton C, Lewin S. Parents' and informal caregivers' views and experiences of communication about routine childhood vaccination: a synthesis of qualitative evidence. Cochrane Database of Systematic Reviews 2017, Issue 2. Art. No: CD011787. [DOI: 10.1002/14651858.CD011787.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ames 2019a
- Ames H, Glenton C, Lewin S. Purposive sampling in a qualitative evidence synthesis: a worked example from a synthesis on parental perceptions of vaccination communication. BMC Medical Research Methodology 2019;19(1):26. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ames 2019b
- Ames HM, Glenton C, Lewin S, Tamrat T, Akama E, Leon N. Clients’ perceptions and experiences of targeted digital communication accessible via mobile devices for reproductive, maternal, newborn, child, and adolescent health: a qualitative evidence synthesis. Cochrane Database of Systematic Reviews 2019, Issue 10. Art. No: CD013447. [DOI: 10.1002/14651858.CD013447] [DOI] [PMC free article] [PubMed] [Google Scholar]
Andersson 2009
- Andersson N, Cockcroft A, Ansari NM, Omer K, Baloch M, Ho Foster A, et al. Evidence-based discussion increases childhood vaccination uptake: a randomised cluster controlled trial of knowledge translation in Pakistan. BMC International Health and Human Rights 2009;9(Suppl 1):S8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Andre 2008
- Andre FE, Booy R, Bock HL, Clemens J, Datta SK, John TJ, et al. Vaccination greatly reduces disease, disability, death and inequity worldwide. Bulletin of the World Health Organization 2008;86(2):140-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Atkins 2008
- Atkins S, Lewin S, Smith H, Engel M, Fretheim A, Volmink J. Conducting a meta-ethnography of qualitative literature: lessons learnt. BMC Medical Research Methodology 2008;8:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
Banerjee 2010
- Banerjee AV, Duflo E, Glennerster R, Kothari D. Improving immunisation coverage in rural India: clustered randomised controlled evaluation of immunisation campaigns with and without incentives. BMJ 2010;340:c2220. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bangure 2015
- Bangure D, Chirundu D, Gombe N, Marufu T, Mandozana G, Tshimanga M, et al. Effectiveness of short message services reminder on childhood immunization programme in Kadoma, Zimbabwe - a randomized controlled trial, 2013. BMC Public Health 2015;15:137. [DOI] [PMC free article] [PubMed] [Google Scholar]
Barham 2005
- Barham T. The Impact of the Mexican Conditional Cash Transfer on Immunization Rates. Berkeley (CA): Department of Agriculture and Resource Economics, 2005. [Google Scholar]
Barnett‐Page 2009
- Barnett-Page E, Thomas J. Methods for the synthesis of qualitative research: a critical review. BMC Medical Research Methodology 2009;9:59. [DOI] [PMC free article] [PubMed] [Google Scholar]
Beck 1992
- Beck U. Risk Society. Towards a New Modernity. London (UK): Sage Publications, 1992. [Google Scholar]
Betsch 2015
- Betsch C, Böhm R, Chapman GB. Using behavioral insights to increase vaccination policy effectiveness. Policy Insights from the Behavioral and Brain Sciences 2015;2(1):61-73. [Google Scholar]
Betsch 2018
- Betsch C, Schmid P, Heinemeier D, Korn L, Holtmann C, Böhm R. Beyond confidence: development of a measure assessing the 5C psychological antecedents of vaccination. PLOS One 2018;13(12):e0208601. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bevan 2007
- Bevan P. Researching wellbeing across the disciplines: some key intellectual problems and ways forward. In: Gough I, McGregor J, editors(s). Wellbeing in Developing Countries: From Theory to Research. Cambridge (UK): Cambridge University Press, 2007:283-315. [Google Scholar]
Bjornson 1997
- Bjornson GL, Scheifele DW, Gold R. Assessment of parent education methods for infant immunization. Canadian Journal of Public Health 1997;88(6):405-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bolam 1998
- Bolam A, Manandhar DS, Shrestha P, Ellis M, Costello AM. The effects of postnatal health education for mothers on infant care and family planning practices in Nepal: a randomised controlled trial. BMJ 1998;316(7134):805-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Booth 2013
- Booth A, Carroll C, Ilott I, Low LL, Cooper K. Desperately seeking dissonance: identifying the disconfirming case in qualitative evidence synthesis. Qualitative Health Research 2013;23(1):126-41. [DOI] [PubMed] [Google Scholar]
Bourdieu 1977
- Bourdieu P. Outline of a Theory of Practice. Cambridge (UK): Cambridge University Press, 1977. [Google Scholar]
Bourdieu 1984
- Bourdieu P. Distinction: A Social Critique of the Judgement of Taste. London (UK): Routledge, 1984. [Google Scholar]
Britten 2002
- Britten N, Campbell R, Pope C, Donovan J, Morgan M, Pill R. Using meta ethnography to synthesise qualitative research: a worked example. Journal of Health Services Research & Policy 2002;7(4):209-15. [DOI] [PubMed] [Google Scholar]
Britten 2012
- Britten N, Pope C. Medicine taking for asthma: a worked example of meta-ethnography. In: Hannes K, Lockwood C, editors(s). Synthesizing Qualitative Research: Choosing the Right Approach. Chichester (UK): Wiley-Blackwell BMJ Books, 2012:41–58. [Google Scholar]
Brown 2010
- Brown KF, Kroll JS, Hudson MJ, Ramsay M, Green J, Long SJ, et al. Factors underlying parental decisions about combination childhood vaccinations including MMR: a systematic review. Vaccine 2010;28(26):4235-48. [DOI] [PubMed] [Google Scholar]
Brown 2016
- Brown VB, Oluwatosin OA, Akinyemi JO, Adeyemo AA. Effects of community health nurse-led intervention on childhood routine immunization completion in primary health care centers in Ibadan, Nigeria. Journal of Community Health 2016;41(2):265-73. [DOI] [PubMed] [Google Scholar]
Brugha 1996
- Brugha RF, Kevany JP. Maximizing immunization coverage through home visits: a controlled trial in an urban area of Ghana. Bulletin of the World Health Organization 1996;74(5):517-24. [PMC free article] [PubMed] [Google Scholar]
Callreus 2010
- Callreus T. Perceptions of vaccine safety in a global context. Acta Paediatrica 2010;99(2):166-71. [DOI] [PubMed] [Google Scholar]
Campbell 1994
- Campbell JR, Szilagyi PG, Rodewald LE, Doane C, Roghmann KJ. Patient-specific reminder letters and pediatric well-child-care show rates. Clinical Pediatrics 1994;33(5):268-72. [DOI] [PubMed] [Google Scholar]
Campbell 2011
- Campbell R, Pound P, Morgan M, Daker-White G, Britten N, Pill R, et al. Evaluating meta-ethnography: systematic analysis and synthesis of qualitative research. Health Technology Assessment 2011;15(43):1-164. [DOI] [PubMed] [Google Scholar]
Candy 2011
- Candy B, King M, Jones L, Oliver S. Using qualitative synthesis to explore heterogeneity of complex interventions. BMC Medical Research Methodology 2011;11:124. [DOI] [PMC free article] [PubMed] [Google Scholar]
Carlsen 2016
- Carlsen B, Glenton C. The swine flu vaccine, public attitudes, and researcher interpretations: a systematic review of qualitative research. BMC Health Services Research 2016;16:203. [DOI] [PMC free article] [PubMed] [Google Scholar]
CASP 2018
- Critical Appraisal Skills Programme (CASP). CASP Qualitative Checklist: 10 questions to help you make sense of a qualitative research. Available at: casp-uk.b-cdn.net/wp-content/uploads/2018/03/CASP-Qualitative-Checklist-2018_fillable_form.pdf (accessed 5 August 2019).
CDC 1999
- Centers for Disease Control and Prevention (CDC). Ten great public health achievements — United States, 1900-1999. Morbidity and Mortality Weekly Report 1999;48(12):241-3. [PubMed] [Google Scholar]
CDC 2012
- Centers for Disease Control and Prevention (CDC). Evaluation of vaccination recall letter system for Medicaid-enrolled children aged 19-23 months — Montana, 2011. Morbidity and Mortality Weekly Report 2012;61(40):811-5. [PubMed] [Google Scholar]
Colvin 2018
- Colvin CJ, Garside R, Wainwright M, Munthe-Kaas H, Glenton C, Bohren MA, et al. Applying GRADE-CERQual to qualitative evidence synthesis findings - paper 4: how to assess coherence. Implementation Science 2018;13(Suppl 1):13. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cooper 2019
- Cooper S, Okeibunor JC, Wiyeh A, Wiysonge CS. Knowledge advances and gaps on the demand side of vaccination. Lancet Infectious Diseases 2019;19(1):13-5. [DOI] [PubMed] [Google Scholar]
Corben 2016
- Corben P, Leask J. To close the childhood immunization gap, we need a richer understanding of parents' decision-making. Human Vaccines & Immunotherapeutics 2016;12(12):3168-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
Crawford 1980
- Crawford R. Healthism and the medicalization of everyday life. International Journal of Health Services 1980;10(3):365-88. [DOI] [PubMed] [Google Scholar]
Crawford 2004
- Crawford R. Risk ritual and the management of control and anxiety in medical culture. Health (London) 2004;8(4):505-28. [DOI] [PubMed] [Google Scholar]
Dabbagh 2018
- Dabbagh A, Laws RL, Steulet C, Dumolard L, Gacic-Dobo M, Mulders M, et al. Progress toward regional measles elimination — worldwide, 2000–2017. Morbidity and Mortality Weekly Report 2018;67:1323–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Daley 2002
- Daley MF, Steiner JF, Brayden R M, Xu S, Morrison S, Kempe A. Immunization registry-based recall for a new vaccine. Ambulatory Pediatrics 2002;2(6):438-43. [DOI] [PubMed] [Google Scholar]
Daley 2004a
- Daley MF, Steiner JF, Kempe A, Beaty BL, Pearson KA, Jones JS, et al. Quality improvement in immunization delivery following an unsuccessful immunization recall. Ambulatory Pediatrics 2004;4(3):217-23. [DOI] [PubMed] [Google Scholar]
Daley 2004b
- Daley MF, Barrow J, Pearson K, Crane LA, Gao D, Stevenson JM, et al. Identification and recall of children with chronic medical conditions for influenza vaccination. Pediatrics 2004;113(1):e26-33. [DOI] [PubMed] [Google Scholar]
de Figueiredo 2016
- Figueiredo A, Johnston IG, Smith DM, Agarwal S, Larson HJ, Jones NS. Forecasted trends in vaccination coverage and correlations with socioeconomic factors: a global time-series analysis over 30 years. Lancet Global Health 2016;4(10):e726-35. [DOI] [PubMed] [Google Scholar]
Dicko 2011
- Dicko A, Toure SO, Traore M, Sagara I, Toure OB, Sissoko MS, et al. Increase in EPI vaccines coverage after implementation of intermittent preventive treatment of malaria in infant with sulfadoxine-pyrimethamine in the district of Kolokani, Mali: results from a cluster randomized control trial. BMC Public Health 2011;11:573. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dini 2000
- Dini EF, Linkins RW, Sigafoos J. The impact of computer-generated messages on childhood immunization coverage. American Journal of Preventive Medicine 2000;18(2):132-9. [DOI] [PubMed] [Google Scholar]
Djibuti 2009
- Djibuti M, Gotsadze G, Zoidze A, Mataradze G, Esmail LC, Kohler JC. The role of supportive supervision on immunization program outcome - a randomized field trial from Georgia. BMC International Health and Human Rights 2009;9(Suppl 1):S11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dombkowski 2012
- Dombkowski KJ, Harrington LB, Dong S, Clark SJ. Seasonal influenza vaccination reminders for children with high-risk conditions: a registry-based randomized trial. American Journal of Preventive Medicine 2012;42(1):71-5. [DOI] [PubMed] [Google Scholar]
Dombkowski 2014
- Dombkowski KJ, Costello LE, Harrington LB, Dong S, Kolasa M, Clark SJ. Age-specific strategies for immunization reminders and recalls: a registry-based randomized trial. American Journal of Preventive Medicine 2014;47(1):1-8. [DOI] [PubMed] [Google Scholar]
Dube 2013
- Dube E, Laberge C, Guay M, Bramadat P, Roy R, Bettinger J. Vaccine hesitancy: an overview. Human Vaccines & Immunotherapeutics 2013;9(8):1763-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dube 2015
- Dube E, Vivion M, MacDonald NE. Vaccine hesitancy, vaccine refusal and the anti-vaccine movement: influence, impact and implications. Expert Review of Vaccines 2015;14(1):99-117. [DOI] [PubMed] [Google Scholar]
Dube 2018
- Dube E, Gagnon D, MacDonald N, Bocquier A, Peretti-Watel P, Verger P. Underlying factors impacting vaccine hesitancy in high income countries: a review of qualitative studies. Expert Review of Vaccines 2018;17(11):989-1004. [DOI] [PubMed] [Google Scholar]
EPOC 2017
- Cochrane Effective Practice and Organisation of Care (EPOC). EPOC Qualitative Evidence Syntheses guidance on when to sample and how to develop a purposive sampling frame. EPOC Resources for review authors; 2017. Available at: epoc.cochrane.org/resources/epoc-resources-review-authors (accessed 01 March 2019).
Falagas 2008
- Falagas ME, Zarkadoulia E. Factors associated with suboptimal compliance to vaccinations in children in developed countries: a systematic review. Current Medical Research and Opinion 2008;24(6):1719-41. [DOI] [PubMed] [Google Scholar]
Favin 2012
- Favin M, Steinglass R, Fields R, Banerjee K, Sawhney M. Why children are not vaccinated: a review of the grey literature. International Health 2012;4(4):229-38. [DOI] [PubMed] [Google Scholar]
Feemster 2013
- Feemster KA. Overview: special focus vaccine acceptance. Human Vaccines and Immunotherapeutics 2013;9(8):1752-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Feldstein 2017
- Feldstein LR, Mariat S, Gacic-Dobo M, Diallo S, Conklin L, Wallace A. Global routine vaccination coverage, 2016. Weekly Epidemiological Record 2017;92(46):701-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ferson 1995
- Ferson MJ, Fitzsimmons G, Christie D, Woollett H. School health nurse interventions to increase immunisation uptake in school entrants. Public Health 1995;109(1):25-9. [DOI] [PubMed] [Google Scholar]
Fine 2011
- Fine P, Eames K, Heymann DL. "Herd immunity": a rough guide. Clinical Infectious Diseases 2011;52(7):911-6. [DOI] [PubMed] [Google Scholar]
Finfgeld‐Connett 2014
- Finfgeld-Connett D. Metasynthesis findings: potential versus reality. Qualitative Health Research 2014;24(11):1581-91. [DOI] [PubMed] [Google Scholar]
Foucault 1977
- Foucault M. Discipline and Punish: The Birth of the Prison. London (UK): Penguin, 1977. [Google Scholar]
Foucault 1989
- Foucault M. The Birth of the Clinic: An Archaeology of Medical Perception. London (UK): Routledge, 1989. [Google Scholar]
Foucault 1991
- Foucault M. Governmentality. In: Burchell G, Gordon C, Miller P, editors(s). The Foucault Effect: Studies in Governmentality. Hemel Hempstead (UK): Harvester Wheatsheaf, 1991. [Google Scholar]
France 2014
- France EF, Ring N, Thomas R, Noyes J, Maxwell M, Jepson R. A methodological systematic review of what's wrong with meta-ethnography reporting. BMC Medical Research Methodology 2014;14:119. [DOI] [PMC free article] [PubMed] [Google Scholar]
France 2019
- France EF, Cunningham M, Ring N, Uny I, Duncan EA, Jepson RG, et al. Improving reporting of meta-ethnography: the eMERGe reporting guidance. Journal of Advanced Nursing 2019;75(5):1126-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
Garside 2008
- Garside R, Britten N, Stein K. The experience of heavy menstrual bleeding: a systematic review and meta-ethnography of qualitative studies. Journal of Advanced Nursing 2008;63(6):550-62. [DOI] [PubMed] [Google Scholar]
Giddens 1990
- Giddens A. The Consequences of Modernity. Cambridge (UK): Polity Press, 1990. [Google Scholar]
Giddens 1991
- Giddens A. Modernity and Self-identity: Self and Society in the Late Modern Age. Cambridge (UK): Polity Press, 1991. [Google Scholar]
Glenton 2020a
- Glenton C, Bohren MA, Downe S, Paulsen EJ, Lewin S, on behalf of Effective Practice and Organisation of Care (EPOC). EPOC Qualitative Evidence Synthesis: Protocol and review template. Version 1.1; 2020. Available at https://zenodo.org/record/5211193#.YVr0wZpBw2w.
Glenton 2020b
- Glenton C, Nilsen ES, Sporstøl Fønhus M, on behalf of Cochrane Norway and Effective Practice and Organisation of Care (EPOC). How to write a plain language summary of a Cochrane EPOC Qualitative Evidence Synthesis. Version 2; 2020. Available at: epoc.cochrane.org/resources/epoc-resources-review-authors#protocol.
Godlee 2011
- Godlee F, Smith J, Marcovitch H. Wakefield's article linking MMR vaccine and autism was fraudulent. BMJ 2011;342:c7452. [DOI] [PubMed] [Google Scholar]
Green 2004
- Green G, Thorogood N. Qualitative Methods for Health Research. London (UK): Sage, 2004. [Google Scholar]
Haji 2016
- Haji A, Lowther S, Ngan'ga Z, Gura Z, Tabu C, Sandhu H, et al. Reducing routine vaccination dropout rates: evaluating two interventions in three Kenyan districts, 2014. BMC Public Health 2016;16:152. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hambidge 2009
- Hambidge SJ, Phibbs SL, Chandramouli V, Fairclough D, Steiner JF. A stepped intervention increases well-child care and immunization rates in a disadvantaged population. Pediatrics 2009;124(2):455-64. [DOI] [PubMed] [Google Scholar]
Hannes 2013
- Hannes K, Booth A, Harris J, Noyes J. Celebrating methodological challenges and changes: reflecting on the emergence and importance of the role of qualitative evidence in Cochrane reviews. Systematic Reviews 2013;2:84. [DOI] [PMC free article] [PubMed] [Google Scholar]
Harraway 1988
- Harraway D. Situated knowledges: the science question in feminism and the privilege of partial perspective. Feminist Studies 1988;14(3):575-599. [Google Scholar]
Harris 2018
- Harris JL, Booth A, Cargo M, Hannes K, Harden A, Flemming K, et al. Cochrane Qualitative and Implementation Methods Group guidance series - paper 2: methods for question formulation, searching, and protocol development for qualitative evidence synthesis. Journal of Clinical Epidemiology 2018;97:39-48. [DOI] [PubMed] [Google Scholar]
Hickler 2015
- Hickler B, Guirguis S, Obregon R. Special issue on vaccine hesitancy. Vaccine 2015;33(34):4155-6. [DOI] [PubMed] [Google Scholar]
Hickler 2017
- Hickler B, MacDonald NE, Senouci K, Schuh HB. Efforts to monitor global progress on individual and community demand for immunization: development of definitions and indicators for the Global Vaccine Action Plan strategic objective 2. Vaccine 2017;35(28):3515-9. [DOI] [PubMed] [Google Scholar]
Hill 2015
- Hill HA, Elam-Evans LD, Yankey D, Singleton JA, Kolasa M. National, state, and selected local area vaccination coverage among children aged 19-35 months - United States, 2014. Morbidity and Mortality Weekly Report 2015;64(33):889-96. [DOI] [PubMed] [Google Scholar]
Houghton 2020
- Houghton C, Dowling M, Meskell P, Hunter A, Gardner H, Conway A, et al. Factors that impact on recruitment to randomised trials in health care: a qualitative evidence synthesis. Cochrane Database of Systematic Reviews 2020, Issue 10. Art. No: MR000045. [DOI: 10.1002/14651858.MR000045.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hu 2017
- Hu Y, Chen Y, Wang Y, Song Q, Li Q. Prenatal vaccination education intervention improves both the mothers' knowledge and children's vaccination coverage: evidence from a randomized controlled trial from eastern China. Human Vaccines & Immunotherapeutics 2017;13(6):1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hull 2017
- Hull BP, Hendry AJ, Dey A, Beard FH, Brotherton JM, McIntyre PB. Immunisation coverage annual report, 2014. Communicable Diseases Intelligence Quarterly Report 2017;41(1):E68-e90. [DOI] [PubMed] [Google Scholar]
Irigoyen 2006
- Irigoyen MM, Findley S, Wang D, Chen S, Chimkin F, Pena O, et al. Challenges and successes of immunization registry reminders at inner-city practices. Ambulatory Pediatrics 2006;6(2):100-4. [DOI] [PubMed] [Google Scholar]
Jaca 2018
- Jaca A, Mathebula L, Iweze A, Pienaar E, Wiysonge CS. A systematic review of strategies for reducing missed opportunities for vaccination. Vaccine 2018;36(21):2921-7. [DOI] [PubMed] [Google Scholar]
Jackson 2008
- Jackson C, Cheater FM, Reid I. A systematic review of decision support needs of parents making child health decisions. Health Expectations 2008;11(3):232-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jackson 2011
- Jackson C, Cheater FM, Harrison W, Peacock R, Bekker H, West R, et al. Randomised cluster trial to support informed parental decision-making for the MMR vaccine. BMC Public Health 2011;11:475. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jacobson‐Vann 2018
- Jacobson-Vann JC, Jacobson RM, Coyne-Beasley T, Asafu-Adjei JK, Szilagyi PG. Patient reminder and recall interventions to improve immunization rates. Cochrane Database of Systematic Reviews 2018, Issue 1. Art. No: CD003941. [DOI: 10.1002/14651858.CD003941.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Karafillakis 2017
- Karafillakis E, Larson HJ. The benefit of the doubt or doubts over benefits? A systematic literature review of perceived risks of vaccines in European populations. Vaccine 2017;35(37):4840-50. [DOI] [PubMed] [Google Scholar]
Karimi‐Shahanjarini 2019
- Karimi-Shahanjarini A, Shakibazadeh E, Rashidian A, Hajimiri K, Glenton C, Noyes J, et al. Barriers and facilitators to the implementation of doctor?nurse substitution strategies in primary care: a qualitative evidence synthesis. Cochrane Database of Systematic Reviews 2019, Issue 4. Art. No: CD010412. [DOI: 10.1002/14651858.CD010412.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kaufman 2018
- Kaufman J, Ryan R, Walsh L, Horey D, Leask J, Robinson P, et al. Face-to-face interventions for informing or educating parents about early childhood vaccination. Cochrane Database of Systematic Reviews 2018, Issue 5. Art. No: CD010038. [DOI: 10.1002/14651858.CD010038.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kempe 2001
- Kempe A, Lowery NE, Pearson KA, Renfrew BL, Jones JS, Steiner JF, et al. Immunization recall: effectiveness and barriers to success in an urban teaching clinic. Journal of Pediatrics 2001;139(5):630-5. [DOI] [PubMed] [Google Scholar]
Kempe 2005
- Kempe A, Daley MF, Barrow J, Allred N, Hester N, Beaty BL, et al. Implementation of universal influenza immunization recommendations for healthy young children: results of a randomized, controlled trial with registry-based recall. Pediatrics 2005;115(1):146-54. [DOI] [PubMed] [Google Scholar]
Kemper 1993
- Kemper KJ, Goldberg H. Do computer-generated reminder letters improve the rate of influenza immunization in an urban pediatric clinic? American Journal of the Diseases of Children 1993;147(7):717-8. [DOI] [PubMed] [Google Scholar]
Lane 2018
- Lane S, MacDonald NE, Marti M, Dumolard L. Vaccine hesitancy around the globe: analysis of three years of WHO/UNICEF Joint Reporting Form data - 2015-2017. Vaccine 2018;36(26):3861-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
Larson 2011
- Larson HJ, Cooper LZ, Eskola J, Katz SL, Ratzan S. Addressing the vaccine confidence gap. Lancet 2011;378(9790):526-35. [DOI] [PubMed] [Google Scholar]
Larson 2014
- Larson HJ, Jarrett C, Eckersberger E, Smith DM, Paterson P. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: a systematic review of published literature, 2007-2012. Vaccine 2014;32(19):2150-9. [DOI] [PubMed] [Google Scholar]
Larson 2018a
- Larson H. The state of vaccine confidence. Lancet 2018;392(10161):2244-6. [DOI] [PubMed] [Google Scholar]
Larson 2018b
- Larson HJ, Clarke RM, Jarrett C, Eckersberger E, Levine Z, Schulz WS, et al. Measuring trust in vaccination: a systematic review. Human Vaccines & Immunotherapeutics 2018;14(7):1599-609. [DOI] [PMC free article] [PubMed] [Google Scholar]
LeBaron 1998
- LeBaron CW, Starnes D, Dini EF, Chambliss JW, Chaney M. The impact of interventions by a community-based organization on inner-city vaccination coverage: Fulton County, Georgia, 1992-1993. Archives of Pediatrics & Adolescent Medicine 1998;152(4):327-32. [DOI] [PubMed] [Google Scholar]
LeBaron 2004
- LeBaron CW, Starnes DM, Rask KJ. The impact of reminder-recall interventions on low vaccination coverage in an inner-city population. Archives of Pediatrics & Adolescent Medicine 2004;158(3):255-61. [DOI] [PubMed] [Google Scholar]
Lemstra 2011
- Lemstra M, Rajakumar D, Thompson A, Moraros J. The effectiveness of telephone reminders and home visits to improve measles, mumps and rubella immunization coverage rates in children. Paediatrics & Child Health 2011;16(1):e1-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lewin 2011
- Lewin S, Hill S, Abdullahi LH, Castro Freire SB, Bosch-Capblanch X, Glenton C, et al. 'Communicate to vaccinate' (COMMVAC). Building evidence for improving communication about childhood vaccinations in low- and middle-income countries: protocol for a programme of research. Implementation Science 2011;6:125. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lewin 2018
- Lewin S, Booth A, Glenton C, Munthe-Kaas H, Rashidian A, Wainwright M, et al. Applying GRADE-CERQual to qualitative evidence synthesis findings: introduction to the series. Implementation Science 2018;13(Suppl 1):2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lieu 1997
- Lieu TA, Black SB, Ray P, Schwalbe JA, Lewis EM, Lavetter A, et al. Computer-generated recall letters for underimmunized children: how cost-effective? Pediatric Infectious Disease Journal 1997;16(1):28-33. [DOI] [PubMed] [Google Scholar]
Lieu 1998
- Lieu TA, Capra AM, Makol J, Black SB, Shinefield HR. Effectiveness and cost-effectiveness of letters, automated telephone messages, or both for underimmunized children in a health maintenance organization. Pediatrics 1998;101(4):E3. [DOI] [PubMed] [Google Scholar]
Lindbladh 2003
- Lindbladh E, Lyttkens CH. Polarization in the reaction to health risk information: a question of social positions? Risk Analysis 2003;23(4):841-55. [DOI] [PubMed] [Google Scholar]
Linkins 1994
- Linkins RW, Dini EF, Watson G, Patriarca PA. A randomized trial of the effectiveness of computer-generated telephone messages in increasing immunization visits among preschool children. Archives of Pediatrics & Adolescent Medicine 1994;148(9):908-14. [DOI] [PubMed] [Google Scholar]
MacDonald 2015
- MacDonald NE. Vaccine hesitancy: definition, scope and determinants. Vaccine 2015;33(34):4161-4. [DOI] [PubMed] [Google Scholar]
Machingaidze 2013a
- Machingaidze S, Wiysonge CS, Hussey GD. Strengthening the expanded programme on immunization in Africa: looking beyond 2015. PLoS Medicine 2013;10(3):e1001405. [DOI] [PMC free article] [PubMed] [Google Scholar]
Machingaidze 2013b
- Machingaidze S, Rehfuess E, Kries R, Hussey GD, Wiysonge CS. Understanding interventions for improving routine immunization coverage in children in low- and middle-income countries: a systematic review protocol. Systematic Reviews 2013;2:106. [DOI] [PMC free article] [PubMed] [Google Scholar]
Malpass 2009
- Malpass A, Shaw A, Sharp D, Walter F, Feder G, Ridd M, et al. "Medication career" or "moral career"? The two sides of managing antidepressants: a meta-ethnography of patients' experience of antidepressants. Social Science & Medicine 2009;68(1):154-68. [DOI] [PubMed] [Google Scholar]
Maluccio 2004
- Maluccio J, Flores R. Impact evaluation of a conditional cash transfer program: the Nicaraguan Red de Protección Social. Food Consumption and Nutrition Division Discussion Paper No. 184; July 2004. Available at: ebrary.ifpri.org/utils/getfile/collection/p15738coll2/id/76633/filename/76634.pdf.
Mason 2000
- Mason BW, Donnelly PD. Targeted mailing of information to improve uptake of measles, mumps, and rubella vaccine: a randomised controlled trial. Communicable Disease and Public Health 2000;3(1):67-8. [PubMed] [Google Scholar]
Mills 2005
- Mills E, Jadad AR, Ross C, Wilson K. Systematic review of qualitative studies exploring parental beliefs and attitudes toward childhood vaccination identifies common barriers to vaccination. Journal of Clinical Epidemiology 2005;58(11):1081-8. [DOI] [PubMed] [Google Scholar]
Morris 2004
- Morris S S, Flores R, Olinto P, Medina J M. Monetary incentives in primary health care and effects on use and coverage of preventive health care interventions in rural Honduras: cluster randomised trial. Lancet 2004;364(9450):2030-7. [DOI] [PubMed] [Google Scholar]
Munabi‐Babigumira 2017
- Munabi-Babigumira S, Glenton C, Lewin S, Fretheim A, Nabudere H. Factors that influence the provision of intrapartum and postnatal care by skilled birth attendants in low- and middle-income countries: a qualitative evidence synthesis. Cochrane Database of Systematic Reviews 2017, Issue 11. Art. No: CD011558. [DOI: 10.1002/14651858.CD011558.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Nadeau 2016
- Nadeau JA, McNutt LA, Shaw J. Vaccination coverage rates and factors associated with incomplete vaccination or exemption among school-age children based in public schools in New York State. Journal of the American Medical Association (JAMA) Pediatrics 2016;170(11):1104-7. [DOI] [PubMed] [Google Scholar]
Nagaraj 2006
- Nagaraj A. Does qualitative synthesis of anecdotal evidence with that from scientific research help in understanding public health issues: a review of low MMR uptake. European Journal of Public Health 2006;16(1):85-8. [DOI] [PubMed] [Google Scholar]
Nagel 1986
- Nagel T. The View from Nowhere. New York (NY): Oxford University Press, 1986. [Google Scholar]
NASEM 2021
- National Academies of Sciences, Engineering, and Medicine. Strategies for Building Confidence in the COVID-19 Vaccines. Washington (DC): National Academies Press, 2021. [PubMed] [Google Scholar]
Noblit 1988
- Noblit GW, Hare RD. Meta-ethnography: Synthesizing Qualitative Studies. London (UK): Sage, 1988. [Google Scholar]
Noblit 2016
- Noblit G. How qualitative (or interpretive or critical) is qualitative synthesis and what we can do about this? A public lecture by Professor George W. Noblit, University of North Carolina at Chapel Hill; June 2016. Available at emergeproject.org/wp-content/uploads/2016/09/How-qualitative.pdf.
Noblit 2019
- Noblit G. Meta-ethnography in Education. Oxford (UK): Oxford University Press, 2019. [Google Scholar]
Noyes 2018
- Noyes J, Booth A, Flemming K, Garside R, Harden A, Lewin S, et al. Cochrane Qualitative and Implementation Methods Group guidance series - paper 3: methods for assessing methodological limitations, data extraction and synthesis, and confidence in synthesized qualitative findings. Journal of Clinical Epidemiology 2018;97:49-58. [DOI] [PubMed] [Google Scholar]
NVAC 2015
- National Vaccine Advisory Committee. Assessing the state of vaccine confidence in the United States: recommendations from the National Vaccine Advisory Committee: approved by the National Vaccine Advisory Committee on June 10, 2015. Public Health Reports 2015;130(6):573-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
Oeffinger 1992
- Oeffinger KC, Roaten SP, Hitchcock MA, Oeffinger PK. The effect of patient education on pediatric immunization rates. Journal of Family Practice 1992;35(3):288-93. [PubMed] [Google Scholar]
Omer 2009
- Omer SB, Salmon DA, Orenstein WA, deHart MP, Halsey N. Vaccine refusal, mandatory immunization, and the risks of vaccine-preventable diseases. New England Journal of Medicine 2009;360(19):1981-8. [DOI] [PubMed] [Google Scholar]
Owais 2011
- Owais A, Hanif B, Siddiqui AR, Agha A, Zaidi AK. Does improving maternal knowledge of vaccines impact infant immunization rates? A community-based randomized-controlled trial in Karachi, Pakistan. BMC Public Health 2011;11:239. [DOI] [PMC free article] [PubMed] [Google Scholar]
Oyo‐Ita 2016
- Oyo-Ita A, Wiysonge CS, Oringanje C, Nwachukwu CE, Oduwole O, Meremikwu MM. Interventions for improving coverage of childhood immunisation in low- and middle-income countries. Cochrane Database of Systematic Reviews 2016, Issue 7. Art. No: CD008145. [DOI: 10.1002/14651858.CD008145.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Pandey 2007
- Pandey P, Sehgal AR, Riboud M, Levine D, Goyal M. Informing resource-poor populations and the delivery of entitled health and social services in rural India: a cluster randomized controlled trial. Journal of the American Medical Association 2007;298(16):1867-75. [DOI] [PubMed] [Google Scholar]
Pearce 2015
- Pearce A, Marshall H, Bedford H, Lynch J. Barriers to childhood immunisation: findings from the longitudinal study of Australian children. Vaccine 2015;33(29):3377-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
Peretti‐Watel 2015
- Peretti-Watel P, Larson HJ, Ward JK, Schulz WS, Verger P. Vaccine hesitancy: clarifying a theoretical framework for an ambiguous notion. PLoS Current Outbreaks 2015;7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pound 2005
- Pound P, Britten N, Morgan M, Yardley L, Pope C, Daker-White G, et al. Resisting medicines: a synthesis of qualitative studies of medicine taking. Social Science & Medicine 2005;61(1):133-55. [DOI] [PubMed] [Google Scholar]
Quinlivan 2003
- Quinlivan JA, Box H, Evans SF. Postnatal home visits in teenage mothers: a randomised controlled trial. Lancet 2003;361(9361):893-900. [DOI] [PubMed] [Google Scholar]
Rainey 2011
- Rainey JJ, Watkins M, Ryman TK, Sandhu P, Bo A, Banerjee K. Reasons related to non-vaccination and under-vaccination of children in low and middle income countries: findings from a systematic review of the published literature, 1999-2009. Vaccine 2011;29(46):8215-21. [DOI] [PubMed] [Google Scholar]
Roberts 2002
- Roberts KA, Dixon-Woods M, Fitzpatrick R, Abrams KR, Jones DR. Factors affecting uptake of childhood immunisation: a Bayesian synthesis of qualitative and quantitative evidence. Lancet 2002;360(9345):1596-9. [DOI] [PubMed] [Google Scholar]
Robertson 2013
- Robertson L, Mushati P, Eaton JW, Dumba L, Mavise G, Makoni J, et al. Effects of unconditional and conditional cash transfers on child health and development in Zimbabwe: a cluster-randomised trial. Lancet 2013;381(9874):1283-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rodewald 1999
- Rodewald LE, Szilagyi PG, Humiston SG, Barth R, Kraus R, Raubertas RF. A randomized study of tracking with outreach and provider prompting to improve immunization coverage and primary care. Pediatrics 1999;103(1):31-8. [DOI] [PubMed] [Google Scholar]
Saeterdal 2014
- Saeterdal I, Lewin S, Austvoll-Dahlgren A, Glenton C, Munabi-Babigumira S. Interventions aimed at communities to inform and/or educate about early childhood vaccination. Cochrane Database of Systematic Reviews 2014, Issue 11. Art. No: CD010232. [DOI: 10.1002/14651858.CD010232.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Saitoh 2013
- Saitoh A, Nagata S, Saitoh A, Tsukahara Y, Vaida F, Sonobe T, et al. Perinatal immunization education improves immunization rates and knowledge: a randomized controlled trial. Preventive Medicine 2013;56(6):398-405. [DOI] [PMC free article] [PubMed] [Google Scholar]
Saitoh 2017
- Saitoh A, Saitoh A, Sato I, Shinozaki T, Kamiya H, Nagata S. Effect of stepwise perinatal immunization education: a cluster-randomized controlled trial. Vaccine 2017;35(12):1645-51. [DOI] [PubMed] [Google Scholar]
Sandelowski 2007
- Sandelowski M, Barroso J. Handbook for Synthesizing Qualitative Research. New York (NY): Springer Publishing Company, 2007. [Google Scholar]
Scheifele 2014
- Scheifele DW, Halperin SA, Bettinger JA. Childhood immunization rates in Canada are too low: UNICEF. Paediatrics and Child Health 2014;19(5):237-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Schuster 2015
- Schuster M, Eskola J, Duclos P. Review of vaccine hesitancy: rationale, remit and methods. Vaccine 2015;33(34):4157-60. [DOI] [PubMed] [Google Scholar]
Schutz 1971
- Schutz A. Collected Papers. Vol. 1. The Hague (Netherlands): Martinus Nijhoff, 1971. [Google Scholar]
Scott 1985
- Scott J. Weapons of the Weak. New Haven (CT): Yale University Press, 1985. [Google Scholar]
Soljak 1987
- Soljak MA, Handford S. Early results from the Northland immunisation register. New Zealand Medical Journal 1987;100(822):244-6. [PubMed] [Google Scholar]
Stehr‐Green 1993
- Stehr-Green PA, Dini EF, Lindegren ML, Patriarca PA. Evaluation of telephoned computer-generated reminders to improve immunization coverage at inner-city clinics. Public Health Reports 1993;108(4):426-30. [PMC free article] [PubMed] [Google Scholar]
Sturm 2005
- Sturm LA, Mays RM, Zimet GD. Parental beliefs and decision making about child and adolescent immunization: from polio to sexually transmitted infections. Journal of Developmental and Behavioral Pediatrics 2005;26(6):441-52. [DOI] [PubMed] [Google Scholar]
Suk 2015
- Suk JE, Lopalco P, Pastore CL. Hesitancy, trust and individualism in vaccination decision-making. PLoS Current 2015;7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Suri 2011
- Suri H. Purposeful sampling in qualitative research synthesis. Qualitative Research Journal 2011;11(2):63-75. [Google Scholar]
Szilagyi 1992
- Szilagyi PG, Rodewald LE, Savageau J, Yoos L, Doane C. Improving influenza vaccination rates in children with asthma: a test of a computerized reminder system and an analysis of factors predicting vaccination compliance. Pediatrics 1992;90(6):871-5. [PubMed] [Google Scholar]
Tauil 2016
- Tauil MC, Sato AP, Waldman EA. Factors associated with incomplete or delayed vaccination across countries: a systematic review. Vaccine 2016;34(24):2635-43. [DOI] [PubMed] [Google Scholar]
Tollestrup 1991
- Tollestrup K, Hubbard BB. Evaluation of a follow-up system in a county health department's immunization clinic. American Journal of Preventive Medicine 1991;7(1):24-8. [PubMed] [Google Scholar]
United Nations 2016
- United Nations Department of Economic and Social Affairs. Leaving no one behind: the imperative of inclusive development. Report on the World Social Situation; 2016. Available at www.un.org/esa/socdev/rwss/2016/full-report.pdf.
Usman 2009
- Usman HR, Akhtar S, Habib F, Jehan I. Redesigned immunization card and center-based education to reduce childhood immunization dropouts in urban Pakistan: a randomized controlled trial. Vaccine 2009;27(3):467-72. [DOI] [PubMed] [Google Scholar]
Usman 2011
- Usman HR, Rahbar MH, Kristensen S, Vermund SH, Kirby RS, Habib F, et al. Randomized controlled trial to improve childhood immunization adherence in rural Pakistan: redesigned immunization card and maternal education. Tropical Medicine & International Health 2011;16(3):334-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
Vivier 2000
- Vivier PM, Alario AJ, O'Haire C, Dansereau LM, Jakum EB, Peter G. The impact of outreach efforts in reaching underimmunized children in a Medicaid managed care practice. Archives of Pediatrics & Adolescent Medicine 2000;154(12):1243-7. [DOI] [PubMed] [Google Scholar]
WHO 2013a
- World Health Organization. Global Vaccine Action Plan 2011-2020; February 2013. Available at www.who.int/immunization/global_vaccine_action_plan/GVAP_doc_2011_2020/en/.
WHO 2013b
- The SAGE Vaccine Hesitancy Working Group, WHO. What influences vaccine acceptance: a model of determinants of vaccine hesitancy; March 2013. Available at www.who.int/immunization/sage/meetings/2013/april/1_Model_analyze_driversofvaccineConfidence_22_March.pdf.
WHO 2014
- World Health Organization. Report of the SAGE Working Group on Vaccine Hesitancy; October 2014. Available at www.who.int/immunization/sage/meetings/2014/october/1_Report_WORKING_GROUP_vaccine_hesitancy_final.pdf.
WHO 2018a
- World Health Organization. 2018 Assessment Report of the Global Vaccine Action Plan. Strategic Advisory Group of Experts on Immunization; Draft version; September 2018. Available at www.who.int/immunization/sage/meetings/2018/october/2_Draft2018GVAP_Ass_Rep.pdf?ua=1.
WHO 2018b
- World Health Organization. Table 1: Summary of WHO Position Papers - Recommendations for routine immunization (updated August 2018). http://www.who.int/immunization/policy/Immunization_routine_table1.pdf?ua=1 (accessed 25 August 2018).
WHO 2019
- World Health Organization. Ten threats to global health in 2019. www.who.int/emergencies/ten-threats-to-global-health-in-2019 (accessed 1 February 2019).
WHO 2021
- WHO. Data for action: achieving high uptake of COVID-19 vaccines; April 2021. Available at www.who.int/publications/i/item/WHO-2019-nCoV-vaccination-demand-planning-2021.1 (accessed 17 June 2021).
Williams 2014
- Williams SE. What are the factors that contribute to parental vaccine-hesitancy and what can we do about it? Human Vaccines & Immunotherapeutics 2014;10(9):2584-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wood 1998
- Wood D, Halfon N, Donald-Sherbourne C, Mazel RM, Schuster M, Hamlin JS, et al. Increasing immunization rates among inner-city, African American children. A randomized trial of case management. Journal of the American Medical Association 1998;279(1):29-34. [DOI] [PubMed] [Google Scholar]
Yaqub 2014
- Yaqub O, Castle-Clarke S, Sevdalis N, Chataway J. Attitudes to vaccination: a critical review. Social Science and Medicine 2014;112:1-11. [DOI] [PubMed] [Google Scholar]
Young 1980
- Young SA, Halpin TJ, Johnson DA, Irvin JJ, Marks JS. Effectiveness of a mailed reminder on the immunization levels of infants at high risk of failure to complete immunizations. American Journal of Public Health 1980;70(4):422-4. [DOI] [PMC free article] [PubMed] [Google Scholar]


