Abstract
Background:
Individuals with multiple sclerosis (MS) frequently report sexual dysfunction, a condition that may result in low sexual satisfaction and decreased quality of life. Although sexual dysfunction is usually treated pharmacologically, physical therapists, especially those trained in pelvic floor physical therapy (PT), are well-equipped to address a variety of impairments that contribute to poor sexual function. The current evidence for effectiveness of PT interventions in improving sexual dysfunction, sexual satisfaction, and the emotional well-being aspect of quality of life was analyzed.
Methods:
The PubMed, CINAHL, and PEDro databases were searched through December 2019. Articles were included if participants had a clinical diagnosis of MS, reported sexual dysfunction or pain with intercourse, and had an intervention within the PT scope that addressed sexual dysfunction. Means and SDs were extracted from each study independently by two authors. Effect sizes (d) and 95% CIs were calculated within and across studies.
Results:
Eight studies met the inclusion criteria. Combined effects were significant and large across six studies for sexual function (d = 0.82, 95% CI, 0.57–1.06), moderate across seven studies for sexual satisfaction (d = 0.65, 95% CI, 0.43–0.87), and moderately large across two studies for emotional well-being (d = 0.78, 95% CI, 0.17–1.40). Between-group differences reached significance for sexual satisfaction (d = 0.29, 95% CI, 0.03–0.55).
Conclusions:
Sexual function, sexual satisfaction, and emotional well-being can all be effectively addressed with various PT interventions. Highly effective interventions included pelvic floor muscle training and mindfulness. Future research should compare PT interventions with non-PT controls to determine best practice in this population.
Keywords: Multiple sclerosis (MS), Sexual dysfunction, Sexual satisfaction
Multiple sclerosis (MS) is an inflammatory, neurodegenerative disease affecting nearly 1 million adults in the United States while they are at their peak of reproductive and sexual activity.1 Focal areas of demyelination and axonal degeneration throughout the central nervous system (CNS) result in disabling symptoms across numerous body systems.2,3 These symptoms may limit independence, restrict social activities, and decrease quality of life (QOL).4 Specific impairments may include fatigue, cognitive deficits, gait disorders, pain, depression, bladder dysfunction, and sexual dysfunction.3,5 Multiple sclerosis pathology and functional deficits are managed via a variety of treatments. Physical therapy (PT) interventions can address patient-specific impairments to reduce disability and improve QOL.5 However, sexual health is often overlooked both clinically and in research despite having a considerable effect on QOL.6
Multiple sclerosis affects sexual health in several ways. The literature classifies these effects as primary, secondary, and tertiary consequences. Primary consequences include impairments related to sexual health that are a direct result of MS-related lesions.7 For example, lesions to the thoracolumbar spinal cord may result in decreased somatic and autonomic outflow to the genital region, impairing muscle control and genital sensation.8 Secondary consequences involve the physical manifestations of MS that indirectly affect sexual health, such as fatigue, spasticity, and pain, which can contribute to decreased libido and difficulty reaching orgasm.7–10 Tertiary consequences encompass the psychological, social, and emotional factors that contribute to sexual experience, such as depression, anxiety, low self-esteem, altered marital roles, and changes in body image.7,8,11 Exacerbations of MS can increase the impact of primary and secondary consequences, thereby negatively affecting sexual function and sexual satisfaction, which may lead to decreases in emotional well-being, a tertiary consequence.12 This pattern demonstrates the profound impact that sexual dysfunction often has on QOL.6
Previous studies have shown that 40% to 80% of females and 50% to 90% of males with MS report sexual dysfunction,6,11,13 compared with 40% of females and 31% of males in the US general population.14,15 Tepavcevic et al6 found that females with MS most commonly reported decreased libido, difficulty achieving orgasm, and decreased lubrication. Males with MS reported decreased libido, incomplete erections, and premature ejaculation.6 The highly variable and intimate symptoms of sexual dysfunction are best assessed by patient-reported outcomes to extract levels of sexual function, sexual satisfaction, and emotional well-being.16 However, Lew-Starowicz and Rola17 found that more than 95% of study participants with MS had not discussed their sexual concerns with a health care professional. Patients' reluctance to talk about this prevalent and impactful topic means that health care providers must work harder to identify effective treatments and address the needs of people with MS.6
The lack of research regarding treatment of sexual dysfunction in individuals with MS necessitates looking to research in the general population for guidance. For example, erectile dysfunction in males can improve with mild- to moderate-intensity aerobic exercise.12 In females, sexual pain disorders such as vaginismus are successfully treated by physical therapists trained in pelvic floor rehabilitation.18 Physical therapy interventions such as electrical stimulation, biofeedback, muscle retraining exercises, counseling, and manual therapy can improve sexual functioning and satisfaction for those with sexual dysfunction without CNS diagnoses.19 Physical therapists contribute to the MS care team's effort to address the psychological aspects of sexual dysfunction, often reported as a decline in emotional well-being, as the literature supports a positive relationship between physical activity and reduced rates of depression, anger, and anxiety.20–23 A review of male and female sexual dysfunction by Rosenbaum19 concluded that physical therapists should be included on the health care team when addressing sexual health concerns. Although these studies focus on populations without CNS diagnoses, the shared outcome of improved sexual health in response to PT interventions shows promise.
Our question examines whether PT interventions are effective in treating sexual dysfunction in individuals with MS. Interventions of interest included treatment techniques within the PT scope of practice, including therapeutic exercise, pelvic floor muscle training (PFMT), mindfulness, and other modalities. No exclusions were made based on comparison group protocol, so controls could receive either no intervention or an alternative treatment. Outcomes of interest included patient-reported sexual function, sexual satisfaction, and emotional well-being. In the remainder of the article, PT intervention will refer to any intervention within the PT scope of practice, even when not administered by a physical therapist.
The null hypotheses state that PT interventions will not result in clinically or statistically significant improvements in sexual function, sexual satisfaction, or emotional well-being in individuals with MS. The alternative hypotheses state that PT interventions will provide clinically and statistically significant improvements in these variables. Evidence of the effectiveness of PT would bolster the argument for including physical therapists on the health care team of individuals with MS and concomitant sexual dysfunction.
Methods
Eligibility Criteria
This review followed the checklist of the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA).24 Articles were included based on the following criteria: 1) participants had a clinical diagnosis of MS; 2) participants reported sexual dysfunction or pain with intercourse; 3) the intervention of interest is within the PT scope of practice and is administered with the intention of treating sexual dysfunction; 4) the outcome measures were patient-reported and included metrics specifically addressing sexual function, sexual satisfaction, and/or emotional well-being; and 5) outcome data were reported for both experimental and control groups before and after the intervention. Articles were excluded if the studies 1) included pharmaceutical intervention as the primary intervention or 2) were less than level II evidence.25 Studies were assessed for quality based on the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) checklist and the Physiotherapy Evidence Database (PEDro) scale.26
Search Procedures
The literature search was performed in the PubMed, Cumulative Index to Nursing and Allied Health Literature (CINAHL), and PEDro databases. The following search terms were used independently and in combination: rehab, exercise, physical therapy, physiotherapy, activity, aerobic, electrother*, rehabilitation, multiple sclerosis, sexual dysfunction, and intercourse. Two researchers (A.G. and R.S.) independently assessed articles for relevance and adherence to inclusion criteria. A recursive search of the references for relevant articles was performed for completion. One researcher (R.S.) calculated the STROBE and PEDro scale scores, which were then verified by a second researcher (A.G.).
Patient-Reported Outcomes
Although patient-reported outcomes limit our ability to quantify objective changes in measures such as pelvic floor muscle function, the intimate and subjective nature of sexual dysfunction renders self-reported sexual experience paramount. The following standardized measures were most commonly reported in this systematic review: the Multiple Sclerosis Quality of Life–54 (MSQOL-54) and the Female Sexual Function Index (FSFI). The MSQOL-54 is validated for use in measuring health-related QOL and includes 12 multi-item scale scores that encompass health-related QOL issues specific to the MS population, including one scale on sexual function. Vickrey et al27 reported internal consistency reliability (Cronbach α) of 0.85 for the sexual function scale score. Test-retest reliability for sexual function was 0.94.28 Psychometrics for the FSFI were not available. Other published measures or tools generated for individual studies were also used.
Data Extraction
Data extracted from the selected articles included number of participants, average age, disease duration, and Expanded Disability Status Scale score.29 Variables of interest were assessed by the MSQOL-54, the FSFI, the Marital Satisfaction Inventory, or a study-specific Likert scale and were classified into one of three categories: first, the extent to which sexual dysfunction affected the participant's sexual function, such as ability to maintain lubrication until completion of sexual activity30; second, the degree of satisfaction with sexual activity or ability to reach orgasm27; and third, the measure of the participant's emotional well-being with emphasis on depression and anxiety.27
Means and SDs were extracted from each study when present. One study31 reported median and interquartile range values for sexual function and sexual satisfaction measures, which were converted to mean and SD estimates.28 Within-group and between-group effect sizes for sexual function, sexual satisfaction, and emotional well-being were calculated using Cohen's d statistic32 and 95% CIs. Depending on the Q heterogeneity statistic, a fixed-effect or a random-effects model was used to calculate grand effect sizes.
Results
Search Strategy
A search of electronic databases in December 2019 identified 134 studies. After removal of duplicates and filtering by title and abstract, 14 articles were assessed for eligibility using the inclusion and exclusion criteria. Seven studies were excluded for not meeting the eligibility criteria, the most restrictive of which were the use of relevant outcome measures and report of pre-post intervention data. One study was added after a recursive reference search. The final eight studies31,33–39 were confirmed by an outside reviewer (nonauthor) to have met all the eligibility criteria. Figure 1 shows the PRISMA diagram for study selection. Randomized controlled trials were assessed for quality using the PEDro scale26; all scored between 6 and 8 of 10, indicating moderate- to high-quality evidence. One cohort study was assessed using the STROBE checklist. Table S1, which is published in the online version of this article at ijmsc.org, presents a summary of the included studies. Of note, seven of the eight studies did not report the subtype of MS in participants.
Figure 1.
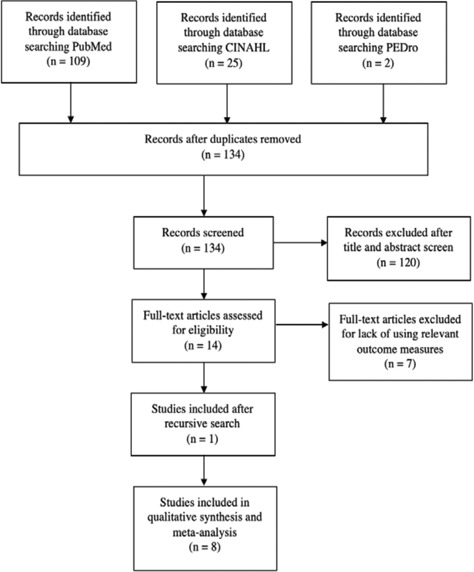
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-analyses) diagram outlining article selection
Study selection process according to PRISMA guidelines. CINAHL, Cumulative Index to Nursing and Allied Health Literature; PEDro, Physiotherapy Evidence Database.
Physical Activity
Three studies33–35 selected physical activity as their primary intervention, two33,34 of which used yoga. Ahmadi et al33 and Najafidoulatabad et al34 studied the effects of yoga on common impairments in individuals with MS. Najafidoulatabad et al34 held yoga sessions supervised by a physical therapist; and Ahmadi et al33 held yoga sessions supervised by both a neurologist and a physical therapist. Both studies randomized patients to either a yoga group or a control group that received no intervention. Ahmadi et al33 observed statistically significant improvements in Berg Balance Scale scores, gait speed, and MSQOL-54 subscores in the yoga group. Najafidoulatabad et al34 similarly found statistically significant improvements in physical activity and sexual function in the yoga group.
The third study was a randomized controlled trial analyzing the effects of aquatic aerobic exercise on QOL and mood in individuals with MS.35 Participants were randomly assigned to an aquatic aerobics group supervised by a physical therapist, or a control group that received no intervention. Outcomes of interest were MSQOL-54 and Profile of Mood States scores. The authors concluded that exercise may improve QOL, including sexual function, and mood in individuals with MS.
External Device
Two studies31,36 selected external devices as interventions of interest. In the first, Alexander et al36 examined the safety and efficacy of a clitoral vacuum suction device compared with vibratory stimulation when treating sexual dysfunction in females diagnosed as having MS (n = 20) or spinal cord injury (n = 11). The intervention was administered by a physical medicine and rehabilitation physician, and the FSFI score was the primary outcome. The suction device group demonstrated statistically significant improvements in the orgasm subscale and total FSFI scores, with improvements maintained at 16-week follow-up. The vibratory stimulation group also demonstrated statistically significant improvements in the orgasm subscale; however, these results were not maintained at 16-week follow-up.
In the second study, Lúcio et al31 studied the effectiveness of PFMT interventions, administered by a physical therapist, in treating sexual dysfunction in females with MS. Participants were randomly allocated into one of three groups: PFMT with electromyography biofeedback and intravaginal neuromuscular electrostimulation (NMES), PFMT with electromyography biofeedback and transcutaneous tibial nerve stimulation, or PFMT with electromyography biofeedback and sham NMES, which served as a control. Outcomes included pelvic floor muscle function and the FSFI score. After the intervention, all three groups demonstrated statistically significant improvements in total FSFI score, including the sexual satisfaction subscore. However, only those who received intravaginal NMES demonstrated statistically significant improvement in the FSFI subscales of pain, desire, and orgasm as well as pelvic floor muscle function.
Cognitive Therapy
Three studies37–39 used forms of cognitive therapy to address sexual dysfunction. Mosalanejad et al37 examined the effects of PFMT and mindfulness on sexual function in females with MS over 8 weeks, administered by a neurologist and physical therapist. Participants were randomly assigned to one of three intervention groups: PFMT alone, mindfulness alone, or PFMT and mindfulness combined. The mindfulness intervention included body scan meditation and diaphragmatic breathing exercises. The FSFI tracked changes in sexual function and demonstrated statistically significant improvements within all three groups. No significant differences were found between groups.
Foley et al38 and Hocaloski et al39 studied how psychoeducational counseling affects sexual dysfunction. Foley et al38 conducted their study on couples experiencing sexual dysfunction, where one partner had been diagnosed as having MS. After collecting baseline data, each couple entered a 2-month waiting period before starting the intervention. Counseling treatment consisted of education about the nature of sexual dysfunction, body mapping, and strategies for communicating with a sexual partner, administered by a psychologist. Due to the individuality of each relationship, this allowed each couple to serve as their own control. The Marital Satisfaction Inventory was the primary outcome measure. Statistically significant improvements were noted in Marital Satisfaction Inventory scores after the intervention, suggesting that counseling may enhance communication and improve problems with sexuality and intimacy. Hocaloski et al39 included females with either MS (n = 6) or spinal cord injury (n = 1) with sexual dysfunction. Participants received individual education on sexual dysfunction, as well as group mindfulness-based therapy that included body mapping, exploring sexual beliefs and myths, and engaging in a daily meditation practice. These interventions were administered by a registered nurse specializing in sexual health rehabilitation and a registered clinical counselor. Changes in sexual function were tracked using the FSFI, and results showed that improvement of sexual functioning was statistically significant, with a very large effect size. This finding suggests that group counseling with mindfulness-based therapy may be beneficial for women with MS or spinal cord injury in improving sexual function.
Data Analysis
Within- and between-group analyses were performed for each of the three outcomes of interest (Figures S1 and S2). Effect sizes and 95% CIs were calculated for individual studies, and a grand effect size was calculated using pooled data for each outcome (Table 1). The Q heterogeneity statistic was used to determine whether a fixed-effect model (P > .05) or a random-effects model (P < .05) was used. Individual effect sizes were weighted based on their inverse variance.
Table 1.
Summary of within-group comparisons with effect sizes and 95% CIs
| Study | Outcome measure | Intervention | Posttest | Pretest | Effect size (SE) | 95% CI | ||
|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||
| No. | Mean ± SD | No. | Mean ± SD | |||||
| Sexual function | ||||||||
| Alexander et al,36 2018 | FSFI | CVSD | 9 | 28.2 ± 7.25 | 10 | 21.48 ± 6.15 | 1.09 (0.49) | 0.13 to 2.06 |
| Vibratory stimulation | 9 | 23.16 ± 5.02 | 10 | 21.46 ± 5.94 | 0.29 (0.46) | −0.62 to 1.19 | ||
| Hocaloski et al,39 2016 | FSFI | Counseling | 5 | 26.28 ±4.39 | 8 | 18.88 ±3.47 | 2.13 (0.71) | 0.75 to 3.52 |
| Lúcio et al,31 2014 | FSFI | PFMT | 6 | 24.6 ± 14.44a | 6 | 14.6 ± 14.30a | 0.70 (0.59) | −0.47 to 1.87 |
| PFMT + NMES | 7 | 29.5 ± 6.37a | 7 | 14.2 ± 12.30a | 1.24 (0.58) | 0.10 to 2.39 | ||
| PFMT + TTNS | 7 | 24.9 ± 7.19a | 7 | 15.4 ± 15.70a | 0.60 (0.55) | −0.47 to 1.68 | ||
| Mosalanejad et al,37 2018 | FSFI | Mindfulness | 23 | 26.9 ± 4.8 | 25 | 19.5 ± 6.4 | 1.16 (0.31) | 0.54 to 1.77 |
| PFMT | 23 | 23.7 ± 5.1 | 25 | 18.8 ± 6.3 | 0.78 (0.30) | 0.19 to 1.37 | ||
| PFMT + mindfulness | 24 | 25.3 ± 5.4 | 25 | 19.6 ± 5.9 | 0.97 (0.30) | 0.37 to 1.56 | ||
| Sutherland et al,35 2001 | MSQOL-54 | Aerobic exercise | 11 | 10.9 ± 3.8 | 11 | 9.9 ± 3.9 | 0.26 (0.43) | −0.58 to 1.10 |
| Ahmadi et al,33 2010 | MSQOL-54 | Yoga | 11 | 75.75 ± 32.8 | 11 | 67.42 ± 34.45 | 0.24 (0.43) | −0.60 to 1.08 |
| Grand effect size | 0.77 (0.13) | 0.52 to 1.02 | ||||||
| Sexual satisfaction | ||||||||
| Alexander et al,36 2018 | FSFI | CVSD | 9 | 4.8 ± 1.48 | 10 | 3.55 ± 1.53 | 0.82 (0.48) | −0.12 to 1.75 |
| Vibratory stimulation | 9 | 4.24 ± 1.23 | 10 | 3.97 ± 1.16 | 0.23 (0.46) | −0.67 to 1.14 | ||
| Foley et al,38 2001 | MSI | Counseling | 9 | 16.17 ± 5.01 | 9 | 13.22 ± 4.21 | 0.70 (0.49) | −0.25 to 1.65 |
| Hocaloski et al,39 2016 | FSFI | Counseling | 5 | 4.24 ±1.34 | 9 | 3.02 ±0.72 | 1.69 (0.64) | 0.43 to 296 |
| Lúcio et al,31 2014 | FSFI | PFMT | 6 | 5 ± 2.22a | 6 | 3.2 ± 2.37a | 0.76 (0.60) | −0.41 to 1.93 |
| PFMT + NMES | 7 | 6 ± 0.74a | 7 | 2.8 ± 2.67a | 1.20 (0.58) | 0.06 to 2.34 | ||
| PFMT + TTNS | 7 | 5 ± 1.48a | 7 | 4 ± 2.37a | 0.42 (0.54) | −0.64 to 1.48 | ||
| Mosalanejad et al,37 2018 | FSFI | Mindfulness | 23 | 4.7 ± 1.7 | 25 | 3.2 ± 1.5 | 1.00 (0.31) | 0.40 to 1.60 |
| PFMT | 23 | 4.2 ± 1.5 | 25 | 3.1 ± 1.7 | 0.65 (0.30) | 0.07 to 1.23 | ||
| PFMT + mindfulness | 24 | 4.7 ± 1.7 | 25 | 3.6 ± 1.3 | 0.85 (0.30) | 0.26 to 1.43 | ||
| Najafidoulatabad et al,34 2014 | Likert scale | Yoga | 30 | 1.4 ± 1.5 | 30 | 2.1 ± 1.2 | 0.52 (0.26) | 0 to 1.03 |
| Ahmadi et al,33 2010 | MSQOL-54 | Yoga | 11 | 77.27 ± 26.11 | 11 | 65.9 ± 35.83 | 0.32 (0.43) | −0.52 to 1.16 |
| Grand effect size | 0.62 (0.11) | 0.39 to 0.84 | ||||||
| Emotional well-being | ||||||||
| Ahmadi et al,33 2010 | MSQOL-54 | Yoga | 11 | 66.36 ± 19.15 | 11 | 51.63 ± 16.24 | 0.91 (0.45) | 0.03 to 1.78 |
| Sutherland et al,35 2001 | MSQOL-54 | Aerobic exercise | 11 | 22.4 ± 4.1 | 11 | 19.6 ± 4.2 | 0.67 (0.44) | −0.19 to 1.53 |
| Grand effect size | 0.78 (0.31) | 0.17 to 1.40 | ||||||
Abbreviations: CVSD, clitoral vacuum suction device; FSFI, Female Sexual Function Index; NMES, neuromuscular electrical stimulation; MSI, Marital Satisfaction Inventory; MSQOL-54, Multiple Sclerosis Quality of Life–54; PFMT, pelvic floor muscle training; TTNS, transcutaneous tibial nerve stimulation.
Mean and SD not reported. Median and interquartile range were used to estimate mean and SD for meta-analysis purposes.
Table 1 provides a summary of within-group comparisons. Results indicate that sexual function, sexual satisfaction, and emotional well-being all improve after PT intervention, with statistically significant grand effect sizes greater than 0.5, indicating a moderate-to-large effect (Figure S1).32 Converting the grand effect size for sexual function (d = 0.82, 95% CI, 0.57–1.06) to clinical units indicates a 27.4% improvement in FSFI score including factors such as lubrication and decreased pain with intercourse. Converting the grand effect size for sexual satisfaction (d = 0.65, 95% CI, 0.43–0.87) to clinical units denotes a 35.7% improvement in the FSFI sexual satisfaction subscore, which includes factors such as satisfaction of sexual relationship and ability to reach orgasm. Finally, converting the grand effect size for emotional well-being (d = 0.78, 95% CI, 0.17–1.40) to clinical units indicates a 16.8% improvement in the MSQOL-54 emotional well-being subscore, including factors such as a decrease in feelings of sadness, disinterest in activities, and anxiety.
Table S2 provides a summary of between-group comparisons. Results indicate that all three outcomes tend to improve compared with control groups, with grand effect sizes less than 0.5.32 Although all three outcomes have small positive grand effect sizes, only sexual satisfaction was statistically significant (d = 0.29, 95% CI, 0.03–0.55).
Harm
Najafidoulatabad et al34 reported a statistically significant (P = .001) exacerbation of MS symptoms among participants in the control group, who did not receive any intervention. However, specifics regarding nature of exacerbations and number of participants affected were not reported. Alexander et al36 performed skin checks on participants after using the clitoral vacuum suction device or the vibration device and reported no adverse events. Mosalanejad et al37 also reported no adverse events in participants undergoing treatment with PFMT and/or mindfulness training. No other studies addressed harm.
Cost
No studies reported cost of intervention per treatment session. Although Alexander et al36 did not report cost of the vibration device, the cost of the clitoral vacuum suction device was $250 USD. Treatment duration for all the studies ranged from 8 to 12 weeks, with in-person session frequency ranging from zero to three times per week; zero indicates that the participant performed the treatment at home with no therapist present. Because all the interventions could be administered in an outpatient PT environment, cost of treatment would be comparable with that of other outpatient PT rehabilitation programs.
Discussion
This review's aim was to evaluate the effectiveness of PT interventions (ie, interventions within the PT scope of practice) in improving sexual function, sexual satisfaction, and emotional well-being in individuals with MS. Eight studies31,33–39 were eligible for inclusion, each with level IIb evidence or higher and moderate-to-high quality. Within-group results allow us to reject the null and support the alternative hypothesis; PT interventions provide clinically and statistically significant improvements in sexual function, satisfaction, and emotional well-being in individuals with MS. Between-group analyses were conducted to establish whether consequences of sexual dysfunction improved with alternative treatments and to what degree compared with experimental interventions. Between-group differences were small, mostly nonsignificant, and may not reflect clinical importance.
For sexual function, the within-group grand effect size from six studies31,33,35–37,39 was large (d = 0.82) and statistically significant. Although the minimal clinically important difference for the FSFI has not been documented, this change nonetheless reflects notable patient-perceived improvement in the domains tracked by the FSFI, including orgasm, arousal, and lubrication. Interventions that did not directly target the pelvic area, namely, yoga and aerobic exercise, tended to produce the lowest effect sizes, whereas interventions that specifically targeted the pelvic region (PFMT with NMES, clitoral vacuum suction device) produced some of the highest effect sizes. Mindfulness training also produced significantly large effect sizes, suggesting that clinicians treating sexual dysfunction in individuals with MS should opt for treatment that targets the pelvic region and includes mindfulness training.
For sexual satisfaction, the within-group grand effect size from seven studies31,33,34,36–39 was moderate (d = 0.65) and statistically significant as well as clinically important, as implied by a substantial percentage change in clinical measures. Similar to those for sexual function, sexual satisfaction effect sizes tended to be largest when the intervention specifically targeted the pelvic region (PFMT with NMES, clitoral vacuum suction device) and smallest with general interventions (yoga, aerobic exercise). In addition, counseling produced a large effect size. This evidence has clinical implications if the most effective treatments for targeting sexual function and sexual satisfaction are the same: pelvic treatments and mindfulness training.
For emotional well-being, the within-group grand effect size from two studies33,35 was moderately large (d = 0.78) and statistically significant. Although the minimal clinically important difference for the MSQOL-54's emotional well-being subscore has not been documented, the substantial percentage change is indicative of improvement in tertiary consequences of sexual dysfunction, including a perception of decreased anxiety and increased happiness. Unlike sexual function and sexual satisfaction, emotional well-being tends to respond fairly well to a general physical exercise approach. The two included studies used yoga and aerobic exercise, with yoga demonstrating a large effect size (d = 0.91). This finding suggests that the incorporation of physical activity with mindfulness and relaxation therapy, two features of yoga-based practice, may improve emotional well-being. Although it may not directly affect sexual function and sexual satisfaction, incorporating aerobic exercise as an adjunct treatment for individuals with MS and sexual dysfunction may help decrease depressive symptoms and, thus, improve QOL.
For between-group analyses, effect sizes for sexual function, sexual satisfaction, and emotional well-being were small (d = 0.08, 0.29, and 0.38, respectively), and only the sexual satisfaction effect size was statistically significant. Limitations due to heterogeneity among control group protocols resulted in the inability to draw strong clinical implications regarding effectiveness of PT interventions versus comparisons. For example, Mosalanejad et al37 used two control groups (PFMT alone and mindfulness therapy alone) to determine whether a combination treatment (PFMT with mindfulness) was superior to each intervention individually. Control group participants either performed PMFT contractions for 10 to 15 minutes each day or attended mindfulness sessions for 90 minutes once a week; the combined intervention group performed both interventions for the same durations. Because the control groups both received PT interventions, determining the isolated benefit of PT interventions is challenging. Although encouraging, further study is needed to provide generalized clinical implications from this analysis.
Initial findings suggest that counseling with mindfulness training and PFMT with intravaginal NMES may be superior to other PT interventions in improving sexual function and sexual satisfaction. This finding aligns with previous literature in people without CNS disorders. Brotto et al40 found improved desire and arousal after a psychoeducational intervention in females experiencing sexual arousal disorder. Rosenbaum19 found that PFMT improves the strength of pelvic floor muscles and can consequently reduce perineal pain and increase the intensity of orgasmic response. Finally, Nappi et al41 found that females with sexual pain disorders experienced an improvement in pain and sexual function after intravaginal NMES. In individuals with concomitant MS and sexual dysfunction, physical therapists can provide interventions to improve secondary and tertiary consequences of sexual dysfunction. External devices and physical activity can improve secondary consequences of sexual dysfunction, such as pain and difficulty reaching orgasm, and mindfulness training and counseling can improve tertiary consequences of sexual dysfunction, such as anxiety and changes in body image.42 Future studies should focus on developing standardized protocols for counseling and mindfulness training and for PFMT with NMES.
In non-MS CNS disorders, evidence-based literature concerning treatment of sexual dysfunction is largely limited to male participants and pharmacotherapy interventions.43 A systematic review by Lombardi et al44 analyzed 31 articles on the management of sexual dysfunction in patients with CNS disorders, most of which involved pharmacotherapy as the primary intervention. Among males with MS, treatment of sexual dysfunction with sildenafil (Viagra, Viatris Inc) had conflicting results: two studies44,45 reported erectile function enhancement, and another46 reported no improvement compared with placebo. Lombardi et al44 noted that no evidence-based therapeutic options exist to treat females with sexual dysfunction and CNS disorders. With a limited variety of interventions and a lack of studies focusing on sexual dysfunction in females with CNS disorders, this review helps address this gap.
Although the purpose of this review was to explore nonpharmaceutical interventions for sexual dysfunction in MS within the PT scope of practice, it is important to acknowledge the necessity of multidisciplinary management given the complexity of MS. Future studies should include PT, pharmaceutical, and other multidisciplinary interventions to assess the combined effectiveness of multimodal treatment strategies to address primary, secondary, and tertiary consequences of sexual dysfunction. Evaluating the effectiveness of various interventions individually and again in combination would help identify best practices in the future regarding the optimal combination of multimodal interventions. Some of the interventions identified in this review do not fall solely within the PT scope of practice and may be implemented by other disciplines (eg, psychologists and mental health professionals also provide counseling). While physical therapists are capable of providing counseling and mindfulness training, this requires specific training. Furthermore, the counseling provided by physical therapists is complementary, not identical to, that provided by a mental health professional.
Regarding patient safety, all the PT interventions included in this review are well-tolerated and safe for individuals with MS. No adverse or harmful effects were reported among the experimental group participants during the studies.
Heterogeneity in control group methods was observed in the included studies. Most studies did not use nonintervention control groups, instead opting to compare the treatment of interest with an alternative treatment. This is understandable because the nature of sexual dysfunction presents some ethical concerns when withholding treatment. In the future, researchers may use a waitlist control method to improve consistency for between-group analyses while still providing treatment to control participants after the study.
Limitations and Inconsistencies
Several limitations may have affected the results of this review. 1) Despite careful selection of databases and search terms, relevant literature may have been missed. 2) Sample sizes were small and participants were predominantly female, reducing the power and external validity of the results. 3) Failure to specify MS subtype decreases generalizability because only one study reported MS subtype.31 Symptoms of MS are highly variable due to its degenerative and unpredictable nature. Progressive and relapsing-remitting MS each present with different challenges and symptoms that significantly affect treatment strategies. Physical therapy interventions may need to be modified for duration, intensity, frequency, and combination of treatment to best address each individual's unique symptoms of sexual dysfunction without exacerbating other symptoms, such as fatigue and heat intolerance. 4) Only one study included long-term follow-up to assess retention.37
Results of between-group sexual function and sexual satisfaction analyses show a negative effect size for Ahmadi et al,33 a result that does not align with the other studies. To examine baseline equivalence, Ahmadi et al33 used MSQOL-54 physical and mental health composite scores rather than specific scores on subscales related to sexual dysfunction. However, the control group began with considerably higher baseline sexual function and sexual satisfaction subscores, making postintervention score comparisons misleading. Although the yoga group experienced a 12.35% and 17.25% increase in sexual function and sexual satisfaction scores, respectively, the final scores did not exceed control group scores after the intervention.
In addition, Mosalanejad et al37 demonstrated a negative effect size for the sexual function between-group analysis comparing treatment with PFMT and mindfulness therapy versus mindfulness therapy alone. We postulate that the increased time demand of performing two different interventions resulted in decreased quality of one or both interventions, thereby negatively affecting patients' final outcomes. This is a valuable lesson for clinicians because it suggests that more time spent on multiple interventions may actually lead to poorer outcomes.
The two studies38,39 that used counseling as an intervention returned vastly different sexual satisfaction effect sizes. This inconsistency may be due to several key differences in study design: treatment focus (communication vs mindfulness and self-observation), dosage, sexual satisfaction outcome measure, and treatment setting.
Esteve-Rios et al47 published a systematic review in February 2020 examining the effectiveness of improving the sexuality of women with MS. Included studies used a variety of interventions, including pharmaceutical drugs, physical activity, and sexual therapy. Although similar studies were examined, the present systematic review focuses on interventions that can be implemented by a licensed physical therapist. In addition, the inclusion of a meta-analysis contributes to robust, level I evidence for the treatment of sexual dysfunction in MS.
Directions for Future Work
Based on the results of this review, more studies focusing on the effects of PFMT with NMES and of counseling with mindfulness-based therapy should be conducted to strengthen existing evidence. Future studies should include a waitlist control group to rule out spontaneous improvement while still providing control group participants with the intervention after the studies if indicated. The efficacy of PT interventions should be examined in comparison to and in combination with pharmacotherapy, a widely used treatment for sexual dysfunction.11 Recruiting both male and female participants with different subtypes or stages of MS would provide information on the treatment that is most effective for each demographic and improve generalizability. Finally, larger sample sizes would increase the power of individual studies and could contribute to clinical practice guidelines for conservative care for sexual dysfunction.
Conclusions
Sexual dysfunction is a prevalent problem in individuals with MS as well as in the general population. Physical therapy interventions can help improve aspects of sexual function, sexual satisfaction, and emotional well-being in individuals with MS. Additional research is needed to establish specific treatment protocols and determine treatment efficacy compared with controls.
PRACTICE POINTS
Sexual dysfunction is prevalent in the MS population, and administering self-report measures such as the Female Sexual Function Index may capture information on primary and secondary consequences.
According to the studies included in this review, regular aerobic exercise resulted in an improvement in emotional well-being, and providing pelvic floor muscle training and/or mindfulness training improved sexual function and sexual satisfaction.
Although objective measures such as pelvic floor muscle tone and flexibility can be clinically observed, they are less useful than self-reported measures in establishing treatment efficacy when the variables of interest incorporate a mix of psycho-socio-emotional factors influencing the sexual experience.
Supplementary Material
Acknowledgments
The authors thank Katherine Sawyer, PT, DPT, and Parisa Rivette, PT, DPT, for their assistance in reviewing and editing the manuscript.
Footnotes
Financial Disclosures: The authors declare no conflicts of interest.
Funding/Support: None.
References
- 1.MS prevalence. National Multiple Sclerosis Society. Accessed January 2, 2019. https://www.nationalmssociety.org/About-the-Society/MS-Prevalence.
- 2.Charil A, Filippi M. Inflammatory demyelination and neurodegeneration in early multiple sclerosis. J Neurol Sci. 2007;259:7–15. doi: 10.1016/j.jns.2006.08.017. [DOI] [PubMed] [Google Scholar]
- 3.Kesselring J, Beer S. Symptomatic therapy and neurorehabilitation in multiple sclerosis. Lancet Neurol. 2005;4:643–652. doi: 10.1016/S1474-4422(05)70193-9. [DOI] [PubMed] [Google Scholar]
- 4.Motl RW, Gosney JL. Effect of exercise training on quality of life in multiple sclerosis: a meta-analysis. Mult Scler. 2008;14:129–135. doi: 10.1177/1352458507080464. [DOI] [PubMed] [Google Scholar]
- 5.Rommer PS, Eichstädt K, Ellenberger D et al. Symptomatology and symptomatic treatment in multiple sclerosis: results from a nationwide MS registry. Mult Scler. 2019;25:1641–1652. doi: 10.1177/1352458518799580. [DOI] [PubMed] [Google Scholar]
- 6.Tepavcevic D, Kostic J, Basuroski I, Stojsavljevic N, Pekmezovic T, Drulovic J. The impact of sexual dysfunction on the quality of life measured by MSQoL-54 in patients with multiple sclerosis. Mult Scler. 2008;14:1131–1136. doi: 10.1177/1352458508093619. [DOI] [PubMed] [Google Scholar]
- 7.Miletta M, Bogliatto F, Bacchio L. Multidisciplinary management of sexual dysfunction, perineal pain, and elimination dysfunction in a woman with multiple sclerosis. Int J MS Care. 2017;19:25–28. doi: 10.7224/1537-2073.2015-082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kessler TM, Fowler CJ, Panicker JN. Sexual dysfunction in multiple sclerosis. Expert Rev Neurother. 2009;9:341–350. doi: 10.1586/14737175.9.3.341. [DOI] [PubMed] [Google Scholar]
- 9.Gruenwald I, Vardi Y, Gartman I et al. Sexual dysfunction in females with multiple sclerosis: quantitative sensory testing. Mult Scler. 2007;13:95–105. doi: 10.1177/1352458506071134. [DOI] [PubMed] [Google Scholar]
- 10.Demirkiran M, Sarica Y, Uguz S, Yerdelen D, Aslan K. Multiple sclerosis patients with and without sexual dysfunction: are there any differences? Mult Scler. 2006;12:209–214. doi: 10.1191/135248506ms1253oa. [DOI] [PubMed] [Google Scholar]
- 11.Lombardi G, Musco S, Kessler TM, Marzi VL, Lanciotti M, Del Popolo G. Management of sexual dysfunction due to central nervous system disorders: a systematic review. BJU Int. 2015;115(suppl 6):47–56. doi: 10.1111/bju.13055. [DOI] [PubMed] [Google Scholar]
- 12.Gerbild H, Larsen CM, Graugaard C, Areskoug Josefsson K. Physical activity to improve erectile function: a systematic review of intervention studies. Sex Med. 2018;6:75–89. doi: 10.1016/j.esxm.2018.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zorzon M, Zivadinov R, Bosco A et al. Sexual dysfunction in multiple sclerosis: a case-control study, I: frequency and comparison of groups. Mult Scler. 1999;5:418–427. doi: 10.1177/135245859900500i609. [DOI] [PubMed] [Google Scholar]
- 14.Shifren JL, Monz BU, Russo PA, Segreti A, Johannes CB. Sexual problems and distress in united states women: prevalence and correlates. Obstet Gynecol. 2008;112:970–978. doi: 10.1097/AOG.0b013e3181898cdb. [DOI] [PubMed] [Google Scholar]
- 15.Laumann EO, Paik A, Rosen RC. Sexual dysfunction in the United States: prevalence and predictors. JAMA. 1999;281:537–544. doi: 10.1001/jama.281.6.537. [DOI] [PubMed] [Google Scholar]
- 16.Smith S, Weldring T. Patient-reported outcomes (PROs) and patient-reported outcome measures (PROMs) Health Serv Insights. 2013;6:61–68. doi: 10.4137/HSI.S11093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lew-Starowicz M, Rola R. Prevalence of sexual dysfunctions among women with multiple sclerosis. Sex Disabil. 2013;31:141–153. doi: 10.1007/s11195-013-9293-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rosenbaum TY. The role of physical therapy in female sexual dysfunction. Curr Sex Health Rep. 2008;5:97–101. Accessed December 27, 2018. https://pdfs.semanticscholar.org/a36f/1bac3ebc30797b1355fdf84f9f14d2a7bf4d.pdf. [Google Scholar]
- 19.Rosenbaum TY. Pelvic floor involvement in male and female sexual dysfunction and the role of pelvic floor rehabilitation in treatment: a literature review. J Sex Med. 2007;4:4–13. doi: 10.1111/j.1743-6109.2006.00393.x. [DOI] [PubMed] [Google Scholar]
- 20.Petajan JH, Gappmaier E, White AT, Spencer MK, Mino L, Hicks RW. Impact of aerobic training on fitness and quality of life in multiple sclerosis. Ann Neurol. 1996;39:432–441. doi: 10.1002/ana.410390405. [DOI] [PubMed] [Google Scholar]
- 21.Petajan JH, White AT. Recommendations for physical activity in patients with multiple sclerosis. Sport Med. 1999;27:179–191. doi: 10.2165/00007256-199927030-00004. [DOI] [PubMed] [Google Scholar]
- 22.Rebar AL, Stanton R, Geard D, Short C, Duncan MJ, Vandelanotte C. A meta-meta-analysis of the effect of physical activity on depression and anxiety in non-clinical adult populations. Health Psychol Rev. 2015;9:366–378. doi: 10.1080/17437199.2015.1022901. [DOI] [PubMed] [Google Scholar]
- 23.Parker AG. The effectiveness of simple psychological and physical activity interventions for high prevalence mental health problems in young people: a factorial randomised controlled trial. J Affect Disord. 2016;196:200–209. doi: 10.1016/j.jad.2016.02.043. [DOI] [PubMed] [Google Scholar]
- 24.Moher D, Liberati A, Tetzlaff J et al. Preferred Reporting Items for Systematic Reviews and Meta-analyses: the PRISMA statement (Chinese edition) J Chin Integr Med. 2009;7:889–896. [PMC free article] [PubMed] [Google Scholar]
- 25.Jewell DV. Guide to EvidenceBased Physical Therapist Practice. Jones & Bartlett Learning; 2011. [Google Scholar]
- 26.Welcome to PEDro, the Physiotherapy Evidence Database. https://www.pedro.org.au.
- 27.Vickrey BG, Hays RD, Harooni R, Myers LW, Ellison GW. A health-related quality of life measure for multiple sclerosis. Qual Life Res. 1995;4:187–206. doi: 10.1007/BF02260859. [DOI] [PubMed] [Google Scholar]
- 28.Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 510 [Updated March 2011] The Cochrane Collaboration; 2011. [Google Scholar]
- 29.Kurtzke JF. Rating neurologic impairment in multiple sclerosis: an Expanded Disability Status Scale (EDSS) Neurology. 1983;33:1444–1452. doi: 10.1212/wnl.33.11.1444. [DOI] [PubMed] [Google Scholar]
- 30.Rosen R, Brown C, Heiman J et al. The Female Sexual Function Index (FSFI): a multidimensional self-report instrument for the assessment of female sexual function. J Sex Marital Ther. 2000;26:191–208. doi: 10.1080/009262300278597. [DOI] [PubMed] [Google Scholar]
- 31.Lúcio A, D'Ancona C, Lopes M, Perissinotto M, Damasceno B. The effect of pelvic floor muscle training alone or in combination with electrostimulation in the treatment of sexual dysfunction in women with multiple sclerosis. Mult Scler. 2014;20:1761–1768. doi: 10.1177/1352458514531520. [DOI] [PubMed] [Google Scholar]
- 32.Cohen J. Statistical Power for the Social Sciences. Laurence Erlbaum Associates; 1988. [Google Scholar]
- 33.Ahmadi A, Nikbakh M, Asghar Arastoo A, Habibi A-H. The effects of a yoga intervention on balance, speed and endurance of walking, fatigue and quality of life in people with multiple sclerosis. J Hum Kinet. 2010;23:71–78. [Google Scholar]
- 34.Najafidoulatabad S, Mohebbi Z, Nooryan K. Yoga effects on physical activity and sexual satisfaction among the Iranian women with multiple sclerosis: a randomized controlled trial. Afr J Tradit Complement Altern Med. 2014;11:78–82. doi: 10.4314/ajtcam.v11i5.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sutherland G, Andersen MB, Stoové MA. Can aerobic exercise training affect health-related quality of life for people with multiple sclerosis? J Sport Exerc Psychol. 2001;23:122–135. [Google Scholar]
- 36.Alexander M, Bashir K, Alexander C, Marson L, Rosen R. Randomized trial of clitoral vacuum suction versus vibratory stimulation in neurogenic female orgasmic dysfunction. Arch Phys Med Rehabil. 2018;99:299–305. doi: 10.1016/j.apmr.2017.09.001. [DOI] [PubMed] [Google Scholar]
- 37.Mosalanejad F, Afrasiabifar A, Zoladl M. Investigating the combined effect of pelvic floor muscle exercise and mindfulness on sexual function in women with multiple sclerosis: a randomized controlled trial. Clin Rehabil. 2018;32:1340–1347. doi: 10.1177/0269215518777877. [DOI] [PubMed] [Google Scholar]
- 38.Foley FW, LaRocca NG, Sanders AS, Zemon V. Rehabilitation of intimacy and sexual dysfunction in couples with multiple sclerosis. Mult Scler. 2001;7:417–421. doi: 10.1177/135245850100700612. [DOI] [PubMed] [Google Scholar]
- 39.Hocaloski S, Elliott S, Brotto LA, Breckon E, McBride K. A mindfulness psychoeducational group intervention targeting sexual adjustment for women with multiple sclerosis and spinal cord injury: a pilot study. Sex Disabil. 2016;34:183–198. [Google Scholar]
- 40.Brotto LA, Basson R, Luria M. A mindfulness-based group psychoeducational intervention targeting sexual arousal disorder in women. J Sex Med. 2008;5:1646–1659. doi: 10.1111/j.1743-6109.2008.00850.x. [DOI] [PubMed] [Google Scholar]
- 41.Nappi RE, Ferdeghini F, Abbiati I, Vercesi C, Farina C, Polatti F. Electrical stimulation (ES) in the management of sexual pain disorders. J Sex Marital Ther. 2003;29:103–110. doi: 10.1080/713847129. [DOI] [PubMed] [Google Scholar]
- 42.Nielsen M, Keefe FJ, Bennell K, Jull GA. Physical therapist-delivered cognitive-behavioral therapy: a qualitative study of physical therapists' perceptions and experiences. Phys Ther. 2014;94:196–209. doi: 10.2522/ptj.20130047. [DOI] [PubMed] [Google Scholar]
- 43.Sanchez Ramos A, Vidal J, Jauregui M et al. Efficacy, safety and predictive factors of therapeutic success with sildenafil for erectile dysfunction in patients with different spinal cord injuries. Spinal Cord. 2001;39:637–643. doi: 10.1038/sj.sc.3101210. [DOI] [PubMed] [Google Scholar]
- 44.Lombardi G, Macchiarella A, Del Popolo G. Efficacy and safety of tadalafil for erectile dysfunction in patients with multiple sclerosis. J Sex Med. 2010 doi: 10.1111/j.1743-6109.2010.01797.x. [DOI] [PubMed] [Google Scholar]
- 45.Fowler CJ, Miller JR, Sharief MK, Hussain IF, Stecher VJ, Sweeney M. A double blind, randomised study of sildenafil citrate for erectile dysfunction in men with multiple sclerosis. J Neurol Neurosurg Psychiatry. 2005;76:700–705. doi: 10.1136/jnnp.2004.038695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Safarinejad MR. Evaluation of the safety and efficacy of sildenafil citrate for erectile dysfunction in men with multiple sclerosis: a double-blind, placebo controlled, randomized study. J Urol. 2009;181:252–258. doi: 10.1016/j.juro.2008.09.003. [DOI] [PubMed] [Google Scholar]
- 47.Esteve-Rios A, Garcia-Sanjuan S, Oliver-Roig A, Cabañero-Martínez MJ. Effectiveness of interventions aimed at improving the sexuality of women with multiple sclerosis: a systematic review. Clin Rehabil. 2020;34:438–439. doi: 10.1177/0269215520901751. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


