Abstract
Objectives:
To compare emergency department (ED) visit rates for suicidal ideation and/or self-harm among youth by urban-rural location of residence.
Study design:
Retrospective analysis of ED visits for suicidal ideation and/or self-harm by youth age 5-to-19 years (N=297,640) in the 2016 Nationwide Emergency Department Sample, a representative sample of all U.S. ED visits. We used weighted Poisson generalized linear models to compare population-based visit rates by urban-rural location of patient residence, adjusted for age, sex, and U.S. Census region. For self-harm visits, we compared injury mechanisms by urban-rural location.
Results:
Among ED visits for suicidal ideation and/or self-harm, the median age was 16 years, 65.9% were female, 15.9% had a rural location of patient residence, and 0.1% resulted in mortality. The adjusted ED visit rate for suicidal ideation/or and self-harm did not differ significantly by urban-rural location. For the subset of visits for self-harm, the adjusted visit rate was significantly higher in small metropolitan (aIRR 1.39, 95% CI 1.01, 1.90), micropolitan (aIRR 1.46, 95% CI 1.10, 1.93), and noncore areas (aIRR 1.39, 95% CI 1.03, 1.87) compared to large metropolitan areas. When stratified by injury mechanism, ED visit rates were higher among youth living in rural than in urban areas for self-inflicted firearm injuries (aIRR = 3.03, 95% CI 1.32, 6.74).
Conclusions:
Compared with youth living in urban areas, youth living in rural areas had higher ED visit rates for self-harm, including self-inflicted firearm injuries. Preventive approaches for self-harm based in community and ED settings might help address these differences.
Keywords: Suicide, Self-Harm, Emergency Medicine, Rural Health
INTRODUCTION
Suicide is the second leading cause of death among youth age 10-to-19 years in the United States (U.S.), with rates rising over the last decade.[1] Youth living in rural areas are nearly twice as likely to die by suicide; the rural-urban disparity in youth suicide rates has been widening.[2] Contributors to youth suicides in rural areas are varied and may include mental health workforce shortages, higher community poverty, and increased access to lethal means such as firearms.[2–4] Many youth who die by suicide visit the emergency department (ED) in the months preceding their death, often for mental health concerns such as suicidal ideation or self-harm.[5,6] One-third of adolescents with suicidal ideation will go on to attempt suicide within 12 months, and suicide attempts increase the risk of subsequent death by suicide.[7,8] Non-suicidal self-harm in adolescents, particularly when frequent or using several different methods, is also associated with increased risk of suicide attempts and deaths.[9] ED visits for suicidal ideation and self-harm among youth have doubled from 2007 to 2015.[10,11]
Studying differences in ED visits for suicidal ideation and self-harm in rural versus urban areas provides an opportunity to identify how youth at risk for suicide interact with the healthcare system and to ensure that approaches to suicide prevention based in ED and community settings appropriately address geographic variation across populations.[12] ED suicide prevention efforts may include screening for suicidal ideation, brief lethal means restriction counseling, timely access to mental health evaluation on-site or via telepsychiatry, and mental health referral assistance.[13–16] Broader community efforts for high-risk geographic areas could focus on integration of mental health care into the medical home, mental health workforce development, and supporting at-risk youth in the community.[17] Regional differences have been noted among youth ED visits for mental health conditions, with the highest visit rates in the Midwest and lowest in the South.[18] A nationally representative study of youth mental health ED visits found a lower visit rate in rural areas, but this study examined all mental health conditions rather than focusing on suicidal ideation and self-harm.[10] Higher rates of hospitalization for self-inflicted youth firearm injuries have been described in rural than in urban areas, but other specific mechanisms of self-harm were not studied and ED visits that did not lead to hospitalization were not included.[19] The objectives of our study were to examine differences in ED visit characteristics for youth suicidal ideation and self-harm in rural versus urban areas, to examine differences in ED visit rates for youth suicidal ideation and self-harm in rural versus urban areas, and to determine whether mechanisms of injury in youth ED visits for self-harm differ in rural versus urban areas.
METHODS
Study Design and Setting:
We performed a retrospective analysis of ED visits for youth suicidal ideation and/or self-harm from 2016 in the Nationwide Emergency Department Sample (NEDS). The NEDS is part of the Healthcare Cost and Utilization Project sponsored by the Agency for Healthcare Research and Quality (AHRQ).[20] The 2016 NEDS is an all-payer database containing 33 million ED visits from 953 hospitals in 37 states, representing a 20% stratified sample of all U.S. hospital EDs. Sampling weights are provided to allow for calculation of estimates representative of all U.S. ED visits nationally. NEDS includes information on patient characteristics (age, sex, insurance payer, quartile of median household income for the patient’s zip code, urban-rural classification of the patient’s county of residence), International Classification of Diseases, 10th Revision, Clinical Modification (ICD-10-CM) diagnostic codes, and disposition. Race/ethnicity is not available for analysis. This study was deemed exempt from approval by the Lurie Children’s Hospital institutional review board.
Study Population:
We defined ED encounters for suicidal ideation and/or self-harm based on the presence of a diagnosis code in any one of the following AHRQ Clinical Classifications Software Revised (CCSR) categories: MBD012 (suicidal ideation/attempt/intentional self-harm), MBD027 (suicide attempt/intentional self-harm; subsequent encounter), or EXT021 (external cause codes: intent of injury, self-harm).[21] Among visits for suicidal ideation and/or self-harm, we used diagnosis code groups from the Child and Adolescent Mental Health Disorders Classification System (CAMHD-CS) to determine the prevalence of mental health comorbidities.[22] Among visits for suicidal ideation and/or self-harm, we used diagnosis codes from the National Center for Health Statistics (NCHS) ICD-10-CM external cause-of-injury matrix to define a subset of these visits for intentional self-harm and classify the injury mechanism in pre-specified categories.[23,24] We further subcategorized visits for poisoning by selected medication classes using diagnosis codes. We included visits for ages 5–19 to allow for alignment with U.S. Census age categories.[25] We excluded 9 visits that were missing age; no visits had missing sex or urban-rural classification.
Measurements:
The primary outcome was the number of ED visits for suicidal ideation and/or self-harm per 10,000 youth. Secondary outcomes included ED visit rates for intentional self-harm, stratified by mechanism of injury. The primary independent variable was urban-rural classification of the patient’s county of residence based on the NCHS Urban-Rural Classification Scheme.[26] We classified patient residence as large metropolitan (≥1 million residents), medium metropolitan (250,000–999,999 residents), small metropolitan (50,000–249,999 residents), micropolitan (10,000–49,999 residents), and noncore (<10,000 residents). For portions of the analysis, we collapsed the classification to a dichotomous rural/urban measure, with micropolitan and noncore residences considered rural and all metropolitan residences classified as urban.[27] From the U.S. Census Bureau, we obtained intercensal population counts by age, sex, NCHS urban-rural classification, and U.S. Census region (Northeast, South, Midwest, or West).[25,28]
We compared ED visits for suicidal ideation and/or self-harm in rural and urban areas with respect to age (5–9, 10–14, or 15–19), sex, insurance payer (public, private, self pay/other), quartile of median household income for the patient’s zip code, hospital urban-rural location, and disposition. Disposition was classified as admission, transfer to a short-term hospital, transfer to another type of facility (including a psychiatric facility), or other.
Data Analysis:
We tabulated ED visit characteristics for suicidal ideation and/or self-harm by urban-rural location of patient residence and tested differences using χ2 test with Rao-Scott correction for survey data.[29] We used NEDS sampling and discharge weights to produce nationally representative estimates of ED visits for youth suicidal ideation and/or self-harm and standard errors and to determine the frequencies of mental health comorbidities among these visits.[30] We calculated the visit rate per 10,000 youth based on U.S. Census Bureau counts. We calculated incidence rate ratios (IRR) for ED visits by age, sex, Census region, and urban-rural location of patient residence. Confidence intervals (CI) for IRR were derived based on the survey-weighted standard errors for the counts using the delta method.[30] We determined the number and rate of ED visits for self-harm stratified by mechanism, and we calculated IRR to compare these visits by urban-rural location. We calculated population-adjusted ED visit rates by urban-rural location of residence, with adjustment for differences in age, sex, and U.S. Census region by fitting weighted Poisson generalized linear models. Analyses were conducted in the open source R software environment, using the R add on package “Survey.”[31–33]
RESULTS
ED visit characteristics for youth suicidal ideation and/or self-harm in rural versus urban areas
In 2016, there were 297,640 ED visits (47.8 ED visits per 10,000 youth) for suicidal ideation and/or self-harm by youth age 5-to-19 years. The median age was 16 (interquartile range 14–17), with 65.9% visits by females and 15.9% visits by youth living in rural areas. Death occurred in the ED in 159 visits (0.05%), and death occurred during hospitalization in 132 visits (0.04%). Among ED visits for suicidal ideation and/or self-harm, 70.2% had a mental health comorbidity based on the presence of a diagnosis code in one of the following groups: 10.3% attention-deficit hyperactivity disorder, 18.5% anxiety disorders, 6.0% bipolar and related disorders, 48.9% depressive disorders, 6.3% disruptive, impulse control, and conduct disorders, 2.6% schizophrenia spectrum and other psychotic disorders, 16.2% substance-related and addictive disorders, and 9.3% trauma and stressor-related disorders. ED visits for suicidal ideation and/or self-harm by youth living in rural areas compared to urban areas were significantly more likely to involve older youth (age 15-to-19 years), public insurance (55.9% vs. 45.6%), lower median household income (lowest quartile: 40.3% vs. 22.9%) and Midwest and Southern U.S. Census regions (p<0.001 for each) (Table 1). Visits by rural youth were less likely to result in admission and more likely to result in transfer to another short-term hospital (p<0.001).
TABLE 1.
Characteristics of ED Visits for Youth Suicidal Ideation and/or Self-Harm by Urban-Rural Location of Residence
| ED Visit Characteristic | ED Visits (%) | Rurala (%) N=47,390 |
Urbana (%) N=250,249 |
P-value (χ2) |
|---|---|---|---|---|
| Age | ||||
| 5–9 | 8081 (3%) | 2.2 | 2.8 | < .001 |
| 10–14 | 89185 (30%) | 29.5 | 30.1 | |
| 15–19 | 200373 (67%) | 68.3 | 67.1 | |
| Sex | ||||
| Male | 101528 (34%) | 34.2 | 34.1 | .938 |
| Female | 196066 (66%) | 65.8 | 65.9 | |
| Primary Payer | ||||
| Public | 140564 (47%) | 55.9 | 45.6 | < .001 |
| Private | 129135 (43%) | 35.7 | 44.9 | |
| Self-Pay/Other | 27621 (9%) | 8.4 | 9.5 | |
| Median Household Income for Patient’s Zip Code | ||||
| Lowest Quartile | 76448 (26%) | 40.3 | 22.9 | < .001 |
| Second Quartile | 74442 (25%) | 42.4 | 21.7 | |
| Third Quartile | 72950 (25%) | 13.7 | 26.5 | |
| Highest Quartile | 69480 (24%) | 2.0 | 27.4 | |
| Census Region | ||||
| Northeast | 53073 (18%) | 10.7 | 19.2 | < .001 |
| Midwest | 80744 (27%) | 41.7 | 24.4 | |
| South | 97861 (33%) | 33.9 | 32.7 | |
| West | 65961 (22%) | 13.8 | 23.8 | |
| Hospital Urban-Rural Status | ||||
| Metropolitan | 257881 (87%) | 21.2 | 99.0 | < .001 |
| Non-metropolitan | 39758 (13%) | 78.8 | 1.0 | |
| Disposition | ||||
| Admission | 58523 (20%) | 15.1 | 20.5 | < .001 |
| Transfer to Short-term Hospital | 29730 (10%) | 16.1 | 8.8 | |
| Transfer to Other Facility, including Psychiatric Facility | 91802 (31%) | 29.3 | 31.1 | |
| Other | 117584 (40%) | 39.5 | 39.5 | |
Rural includes micropolitan and noncore areas. Urban includes large, medium, and small metropolitan areas.
ED visit rates for youth suicidal ideation and/or self-harm in rural versus urban areas
In 2016, there were 47.8 ED visits for youth suicidal ideation and/or self-harm per 10,000 youth. ED visit rates for suicidal ideation and/or self-harm were higher among youth age 15-to-19 vs. 5-to-9 years (IRR 24.0, 95% CI 19.1, 30.1), higher among females than males (IRR 2.02, 95% CI 1.74, 2.34), and higher in the Midwest than the South (RR 1.49, 95% CI 1.13, 1.96) (Table 2). Across urban-rural categories, the largest number of ED visits for suicidal ideation and/or self-harm (153,433 visits) occurred among youth living in large metropolitan areas and the highest ED visit rate (58.1 visits per 10,000 youth) occurred among youth living in micropolitan areas. The ED visit rate for suicidal ideation and/or self-harm did not significantly differ by urban-rural location of patient residence.
TABLE 2.
ED Visits for Youth Suicidal Ideation and/or Self-Harm by Demographics and Urban-Rural Location of Residence
| Visits for Suicidal Ideation and/or Self-Harm | Visits for Self-Harm | |||||
|---|---|---|---|---|---|---|
| ED Visit Characteristic | ED Visitsa | Visit Rateb per 10,000 Youth | Incidence Rate Ratio (95% CI) | ED Visitsa | Visit Rateb per 10,000 Youth | Incidence Rate Ratio (95% CI) |
| Total youth age 5–19 | 297640 | 47.8 | N/A | 106181 | 17.1 | N/A |
| Age | ||||||
| 5–9 | 8081 | 4.0 | Ref | 574 | 0.3 | Ref |
| 10–14 | 89185 | 43.2 | 10.9 (8.5, 14.1)c | 27876 | 13.5 | 48.1 (36.9, 62.7)c |
| 15–19 | 200373 | 94.7 | 24.0 (19.1, 30.1)c | 77731 | 36.7 | 130.8 (102.2, 167.4)c |
| Sex | ||||||
| Male | 101528 | 32.0 | Ref | 25858 | 8.1 | Ref |
| Female | 196066 | 64.4 | 2.02 (1.74, 2.34)c | 80302 | 26.4 | 3.24 (2.88, 3.65)c |
| U.S. Census Region | ||||||
| Northeast | 53073 | 52.2 | 1.27 (0.96, 1.70) | 13364 | 13.2 | 0.84 (0.66, 1.07) |
| Midwest | 80744 | 61.1 | 1.49 (1.13, 1.96)d | 30763 | 23.3 | 1.48 (1.18, 1.85)c |
| South | 97861 | 41.0 | Ref | 37523 | 15.7 | Ref |
| West | 65961 | 44.1 | 1.07 (0.81, 1.42) | 24530 | 16.4 | 1.04 (0.84, 1.29) |
| Urban-Rural Location of Residence | ||||||
| Large Metropolitan (≥1 million residents) | 153433 | 44.3 | Ref | 51096 | 14.8 | Ref |
| Medium Metropolitan (250,000 – 999,999 residents) | 65256 | 49.2 | 1.11 (0.85, 1.45) | 24264 | 18.3 | 1.24 (0.99, 1.55) |
| Small Metropolitan (50,000–249,999 residents) | 30792 | 54.5 | 1.23 (0.93, 1.63) | 11924 | 21.1 | 1.43 (1.12, 1.82)d |
| Micropolitan (10,000–49,999 residents) | 30328 | 58.1 | 1.31 (1.07, 1.60)d | 11486 | 22.0 | 1.49 (1.25, 1.78)c |
| Noncore (<10,000 residents) | 17062 | 49.1 | 1.11 (0.90, 1.35) | 7195 | 20.7 | 1.40 (1.17, 1.68)c |
Weighted estimates
U.S. Census population subtotals used in rate calculations.
P < 0.001.
P < 0.01.
In 2016, there were 106,181 ED visits for self-harm (17.1 visits per 10,000 youth). ED visit rates for self-harm were higher among youth age 15-to-19 vs. 5-to-9 years (IRR 130.8, 95% CI 102.2, 167.4), higher among females than males (IRR 3.24, 95% CI 2.88, 3.65), and higher in the Midwest compared to the South (IRR 1.48, 95% CI 1.18, 1.85). Across urban-rural categories, the largest number of ED visits for self-harm (51,096 visits) occurred among youth living in large metropolitan areas and the highest ED visit rate (22.0 visits per 10,000 youth) occurred among youth living in micropolitan areas. The ED visit rate for self-harm was significantly higher among youth living in small metropolitan areas (IRR 1.43, 95% CI 1.12, 1.82), micropolitan areas (IRR 1.49, 95% CI 1.12, 1.82), and noncore areas (IRR 1.40, 95% CI 1.17, 1.68) compared to youth living in large metropolitan areas.
After population-adjusting for age, sex, and U.S. Census region, there remained no significant differences for ED visit rates for suicidal ideation and/or self-harm among urban-rural categories (Table 3). In the adjusted model, there was no significant difference in ED visit rates for suicidal ideation and/or self-harm by U.S. Census region. The population-adjusted ED visit rate for self-harm was significantly higher for youth living in small metropolitan (adjusted incidence rate ratio [aIRR] 1.39, 95% CI 1.01, 1.90), micropolitan (aIRR 1.46, 95% CI 1.10, 1.93), and noncore areas (aIRR 1.39, 95% CI 1.03, 1.87) compared to large metropolitan areas.
TABLE 3.
Population-Adjusted Relative ED Visit Rates for Youth Suicidal Ideation and/or Self-Harm by Urban-Rural Location of Residence
| ED Visit Type | Adjusteda Incidence Rate Ratio (95% CI) | |
|---|---|---|
| Suicidal Ideation and/or Self-Harm |
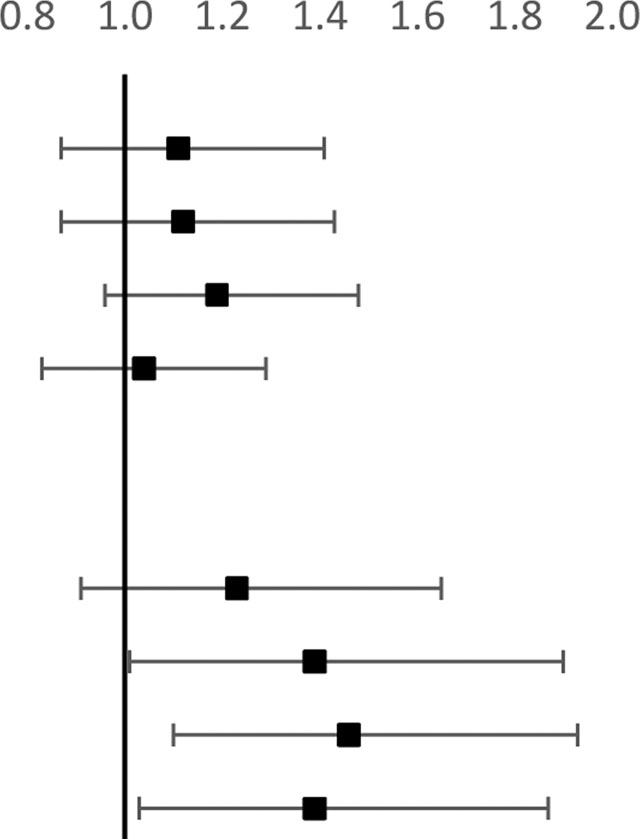
|
|
| Large Metropolitan | Ref | |
| Medium Metropolitan | 1.11 (0.87, 1.41) | |
| Small Metropolitan | 1.12 (0.87, 1.43) | |
| Micropolitan | 1.19 (0.96, 1.48) | |
| Noncore | 1.04 (0.83, 1.29) | |
| Self-Harm | ||
| Large Metropolitan | Ref | |
| Medium Metropolitan | 1.23 (0.91, 1.65) | |
| Small Metropolitan | 1.39 (1.01, 1.90)b | |
| Micropolitan | 1.46 (1.10, 1.93)b | |
| Noncore | 1.39 (1.03, 1.87)b | |
Adjusted for age, sex, and U.S. Census Region
P < 0.05
Mechanisms of injury for ED visits by youth for self-harm in rural versus urban areas
The most frequent mechanisms of injury due to self-harm were poisoning (79.2%) and cutting/piercing (13.5%), with self-inflicted firearm injuries accounting for only 0.1% of visits. ED visit rates were higher among youth living in rural than urban areas for self-inflicted firearm injuries (IRR 3.58; 95% CI 1.31, 9.81) and poisoning (IRR 1.31, 95% CI 1.14, 1.51) (Table 4). After population adjustment, ED visit rates remained significantly higher in rural versus urban areas for self-inflicted firearm injuries (aIRR 3.03, 95% CI 1.32, 6.74). Selected ED visit rates for poisoning with intent to self-harm by medication class are presented in Table 5 (online), with higher ED visit rates found among youth living in rural areas for antiallergic/antiemetic drugs and amphetamines, among other medication classes, but no significant difference in visit rates for opiates/opioids.
TABLE 4.
Youth ED Visits for Self-Harm by Injury Mechanism and Urban-Rural Location of Residence
| Mechanism | ED Visits (%)a | ED Visit Rate per 100,000 Youth | Incidence Rate Ratio (95% CI) | Adjustedc Incidence Rate Ratio (95% CI) | |
|---|---|---|---|---|---|
| Urban (95% CI)b | Rural (95% CI)b | ||||
| Cut/Pierce | 14341 (13.5%) | 22.40 (19.60, 25.20) | 27.06 (22.53, 31.58) | 1.21 (0.98, 1.49) | 1.20 (1.00, 1.43) |
| Firearm | 74 (0.1%) | 0.09 (0.04, 0.14) | 0.31 (0.06, 0.57) | 3.58 (1.31, 9.81)e | 3.03 (1.32, 6.74)e |
| Poisoning | 84083 (79.2%) | 129.47 (117.23, 141.7) | 170.22 (152.93, 187.52) | 1.31 (1.14, 1.51)f | 1.28 (0.99, 1.66) |
| Suffocation | 1019 (1.0%) | 1.59 (1.29, 1.89) | 1.93 (1.14, 2.71) | 1.21 (0.77, 1.90) | 1.23 (0.72, 2.02) |
| Otherd | 21653 (20.4%) | 3.273 (2.925, 3.621) | 4.761 (4.109, 5.412) | 1.45 (1.22, 1.73)f | 1.37 (0.98, 1.90) |
| All Mechanisms | 106181 (100%) | 163.52 (148.29, 178.75) | 214.76 (194.04, 235.49) | 1.31 (1.15, 1.50)f | 1.27 (0.96, 1.68) |
Percentage among ED visits for self-harm. Percentages add to greater than 100% because visits could involve more than one mechanism.
Urban includes large, medium, and small metropolitan areas. Rural includes micropolitan and noncore areas.
Adjusted for age, sex, U.S. Census region.
Other includes: Drowning/Submersion, Fire/Burn, Fall, All Transportation, Natural Environment, Struck by/against, Other Specified, Unspecified.
P<0.01
P<0.001
DISCUSSION
In this nationally representative study of U.S. ED visits, we found no difference in youth ED visit rates for suicidal ideation and/or self-harm by urban-rural location of residence, but when we examined the subset of visits for self-harm, we found higher visit rates in small metropolitan, micropolitan, and noncore areas. These differences in ED visits for self-harm remained significant after adjustment for population demographics. ED visit rates for self-inflicted firearm injuries were higher in rural than in urban areas. Understanding suicide-related healthcare visits by level of urbanization is important, as it may help identify geographic areas of highest risk and focus prevention efforts.
There are limited prior studies that compare rates of suicidal ideation and self-harm in youth between rural and urban settings. Youth are nearly twice as likely to die by suicide in rural compared to urban areas, but prior studies have not examined ED visit rates or differences in self-injury mechanisms with attention to urban and rural location. [2] In a large national sample, the number of ED visits for suicide attempts and ideation among youth doubled between 2007 and 2015.[11] Our finding that nearly 300,000 ED visits occurred nationally among youth for suicidal ideation and self-harm in 2016, with more than one-third of those for self-harm, indicates the scale of this national mental health crisis. As presentations to the ED only reflect cases that are recognized and deemed to require emergent evaluation, the prevalence of youth suicidal ideation and self-harm in the overall population is likely much greater.
Youth ED visits for self-harm could be higher in rural areas for several reasons. Prior literature has described higher injury-related ED visit rates in rural compared to urban areas, although intentional self-injury accounts for only a small proportion of all injuries.[34] Disparities in access to mental health care exist in rural areas, with shortages of mental health providers such as psychiatrists and psychologists leading to unmet mental health needs.[35–37] Moreover, national survey data indicate that mental, behavioral, and developmental disorders are more prevalent among children in rural areas.[38] Because rural families have lower family incomes, they are less likely to have health insurance with adequate mental health benefits.[39] Rural residents travel longer distances to seek care, with transportation problems more frequently reported as a barrier to care.[40,41] Due to the small size of rural communities, rural residents may have greater concerns regarding lack of anonymity when seeking mental health care.[2] Together, these factors may cause rural youth to delay accessing outpatient mental health services until more serious symptoms or crisis develop.
Prior literature has demonstrated regional differences by U.S. Census regions in ED visit rates by youth for all mental health conditions combined, with the highest rates in the Midwest and lowest in the South.[18] Nationally, youth suicide deaths are also highest in the Midwest.[1] We found a similar pattern for unadjusted ED visit rates for suicidal ideation and/or self-harm, which were highest in the Midwest and lowest in the South, however these regional differences were no longer significant in our adjusted model.
In our unadjusted analysis of injury mechanisms, we found higher visit rates for self-inflicted poisoning and firearm injuries by youth in rural than in urban areas, but this relationship remained significant only for self-inflicted firearm injuries after adjusting for population demographics. Rural areas have been disproportionately affected by the opioid epidemic, and opioid misuse is associated with increased risk for suicide.[42,43] However we did not find significantly higher ED visit rates for opioid poisoning with intent to self-harm among youth in rural areas. We found a more than 3-fold higher ED visit rate for self-inflicted firearm injuries in rural areas, which is consistent with prior work demonstrating higher rural hospitalization rates for youth self-inflicted firearm injuries.[19] Youth in rural areas may have increased familiarity with and access to firearms, as rural families are more likely than urban families to own firearms.[4,44] Household firearm ownership has been correlated with higher suicide rates, and safe firearm storage in the home is protective against adolescent firearm suicide attempts.[45–47] However, only one third of firearm-owning households with children store their firearms safely (locked and unloaded), with no difference in storage practices in rural versus urban areas.[44,48] This highlights the importance of lethal means restriction as a strategy to prevent youth suicide and self-harm, particularly in rural areas.
Our findings confirm previously described differences in epidemiology between suicide-related ED visits and suicide deaths. We found that poisoning and cutting/piercing were the most common injury mechanisms among youth ED visits for self-harm.[49] We found that suffocation (such as hanging) and firearms account for a very small percentage of ED visits for self-harm, despite being the top two mechanisms involved in youth suicide death.[50] Suicide attempts via hanging and firearms have higher case-fatality rates, as many youth who attempt suicide via these mechanisms will not survive to be brought to the ED for evaluation.[51] In contrast to youth suicide deaths, which are more common among males, we confirmed that ED visits for suicidal ideation and self-harm are more common among females.[1]
We found several other notable differences between ED visits by youth for suicidal ideation and self-harm in rural versus urban areas. Visits in rural areas were more likely to involve public insurance and lower median household income, which underscores the need for public health insurance plans to incorporate comprehensive mental health benefits as a strategy to reduce rural youth suicides.[39] We found that nearly one-quarter of youth with a rural residence travel to be seen at an ED located in a metropolitan area, which may reflect the limited availability of mental health services in rural areas. After being seen in the ED, a higher proportion of rural youth are transferred to another short-term hospital, which suggests a lack of definitive mental health capacity at the initial ED. Rural EDs may not be as well prepared to care for youth with mental health needs, as few have recommended policies and transfer guidelines in place for the care of children with mental health conditions.[52,53] For rural children requiring admission for mental health conditions, only 20% are hospitalized in rural hospitals, and 30-day readmission rates at these hospitals are higher than for hospitalizations in metropolitan areas, suggesting provision of lower quality care.[54] Telepsychiatry evaluation is an emerging alternative that may enhance access and reduce the need for transfer to metropolitan areas for specialty mental health evaluation.[55]
Our study has several limitations. The primary limitation is that it relies on administrative data, in particular ICD-10-CM codes, which are subject to coding and misclassification errors. Sometimes the intent of an injury cannot be determined by ED personnel, as when the patient does not disclose the intent or when the patient’s ability to communicate is impaired by injury or intoxication. In these cases, codes for unintentional or undetermined intent may be assigned instead, and thus we likely underestimated the total number of injuries due to intentional self-harm.[56] ICD-10-CM codes for intentional self-harm do not distinguish between self-harm with suicidal intent (i.e. suicide attempt) and self-harm without intent to die (i.e. non-suicidal self-harm).[24] Also, as some suicide attempts do not result in injury, visits for self-harm described in this study do not encompass all visits for suicide attempts. The degree and extent of the injuries also cannot be determined. Race and ethnicity are not available for study in the NEDS, prohibiting their analysis. Since this study is limited to patients who presented to the ED, it cannot account for youth with suicidal ideation or self-harm who did not come to the ED, who were admitted directly to inpatient care, or who died before being transported to the ED. Finally, as there is no unique patient identifier in the NEDS dataset to allow for tracking of an individual, each unit of analysis in this study is an ED visit and not an individual patient, and we were unable to assess patterns of ED use by individuals over time.
ED visits for suicidal ideation and self-harm by youth represent a critical opportunity for risk assessment and initiation of suicide prevention interventions.[12,16] A meta-analysis of brief suicide prevention interventions delivered in acute care settings demonstrated increased linkage to follow up mental health care and a reduction in subsequent suicide attempts.[57] Components of successful interventions included: (1) brief contacts, such as follow up calls and text messages, (2) care coordination, such as scheduling visits, collaboration to reduce barriers to attendance, and handoffs to the mental health care team, and (3) safety planning interventions, which involve identifying warning signs, coping strategies, available supports, and reducing access to lethal means.[57] The Suicide Prevention Resource Center guide offers concrete steps and sample materials for implementation of these strategies.[58] The Health Services and Resources Administration “Critical Crossroads” toolkit also provides guidance for EDs on best practices for triage, screening, and assessment of youth with suicidal ideation, which are readily adaptable by low-resource EDs such as those in rural settings.[16] Recent data demonstrate higher positivity rates on ED suicide screening questions for youth since the onset of the COVID-19 pandemic, lending particular urgency to this effort.[59] Our findings may help inform resource allocation and areas of focus for ED-based programs to prevent suicide and self-harm.
At the community level, rural areas may require tailored and innovative strategies to reduce youth suicide-related ED visits and suicides. Youth living in rural areas might particularly benefit from suicide prevention efforts that address mental health provider shortages, promote increased treatment accessibility via the phone or web, and enhance youth connectedness through community engagement.[60] Pediatricians can integrate mental health care into primary care, provide education on lethal means restriction such as safe firearm storage, and work with schools and communities to implement preventive interventions.[61,62]
Supplementary Material
Funding/Support:
Supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) Children and Youth with Special Health Care Needs Research Network (UA6MC31101 [to JB]) and by the U.S. Agency for Healthcare Research and Quality (5K12HS026385-03 [to JAH]). This information or content and conclusions are those of the authors and should not be construed as the official position or policy of, nor should any endorsements be inferred by HRSA, HHS, or the U.S. Government.
Conflict of Interests Disclosure:
The authors have no conflicts of interest relevant to this article to disclose. The funder/sponsor did not participate in the study design; the collection, analysis, or interpretation of data; the writing of the report; or the decision to submit the manuscript for publication. The first draft of the manuscript was written by Dr. Jennifer Hoffmann. No honorarium, grant, or other form of payment was given to anyone to produce the manuscript.
ABBREVIATIONS
- U.S.
United States
- ED
Emergency department
- NEDS
Nationwide Emergency Department Sample
- AHRQ
Agency for Healthcare Research and Quality
- NCHS
National Center for Health Statistics
- ICD-10-CM
International Classification of Diseases, Tenth Edition, Clinical Modification
- CAMHD-CS
Child and Adolescent Mental Health Disorders Classification System
- CI
Confidence interva
Footnotes
Prior Presentation as an Abstract and Poster: Hoffmann JA, Hall M, Lorenz D, Berry J. Urban-rural differences in youth emergency department visits for suicidal ideation and self-harm. Virtual Poster at the American Academy of Pediatrics National Conference and Exhibition. October 3–5, 2020.
REFERENCES
- [1].Centers for Disease Control and Prevention: National Center for Injury Prevention and Control. Web-based Injury Statistics Query and Reporting System (WISQARS) 2005. https://www.cdc.gov/violenceprevention/suicide/statistics/index.html (accessed June 11, 2018).
- [2].Fontanella CA, Hiance-Steelesmith DL, Phillips GS, Bridge JA, Lester N, Sweeney HA, et al. Widening Rural-Urban Disparities in Youth Suicides, United States, 1996–2010. JAMA Pediatr 2015;169:466. 10.1001/JAMAPEDIATRICS.2014.3561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Hoffmann JA, Farrell CA, Monuteaux MC, Fleegler EW, Lee LK. Association of Pediatric Suicide with County-Level Poverty in the United States, 2007–2016. JAMA Pediatr 2020;174:287–94. 10.1001/jamapediatrics.2019.5678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Hirsch JK, Cukrowicz KC. Suicide in rural areas: An updated review of the literature. J Rural Ment Heal 2014;38:65–78. 10.1037/rmh0000018. [DOI] [Google Scholar]
- [5].King CA, Berona J, Czyz E, Horwitz AG, Gipson PY. Identifying Adolescents at Highly Elevated Risk for Suicidal Behavior in the Emergency Department. J Child Adolesc Psychopharmacol 2015;25:100–8. 10.1089/cap.2014.0049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Fontanella CA, Warner LA, Steelesmith D, Bridge JA, Sweeney HA, Campo JV. Clinical Profiles and Health Services Patterns of Medicaid-Enrolled Youths Who Died by Suicide. JAMA Pediatr 2020. 10.1001/jamapediatrics.2020.0002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Nock MK, Green JG, Hwang I, McLaughlin KA, Sampson NA, Zaslavsky AM, et al. Prevalence, correlates, and treatment of lifetime suicidal behavior among adolescents: Results from the national comorbidity survey replication adolescent supplement. JAMA Psychiatry 2013;70:300–10. 10.1001/2013.jamapsychiatry.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Finkelstein Y, Macdonald EM, Hollands S, Hutson JR, Sivilotti MLA, Mamdani MM, et al. Long-term outcomes following self-poisoning in adolescents: A population-based cohort study. The Lancet Psychiatry 2015;2:532–9. 10.1016/S2215-0366(15)00170-4. [DOI] [PubMed] [Google Scholar]
- [9].Grandclerc S, De Labrouhe D, Spodenkiewicz M, Lachal J, Moro M-R. Relations between Nonsuicidal Self-Injury and Suicidal Behavior in Adolescence: A Systematic Review. PLoS One 2016;11:e0153760. 10.1371/journal.pone.0153760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Lo CB, Bridge JA, Bridge JA, Bridge JA, Shi J, Shi J, et al. Children’s mental health emergency department visits: 2007–2016. Pediatrics 2020;145. 10.1542/peds.2019-1536. [DOI] [PubMed] [Google Scholar]
- [11].Burstein B, Agostino H, Greenfield B. Suicidal Attempts and Ideation Among Children and Adolescents in US Emergency Departments, 2007–2015. JAMA Pediatr 2019. 10.1001/jamapediatrics.2019.0464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Babeva K, Hughes JL, Asarnow J. Emergency Department Screening for Suicide and Mental Health Risk. Curr Psychiatry Rep 2016;18:100. 10.1007/s11920-016-0738-6. [DOI] [PubMed] [Google Scholar]
- [13].Runyan CW, Becker A, Brandspigel S, Barber C, Trudeau A, Novins D. Lethal means counseling for parents of youth seeking emergency care for suicidality. West J Emerg Med 2016;17:8–14. 10.5811/westjem.2015.11.28590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Stone D, Holland K, Bartholow B, Crosby A, Davis S, Wilkins N. Preventing Suicide: A Technical Package of Policy, Programs, and Practices. Atlanta, GA: 2017. [Google Scholar]
- [15].Horowitz L, Ballard E, Teach SJ, Bosk A, Rosenstein DL, Joshi P, et al. Feasibility of screening patients with nonpsychiatric complaints for suicide risk in a pediatric emergency department: a good time to talk? Pediatr Emerg Care 2010;26:787–92. 10.1097/PEC.0b013e3181fa8568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].U.S. Department of Health and Human Services, Health Resources and Services Administration, Maternal and Child Health Bureau. Critical Crossroads: Pediatric Mental Health Care in the Emergency Department. A Care Pathway Resource Toolkit. 2019. [Google Scholar]
- [17].Hoffmann JA, Grupp-Phelan J. Advocacy Opportunities for Pediatricians and Emergency Physicians to Prevent Youth Suicide. Clin Pediatr Emerg Med 2020;21:100776. 10.1016/j.cpem.2020.100776. [DOI] [Google Scholar]
- [18].Rogers SC, Mulvey CH, Divietro S, Sturm J. Escalating Mental Health Care in Pediatric Emergency Departments. Clin Pediatr (Phila) 2017;56:488–91. 10.1177/0009922816684609. [DOI] [PubMed] [Google Scholar]
- [19].Herrin BR, Gaither JR, Leventhal JM, Dodington J. Rural Versus Urban Hospitalizations for Firearm Injuries in Children and Adolescents. Pediatrics 2018;142:e20173318. 10.1542/peds.2017-3318. [DOI] [PubMed] [Google Scholar]
- [20].Agency for Healthcare Research and Quality, U.S. Department of Health and Human Services. Healthcare Cost and Utilization Project n.d. https://www.hcup-us.ahrq.gov/ (accessed December 9, 2019).
- [21].Agency for Healthcare Quality and Research, U.S. Department of Health and Human Services. Clinical Classifications Software Refined (CCSR) for ICD-10-CM Diagnoses n.d https://www.hcup-us.ahrq.gov/toolssoftware/ccsr/ccs_refined.jsp (accessed December 9, 2019).
- [22].Zima BT, Gay JC, Rodean J, Doupnik SK, Rockhill C, Davidson A, et al. Classification system for international classification of diseases, ninth revision, clinical modification and tenth revision pediatric mental health disorders. JAMA Pediatr 2020;174:620–2. 10.1001/jamapediatrics.2020.0037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Hedegaard H, Johnson RL, Garnett MF, Thomas KE. The International Classification of Diseases, 10th Revision, Clinical Modification (ICD–10–CM) External Cause-of-injury Framework for Categorizing Mechanism and Intent of Injury. Natl Heal Stat Rep 2019;136:1–22. [PubMed] [Google Scholar]
- [24].Canner JK, Giuliano K, Selvarajah S, Hammond ER, Schneider EB. Emergency department visits for attempted suicide and self harm in the USA: 2006–2013. Epidemiol Psychiatr Sci 2018;27:94–102. 10.1017/S2045796016000871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].U.S. Census Bureau. Population Estimates by Age, Sex, Race and Hispanic Origin n.d https://www.census.gov/newsroom/press-kits/2018/estimates-characteristics.html (accessed February 9, 2019).
- [26].National Center for Health Statistics. NCHS Urban-Rural Classification Scheme for Counties n.d https://www.cdc.gov/nchs/data_access/urban_rural.htm (accessed December 9, 2019).
- [27].Zhang W, Mason AE, Boyd B, Sikich L, Baranek G. A Rural–Urban Comparison in Emergency Department Visits for U.S. Children with Autism Spectrum Disorder. J Autism Dev Disord 2017;47:590–8. 10.1007/s10803-016-2982-3. [DOI] [PubMed] [Google Scholar]
- [28].U.S. Census Bureau. County Intercensal Datasets: 2000–2010 n.d https://www.census.gov/data/datasets/time-series/demo/popest/intercensal-2000-2010-counties.html (accessed February 9, 2019).
- [29].Rao J, Scott G. On Chi-squared Tests For Multiway Contingency Tables with Proportions Estimated From Survey Data. Ann Stat 1984;12:46–60. [Google Scholar]
- [30].Houchens R, Elixhauser A. HCUP Methods Series Report: Final Report on Calculating Nationwide Inpatient Sample (NIS) Variances for Data Years 2011 and Earlier. 2015.
- [31].R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing. Vienna, Austria: 2020. [Google Scholar]
- [32].Lumley T Analysis of complex survey samples. J Stat Softw 2004;9:1–19. [Google Scholar]
- [33].Lumley T Survey: Analysis of complex survey samples. R package version 4.0 2020. [Google Scholar]
- [34].Kim K, Ozegovic D, Voaklander DC. Differences in incidence of injury between rural and urban children in Canada and the USA: A systematic review. Inj Prev 2012;18:264–71. 10.1136/injuryprev-2011-040306. [DOI] [PubMed] [Google Scholar]
- [35].Thomas KC, Ellis AR, Konrad TR, Holzer CE, Morrissey JP. County-Level Estimates of Mental Health Professional Shortage in the United States. Psychiatr Serv 2009;60:1323–8. 10.1176/ps.2009.60.10.1323. [DOI] [PubMed] [Google Scholar]
- [36].McBain RK, Kofner A, Stein BD, Cantor JH, Vogt WB, Yu H. Growth and Distribution of Child Psychiatrists in the United States: 2007–2016. Pediatrics 2019;144. 10.1542/peds.2019-1576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].WWAMI Rural Health Research Center. Supply and Distribution of the Behavioral Health Workforce in Rural America. 2016.
- [38].Robinson LR, Holbrook JR, Bitsko RH, Hartwig SA, Kaminski JW, Ghandour RM, et al. Differences in Health Care, Family, and Community Factors Associated with Mental, Behavioral, and Developmental Disorders Among Children Aged 2–8 Years in Rural and Urban Areas — United States, 2011–2012. MMWR Surveill Summ 2017;66:1–11. 10.15585/mmwr.ss6608a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].U.S. Department of Health and Human Services, Health Resources and Services Administration. The Health and Well-Being of Children in Rural Areas: A Portrait of the Nation 2007. Rockville, MD: 2011. [Google Scholar]
- [40].Probst JC, Laditka SB, Wang JY, Johnson AO. Effects of residence and race on burden of travel for care: Cross sectional analysis of the 2001 US National Household Travel Survey. BMC Health Serv Res 2007;7. 10.1186/1472-6963-7-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Skinner AC, Slifkin RT. Rural/urban differences in barriers to and burden of care for children with special health care needs. J Rural Heal 2007;23:150–7. 10.1111/j.1748-0361.2007.00082.x. [DOI] [PubMed] [Google Scholar]
- [42].Paulozzi LJ, Xi Y. Recent changes in drug poisoning mortality in the United States by urban-rural status and by drug type. Pharmacoepidemiol Drug Saf 2008;17:997–1005. 10.1002/pds.1626. [DOI] [PubMed] [Google Scholar]
- [43].Chesney E, Goodwin GM, Fazel S. Risks of all-cause and suicide mortality in mental disorders: A meta-review. World Psychiatry 2014;13:153–60. 10.1002/wps.20128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].DuRant RH, Barkin S, Craig JA, Weiley VA, Ip EH, Wasserman RC. Firearm ownership and storage patterns among families with children who receive well-child care in pediatric offices. Pediatrics 2007;119:e1271–9. 10.1542/peds.2006-1485. [DOI] [PubMed] [Google Scholar]
- [45].Miller M, Lippmann SJ, Azrael D, Hemenway D. Household Firearm Ownership and Rates of Suicide Across the 50 United States. J Trauma Inj Infect Crit Care 2007;62:1029–35. 10.1097/01.ta.0000198214.24056.40. [DOI] [PubMed] [Google Scholar]
- [46].Grossman DC, Mueller BA, Riedy C, Dowd MD, Villaveces A, Prodzinski J, et al. Gun Storage Practices and Risk of Youth Suicide and Unintentional Firearm Injuries. JAMA 2005;293:707. 10.1001/jama.293.6.707. [DOI] [PubMed] [Google Scholar]
- [47].Monuteaux MC, Azrael D, Miller M. Association of Increased Safe Household Firearm Storage with Firearm Suicide and Unintentional Death among US Youths. JAMA Pediatr., vol. 173, American Medical Association; 2019, p. 657–62. 10.1001/jamapediatrics.2019.1078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Azrael D, Cohen J, Salhi C, Miller M. Firearm Storage in Gun-Owning Households with Children: Results of a 2015 National Survey. J Urban Heal 2018;95. 10.1007/s11524-018-0261-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Sulyman N, Kim MK, Rampa S, Allareddy V, Nalliah RP, Allareddy V. Self Inflicted Injuries among Children in United States – Estimates from a Nationwide Emergency Department Sample. PLoS One 2013;8:e69874. 10.1371/journal.pone.0069874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Ruch DA, Sheftall AH, Schlagbaum P, Rausch J, Campo JV, Bridge JA. Trends in Suicide Among Youth Aged 10 to 19 Years in the United States, 1975 to 2016. JAMA Netw Open 2019;2:e193886. 10.1001/jamanetworkopen.2019.3886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Elnour AA, Harrison J. Lethality of suicide methods. Inj Prev 2008;14:39–45. 10.1136/ip.2007.016246. [DOI] [PubMed] [Google Scholar]
- [52].Iglehart JK. The Challenging Quest to Improve Rural Health Care. N Engl J Med 2018;378:473–9. 10.1056/NEJMhpr1707176. [DOI] [PubMed] [Google Scholar]
- [53].Pilkey D, Edwards C, Richards R, Olson LM, Ely M, Edgerton EA. Pediatric Readiness in Critical Access Hospital Emergency Departments. J Rural Heal 2019;35:480–9. 10.1111/jrh.12317. [DOI] [PubMed] [Google Scholar]
- [54].Bettenhausen JL, Hall M, Doupnik SK, Markham JL, Feinstein JA, Berry JG, et al. Hospitalization Outcomes for Rural Children with Mental Health Conditions. J Pediatr 2021;229:240–246.e1. 10.1016/j.jpeds.2020.09.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [55].Roberts N, Hu T, Axas N, Repetti L. Child and Adolescent Emergency and Urgent Mental Health Delivery Through Telepsychiatry: 12-Month Prospective Study. Telemed e-Health 2017;23:842–6. 10.1089/tmj.2016.0269. [DOI] [PubMed] [Google Scholar]
- [56].Hedegaard H, Schoenbaum M, Claassen C, Crosby A, Holland K, Proescholdbell S. Issues in Developing a Surveillance Case Definition for Nonfatal Suicide Attempt and Intentional Self-harm Using International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) Coded Data. 2018. [PubMed] [Google Scholar]
- [57].Doupnik SK, Rudd B, Schmutte T, Worsley D, Bowden CF, McCarthy E, et al. Association of Suicide Prevention Interventions with Subsequent Suicide Attempts, Linkage to Follow-up Care, and Depression Symptoms for Acute Care Settings: A Systematic Review and Meta-analysis. JAMA Psychiatry 2020. 10.1001/jamapsychiatry.2020.1586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [58].Allen M, Anna Gary Behrman C, Jon Berlin L, Berman L, Bernstein E, Emmy Betz F, et al. Caring for Adult Patients with Suicide Risk: A Consensus Guide for Emergency Departments. 2015.
- [59].Hill RM, Rufino K, Kurian S, Saxena J, Saxena K, Williams L. Suicide Ideation and Attempts in a Pediatric Emergency Department Before and During COVID-19. Pediatrics 2020:e2020029280. 10.1542/peds.2020-029280. [DOI] [PubMed] [Google Scholar]
- [60].Kegler SR, Stone DM, Holland KM. Trends in Suicide by Level of Urbanization — United States, 1999–2015. MMWR Morb Mortal Wkly Rep 2017;66:270–3. 10.15585/mmwr.mm6610a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [61].Walter HJ, Vernacchio L, Trudell EK, Bromberg J, Goodman E, Barton J, et al. Five-Year Outcomes of Behavioral Health Integration in Pediatric Primary Care. Pediatrics 2019:e20183243. 10.1542/PEDS.2018-3243. [DOI] [PubMed] [Google Scholar]
- [62].Wasserman D, Hoven CW, Wasserman C, Wall M, Eisenberg R, Hadlaczky G, et al. School-based suicide prevention programmes: the SEYLE cluster-randomised, controlled trial. Lancet 2015;385:1536–44. 10.1016/S0140-6736(14)61213-7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


