Abstract
Background:
Theoretical and empirical evidence suggests that maternal anxiety relates to overprotection, yet studies have found conflicting evidence. The literature would benefit from a systematic review.
Methods:
In April 2020, a systematic review on the relation between maternal anxiety and overprotection was conducted. The search was updated in January 2021. A total of 13 articles were included.
Results:
Of 16 reported bivariate correlations, 12 showed that maternal anxiety accounted for significant variance in overprotection (7 reported a small effect and 5 reported a medium effect). In a group differences study, mothers with anxiety showed greater overprotection. Additionally, in 4 out of 7 multivariate relations maternal anxiety accounted for significant variance in overprotection over and above other factors while 3 suggested that maternal anxiety did not account for significant variance in overprotection. In a multivariate, longitudinal study, maternal anxiety predicted overprotection, over and above other factors. Given conflicting evidence, we evaluated article’s methodological strength and found stronger evidence supporting a small to medium size relation compared to evidence supporting no significant relation.
Limitations:
We report ranges of coefficients and effect sizes, but meta-analytic results are needed to determine the magnitude of these relations based on various factors. More longitudinal studies are needed to determine directionality.
Conclusions:
Although the literature shows conflicting results, the present review supports that maternal anxiety relates to overprotection, though the effect of this relation is small to medium. It may be beneficial to incorporate mental health for parents into existing parenting interventions.
Keywords: Maternal anxiety, overprotection, parenting, parent-child relations
Introduction
Overprotective parenting, a parenting behavior falling under the larger umbrella of overcontrolling parenting, has often been implicated in the development of child anxiety disorders and symptoms (Bögels & van Melick, 2004; Creveling et al., 2010; Nishikawa et al., 2010). Anxiety disorders and symptoms are prevalent in childhood and persist into adulthood (Costello et al., 2005; Ghandour et al., 2019). To develop effective interventions for families who have children with or at risk for anxiety, it is essential to understand factors that may predict parenting behaviors that heighten children’s anxiety symptoms.
Despite a robust body of literature showing the negative effects of overprotective parenting (Costa & Weems, 2005; Creveling et al., 2010; Nishikawa et al., 2010; Reitman & Asseff, 2010), little research has identified factors that contribute to these behaviors. Maternal characteristics, such as maternal anxiety, may relate to greater use of overprotection (Bögels & van Melick, 2004; Clarke et al., 2013; Root et al., 2016). Research has identified theoretical and empirical evidence for this relation (Bögels & van Melick, 2004; Clarke et al., 2013; Root et al., 2016), but the literature also shows conflicting evidence (Ginsburg et al., 2004; Manassis & Bradley, 1994; Moore et al., 2004). It is imperative that we understand if there is enough empirical evidence to support the link between maternal anxiety and overprotection to inform future research and design effective clinical interventions. Therefore, the present review will systematically evaluate the evidence for the link between maternal anxiety and overprotection and propose avenues for future research.
Overprotective Parenting
Overprotection is defined as unnecessarily supportive and warm parenting behaviors that limit children’s opportunities to cope independently with developmentally appropriate challenges (Chorpita & Barlow, 1998; Rubin et al., 1997). These behaviors can jeopardize children’s sense of mastery over their environment, decreasing their self-competence, and fostering dependence on the caregiver (Affrunti & Ginsburg, 2012; Chorpita & Barlow, 1998; Hudson & Rapee, 2004; Wood, 2006). Additionally, overprotection can communicate to children that the world is a dangerous place, encourage and reinforce avoidance, and limit children’s chances to approach challenges that can foster confidence and skill building (Chorpita & Barlow, 1998; Rapee, 1997). In order to improve the mental health of children and families, it is important to study and prevent overprotective behaviors in environments where children are faced with developmentally appropriate challenges.
Several decisions were made when determining the criteria for the current review. First, we focused our search on overprotection rather than on autonomy granting because previous research suggests that these variables may be distinct constructs rather than opposite ends of a continuum (Silk et al., 2003) and the literature has shown inconsistent correlations between autonomy granting and overprotection (Holmbeck et al., 2002). Second, we limited our search to overprotection in mothers of infants, toddlers, and children (i.e., aged approximately 0–12 years old) because overprotection may play a particularly important role in earlier years when the family environment is a dominant source of influence on development (Baumrind, 1967). Finally, we studied overprotection in mothers as the majority of research on parenting related to child anxiety has tested the influence of maternal parenting (Bögels & Phares, 2008), despite growing literature supporting the importance of fathers and other caregivers on development.
Maternal Anxiety
Maternal anxiety may be a trait that is relevant to maternal overprotection, as mothers with anxiety may engage in overprotective parenting as a way of decreasing their own distress (Turner et al., 2003). Additionally, mothers with anxiety may engage in overprotection because of a greater tendency to perceive threats to their children in the environment (Lindhout et al., 2006). Cognitive theories for anxiety suggest that anxiety leads to a narrowing of attention and an attentional bias towards threat (Becker et al., 2001; Najmi et al., 2012). Additionally, individuals with anxiety show hypervigilance, in which an individual scans the environment for threats, resulting in a greater likelihood of detecting potentially threatening cues in the environment (Eysenck, 1992). Indeed, numerous studies have found that maternal anxiety is related to greater use of overprotection (Bögels & van Melick, 2004; Clarke et al., 2013; Root et al., 2016). However, the literature also shows conflicting evidence for this relation (Ginsburg et al., 2004; Manassis & Bradley, 1994; Moore et al., 2004), suggesting the need to systematically review the literature on the relation between maternal anxiety and overprotection in order to determine whether the relation is robust.
Despite numerous studies testing the link between maternal anxiety and overprotection, a systematic review of these studies has not been conducted. A meta-analysis testing the relation between parent anxiety and parental overcontrol was conducted, but no studies examining overprotection were included (van der Bruggen et al., 2008). Instead, the authors included articles testing parental control, psychological control, negative control, parental control involvement, intrusiveness, command, watching or controlling, restriction, and granting of autonomy. Although some aspects of overprotection may be captured in these constructs, authors have argued that within the broader construct of parental control, overprotection is especially influential in child anxiety development because it encourages an avoidant coping style (Hudson & Rapee, 2004; Rubin et al., 2009). Thus, overprotection must be studied, specifically.
Research also suggests that children are active contributors to the parenting they receive (Dadds & Roth, 2001). Although not the focus of the present review, it is important to note that parenting takes place in an interaction between the parent and the child. Thus, maternal anxiety likely will not explain all of the variance in overprotection. However, determining if maternal anxiety is one of the robust predictors of overprotection is necessary to move the literature forward and effectively develop interventions for overprotection and child anxiety development.
Objectives of the review
Although current literature theorizes that maternal anxiety contributes to greater use of overprotective parenting behaviors, it is unclear whether this relation has substantial empirical support. Therefore, the aim of the current review is to systematically evaluate the existing literature on the relation between maternal anxiety and overprotection. Specifically, this review will (1) evaluate empirical studies that report statistics on the association between maternal anxiety and overprotective parenting and (2) discuss strengths and limitations of the current literature, providing directions for future research to advance our understanding of the influence of maternal anxiety and overprotection.
Method
Literature Review
A literature search using PsycINFO and Pubmed was conducted in April 2020. An updated search was conducted in January 2021 to determine if any additional articles were published that should be included in the current study. However, no additional articles met the inclusion criteria. Search terms and word stems for anxiety included “anxi-” and “worr-,” which were cross referenced with the following terms for mother, “maternal,” “mother-,” and “parent-,” and the following terms for overprotection, “overpro-,” “prot-,” “control-,” and “overcontrol.” Additionally, in order to limit the search to studies that included parents of children rather than adolescents, the search terms included “not adolescent” and “not teen-.” Publication type was restricted to academic articles and empirical studies that were written in English. Due to this restriction, gray literature including doctoral dissertations were not included in the current review, the strengths and limitations of which are included in the discussion section. Additionally, articles were limited to a publishing date between January 2010 and April 2020 in order to limit the overlap between the review of parental anxiety and overcontrol that was published in 2008 (van der Bruggen et al., 2008) and to focus on the most recent literature.
Abstracts and titles were subsequently screened to eliminate irrelevant articles based on the inclusion criteria outlined below. Additionally, after completing the literature search in each database, the reference sections of all identified manuscripts were screened for additional studies. Once the initial screening process was completed, the full texts of articles that passed the screening process were reviewed for inclusion by the author and a second reviewer. Initially, the two reviewers agreed on 90% of the articles. All noted discrepancies were discussed and a final decision was made based on the inclusion criteria.
Inclusion Criteria
The studies that were used for this systematic review met the following four primary inclusion criteria: (1) tested maternal anxiety in relation to overprotective parenting and reported a statistic of this association, (2) measured maternal anxiety through anxiety symptoms, worry, or diagnosed anxiety but not through internalizing problems, a combination of anxiety and depression, or anxiety sensitivity (3) used a sample of mothers with children who were in the developmental period of infancy to middle childhood (i.e., approximately 0–12 years old) (4) reported statistics specifically for mothers or had a sample that was 80% or more mothers rather than a more even combination of mothers and fathers. Studies that tested overcontrolling parenting (e.g., intrusive, overcontrol, psychological control), autonomy granting, or anxious modeling rather than overprotection were excluded from the review in order to focus on the specific relation between maternal anxiety and overprotection.
One difficulty of the current literature is the many different measures used to test overprotection. In order to determine if each of these measures of overprotection fit the inclusion criteria of the current study, each method section was carefully reviewed in the phase of the literature search where full-text articles were examined for eligibility. Specifically, the author examined Bayer et al.’s (2006, 2010) overinvolved/protective parenting scale used in Bayer et al. (2019) and Cooklin et al. (2013), the overprotection subscale used in Root et al. (2016; i.e., 14 items reflecting discouragement of independence and protectiveness from the Child Rearing Practices Report; Chen et al., 1998), the overprotection/over-controlling subscale of the Parental Bonding Instrument (Parker et al., 1979) used in Booker et al. (2018), the composite of the parental overprotection and parental anxiety and concern scales from the Anxiety and Overprotection Scale (Pereira et al., 2013) used in Pereira et al. (2014), and the EMBU (Egna Minnen Beträffande Uppfostran; Castro et al., 1997; Castro et al., 1993). Given the studies’ descriptions of these measures and the example items provided, it was determined that each of these scales other than the EMBU met the current review’s definition of overprotection (i.e., unnecessarily supportive and warm parenting behaviors that limit children’s opportunities to cope independently with developmentally appropriate challenges, communicate to children that the world is a dangerous place, encourage and reinforce avoidance, and limit children’s chances to approach challenges that can foster confidence and skill building; Chorpita & Barlow, 1998; Rapee, 1997). The EMBU was used in three articles that would have otherwise met criteria for the current review (Affrunti & Ginsburg, 2012a; Affrunti & Ginsburg, 2012b; Drake & Ginsburg, 2011). However, upon close examination, the subscale of this measure labeled, “control attempts/overprotection” was determined to fall more closely under the definition of overcontrol more broadly, rather than overprotection specifically. Therefore, any articles using this measure of overprotection were excluded from the current review.
Study selection
Figure 1 summarizes the number of articles that were retained at each step of the review. After completing an initial search, screening the titles, screening the abstracts, and screening the reference sections of identified articles, a total of 141 full-text articles were obtained and screened. Of the 141 full-text articles, 128 articles were excluded because they did not meet the inclusion criteria. In summary, 13 articles were included in the current systematic review.
Figure 1.
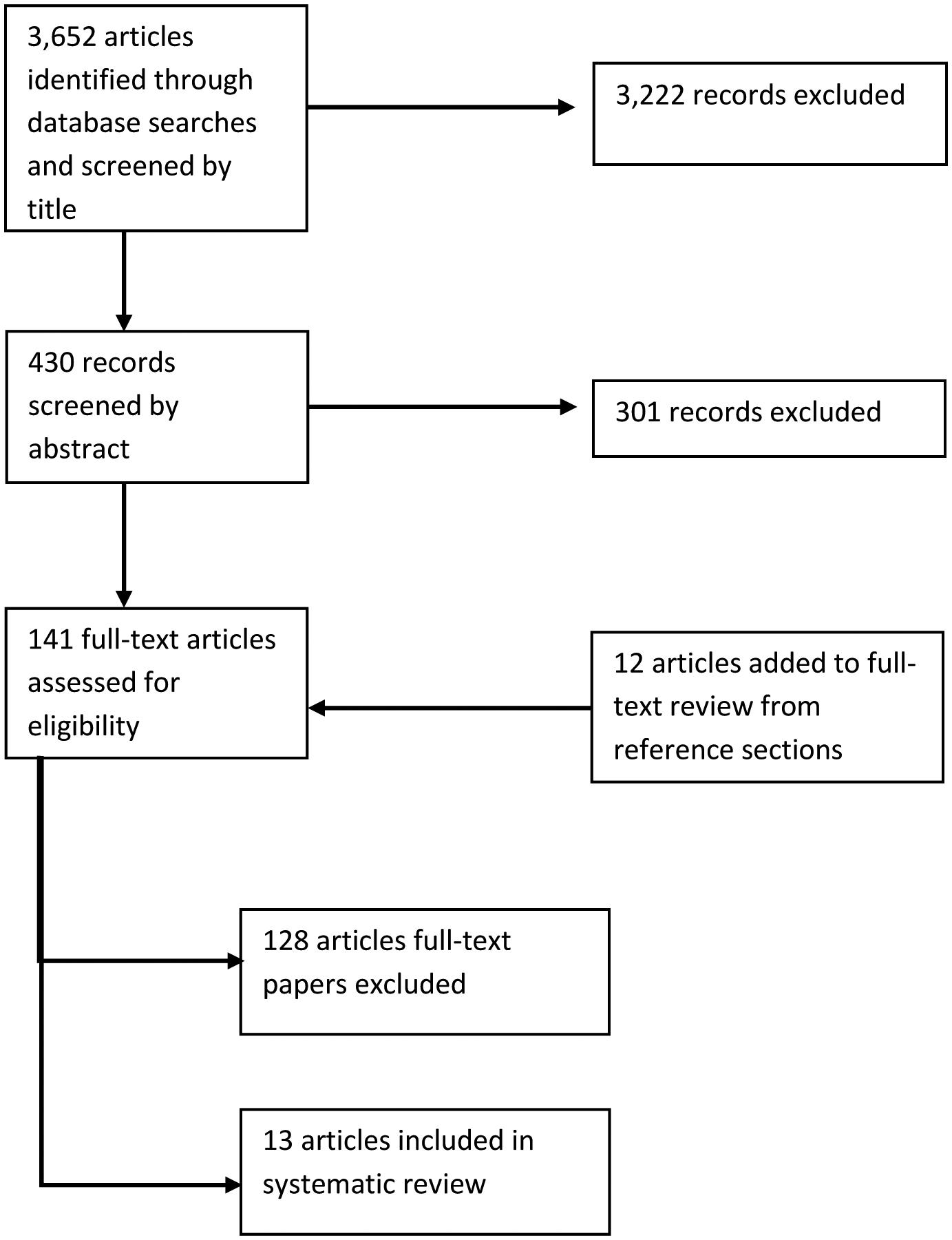
Search Strategy and Results
A summary of relevant sample information for each of the 13 articles is included in Table 1 (e.g., number of participants, child age, maternal race, location [i.e., country]). Additionally, Table 1 includes how maternal anxiety and overprotection were measured, the study design, and effect sizes for the relation between maternal anxiety and overprotection. The type of effect sizes presented varied based on the specific analyses used. Pearson’s r was reported if correlational analyses were used for the relation between maternal anxiety and overprotection, and semi-partial correlations or standardized beta coefficients were reported for multivariate analyses. Although some researchers argue that beta coefficients can signify effect-size (Farley et al., 1995; Rosenthal & DiMatteo, 2001), it is generally recommended that beta coefficients should not be used in replacement of correlation coefficients as a way to determine effect size (Hunter & Schmidt, 1990). However, standardized beta coefficients are easily comparable and can be helpful in assessing the relative strength of predictors. Additionally, Peterson and Brown (2005) found that the relation between corresponding standardized beta coefficients and correlation coefficients is robust and independent of sample size and number of predictor variables. Because the current review is not a meta-analysis that would use the effect size values for quantitative tests, the strengths listed above outweigh the concerns related to discussing standardized betas and using them as evidence for the relation between maternal anxiety and overprotection. Therefore, although standardized betas will not be used as an effect size in the current review, they will be reported and discussed.
Table 1.
Description of Retained Studies.
| Study | n, race, sample | Child Age (Range, M, SD) | Maternal Anxiety Measure | Overprotection Measure | Method Design | Results of relation between anxiety and overprotection | Strength of methodology/Risk of bias score |
|---|---|---|---|---|---|---|---|
| Bayer et al., 2019 |
n = 545 parents (94% mothers); Race/ethnicity not reported; Recruited if child was inhibited; Australia |
M = 4.5 years, SD = 0.4 | DASS (anxiety subscale) | Bayer et al.’s (2006, 2010) overinvolve d/protective parenting scale | Correlation; Longitudinal | DASS and overinvolved/protective at age 4 (r = .20), age 5 (r = .13), age 6 (r = .08) | 5 |
| Booker et al., 2018 |
n = 113 (not specified how many mothers versus fathers but data is reported separately for mothers and fathers); Race and ethnicity not reported; Children from a clinical sample; United States |
6–15 years (M = 8.77 years, SD = 1.75) | BSI (anxiety subscale) | PBI (self-report and child report) | Correlation and multivariate; Cross-sectional | BSI and PBI (self-report; r = .07) BSI and PBI (child-report; r = .31); BSI did not uniquely predict overprotection for the self-report PBI over and above months since intervention, treatment group (trends over time), and maternal grandmother’s level of overprotection (b = 0.22, SE = 0.18; d = 0.06); or the child-report PBI over and above months since intervention and child gender (b = −0.27, SE = 0.29; d = −0.07). |
5 |
| Clarke et al., 2013 |
n = 90; 89% White British Origin; Children were clinical sample and non-clinical controls; English |
7–12 years (M = 9.30 years, SD = 1.40) | DASS (anxiety subscale) | OP | Multivariate; Cross-sectional | Association between DASS (anxiety subscale) and OP controlling for child age and maternal depression (ß = 0.27, b = 0.63, SE = 0.29). | 3 |
| Cooklin et al., 2013 |
n = 3,103; Race/ethnicity not reported; Community sample; Australia |
Wave 1: 3–12 months Wave 2: 2–3 years |
MSAS | Bayer et al.’s (2006, 2010) overinvolve d/protective parenting scale | SEM; Longitudinal |
MSAS wave 1 and overprotective parenting wave 2 (ß=.49) | 3 |
| Creswell et al., 2013 |
n = 88; 81.82% White British Origin; Children were clinical sample; Mothers were half clinical sample and half non-clinical sample; England |
7–12 years | ADIS; DASS (anxiety subscale) | Observed behaviors in 3 tasks (i.e., speech, tangram puzzles, and black box); Measured dichotomously | Group differences; Cross-sectional |
Maternal anxiety group differences in overprotection (b = 0.12, 95% CI = [0.001, 20.95]) | 1 |
| Fliek et al., 2015 |
n = 105; Did not report race/ethnicity; Community sample; Belgium |
2–6 years (M = 4.27 years, SD = 1.07) | STAI | POM | Correlation; Cross-sectional | STAI and POM (r = .02) | 4 |
| Gibler et al., 2018 |
n = 94; 92.55% European American, 1.06% African American, 4.26% Asian American, 2.13% Latina; Community sample; United States |
n = 60 (M = 14.11 months, SD = 1.34); n = 34 (M = 26.59 months, SD = 1.93) | DASS (anxiety subscale) | CRPR (overprotection subscale) | Correlation and multivariate; Cross-sectional | DASS and CRPR (r = .15); Path between DASS and CRPR in model of relations among paternal anxiety, maternal anxiety, paternal overprotection, maternal overprotection, and child anxiety risk (b = 0.10, SE = 0.08) | 4 |
| Kalomiris & Kiel, 2016 | n = 117; 87% European American, 3% African American, 5% Asian American, 1% American Indian, 2% other, 1% Latina; Community sample; United States | 23.97–27.00 months (M = 24.71 months) | PSWQ | NFV; Observed behaviors (composite of behaviors during interaction with a clown and a puppet show) | Correlation; Cross-sectional | PSWQ and NFV (r = .23) PSWQ and Observed OP (r = .14) Association between PSWQ and NFV (b = 0.11, SE = 0.05, t = 2.14, p = 0.36) and PSWQ and observed OP (b = 0.02, SE = 0.01, t = 1.15, p = 0.253 controlling for primiparous motherhood |
2 |
| Kiel & Maack, 2012 |
n = 91; 90% European American, 2% African American, 6% Asian American, 2% Other; Community sample; United States |
(M = 24.74 months, SD = 0.70) | SIAS | NFV | Correlation; Cross-sectional | SIAS and NFV (r = .06) | 4 |
| Kiel et al., 2019 |
n = 108; 88.0% European American, 1.9% African American, 3.7% Asian or Pacific Islander, 0.9% Native American; 0.9% Other; 1.9% Hispanic or Latina; Community sample; United States |
24 to 30 months old (M = 26.84 months, SD = 2.10 months) | DASS (anxiety subscale); PSWQ; SIAS | NFV | Correlation; Cross-sectional | DASS and NFV (r = .36); PSWQ and NFV (r = .34); SIAS and NFV (r = .26) |
4 |
| Orgilés et al., 2018 |
n = 235; Race/ethnicity not reported; Community sample; Spain |
3–6 years (M = 4.07 years, SD = 1.11) | STAI | PEE | Multivariate; Cross-sectional | STAI and PEE (r = .41); STAI on PEE over and above child sex, child age, # of siblings, maternal age, and assertive, punitive, and inhibited parenting, (ß = .12, SE = 0.02, 95% CI = [0.08, 0.15], p < 0.001) | 4 |
| Pereira et al., 2014 |
n = 80 (not specified how many mothers versus fathers but data is reported separately for mothers and fathers); Race/ethnicity not reported; Children were clinical sample and non-clinical controls; Portugal |
7–12 years (M = 9.84 years, SD = 1.23) | STAI | EASP | Correlation; Cross-sectional | STAI and EASP (r = .42) | 4 |
| Root et al., 2016 |
n = 66; 97% Caucasian, 3% did not report; Community sample; United States |
4-year olds (M = 50.95 months, SD = 1.35) | Composite of the Leary Interaction Anxiousness Scale and the Cheek and Buss Shyness Scale | CRPR (overprotective subscale) | Multivariate | Anxiety composite and CRPR (r = .21); In moderation analysis, maternal anxiety related to overprotection at mean and low vagal regulation (i.e., mean RSA; ß = .24, low ß = .50) | 4 |
Note. n = number of mothers in the study unless specified that total n is fathers and mothers.
Sample Characteristics
The 13 articles included in this review were published from 2012 to 2019. The studies took place in six different countries including the United States (n = 6), England (n = 2), Australia (n = 2), Spain (n = 1), Portugal (n = 1), and Belgium (n = 1). Sample sizes ranged from n = 66 (Root et al., 2016) to n = 3,103 (Cooklin et al., 2013), with most studies (n = 9) having between 80 and 120 participants. The majority of studies included in the review used a community sample (n = 9), with the remainder of studies using a mixed community and clinical sample of children (n = 2), or a solely clinical sample of children (n = 2). The developmental stage of children in the included studies were evenly split among toddlerhood (n = 5), early childhood (n = 4), and middle childhood (n = 4). Of the studies in the middle childhood range, three included children ages 7–12 years, whereas Booker et al. (2018) included children ages 6–15 years. Even though the upper end of this age range included adolescents, the study was retained because the mean age of the sample was 8.77 years (SD = 1.75). Thus, it stands to reason that the results of the study are likely driven by individuals in the middle childhood age range.
Method Characteristics
Study Design
The majority of the studies included in the review used a concurrent design (n = 11). However, two studies utilized a longitudinal design (Bayer et al., 2019; Cooklin et al., 2013).
Measures of Maternal Anxiety
Various measures were used to assess maternal anxiety disorders and symptomatology. The anxiety subscale of the Depression Anxiety Stress Scale (DASS; Lovibond & Lovibond, 1995; n = 3) and the State Trait Anxiety Inventory (STAI; Spielberger et al., 1970; n = 3) were the most commonly used measures. Fliek et al. (2015) used the Dutch translation of the STAI (Van der Ploeg et al., 1980), and Orgiles et al. (2018) used the Spanish version of the STAI (Fonseca-Pedrero et al., 2012). The remainder of the studies used the anxiety subscale of the Brief Symptoms Inventory (BSI; Derogatis, 1975), six items from the Maternal Separation Anxiety Scale (MSAS; Hock et al., 1988; Hock et al., 1989), the Penn State Worry Questionnaire (PSWQ; Meyer et al., 1990), and the Social Interaction Anxiety Scale (SIAS; Mattick & Clarke, 1998). Additionally, Root et al. (2016) used a composite of the Leary Interaction Anxiousness Scale (Leary & Kowalski, 1993) and the Revised Cheek and Buss Shyness Scale (Cheek, 1983; Cheek & Buss, 1981). Kiel et al. (2019) used three separate measures of maternal anxiety (i.e., DASS, PSWQ, and SIAS) and provided correlations between overprotection and each measure.
One study utilized a multimethod approach for assessing maternal anxiety (Creswell et al., 2013). Creswell et al. (2013) used the Anxiety Disorders Interview Schedule for DSM-IV (ADIS-IV; Brown et al., 2004) to differentiate mothers with an anxiety disorder and mothers without an anxiety disorder. The authors also used the DASS Anxiety subscale (Lovibond & Lovibond, 1995), but they did not report any statistic testing the relation between the DASS anxiety subscale and overprotection. Therefore, only the ADIS-IV is discussed from this study in the current review.
Measures of Maternal Overprotection
Various measures were also used to measure maternal overprotection. The majority of studies used a self-report measure of overprotection. The most common measures used were the overprotection subscale of the New Friends Vignettes (NFV; McShane & Hastings, 2009; n = 3) and Bayer et al.’s (2006, 2010) overinvolved/protective parenting scale (n = 2). Two studies used the Child Rearing Practices Report (CRPR; Block, 1965; Rickel & Biasatti, 1982; n = 2) as a measure of overprotection, but they calculated this in different ways. The first, Root et al. (2016), calculated overprotection using 14 items reflecting discouragement of independence and protectiveness based on a previous study (Chen et al., 1998). The second, Gibler et al. (2018), used 4 items as a measure of overprotection. Other measures of overprotection included the Parental Overprotection Measure (OP; Edwards et al., 2008; n = 1), the overprotective subscale of the Profile of Parenting Styles (PEE; Magaz & García, 1998; n = 1), and a composite of the parental overprotection and parental anxiety and concern scales from the Anxiety and Overprotection Scale (EASP; Pereira et al., 2013; n = 1).
Booker et al. (2018) used the overprotection/over-controlling subscale of the Parental Bonding Instrument (PBI; Parker et al., 1979) but included both a self-report version and a child-report version. The authors reported the correlation between maternal anxiety and the PBI self-report as well as the correlation between maternal anxiety and the PBI child-report.
Two studies used an observational measure of overprotection. Creswell et al. (2013) coded for overprotective behaviors in three tasks (i.e., speech task, tangram puzzles task, and black box task) based on scales developed by Murray et al. (2012). Behaviors were coded on a scale of 1 to 5 with high scores indicating pervasive and strong uses of overprotective behaviors defined as initiating emotional or practical support that is not required (e.g., stroking, kissing, unnecessarily helping when child is coping independently). Mean scores on each of the three tasks were summed to provide a total score across all three tasks (Creswell et al., 2013). Additionally, the study dichotomized scores on overprotection according to the presence or absence of the behavior because the distribution of overprotective behaviors was highly skewed (Creswell et al., 2013). Kalomiris and Kiel (2016) used two separate measures of overprotection and provided correlations between maternal anxiety and each measure. Additionally, they tested the relation between maternal anxiety and overprotection over and above primiparous parent status. The authors used the overprotection subscale of the NFV (McShane & Hastings, 2009) as a self-report measure of overprotection, and they coded for overprotective behaviors using a composite of behaviors observed during a puppet show and an interaction with a friendly clown (Buss, 2011). Behaviors were coded on a scale of 0 to 3 with high scores reflecting excessive physical affection and/or shielding child from the stimulus.
Results
Concurrent Bivariate Correlations
Nine studies reported concurrent bivariate correlations between maternal anxiety and overprotection. However, some studies used multiple assessments of maternal anxiety and overprotection and thus reported numerous correlations (Booker et al., 2018; Kalomiris & Kiel, 2016; Kiel et al., 2019). Therefore, a total of 13 bivariate correlations are discussed.
Community Sample
Of the studies that reported concurrent bivariate correlations, the majority of studies (n = 7) used a community sample. Out of 10 bivariate correlations presented across seven studies, the majority found a small to medium size relation (rs = .14 to .41; n = 8). However, two correlations showed no meaningful relation between maternal anxiety and overprotection (Fliek et al., 2015; Kiel & Maack, 2012).
Interestingly, Kiel and Maack (2012) measured maternal anxiety via the SIAS and measured overprotection via the NFV and found no meaningful effect (r = .06), whereas Kiel et al. (2019) used the same measures and found a small effect size (r = .26). Although these studies had independent samples, both studies used data from community samples in the United States. However, Kiel and Maack (2012) had a slightly smaller sample (n = 91) compared to Kiel et al. (2019) (n = 108). Fliek et al. (2015) was the other study that found no meaningful correlation (r = .02).
For the studies using a community sample that found a meaningful relation between maternal anxiety and overprotection, the majority of effect sizes reported were small (n = 5; rs = .14 to .26; Gibler et al., 2018; Kalomiris & Kiel, 2016, Root et al., 2016; Kiel et al., 2019). Kalomiris and Kiel (2016) measured overprotection via both self-report and observation and found small effect sizes for both relations (self-reported overprotection: r = .23, observed overprotection: r = .14). However, three correlations showed a medium effect size (rs = .34 to .41; Kiel et al., 2019; Orgilés et al., 2018). Orgilés et al. (2018) had the largest sample size (n = 235) of the studies that utilized community samples and reported a concurrent bivariate correlation. They found the largest reported effect in a community sample (r = .41).
Clinical Sample
Two of the nine studies testing a concurrent bivariate correlation used a clinical sample (Booker et al., 2018; Pereira et al., 2014). Booker et al. (2018) had a clinical sample of children with anxiety disorders and their mothers from the United States. Additionally, Booker et al. (2018) reported correlations for both self- and child-report of maternal overprotection. The study found no meaningful correlation between maternal anxiety and self-reported overprotection (r = .07) but a medium correlation between maternal anxiety and child-reported overprotection (r = .31). Pereira et al. (2014) had a sample of both mothers of children with anxiety disorders and mothers of children without anxiety disorders from Portugal. The study found a medium size effect (r = .42).
Taken together, the majority of the 13 reported concurrent bivariate correlations were split between small (n = 5; Gibler et al., 2018; Kalomiris & Kiel, 2016; Kiel et al., 2019; Root et al., 2016) and medium effect sizes (n = 5; Booker et al., 2018; Kiel et al., 2019; Orgilés et al., 2018; Pereira et al., 2014). However, three correlations showed no meaningful relation (Fliek et al., 2015; Kiel & Maack, 2012; Booker et al., 2018).
Longitudinal Bivariate Correlations
Bayer et al. (2019) reported bivariate correlations between maternal anxiety and overprotection at three different time points (i.e., child age 4, 5, and 6). However, because only separate bivariate correlations were reported at each time point, we are unable to draw conclusions about maternal anxiety predicting overprotection over time. This study had a very large sample size and consisted of participants from Australia (n = 545 parents; 94% mothers). Results revealed relations with small effect sizes using spearman’s rank correlations at age four and age five (r = .20, r = .13, respectively). At age six, the relation between maternal anxiety and overprotection was no longer meaningful (r = .08). Therefore, results found the largest effect size at age four, subsequently decreasing effect sizes each year. If each correlation found in Bayer et al. (2019) is included with the other bivariate correlations reviewed in the current study, results reveal that 7 out of 16 correlations found a significant relation between maternal anxiety and overprotection at a small effect size, 5 out of 16 correlations found a significant relation between maternal anxiety and overprotection at a medium effect size, and 4 out of 16 correlations found no meaningful relation between maternal anxiety and overprotection.
Group Differences
One study tested for the difference in overprotection based on maternal anxiety disorder status (Creswell et al., 2013). Maternal anxiety group membership was based on diagnosis using the Anxiety Disorders Interview Schedule for DSM-IV (ADIS-IV), and this study consisted of participants from England. In this study, mothers diagnosed with anxiety showed significantly greater levels of overprotective behaviors in three observational tasks (i.e., speech, tangram puzzles, and black box; b = 0.12, 95% CI = [0.001, 20.95]) compared to mothers without an anxiety diagnosis.
Multivariate Relations
Six studies tested whether maternal anxiety related to overprotection over and above child factors and parent factors (Booker et al., 2018; Clarke et al., 2013; Gibler et al., 2018; Kalomiris & Kiel, 2016; Orgilés et al., 2018; Root et al., 2016), however, Kalomiris & Kiel used multiple assessments of maternal anxiety and overprotection. Thus, seven multivariate relations are discussed. Four multivariate relations found that maternal anxiety accounted for significant variance in overprotection, over and above other factors (Clarke et al., 2013; Orgilés et al., 2018; Root et al., 2016). Clarke et al. (2013) found that maternal anxiety related to overprotection over and above maternal age and maternal depression (ß = 0.27, b = 0.63, SE = 0.29, p = .03). Orgilés et al. (2018) found that maternal anxiety related to overprotection over and above child sex, child age, number of siblings, maternal age, and assertive, punitive, and inhibited parenting (ß = 0.12, SE = 0.01, 95% CI = [0.08, 0.15], p < 0.001). Kalomiris & Kiel (2016) found that maternal anxiety related to self-reported overprotection over and above primiparous status. Finally, Root et al. (2016) tested the interaction between maternal anxiety and maternal RSA and found that maternal anxiety related to overprotection at low baseline RSA (ß = .50), and mean baseline RSA (ß = 0.24) over and above child age and child gender.
However, three multivariate relations revealed that maternal anxiety did not account for significant variance in overprotection, over and above other factors (Booker et al., 2018; Gibler et al., 2018; Kalomiris & Kiel, 2016). Gibler et al. (2018) tested an Actor Partner Interdependence Model and reported relations among maternal anxiety, paternal anxiety, maternal overprotection, paternal overprotection, and child anxiety risk. In this model, the path between maternal anxiety and maternal overprotection was non-significant (b = 0.10, SE = 0.08, p >.10). However, at the bivariate level, Gibler et al. (2018) found a small correlation (DASS and CRPR, r = .15). Additionally, Booker et al. (2018) tested the relation between maternal anxiety and overprotection in a sample of mothers of children participating in a clinical trial for specific phobia. Using hierarchical regression, the authors found that maternal anxiety did not uniquely relate to self-reported overprotection, over and above months since intervention, treatment group (trends over time), and maternal grandmother’s level of overprotection (b = 0.22, SE = 0.18; d = 0.06). Additionally, maternal anxiety did not uniquely predict child-reported maternal overprotection, over and above months since intervention and child gender (b = −0.27, SE = 0.29; d = −0.07). At the bivariate level, the relation was only meaningful for child-report, in which a medium size correlation was found (child-report, r = .31; self-report, r = .07). Kalomiris and Kiel (2016) used a community sample and found that maternal anxiety did not relate to observed overprotection over and above primiparous status. At the bivariate level, a small relation was found for both observed overprotection and self-reported overprotection, but self-reported overprotection was slightly stronger in magnitude (observed, r = .14; self-reported, r = .23).
Taken together, four out of the seven statistics reporting the relation of maternal anxiety to overprotection over and above other factors found that maternal anxiety accounted for unique variance in overprotection. Interestingly, Root et al. (2016) found the strongest effect while testing the relation between maternal anxiety and overprotection in the context of low maternal RSA. Three out of the seven studies did not find a significant relation between maternal anxiety and overprotection over and above other factors.
Longitudinal Design
One study tested the relation between maternal postpartum separation anxiety at child age 3–12 months and overprotection at child age 2–3 years using structural equation modeling (Cooklin et al., 2013). This study had a very large sample size and consisted of participants from Australia (n = 3,103). Results revealed a strong relation between maternal separation anxiety at child age 3–12 months and overprotection at child age 2–3 years while accounting for maternal separation anxiety at time one, maternal psychological distress at time one, and maternal psychological distress at time two (ß = .49).
Other Factors/Possible Moderators
The current review coded for variables including location (i.e., country), age of children, and biological sex distribution of children in the sample. Because the current review is a systematic review rather than a meta-analysis, it was not possible to quantitatively analyze if the studies were significantly different based on these variables, but rather we will comment on differences qualitatively. Effect sizes and the number of significant multivariate models did not differ greatly based on location, age of children, or biological sex distribution. However, given the relatively small number of studies included and the lack of quantitative methods used to assess differences based on each study, a meta-analysis would be required to assess whether these variables may serve as moderators in the relation.
Quality Assessment
The current review also assessed for the strength of methodology and design in order to help differentiate high-quality studies from low-quality studies. The author used a self-developed scale ranging from 0 to 6 with a higher score reflecting higher risk of bias and lower methodological quality. The criteria included were modeled off of other criteria used in the literature (e.g., Korja et al., 2017; Petzoldt, 2018; Wolke et al., 2017). The following criteria were evaluated: informant of maternal anxiety (0- expert, 1- mother), measure of overprotection (0- observation, 1- self-report or other-report), study design (0- longitudinal, 1- cross-sectional), analysis (0- group difference or multivariate, 1- bivariate correlation), internal consistency of measure for maternal anxiety (0- >.70, 1- <.70), internal consistency of measure for maternal overprotection (0- >.70, 1- <.70; Taber, 2018) or interrater reliability of measure for maternal overprotection (0- >.80, 1- <.80; McHugh, 2012). If information for any criteria was missing, the maximum score of 1 was assigned. If more than one category was true for any criteria, then the minimum score of 0 was assigned.
After completing the scoring for each study, it was determined that the majority of studies scored a 4 on this scale (n = 7; Fliek et al., 2015; Gibler et al., 2018; Kiel & Maack, 2012; Kiel et al., 2019; Orgilés et al., 2018; Pereira et al., 2014; Root et al., 2016). However, two studies scored a 5 (Bayer et al., 2019; Booker et al., 2018), two studies scored a 3 (Clarke et al., 2013; Cooklin et al., 2013), one study scored a 2 (Kalomiris & Kiel., 2016), and one study scored a 1 on this scale (Creswell et al., 2013). Mean and median of the scores were then calculated (M = 3.62; Mdn = 4). In light of the conflicting results found in the current review, the studies that showed greater methodological quality and lower risk of bias were weighted more heavily. All four studies with a score of 3 or lower found a meaningful relation between maternal anxiety and overprotection. Kalomiris and Kiel (2016) found small concurrent bivariate correlations for maternal anxiety with observed overprotection and self-reported overprotection. However, when testing multivariate relations results revealed that maternal anxiety related to self-reported overprotection but not observed overprotection, over and above primiparous motherhood. Clarke et al. (2013) and Cooklin et al. (2013) found a significant relation between maternal anxiety and overprotection over and above other factors. Finally, Creswell et al. (2013) found that mothers with an anxiety diagnosis used significantly higher levels of overprotection compared to mothers without an anxiety diagnosis.
Although the literature shows conflicting results, after comparing the methodological strength of studies, a meaningful relation between maternal anxiety and overprotection is supported by results from varied samples and varied designs. This relation was shown, not only through numerous studies reporting bivariate correlations, but also through studies using more rigorous designs including longitudinal, observational, multivariate, and group differences. However, studies in this review demonstrated that this relation is small to moderate.
Discussion
The purpose of this systematic review was to synthesize the current research on the relation between maternal anxiety and overprotection and to determine if there is enough empirical evidence to support that this relation exists. Although a previous meta-analysis was conducted that tested the relation between parental anxiety and parental overcontrol (van der Bruggen et al., 2008), importantly, no studies testing overprotection, specifically, were included. Research suggests that overprotection may be especially relevant to child anxiety development compared to other forms of overcontrol (Hudson & Rapee, 2004; Rubin et al., 2009). Additionally, the influence of maternal anxiety has long been theorized to relate to overprotection, but research has shown mixed results (Bögels & van Melick, 2004; Root et al., 2016; Ginsburg et al., 2004; Moore et al., 2004). Therefore, it is important to synthesize the evidence for this relation.
The studies included in the current review contained samples with varying characteristics (e.g., different countries of origin; community versus clinical sample) and used various methodological approaches and designs (e.g., self-report, child-report, observational, longitudinal, correlational, multivariate). Findings from the current review showed mixed results. However, after comparing the relative methodological strength and risk of bias of our studies. Results revealed that the majority of studies with the highest methodological strength and lowest risk of bias found a meaningful relation between maternal anxiety and overprotection at a small to medium effect size. However, it is important to note that many of the multivariate studies included in the review did not report an effect size (e.g., Cohen’s d) and thus an effect size could not be determined. The findings from the current study are in line with theory that suggests that anxiety influences early attentional processes that relate to threat processing, which makes individuals with anxiety more likely to detect threats in the environment (Becker et al., 2001; Najmi et al., 2012; Williams et al., 1998, 1997). Applying this theory to the current review, mothers with anxiety may detect threats in their children’s environments at a higher rate, leading them to engage in overprotective behaviors. Additionally, mothers with anxiety may experience more distress when there is a potential threat in the environment and engage in overprotection as a way to decrease their own distress (Turner et al., 2003).
However, it is important to interpret these results with caution, as 4 out of 16 bivariate correlations and 3 out of 7 multivariate relations found that maternal anxiety did not account for significant variance in overprotection. Further when effects were found, they were small to medium in size. These findings suggest that although maternal anxiety likely accounts for some of the variance in overprotection, there are also likely other variables that account for substantial variance in overprotection and are worthy of future research (e.g., child fearful temperament, maternal beliefs and values around overprotection; maternal anxiety sensitivity). Additionally, these findings raise the possibility that there may be relevant contextualizing factors for the relation between maternal anxiety and overprotection that could serve to strengthen or weaken this relation. For instance, in the current review, Root et al. (2016) found a marginally significant, small effect between maternal anxiety and overprotection at the bivariate level, but found that, in the context of low baseline RSA, maternal anxiety related to overprotection at a stronger level.
Some of the variables in the literature that have been posited to account for variance in overprotection may also function as contextualizing factors in the relation between maternal anxiety and overprotection (e.g., child fearful temperament, maternal beliefs and values around overprotection; maternal anxiety sensitivity). For instance, a mother with anxiety may not be driven to engage in overprotective behaviors unless her child has a fearful temperament, which can solicit overprotection in parents (Dadds & Roth, 2001; Kagan et al., 1984). Additionally, maternal anxiety sensitivity, defined as fear of anxiety symptoms resulting from the belief that anxiety symptoms are harmful (Reiss, 1991), may lead mothers to view their children’s anxiety as harmful as well, motivating them to relieve their children’s anxiety symptoms as quickly as possible. It is possible that maternal anxiety would show a stronger relation to overprotection if mothers are also high in anxiety sensitivity, and thus motivated to end the experience of anxiety for themselves and their children. Future research should test variables such as child fearful temperament and maternal anxiety sensitivity as contextualizing factors in the relation between maternal anxiety and overprotection.
Clinical Implications
Evidence-based treatments for child anxiety often include a component of psychoeducation about the negative effects of overprotective parenting or explicit exercises to decrease this behavior (Bayer et al., 2011; Rapee et al., 2005). Based on the link most commonly found between maternal anxiety and overprotection in the current review, it is possible that treating maternal anxiety may have a positive effect on decreasing overprotective behaviors. Therefore, parenting interventions should consider taking a holistic approach to treatment by including components of personal mental health for the parents or providing resources for them to receive mental health care. Additionally, programs designed to prevent the development of child anxiety may consider targeting mothers who may be at heightened risk for overprotective parenting due to maternal characteristics such as anxiety. However, given the small to medium effect size of the relation between maternal anxiety and overprotection, treating maternal anxiety likely will not greatly decrease overprotective behaviors unless other relevant factors are also addressed. Additionally, not all mothers who are seeking treatment for their children’s anxiety will have anxiety themselves. Therefore, other factors or characteristics will be necessary to consider when working with mothers on decreasing overprotection. Future research can seek to clarify what these factors are and how they may interact with one another.
Limitations of the Literature and Future Directions
There are notable limitations in the current literature on maternal anxiety and overprotection. First, the majority of studies reported concurrent bivariate correlations. Although concurrent studies are an important first step in understanding the relation between constructs, longitudinal data and experimental data is essential in understanding the directionality and causality of the relation between maternal anxiety and overprotection. Further, in the multivariate studies included in the review, an effect size (e.g., Cohen’s d) was not reported making it difficult to interpret the size of effects. Going forward in the literature, it will be essential to test the relation between maternal anxiety and overprotection using longitudinal or experimental designs and include effect sizes.
Additionally, the current literature is limited by the lack of representation of diverse ethnicities and racial backgrounds, as the majority of participants in the included studies identified as European American/Caucasian. It is essential to increase the diversity in samples going forward in order to increase the generalizability of these results. The diversity of samples in the literature should include both diverse ethnicities and racial backgrounds and diverse locations (i.e., countries). Although the current review included studies from numerous countries (i.g., England, Australia, Spain, Portugal, Belgium, and the United States) no studies were included using samples from Asia, Africa, or South America. Although some research looks at parenting in Asia, very little research focuses on parenting in Africa and South America. Research that has examined differences in parenting between traditionally Western and Eastern cultures has found meaningful differences in parenting styles more broadly (Dwairy & Menshar, 2006; Keshavarz & Baharudin, 2013; Mousavi et al., 2016; Rudy & Grusec, 2006; Wittmer & Petersen, 2006; Xu et al., 2005), but research on the relation between maternal anxiety and overprotection across cultures is lacking. Extending this research to more cultural backgrounds including Asian, African, and South American cultures and more diverse racial and ethnic groups is imperative to understand how these relations may function differently across cultures.
Another limitation of the current literature is the reliance on self-reported parenting behaviors. Although there is evidence that self-report on parenting vignettes shows modest associations with observational assessments (McShane & Hastings, 2009), the extent to which self-reported overprotection and observed overprotection are measuring the same behavioral construct has been understudied (van der Bruggen et al., 2008). Additionally, the validity of conclusions that can be drawn from self-reported parenting remains unclear (McLeod et al., 2007). Therefore, it is essential to increase the amount of studies including observed overprotective behaviors and clarify the relation between self-reported overprotection and observed overprotection.
Limitations of the Current Review
There are also notable limitations of the current review that are necessary to consider. First, the current review only included published studies and therefore did not have access to gray literature. Many null findings may not be published in empirical studies, which suggests that the magnitude of the relation found in the current study may be weaker. Including gray literature in future research could allow for less publication bias. Second, the current review only included mothers, despite a growing body of literature to support the importance of overprotection from fathers and other caregivers. Future reviews should consider testing whether these results extend to caregivers other than mothers. Additionally, the current study was limited to studies of infancy through middle childhood and excluded all studies that tested overprotection in parents of adolescents. Although beyond the scope of the current review, this will be an important direction for future studies.
Another limitation of the current review is that results were reported through providing ranges of coefficients and effect sizes. Although this is an important initial step, if meta-analytic results were provided it would help further understand the magnitude of these relations based on various samples and demographic characteristics and is therefore an important direction for future research. A final limitation of the current review is that it is limited to understanding the link between maternal anxiety and overprotection, rather than the bi-directional influence of child characteristics such as fearful temperament or child anxiety on parenting behavior. It is important to include the bi-directional influence of child characteristics on parenting because research shows that parenting occurs in an interaction between the parent and the child and that child traits can solicit overprotection from caregivers (Dadds & Roth, 2001; Kagan et al., 1984). In order to understand the influence of maternal traits on parenting behavior, it is essential to understand how child characteristics interact with maternal traits to predict parenting behavior.
Conclusion
The current review presents a systematic investigation of the relation between maternal anxiety and overprotection. Studies in the current review showed mixed results. However, after considering the methodological strength of studies, the review supported a small to medium size relation between maternal anxiety and overprotection in community and clinical samples and across cross-sectional, multivariate, group difference, and longitudinal designs. Although a relation between these variables was found, the small to medium effect size of the relation and the studies finding non-significant relations suggest that there are other relevant factors accounting for variance in overprotection and support the need for identifying contextualizing factors in the relation. Future research would benefit from testing these factors.
Highlights.
Reviewed studies of the relation between maternal anxiety and overprotection
Thirteen studies met inclusion criteria
Evidence supported a small to medium size effect for the relation
Maternal anxiety is one factor accounting for variance in overprotection
Acknowledgements
We express our appreciation to Dr. Aaron M. Luebbe, Dr. Brooke R. Spangler-Cropenbaker, Dr. Jennifer H. Green, and Dr. Kristy L. Brann for their feedback on this manuscript.
Role of Funding
The time to work on this paper was supported by funds from Miami University and an R15 area award from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (R15 HD076158) of the National Institutes of Health, granted to Elizabeth Kiel. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declaration of Competing Interest
The authors declare that they have no conflicts of interest to report.
References
- Affrunti NW, & Ginsburg GS (2012). Maternal overcontrol and child anxiety: The mediating role of perceived competence. Child Psychiatry & Human Development, 43(1), 102–112. 10.1007/s10578-011-0248-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Affrunti NW, & Ginsburg GS (2012). Exploring parental predictors of child anxiety: The mediating role of child interpretation bias. Child & youth care forum, 41(6), 517–527. 10.1007/s10566-012-9186-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baumrind D (1967). Child care practices anteceding three patterns of preschool behavior. Genetic Psychology Monographs, 75(1), 43–88. [PubMed] [Google Scholar]
- Bayer JK, Morgan A, Prendergast LA, Beatson R, Gilbertson T, Bretherton L, … & Rapee RM (2019). Predicting temperamentally inhibited young children’s clinical-level anxiety and internalizing problems from parenting and parent wellbeing: a population study. Journal of Abnormal Child Psychology, 47(7), 1165–1181. 10.1007/s10802-018-0442-6 [DOI] [PubMed] [Google Scholar]
- Bayer JK, Sanson AV, & Hemphill SA (2006). Parent influences on early childhood internalizing difficulties. Journal of Applied Developmental Psychology, 27, 542–559. 10.1016/j.appdev.2006.08.002 [DOI] [Google Scholar]
- Bayer JK, Hastings PD, Sanson AV, Ukoumunne OC, & Rubin KH (2010). Predicting mid-childhood internalizing symptoms: A longitudinal community study. International Journal of Mental Health Promotion, 12, 5–17. 10.1080/14623730.2010.9721802 [DOI] [Google Scholar]
- Bayer JK, Rapee RM, Hiscock H, Ukoumunne OC, Mihalopoulos C, & Wake M (2011). Translational research to prevent internalizing problems early in childhood. Depression and Anxiety, 28(1), 50–57. 10.1002/da.20743 [DOI] [PubMed] [Google Scholar]
- Becker ES, Rinck M, Margraf J, & Roth WT (2001). The emotional Stroop effect in anxiety disorders: General emotionality or disorder specificity? Journal of Anxiety Disorders, 15(3), 147–159. 10.1016/s0887-6185(01)00055-x [DOI] [PubMed] [Google Scholar]
- Block JH (1965). The child-rearing practices report. Berkley: Institute of Human Development, University of California. [Google Scholar]
- Bögels S, & Phares V (2008). Fathers’ role in the etiology, prevention and treatment of child anxiety: A review and new model. Clinical Psychology Review, 28(4), 539–558. 10.1016/j.cpr.2007.07.011 [DOI] [PubMed] [Google Scholar]
- Bögels SM, & van Melick M (2004). The relationship between child-report, parent self-report, and partner report of perceived parental rearing behaviors and anxiety in children and parents. Personality and Individual Differences, 37(8), 1583–1596. 10.1016/j.paid.2004.02.014 [DOI] [Google Scholar]
- Booker JA, Capriola-Hall NN, & Ollendick TH (2018). Parental influences and child internalizing outcomes across multiple generations. Journal of Child and Family Studies, 27(7), 2217–2231. 10.1007/s10826-018-1067-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown BB (2004). Adolescents’ relationships with peers. In Lerner RM & Steinberg L (Eds.), Handbook of adolescent psychology (p. 363–394). John Wiley & Sons Inc. 10.1002/9780471726746.ch12 [DOI] [Google Scholar]
- Buss KA (2011). Which fearful toddlers should we worry about? Context, fear regulation, and anxiety risk. Developmental Psychology, 47, 804–819. 10.1037/a0023227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castro J, de Pablo J, Gómez J, Arrindell WA, & Toro J (1997). Assessing rearing behaviour from the perspective of the parents: a new form of the EMBU. Social Psychiatry and Psychiatric Epidemiology, 32(4), 230–235. 10.1007/BF00788243 [DOI] [PubMed] [Google Scholar]
- Castro J, Toro J, Van der Ende J, & Arrindell WA (1993). Exploring the feasibility of assessing perceived parental rearing styles in Spanish children with The EMBU. International Journal of Social Psychiatry, 39(1), 47–57. 10.1177/002076409303900105 [DOI] [PubMed] [Google Scholar]
- Cheek JM (1983). The revised cheek and buss shyness scale (RCBS). Unpublished manuscript. Wellesley College, Wellesley MA. [Google Scholar]
- Cheek J, & Buss A (1981). Shyness and sociability. Journal of Personality and Social Psychology, 41, 330–339. 10.1037/0022-3514.41.2.330 [DOI] [Google Scholar]
- Chen X, Hastings P, Rubin KH, Chen H, Cen G, & Stewart SL (1998). Child-rearing attitudes and behavioral inhibition in Chinese and Canadian toddlers: A cross-cultural study. Developmental Psychology, 34, 677–686. 10.1037/0012-1649.34.4.677 [DOI] [PubMed] [Google Scholar]
- Chorpita BF, & Barlow DH (1998). The development of anxiety: The role of control in the early environment. Psychological Bulletin, 124(1), 3–21. 10.1037/0033-2909.124.1.3 [DOI] [PubMed] [Google Scholar]
- Clarke K, Cooper P, & Creswell C (2013). The Parental Overprotection Scale: Associations with child and parental anxiety. Journal of Affective Disorders, 151(2), 618–624. 10.1016/j.jad.2013.07.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooklin AR, Giallo R, D’Esposito F, Crawford S, & Nicholson JM (2013). Postpartum maternal separation anxiety, overprotective parenting, and children’s social-emotional well-being: Longitudinal evidence from an Australian cohort. Journal of Family Psychology, 27(4), 618. 10.1037/a0033332 [DOI] [PubMed] [Google Scholar]
- Costa NM, & Weems CF (2005). Maternal and child anxiety: Do attachment beliefs or children’s perceptions of maternal control mediate their association? Social Development, 14(4), 574–590. 10.1111/j.1467-9507.2005.00318.x [DOI] [Google Scholar]
- Costello EJ, Egger HL, & Angold A (2005). The developmental epidemiology of anxiety disorders: Phenomenology, prevalence, and comorbidity. Child and Adolescent Psychiatric Clinics of North America, 14, 631–648. 10.1016/j.chc.2005.06.003 [DOI] [PubMed] [Google Scholar]
- Creswell C, Apetroaia A, Murray L, & Cooper P (2013). Cognitive, affective, and behavioral characteristics of mothers with anxiety disorders in the context of child anxiety disorder. Journal of Abnormal Psychology, 122(1), 26. 10.1037/a0029516 [DOI] [PubMed] [Google Scholar]
- Creveling CC, Varela RE, Weems CF, & Corey DM (2010). Maternal control, cognitive style, and childhood anxiety: A test of a theoretical model in a multi-ethnic sample. Journal of Family Psychology, 24(4), 439–448. 10.1037/a0020388 [DOI] [PubMed] [Google Scholar]
- Dadds MR, & Roth JH (2001). Family processes in the development of anxiety problems. In Vasey MW & Dadds MR (Eds.), The developmental psychopathology of anxiety (pp. 278–303). New York: Oxford University Press, Inc. 10.1093/med:psych/9780195123630.003.0013 [DOI] [Google Scholar]
- Derogatis LR (1975). Brief symptom inventory. Baltimore: Clinical Psychometric Research. [Google Scholar]
- Drake KL, & Ginsburg GS (2011). Parenting practices of anxious and nonanxious mothers: A multimethod, multi-informant approach. Child & family behavior therapy, 33(4), 299–321. 10.1080/07317107.2011.623101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dwairy M, & Menshar KE (2006). Parenting style, individuation, and mental health of Egyptian adolescents. Journal of Adolescence, 29(1), 103–117. 10.1016/j.adolescence.2005.03.002 [DOI] [PubMed] [Google Scholar]
- Edwards Rapee, & Kennedy, (2008). Psychometric properties of a parent-report measure of overprotection in preschool-aged children. Unpublished manuscript.
- Eysenck MW (1992). Anxiety: The cognitive perspective. Hove, UK: Erlbaum [Google Scholar]
- Farley JU, Lehmann DR, & Sawyer A (1995). Empirical marketing generalization using meta-analysis. Marketing Science, 14, G36–G46. 10.1287/mksc.14.3.G36 [DOI] [Google Scholar]
- Fliek L, Daemen E, Roelofs J, & Muris P (2015). Rough-and-tumble play and other parental factors as correlates of anxiety symptoms in preschool children. Journal of Child and Family Studies, 24(9), 2795–2804. 10.1007/s10826-014-0083-5 [DOI] [Google Scholar]
- Fonseca-Pedrero E, Paino M, Sierra-Baigrie S, Lemos-Giráldez S, & Muñiz J (2012). Propiedades psicométricas del Cuestionario de ansiedad estado-rasgo (STAI) en universitarios. Behavioral Psychology-Psicología Conductual, 20(3), 547–561. [Google Scholar]
- Ghandour RM, Sherman LJ, Vladutiu CJ, Ali MM, Lynch SE, Bitsko RH, & Blumberg SJ (2019). Prevalence and treatment of depression, anxiety, and conduct problems in US children. The Journal of Pediatrics, 206, 256–267. 10.1016/j.jpeds.2018.09.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibler RC, Kalomiris AE, & Kiel EJ (2018). Paternal anxiety in relation to toddler anxiety: The mediating role of maternal behavior. Child Psychiatry and Human Development, 49(4), 512–522. 10.1007/s10578-017-0771-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ginsburg GS, Grover RL, & Ialongo N (2004). Parenting behaviors among anxious and non-anxious mothers: Relation with concurrent and long-term child outcomes. Child & Family Behavior Therapy, 26(4), 23–41. 10.1300/J019v26n04_02 [DOI] [Google Scholar]
- Hock E, DeMeis D, & McBride S (1988). Maternal separation anxiety: Its role in the balance of employment and motherhood in mothers of infants. In Gottfried AE & Gottfried AW (Eds.), Maternal employment and children’s development: Longitudinal research (pp. 191–229). New York, NY: Plenum Press. 10.1007/978-1-4899-0830-8_7 [DOI] [Google Scholar]
- Hock E, McBride S, & Gnezda M (1989). Maternal separation anxiety: Mother-infant separation from the maternal perspective. Child Development, 60, 793–802. 10.2307/1131019 [DOI] [Google Scholar]
- Holmbeck GN, Johnson SZ, Wills KE, McKernon W, Rose B, Erklin S, & Kemper T (2002). Observed and perceived parental overprotection in relation to psychosocial adjustment in preadolescents with a physical disability: The mediational role of behavioral autonomy. Journal of Consulting and Clinical Psychology, 70(1), 96–110. 10.1037//0022-006x.70.1.96 [DOI] [PubMed] [Google Scholar]
- Hudson JL, & Rapee RM (2004). From anxious temperament to disorder: An etiological model. In Heimberg RG, Turk CL, & Mennin DS (Eds.), Generalized anxiety disorder: Advances in research and practice (pp. 51–74). New York, NY, US: Guilford Press. [Google Scholar]
- Hunter JE, & Schmidt FL (1990). Methods of meta-analysis: Correcting error and bias in research findings. Newbury Park, CA: Sage. [Google Scholar]
- Kagan J, Reznick JS, Clarke C, Snidman N, & Garcia-Coll C (1984). Behavioral inhibition to the unfamiliar. Child Development, 55(6), 2212–2225. 10.2307/1129793 [DOI] [Google Scholar]
- Kalomiris AE, & Kiel EJ (2016). Maternal anxiety and physiological reactivity as mechanisms to explain overprotective primiparous parenting behaviors. Journal of Family Psychology, 30(7), 791–801. 10.1037/fam0000237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keshavarz S, & Baharudin R (2013). Perceived parenting style of fathers and adolescents’ locus of control in a collectivist culture of Malaysia: The moderating role of fathers’ education. The Journal of Genetic Psychology, 174(3), 253–270. 10.1080/00221325.2012.678419 [DOI] [PubMed] [Google Scholar]
- Kiel EJ, & Maack DJ (2012). Maternal BIS sensitivity, overprotective parenting, and children’s internalizing behaviors. Personality and Individual Differences, 53(3), 257–262. 10.1016/j.paid.2012.03.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiel EJ, Wagers KB, & Luebbe AM (2019). The Attitudes About Parenting Strategies for Anxiety Scale: A Measure of parenting attitudes about protective and intrusive behavior. Assessment, 26(8), 1504–1523. 10.1177/1073191117719513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korja R, Nolvi S, Grant KA, & McMahon C (2017). The relations between maternal prenatal anxiety or stress and child’s early negative reactivity or self-regulation: a systematic review. Child Psychiatry & Human Development, 48(6), 851–869. 10.1007/s10578-017-0709-0. [DOI] [PubMed] [Google Scholar]
- Leary MR, & Kowalski RM (1993). The interaction anxiousness scale: Construct and criterion-related validity. Journal of Personality Assessment, 61(1), 136–146. 10.1207/s15327752jpa6101_10 [DOI] [PubMed] [Google Scholar]
- Lindhout I, Markus M, Hoogendijk T, Borst S, Maingay R, Spinhoven P, … Boer F (2006). Childrearing style of anxiety-disordered parents. Child Psychiatry and Human Development, 37(1), 89–102. 10.1007/s10578-006-0022-9 [DOI] [PubMed] [Google Scholar]
- Lovibond PF, & Lovibond SH (1995). The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behaviour Research and Therapy, 33(3), 335–343. 10.1016/0005-7967(94)00075-u [DOI] [PubMed] [Google Scholar]
- Magaz A, & García EM (1998). PEE, perfil de estilos educativos: Manual de referencia [Profile of Parenting Styles: Reference manual]. Vizcaya, Spain: Albor-COHS group. [Google Scholar]
- Manassis K, & Bradley SJ (1994). The development of childhood anxiety disorders: Toward an integrated model. Journal of Applied Developmental Psychology, 15(3), 345–366. 10.1016/0193-3973(94)90037-X [DOI] [Google Scholar]
- Mattick RP, & Clarke JC (1998). Development and validation of measures of social phobia scrutiny fear and social interaction anxiety. Behaviour Research and Therapy, 36(4), 455–470. 10.1016/S0005-7967(97)10031-6 [DOI] [PubMed] [Google Scholar]
- McHugh ML (2012). Interrater reliability: the kappa statistic. Biochemia medica: Biochemia medica, 22(3), 276–282. 10.11613/BM.2012.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLeod BD, Wood JJ, & Weisz JR (2007). Examining the association between parenting and childhood anxiety: A meta-analysis. Clinical Psychology Review, 27, 155–172. 10.1016/j.cpr.2006.09.002 [DOI] [PubMed] [Google Scholar]
- McShane KE, & Hastings PD (2009). The New Friends Vignettes: Measuring parental psychological control that confers risk for anxious adjustment in preschoolers. International Journal of Behavioral Development, 33(6), 481–495. 10.1177/0165025409103874 [DOI] [Google Scholar]
- Meyer TJ, Miller ML, Metzger RL, & Borkovec TD (1990). Development and validation of the Penn State Worry Questionnaire. Behaviour Research and Therapy, 28(6), 487–495. 10.1016/0005-7967(90)90135-6 [DOI] [PubMed] [Google Scholar]
- Moore PS, Whaley SE, & Sigman M (2004). Interactions between mothers and children: Impacts of maternal and child anxiety. Journal of Abnormal Psychology, 113(3), 471–476. 10.1037/0021-843X.113.3.471 [DOI] [PubMed] [Google Scholar]
- Mousavi SE, Low WY, & Hashim AH (2016). Perceived parenting styles and cultural influences in adolescent’s anxiety: A cross-cultural comparison. Journal of Child and Family Studies, 25(7), 2102–2110. 10.1007/s10826-016-0393-x [DOI] [Google Scholar]
- Murray L, Lau PY, Arteche A, Creswell C, Russ S, Della Zoppa L, … Cooper P (2012). Parenting by anxious mothers: Effects of disorder subtype, context, and child characteristics. Journal of Child Psychology and Psychiatry, 53, 188–196. 10.1111/j.1469-7610.2011.02473.x [DOI] [PubMed] [Google Scholar]
- Najmi S, Kuckertz JM, & Amir N (2012). Attentional impairment in anxiety: inefficiency in expanding the scope of attention. Depression and Anxiety, 29(3), 243–249. 10.1002/da.20900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nishikawa S, Sundbom E, & Hägglöf B (2010). Influence of perceived parental rearing on adolescent self-concept and internalizing and externalizing problems in Japan. Journal of Child and Family Studies, 19(1), 57–66. 10.1007/s10826-009-9281-y [DOI] [Google Scholar]
- Orgilés M, Penosa P, Morales A, Fernández-Martínez I, & Espada JP (2018). Maternal anxiety and separation anxiety in children aged between 3 and 6 years: The mediating role of parenting style. Journal of Developmental & Behavioral Pediatrics, 39(8), 621–628. 10.1097/DBP.0000000000000593 [DOI] [PubMed] [Google Scholar]
- Parker G (1979). Reported parental characteristics in relation to trait depression and anxiety levels in a non-clinical group. Australian and New Zealand Journal of Psychiatry, 13(3), 260–264. 10.3109/00048677909159146 [DOI] [PubMed] [Google Scholar]
- Pereira AIF, Barros L, & Beato A (2013). Escala de avaliação da ansiedade e superprotecção parentais: estudo psicométrico numa amostra de pais e mães de crianças em idade escolar [Parental anxiety and overprotection scale: A psychometric study with a sample of parents of school age-children]. Revista Ibero-Americana de Diagnóstico Y Evaluación, 35, 35–55. [Google Scholar]
- Pereira AI, Barros L, Mendonça D, & Muris P (2014). The relationships among parental anxiety, parenting, and children’s anxiety: The mediating effects of children’s cognitive vulnerabilities. Journal of Child and Family Studies, 23(2), 399–409. 10.1007/s10826-013-9767-5 [DOI] [Google Scholar]
- Peterson RA, & Brown SP (2005). On the use of beta coefficients in meta-analysis. Journal of Applied Psychology, 90(1), 175–181. 10.1037/0021-9010.90.1.175 [DOI] [PubMed] [Google Scholar]
- Petzoldt J (2018). Systematic review on maternal depression versus anxiety in relation to excessive infant crying: it is all about the timing. Archives of Women’s Mental Health, 21(1), 15–30. 10.1007/s00737-017-0771-4 [DOI] [PubMed] [Google Scholar]
- Rapee RM (1997). Potential role of childrearing practices in the development of anxiety and depression. Clinical Psychology Review, 17(1), 47–67. 10.1016/S0272-7358(96)00040-2 [DOI] [PubMed] [Google Scholar]
- Rapee RM, Kennedy SJ, Ingram M, Edwards SL, & Sweeney L (2005). Prevention and early intervention of anxiety disorders in inhibited preschool children. Journal of Consulting and Clinical Psychology, 73(3), 488–497. 10.1037/0022-006X.73.3.488 [DOI] [PubMed] [Google Scholar]
- Reiss S (1991). Expectancy model of fear, anxiety, and panic. Clinical Psychology Review, 11(2), 141–153. 10.1016/0272-7358(91)90092-9 [DOI] [Google Scholar]
- Reitman D, & Asseff J (2010). Parenting practices and their relation to anxiety in young adulthood. Journal of Anxiety Disorders, 24, 565–572. 10.1016/j.janxdis.2010.03.016 [DOI] [PubMed] [Google Scholar]
- Rickel AU, & Biasatti LL (1982). Modification of the block child rearing practices report. Journal of Clinical Psychology, 38(1), 129–134. [DOI] [Google Scholar]
- Root AE, Hastings PD, & Rubin KH (2016). The parenting behaviors of shy–anxious mothers: The moderating role of vagal tone. Journal of Child and Family Studies, 25(4), 1325–1333. 10.1007/s10826-015-0296-2 [DOI] [Google Scholar]
- Rosenthal R, & DiMatteo MR (2001). Meta-analysis: Recent developments in quantitative methods for literature reviews. In Fiske ST, Schacter D, & Zahn-Waxler C (Eds.), Annual Review of Psychology (Vol. 52, pp. 59–82). Palo Alto, CA: Annual Reviews. 10.1146/annurev.psych.52.1.59 [DOI] [PubMed] [Google Scholar]
- Rubin KH, Coplan RJ, & Bowker JC (2009). Social withdrawal in childhood. Annual Review of Psychology, 60, 141–171. 10.1146/annurev.psych.60.110707.163642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin KH, Hastings PD, Stewart SL, Henderson HA, & Chen X (1997). The consistency and concomitants of inhibition: Some of the children, all of the time. Child Development, 68(3), 467–483. 10.2307/1131672 [DOI] [PubMed] [Google Scholar]
- Rudy D, & Grusec JE (2006). Authoritarian parenting in individualist and collectivist groups: Associations with maternal emotion and cognition and children’s self-esteem. Journal of Family Psychology, 20(1), 68. 10.1037/0893-3200.20.1.68 [DOI] [PubMed] [Google Scholar]
- Silk JS, Morris AS, Kanaya T, & Steinberg L (2003). Psychological control and autonomy granting: Opposite ends of a continuum or distinct constructs?. Journal of research on adolescence, 13(1), 113–128. 10.1111/1532-7795.1301004 [DOI] [Google Scholar]
- Spielberger CD, Gorsuch R, & Lushene R (1970). Manual for the State-Trait Anxiety Inventory. Palo Alto, California: Consulting Psychologist Press. [Google Scholar]
- Taber KS (2018). The use of Cronbach’s alpha when developing and reporting research instruments in science education. Research in Science Education, 48(6), 1273–1296. 10.1007/s11165-016-9602-2 [DOI] [Google Scholar]
- Turner SM, Beidel DC, Roberson-Nay R, & Tervo K (2003). Parenting behaviors in parents with anxiety disorders. Behaviour Research and Therapy, 41(5), 541–554. 10.1016/s0005-7967(02)00028-1 [DOI] [PubMed] [Google Scholar]
- van der Bruggen CO, Stams GJJM, & Bögels SM (2008). Research review: The relation between child and parent anxiety and parental control: A meta-analytic review. Journal of Child Psychology and Psychiatry, 49(12), 1257–1269. 10.1111/j.1469-7610.2008.01898.x [DOI] [PubMed] [Google Scholar]
- Van der Ploeg HM, Defares PB, & Spielberger CD (1980). Handleiding bij de zelfbeoordelingsvragenlijst, ZBV: een Nederlandse vertaling van de Spielberger State-Trait Anxiety Inventory. Lisse: Swets & Zeitlinger. [Google Scholar]
- Williams JMG, Watts FN, MacLeod C, & Mathews A (1988). Cognitive psychology and emotional disorders. Chichester, UK: Wiley. [Google Scholar]
- Williams JMG, Watts FN, MacLeod C, & Mathews A (1997). Cognitive psychology and emotional disorders. (2nd ed.). Chichester, UK: Wiley. [Google Scholar]
- Wittmer DS, & Petersen SH (2006). Infant and toddler development and responsive program planning: A relationship-based approach: Recording for the Blind & Dyslexic. [Google Scholar]
- Wolke D, Bilgin A, & Samara M (2017). Systematic review and meta-analysis: fussing and crying durations and prevalence of colic in infants. The Journal of Pediatrics, 185, 55–61. 10.1016/j.jpeds.2017.02.020 [DOI] [PubMed] [Google Scholar]
- Wood JJ (2006). Parental intrusiveness and children’s separation anxiety in a clinical sample. Child Psychiatry and Human Development, 37(1), 73–87. 10.1007/s10578-006-0021-x [DOI] [PubMed] [Google Scholar]
- Xu Y, Ann J, Farver M, Zhang Z, Zeng Q, Yu L, & Cai B (2005). Mainland Chinese parenting styles and parent–child interaction. International Journal of Behavioral Development, 29, 524–533. 10.1177/01650250500147121 [DOI] [Google Scholar]


