Abstract
Reverse transcriptase polymerase chain reaction (RT-PCR) is a key tool to diagnose Covid-19. Yet it may not be the most efficient test in all patients. In this paper, we develop a clinical strategy for prescribing RT-PCR to patients based on data from COVIDOM, a French cohort of 54,000 patients with clinically suspected Covid-19, including 12,810 patients tested by RT-PCR. We use a machine-learning algorithm (decision tree) in order to predict RT-PCR results based on the clinical presentation. We show that symptoms alone are sufficient to predict RT-PCR outcome with a mean average precision of 86%. We identify combinations of symptoms that are predictive of RT-PCR positivity (90% for anosmia/ageusia) or negativity (only 30% of RT-PCR+ for a subgroup with cardiopulmonary symptoms): in both cases, RT-PCR provides little added diagnostic value. We propose a prescribing strategy based on clinical presentation that can improve the global efficiency of RT-PCR testing.
Subject terms: Diseases, Infectious diseases, DNA
Introduction
The coronavirus disease (Covid-19) epidemic started in China in December 2019 and has spread worldwide, infecting more than 160 million people by May 20211. Making the diagnosis of Covid-19 infection can be difficult, since the clinical presentation is versatile, including associations of fever, myalgia, fatigue, cough, shortness of breath, gastrointestinal signs, headaches, upper respiratory tract symptoms…2. Several tests have proved helpful to diagnose Covid-19 infection3–5. The current reference test is reverse transcriptase polymerase chain reaction (RT-PCR), which attests the presence of viral RNA in the sample, usually nasopharyngeal swabs6.
There is a strong need for a practical strategy to approach diagnostic investigations. RT-PCR is costly and remains difficult to use in practice with a significant time from sampling to results7. Moreover, RT-PCR is highly specific of the presence of viral nucleic acid in the sample, yet it lacks sensitivity: a negative test does not negate the possibility that an individual is infected4. This creates a diagnostic doubt, and first-line alternative investigations, such as chest imaging, may sometimes be more relevant.
Basing our analyses on a large ambulatory cohort of 54,000 patients followed by a unique telemonitoring platform in the greater Paris region in France during the first wave of the epidemics, we analyzed the RT-PCR usefulness as a diagnostic tool in different clinical presentations. The aim was to develop and assess a strategy for RT-PCR testing in patients with suspected Covid-19.
Methods
We first described the access to RT-PCR testing, based on patients’ characteristics and symptoms. We studied whether RT-PCR-positive (RT-PCR+) and RT-PCR-negative (RT-PCR−) patients have different clinical profiles. We then performed a multivariate predictive study: we identified combinations of symptoms that are predictive of either a high or a low chance of RT-PCR positivity with weighing on the propensity score for RT-PCR testing. Based on these identified combinations, we proposed a triage strategy to target RT-PCR testing in patients for whom RT-PCR results will bring the highest additional information for Covid-19 diagnosis.
Population—COVIDOM telemonitoring program
In France, a telemonitoring web-application called COVIDOM has been developed for home management of suspected or confirmed Covid-19 patients. In this application, self-administered daily questionnaires can trigger alerts that are handled in a regional medicalized control center. It was launched in the Greater Paris area on March 9th, 2020, and aims at efficiently detecting patients at risk of deterioration while relieving the burden for healthcare professionals. Patients are included in COVIDOM after seeking medical care in an outpatient setting (emergency services or general practitioners) or after being discharged from hospital. We included in our analysis all patients followed until May 6th, 2020. We excluded all patients under 18.
During registration, patients provided an electronic consent for the COVIDOM telemonitoring program and they were informed of the potential use of anonymized data for research purposes. This use was approved by the Scientific and ethical committee of APHP (IRB00011591).
Data
Patients in COVIDOM filled out questionnaires, specifying characteristics (age, sex, weight, height), comorbidities (diabetes, hypertension, chronic obstructive pulmonary disease, asthma, heart failure, coronary heart disease, cancer under treatment, chronic kidney disease, other chronic disease), smoking status, symptoms since the beginning of the suspected Covid-19 disease (fatigue, myalgia, breathlessness, ageusia, anosmia, anorexia, chest pain, chest oppression, cough, fever, diarrhea, vomiting, shivers, rash, frostbites, conjunctivitis, other symptoms), hospitalisation history, investigations that were performed (RT-PCR, chest CT-scan, chest X-ray), and RT-PCR results. The questionnaire is available in Fig. S1. For each patient, we collected the information in a single copy. These patient-reported data are completed with RT-PCR results from the French Assistance Publique-Hôpitaux de Paris (AP-HP) data warehouse, also known as Entrepôt de Données de Santé (EDS). AP-HP is the network of all university hospitals in the greater Paris region. RT-PCR were performed according to international guidelines on respiratory samples, mainly nasopharyngeal swabs6.
Analyses
Access to RT-PCR testing
In a retrospective analysis, we seek to identify patients who had RT-PCR testing (Fig. 1), and to report associations of patient characteristics with RT-PCR results (Fig. 2). For this, we consider the following covariates: sex; age (quantized in 5 groups); tobacco consumption (current smoker or not); comorbidities: respiratory, cardio-vascular, diabetes or obesity; presence of symptoms: breathlessness, anorexia, tiredness, digestive signs (diarrhea or vomiting), conjunctivitis, cutaneous symptoms (rash or frostbites), shivers, myalgia, cough, fever, cardiopulmonary symptoms (breathlessness associated to chest pain or chest oppression) or chemosensory impairment (anosmia or ageusia); ambulatory status (has the patient been hospitalized or not).
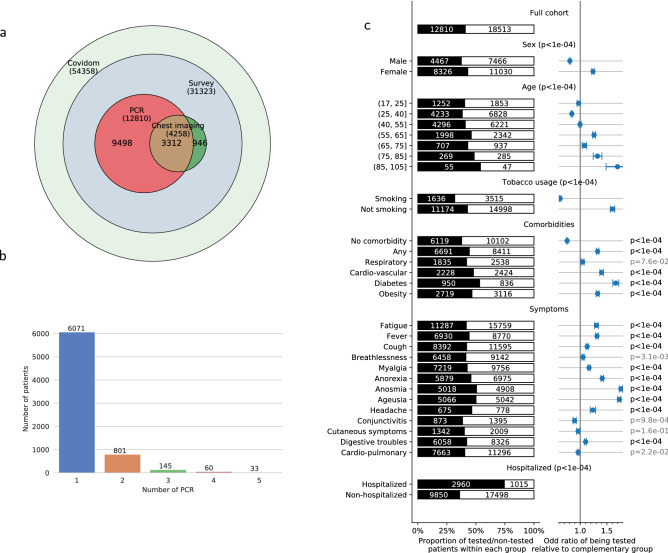
Figure 1.
Differentiated access to RT-PCR testing in patients who answered the COVIDOM survey (N = 31,323). (a) Description of the investigations in the COVIDOM cohort combining the survey and the EDS database: 54,358 patients are included in the web-application for daily monitoring, among which 31,323 answered the complete survey. (b) Description of repeated RT-PCR testing for patients included in the Corona OMOP database (N = 6621). Patients benefited from 1 to 10 RT-PCR tests each. Median time between RT-PCR1 and RT-PCR2 was 8 days, RT-PCR1 and RT-PCR3: 13 days, RT-PCR1 and RT-PCR4: 15 days, RT-PCR1 and RT-PCR5: 21 days. (c) Access to RT-PCR testing in patients who answered the COVIDOM survey, as a function of various patient characteristics. The size of the black bar indicates the proportion that has been tested of a given group.. The population is stratified based on demographic characteristics, tobacco usage, comorbidities (“any” includes any of the following or hypertension, chronic kidney disease, cancer under treatment or other as indicated by the patient, “respiratory” indicates asthma or COPD, “cardio-vascular” indicates heart failure or coronary disease, obesity a BMI above 30), symptoms experienced at some point of the disease (“cardiopulmonary” indicates breathlessness associated to chest oppression or chest pain), need for admission in hospital before or after inclusion in COVIDOM. The right column indicates the odd-ratios of being tested in each group, compared to the complementary group. We test whether these odds ratios significantly differ from 1 using a Wald test. Table S1 provides all numerical data.
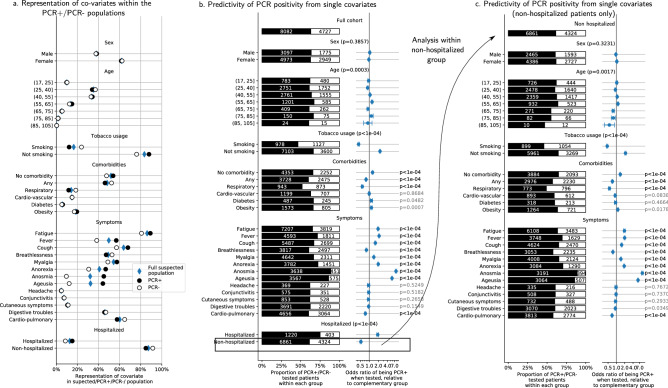
Figure 2.
Effects of patient characteristics on RT-PCR results. We apply a propensity-scoring weight to each patient, to remove the testing-propensity confound. We report weighted counts/proportions/odds-ratios. (a) Representation of each characteristic in the whole cohort (blue diamonds), the RT-PCR+ cohort (black dot) and the RT-PCR− cohort (white dot). (b) RT-PCR results as a function of different characteristics in the tested population (cf Fig. 1c for categories). Odds ratios of being RT-PCR+ when belonging to a given subgroup, and p-values that these ratios are significantly different from 1 (using a Wald test). Patients without comorbidities nor smoking are more likely to be RT-PCR+, so do patients with anosmia, ageusia, anorexia, fever, fatigue, cough, myalgia. On the opposite, comorbidities, in particular respiratory diseases, and symptoms such as breathlessness and cardiopulmonary symptoms are associated with RT-PCR. (c) Same analysis as (b), within the subpopulation that has not been hospitalized. Results are similar. Table S1 provides all numerical data.
Within the population of patients who answered the questionnaire, we evaluate the associations between patient characteristics and RT-PCR testing: for this, we estimate odds ratio for each variable using univariate logistic regression models. We test whether the odds ratio significantly differs from 1 using a Wald test.
Associations of patient characteristics with RT-PCR results
Within the tested population, we evaluate the association of each covariate with RT-PCR results. To account for the lack of homogeneity in testing and correct for a possible indication bias, we use a propensity score for weighting each patient: for this, we estimate the probability of being tested using a multivariate logistic model (with all covariates introduced above). We then assign a weight to each patient that is inversely proportional to this probability. By counting weighted patients, we construct a pseudo-. Weighting results in a pseudo-population of size twice the number of tested patients, where covariates proportion are similar within the whole cohort and the tested population, thus correcting a possible indication bias..
We then estimate one univariate logistic regression model per covariate to predict RT-PCR positivity, and report associated pseudo-counts (i.e. counts of patients, weighted by using the propensity score) and odds ratios. Complementarily, we compare the weighted proportion of a given covariate within the (propensity score weighted) RT-PCR+ and RT-PCR− populations (Fig. 1c).
Predicting RT-PCR results from patient symptoms
To prioritize patients due for a RT-PCR test, we seek combinations of symptoms that are predictive of the RT-PCR result. For this, we estimate a multivariate decision tree8 that, for each patient, predicts the result of the RT-PCR test based on his/her symptoms. A decision tree recursively splits the population based on the presence or not of a given symptom, so as to progressively separate RT-PCR+ and RT-PCR− into different groups. It thus automatically provides predictive combinations of symptoms, whose importance is then verified on a set of patients not used for estimation. As in the univariate analysis, we use propensity score weighing during estimation and evaluation.
We train a decision tree on 80% of the tested patients and evaluate its performance on the 20% held-out group. We repeat the training procedure across multiple separations of training and held-out data to evaluate the variance of the predictive model performance. Details on decision-tree parameters, architecture choices and weighing procedure are reported in the supplementary material. We report precision-recall curves, average precision of the model, and a description of the splits performed by the trained decision tree. We evaluate the importance of each symptom in predicting the RT-PCR outcome by measuring how hiding this observed variable from the decision tree affects its performance9.
Finally, in each group defined by the decision tree, we report the odds ratio of being RT-PCR+, and report RT-PCR+ proportion. Odds and proportions are weighted by propensity scores. We simplify the decision tree to propose actionable rules to prioritize RT-PCR access.
We use the Python packages scikit-learn and stats models to perform statistical analyses9,10. The code for reproduction and reuse is available at the address http://github.com/arthurmensch/covidom_analysis.
Ethical approval
This study received the ethical approval of the ethical committee of AP-HP (IRB00011591).
Results
Cohort description
From inception to May 6th, 2020, 54,358 patients were registered in COVIDOM by a physician for daily monitoring, 31,323 answered the questionnaire (flow-chart of Fig. 1a). 3774 patients (12%) were included after hospitalization. There was a median of 16 days (IQ9-23) after the first symptoms and 10 days (IQ2-16) after the inclusion in COVIDOM when the patients filled up the forms (Fig. S2).
The mean age of the patients is 43.6 ± 14.3 with 28,779 (92%) under 65 year-old. As detailed in Fig. 2 and Table S1, the most frequent symptoms in the whole cohort were fatigue (86%), cough (64%), myalgia (54%), fever (50%), breathlessness (50%), and digestive symptoms (46%). Breathlessness associated with chest oppression or pain was mentioned by 61%. Anosmia and ageusia are present in respectively 32% and 32% of patients, with 26% presenting both symptoms. Anosmia or ageusia is more frequent in women (28% of women present both symptoms versus 22% of men, p < 0.0001), and the mean age of patients with chemosensory impairment is 42.2 ± 13.2 years, younger than the rest of the cohort (p < 0.0001).
In total, 12,810 patients (41%) were tested by RT-PCR, after we excluded 75 patients with undetermined results (0.6%). Chest imaging was performed in 5010 patients (16%). In patients who had RT-PCR, the mean number of RT-PCR was 1.2 ± 0.6 and the median time between RT-PCR1 and RT-PCR2 was 7 days (IQ2-19) (Figs. 1b and S3).
Differentiated access to RT-PCR testing in the COVIDOM cohort
Studying RT-PCR access in the COVIDOM cohort shows that the test is not systematically performed for all symptomatic patients, as detailed in Figs. 1c and S5. Patients more prone to be tested are women (43% vs 37% for men, p < 0.0001), elderly patients (p < 0.0001), and non-smokers (43% vs 32% for smokers, p < 0.0001). Patients with comorbidities are tested more often (44% vs 37% for healthy patients, p < 0.0001), especially patients with diabetes (53%), cardio-vascular disease (48%) or obesity (47%), but not patients with respiratory comorbidities. Concerning clinical presentation, patients with anosmia or ageusia are more likely to be tested (respectively 51% and 50%). On the opposite, patients with cardiopulmonary signs, i.e. breathlessness associated with chest oppression or chest pain, are as likely to be tested as the whole cohort (40%). As expected, patients who were hospitalized before or after their inclusion in COVIDOM were tested more often than outpatients (3134, 80% for hospitalized patients, vs 10,724, 40% for outpatients).
Associations of patient characteristics with RT-PCR results
The remaining analyses are performed with propensity-score weighing; from now, we report counts, proportions and odds ratios for the weighted population, unless specified otherwise. Figure S5 reports weighted counts and proportions in access to RT-PCR testing: weighing ensures that the characteristics of the tested population are similar to those of the whole cohort.
RT-PCR is positive in 63% of tested cases. We report results on the tested population in Fig. 2a,b, and Table S1. We do not find any significant effect of age and sex. Tested smokers are less likely to be RT-PCR+ (46% are RT-PCR+ vs 66%, p < 0.0001). Patients without comorbidities are more likely to be RT-PCR+ (66% vs 60% for patients with comorbidities, p < 0.0001), as well as patients with anosmia, ageusia, anorexia, fever, fatigue, cough, myalgia (p < 0.0001). In contrast, patients with breathlessness and cardiopulmonary symptoms are less likely to be RT-PCR+ (60% vs 63%, p < 0.0001), suggesting that RT-PCR is less sensitive for patients with pulmonary symptoms than for other patients with suspected Covid-19, although indication bias could also impact this result. In echo to this observation, patients with respiratory comorbidities are less likely to be tested positive than other patients (52% vs 63% for patients without respiratory comorbidities, p < 0.0001). Other comorbidities have no significant association with RT-PCR results.
Hospitalized patients are more likely to be RT-PCR+ than non-hospitalized patients (75% vs 61% for outpatients, p < 0.0001), a potential cause of bias in our analysis; yet, as indicated in Figs. 2c and S4, the findings above also hold within the population of non-hospitalized patients. We note that RT-PCR tests performed more than 12 days after the first symptoms were 58% negative (4.2 times more negative than average, Fig. S3b).
Anosmia/ageusia, cardiopulmonary signs and fever predict RT-PCR result in patients with clinically suspected Covid-19 infection
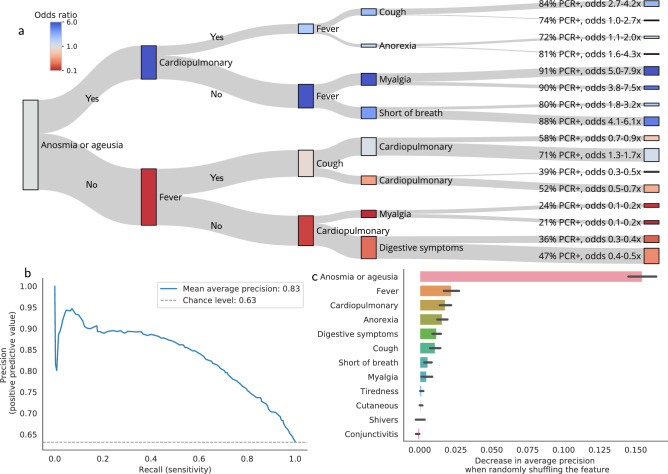
The strong association between symptoms and RT-PCR result encourages us to verify how symptoms effectively predict the RT-PCR result. We focus on symptoms as predictive factors to train a decision tree for RT-PCR testing.
In the held-out group (2562 patients), the decision tree (trained on 10,248 patients) achieves 0.83 mean average precision (Fig. 3c, 0.63 chance level). It identifies combinations of symptoms that efficiently separate RT-PCR+ from RT-PCR− patients (Fig. 3a), and predict RT-PCR results on newly seen patients. Permutation importance (PI, Fig. 3b) tests show that anosmia/ageusia is the most important splitting criteria (PI = 0.133 ± 0.009), followed by cardiopulmonary symptoms (PI = 0.017 ± 0.004) and fever (PI = 0.016 ± 0.004). As reported in Fig. 3a, in the evaluation cohort, 86% of the patients with anosmia/ageusia are RT-PCR+ (OR 6.18, IC[5.89–6.47]). In the non anosmic/ageusic group (1403 patients), patients with fever are less likely to be RT-PCR+ (OR 0.83, IC[0.80–0.86]). Patients with cardiopulmonary symptoms and no fever are very unlikely to be RT-PCR+ (OR 0.18, IC[0.17–0.20]). The decision tree splits on the held-out data and on the whole cohort are reported in Figs. S6 and S7, with associated values reported in Tables S2 and S3. Overall, the trained decision tree identifies combinations of symptoms that are predictive of high chance of RT-PCR positivation (anosmia or ageusia), or low chance of RT-PCR positivation (no anosmia or ageusia, no fever but cardiopulmonary symptoms). Those respectively correspond to cases where Covid disease is very likely, and cases for which RT-PCR has a low sensitivity. For patients experiencing such symptoms, performing a RT-PCR has a low marginal value to adjust Covid-19 diagnosis.
Figure 3.
Marginal value of RT-PCR testing in patients with clinically suspected Covid-19 infection. Estimation and evaluation using testing propensity-score weights. (a) Decision paths of the tree, applied to evaluation patients. A decision tree classifier is trained on 80% of the tested patients. It predict RT-PCR positivity using 12 features: breathlessness, anorexia, tiredness, digestive signs (diarrhea/vomiting), conjunctivitis, cutaneous symptoms (rash/frostbites), shivers, myalgia, cough, fever, cardiopulmonary symptoms (breathlessness + chest pain/oppression) and chemosensory impairment (anosmia/ageusia). We evaluate the decision tree on 20% held-out patients and illustrate how it splits this population. Each node is a splitting criterion (presence of the symptoms to the top, absence to the bottom). The colour of each node corresponds to the odds ratio of being RT-PCR+ at this stage of the decision path. For each leaf, the probability and odds ratio of being RT-PCR+ are reported (see Figs. S6, S8 and Table S1 for details). (b) Permutation features importance on the evaluation set. The permutation importance is an indicator of the relevance of a feature at predicting RT-PCR positivity. It measures the decrease in the model score (here, average precision) when a single feature is randomly shuffled. We report the permutation importance on the left-out evaluation data (20% of the dataset) for each feature of the decision tree. Error bars are the standard deviations of the importance through 50 different permutations. (c) Performance of the decision tree on the test set. Precision-recall curve of the decision tree on the 20% held-out set of tested patients.
The findings that we report hold for multiple training/held-out data separation (Fig. S8); they remain similar without propensity score weighing (Fig. S9), and when performing the analysis within the population of ambulatory patients only (Fig. S10).
Diagnostic strategy based on symptoms to target RT-PCR testing in patients suspected with Covid-19 infection
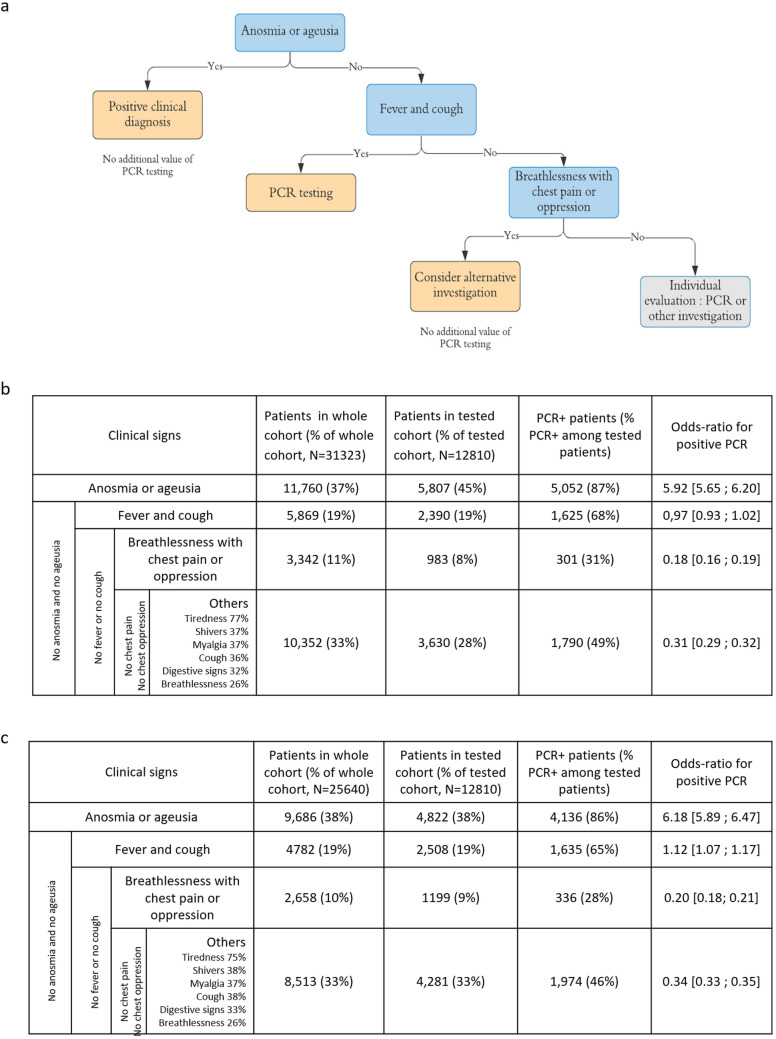
We adapted the estimated decision tree into an actionable testing strategy based on clinical signs (Fig. 4a), taking into account that RT-PCR positivity establishes the diagnosis of Covid-19 infection, but that RT-PCR negativity is of little clinical help, since RT-PCR negativity on the nasopharyngeal swab may reflect either the complete absence of virus, or the absence of virus in the nasal cavity at the time of the swab, or a poorly performed swab, or a false negative RT-PCR, for instance due to a low quantity of virus4. The grouping of patients who have answered the questionnaire based on the decision tree criteria is reported in Fig. 4b, along with the results of RT-PCR in each group. Anosmia or ageusia (observed in 45% of tested patients) are highly predictive of RT-PCR+ (86% RT-PCR+), which justifies establishing a clinical diagnosis of Covid-19 infection without performing a RT-PCR. In the absence of ageusia/anosmia, the association of fever and cough (19% of patients) is not specific to Covid-19 infection: RT-PCR is useful in this case (65% of the group is RT-PCR+).
Figure 4.
Added value of RT-PCR testing in patients with clinically suspected moderate Covid-19 infection based on their symptoms. (a) Proposal of a diagnostic strategy in medical practice, for patients with clinical suspicion of moderate Covid-19 infection by a physician. Anosmia or ageusia are predictive of RT-PCR+ and these patients could be diagnosed based on clinical symptoms only. In case of fever and cough, RT-PCR testing has a good diagnostic value. Then, breathlessness associated with chest pain or oppression is predictive of RT-PCR−, although these symptoms may be signs of Covid-19 pulmonary infection. Therefore, RT-PCR is little valuable in this group and an alternative investigation, such as chest imaging, is indicated. For the remaining patients, RT-PCR is of little added value, but this group is heterogeneous and RT-PCR or alternative investigations should be considered depending on the clinical presentation. (b) Description of the different clinical groups defined by the decision tree. The non-weighted numbers, proportions and odds-ratios of being RT-PCR+ in each group are provided. RT-PCR testing has a different added value for each group: it is less useful for groups with RT-PCR+ odds ratios far away from 1. (c) Same description as (b) with propensity-score weighing. Findings are similar.
Cardiopulmonary symptoms, i.e. breathlessness with chest oppression or pain, are predictive of negative RT-PCR results (28% of the group is RT-PCR+, 8% of tested patients). RT-PCR thus has a poor diagnostic value in this case, justifying the use of another diagnostic investigation, especially in those patients who may be at high risk of complication. The rest of the patients is a heterogeneous group presenting with flu-like illness, moderate breathlessness or digestive symptoms and could benefit from RT-PCR or other investigations depending on the physician evaluation.
Figure 4c reports numbers without propensity-score weighing, with similar findings. Among patients that have answered the survey, the decision tree validates the diagnosis of Covid-19 without any investigation in 11,760 patients (true counts, 38% of the whole cohort). It leads to maintaining RT-PCR as a first-line diagnostic tool in 19% of cases. Among patients without anosmia/ageusia and with cardiopulmonary signs, chest imaging was only performed in 18% (13% among the complementary group), where the decision tree recommends systematic testing.
Discussion
In this study, we estimated a model that predicts RT-PCR results from clinical presentation, based on 12,810 symptomatic patients with suspected Covid-19 infection, in order to prioritize RT-PCR access and adapt the diagnostic strategy to each patient. Until now, several tests have been used to confirm the diagnosis of Covid-19 infection, and RT-PCR is the closest to a gold standard. It is a very specific test for this disease, with a high positive predictive value. Yet it is not sensitive to the disease in general4, due to the possible presence of the virus in other localizations and to many biases in its realization11. High priority patients who should be tested include hospitalized patients, symptomatic healthcare workers, symptomatic residents in congregate living settings, and selected contacts. Ideally, all symptomatic patients, regardless of the symptoms, and all selected asymptomatic people should be tested12. Other investigations, especially chest imaging, improve the sensitivity of Covid-19 diagnosis in some groups of patients13. Serological tests are developing but turn positive late for diagnosis14. In this context, a diagnostic strategy combining clinical evaluation and targeted investigations is necessary, to ensure effective identification of all cases and security of patients at risk of severe disease. Artificial intelligence has been used to optimize diagnostic testing in the epidemics context, based on CT-scan automated interpretation, whereas our approach is based on the clinical presentation15. This approach underlines the importance of a precise clinical evaluation in the case of a newly emerging disease, necessary to gather information about different symptomatic presentations.
The COVIDOM cohort is one of the largest ambulatory populations with suspected Covid-19. Patients are younger than in the series of hospitalized patients and predominantly women2. Our clinical findings are congruent with data already published. Focusing on the patients with chemosensory symptoms, who form an important clinical subgroup in our decision algorithm, we found the same characteristics in the COVIDOM cohort as in the literature: in comparison with Covid-19 patients in general, they are younger, predominantly women, and they have fewer comorbidities, except for asthma which was more frequent14,15. According to recent discussions, anosmia is likely due to both mucosal inflammatory reaction and central nervous system infection through the olfactory nerve22, as described for SARS-CoV in mice23.
Access to RT-PCR in the COVIDOM cohort does not follow the theoretical guidelines: RT-PCR is neither systematically performed on hospitalized patients (80%), nor on symptomatic patients (41%). Some groups of patients, not supposed to be at high risk, including women and non-smokers, are tested more often (both 43%). In addition to showing that RT-PCR is not available for all patients who should be tested, Fig. 1c underlines that smokers with a priori higher respiratory risk are less likely to be tested (p < 0.0001), which was not expected. This disparity in RT-PCR testing is not due to explicit medical targeting, but to limited access, which confirms the need for a strategy to prioritize those tests. Although political decisions are being taken to make testing as widely available as possible, the number of RT-PCR will be limited. Moreover, performing RT-PCR in some patients will not systematically help us to correctly diagnose, isolate and treat.
We found that, in the Covid-19 epidemic context, the clinical presentation is predictive of the positivity of RT-PCR in some groups. Patients with anosmia or ageusia represent 50% of our cohort, 47% of symptomatic patients with RT-PCR+ in Europe16, and up to 86% of symptomatic patients referred to an ENT clinic17. We show that 90% of tested patients with these symptoms (OR 5.61–6.14) turn out to be RT-PCR+, which is consistent with the high positive predictive values of anosmia (84.7%) and ageusia (88.1%) for SARS-CoV-2 infection found by Fontanet et al. also in France18. In the current context, those patients can be considered as infected with Covid-19 with little approximation even without RT-PCR testing. This validates with statistical rigor the empirical recommendations found in the literature19,20. In addition, the specific form that these symptoms take for Covid-19 limits the risk of false positive diagnosis: although the prevalence of olfactory and taste dysfunction in adults ranges between 3.8 and 13.5%21,22, with 39% of cases retrospectively attributed to an upper respiratory tract infection23, unexplained sudden onset anosmia or ageusia is extremely rare in clinical practice. Finally, our analysis is based on a very coarse evaluation of anosmia or ageusia, defined as the recent onset of loss of smell or taste, as subjectively reported by the patient in a multiple choice question. There is no doubt that critical and precise medical history taking helps reduce the rate of false positive diagnoses (10% of RT-PCR− in our cohort, which means maximum 10% of differential diagnosis), thanks to the descriptions of SARS-CoV2-associated olfactory and gustatory symptoms16,17.
Our analysis then underlines that in patients without chemosensory symptoms but with cough and fever, which are non specific symptoms, representing 19% of our cohort, RT-PCR results cannot be predicted and testing has a relevant clinical value. RT-PCR has a useful positive value and seems clinically relevant to separate differential diagnoses, although RT-PCR+ is not systematically evidence of Covid-19 and proves only SARS-Cov-2 presence in the sample4.
Finally, our study singles out a third particular group, namely patients with breathlessness and chest pain or oppression, among those without anosmia/ageusia and fever with cough, namely 11% of our cohort. RT-PCR testing has a poor diagnostic value in this group, with only 30% of positive results. Whether the remaining patients have Covid-19 with RT-PCR− or a differential diagnosis is not established in our series. In both situations, chest CT-scan, whenever available, may be more reliable by showing specific pulmonary lesions, such as ground-glass opacities13. One physiopathological hypothesis in Covid-19 transmission is that the SARS-CoV-2 is transmitted through the upper respiratory tract, where it could either remain, after a general efficacious inflammatory reaction, or spread to the lower respiratory tract, causing severe pneumonia. In this scenario, anosmia and ageusia would not only be of high diagnostic value: they may be predictors of good outcome19. This finding is compatible with the findings in our cohort: the non anosmic/ageusic group is more likely to be admitted in hospital. A positive RT-PCR thus appears to be an indicator of persistent virus in the nose and throat, whereas a negative RT-PCR may indicate migration of the virus and potential respiratory complications.
In the COVIDOM cohort, applying the diagnostic strategy would lead to making a purely clinical diagnosis in 37% of symptomatic cases. This would allow better targeting of RT-PCR testing, particularly indicated in non anosmic/ageusic patients with fever and cough. The other patients who additionally present breathlessness, chest pain or oppression will rather benefit from another first-line investigation: 70% of RT-PCR are negative in this case despite Covid-19 suspicion, which suggests a high false negative rate.
As RT-PCR testing has a low sensitivity to Covid-19 infection,we may wonder how many times this test should be replicated for reliability. In some studies, RT-PCR testing was performed as many times as necessary to confirm the infection when clinical suspicion was very high24,25. In our study, the mean number of tests was 1.20 ± 0.64 and did not differ in particular population groups. The clinical presentation would be a clue for the clinician to decide whether repeating the test will be useful, and the evolution may also lead to alternative investigations. Moreover, as already observed10, the delay between the first symptoms and the RT-PCR test has a significant effect on the RT-PCR result (odds of being RT-PCR+ are 1.03–1.04 times lower on day J + 1 than day J, cf Fig. S3b), which prompts to perform RT-PCR as early as possible, in the absence of chemosensory symptoms.
There are a number of important limits in our study. First, the results of this study are to be interpreted in the specific setting of the Covid-19 epidemics. The cohort is recruited in a region with a high prevalence of the disease, with up to 26% of infected people in some areas of France18. The criterion motivating inclusion in the COVIDOM cohort is the clinical suspicion by a physician of Covid-19 infection. This inclusion criterion is subjective, and highly depends on the epidemiological context in the area. Some patients with a differential diagnosis have inevitably been included in the cohort. RT-PCR− may be due, in our series and in general practice, to a false negative result or to a differential diagnosis, so that RT-PCR− is actually considered as diagnostically inconclusive, due to its low sensitivity4.
Most parameters analyzed were harbored from self-reported questionnaires, with an inevitable rate of mistakes. In particular, performance of the test partially relies on the patient's recollection, whereas RT-PCR results are verified by a medical database. In addition, our study falls short of considering that symptoms appear progressively. We analyze symptoms present during the course of the disease; those may not be present during the first medical evaluation. However, anosmia/ageusia are early signs, developing on average 4.4 days after infection16. They are likely to have developed when the patient seeks medical care (median 5 days, IQ2-8, after the beginning of the symptoms in the COVIDOM cohort). Less importantly, we only analyzed the symptoms provided by the forms submitted to the patients. These forms did not investigate all possible clinical signs and comorbidities that may influence the results; additional symptoms were identified manually in the patients commentaries, especially headaches, vertigo and upper respiratory tract symptoms (rhinitis or chronic rhinosinusitis, nasal obstruction, rhinorrhea, throat pain). Preliminary analyses show that these items are not key symptoms to predict RT-PCR results; yet they should be probed in future clinical investigations.
Finally, in the methods we used, our analysis of RT-PCR results is based on the tested population, which is not representative of all patients infected with SARS-CoV-2. We challenged our reweighing strategy by reproducing the same analysis without this strategy and note that a similar decision tree is obtained, which shows that the final diagnostic algorithm is reliable. It could also be completed by adding the date of the beginning of the symptoms and the patient’s characteristics as predictors, in addition to the clinical presentation.
Conclusion
In the context of SARS-CoV-2 epidemics, we found that the clinical presentation may be predictive of RT-PCR+ in subjectively anosmic/ageusic patients, allowing to make the diagnosis without any investigation. We propose that patients with fever and cough be tested by RT-PCR in priority, and we show that RT-PCR does not provide useful results for patients with breathlessness and chest pain or oppression. In that group, chest imaging as a first-line investigation may be more useful. Our findings may help target RT-PCR tests in the symptomatic population, and contribute to crafting the best strategy to manage the pandemic.
Supplementary Information
Acknowledgements
Data used in preparation of this article were obtained from the AP-HP Covid CDW Initiative (ACCI) database. A complete listing of the ACCI members can be found at: (https://eds.aphp.fr/covid-19).
We thank FALZON Alexandre, FAYOLLE Guillaume, LAPORTE Fanny, Amélie TORTEL and all the Nouveal-e Santé team for their help in the web application and regional center surveillance interface development. We also thank DEBASTARD Laurent, GRENIER Alexandre, HODY Julien, PENN Thomas and the Paris region URPS (Union régionale des professionnels de santé) for their help in the development and spreading of the Covidom solution.
We thank the Polytechnique network for helping with the volunteers recruitment.
Author contributions
C.A., C.C. and A.M. were involved in the study conception, data extraction, data analysis, interpretation of results, drafting the manuscript and approving the final version of the manuscript. J.M. was involved in the study conception, data extraction, data analysis, and approving the final version of the manuscript. M.B., A.G. was involved in the study conception, data extraction, data analysis, interpretation of results, and approving the final version of the manuscript. A.D. was involved in the study conception, data analysis, interpretation of results, critically revising the manuscript and approving the final version of the manuscript. E.D. was involved in critically revising the manuscript and approving the final version of the manuscript. A.D. was involved in interpretation of the results, critically revising the manuscript and approving the final version of the manuscript. X.L. was involved in COVIDOM development, in interpretation of the results, critically revising the manuscript and approving the final version of the manuscript. Y.Y. was involved in the study conception, data analysis, interpretation of results, critically revising the manuscript and approving the final version of the manuscript. P.J. was involved in COVIDOM development, in the study conception, interpretation of results, critically revising the manuscript and approving the final version of the manuscript. N.P. was involved in EDS data access and function, and approving the final version of the manuscript.
Funding
The authors declare no specific funding for this study. COVIDOM received funding by the Programme Hospitalier de Recherche Clinique 2020 of the French Ministry of Health, by a research fund by APHP-Fondation de France and from the EIT Health specific Covid-19 fund. Arthur Mensch was funded by ERC grant Noria.
Data availability
Data available upon request for academic researchers.
Competing interests
All authors have completed the ICMJE uniform disclosure form at http://www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) and declare: no support from any organisation for the submitted work; no financial relationships with any organisations that might have an interest in the submitted work in the previous 3 years; no other relationships or activities that could appear to have influenced the submitted work.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Caroline Apra, Charlotte Caucheteux and Arthur Mensch.
A list of authors and their affiliations appears at the end of the paper.
Contributor Information
The AP-HP/Universities/Inserm COVID-19 Research Collaboration:
Caroline Apra, Charlotte Caucheteux, Arthur Mensch, Jenny Mansour, Mélodie Bernaux, Agnès Dechartres, Erwan Debuc, Xavier Lescure, Aurélien Dinh, Youri Yordanov, Patrick Jourdain, Arthur Mensch, Charlotte Caucheteux, Caroline Apra, Jenny Mansour, Nicolas Paris, Alexandre Gramfort, Amélie Aime-Eusebi, Caroline Apra, Alexandre Bleibtreu, Erwan Debuc, Agnès Dechartres, Laurène Deconinck, Aurélien Dinh, Patrick Jourdain, Christine Katlama, Josselin Lebel, François-Xavier Lescure, Youri Yordanov, Yves Artigou, Amélie Banzet, Elodie Boucheron, Christiane Boudier, Edouard Buzenac, Marie-Claire Chapron, Dalhia Chekaoui, Laurent De Bastard, Erwan Debuc, Aurélien Dinh, Alexandre Grenier, Pierre-Etienne Haas, Julien Hody, Michèle Jarraya, Patrick Jourdain, Louis Lacaille, Aurélie Le Guern, Jeremy Leclert, Fanny Male, Jerôme Marchand-Arvier, Emmanuel Martin-Blondet, Apolinne Nassour, Oussama Ourahou, Thomas Penn, Ambre Ribardiere, Nicolas Robin, Camille Rouge, Nicolas Schmidt, and Pascaline Villie
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-021-99991-6.
References
- 1.Coronavirus Update (Live): 3,688,107 Cases and 255,174 Deaths from COVID-19 Virus Pandemic—Worldometer (2020).
- 2.Chen N, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. Lancet. 2020;395:507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Xu B, et al. Chest CT for detecting COVID-19: A systematic review and meta-analysis of diagnostic accuracy. Eur. Radiol. 2020 doi: 10.1007/s00330-020-06934-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Patel R, et al. Report from the American Society for Microbiology COVID-19 International Summit, 23 March 2020: Value of Diagnostic Testing for SARS–CoV-2/COVID-19. mBio. 2020;11(2):e00722-20. doi: 10.1128/mbio.00722-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5., Place des tests sérologiques dans la stratégie de prise en charge de la maladie COVID-19. Haute Aut. Santé (2020).
- 6.Institut Pasteur, WHO, Protocol: Real-time RT-PCR assays for the detection of SARS-CoV-2 (2020).
- 7.Reusken CBEM, et al. Laboratory readiness and response for novel coronavirus (2019-nCoV) in expert laboratories in 30 EU/EEA countries, January 2020. Eurosurveillance. 2020;25:2000082. doi: 10.2807/1560-7917.ES.2020.25.6.2000082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Breiman L, Friedman JH, Olshen RA, Stone CJ. Classification and Regression Trees. Wadsworth; 1984. [Google Scholar]
- 9.Pedregosa F, et al. Scikit-learn: Machine learning in python. J. Mach. Learn. Res. 2011;12:2825–2830. [Google Scholar]
- 10.Seabold, S. & Perktold, J. Statsmodels: econometric and statistical modeling with python. In Proc. 9th Python Sci. Conf., 92–96 (2010).
- 11.Lippi G, Simundic A-M, Plebani M. Potential preanalytical and analytical vulnerabilities in the laboratory diagnosis of coronavirus disease 2019 (COVID-19) Clin. Chem. Lab. Med. 2020;58(7):1070–1076. doi: 10.1515/cclm-2020-0285. [DOI] [PubMed] [Google Scholar]
- 12.CDC, Coronavirus Disease 2019 (COVID-19). Cent. Dis. Control Prev. (2020).
- 13.Kim H, Hong H, Yoon SH. Diagnostic performance of CT and reverse transcriptase-polymerase chain reaction for coronavirus disease 2019: A meta-analysis. Radiology. 2020;296(3):E145–E155. doi: 10.1148/radiol.2020201343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sethuraman N, Jeremiah SS, Ryo A. Interpreting diagnostic tests for SARS-CoV-2. JAMA. 2020 doi: 10.1001/jama.2020.8259. [DOI] [PubMed] [Google Scholar]
- 15.Mei X, et al. Artificial Intelligence-enabled rapid diagnosis of patients with COVID-19. Nat. Med. 2020 doi: 10.1038/s41591-020-0931-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Klopfenstein T, et al. Features of anosmia in COVID-19. Med. Mal. Infect. 2020 doi: 10.1016/j.medmal.2020.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lechien JR, et al. Olfactory and gustatory dysfunctions as a clinical presentation of mild-to-moderate forms of the coronavirus disease (COVID-19): A multicenter European study. Eur. Arch. Oto-Rhino-Laryngol. Off. J. Eur. Fed. Oto-Rhino-Laryngol. Soc. EUFOS Affil. Ger. Soc. Oto-Rhino-Laryngol. Head Neck Surg. 2020 doi: 10.1007/s00405-020-05965-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fontanet A, et al. Cluster of COVID-19 in northern France: A retrospective closed cohort study. medRxiv. 2020 doi: 10.1101/2020.04.18.20071134. [DOI] [Google Scholar]
- 19.Villalba NL, et al. Anosmia and dysgeusia in the absence of other respiratory diseases: Should COVID-19 infection be considered? Eur. J. Case Rep. Intern. Med. 2020;7:001641. doi: 10.12890/2020_001641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wee LE, et al. The role of self-reported olfactory and gustatory dysfunction as a screening criterion for suspected COVID-19. Eur. Arch. Otorhinolaryngol. 2020 doi: 10.1007/s00405-020-05999-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schubert CR, et al. Olfactory impairment in an adult population: The Beaver Dam Offspring Study. Chem. Senses. 2012;37:325–334. doi: 10.1093/chemse/bjr102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liu G, Zong G, Doty RL, Sun Q. Prevalence and risk factors of taste and smell impairment in a nationwide representative sample of the US population: A cross-sectional study. BMJ Open. 2016;6:e013246. doi: 10.1136/bmjopen-2016-013246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Merkonidis C, et al. Characteristics of chemosensory disorders—Results from a survey. Eur. Arch. Oto-Rhino-Laryngol. Off. J. Eur. Fed. Oto-Rhino-Laryngol. Soc. EUFOS Affil. Ger. Soc. Oto-Rhino-Laryngol. Head Neck Surg. 2015;272:1403–1416. doi: 10.1007/s00405-014-3210-4. [DOI] [PubMed] [Google Scholar]
- 24.Ramdas K, Darzi A, Jain S. ‘Test, re-test, re-test’: using inaccurate tests to greatly increase the accuracy of COVID-19 testing. Nat. Med. 2020;26:810–811. doi: 10.1038/s41591-020-0891-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jiang X-L, et al. Transmission potential of asymptomatic and paucisymptomatic SARS-CoV-2 infections: A three-family cluster study in China. J. Infect. Dis. 2020 doi: 10.1093/infdis/jiaa206. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data available upon request for academic researchers.