Abstract
Background:
Preventing subsequent falls in persons recovering from hip fracture is paramount. The Four Square Step Test (FSST) is a fast, easy measure of dynamic balance, with times >15s previously associated with multiple falls risk in older adults. This study investigates among hip fracture patients (1) FSST performance, and how (2) unique population characteristics (such as fracture side) and (3) cognition impact FSST performance.
Methods:
Hip fracture patients (n=40) age 60 and older came from an ancillary study to a larger randomized controlled trial testing two 16-week in-home physical therapy interventions after completion of usual care rehabilitation. Baseline measurers included: FSST, demographics, fracture characteristics, Modified Mini-Mental Examination (3MS), Hooper Visual Organizational Test (HVOT), and Trails Making Tests (TMT) A and B.
Results:
Of 40 hip fracture patients, 13 did not complete the FSST at baseline and were significantly older (p=0.040) and performed worse on cognitive tests (3MS, HVOT, TMT-B; p<0.05). Mean FSST time was 24.3±13.1(s) for the other 27, of whom 7 finished in <15s. A significant 3-way interaction was observed, such that those with left side pertrochanteric fractures who performed poorly on the HVOT did significantly worse on the FSST (p<.01, R-square=0.93).
Discussion:
Almost one-third of hip fracture patients could not perform the FSST after completing usual care rehabilitation. Inability to perform FSST was not random, as those without FSST tests were physically and cognitively worse than those who did perform the FSST. Among those who could attempt the FSST, few performed well. Cognitive ability related to spatial orientation and fracture characteristics such as fracture side and fracture type has a synergistic effect on FSST performance.
Conclusions:
This is one of the first studies to assess FSST in a hip fracture population. At 4 months post- hip fracture, most patients cannot perform the FSST in <15 seconds. Fracture side and fracture type appear important to FSST performance, as does cognition. More work needs to be done longitudinally to study FSST in hip fracture patients.
Keywords: Four Square Step Test, Hip Fracture, Cognition, Fracture Side
INTRODUCTION
Hip fractures are acute injuries resulting in chronic pain and disability. Among adults 65 and older in the United States there are approximately 300,000 hip fractures per year;1 95% of which occur after a fall from standing height.2 Given that falls are the primary instigating incident for hip fractures,1 and hip fracture patients are at increased risk for secondary falls, it is valuable to assess fall risk in this vulnerable population. A unique characteristic of the hip fracture population is the unilateral weakening and pain of the fractured side, although global deconditioning has been observed as patients recuperate, resulting in increased instability especially during compromised balance scenarios.2–4
Cognitive status is a known risk factor for hip fracture and falls.3,4 It has been estimated that 20% of hip fracture patients have pre-existing dementia.5 Cognitive impairment increases risk for hip fracture 3-fold compared to non-impaired older adults.6,7 Given that cognition impacts both falls and hip fracture risk independently, it is reasonable to assume that cognition will also impact balance tests.
The Four Square Step Test (FSST) was developed by Dite and Temple8 as a quick and easy-to-administer test for community-dwelling older adults, testing balance and motor planning to predict falls risk. Completing the FSST in >15 seconds has been found to be indicative of multiple falls risk according to normative data.8 FSST has superb sensitivity (92%), specificity (93%), positive (86%) and negative predictive value (96%) for predicting multiple versus non-multiple fallers. The reliability and validity of FSST compared to other mobility and balance tests [i.e., Six Minute Walk Test (SMWT)9, Timed Up and Go10, Step Test11] has been assessed across multiple disease conditions including stroke, Parkinson’s disease, muscular sclerosis, traumatic brain injury, and vestibular dysfunction.12–15 Despite the use of FSST in other mobility limited populations, FSST has not been studied among hip fracture patients.
This study is one of the first to implement and assess the FSST in an older adult hip fracture population. To our knowledge, it is also unique in examining the relationship between FSST performance and fracture side, a critical trait of the hip fracture population that could impact a patient’s ability to complete the FSST. Lastly, the association between FSST and cognitive status of hip fracture patients has not been established.
The study aims are (1) to determine if FSST can be performed by hip fracture patients, (2) if unique population characteristics such as fracture side impact FSST performance, and (3) to what extent cognition impacts FSST performance in hip fracture patients. It was hypothesized that fracture side will not impact FSST performance and that those with better cognition will have faster FSST times.
METHODS
Study Design and Participants
This current study design was a cross-sectional analysis utilizing baseline data of the Community Ambulation Mechanistic Pathways (CAP-MP) study. CAP-MP was an ancillary study to The Community Ambulation Project (CAP): a multi-site randomized controlled trial (RCT) testing two home-based physical therapy interventions in hip fracture patients.16,17 CAP recruited from 4 area hospitals from August 2013-August 2017. Subjects were recruited in hospital, completed baseline testing, and were randomized for the RCT within 26 weeks of admission after completing standard care rehabilitation as prescribed by their individual doctors before randomization. Mean number of weeks from hospital admission to baseline testing was 16.15 (5.68). CAP-MP was offered at one clinical site. Baseline measures for CAP-MP were collected after baseline data was complete for the parent study and prior to randomization. Baseline testing for CAP-MP had to be completed within 7 days of baseline testing for the parent study. CAP and CAP-MP were approved by the University Institutional Review Board.
Participants were eligible to participate based on the following inclusion criteria: (1) age 60 or older, (2) community-dwelling at the time of fracture and randomization, (3) hip fracture requiring surgical fixation, (4) finished standard rehabilitation prior to enrollment, (4) ambulated without human assistance within 2 months before fracture, (5) had a minimal trauma, non-pathologic fracture, (6) unable to walk 300m or more in 6 minutes, and (7) randomized within 26 weeks from the hospital admission. The primary outcome for CAP RCT was being a community ambulator walking 300 meters or more in 6 minutes so people already achieving that threshold at baseline were excluded. Exclusion criteria for safety and feasibility: walked <4 meters in 40 seconds for the first four meters of the SMWT or if they developed chest pain, intolerable dyspnea, or severe pain during the SMWT; score ≤73 on the Modified Mini Mental State Examination (3MS); any lower extremity amputation, severely diminished sensation, or ulceration; not fully weight-bearing on fractured or non-fractured leg at randomization, and medical contraindications for exercise.
Measures
Demographics, Modified Mini-Mental State Examination (3MS)18, and Short Physical Performance Battery (SPPB)19 were collected as part of the CAP baseline visit. The FSST8, Hooper Visual Organization Task (HVOT)20, Trail-Making Test21,22, and 50ft gait speed23 were collected at the CAP-MP baseline visit. Time to baseline FSST testing was calculated as the difference between the hospital admission date and FSST testing date. See Table 1.
Table 1.
CAP-MP Sample Characteristics and FSST (s) Correlations
| Mean (SD) | r (p-value) | |
|---|---|---|
| Age (years) | 77.60 (7.02) | 0.20 (0.321) |
| Years of Education | 12.74 (2.06) | 0.19 (0.332) |
| Weeks between Admission and FSST | 16.15 (5.68) | −0.08 (0.659) |
| BMI | 25.91 (3.80) | 0.18 (0.366) |
| Comorbidities | 6.1 (2.84) | −0.132 (0.519) |
| HVOT Score (0–30) | 20.48 (5.06) | −0.46 (0.014) |
| 3MS Score (73–100) | 91.97 (6.04) | 0.05 (0.806) |
| SPPB Score (0–12) | 5.86 (214) | −0.39 (0.047) |
| 50feet gait speed (m/s) | 0.66 (0.19) | −0.43 (0.023) |
| FSST (s) | 24.31 (13.05) | |
| Median (IQR) | ||
| SPPB | 6.00 (3.00) | −0.40 (0.047) |
| Trails | ||
| Trails A (s) | 65.94 (48.10) | 0.40 (0.035) |
| Trails B (s) | 51.00 (31.00) | 0.23 (0.240) |
| N (%) | ||
| Fracture Side | −0.68 (<0.001) | |
| Left | 21 (52.5) | |
| Right | 19 (47.5) | |
| Fracture Type | 0.46 (0.014) | |
| Femoral Neck | 20 (50) | |
| Pertrochanteric | 17 (42.5) | |
| Unspecified | 3 (7.5) | |
| Sex | −0.39 (0.041) | |
| Male | 13 (32.5) | |
| Female | 27 (67.5) | |
| Finished FSST | 27 (67.5) | |
| Passed FSST (<15 s) | 7 (25.93) | |
| Competent HVOT (≤19) | 27 (69.23) | −0.74 (<0.001) |
| Competent Trails A (≤78 s) | 32 (80) | −0.43 (0.023) |
| Competent Trails B (≤ 273 s) | 30 (75) | −0.12 (0.538) |
Note FSST: Four Square Step Test, BMI: Body Mass Index, HVOT: Hooper Visual Organization Test, 3MS: Modified Mini-Mental State Examination, SPPB: Short Physical Performance Battery
Cognitive Measures
Modified mini-mental state examination (3MS)
Modified mini-mental state examination (3MS) assesses attention and working memory, verbal recall, expressive language, verbal fluency, visual construction, and reasoning and judgment.24,25 Scores range from 0 to 100, but participants with 3MS <73 were excluded from CAP.26 The 3MS has been found to be reliable (Cronbach’s alpha = 0.871 to 0.839) and have excellent construct validity (even marginally better than the Mini Mental State Examination) and has been shown to be a predictor of functional outcomes than the Mini Mental State Examination.24,27
Hooper visual organization test (HVOT)
Hooper visual organization test (HVOT)20 measures general and specific cognition, particularly visual analysis and synthesis, short- and long-term memory, and labeling familiar objects. HVOT is significantly related to “visual-perceptual-constructional skills”.28 The cut-off score for HVOT is ≤19 (Impaired HVOT), scores range from 0 to 30.20,28 HVOT has been demonstrated to be reliable (Cronbach’s alpha = 0.882) and have excellent internal consistency.28,29
Trails A & B
Trails A & B were measured separately in total time to completion(s). The Trail-Making Tests cover domains of mental tracking and executive function.25 The cut-point for impairment on Trails A is 78 seconds, Trails B is 273 seconds.25,30 The maximum allowed time was 5 minutes for both scales, with longer times set to 301seconds. Trail Making Test A has good to adequate retest reliability (0.76–0.89) and Trials B has excellent re-test reliability (0.86–0.94).31 The construct validity for the direct and derived Trails items are also good, though Trails B may be more difficult due to additional motor skills demands.32
Physical Function Measures
Four square step test (FSST)
Four square step test (FSST) is administered by placing four canes on the floor forming quadrants.8 The test is timed and assesses rapid stepping and obstacle avoidance. FSST was first demonstrated with verbal instructions to participants and then administered in two timed trials, the best (fastest) time of the two was used. Times over one minute were recorded as 61 seconds. Participants start from the upper right quadrant moving clockwise, stepping laterally to the right, backwards, laterally to the left, forwards, and then counterclockwise over the canes. Participants attempt to remain facing forward while moving into the quadrants, with two feet in each quadrant before moving on to the next, leading with their preferred foot. If participants reported pain or shortness of breath during the measure, the test was stopped and marked as incomplete. No participants reported pain during testing.
Short physical performance battery (SPPB)
Short physical performance battery (SPPB) measures lower extremity function, assessing standing balance, time to rise from a chair 5 times, and 4m gait speed walking at usual pace.19 The SPPB is scored from 0–12. In studies on the predictive validity of the SPPB, scores <10 were predictive of all-cause mortality and higher odds of mobility disability in community dwelling older adults.33 SPPB has excellent test-retest reliability (intraclass correlation coefficient = 0.81).34
50ft gait speed
50ft gait speed was conducted as part of the Modified Physical Performance Test was also used to capture normal gait speed over longer distances.23 Reliability of 50 ft gait speed is excellent (Cronbach’s alpha = 0.97) and it demonstrates concurrent validity with skeletal muscle mass and maximal walking pace.35,36
Statistical Analyses
All analyses were performed using SAS 9.4. Preliminary analysis included descriptive statistics, correlations, chi-square, and t-tests as appropriate for all measures. Binary pass-fail variables were created for cognitive tests and the SPPB, based on cut-points from the literature. Statistical significance was set at p < 0.05.
For Aim1, t-tests and chi-squares (fisher’s exact) were used to compare those participants who could and those who could not complete or attempt the FSST. Unadjusted linear models were run for all participants with FSST times and key variable.
For Aim 2, fracture side was assessed using t-test and chi-square to ensure no group differences. Significant covariates from the unadjusted linear regression models and fracture side|covariate interaction terms were assessed as part of a linear regression model using forward selection based on bivariate significance and R2 values. The best model was selected from the p-value, R2 value, and clinical ease of acquiring the information.
For Aim 3, cognitive measures from the regression models in Aim 1 and the significant interaction terms in Aim 2 were interpreted in the context of hip fracture.
RESULTS
FSST in Hip Fracture Patients
Of the 71 eligible CAP participants randomized at the study site, 40 participated in CAP-MP. See Figure 1. The sample was majority female (67.5%), with a high school education, and only 2 participants were non-white. On average participants were 77.6 ±7.0 years old, had 6 comorbidities, and performed baseline testing 4 months after hip fracture (range 2.5–5 months). Fracture side and fracture type were almost evenly distributed in the sample. Participants who did complete the FSST (n=27; 68%) had a mean completion time of 25.6±14.6s. The minimum time was 11.38s. Most participants, 74% (n=20), took >15 seconds to complete the test. See Table 1.
Figure 1. CAP-MP Consort Diagram.
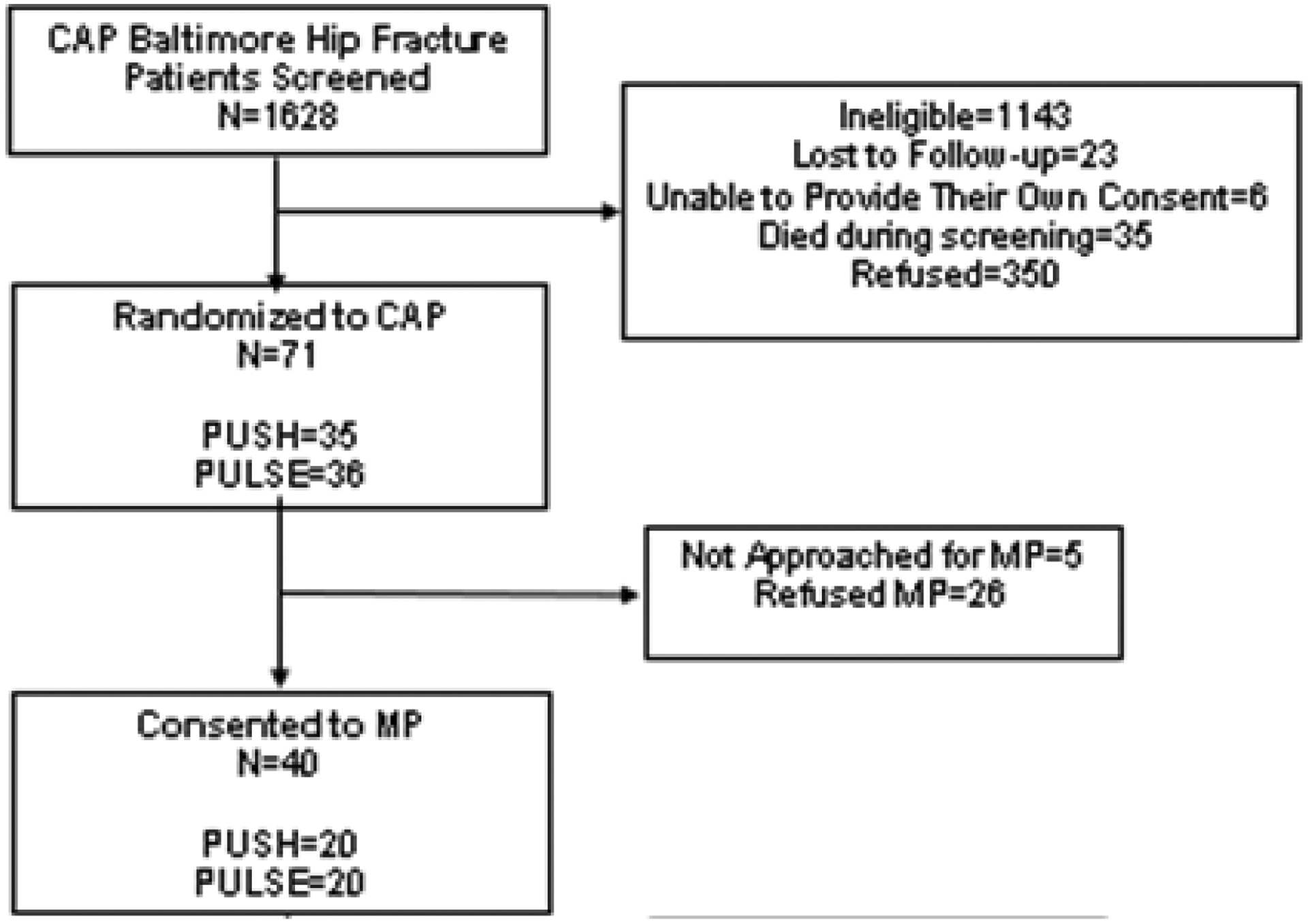
Consort diagram of the study sample from CAP single study site and sub-sample included in CAP-MP. PUSH and PULSE are the treatment arms of the parent CAP study and are described in published work.16, 17 PUSH was an active intervention arm which received 16 weeks of progressive in-home physical therapy, while PULSE was an active control arm which was administered Transcutaneous Electrical Nerve Stimulation (TENS) in the home for 16 weeks.
The covariates that had statistically significant correlations with FSST(s) were the HVOT, Trails A, 50ft gait speed, SPPB, sex, fracture type, and fracture side (all p <.05). In linear regression models of FSST time, Trails A, HVOT, SPPB, 50ft gait speed, sex, and fracture type were all significant (all p< 0.05). Impaired HVOT and fracture side were both significant (p<0.001) with R2 of 0.46 and 0.54 respectively. Forward selection of covariates for regression models did not find any significant demographic covariates listed in Table 1 besides fracture side.
Of the 40 CAP-MP participants 13 did not contribute FSST data. The 13 participants who did not attempt FSST either refused (25%) or were deemed unsafe or unable to perform the test by the administrator (74%). One participant’s values were invalid. There were significant differences between the groups who did and those who did not complete the FSST. See Table 3. Participants who did not contribute FSST data were significantly older, had worse cognitive test scores except Trails A, and performed worse on all physical function tests than participants who performed the FSST (all p< 0.05).
Table 3.
Fracture Side Comparison
| Left Fracture N=20 |
Right Fracture N=19 |
p-value | |
|---|---|---|---|
| Demographics | Mean (SD) | Mean (SD) | |
| Age | 77.81 (8.47) | 77.37 (5.19) | 0.846 |
| Education | 12.65 (2.15) | 12.84 (2.00) | 0.775 |
| BMI | 25.76 (3.78) | 26.07 (3.92) | 0.802 |
| Comorbid Conditions | 6.24 (2.86) | 5.95 (2.89) | 0.751 |
| Weeks from Admission to Randomization | 17.10 (5.85) | 16.81 (5.00) | 0.868 |
| Cognitive Tests | |||
| HVOT | 19.00 (5.96) | 22.05 (3.39) | 0.057 |
| 3MS | 91.43 (6.21) | 92.57 (5.94) | 0.554 |
| Trails A | 77.75 (62.37) | 53.52 (21.46) | 0.115 |
| Trails B | 212.00 (132.9) | 193.00 (137.5) | 0.663 |
| Physical Function Tests | |||
| SPPB | 5.63 (1.67) | 6.11 (2.58) | 0.505 |
| 50ft gait speed (m/s) | 0.61 (0.17) | 0.71 (0.20) | 0.112 |
| FSST | 36.59 (15.47) | 16.93 (4.96) | 0.003 |
| N (Row %) | N (Row %) | ||
| Sex (Female) | 13 (61.90) | 14 (73.68) | 0.427 |
| Completed Four Square (Yes) | 11 (52.38) | 15 (78.95) | 0.079 |
| Education (High school or less) | 13 (52.00) | 12 (48.00) | 0.905 |
| Comorbid Conditions (5–9) | 10 (43.48) | 13 (56.52) | 0.370 |
| SPPB (<6) | 10 (45.45) | 12 (54.55) | 0.324 |
| HVOT (≤ 19) | 11 (40.74) | 16 (59.26) | 0.082 |
| Trails A (≤ 78) | 15 (46.88) | 17 (53.13) | 0.241 |
| Trails B (>273) | 15 (50.00) | 15 (50.00) | 0.721 |
| Fracture Type (Femoral neck) | 8 (40.00) | 12 (60.00) | 0.141 |
Note: BMI= Body Mass Index, HVOT= Hooper visual Organization Task, 3MS= Modified Mini-Mental State Examination, SPPB= Short Physical Performance Battery; p-value based on chi-square and fisher’s exact test as appropriate.
Exploring Fracture Side
T-tests for significant group differences on other measures between left- and right-side fracture were assessed. Only continuous FSST, and Pass/Fail (</> 15 sec) FSST were significantly different by fracture side (p <0.01). Of those with FSST times, 12 were left-side fractures, 15 were right-side fractures. However, zero left-side fractures completed FSST in under 15 seconds compared to 7 right-side fractures. See Figure 2.
Figure 2. FSST Time in Seconds by Side of Fracture.

Best FSST performance in seconds out of two trials at baseline visit stratified by side of fracture (left or right). The dotted line indicates the 15 second cut-point for normative data from community dwelling older adults indicating multiple falls risk. The maximum time is 61 seconds, these individuals failed the test but attempted and completed the maneuvers.
In correlations with FSST(s) only Trails A (R2=0.61), HVOT (R2=0.61), and fracture type (R2=0.62) remained significant when adjusting for fracture side (all p < 0.05). Fracture side was a unique feature of the hip fracture population that was not anticipated to be so strongly associated with FSST.
Interactions with fracture side were assessed. Fracture type, 3MS, Trails B, Impaired HVOT, SPPB all had significant interactions with fracture side (all p<0.05); the HVOT interaction was nearly significant (p = 0.054). Trails B and 3MS, although significant, had relatively small R2 values (0.6) and contributed little to multivariable models. SPPB and HVOT were significantly correlated, and Impaired HVOT had better R2 value, making it more valuable for predictive modeling. The model with fracture side by Impaired HVOT, and fracture side by fracture type was significant at p<.0001, R2 = 0.90. Fracture side by Impaired HVOT had convergence issues when assessing the 3-way interaction between fracture side by fracture type by Impaired HVOT due to 0 cell values. We accepted the slightly less significant interaction from continuous HVOT scores to be able to assess the 3-way interaction of fracture side by fracture type by HVOT. Fracture side by fracture type by HVOT was significant (R2=0.93). See Figure 3.
Figure 3. FSST Time (s) Fracture Side, Fracture Type, and HVOT 3-way Interaction.
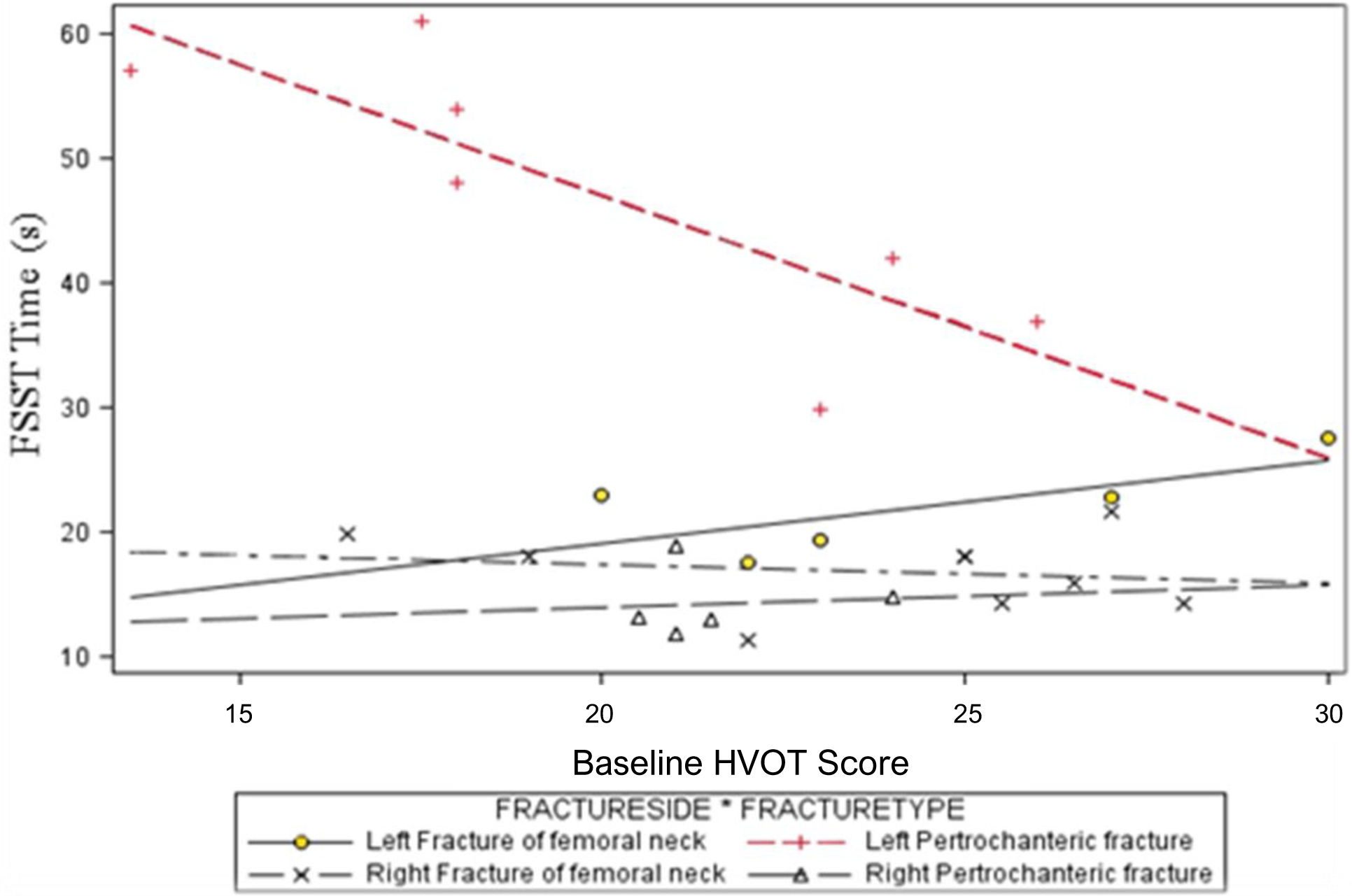
As HVOT performance improves, so too does FSST performance time on average. Everyone with left side fractures failed the FSST. Participants with left side pertrochanteric fracture performed the worst. The mechanisms behind this are not yet known.
As shown in Figure 2, left-side fractures had over-all worse FSST performance. Left-side fractures with non-femoral neck fracture types performed worse than other left-side fractures (with femoral neck fractures). As HVOT performance improved, FSST time significantly improved, making pertrochanteric left-side fractures look more like the other fracture types and right-side fractures, however as the HVOT score becomes lower, indicating worse cognition, there is a dramatic shift in performance and the groups begin to separate distinctly.
FSST and Cognition
Binary HVOT accounted for more variance than continuous HVOT. When modeling fracture side and fracture type, HVOT was no longer significant (p=0.059), however Impaired HVOT and all other covariates are significant at p<0.001, R2=0.84. If Trails A is included in the model, all covariates are significant, and the model explains about 86% of the variance in FSST(s).
DISCUSSION
FSST in Hip Fracture Patients
This study aimed to determine if FSST could be performed by hip fracture patients. Average FSST performance time was 24 seconds, only 7 (25.93%) participants performed the FSST in <15s. FSST performance time was significantly correlated with cognitive and functional measures including HVOT, Trails A, total SPPB, and 50-ft gait speed but not with demographic variables such as age, education, number of comorbidities, or time from hospital admission. Of the 40 CAP-MP participants 32.5% did not attempt to perform the FSST. Performance on cognitive (HVOT, 3MS, Trails B) and functional (SPPB, and 50-ft gait speed) measures were associated with not having performed FSST. Older age was the only demographic covariate that was associated with not performing the FSST. When modeling for FSST performance, fracture side was shown to be a key variable in this population.
Hip fracture patients can attempt the FSST after standard care rehabilitation but will be unlikely to pass given standards derived from non-fracture community-dwelling older adults. Stroke patients have previously attempted a version with tape rather than canes, but clearing obstacles is important to fall prevention. As such, expanding the research for multiple falls risk indication FSST times in hip fracture may be better than altering the test format for this population.
The use of FSST has been assessed by several of the Neurology Section of the American Physical Therapy Association’s Task Forces: Stroke, multiple sclerosis, traumatic brain injury, spinal cord injury, Parkinson disease, vestibular disorders. However, hip fracture was not considered despite comparable rehabilitation needs and secondary falls risks. CAP-MP hip fracture patients were slower on average than other populations12–15,37 and the range of scores was wider than other populations. CAP-MP hip fracture patients who completed standard care rehabilitation therapy were most comparable to initial stroke patients.13 Compared to initial stroke patients (median 66 days, range 9–1094 days) where 14% could not be scored, 32.5% of CAP-MP patients were unable to be scored on the FSST at 16 weeks after hospital admission for hip fracture. Additionally, while 62% of stroke patients who performed the FSST failed, 74% of CAP-MP participants failed the FSST (>15s).13 These comparisons highlight the prevalent disability in hip fracture patients but suggest the FSST may still have sufficient range to discriminate those with lesser verses greater risk for repeat falls.
Hip Fracture Characteristics and FSST Performance
This study also aimed to assess characteristics of hip fracture for their impact on FSST performance. The only significant effect of fracture side was on FSST performance; all other characteristics and test outcomes are comparable by fracture side at baseline. However, to date, the impact of sidedness on FSST has not been reported in other conditions for which sidedness may be relevant for functional outcomes (i.e. joint replacement and stroke).13,38,39 The mechanism by which left fracture side is related to impaired FSST time is not yet clear. Pizac et al. (2020) recently showed significant differences in movement time (time from foot lift to touch down) and reaction speed between fractured and non-fractured limbs among hip fracture patients for lateral and forward movements.40 One hypothesis included that people with left-side fracture may be slower to initiate movement through the early quadrants. To achieve lateral movement in the clockwise direction and remain facing forward, weight would need to be held on the fractured (left) leg while stepping. It is possible that those with left side fractures were not making up for the initial delay in momentum in the clockwise rotation during the counterclockwise movement. The counter to this hypothesis is that the test includes a counter-direction that should equalize start to movement for left- and right-side fractures. Most biomechanical explanations for the discrepancy are confounded by this bidirectional movement inherent to the test.
Cognition and FSST
Finally, this study aimed to examine the impact of impaired cognition on FSST performance. HVOT and Trails A but not 3MSwere significantly associated with FSST time. This may be attributable to floor effects created by inclusion/exclusion criteria for the parent CAP study. The cognitive measures used were significantly inter-correlated and were significantly correlated with the physical function measures. In multivariable models, HVOT and Trails A remained significant when adjusting for fracture side. HVOT, Trails B, and 3MS have significant interactions with fracture side. Although all the models were significant, including multiple cognitive tests and interactions into the model did little to improve the R2 value. HVOT requires dynamic visual planning and orientation, these skills may be what translates to FSST performance as participants move in multiple directions. Participants who are less adept at using visual planning may struggle to adeptly move about the canes of the FSST, requiring more time with each direction change to feel safe in their movement. With this evidence HVOT is parsimonious assessment for predicting FSST performance. This evidence may change as more hip fracture patients at varying levels of cognitive impairment are included in study samples. Based on provided models HVOT performance, fracture side, and fracture type could act as predictors of FSST performance.
Three Way Interaction: HVOT, Fracture Side, Fracture Type
The observed 3-way interaction between HVOT, Fracture Side, and Fracture Type on FSST performance emphasized that unique characteristics of the hip fracture population are related to FSST performance. Right-side fractures (both femoral neck and pertrochanteric fractures) tended to be faster on FSST as HVOT performance improved, but the FSST performance time margin was small (10 seconds) compared to left-side fractures time margins as HVOT performance declines. Left-side fractures performing below 19 on HVOT had notably poorer FSST performance than other hip fracture patients. As left-side pertrochanteric fracture patients performed better on the HVOT, they looked more similar to left femoral neck fractures but were still taking twice as long to complete the FSST compared to right-side fractures.
Study Limitations
The study findings are limited by a small sample size, limited score range for 3MS due to inclusion criteria, and the study not assessing for variables such a leg dominance, fear of movement and falling, or pre-fracture physical ability to better interpret the findings. Among the small sample size of 40 only 27 patients provided FSST baseline data. This reduced the sample size and could increase chances that data were not missing at random, as supported by the significant differences in participant characteristics for the missing and non-missing (Table 2). Additional limitations include that 60% (n=12) of the impaired HVOT observations were censored from the analysis due to non-performance of FSST. Table 3 showed that 7 of 12 impaired HVOT participants did not complete the FSST, compared to 5 to 27 normal HVOT participants. The 3MS enrollment exclusion criteria (<73 excluded) which created a floor effect and may have impacted the impact of this measure in predicting FSST time. CAP was an efficacy study and is therefore less generalizable due to restrictions on sample entry. Information about leg dominance may have contributed to the understanding of the findings but was not available for this study. Fear of falling may have impacted FSST performance time and should be included in future work. Finally, this cross-sectional analysis does not allow for follow-up information on secondary falls using normative cut-points for FSST. However, CAP-MP is one of the first hip fracture studies to utilize the FSST, despite the importance of predicting falls in a hip fracture population. Additionally, this study is one of the only studies to emphasize sidedness as potentially impacting FSST outcomes.
Table 2.
Characteristics of those who did and did not perform the FSST
| No FSST N=13 |
Complete FSST N=27 |
t-test p-value |
|
|---|---|---|---|
| Mean (SD) | Mean (SD) | ||
| Demographics | |||
| Age | 80.84 (6.60) | 76.03 (6.78) | 0.041 |
| Education | 12.83 (3.01) | 12.70 (1.53) | 0.890 |
| BMI | 25.50 (4.57) | 26.10 (3.45) | 0.679 |
| Comorbid Conditions | 6.46 (2.66) | 5.92 (2.96) | 0.584 |
| Admission to Randomization (weeks) | 17.74 (4.66) | 16.58 (5.76) | 0.532 |
| Cognitive Tests | |||
| HVOT | 16.29 (4.91) | 22.35 (3.94) | <0.001 |
| 3MS | 88.07 (5.76) | 93.85 (5.30) | 0.003 |
| Trails A | 98.25 (74.91) | 51.59 (17.65) | 0.056 |
| Trails B | 238.90 (79.96) | 154.10 (80.41) | 0.012 |
| Physical Function Tests | |||
| SPPB | 4.33 (1.43) | 6.6 (2.06) | 0.002 |
| 50ft gait speed (m/s) | 0.53 (0.20) | 0.71 (0.16) | 0.005 |
| N (Col %) | N (Col %) | χ2 p-value | |
| Sex (Female) | 9 (69.23) | 18 (67.50) | 0.871 |
| Fracture Side (Right) | 12 (57.14) | 15 (78.95) | 0.186 |
| Education (High school or less) | 7 (58.00) | 18 (66.67) | 0.723 |
| Comorbid Conditions (5–9) | 8 (61.54) | 15 (55.56) | 0.070 |
| SPPB (<6) | 19 (86.36) | 8 (44.44) | 0.007 |
| HVOT (≤ 19) | 5 (41.67) | 22 (56.41) | 0.013 |
| Trails A (≤ 78) | 3 (37.50) | 24 (75.00) | 0.086 |
| Trails B (>273) | 5 (41.67) | 22 (78.57) | 0.022 |
| Fracture Type (Femoral neck) | 6 (30) | 14 (70) | 0.404 |
Note: This table uses weeks to randomization and not to FSST because no FSST data means there is no end time to calculate from. BMI= Body Mass Index, HVOT= Hooper Visual Organization Task, 3MS= Modified Mini-Mental State Examination, SPPB= Short Physical Performance Battery
CONCLUSIONS
Many hip fracture patients cannot perform the FSST even after completing the full course of standard rehabilitation therapy, and of those who can, few successfully complete the measure compared to community-dwelling non-fracture older adults. The interesting differences seen by fracture side and fracture type, a finding that appears unique to hip fracture populations, may indicate a new target area for rehabilitation, or may be an indicator that FSST is not an appropriate test for hip fracture patients. Another possible implication of these findings is that balance still remains very impaired (and subsequent fall risk very high) after usual rehabilitation, and may be a target for additional goals in rehabilitation after hip fracture before discharge to the community.
Foremost from this research come questions about side of test initiation among hip fracture patients. Without more information about how side of fracture affected step initiation, it is difficult to make more interpretations of these results. Research will also need to be done on longitudinal data in hip fracture patients to validate the 15s cut point for falls risk, and potentially rehabilitation outcomes. Additional work should attempt to predict FSST performance for unscored patients using machine learning and the recommended models. Finally, future research will assess some of the proposed mechanisms for the effect of fracture side; including beginning the FSST in reverse order, or potentially infra-red mapping movement during FSST to isolate the source of lag.
This study was among the first known to assess FSST in hip fracture patients despite the ease of administration and importance of the fall risk prediction especially to a population hindered by a fear of falling. This has also been one of the few studies to use the HVOT, which turned out to provide unique cognitive data. We anticipate the FSST may be a valuable tool for use in standard care rehabilitation as a continuous metric of patient performance, goal setting, and recovery. Predicting secondary falls is an important future use of FSST in hip fracture patients and should considered in future research.
Acknowledgements for CAP-MP study
Assistance was provided by the Baltimore Geriatric Research, Education and Clinical Center (GRECC) of the Veterans Affairs Maryland Health Care System (VAMCS). Special thanks to Justine Golden from the University of Maryland School of Medicine for their efforts in assisting with data collection and management.
Conflicts of Interest and Sources of Funding:
This work was supported by grants from the National Institute on Aging (NIA) and the National Institute of Child Health and Human Development at the National Institutes of Health (NIH) [R21 HD043269, R01 AG029315, R37 AG09901, T32 AG00262, and P30 AG028747]. Heather Mutchie reports grants from the NIH during the conduct of the study; Dr. Magaziner reports grants from NIA, during the conduct of the study; personal fees from Novartis, Pluristem, Viking, UCB, and American Orthopedic Association Own the Bone Multi-Disciplinary Advisory Board; other support from Fragility Fracture Network outside of the submitted work. Dr. Gruber Baldini reports grants from NIH, during the conduct of the study; grants from the Gilead Foundation, and grants from the NIH outside of the submitted work. For the other authors, none were declared.
Footnotes
ClinicalTrials.gov Registration Number: NCT01783704
Previous Presentation: Parts of this work were presented as a poster at the Gerontological Society of American Annual Scientific Meeting in 2018.
REFERENCES
- 1.CDC Injury Center. Hip fractures among older adults | Home and recreational safety. https://www.cdc.gov/homeandrecreationalsafety/falls/adulthipfx.html Accessed April 22, 2019.
- 2.Stevens JA, Olson S. Reducing falls and resulting hip fractures among older women. https://www.cdc.gov/mmwr/preview/mmwrhtml/rr4902a2.htm Accessed September 5, 2019. [DOI] [PubMed]
- 3.Gruber-Baldini AL, Zimmerman S, Morrison RS, et al. Cognitive impairment in hip fracture patients: timing of detection and longitudinal follow-up. J Am Geriatr Soc. 2003;51(9):1227–1236. [DOI] [PubMed] [Google Scholar]
- 4.Gruber-Baldini A, Hosseini M, Orwig D, et al. Cognitive differences between men and women who fracture their hip and impact on six-month survival. J Am Geriatr Soc. 2017;65(3):e64–e69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Seshadri S, Wolf PA, Beiser A, et al. Lifetime risk of dementia and Alzheimer’s disease. Neurology. 1997;49(6):1498. [DOI] [PubMed] [Google Scholar]
- 6.Friedman SM, Menzies IB, Bukata SV, Mendelson DA, Kates SL. Dementia and hip fractures: development of a pathogenic framework for understanding and studying risk. Geriatr Orthop Surg Rehabil. 2010;1(2):52–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fischer BL, Gleason CE, Gangnon RE, Janczewski J, Shea T, Mahoney JE. Declining cognition and falls: role of risky performance of everyday mobility activities. Phys Ther. 2014;94(3):355–362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dite W, Temple VA. A clinical test of stepping and change of direction to identify multiple falling older adults. Arch Phys Med Rehabil. 2002;83(11):1566–1571. [DOI] [PubMed] [Google Scholar]
- 9.Guyatt GH, Sullivan MJ, Thompson PJ, et al. The 6-minute walk: a new measure of exercise capacity in patients with chronic heart failure. Can Med Assoc J. 1985;132(8):919–923. [PMC free article] [PubMed] [Google Scholar]
- 10.Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39(2):142–148. [DOI] [PubMed] [Google Scholar]
- 11.Hill KD, Bernhardt J, McGann AM, Maltese D, Berkovits D. A new test of dynamic standing balance for stroke patients: reliability, validity and comparison with healthy elderly. Physiother Can. Published online April 8, 2009. [Google Scholar]
- 12.Duncan RP, Earhart GM. Four square step test performance in people with Parkinson disease. J Neurol Phys Ther JNPT. 2013;37(1):2–8. [DOI] [PubMed] [Google Scholar]
- 13.Blennerhassett JM, Jayalath VM. The Four Square Step Test is a feasible and valid clinical test of dynamic standing balance for use in ambulant people poststroke. Arch Phys Med Rehabil. 2008;89(11):2156–2161. [DOI] [PubMed] [Google Scholar]
- 14.Whitney SL, Marchetti GF, Morris LO, Sparto PJ. The reliability and validity of the Four Square Step Test for people with balance deficits secondary to a vestibular disorder. Arch Phys Med Rehabil. 2007;88(1):99–104. [DOI] [PubMed] [Google Scholar]
- 15.Dite W, Connor HJ, Curtis HC. Clinical identification of multiple fall risk early after unilateral transtibial amputation. Arch Phys Med Rehabil. 2007;88(1):109–114. [DOI] [PubMed] [Google Scholar]
- 16.Orwig D, Mangione K, Baumgarten M, et al. Improving community ambulation after hip fracture: protocol for a randomised, controlled trial. J Physiother. 2017;63(1):45–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Magaziner J, Mangione KK, Orwig D, et al. Effect of a multicomponent home-based physical therapy intervention on ambulation after hip fracture in older adults. JAMA. 2019;322(10):946–956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–198. [DOI] [PubMed] [Google Scholar]
- 19.Guralnik JM, Simonsick EM, Ferrucci L, et al. A Short Physical Performance Battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49(2):M85–M94. [DOI] [PubMed] [Google Scholar]
- 20.Hooper HE The Hooper Visual Organization Test (VOT) manual. Published online 1958.
- 21.Battery AIT. Manual of Directions and Scoring. Washington, DC: War Department, Adjutant General’s Office; 1944. [Google Scholar]
- 22.Bornstein RA. Normative data on selected neuropsychological measures from a nonclinical sample. J Clin Psychol. 1985;41(5):651–659. [Google Scholar]
- 23.Reuben DB, Siu AL. An objective measure of physical function of elderly outpatients. The Physical Performance Test. J Am Geriatr Soc. 1990;38(10):1105–1112. [DOI] [PubMed] [Google Scholar]
- 24.Grace J, Nadler JD, White DA, et al. Folstein vs Modified Mini-Mental State Examination in geriatric stroke: stability, validity, and screening utility. Arch Neurol. 1995;52(5):477–484. [DOI] [PubMed] [Google Scholar]
- 25.Salthouse TA. What cognitive abilities are involved in trail-making performance? Intelligence. 2011;39(4):222–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jones TG, Schinka JA, Vanderploeg RD, Small BJ, Graves AB, Mortimer JA. 3MS normative data for the elderly. Arch Clin Neuropsychol. 2002;17(Journal Article):171–177. [PubMed] [Google Scholar]
- 27.Weeks DL, Ambrose SB, Tindall AG. The utility of the Modified Mini-Mental State Examination in inpatient rehabilitation for traumatic brain injury: preliminary findings. Brain Inj. 2020;34(7):881–888. [DOI] [PubMed] [Google Scholar]
- 28.Lopez MN, Lazar MD, Oh S. Psychometric properties of the Hooper Visual Organization Test. Assessment. 2003;10(1):66–70. [DOI] [PubMed] [Google Scholar]
- 29.Nadler JD, Grace J, White DA, Butters MA, Malloy PF. Laterality differences in quantitative and qualitative hooper performance. Arch Clin Neuropsychol. 1996;11(3):223–229. [PubMed] [Google Scholar]
- 30.Ashendorf L, Jefferson AL, O’Connor MK, Chaisson C, Green RC, Stern RA. Trail Making Test errors in normal aging, mild cognitive impairment, and dementia. Arch Clin Neuropsychol Off J Natl Acad Neuropsychol. 2008;23(2):129–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wagner S, Helmreich I, Dahmen N, Lieb K, Tadić A. Reliability of three alternate forms of the Trail Making Tests A and B. Arch Clin Neuropsychol. 2011;26(4):314–321. [DOI] [PubMed] [Google Scholar]
- 32.Sánchez-Cubillo I, Periáñez JA, Adrover-Roig D, et al. Construct validity of the Trail Making Test: role of task-switching, working memory, inhibition/interference control, and visuomotor abilities. J Int Neuropsychol Soc. 2009;15(3):438–450. [DOI] [PubMed] [Google Scholar]
- 33.Pavasini R, Guralnik J, Brown JC, et al. Short Physical Performance Battery and all-cause mortality: systematic review and meta-analysis. BMC Med. 2016;14(1):215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mangione KK, Craik RL, McCormick AA, et al. Detectable changes in physical performance measures in elderly African Americans. Phys Ther. 2010;90(6):921–927. [DOI] [PubMed] [Google Scholar]
- 35.Unver B, Kalkan S, Yuksel E, Kahraman T, Karatosun V. Reliability of the 50-foot walk test and 30-sec chair stand test in total knee arthroplasty. Acta Ortop Bras. 2015;23(4):184–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kim H, Park I, Lee H, Lee O. The reliability and validity of gait speed with different walking pace and distances against general health, physical function, and chronic disease in aged adults. J Exerc Nutr Biochem. 2016;20:46–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shirley Ryan AbilityLab. Four Step Square Test. https://www.sralab.org/rehabilitation-measures/four-step-square-test Accessed February 27, 2020.
- 38.Belgen B, Beninato M, Sullivan PE, Narielwalla K. The association of balance capacity and falls self-efficacy with history of falling in community-dwelling people with chronic stroke. Arch Phys Med Rehabil. 2006;87(4):554–561. [DOI] [PubMed] [Google Scholar]
- 39.Roos MA, Reisman DS, Hicks G, Rose W, Rudolph KS. Development of the Modified Four Square Step Test and its reliability and validity in people with stroke. J Rehabil Res Dev. 2016;53(3):403–412. [DOI] [PubMed] [Google Scholar]
- 40.Pizac D, Savin D, Orwig D, et al. Neurocognitive measures predict voluntary stepping performance in older adults post-hip fracture. Clin Biomech Bristol Avon. Published online November 12, 2020:105234–105234. [DOI] [PMC free article] [PubMed] [Google Scholar]


