Abstract
In addition to respiratory complications produced by SARS‐CoV‐2, accumulating evidence suggests that some neurological symptoms are associated with the disease caused by this coronavirus. In this study, we investigated the effects of the SARS‐CoV‐2 spike protein S1 stimulation on neuroinflammation in BV-2 microglia. Analyses of culture supernatants revealed an increase in the production of TNF-α, IL-6, IL-1β and iNOS/NO. S1 also increased protein levels of phospho-p65 and phospho-IκBα, as well as enhanced DNA binding and transcriptional activity of NF-κB. These effects of the protein were blocked in the presence of BAY11-7082 (1 µM). Exposure of S1 to BV-2 microglia also increased the protein levels of NLRP3 inflammasome and enhanced caspase-1 activity. Increased protein levels of p38 MAPK was observed in BV-2 microglia stimulated with the spike protein S1 (100 ng/ml), an action that was reduced in the presence of SKF 86,002 (1 µM). Results of immunofluorescence microscopy showed an increase in TLR4 protein expression in S1-stimulated BV-2 microglia. Furthermore, pharmacological inhibition with TAK 242 (1 µM) and transfection with TLR4 small interfering RNA resulted in significant reduction in TNF-α and IL-6 production in S1-stimulated BV-2 microglia. These results have provided the first evidence demonstrating S1-induced neuroinflammation in BV-2 microglia. We propose that induction of neuroinflammation by this protein in the microglia is mediated through activation of NF-κB and p38 MAPK, possibly as a result of TLR4 activation. These results contribute to our understanding of some of the mechanisms involved in CNS pathologies of SARS-CoV-2.
Supplementary Information
The online version contains supplementary material available at 10.1007/s12035-021-02593-6.
Keywords: SARS-CoV-2 spike protein S1, Neuroinflammation, Microglia, NF-κB, TLR4
Introduction
The emergence of the severe acute respiratory syndrome coronavirus‐2 (SARS-CoV‐2) in 2019 has resulted in a global pandemic affecting most countries and territories. To date, there are 234,809,103 confirmed cases and 4,800,375 deaths [1]. The most common complications of illness due to SARS‐CoV‐2 infection are mainly related to respiratory symptoms [2–4]. SARS‐CoV‐2 infection causes significant damage to the alveolus, interstitial and intra-alveolar oedema and infiltration of inflammatory cells (mainly macrophages) [5].
In addition to respiratory complications of SARS-CoV-2 illness, accumulating pieces of evidence suggest that neurological symptoms are associated with COVID-19, the disease caused by the novel coronavirus [6]. These symptoms include headaches, loss of smell, confusion and strokes [7]. Furthermore, a retrospective study in China reported neurological symptoms such as cerebrovascular diseases, consciousness impairment and skeletal muscle symptoms [8]. Interestingly, the SARS-CoV-2 sub-unit S1 has been shown in a study to promote loss of barrier integrity and trigger a pro-inflammatory response in a 3D model of the human blood–brain barrier [9], suggesting a possible mechanism for the neurological symptoms induced by the coronavirus. Other studies have proposed mechanisms of SARS-CoV-2–mediated CNS dysfunction [10, 11]. Further understanding of the cellular mechanisms involved in neurological consequences of SARS-CoV-2 infection is critical for identifying pharmacological strategies for prevention and treatment.
Microglia are brain-resident macrophages that regulate brain development, maintenance of neuronal networks and injury repair [12]. In the resting state, microglia survey their surrounding microenvironment through the projection and retraction of their highly motile processes [13]. However, in the presence of injury or pathology within the CNS, they become activated [14]. During neuroinflammation, polarised M1 microglia produce pro-inflammatory cytokines and neurotoxic molecules, such as tumour necrosis factor (TNF)-α, interleukin (IL)-6, IL-1β, nitric oxide (NO) and reactive oxygen species (ROS), which contribute to neuronal dysfunction, while polarised M2 microglia secrete anti-inflammatory mediators such as IL-10 and transforming growth factor (TGF)-β, which are involved in restoring homeostasis [15–18]. Microglia-mediated neuroinflammation therefore plays significant roles in many neurological [19–23] and neuropsychiatric [24–27] disorders. Based on evidence linking SARS-CoV-2 infection with neurological symptoms, we carried out investigations to determine the effects of a recombinant SARS-CoV-2 spike protein S1 sub-unit on the release of pro-inflammatory mediators in BV-2 microglia.
Materials and Methods
Materials
Recombinant human coronavirus SARS-CoV-2 spike protein S1 (Accession MN908947) was purchased from Abcam. The protein was suspended in sterile water for functional studies. The following drugs were used: BAY11-7082 (Sigma), CRID3 sodium salt (Tocris), SKF 86,002 dihydrochloride (Tocris) and TAK 242 (Tocris).
Cell Culture
BV-2 mouse microglial cell line (ICLCATL03001) was purchased from Interlab Cell Line Collection (Banca Biologica e Cell Factory, Italy) and cultured in RPMI medium supplemented with 10% foetal bovine serum.
Determination of Cytokine Production
Initial pilot experiments were conducted to evaluate effects of 10 ng/ml, 50 ng/ml, 100 ng/ml, 500 ng/ml and 1000 ng/ml of S1 on TNF-α production in BV-2 microglia seeded out in 24-well plates at 5 × 104 cells/ml. These concentrations of the protein were used to stimulate the cells for 1 h, 3 h, 6 h, 12 h and 24 h. Levels of TNF-α in culture supernatants were then determined using mouse instant ELISA™ kit (Thermo Scientific).
Subsequent experiments employed 10 ng/ml, 50 ng/ml and 100 ng/ml of S1 in determining effects on TNF-α, IL-6 and IL-1β. In this case, cultured BV-2 microglia were seeded out in a 24-well plate at 5 × 104 cells/ml and treated with protein S1 (10 ng/ml, 50 ng/ml and 100 ng/ml) for 24 h. Thereafter, medium was collected and centrifuged to obtain culture supernatants. Levels of TNF-α were determined as described above, while levels of IL-6 in supernatants were determined using IL-6 mouse ELISA kit (Thermo Scientific). Similarly, levels of IL-1β were evaluated using IL-1β mouse ELISA kit (Thermo Scientific).
Measurement of NO Production
The Griess reagent (Promega) was used to determine the levels of NO in supernatants of cultured BV-2 microglia treated with protein S1 (10 ng/ml, 50 ng/ml and 100 ng/ml) for 24 h. Following treatment with S1, Griess assay (which measures nitrite, a stable breakdown product of NO) was carried out by adding 50 µL of sulphanilamide to 50 µL of culture supernatants, followed by incubation in the dark at room temperature for 10 min. Thereafter, 50 µl of N-(1-naphthyl)ethylenediamine dihydrochloride (NED) was added and the mixture incubated for a further 10-min period. Absorbance was measured at 540 nm using a Tecan Infinite M microplate reader. Nitrite concentrations were determined from a nitrite standard reference curve.
In-Cell Western/Cytoblot
The In-Cell Western assay is a proven method for the rapid quantification of proteins in cells [28, 29]. BV-2 microglia were seeded into a 96-well plate at 5 × 104 cells/ml, and cells treated at 70% confluence. At the end of each experiment, cells were fixed with 8% formaldehyde solution (100 µL) for 15 min, followed by washing with PBS. The cells were then incubated with primary antibodies overnight at 4 °C. The following antibodies were used: rabbit anti-iNOS (Abcam), rabbit anti-phospho-p65 (Cell Signalling Technology), rabbit anti-phospho-IκBα (Santa Cruz Biotechnology), rabbit anti-NLRP3 (Abcam) and rabbit anti-phospho-p38 (Cell Signalling Technology) antibodies. Thereafter, cells were washed with PBS and incubated with anti-rabbit HRP secondary antibody for 2 h at room temperature. Then, 100 µl of HRP substrate was added to each well and absorbance measured at 450 nm with a Tecan Infinite M microplate reader. Readings were normalised with Janus Green normalisation stain (Abcam).
NF-κB Luciferase Reporter Gene Assay
BV-2 cells were seeded in a 24-well plate at a density of 4 × 104 cells/ml. At 60% confluence, RPMI medium was replaced with Opti-MEM, with a further incubation period of 2 h at 37 °C. Transfection of BV-2 cells was performed by preparing a Glial-Mag transfection reagent (OZ Biosciences) and Cignal NF-κB luciferase reporter (Qiagen) complex at a ratio of 3:1 in 50 µL Opti-MEM. The complex was added to BV-2 cells, and the plate placed on a magnetic plate (OZ Biosciences) and incubated at 37 °C for 30 min, followed by a further magnetic plate-free incubation period of 2 h.
Thereafter, the medium was changed to serum-free RPMI and cells were treated with spike S1 (10 ng/ml, 50 ng/ml and 100 ng/ml) for 6 h. This was followed by a Dual-Glo® reporter assay (Promega). Firefly and Renilla luminescence were measured using a FLUOstar OPTIMA microplate reader (BMG Labtech).
NF-κB Transcription Factor Binding Assay
The NF-κB p65 transcription factor assay is a non-radioactive ELISA-based assay for evaluating DNA binding activity of NF-κB in nuclear extracts. BV-2 microglia were seeded in a 6-well plate at a density of 4 × 104 cells/ml. The cells were then incubated with 10 ng/ml, 50 ng/ml and 100 ng/ml of S1 for 60 min. At the end of the incubation, nuclear extracts were prepared from the cells and subjected to NF-κB transcription factor binding assay according to the instructions of the manufacturer (Abcam).
Caspase-Glo® 1 Inflammasome Assay
The Caspase-Glo® 1 Inflammasome Assay (Promega) was used to measure the activity of caspase-1 directly in live cells or culture supernatants [30]. BV-2 microglia were seeded out in a 24-well plate at a density of 4 × 104 cells/ml and stimulated with S1 (10 ng/ml, 50 ng/ml and 10 ng/ml) for 24 h. After incubation, cell culture supernatants were collected and mixed with an equal volume of Caspase-Glo® 1 reagent or Caspase-Glo® 1 reagent + YVAD-CHO (1 µM) in a 96-well plate. The contents of the wells were mixed using a plate shaker at 400 rpm for 30 s. The plate was then incubated at room temperature for 60 min, followed by luminescent measurement of caspase-1 activity with a FLUOstar OPTIMA reader (BMG Labtech).
Effects of BAY11-7082, CRID3 and SKF 86002 on S1-Induced Neuroinflammation
BAY11-7082 is an anti-inflammatory small molecule inhibitor of NF-κB, which has also been proposed as a potential disease-modifying strategy to combat the severity of COVID-19 [31]. CRID3 is an NLRP3 inflammasome inhibitor, which has been shown to reduce IL-1β production in vivo and attenuate the severity of experimental autoimmune encephalomyelitis [32]. SKF 86,002 is a bicyclic pyridinylimidazole which has been widely reported to inhibit cytokine production by targeting p38 MAPK [33].
Consequently, the effects of these inhibitors on the release of TNF-α, IL-6 and IL-1β were investigated by pre-treating BV-2 microglia with BAY11-7082 (1 µM), CRID3 (1 µM) and SKF 86,002 (1 µM) 60 min prior to stimulation with S1 (100 ng/ml) for a further 24-h period. Culture supernatants were collected and analysed for levels of TNF-α, IL-6 and IL-1β using mouse ELISA kits (Thermo Scientific).
Immunofluorescence Microscopy
Immunofluorescence microscopy was carried out by seeding out BV-2 microglia in a 24-well cell imaging plate (Eppendorf) at a density of 5 × 104 cells/ml. Thereafter, cells were stimulated with S1 (100 ng/ml) for 24 h. After stimulation, cells were washed with PBS and fixed with 500 µl formaldehyde (4%) for 15 min at room temperature. This was followed by PBS washing and blocking with 500 µl of 5% bovine serum albumin for 60 min at room temperature. Cells were then incubated overnight at 4 °C with either Iba-1 Alexa Fluor® 488 antibody (Santa Cruz Biotechnology; 1:500) or Toll-like receptor 4 (TLR4) antibody (Santa Cruz Biotechnology; 1:500). In experiments employing unconjugated primary antibody, cells were washed with PBS and further incubated in the dark for 2 h with Alexa Fluor® 488–conjugated donkey anti-rabbit IgG secondary antibody (Thermo Scientific; 1:500). Then, cells were stained with 50 nM of 4′,6-diamidino-2-phenylindole dihydrochloride (DAPI; Invitrogen) for 3 min and washed. Images were captured using EVOS FLoid® cell imaging station (Invitrogen).
Effects of TAK 242 on Spike Protein S1–Induced Increased Production of Pro-inflammatory Mediators
TAK 242 is a small molecule inhibitor of inflammation which has been reported to reduce nitric oxide and cytokine production in LPS-stimulated mouse macrophages and in a mouse model [34]. The anti-inflammatory activity of TAK 242 has been confirmed to be mediated through inhibition of TLR4 signalling [35]. The effects of TAK 242 were therefore investigated on S1-induced increased production of TNF-α, IL-6 and IL-1β. BV-2 microglia were pre-treated with TAK 242 (1 µM). After 60 min, cells were stimulated with S1 (100 ng/ml) for a further 24-h period. Levels of TNF-α and IL-6 in culture supernatants were measured using mouse ELISA kits (Thermo Scientific).
Small Interfering RNA–Mediated Knockdown of TLR4
In order to further confirm the possible roles of TLR4 in S1-induced increased production of pro-inflammatory mediators, experiments were carried out to knockdown TLR4 in BV-2 microglia. BV-2 cells were seeded out into 6-well plates at a concentration of 4 × 104 cells/ml and cultured until 60% confluence was achieved. Thereafter, the culture medium in each well was changed to Opti-MEM (1000 µl) followed by incubation for 2 h at 37 °C. Complexes containing 1.8 µl of the Glial-Mag transfection reagent (OZ Biosciences) and 2 µl of TLR4 or control small interfering RNA (siRNA) (Santa Cruz Biotechnology) were then added to the cells. The culture plate was placed on a magnetic plate (OZ Biosciences) for 30 min, followed by incubation at 37 °C for a further 24-h period. Following successful transfection, the effects of loss of function of TLR4 were evaluated by stimulating the cells with SARS-CoV-2 spike protein S1 (100 ng/ml) for 24 h. Culture supernatants were collected and analysed for levels of TNF-α and IL-6 using mouse ELISA kits.
Statistical Analyses
Data are expressed as mean ± SEM for at least three independent experiments (n = 3) and analysed using one-way analysis of variance (ANOVA) with post hoc Tukey’s test (for multiple comparisons). Statistical analysis was conducted using GraphPad Prism software (version 9).
Results
Effects of S1 on Pro-inflammatory Cytokine Release in BV-2 Microglia
Results of pilot experiments to determine effects of stimulation with 10 ng/ml, 50 ng/ml, 100 ng/ml, 500 ng/ml and 1000 ng/ml of S1 on the production of TNF-α in BV-2 microglia at 1 h, 3 h, 6 h, 12 h and 24 h are shown in the Supplementary Data. Stimulation with all concentrations of the spike protein resulted in a steady increase in the production of TNF-α from 1 h post-stimulation, with the maximum release observed 24 h post-stimulation.
Furthermore, there was a concentration-dependent increase in S1-induced increase in TNF-α production, which reached a maximum at 100 ng/ml at 3 h, 6 h, 12 h and 24 h post-stimulation. When compared with effects of 100 ng/ml of S1, there were no further significant increases in TNF-α production when the concentration of S1 was increased to 500 ng/ml and 1000 ng/ml.
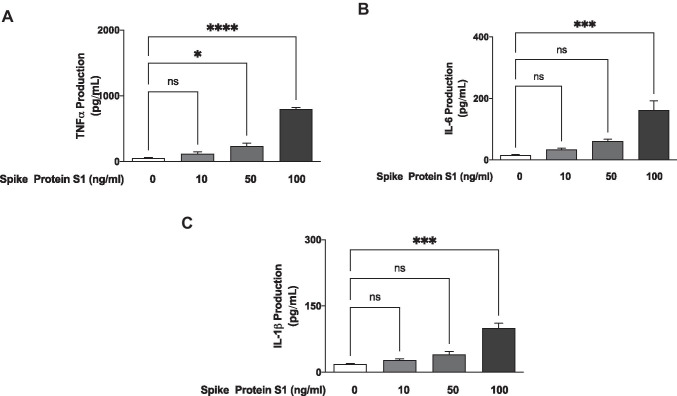
Consequently, in subsequent confirmatory experiments, 10 ng/ml, 50 ng/ml and 100 ng/ml of S1 were then incubated with BV-2 cells for 24 h. Results show that with 10 ng/ml of S1, there was an insignificant (p < 0.05) elevation in the secretion of TNF-α. However, on increasing the concentration to 50 ng/ml, a significant (p < 0.05) increase in the production of TNF-α was observed (Fig. 1A). On increasing the concentration of the protein to 100 ng/ml, there was a ~ 15-fold increase in the levels of TNF-α in culture supernatants (Fig. 1A).
Fig. 1.
S1 increased levels of TNF-α (A), IL-6 (B) and IL-1β (C) in BV-2 microglia after a 24-h incubation. All values are expressed as mean ± SEM for three independent experiments. Data were analysed using one-way ANOVA followed by a post hoc Tukey’s multiple comparison test. *p < 0.05, ***p < 0.001, ****p < 0.0001, ns (not significant at p < 0.05), compared with untreated control
S1 Induced an Increase in IL-6 and IL-1β Production
Results in Fig. 1B show that the release of IL-6 was not significantly elevated in BV-2 microglia treated with 10 ng/ml and 50 ng/ml of S1, in comparison with untreated (control) cells. However, incubation of the cells with 100 ng/ml of S1 resulted in a ~ 10.2-fold and significant (p < 0.001) increase in the secretion of IL-6 into culture medium. Similar observations were made in experiments to determine the effects of S1 sub-unit on IL-1β production; at 10 ng/ml and 50 ng/ml of S1, there was no significant effect on the release of IL-1β. A ~ 5.5-fold elevation of IL-1β levels was, however, observed with 100 ng/ml of S1 (Fig. 1C).
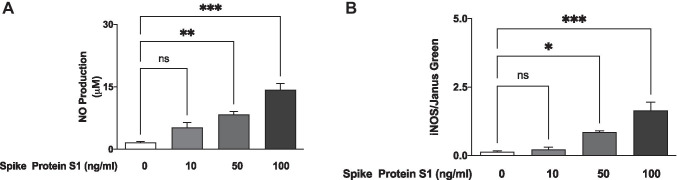
S1 Induced an Increase in NO Production and iNOS Protein Expression in BV-2 Microglia
Analyses of culture supernatants obtained from BV-2 microglia incubated with S1 (10 ng/ml) showed an insignificant (p < 0.05) increase in the levels of NO, when compared with untreated (control) cells. We further showed that incubation with 50 ng/ml and 100 ng/ml of S1 caused a ~ 5.1 and 8.7 increase in NO production, respectively (p < 0.01) (Fig. 2A).
Fig. 2.
S1 increased levels of NO (A) and iNOS protein (B) in BV-2 microglia after a 24-h incubation. NO levels in culture supernatants were measured using the Griess assay, while In-Cell Western (cytoblot) assay was used to detect iNOS protein expression. All values are expressed as mean ± SEM for three independent experiments. Data were analysed using one-way ANOVA followed by a post hoc Tukey’s multiple comparison test. *p < 0.05, **p < 0.01, ***p < 0.001, ns (not significant at p < 0.05), compared with untreated control
We also used In-Cell Western analyses to further demonstrate that incubation with S1 (50 ng/ml and 100 ng/ml) resulted in a significant (p < 0.05) increase in protein levels of iNOS, in comparison with unstimulated cells (Fig. 2B).
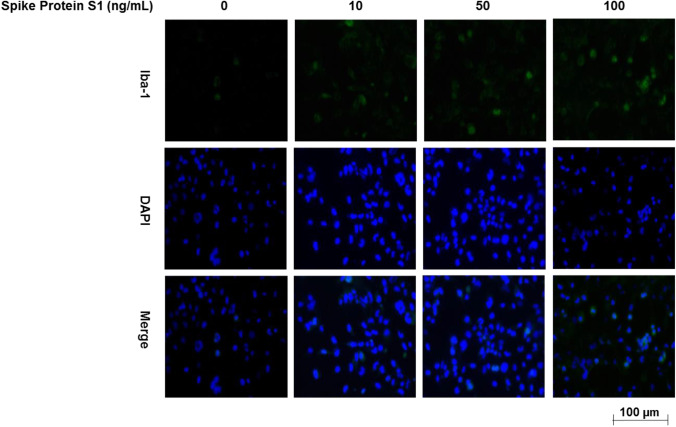
S1 Increased Iba-1 Expression in BV-2 Microglia
Immunofluorescence microscopy revealed that unstimulated BV-2 microglia express low levels of Iba-1 protein. However, on activation with S1 (10-100 ng/ml), there were marked increases in the expression of Iba-1 (Fig. 3).
Fig. 3.
Immunofluorescence microscopy showing an increase in Iba-1 protein expression in BV-2 microglia incubated with 10 ng/ml, 50 ng/ml and 100 ng/ml of S1
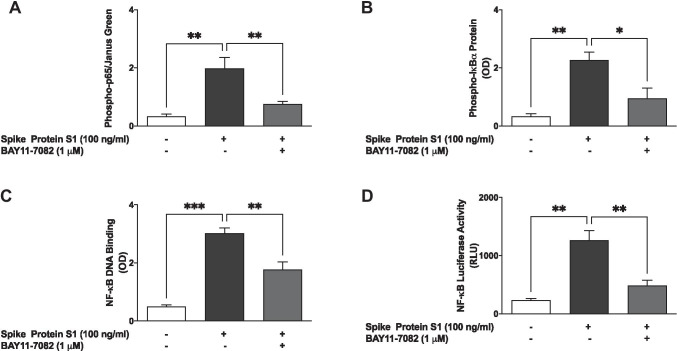
Spike Protein S1 Activated NF-κB in BV-2 Microglia
Following our observation that S1 induced a significant increase in the production of pro-inflammatory mediators at 100 ng/ml, we were next interested in evaluating the role of NF-κB in its activity at this concentration. Firstly, we used In-Cell Western assays to investigate effects of the protein on the cytoplasmic activation of p65 and IκBα. Results show that S1 (100 ng/ml) significantly (p < 0.01) increased protein levels of both phospho-p65 and phospho-IκBα following incubation with BV-2 microglia for 15 min (Fig. 4A, B). These results also show that protein levels of phospho-p65 and phospho-IκBα were reduced in the presence of the NF-κB inhibitor BAY11-7082 (1 µM).
Fig. 4.
S1 activated NF-κB signalling in BV-2 microglia. Nuclear extracts were collected from cells stimulated with S1 (100 ng/ml) in the absence or presence of BAY11-7082 (1 µM) for 60 min and subjected to DNA binding assays (A). Results of luciferase reporter gene assay showing increased NF-κB transcriptional activity by S1 and its inhibition by BAY11-7082 (1 µM) (B). In-Cell Western (cytoblot) analyses showing increased protein expressions of phospho-p65 sub-unit (C) and phospho-IκBα (D) following stimulation with S1 (100 ng/ml) for 15 min and inhibition by BAY11-7082 (1 µM). Data were analysed using one-way ANOVA followed by a post hoc Tukey’s multiple comparison test. *p < 0.05, **p < 0.01, ***p < 0.001, ns (not significant at p < 0.05), compared with untreated control or S1 stimulation alone
Results of an NF-κB p65 transcription factor assay revealed that following the treatment of BV-2 microglia with S1 (100 ng/ml) for 60 min, there was a significant (p < 0.001) increase in the binding of NF-κB in nuclear extracts to consensus binding sites in the DNA. Interestingly, pre-treatment of BV-2 cells with BAY11-7082 (1 µM) prior to stimulation with S1 produced an inhibition in binding to a double-stranded DNA sequence containing the NF-κB response element (Fig. 4C). Luciferase reporter gene assays to evaluate the effects of S1 on transcriptional activity showed that S1 stimulation of BV-2 microglia that were transfected with NF-κB plasmid vector resulted in a significant (p < 0.01) increase in luciferase activity, in comparison with untreated transfected cells. We further showed that on pre-treating the cells with BAY11-7082 (1 µM), an S1-induced increase in NF-κB luciferase activity was markedly reduced (Fig. 4D).
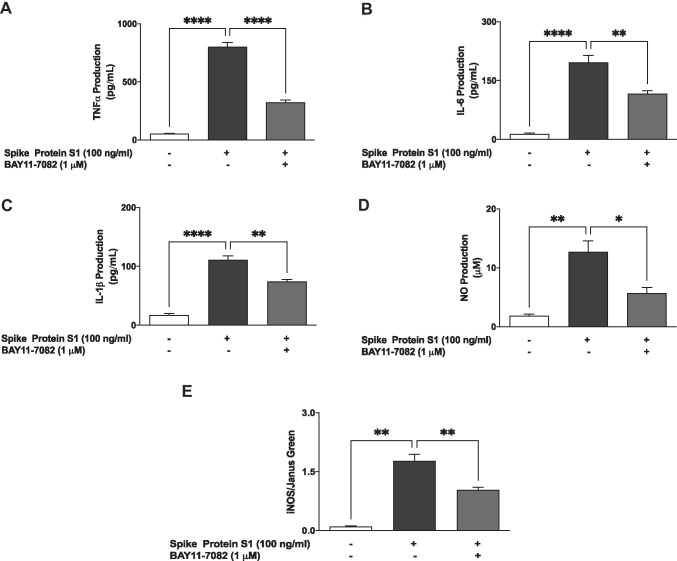
Pre-treatment with BAY11-7082 Reduced S1-Induced Production of Pro-inflammatory Mediators
In order to further confirm the roles of NF-κB in S1-induced neuroinflammation, BV-2 microglia were pre-treated with BAY11-7082 prior to stimulation with the protein for 24 h, followed by measurements of the release of pro-inflammatory cytokines (TNF-α, IL-6 and IL-1β) in culture supernatants. In the presence of BAY11-7082 (1 µM), S1-induced increases in TNF-α, IL-6 and IL-1β production in BV-2 microglia were reduced by ~ 59.6%, ~ 40.6% and ~ 32.8%, respectively (Fig. 5A–C).
Fig. 5.
Pre-treatment with BAY11-7082 (1 µM) resulted in inhibition of S1-induced increased production of TNF-α (A), IL-6 (B) and IL-1β (C) in BV-2 microglia. Culture supernatants were analysed using ELISA following stimulation for 24 h. Data were analysed using one-way ANOVA followed by a post hoc Tukey’s multiple comparison test. **p < 0.01, ****p < 0.0001, compared with untreated control or S1 stimulation alone. Pre-treatment with BAY11-7082 (1 µM) resulted in inhibition of S1-induced increased production of NO (D) and iNOS protein (E) in BV-2 microglia, following stimulation for 24 h. Culture supernatants were analysed using Griess assay, and In-Cell Western (cytoblot) was used for iNOS detection. Data were analysed using one-way ANOVA followed by a post hoc Tukey’s multiple comparison test. *p < 0.05, **p < 0.01, compared with untreated control or S1 stimulation alone
Results in Fig. 5D and E also show that an S1-induced increase in NO production and iNOS protein expression was significantly (p < 0.01) reduced when the cells were treated with BAY11-7082 (1 µM) prior to S1 stimulation.
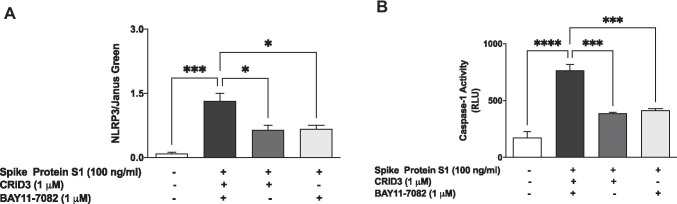
S1 Triggers Activation of NLRP3 Inflammasome/Caspase-1 in BV-2 Microglia
The NLRP3 inflammasome is known to contribute to the secretion of IL-1β during inflammation. Encouraged by results of experiments showing an increase in the production of this cytokine following BV-2 stimulation with S1, we next investigated its effect on protein levels of NLRP3 in the presence and absence of known NLRP3 inhibitors, CRID3 and BAY11-7082. Cytoblot analyses revealed that stimulation of BV-2 microglia with S1 (100 ng/ml) for 6 h resulted in an ~ 11-fold increase in levels of NLRP3 protein. We also observed that an S1-induced increase in NLRP3 protein levels was significantly reduced (p < 0.05) in the presence of CRID3 (1 µM) and BAY11-7082 (1 µM) (Fig. 6A).
Fig. 6.
A Stimulation of BV-2 microglia with S1 (100 ng/ml) increased the protein expression of NLRP3 inflammasome and was inhibited in the presence of CRID3 (1 µM) and BAY11-7082 (1 µM). B Increased caspase-1 activity by S1 (100 ng/ml) BV-2 microglia was reduced in the presence of CRID3 (1 µM) and BAY11-7082 (1 µM). Data were analysed using one-way ANOVA followed by a post hoc Tukey’s multiple comparison test. *p < 0.05, ***p < 0.001, ****p < 0.0001, compared with untreated control or S1 stimulation alone
We next determined measured caspase-1 activity in culture media of BV-2 cells that were stimulated with S1 for 6 h. Results in Fig. 6B show a ~ 4.4-fold increase in caspase-1 activity as a result of S1 stimulation. Furthermore, both CRID3 (1 µM) and BAY11-7082 (1 µM) produced significant (p < 0.001) inhibition in S1-induced increased caspase-1 activity.
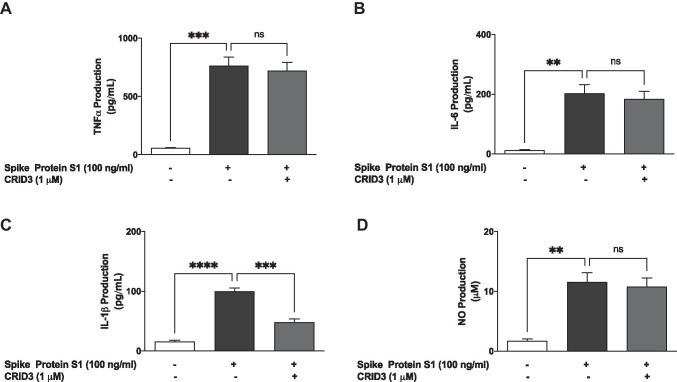
CRID3 Prevented S1-Induced Increase in IL-1β Production
Experiments to evaluate the effects of CRID3 on S1-induced increased secretion of TNF-α, IL-6 and IL-1β in BV-2 microglia revealed that pre-treatment with CRID3 (1 µM) was ineffective in reducing TNF-α (Fig. 7A) and IL-6 (Fig. 7B) production. However, pre-treatment of S1-stimulated BV-2 cells with CRID3 significantly (p < 0.001) reduced IL-1β production (Fig. 7C). We also observed that S1-induced NO production was not reduced by pre-treatment with CRID3 (Fig. 7D).
Fig. 7.
Pre-treatment with CRID3 (1 µM) did not prevent the S1-induced increased production of TNF-α (A), IL-6 (B) and NO (D) while the IL-1β production was reduced (C) in BV-2 microglia. Culture supernatants were analysed using ELISA following stimulation for 24 h. Data were analysed using one-way ANOVA followed by a post hoc Tukey’s multiple comparison test. **p < 0.01, ***p < 0.001, ****p < 0.0001, ns (not significant at p < 0.05), compared with untreated control or S1 stimulation alone
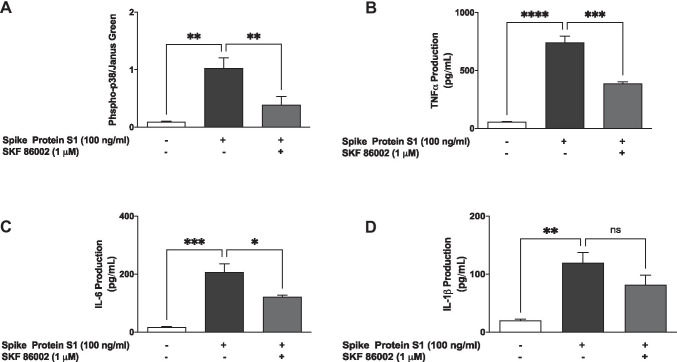
S1 Activated p38 MAP Kinase in BV-2 Microglia
Incubation of spike protein S1 (100 ng/ml) with BV-2 microglia for 60 min resulted in a significant (p < 0.01) and ~ 11.3-fold increase in protein levels of phospho-p38, an outcome that was prevented by pre-treating the cells with SKF 86002 (1 µM) for 60 min prior to S1 stimulation (Fig. 8A).
Fig. 8.
Stimulation of BV-2 microglia with S1 (100ng/ml) increased the protein expression of phospho-p38 MAPK (A), which was inhibited in the presence of SKF 86002 (1 μM). Data were analysed using one-way ANOVA followed by a post hoc Tukey’s multiple comparison test. **p < 0.01, compared with untreated control or S1 stimulation alone. Effects of SKF 86002 (1 μM) on S1-induced increased production of TNFa (B), IL-6 (C) and IL-1β (D) in BV-2 microglia. Culture supernatants were analysed using ELISA following stimulation for 24h. Data were analysed using one-way ANOVA followed by a post hoc Tukey’s multiple comparison test. *p < 0.05, **p < 0.01, ***p < 0.001, ****p < 0.0001, ns (not significant at p<0.05), compared with untreated control, or S1 stimulation alone
Based on the results showing that S1 caused an increase in protein levels of phospho-p38 and its inhibition by SKF 86,002, we were next interested to determine the effects of this inhibitor on cytokine production in S1-stimulated BV-2 microglia. In the presence of SKF 86002 (1 µM), TNF-α production was reduced by ~ 47.9% compared with S1 alone (Fig. 8B). Similarly, S1-induced increased production of IL-6 was significantly (p < 0.05) reduced in the presence of SKF 86002 (1 µM) (Fig. 8C). However, there was an insignificant reduction in the production of IL-1β by SKF 86002 (Fig. 8D).
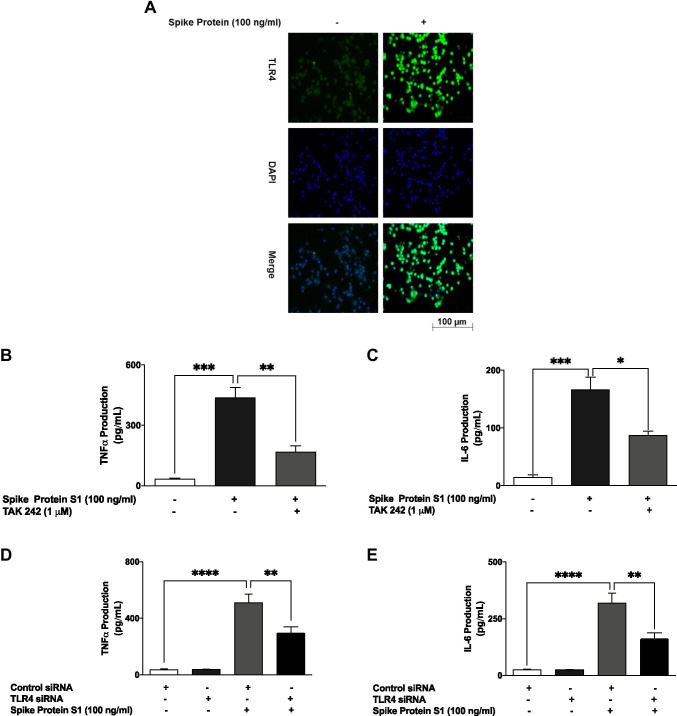
S1-Induced Increased Production of TNF-α and IL-6 Was Reduced by TAK 242 and TLR4 siRNA
Immunofluorescence microscopy revealed that stimulation of BV-2 microglia with 100 ng/ml S1 resulted in a marked increase in TLR4 expression (Fig. 9A). Further experiments showed that pre-treatment with the TLR4 signalling inhibitor TAK 242 (1 µM) resulted in a significant (p < 0.05) reduction in the production of TNF-α and IL-6 (Fig. 9B, C).
Fig. 9.
Immunofluorescence microscopy showing an increase in TLR4 protein expression following stimulation of BV-2 microglia with S1 (100 ng/mL) (A). Pre-treatment of S1-stimulated BV‑2 microglia with TAK 242 (1 μM) reduced the production of TNFα (B) and IL-6 (C). Data were analysed using one-way ANOVA followed by a post hoc Tukey’s multiple comparison test. *p < 0.05, **p < 0.01, ***p < 0.001, compared with untreated control, or S1 stimulation alone. Transfection of S1-stimulated BV-2 microglia with mouse TLR4 siRNA reduced TNFα (D) and IL-6 production (E). Data were analysed using one-way ANOVA followed by a post hoc Tukey’s multiple comparison test. **p < 0.01, ****p < 0.0001, control siRNA versus TLR4 siRNA
Furthermore, TLR4 knockdown experiments revealed that TNF-α production was significantly (p < 0.01) reduced in S1-stimulated BV-2 microglia transfected with TLR4 siRNA, in comparison with cells transfected with control siRNA (Fig. 9D). Similarly, TLR4 knockdown resulted in reduced IL-6 production, when compared with control (Fig. 9E).
Discussion
During SARS-CoV-2 infection, viral attachment, fusion and entry into the host’s cells are facilitated by the spike proteins which protrude from the surface of mature virions, by binding to the host ACE2 protein [36, 37]. However, accumulating pieces of evidence show that in addition to facilitating its fusion to the cell membrane, the location of the spike protein on SARS-CoV-2 also makes it a direct target for host immune responses [36]. With respect to immune responses induced by SARS-CoV-2 infection, it is now established that this may involve an exaggerated inflammation, also known as cytokine storm [38–40]. Recently, we reported induction of increased release of pro-inflammatory cytokines in human peripheral blood mononuclear cells stimulated with the recombinant SARS-CoV-2 spike protein sub-unit S1, further confirming the role of the spike protein in COVID-19 cytokine storm [41].
In this study, we showed for the first time that the recombinant SARS-CoV-2 spike protein sub-unit S1 activated BV-2 microglia as demonstrated by an increase in the protein expression of Iba-1, which is mainly expressed by the microglia and increased by the activation of these cells [42, 43]. We further demonstrated that activation of BV-2 microglia by S1 resulted in the increased release of TNF-α, IL-6 and IL-1β, which are hallmarks of neuroinflammation. Activation of neuroinflammatory processes by the spike S1 protein was further confirmed by results showing increased iNOS-mediated production of NO by the protein in microglia. Elevated iNOS/NO has been previously linked to a wide range of CNS disorders including Alzheimer’s disease, Parkinson’s disease, multiple sclerosis, epilepsy and migraine [44].
These are interesting outcomes, considering the roles played by microglial activation and subsequent increased release of pro-inflammatory mediators in neurological disorders. In Parkinson’s disease for example, a significant increase in the expression of IL-1β was shown in the substantia nigra and frontal cortex, compared to controls [45]. Pro-inflammatory cytokine (IL-1β, TNF-α, IL-6) release has also been linked to depression-like behaviours and cognitive defects in mice [46]. Further studies are therefore needed to elucidate the link between COVID-19–mediated hyper-inflammation and the pathogenesis of neurological symptoms that have been reported to be associated with the disease.
In neuroinflammation, the NF-κB transcription factor regulates the production of multiple pro-inflammatory genes, including the pro-inflammatory cytokines such as TNF-α, IL-6 and IL-1β, as well as iNOS. We further showed that activation of microglial NF-κB signalling mediates the production of pro-inflammatory mediators in the microglia by SARS-CoV-2 spike S1 protein through its ability to promote cytoplasmic phosphorylation of the p65 sub-unit and IκBα, as well as the DNA binding of p65 sub-unit and NF-κB transcriptional activity. Interestingly, these effects were blocked by the potent NF-κB inhibitor BAY11-7082. The involvement of NF-κB in S1 protein–induced neuroinflammation was further confirmed by results showing the effectiveness of BAY11-7082 in blocking S1-induced production of TNF-α, IL-6 and IL-1β, and iNOS/NO in BV-2 microglia. In a similar study reported by Patra et al. [47], SARS-CoV-2 spike protein was shown to promote IL-6 signalling through NF-κB in epithelial cells to initiate coordination of a hyper-inflammatory response. To our knowledge, this is the first evidence demonstrating the role of NF-κB activation in S1-induced microglial activation.
Reports in scientific literature suggest that the NLRP3 inflammasome may be contributing to the release of cytokines such as IL-1β in SARS-CoV-2–induced hyper-inflammation [48–50]. In the microglia, activation of NLRP3 by extracellular ATP, certain bacterial toxins and crystalline and particulate matters results in caspase-1 activation which then cleaves the precursors of IL-1β and IL-18 to generate active IL-1β and IL-18, resulting in neuroinflammation and pyroptosis [51–53]. In this study, we showed that in addition to increasing IL-1β production, SARS-CoV-2 spike S1 protein activated NLRP3 inflammasome and increased caspase-1 activity in BV-2 microglia. These effects were also shown to be attenuated by CRID3 and BAY11-7082, which are known inhibitors of NLRP3. Furthermore, pre-treatment of BV-2 microglia with CRID3 prevented SARS-CoV-2 spike S1 protein–induced IL-1β production, but not TNF-α, IL-6 or NO, suggesting an involvement of the NLRP3 inflammasome activation in neuroinflammation induced by S1 in BV-2 microglia. The observed effects of BAY11-7082 on both NF-κB and NLRP3 activation in S1-stimulated BV-2 microglia reflect a potential therapeutic benefit of this compound in SARS-CoV-2 infection. Previous studies on this inhibitor of NF-κB have shown that it improved survival and reduced pro-inflammatory cytokine levels in the lungs of SARS-CoV–infected mice [54].
It has been suggested that activation of NF-κB could trigger NLRP3 through caspase-1, with subsequent release of mature IL-1β [55]. It is not clear from this study if the activation of NLRP3/caspase-1 by S1 was due to a direct effect on NLRP3 or an indirect action as a result of activating NF-κB. The role of NLRP3 inflammasome activation in S1-induced neuroinflammation therefore requires further investigation.
Our results showing activation of p38 MAPK by S1, coupled with inhibition of S1-induced increased production of TNF-α and IL-6 by the p38 inhibitor (SKF 86002), suggest the involvement of the p38 MAPK signalling in its pro-inflammatory effect in BV-2 microglia. One possible explanation for this effect is the activation by S1 of upstream signals which activate both NF-κB and MAPK signalling in the microglia.
To explore the potential mechanisms involved in dual activation of NF-κB and MAPK by S1 in BV-2 microglia, we conducted experiments that showed an increase in the expression of Toll-like receptor 4 (TLR4) by the protein. Interestingly, a known inhibitor of TLR4 signalling (TAK 242) inhibited S1-induced increased production of both TNF-α and IL-6, which further demonstrates a potential involvement of this pattern recognition receptor (PRR) in S1-induced neuroinflammation.
Our findings seem to confirm those reported from a study by Shirato and Kizaki [56], as they demonstrated involvement of TLR4 in the induction of pro-inflammatory responses in mouse and human macrophages by the SARS-CoV-2 spike protein S1 sub-unit. Similar observations linking TLR4 to induction of inflammation in THP-1 cells have been reported by Zhao et al. [57]. Studies to elucidate detailed modulatory effects of SARS-CoV-2 spike protein S1 sub-unit on microglia TLR4 signalling are required in order to provide a better understanding of the impact of SARS-CoV-2 infection on the brain.
The obtained results from these experiments have provided the first evidence demonstrating the activation of BV-2 microglia by SARS-CoV-2 spike S1 protein, resulting in the production of pro-inflammatory mediators TNF-α, IL-6, IL-1β and NO. We propose that induction of neuroinflammation by this protein in the microglia is mediated through activation of NF-κB and p38 MAPK, possibly as a result of TLR4 activation. These results contribute to our understanding of some of the mechanisms involved in CNS pathologies of SARS-CoV-2.
Supplementary Information
Below is the link to the electronic supplementary material.
Author Contribution
Olumayokun A. Olajide: conceptualisation, methodology, investigation, writing of the original draft, writing which included review and editing and project administration. Victoria U. Iwuanyanwu, Oyinkansola D. Adegbola and Alaa A. Al-Hindawi: investigation.
Data Availability
The datasets generated and/or analysed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics Approval and Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Conflict of Interest
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.World Health Organization (WHO). Novel coronavirus (2019-nCoV) situation reports
- 2.Yang R, Gui X, Xiong Y. Patients with respiratory symptoms are at greater risk of COVID-19 transmission. Respir Med. 2020;165:105935. doi: 10.1016/j.rmed.2020.105935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pollard CA, Morran MP, Nestor-Kalinoski AL. The COVID-19 pandemic: a global health crisis. Physiol Genomics. 2020;52:549–557. doi: 10.1152/physiolgenomics.00089.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhang L, Peres TG, Silva MVF, Camargos P. What we know so far about Coronavirus Disease 2019 in children: a meta-analysis of 551 laboratory-confirmed cases. Pediatr Pulmonol. 2020;55:2115–2127. doi: 10.1002/ppul.24869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Carsana L, Sonzogni A, Nasr A, Rossi RS, Pellegrinelli A, Zerbi P, Rech R, Colombo R, et al. Pulmonary post-mortem findings in a series of COVID-19 cases from Northern Italy: a two-centre descriptive study. Lancet Infect Dis. 2020;20:1135–1140. doi: 10.1016/S1473-3099(20)30434-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cataldi M, Pignataro G, Taglialatela M. Neurobiology of coronaviruses: potential relevance for COVID-19. Neurobiol Dis. 2020;143:105007. doi: 10.1016/j.nbd.2020.105007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Iadecola C, Anrather J, Kamel H. Effects of COVID-19 on the nervous system. Cell. 2020;183:16–27.e1. doi: 10.1016/j.cell.2020.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mao L, Jin H, Wang M, Hu Y, Chen S, He Q, Chang J, Hong C, et al. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan. China JAMA Neurol. 2020;77:683–690. doi: 10.1001/jamaneurol.2020.1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Buzhdygan TP, DeOre BJ, Baldwin-Leclair A, McGary H, Razmpour R, Galie PA, Potula R, Andrews AM, et al. The SARS-CoV-2 spike protein alters barrier function in 2D static and 3D microfluidic in vitro models of the human blood-brain barrier. Neurobiol Dis. 2020;146:105131. doi: 10.1016/j.nbd.2020.105131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yachou Y, El Idrissi A, Belapasov V, Ait Benali S. Neuroinvasion, neurotropic, and neuroinflammatory events of SARS-CoV-2: understanding the neurological manifestations in COVID-19 patients. Neurol Sci. 2020;41:2657–2669. doi: 10.1007/s10072-020-04575-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bodnar B, Patel K, Ho W, Luo JJ, Hu W. Cellular mechanisms underlying neurological/neuropsychiatric manifestations of COVID-19. J Med Virol. 2021;93:1983–1998. doi: 10.1002/jmv.26720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Colonna M, Butovsky O. Microglia function in the central nervous system during health and neurodegeneration. Annu Rev Immunol. 2017;35:441–468. doi: 10.1146/annurev-immunol-051116-052358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nimmerjahn A, Kirchhoff F, Helmchen F. Resting microglial cells are highly dynamic surveillants of brain parenchyma in vivo. Science. 2005;308:1314–1318. doi: 10.1126/science.1110647. [DOI] [PubMed] [Google Scholar]
- 14.Cartier N, Lewis CA, Zhang R, Rossi FM. The role of microglia in human disease: therapeutic tool or target? Acta Neuropathol. 2014;128:363–380. doi: 10.1007/s00401-014-1330-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Du L, Zhang Y, Chen Y, Zhu J, Yang Y, Zhang HL. Role of microglia in neurological disorders and their potentials as a therapeutic target. Mol Neurobiol. 2017;54:7567–7584. doi: 10.1007/s12035-016-0245-0. [DOI] [PubMed] [Google Scholar]
- 16.Mahad DJ, Ransohoff RM. The role of MCP-1 (CCL2) and CCR2 in multiple sclerosis and experimental autoimmune encephalomyelitis (EAE) Semin Immunol. 2003;15:23–32. doi: 10.1016/s1044-5323(02)00125-2. [DOI] [PubMed] [Google Scholar]
- 17.Loane DJ, Byrnes KR. Role of microglia in neurotrauma. Neurotherapeutics. 2010;7:366–377. doi: 10.1016/j.nurt.2010.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Michell-Robinson MA, Touil H, Healy LM, Owen DR, Durafourt BA, Bar-Or A, Antel JP, Moore CS. Roles of microglia in brain development, tissue maintenance and repair. Brain J Neurol. 2015;138:1138–1159. doi: 10.1093/brain/awv066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jimenez S, Baglietto-Vargas D, Caballero C, Moreno-Gonzalez I, Torres M, Sanchez-Varo R, Ruano D, Vizuete M, et al. Inflammatory response in the hippocampus of PS1M146L/APP751SL mouse model of Alzheimer’s disease: age-dependent switch in the microglial phenotype from alternative to classic. J Neurosci. 2008;28:11650–11661. doi: 10.1523/JNEUROSCI.3024-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Varnum MM, Ikezu T. The classification of microglial activation phenotypes on neurodegeneration and regeneration in Alzheimer’s disease brain. Arch Immunol Ther Exp. 2012;60:251–266. doi: 10.1007/s00005-012-0181-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Liao B, Zhao W, Beers DR, Henkel JS, Appel SH. Transformation from a neuroprotective to a neurotoxic microglial phenotype in a mouse model of ALS. Exp Neurol. 2012;237:147–152. doi: 10.1016/j.expneurol.2012.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cherry JD, Olschowka JA, O'Banion MK. Neuroinflammation and M2 microglia: the good, the bad, and the inflamed. J Neuroinflammation. 2014;11:98. doi: 10.1186/1742-2094-11-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gerhard A, Pavese N, Hotton G, Turkheimer F, Es M, Hammers A, Eggert K, Oertel W, et al. In vivo imaging of microglial activation with [11C](R)-PK11195 PET in idiopathic Parkinson’s disease. Neurobiol Dis. 2006;21:404–412. doi: 10.1016/j.nbd.2005.08.002. [DOI] [PubMed] [Google Scholar]
- 24.Mondelli V, Vernon AC, Turkheimer F, Dazzan P, Pariante CM. Brain microglia in psychiatric disorders. Lancet Psychiatry. 2017;4:563–572. doi: 10.1016/S2215-0366(17)30101-3. [DOI] [PubMed] [Google Scholar]
- 25.Ikawa D, Makinodan M, Iwata K, et al. Microglia-derived neuregulin expression in psychiatric disorders. Brain Behav Immun. 2017;61:375–385. doi: 10.1016/j.bbi.2017.01.003. [DOI] [PubMed] [Google Scholar]
- 26.Dowlati Y, Herrmann N, Swardfager W, Liu H, Sham L, Reim EK, Lanctôt KL. A meta-analysis of cytokines in major depression. Biol Psychiatry. 2010;67:446–457. doi: 10.1016/j.biopsych.2009.09.033. [DOI] [PubMed] [Google Scholar]
- 27.Frick LR, Williams K, Pittenger C. Microglial dysregulation in psychiatric disease. Clin Dev Immunol. 2013;2013:608654. doi: 10.1155/2013/608654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Velagapudi R, Lepiarz I, El-Bakoush A, Katola FO, Bhatia H, Fiebich BL, Olajide OA. Induction of autophagy and activation of SIRT-1 deacetylation mechanisms mediate neuroprotection by the pomegranate metabolite urolithin A in BV2 microglia and differentiated 3D human neural progenitor cells. Mol Nutr Food Res. 2019;63:e1801237. doi: 10.1002/mnfr.201801237. [DOI] [PubMed] [Google Scholar]
- 29.Olajide OA, Akande IS, da Silva Maia Bezerra Filho C, Lepiarz-Raba I, de Sousa DP. Methyl 3,4,5-trimethoxycinnamate suppresses inflammation in RAW264.7 macrophages and blocks macrophage-adipocyte interaction. Inflammopharmacology. 2020;28:1315–1326. doi: 10.1007/s10787-020-00720-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Velagapudi R, Kosoko AM, Olajide OA. Induction of neuroinflammation and neurotoxicity by synthetic hemozoin. Cell Mol Neurobiol. 2019;39:1187–1200. doi: 10.1007/s10571-019-00713-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kandasamy M. NF-κB signalling as a pharmacological target in COVID-19: potential roles for IKKβ inhibitors. Naunyn Schmiedebergs Arch Pharmacol. 2021;394:561–567. doi: 10.1007/s00210-020-02035-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Coll RC, Robertson AA, Chae JJ, et al. A small-molecule inhibitor of the NLRP3 inflammasome for the treatment of inflammatory diseases. Nat Med. 2015;21:248–255. doi: 10.1038/nm.3806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lee JC, Kumar S, Griswold DE, Underwood DC, Votta BJ, Adams JL. Inhibition of p38 MAP kinase as a therapeutic strategy. Immunopharmacology. 2000;47:185–201. doi: 10.1016/s0162-3109(00)00206-x. [DOI] [PubMed] [Google Scholar]
- 34.Yamada M, Ichikawa T, Ii M, Sunamoto M, Itoh K, Tamura N, Kitazaki T. Discovery of novel and potent small-molecule inhibitors of NO and cytokine production as antisepsis agents: synthesis and biological activity of alkyl 6-(N-substituted sulfamoyl)cyclohex-1-ene-1-carboxylate. J Med Chem. 2005;48:7457–7467. doi: 10.1021/jm050623t. [DOI] [PubMed] [Google Scholar]
- 35.Takashima K, Matsunaga N, Yoshimatsu M, Hazeki K, Kaisho T, Uekata M, Hazeki O, Akira S, et al. Analysis of binding site for the novel small-molecule TLR4 signal transduction inhibitor TAK-242 and its therapeutic effect on mouse sepsis model. Br J Pharmacol. 2009;157:1250–1262. doi: 10.1111/j.1476-5381.2009.00297.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Walls AC, Park YJ, Tortorici MA, Wall A, McGuire AT, Veesler D. Structure, function, and antigenicity of the SARS-CoV-2 spike glycoprotein. Cell. 2020;181:281–292.e6. doi: 10.1016/j.cell.2020.02.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Duan L, Zheng Q, Zhang H, Niu Y, Lou Y, Wang H. The SARS-CoV-2 spike glycoprotein biosynthesis, structure, function, and antigenicity: implications for the design of spike-based vaccine immunogens. Front Immunol. 2020;11:576622. doi: 10.3389/fimmu.2020.576622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Moradian N, Gouravani M, Salehi MA, Heidari A, Shafeghat M, Hamblin MR, Rezaei N. Cytokine release syndrome: inhibition of pro-inflammatory cytokines as a solution for reducing COVID-19 mortality. Eur Cytokine Netw. 2020;31:81–93. doi: 10.1684/ecn.2020.0451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hirawat R, Saifi MA, Godugu C. Targeting inflammatory cytokine storm to fight against COVID-19 associated severe complications. Life Sci. 2021;267:118923. doi: 10.1016/j.lfs.2020.118923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yang L, Liu S, Liu J, Zhang Z, Wan X, Huang B, Chen Y, Zhang Y. COVID-19: immunopathogenesis and immunotherapeutics. Signal Transduct Target Ther. 2020;5:128. doi: 10.1038/s41392-020-00243-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Olajide OA, Iwuanyanwu VU, Lepiarz-Raba I, Al-Hindawi AA. Induction of exaggerated cytokine production in human peripheral blood mononuclear cells by a recombinant SARS-CoV-2 spike glycoprotein S1 and its inhibition by dexamethasone. Inflammation. 2021;44:1865–1877. doi: 10.1007/s10753-021-01464-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Imai Y, Ibata I, Ito D, Ohsawa K, Kohsaka S. A novel gene iba1 in the major histocompatibility complex class III region encoding an EF hand protein expressed in a monocytic lineage. Biochem Biophys Res Commun. 1996;224:855–862. doi: 10.1006/bbrc.1996.1112. [DOI] [PubMed] [Google Scholar]
- 43.Ito D, Imai Y, Ohsawa K, Nakajima K, Fukuuchi Y, Kohsaka S. Microglia-specific localisation of a novel calcium binding protein, Iba1. Brain Res Mol Brain Res. 1998;57:1–9. doi: 10.1016/s0169-328x(98)00040-0. [DOI] [PubMed] [Google Scholar]
- 44.Tripathi MK, Kartawy M, Amal H. The role of nitric oxide in brain disorders: autism spectrum disorder and other psychiatric, neurological, and neurodegenerative disorders. Redox Biol. 2020;34:101567. doi: 10.1016/j.redox.2020.101567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kouli A, Camacho M, Allinson K, Williams-Gray CH. Neuroinflammation and protein pathology in Parkinson’s disease dementia. Acta Neuropathol Commun. 2020;8:211. doi: 10.1186/s40478-020-01083-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zhang J, He H, Qiao Y, Zhou T, He H, Yi S, Zhang L, Mo L, et al. Priming of microglia with IFN-γ impairs adult hippocampal neurogenesis and leads to depression-like behaviors and cognitive defects. Glia. 2020;68:2674–2692. doi: 10.1002/glia.23878. [DOI] [PubMed] [Google Scholar]
- 47.Patra T, Meyer K, Geerling L, Isbell TS, Hoft DF, Brien J, Pinto AK, Ray RB, et al. SARS-CoV-2 spike protein promotes IL-6 trans-signaling by activation of angiotensin II receptor signaling in epithelial cells. PLoS Pathog. 2020;16:e1009128. doi: 10.1371/journal.ppat.1009128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Freeman TL, Swartz TH. Targeting the NLRP3 inflammasome in severe COVID-19. Front Immunol. 2020;11:1518. doi: 10.3389/fimmu.2020.01518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Chang YS, Ko BH, Ju JC, Chang HH, Huang SH, Lin CW. SARS unique domain (sud) of severe acute respiratory syndrome coronavirus induces NLRP3 inflammasome-dependent CXCL10-mediated pulmonary inflammation. Int J Mol Sci. 2020;21:3179. doi: 10.3390/ijms21093179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Rodrigues TS, de Sá KSG, Ishimoto AY, et al. Inflammasomes are activated in response to SARS-CoV-2 infection and are associated with COVID-19 severity in patients. J Exp Med. 2021;218:e20201707. doi: 10.1084/jem.20201707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Venegas C, Heneka MT. Danger-associated molecular patterns in Alzheimer’s disease. J Leukoc Biol. 2017;101:87–98. doi: 10.1189/jlb.3MR0416-204R. [DOI] [PubMed] [Google Scholar]
- 52.Zhang Y, Zhao Y, Zhang J, Yang G. Mechanisms of NLRP3 inflammasome activation: its role in the treatment of Alzheimer’s disease. Neurochem Res. 2020;45:2560–2572. doi: 10.1007/s11064-020-03121-z. [DOI] [PubMed] [Google Scholar]
- 53.Chang Y, Zhu J, Wang D, et al. NLRP3 inflammasome-mediated microglial pyroptosis is critically involved in the development of post-cardiac arrest brain injury. J Neuroinflammation. 2020;17:219. doi: 10.1186/s12974-020-01879-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.DeDiego ML, Nieto-Torres JL, Regla-Nava JA, et al. Inhibition of NF-κB–mediated inflammation in severe acute respiratory syndrome coronavirus-infected mice increases survival. J Virol. 2014;88:913–924. doi: 10.1128/JVI.02576-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kersse K, Bertrand MJ, Lamkanfi M, Vandenabeele P. NOD-like receptors and the innate immune system: coping with danger, damage and death. Cytokine Growth Factor Rev. 2011;22:257–276. doi: 10.1016/j.cytogfr.2011.09.003. [DOI] [PubMed] [Google Scholar]
- 56.Shirato K, Kizaki T. SARS-CoV-2 spike protein S1 subunit induces pro-inflammatory responses via toll-like receptor 4 signaling in murine and human macrophages. Heliyon. 2021;7:e06187. doi: 10.1016/j.heliyon.2021.e06187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Zhao Y, Kuang M, Li J, Zhu L, Jia Z, Guo X, Hu Y, Kong J, et al. SARS-CoV-2 spike protein interacts with and activates TLR41. Cell Res. 2021;31:818–820. doi: 10.1038/s41422-021-00495-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated and/or analysed during the current study are available from the corresponding author on reasonable request.