Abstract
Background:
Diastasis of the rectus abdominis muscle is a common condition. There are no generally accepted criteria for diagnosis or treatment of diastasis of the rectus abdominis muscle, which causes uncertainty for the patient and healthcare providers alike.
Methods:
The consensus document was created by a group of Swedish surgeons and based on a structured literature review and practical experience.
Results:
The proposed criteria for diagnosis and treatment of diastasis of the rectus abdominis muscle are as follows: (1) Diastasis diagnosed at clinical examination using a caliper or ruler for measurement. Diagnostic imaging by ultrasound or other imaging modality, should be performed when concurrent umbilical or epigastric hernia or other cause of the patient’s symptoms cannot be excluded. (2) Physiotherapy is the firsthand treatment for diastasis of the rectus abdominis muscle. Surgery should only be considered in diastasis of the rectus abdominis muscle patients with functional impairment, and not until the patient has undergone a standardized 6-month abdominal core training program. (3) The largest width of the diastasis should be at least 5 cm before surgical treatment is considered. In case of pronounced abdominal bulging or concomitant ventral hernia, surgery may be considered in patients with a smaller diastasis. (4) When surgery is undertaken, at least 2 years should have elapsed since last childbirth and future pregnancy should not be planned. (5) Plication of the linea alba is the firsthand surgical technique. Other techniques may be used but have not been found superior.
Discussion:
The level of evidence behind these statements varies, but they are intended to lay down a standard strategy for treatment of diastasis of the rectus abdominis muscle and to enable uniformity of management.
Keywords: Diastasis of the rectus abdominis muscles, guidelines, linea alba, pregnancy, physiotherapy, mesh
Introduction
Diastasis of the rectus abdominis muscles (DRAM) is defined as increased separation of the medial edges of the two rectus muscles due to stretching and laxity of the linea alba 1 . It is commonly associated with an abdominal bulge without fascial defect. The upper limit of physiological separation of the rectus muscles varies in different studies as does the recommended point of measurement2,3.
DRAM is not a hernia and there is no risk of incarceration. The widening and thinning of the linea alba as well as the bulging of the abdominal wall may, however, be associated with increased risk of developing midline herniation such as epigastric and umbilical hernia4,5. The increased inter-rectus distance (IRD) in pregnant women represents one aspect of the general physiological relaxation of connective tissues in anticipation of partus. The increase in intra-abdominal pressure also plays a role in the pathophysiology of DRAM5 –9.
DRAM may cause cosmetic impairment, abdominal and lower back pain, as well as reduced strength of the trunk muscles6,7. It has been suggested that it is not the diastasis per se but rather the bulging or protrusion of the entire abdominal wall that causes functional disability8,9.
Core training improves physical function and quality of life 7 . Its effect on reducing the diastasis as such, however, is not well-established10 –12.
The role of surgery in the treatment of DRAM is controversial. Most operations are still done for aesthetic reasons and as part of abdominoplasty10,13 –15. Since surgery solely aiming at correction of cosmetic defects is currently not supported by the Swedish public healthcare system, most diastasis patients are operated in private hospitals. However, functional disability related to DRAM falls under the responsibility of the public healthcare system, and substantial regional differences in access to DRAM surgery have been identified. If we are to provide the treatment necessary on equal terms, we must have Swedish national guidelines on the management of DRAM.
The objective of this document was to define and present recommendations for the management of patients with symptomatic diastasis of the rectus muscles (DRAM) for use as a basis for future guidelines. These recommendations will focus on indications for surgery.
Methods
In 2017, a group of Swedish specialists in surgery were gathered together by the Swedish Association of Innovative Surgical Technology and the Swedish Surgical Society to discuss and present evidence-based recommendations to be used in future guidelines on the management of DRAM. The group consisted of abdominal surgeons and plastic surgeons with experience in DRAM surgery.
The present recommendations have been developed in collaboration with the Health Technology Assessment Group of the South-East Region of Sweden.
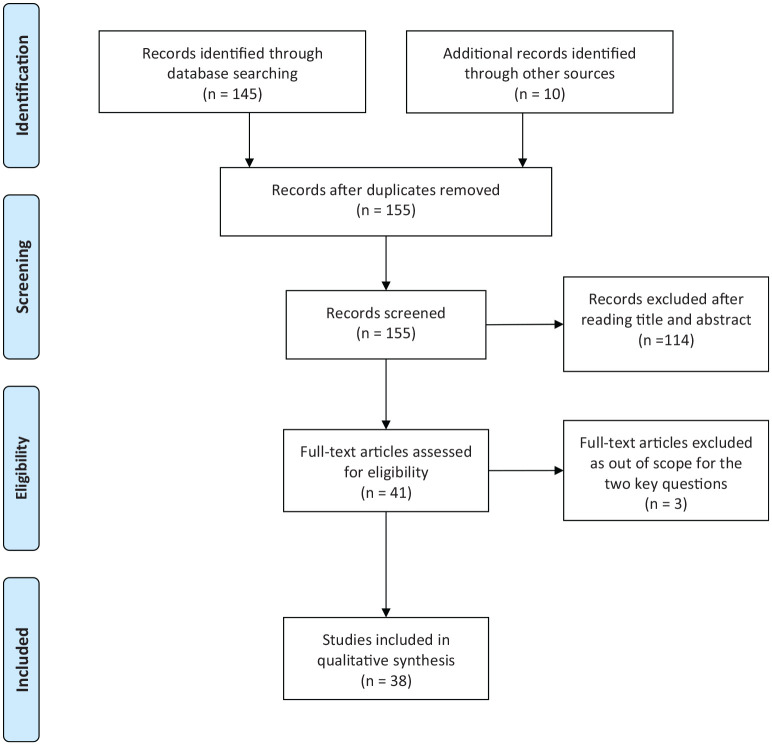
A search in PubMed was performed by the Health Technology Assessment Group of the South-East Region of Sweden 2019-11-07. A total of 86 references were identified using the following search terms: Diastasis (All Fields) AND recti (All Fields) AND (“therapy”(Subheading) OR “therapy”(All Fields) OR “treatment”(All Fields) OR “therapeutics”(MeSH Terms) OR “therapeutics”(All Fields)). A further 59 references were found using the following search terms: Diastasis (All Fields) OR (divarication (All Fields) AND recti(All Fields)) OR rectus(All Fields)) AND (randomized(All Fields) AND controlled(All Fields)). See prisma flow diagram (Fig. 1).
Fig. 1.
Prisma flow chart.
The recommendation group identified the following key-questions:
What is the expected outcome of physiotherapy in patients with DRAM?
Which patients should be considered for operative correction of DRAM (Indications and contraindications for surgery)?
The levels of evidence and grades of recommendations were rated according to the Oxford Center for Evidence-based Medicine—Levels of Evidence 16 .
Results
Studies identified in the search are listed in Table 1. Studies exploring the outcome after surgery are listed in Table 2.
Table 1.
Studies included in the qualitative synthesis.
| Author | Year | Study type | No. of patients | Main finding |
|---|---|---|---|---|
| Effect of physiotherapy | ||||
| Mota et al. 28 | 2015 | Longitudinal cohort study | 84 | Abdominal Crunch Exercise produced significant narrowing of the IRD |
| Gluppe et al. 29 | 2018 | RCT | 175 | No significant effect on IRD of a postpartum training program |
| Thabet et al. 12 | 2019 | RCT | 40 | A deep core stabilizing program reduces inter-recti distance (IRD) in postpartum women with DRAM |
| Emanuelsson et al. 9 | 2016 | RCT | 32 | Improved muscular strength, function, and quality of life after a 3 months training program in patients with DRAM |
| Width of the diastasis | ||||
| Mota et al. 18 | 2018 | Prospective cohort study | 84 | Definition of normal IRD during pregnancy and 6 months postpartum |
| Ranney 4 | 1990 | Cross-sectional descriptive study | 1763 | Classification of DRAM. High prevalence of umbilical hernias in women with DRAM. |
| Liaw et al. 20 | 2011 | Prospective cohort study | 40 + 20 controls | No clear relationships found between width of diastasis and abdominal muscle function in postpartum women. |
| Gunnarsson et al. 21 | 2015 | Cross-sectional descriptive study | 57 | A positive correlation existed between abdominal muscle strength and IRD below the umbilicus, but not when IRD was measured above the umbilicus. |
| Kohler et al. 30 | 2018 | Case series | 20 | Concomitant repair of ventral hernias and DRAM |
| Olsson et al. 5 | 2019 | Prospective cohort study | 60 | 75% of women operated for DRAM had concomitant ventral hernias |
| Preoperative diagnostic imaging | ||||
| Mota et al. 24 | 2012 | Test–retest reliability study | 24 | Ultrasound imaging is a reliable method for measuring the IRD |
| Keshwani et al. 23 | 2018 | Cross-sectional study | 32 | Ultrasound measurement of IRD in the early postpartum period correlated well to symptoms of DRAM. |
| Emanuelsson et al. 31 | 2014 | Cross-sectional study | 55 | Clinical assessment prior to surgery provides more accurate information than CT scanning in the assessment of ARD width. |
| Time between last childbirth and operation | ||||
| Boissonnault et al. 25 | 1988 | Cross-sectional study | 71 | DRAM most common in third trimester and persists in the immediate postpartum period. |
| Sperstad et al. 26 | 2016 | Prospective cohort study | 300 | Prevalence of DRAM was 33% 12 months after delivery. |
| Ranney 4 | 1990 | Cross-sectional study | 1738 | Less than 1% of parous women had a “severe” diastasis exceeding 5 cm. |
| Surgical methods | ||||
| Van Uchelen et al. 32 | 2001 | Cross-sectional study | 40 | 40% recurrence rate after repair of DRAM as part of abdominoplasty. |
| Bellido Luque et al. 33 | 2015 | Prospective cohort study | 21 | No recurrence after totally endoscopic approach to diastasis recti associated with midline hernias (no mesh) |
| Köhler et al. 30 | 2018 | Prospective cohort study | 20 | No recurrence at 5 months after minimal invasive linea alba reconstruction (MILAR) |
| Köckerling et al. 34 | 2016 | Prospective cohort study | 40 | No early recurrences after endoscopic-assisted linea alba reconstruction plus mesh augmentation (ELAR plus) |
| Emanuelsson et al. 9 | 2016 | RCT | 86 | No difference in outcome between retromuscular mesh repair and double-row self-retaining sutures. |
| Nahas et al. 35 | 2005 | Case series | 12 | No recurrence rate 6–7 years after plication of DRAM. |
| Olsson et al. 5 | 2019 | Prospective cohort study | 60 | Significant improvement in quality of life and abdominal trunk function after surgical repair of DRAM. |
IRD: inter-recti distance; RCT: randomized controlled trials; DRAM: diastasis of the rectus abdominis muscle; ARD: abdominal rectus diastasis; MILAR: minimal invasive linea alba reconstruction; ELAR: endoscopic-assisted linea alba reconstruction plus mesh augmentation.
Table 2.
DRAM: Outcome of surgery.
| Author | Year | Study type | No | Follow-up | Main findings |
|---|---|---|---|---|---|
| Emanuelsson et al. 9 | 2016 | RTC Retro muscular mesh repair versus double-row self-retaining sutures (Quill) |
86 | 1 year | Improved abdominal wall stability and muscle strength. Improved functional ability and quality of life. No difference between the two groups at 1 year. One early recurrence in the Quill group. Five (6%) patients with encapsulated seroma needing reoperation. |
| Olsson et al. 5 | 2019 | Prospective Cohort study. Women with DRAM and symptoms resistant to training. Open double-row plication of linea alba (Quill) |
60 | 1 year | Surgical reconstruction resulted in improved abdominal trunk function and quality of life (SF-36) at 1 year. No recurrence was noted at one year of follow-up. Postoperative complications (bleeding, wound infection and seroma) was found in eleven patients. Reoperation was required in four patients. |
| Van Uchelen et al. 32 | 2001 | Cross-sectional study | 40 | 32–109 months | 40% recurrence rate after suture repair of DRAM in connection with abdominoplasty. |
| Nahas et al. 35 | 2005 | Case series | 12 | 76–84 months | No recurrent diastasis after repair with non-absorbable suture in connection with abdominoplasty |
| Shirah and Shirah 36 | 2016 | Retrospective cohort study Comparing open and laparoscopic mesh repair |
216 | 2 years | Wound infections and seroma more common in the open repair group. No recurrence in any of the two groups after 24 months of follow-up. |
DRAM: diastasis of the rectus abdominis muscle.
Effect of Physiotherapy
Evidence supporting an effect of training programs in the prevention or treatment of DRAM width is generally weak 17 . In a recently published report, however, Thabet and Alshehri(12) showed a significant reduction in IRD after 8 weeks of a “deep core stability exercise program” compared to a control group who underwent a traditional exercise program.
However, there is strong evidence in favor of a positive effect of core training on abdominal muscle strength and function. Emanuelsson and his colleagues7,9 found that a 3-month training program improved objectively measured muscular strength. In their study, significant functional improvement reported in a validated questionnaire, the Ventral Hernia Pain Questionnaire (VHPQ), was seen. The training program also had a positive effect on quality of life. However, neither compliance with the training program nor the long-term impact on functional outcome was reported7,9.
Although there are few studies showing a long-lasting effect of core training on symptoms related to DRAM, there is widespread agreement that non-invasive treatment is the firsthand choice for a condition that is essentially related to abdominal trunk function and not associated with any potentially severe event requiring surgical treatment 10 .
Level of evidence 2C: Outcome studies.
Recommendation (Grade C): The firsthand treatment for DRAM is core training. Surgery should not be considered until the patient has undergone a training program for at least 6 months.
Width of the Diastasis
There are several classifications of DRAM based on the width of the diastasis at different points of measurement.
In a longitudinal study of 84 primiparous women using ultrasound, Mota et al. (18) found the upper limits of IRD to be 28 mm above the umbilicus and 21 mm below the umbilicus at 6 months postpartum.
The following classification of DRAM was proposed by Ranney in 1990: mild diastasis < 3 cm, moderate 3–5 cm, and severe diastasis > 5 cm 4 . A classification of rectus diastasis using five points of measurements along the midline has recently been proposed by Reinpold et al. 19 .
There is no clear association between the width of the diastasis and abdominal muscle function in postpartum women 20 . Gunnarsson et al. 21 found a strong correlation between muscle strength and rectus diastasis width below the umbilicus. The correlation, however, was only statistically significant when using intraoperative measurement of the diastasis. In their study, no correlation was found between muscle strength and IRD above the umbilicus.
The presence of an associated ventral hernia may be an indication for surgery, regardless of the size of a concomitant diastasis2,4. The surgical procedure should focus on the repair of the hernia, but may also include closure of the diastasis. In a cohort study, Olsson et al. (5) showed a perioperative incidence of concomitant epigastric and/or umbilical hernia of 75%.
Level of evidence 4: consensus agreement.
Recommendation (Grade D): The largest width of the diastasis should be at least 5 cm (“severe diastasis”) for surgery to be considered. Surgical repair of the diastasis is recommended in patients with a symptomatic ventral hernia irrespective of the width of the diastasis. In the case of pronounced abdominal bulging or when performing trials, surgery on patients with a diastasis exceeding 3 cm may be considered.
Preoperative Diagnostic Imaging
There is no international consensus on which method of measurement should be used to measure the inter-recti distance in DRAM22 –24. In a systematic review of different methods, van de Water and Benjamin concluded that both calipers and ultrasound are adequate tools to assess DRAM, although ultrasound imaging is most widely used 22 . The advantage of ultrasound is its ability to detect any associated hernia, which may strengthen the indication for surgical repair.
Level of evidence 2C: outcome studies.
Recommendation (Grade C): Diagnostic imaging by ultrasound should be done prior to surgery in cases where concurrent umbilical or epigastric hernia is suspected or it is not possible to determine the width of the diastasis at clinical examination. Computed tomography (CT) scan may be used to rule out other pathology.
Time Between Last Childbirth and Surgery
Most women develop DRAM during the last trimester, and this persists into the immediate postpartum period 25 . Separation of the rectus muscles gradually decreases with time after delivery. In a cohort study of 300 women, Sperstad et al. 26 found a 60% prevalence of DRAM 6 weeks postpartum gradually decreasing to 33% 12 months after delivery. In their study, measuring inter-recti distance using a finger-width method, no woman was found to have severe diastasis (exceeding 5–6 cm) and only two women had a diastasis that could be classified as “moderate.” This finding corresponds well with figures reported by Ranney 1990, that only 0.7% of 1738 parous women had a diastasis exceeding 5 cm 4 .
Level of evidence 4: Consensus agreement.
Recommendation (Grade D): At least 2 years should have elapsed since last childbirth before considering surgery, and pregnancy thereafter should not be planned.
Surgical Methods
Different techniques for surgical treatment of DRAM have been described.
The two predominating questions are whether to use an open or laparoscopic technique and whether to reinforce the linea alba with a mesh 27 . In a recent review, Mommers et al. 10 reported that 85% of repairs use an open procedure. In open surgery, the incision is either midline or transverse in the lower half of the abdomen. The best cosmetic outcome is generally considered to be achieved through a transverse incision in the lower half of the abdomen combined with abdominoplasty, but this is a longer procedure and requires more surgical experience than simple plication of the linea alba via a midline incision. Most studies on surgical technique are retrospective case studies with low to moderate quality ( 10 ; Table 1).
Outcome and complications.
Recurrence rates vary from 0% to 40% in the long-term follow-up studies 32,35. There are only a few randomized controlled trials (RCT) comparing the outcomes of different techniques. In an RCT including 56 patients comparing a Quill suture technique with mesh reinforcement, Emanuelsson et al. 9 found no difference between groups in recurrence rate or functional results 1 year after surgery and at a 5-year follow-up (data submitted for publication). In a retrospective study comparing open and laparoscopic mesh repair, Shirah and Shirah 36 found no differences in postoperative complication or recurrence rates 2 years after surgery. In their cohort, the mean inter-recti distance was 10 cm in both groups, which could question the external validity of the study.
Postoperative complications include formation of seroma, wound infection, and chronic pain. Persistent loss of sensation due to nerve injury has been reported after procedures involving abdominoplasty 37 . Patient satisfaction is generally reported to be acceptable, but few studies have used a validated instrument for the evaluation of patient-reported outcome (PRO). Olsson et al. (5) showed significant improvements in self-reported functionality and quality of life using two validated forms, the Disability Rating Index (DRI) and the short form-36 (SF-36) quality-of-life assessment form, 1 year after surgery. Emanuelsson et al. 9 used a validated questionnaire for pain assessment (VHPQ) and reported significant improvement in all modalities at follow-up. Furthermore, they found a significant improvement in quality of life (SF-36) 1 year postoperatively with no difference seen between the two study arms.
Level of evidence 1B: RCTs of good quality.
Recommendation (Grade B): Plication of the linea alba is the gold standard and firsthand surgical technique. Other techniques may be practiced locally but have not been found superior in terms of abdominal trunk function.
Quality assessment.
As there is very limited evidence regarding the benefit of surgery for DRAM, there is a need for standardized validated tools to assess function and patient-reported symptoms pre- and postoperatively, as well as a dedicated register for postoperative complications and recurrence after surgery for DRAM.
Level of evidence 4: consensus agreement.
Recommendation (Grade D): There should be standardized follow-up and quality assessment of surgical treatment for DRAM, preferably using a nationwide patient register.
Discussion
There is still no international consensus on the treatment of diastasis recti. The role of surgery is controversial and international guidelines are lacking 10 . Most DRAM procedures are performed during abdominoplasty or for cosmetic reasons and consequently not covered by the public healthcare system in Sweden. Growing evidence that diastasis may also be associated with substantial functional impairment with negative impact on the woman’s quality of life has led to an increase in the demand for national guidelines, and this has recently received considerable attention in the Swedish media. Management of DRAM varies substantially between regions in Sweden. The focus of the present paper concerns indications for surgical correction of DRAM aiming to provide recommendations that may be implemented in future national guidelines.
The results of the present investigation confirm several previous reports that there are few evidence-based recommendations for the management of DRAM. Most reports are of low to moderate scientific quality. Comparison between studies is difficult due to lack of consensus on cut-off points and measurement tools that should be used in the definition of DRAM. Furthermore, studies on long-term outcome comparing core training and surgery are lacking. Most studies have been done on postpartum women and may not necessarily apply to men or nulliparous women.
Core training programs may only partially reduce the inter-recti distance in women with established DRAM, with limited effect on cosmetic outcome. However, there is evidence that core training may lead to considerable functional improvement and increase in abdominal trunk muscle strength. Emanuelsson et al. (9, 13), however, reported that patient satisfaction was lower after a 3-month training program compared to patients who were operated. We need to define how core training should be performed and after how long its effect should be evaluated.
We recommend that all patients should undergo a core training program for a period of at least 6 months before being considered for surgical correction of the diastasis.
At present, there are few reports in the literature regarding the correlation between the width of the diastasis and physical symptoms. Gunnarsson et al. reported a negative correlation between objectively measured muscle strength and inter-recti distance. This, however, was only statistically significant for diastases below the umbilicus. The authors concluded that diastasis width should be used as one of the criteria for surgical treatment. There is an urgent need for studies on the relationship between the degree of diastasis (both width and length), measured in a standardized manner, and physical symptoms.
We recommend that an inter-recti distance of at least 5 cm measured at the widest point along the linea alba should be used as a criterion for surgical treatment. This corresponds to “severe diastasis” according to the classification suggested by Ranney 4 . An IRD less than 5 cm may be accepted for surgery when there is excessive bulging of the abdominal wall or in the presence of an epigastric or umbilical hernia. A diastasis less than 5 cm may also be accepted as a criterion in clinical trials.
It is essential that the IRD is measured and recorded in a standardized manner with the patient in a relaxed supine position. Ultrasound is the most commonly used method in current research and has the advantage of being able to detect a small ventral herniation. The use of calipers or a ruler is a validated alternative. Reinpold et al. (19) in a recent review recommended a classification of DRAM based on five points for IRD measurement as well as the length of the diastasis. An instrument for measuring symptom load including abdominal bulging would be valuable.
When deciding on the method of repair, it must be remembered that DRAM is not a hernia and therefore carries no potential risk of strangulation.
DRAM repair is often combined with abdominoplasty in order to improve the cosmetic outcome. This procedure is technically more difficult with a potentially higher rate of long-term complications 6 . Such cases should be referred to centers with experience in these procedures. Based on the findings of Emanuelsson et al. 9 that mesh reinforcement has no advantage over Quill repair at 1 year, we recommend that plication of the linea alba with double-row sutures via a midline incision be the standard procedure in a general surgical setting. In a recently published cohort study on 60 postpartum women who had not responded to training, Olsson et al. (5) showed significant improvements in abdominal trunk function and quality of life (SF-36) 1 year after surgery using double-row plication of the linea alba without mesh.
Novel minimally invasive endoscopic methods, including mesh reinforcement, have been described for the repair of DRAM with associated ventral hernia33,34,38. Comparative studies and long-term results are not yet available.
PRO, that is, functional results and quality of life including satisfactory cosmetic result should be included in future studies 10 .
There is an urgent need for further studies comparing different repair techniques with PRO as primary outcome. Qualitative methods, focusing on the patient’s perspective and expectations, may be of value in this respect.
As the evidence in favor of surgery for DRAM is very limited, there is a need for standardized assessment of short- and long-term outcomes after DRAM repair. If there is to be support for surgical repair of a condition that is not associated with mortality or unequivocally defined morbidity in a publicly financed healthcare system, outcomes must be meticulously assessed and transparently presented to the healthcare provider.
Summary and Conclusion
This consensus report, based on current literature, was produced by a working group under the auspices of the Swedish Surgical Society. It provides recommendations that may be used in future national guidelines on the management of DRAM.
Rectus diastasis is associated with both cosmetic and functional disability, especially in women after childbirth. The level of evidence for management of rectus diastasis is generally low and great regional differences in treatment exist in Sweden. Training programs specifically targeting DRAM lead to significant increases in physical function though cosmetic improvement is limited.
The indication for surgical treatment of DRAM in the absence of associated ventral hernia is still controversial. Several methods of repair have been described including plication with or without mesh reinforcement. Open repair techniques dominate but new minimally invasive endoscopic or endoscopic-assisted methods have been described with promising short-term results.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
ORCID iD: Gabriel Sandblom  https://orcid.org/0000-0002-7416-4951
https://orcid.org/0000-0002-7416-4951
Contributor Information
Anders Carlstedt, Department of Surgery, Karlstad Central Hospital, Karlstad, Sweden.
Sven Bringman, Department of Surgery, Södertälje Hospital, Stockholm, Sweden; Department of Clinical Sciences, Danderyds Hospital, Karolinska Institutet, Stockholm, Sweden.
Mattias Egberth, Department of Surgery, Mora hospital, Mora, Sweden.
Peter Emanuelsson, Department of Molecular Medicine and Surgery, Karolinska Institutet, Solna, Sweden.
Anders Olsson, Department of Clinical Science and Education Södersjukhuset, Karolinska Institutet, Stockholm, Sweden; Clinic of Surgery, Capio CFTK, Stockholm, Sweden.
Ulf Petersson, Department of Surgery, Skåne University Hospital, Lund University, Malmö, Sweden.
Joakim Pålstedt, Department of Clinical Sciences, Danderyds Hospital, Karolinska Institutet, Stockholm, Sweden; Department of Surgery, Ersta Hospital, Stockholm, Sweden.
Gabriel Sandblom, Department of Surgery, Södersjukhuset, Stockholm, 118 83, Sweden. Department of Clinical Science and Education Södersjukhuset, Karolinska Institutet, Stockholm, Sweden.
Rune Sjödahl, Department of Surgery, Linköping University Hospital, Linköping, Sweden.
Birgit Stark, Department of Molecular Medicine and Surgery, Karolinska Institute, Solna, Sweden.
Karin Strigård, Department of Surgical and Perioperative Sciences, Umeå University, Umeå, Sweden.
Jael Tall, Department of Clinical Sciences, Danderyds Hospital, Karolinska Institutet, Stockholm, Sweden; Department of Surgery, Ersta Hospital, Stockholm, Sweden.
Elvar Theodorsson, Department of Clinical Chemistry and Department of Clinical and Experimental Medicine, Linköping University, Linköping, Sweden.
References
- 1. Werner LA, Dayan M: Diastasis recti abdominis-diagnosis, risk factors, effect on musculoskeletal function, framework for treatment and implications for the pelvic floor. Curr Womens Health R 2019;15:86–101. [Google Scholar]
- 2. Kimmich N, Haslinger C, Kreft M, et al. : [Diastasis recti abdominis and pregnancy]. Praxis 2015;104:803–806. [DOI] [PubMed] [Google Scholar]
- 3. Emanuelsson P: Alternatives in the Treatment of Abdominal Rectus Muscle Diastasis: An Evaluation. Karolinska Institutet, Stockholm, 2014. [Google Scholar]
- 4. Ranney B: Diastasis recti and umbilical hernia causes, recognition and repair. S D J Med 1990;43(10):5–8. [PubMed] [Google Scholar]
- 5. Olsson A, Kiwanuka O, Wilhelmsson S, et al. : Cohort study of the effect of surgical repair of symptomatic diastasis recti abdominis on abdominal trunk function and quality of life. BJS Open 2019;3(6):750–758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Akram J, Matzen SH: Rectus abdominis diastasis. J Plast Surg Hand Surg 2014;48:163–169. [DOI] [PubMed] [Google Scholar]
- 7. Hills NF, Graham RB, McLean L: Comparison of trunk muscle function between women with and without diastasis recti abdominis at 1 year postpartum. Phys Ther 2018;98:891–901. [DOI] [PubMed] [Google Scholar]
- 8. Brauman D: Diastasis recti: Clinical anatomy. Plast Reconstr Surg 2008;122:1564–1569. [DOI] [PubMed] [Google Scholar]
- 9. Emanuelsson P, Gunnarsson U, Dahlstrand U, et al. : Operative correction of abdominal rectus diastasis (ARD) reduces pain and improves abdominal wall muscle strength: A randomized, prospective trial comparing retromuscular mesh repair to double-row, self-retaining sutures. Surgery 2016;160(5):1367–1375. [DOI] [PubMed] [Google Scholar]
- 10. Mommers EHH, Ponten JEH, Al Omar AK, et al. : The general surgeon’s perspective of rectus diastasis. Surg Endosc 2017;31(12):4934–4949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Benjamin DR, Frawley HC, Shields N, et al. : Relationship between diastasis of the rectus abdominis muscle (DRAM) and musculoskeletal dysfunctions, pain and quality of life: A systematic review. Physiotherapy 2019;105(1):24–34. [DOI] [PubMed] [Google Scholar]
- 12. Thabet AA, Alshehri MA: Efficacy of deep core stability exercise program in postpartum women with diastasis recti abdominis: A randomised controlled trial. J Musculoskelet Neuronal Interact 2019;19:62–68. [PMC free article] [PubMed] [Google Scholar]
- 13. Emanuelsson P, Gunnarsson U, Strigard K, et al. : Early complications, pain, and quality of life after reconstructive surgery for abdominal rectus muscle diastasis: A 3-month follow-up. J Plast Reconstr Aesthet Surg 2014;67(8):1082–1088. [DOI] [PubMed] [Google Scholar]
- 14. Nahabedian MY: Management strategies for diastasis recti. Semin Plast Surg 2018;32(3):147–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Rosen CM, Ngaage LM, Rada EM, et al. : Surgical management of diastasis recti: A systematic review of insurance coverage in the United States. Ann Plast Surg 2019;83:475–480. [DOI] [PubMed] [Google Scholar]
- 16. CEBM: OCEBM levels of evidence 2019, https://www.cebm.net/2016/05/ocebm-levels-of-evidence/
- 17. Benjamin DR, van de Water AT, Peiris CL: Effects of exercise on diastasis of the rectus abdominis muscle in the antenatal and postnatal periods: A systematic review. Physiotherapy 2014;100(1):1–8. [DOI] [PubMed] [Google Scholar]
- 18. Mota P, Pascoal AG, Carita AI, et al. : Normal width of the inter-recti distance in pregnant and postpartum primiparous women. Musculoskelet Sci Pract 2018;35:34–37. [DOI] [PubMed] [Google Scholar]
- 19. Reinpold W, Kockerling F, Bittner R, et al. : Classification of rectus diastasis: A proposal by the German Hernia Society (DHG) and the International Endohernia Society (IEHS). Front Surg 2019;6:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Liaw LJ, Hsu MJ, Liao CF, et al. : The relationships between inter-recti distance measured by ultrasound imaging and abdominal muscle function in postpartum women: A 6-month follow-up study. J Orthop Sports Phys Ther 2011;41(6):435–443. [DOI] [PubMed] [Google Scholar]
- 21. Gunnarsson U, Stark B, Dahlstrand U, et al. : Correlation between abdominal rectus diastasis width and abdominal muscle strength. Dig Surg 2015;32(2):112–116. [DOI] [PubMed] [Google Scholar]
- 22. Van de Water AT, Benjamin DR: Measurement methods to assess diastasis of the rectus abdominis muscle (DRAM): A systematic review of their measurement properties and meta-analytic reliability generalisation. Man Ther 2016;21:41–53. [DOI] [PubMed] [Google Scholar]
- 23. Keshwani N, Mathur S, McLean L: Relationship between interrectus distance and symptom severity in women with diastasis recti abdominis in the early postpartum period. Phys Ther 2018;98:182–190. [DOI] [PubMed] [Google Scholar]
- 24. Mota P, Pascoal AG, Sancho F, et al. : Test-retest and intrarater reliability of 2-dimensional ultrasound measurements of distance between rectus abdominis in women. J Orthop Sports Phys Ther 2012;42(11):940–946. [DOI] [PubMed] [Google Scholar]
- 25. Boissonnault JS, Blaschak MJ: Incidence of diastasis recti abdominis during the childbearing year. Phys Ther 1988;68(7):1082–1086. [DOI] [PubMed] [Google Scholar]
- 26. Sperstad JB, Tennfjord MK, Hilde G, et al. : Diastasis recti abdominis during pregnancy and 12 months after childbirth: Prevalence, risk factors and report of lumbopelvic pain. Br J Sports Med 2016;50(17):1092–1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Hickey F, Finch JG, Khanna A: A systematic review on the outcomes of correction of diastasis of the recti. Hernia 2011;15(6):607–614. [DOI] [PubMed] [Google Scholar]
- 28. Mota P, Pascoal AG, Carita AI, et al. : The immediate effects on inter-rectus distance of abdominal crunch and drawing-in exercises during pregnancy and the postpartum period. J Orthop Sports Phys Ther 2015;45(10):781–788. [DOI] [PubMed] [Google Scholar]
- 29. Gluppe SL, Hilde G, Tennfjord MK, et al. : Effect of a postpartum training program on the prevalence of diastasis recti abdominis in postpartum primiparous women: A randomized controlled trial. Phys Ther 2018;98:260–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Kohler G, Fischer I, Kaltenbock R, et al. : Minimal invasive linea alba reconstruction for the treatment of umbilical and epigastric hernias with coexisting rectus abdominis diastasis. J Laparoendosc Adv Surg Tech A 2018;28(10):1223–1228. [DOI] [PubMed] [Google Scholar]
- 31. Emanuelsson P, Dahlstrand U, Stromsten U, et al. : Analysis of the abdominal musculo-aponeurotic anatomy in rectus diastasis: Comparison of CT scanning and preoperative clinical assessment with direct measurement intraoperatively. Hernia 2014;18(4):465–471. [DOI] [PubMed] [Google Scholar]
- 32. Van Uchelen JH, Kon M, Werker PM: The long-term durability of plication of the anterior rectus sheath assessed by ultrasonography. Plast Reconstr Surg 2001;107(6):1578–1584. [DOI] [PubMed] [Google Scholar]
- 33. Bellido Luque J, Bellido Luque A, Valdivia J, et al. : Totally endoscopic surgery on diastasis recti associated with midline hernias. Hernia 2015;19(3):493–501. [DOI] [PubMed] [Google Scholar]
- 34. Köckerling F, Botsinis MD, Rohde C, et al. : Endoscopic-assisted linea alba reconstruction plus mesh augmentation for treatment of umbilical and/or epigastric hernias and rectus abdominis diastasis: Early results. Front Surg 2016;3:27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Nahas FX, Ferreira LM, Augusto SM, et al. : Long-term follow-up of correction of rectus diastasis. Plast Reconstr Surg 2005;115(6):1736–1741; discussion 1742–1743. [DOI] [PubMed] [Google Scholar]
- 36. Shirah BH, Shirah HA: The effectiveness of polypropylene mesh in the open and laparoscopic repair of divarication of the rect. Med Imp Surg 2016;1:105. [Google Scholar]
- 37. Ducic I, Zakaria HM, Felder JM, 3rd, et al. : Abdominoplasty-related nerve injuries: Systematic review and treatment options. Aesthet Surg J 2014;34(2):284–297. [DOI] [PubMed] [Google Scholar]
- 38. Kockerling F, Botsinis MD, Rohde C, et al. Endoscopic-assisted linea alba reconstruction: New technique for treatment of symptomatic umbilical, trocar, and/or epigastric hernias with concomitant rectus abdominis diastasis. Eur Surg 2017;49(2):71–75. [DOI] [PMC free article] [PubMed] [Google Scholar]