Abstract
Introduction and importance
Delayed Splenic Rupture (DSR) is a rare but well-known presentation of Blunt Splenic Injury (BSI), most of which occur due to motor accidents, fall from height or direct blow to the left thorax or abdomen. Here we present a case of DSR five days after a trivial trauma.
Case presentation
A 37-year-old female presented with pain in the left-hypochondrium after an accidental bump against a furniture at home. Initially, it was a grade III splenic injury but upon arrival to our hospital from her hometown it had progressed to grade IV. Since the patient was hemodynamically stable, non-operative management (NOM) was chosen with close monitoring at the intensive care unit (ICU). However, the next morning, the patient deteriorated, showing signs of hemorrhagic shock, and a successful emergency splenectomy was done.
Clinical discussion
Over the last two decades, there has been an increasing inclination of surgeons towards NOM, even for high grade injury. NOM failure has been found to be associated with advancing age, high Injury Severity Score (ISS) or splenic injury. Some factors that improve the success of NOM are admission to ICU/floor, frequent monitoring of hemoglobin/hematocrit, vital signs, abdominal examination, and limiting heavy physical activity.
Conclusion
Clinicians should not limit the possibility of occurrence of DSR to only major traumatic events. It is imperative that a detailed history of major or trivial trauma in the preceding weeks be elicited for any patients presenting with abdominal pain.
Keywords: Abdominal injuries, Blunt splenic injury, Splenic rupture, Delayed splenic rupture, Trivial trauma, Case report
Highlights
-
•
Delayed Splenic Rupture is a rare but well reported presentation following blunt splenic injury.
-
•
Delayed Splenic Rupture can even occur following trivial trauma.
-
•
Clinicians must consider the entire clinical scenario to decide between operative or non-operative management.
-
•
A detailed history of major or minor trauma must be elicited for any patients with abdominal pain.
1. Introduction and importance
Delayed Splenic Rupture (DSR) was defined in 1907 by Baudet as a rupture of spleen 48h or later after injury [1]. This asymptomatic period is also known as the “latent period of Baudet”. Most of the DSR occur within a week after injury [2]. Over the past few decades, there has been an increasing shift from operative management (OM) to non-operative management (NOM) of blunt splenic injury (BSI) to preserve immunological functions of spleen and reduce the risk of surgery [3], [4].
Most of the reported cases of high-grade splenic injury and DSR were following major traumatic events, such as road traffic accidents, fall from height or contact sports [5]. Here we present a case of delayed splenic rupture five days following a trivial trauma to the left hypochondrium. We further reflect on the NOM failure of our case and lineate factors to improve NOM, even in high-grade splenic injuries.
2. Method
We report this case in line with the updated consensus-based surgical case report (SCARE) guidelines [6].
3. Case presentation
A 37-year-old female, homemaker by occupation, presented at our hospital in Kathmandu with pain in the left hypochondrium for past four days. The patient was initially treated in the local hospital near her home in Birgunj. The patient reported a trivial injury to her left hypochondrium by accidentally bumping into a furniture at home, with no other relevant medical and surgical history. During her treatment in Birgunj, she was hemodynamically stable and on investigation, Focused Assessment with Sonography for Trauma (FAST) scan showed minimal fluid collection on the day of injury. Transabdominal ultrasonography showed no hollow and solid organ injury. The patient was discharged with oral analgesics and an advice for a complete bed rest. As her pain worsened, the patient was advised for a CT scan later which showed Grade III splenic injury, minor injury to the left kidney and pancreatic tail (Fig. 1, Fig. 2). She then decided to pursue her further treatment in our hospital.
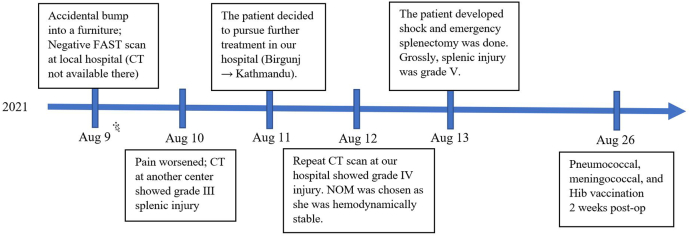
Fig. 1.
Post contrast transverse image showing large subcapsular hematoma (white arrow) involving more than 50% of splenic surface area.
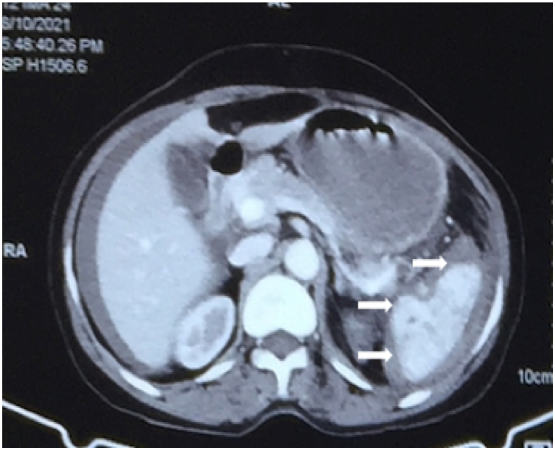
Fig. 2.
Post contrast transverse image showing multiple areas of intraparenchymal hematoma (white arrow).
On her arrival at our hospital, the patient appeared stable with a blood pressure of 110/78 mmHg and a heart rate of 60 beats/min. The patient's respiratory rate was 26 per minute, and she was afebrile. The initial abdominal examination showed minimal tenderness in the left hypochondrium with normal bowel sounds, but the remainder of the physical examination was unremarkable. Her laboratory investigation showed a hemoglobin (Hb) level of 11.6 g/dL with no obvious history of bleeding and a white blood cell count of 13.8 × 109 cells/L. Liver enzymes, electrolytes, blood glucose, blood urea nitrogen, creatinine, and amylase were essentially normal, and an electrocardiogram was unremarkable (Table 1).
Table 1.
Laboratory parameters on admission, during surgical intervention and post-op.
| S. no. | Laboratory test | Normal range | On admission | During laparotomy | Post-op |
|---|---|---|---|---|---|
| 1. | WBC count (×109 cells/L) | 3.5–9.5 | 9.0 | 7.1 | 9.0 |
| 2. | Neutrophil (%) | 50–70 | 73 | 79 | 83 |
| 3. | Lymphocyte (%) | 20–40 | 24 | 32 | 35 |
| 4. | Hemoglobin (g/dL) | 11.4/12–16 | 11.6 | 8.6 | 10.3 |
| 5. | Platelet count (×109 cells/L) | 125–350 | 180 | 170 | 240 |
| 6. | Hematocrit (%) | 36–48 | 42 | 44 | 35 |
| 7. | AST (U/L) | 5–45 | 123 | 127 | 149 |
| 8. | ALT (U/L) | 5–40 | 97 | 111 | 102 |
| 9. | Albumin (g/L) | 3.5–5.5 | 2.6 | 3.4 | 3.3 |
| 10. | Amylase (U/L) | 0–140 | 123 | 131 | 147 |
| 11. | Lipase (U/L) | 0–60 | 48 | 51 | 41 |
| 12. | Blood sodium level (mEq/L) | 135–145 | 139 | 137 | 145 |
| 13. | Blood potassium level (mEq/L) | 3.6–5.2 | 3.9 | 3.7 | 4.7 |
| 14. | Blood calcium level (mg/dL) | 8.5–10.5 | 6.7 | 6.9 | 7.7 |
| 15. | Triglyceride (mg/dL) | 40–150 | 210 | 200 | 219 |
| 16. | Blood urea nitrogen (mg/dL) | 8–20 | 17 | 20 | 21 |
| 17. | Creatinine (mg/dL) | 0.5–1.2 | 1.2 | 1.2 | 1.4 |
A repeat Contrast Enhanced Computed Tomography (CECT) scan confirmed that the patient had a Grade IV splenic injury with significant hemoperitoneum (Fig. 3). Since the patient was hemodynamically stable, NOM was chosen with close monitoring at the ICU. The next morning after admission (5th day post-trauma), she started deteriorating, showing signs of hemorrhagic shock; blood pressure of 80/60 mmHg, Hb of 8.6 g/dL. She complained of intense pain persisting even after a total of 20 mg of intravenous Morphine and 20 mg of intravenous Hyoscine.
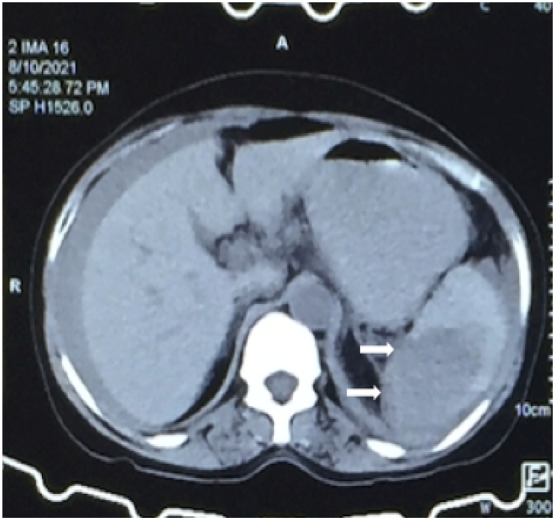
Fig. 3.
Post contrast showing multiple fragments of splenic parenchyma (arrows); few of the fragments are non-enhancing (avascular) with hemoperitoneum.
She was then taken to the operating room immediately for an emergency splenectomy. Intraoperatively, the splenic vein appeared to be injured and presented a clot in the hilum of spleen measuring 2 × 3 × 3 cm, which might have caused the delayed presentation of shock. Intraoperatively, she was transfused three pints of whole blood. On gross examination after resection, the spleen was confirmed to have a grade V injury (Fig. 4). We checked thoroughly to see if there was any injury to the tail of pancreas. Both the pancreas and left kidney were normal intraoperatively. The pathology report of our patient's spleen later documented an organ weighing 243 g and measuring 15 × 9 × 6 cm. This weight is within the reported range of normal. Approximately more than 50% of the splenic parenchyma contained dilated hemorrhage filled vascular areas. The patient's post-operative recovery was uneventful, and was discharged home one week after presentation. She was vaccinated with pneumococcal, meningococcal, and Hib vaccine 2 weeks post-splenectomy. The timeline of events and interventions is given below (Fig. 5). The patient is called for follow-up 3 months later.
Fig. 4.

Gross examination of spleen after resection.
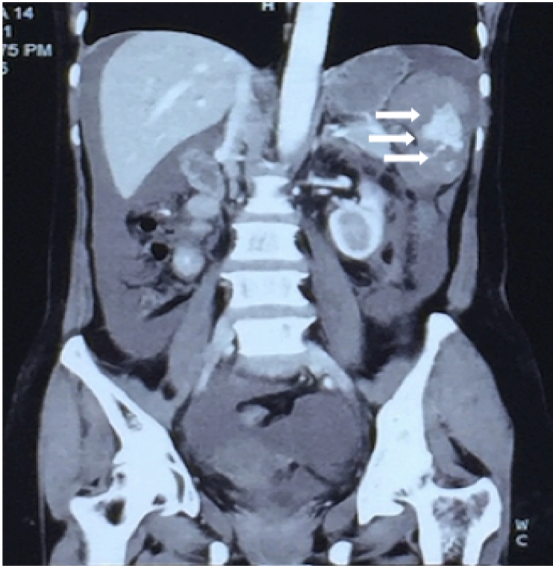
Fig. 5.
Timeline of events and interventions.
4. Clinical discussion
Spleen is the most commonly injured organ in blunt abdominal trauma [7]. Through much of the last century, BSI were predominantly managed operatively. However, advent of detailed diagnostic modalities to visualize the extent of injury, increased recognition of the immunological importance of the spleen, and the overwhelming success of NOM in pediatric population [4] has inclined surgeons towards NOM for adults as well.
In hemodynamically stable patients, abdominal CECT scan is the gold-standard to determine the grade of injury, associated injuries and evidence of active internal bleeding. The latter would require angioembolization or surgical exploration. The most widely used grading system for splenic injury is the American Association for the Surgery of Trauma (AAST) splenic injury scale, most recently revised in 2018 [8]. However, CT scans are known to underestimate injury grade, hence surgeons should not rely solely on the injury grade to decide on the management plan [9].
For hemodynamically unstable patients, a positive FAST scan is an absolute indication for emergency exploratory laparotomy. However, a negative FAST scan cannot reliably exclude intraabdominal hemorrhage [10]. Thus, clinicians must consider a Diagnostic Peritoneal Aspiration or Lavage (DPA/DPL) to rule it out.
Since the patient reported only a trivial injury with mild pain, a FAST scan was done at her low resource setting hometown hospital where CECT scan was not available. FAST scan has poor sensitivity in diagnosing solid organ injury [11], hence the extent of injury might not have been properly delineated. The repeat CECT scan at our hospital showed a Grade IV splenic injury. Since the patient's hemodynamics and vitals were stable, NOM was chosen. A retrospective analysis of BSI at a Level I trauma center by Haan et al. showed angioembolization had a 80% success rate of NOM for grade IV/V BSI [12]. Despite its increasing success, angioembolization is still not available in many institutions in Nepal, including ours.
However, on gross examination of the spleen after resection, a Grade V injury was confirmed. This shows the CT scans may underestimate the injury grade and cannot be considered as the sole determinant of treatment modality. Hence, a careful judgement of the entire clinical scenario must be done to decide between the OM or NOM.
The injury might have been exacerbated as the patient continued her normal daily activities, and even travelled over 100 kms by rough road to Kathmandu for further evaluation. A survey of Eastern Association for the Surgery of Trauma (EAST) members showed most surgeons advised their patients to resume full physical activity only after 6 weeks or 4 to 6 months depending upon the injury grade [13]. This highlights the importance of refraining from heavy physical activity after splenic injury, even in trivial injuries with limited radiographic findings and symptoms.
Through this case report, we want to emphasize that clinicians should keep an eye on the risk of Delayed Splenic Rupture even after trivial abdominal trauma. A systematic review by Olthof, et al. showed prognostic factors of NOM failure were age of 40 years or above, Injury Severity Score (ISS) of 25 or greater, and splenic injury grade of 3 or greater, as well as transfusion of 1 or more unit of packed red blood cells [14]. In order to improve the success of NOM, following factors must be considered by clinicians: admission to ICU/floor, frequency of monitoring of hemoglobin/hematocrit, vital signs, and abdominal examination, resumption of diet and ambulation, repeat imaging, and length of stay [15].
Few cases of apparently spontaneous rupture of a normal spleen have been reported [16]. However, history of minor trauma might have been overlooked in these cases. Hence, a detailed history of major or minor trauma in the preceding weeks must be elicited for any patients presenting with abdominal pain.
Although follow-up CT scan is not routine, proper discharge instructions and conditions for follow-up must be given to the patient.
5. Conclusion
Delayed splenic rupture is a rare case following major traumatic events and even rarer following trivial trauma. A clinician must consider the entire clinical scenario to decide between the OM or NOM, rather than the CT injury grade alone. In any patient presenting with abdominal pain, a detailed history of major or minor trauma in the preceding weeks must be sought for.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Ethical approval
The case report is exempt from ethical approval in our institution.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Guarantor
Sunil Basukala
Research registration number
Not applicable.
Provenance and peer review
Not commissioned, externally peer-reviewed.
CRediT authorship contribution statement
Sunil Basukala (SB), Bibek Karki (BK) = Conceptualization, Supervision.
Ayush Tamang (AT), Shriya Sharma (SS), Ujwal Bhusal (UB) = Writing - original draft.
SB, AT, BK = Visualization, Writing - review & editing.
All the authors read and approved the final manuscript.
Declaration of competing interest
All authors declare that they have no conflict of interest.
Acknowledgments
The authors wish to acknowledge the patient included in this report. We would also like to thank our head of department of surgery at Shree Birendra Hospital, Lt. Col. Dr. Narayan Thapa, for his guidance for this case report.
References
- 1.Baudet R. Ruptures de la rate. Med. Pract. 1907;3:565. [Google Scholar]
- 2.Clancy A.A., Tiruta C., Ashman D., Ball C.G., Kirkpatrick A.W. The song remains the same although the instruments are changing: complications following selective non-operative management of blunt spleen trauma: a retrospective review of patients at a level I trauma Centre from 1996 to 2007. J. Trauma Manag. Outcomes. 2012;6:4. doi: 10.1186/1752-2897-6-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brasel K.J., DeLisle C.M., Olson C.J., Borgstrom D.C. Splenic injury: trends in evaluation and management. J. Trauma Acute Care Surg. 1998;44 doi: 10.1097/00005373-199802000-00006. https://journals.lww.com/jtrauma/Fulltext/1998/02000/Splenic_Injury__Trends_in_Evaluation_and.6.aspx [DOI] [PubMed] [Google Scholar]
- 4.Peitzman A.B., Heil B., Rivera L., Federle M.B., Harbrecht B.G., Clancy K.D., Croce M., Enderson B.L., Morris J.A., Shatz D., Meredith J.W., Ochoa J.B., Fakhry S.M., Cushman J.G., Minei J.P., McCarthy M., Luchette F.A., Townsend R., Tinkoff G., Block E.F.J., Ross S., Frykberg E.R., Bell R.M., Davis F.I.I.I., Weireter L., Shapiro M.B., Kealey G.P., Rogers F., Jones L.M., Cone J.B., Dunham C.M., McAuley C.E. Blunt splenic injury in adults: multi-institutional study of the eastern Association for the Surgery of trauma. J. Trauma Acute Care Surg. 2000;49 doi: 10.1097/00005373-200008000-00002. https://journals.lww.com/jtrauma/Fulltext/2000/08000/Blunt_Splenic_Injury_in_Adults_.2.aspx [DOI] [PubMed] [Google Scholar]
- 5.Johnson N. Traumatic rupture of the spleen; a review of eighty-five cases. Aust. N. Z. J. Surg. 1954;24:112–124. doi: 10.1111/j.1445-2197.1954.tb05079.x. [DOI] [PubMed] [Google Scholar]
- 6.Agha R.A., Franchi T., Sohrabi C., Mathew G., for the SCARE Group The SCARE 2020 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 7.Cirocchi R., Boselli C., Corsi A., Farinella E., Listorti C., Trastulli S., Renzi C., Desiderio J., Santoro A., Cagini L., Parisi A., Redler A., Noya G., Fingerhut A. Is non-operative management safe and effective for all splenic blunt trauma? A systematic review. Crit. Care. 2013;17 doi: 10.1186/cc12868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kozar R.A., Crandall M., Shanmuganathan K., Zarzaur B.L., Coburn M., Cribari C., Kaups K., Schuster K., Tominaga G.T., the A.P.A. Committee Organ injury scaling 2018 update: spleen, liver, and kidney. J. Trauma Acute Care Surg. 2018;85 doi: 10.1097/TA.0000000000002058. https://journals.lww.com/jtrauma/Fulltext/2018/12000/Organ_injury_scaling_2018_update__Spleen,_liver,.12.aspx [DOI] [PubMed] [Google Scholar]
- 9.Shapiro M.J., Krausz C., Durham R.M., Mazuski J.E. Overuse of splenic scoring and computed tomographic scans. J. Trauma. 1999;47:651–658. doi: 10.1097/00005373-199910000-00008. [DOI] [PubMed] [Google Scholar]
- 10.Schnüriger B., Kilz J., Inderbitzin D., Schafer M., Kickuth R., Luginbühl M., Candinas D., Exadaktylos A.K., Zimmermann H. The accuracy of FAST in relation to grade of solid organ injuries: a retrospective analysis of 226 trauma patients with liver or splenic lesion. BMC Med. Imaging. 2009;9:3. doi: 10.1186/1471-2342-9-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kendall J.L., Faragher J., Hewitt G.J., Burcham G., Haukoos J.S. Emergency department ultrasound is not a sensitive detector of solid organ injury. West. J. Emerg. Med. 2009;10:1–5. [PMC free article] [PubMed] [Google Scholar]
- 12.Haan J.M., Biffl W., Knudson M.M., Davis K.A., Oka T., Majercik S., Dicker R., Marder S., Scalea T.M. Splenic embolization revisited: a multicenter review. J. Trauma. 2004;56:542–547. doi: 10.1097/01.ta.0000114069.73054.45. [DOI] [PubMed] [Google Scholar]
- 13.Fata P., Robinson L., Fakhry S.M. A survey of EAST member practices in blunt splenic injury: a description of current trends and opportunities for improvement. J. Trauma. 2005;59:832–836. doi: 10.1097/01.ta.0000187652.55405.73. [DOI] [PubMed] [Google Scholar]
- 14.Olthof D.C., Joosse P., van der Vlies C.H., de Haan R.J., Goslings J.C. Prognostic factors for failure of nonoperative management in adults with blunt splenic injury: a systematic review. J. Trauma Acute Care Surg. 2013;74:546–557. doi: 10.1097/ta.0b013e31827d5e3a. [DOI] [PubMed] [Google Scholar]
- 15.Cocanour C.S. Blunt splenic injury. Curr. Opin. Crit. Care. 2010;16:575–581. doi: 10.1097/MCC.0b013e3283402f3a. [DOI] [PubMed] [Google Scholar]
- 16.Renzulli P., Hostettler A., Schoepfer A.M., Gloor B., Candinas D. Systematic review of atraumatic splenic rupture. Br. J. Surg. 2009;96:1114–1121. doi: 10.1002/bjs.6737. [DOI] [PubMed] [Google Scholar]