Abstract
Aim
Chest compression depth (CCD) in cardiopulmonary resuscitation is important. However, lightweight rescuers have difficulty achieving an appropriate depth. Chest compression force (CCFORCE) can be increased by placing the arms at 100° to the patient’s frontal plane. In a simulation manikin study, we compared the CCD at 90° and 100° among lightweight Asian females and hypothesized that the CCD would be greater when the arms were placed at 100°.
Methods
We included 35 lightweight female students from Shimane University who performed compressions 30 times each at 90° and 100°. The CCFORCE and CCD and the residual force on the chest wall during decompression for each chest compression were compared using CPRmeter-2.
Results
Of the 35 participants, 3 were excluded because their angles deviated from the prescribed angle. Thirty-two participants were categorized according to CCD at 90°: ≤40 mm (group 1), 41–49 mm (group 2), and ≥ 50 mm (group 3). The overall mean CCD increased from 90° to 100° (44.3 ± 8.2 mm vs. 48.1 ± 7.2 mm; p < 0.05). The mean CCD changes between 90° and 100° were 34.4 ± 4.7 mm vs. 42.9 ± 4.8 mm (p < 0.05) in group 1, 44.9 ± 2.5 mm vs. 47.0 ± 4.2 mm (p = 0.17) in group 2, and 53.0 ± 2.7 mm vs. 55.4 ± 5.6 mm (p < 0.05) in group 3. The residual force was greater when the chest compression angle was 100°.
Conclusion
CCD can be increased for lightweight rescuers when using a forward leaning position of 100° to the frontal plane of the patient. Further research is required to obtain more realistic situations.
Keywords: Cardiopulmonary resuscitation, Chest compression angle, Depth, Lightweight
Abbreviations: CPR, cardiopulmonary resuscitation; CCD, chest compression depth; CCA, chest compression angle; CCFORCE, chest compression force
Introduction
In 2000, the American Heart Association and the International Liaison Committee on Resuscitation jointly published the Guidelines 2000 (G2000),1 which has become the standard for cardiopulmonary resuscitation (CPR) worldwide. These standards have been revised based on scientific evidence, including prescribed chest compression depth (CCD). In G2000, the prescribed CCD was 35–50 mm, but in G2005, it was modified to 40–50 mm.2 In G2010, it was modified to ≥ 50 mm3., 4. and in G2015 and G2020, to 50–60 mm.5 A high CCD has been associated with survival outcomes, with a depth of ≥ 50 mm increasing the rate of survival after resuscitation.6., 7. In particular, with a CCD of ≤ 40 mm, the success rate of defibrillation shocks decreases considerably, impacting the survival rate after resuscitation.8 However, some medical professionals still perform chest compressions at shallow depths.9 While teaching CPR to adults, we observed that lightweight individuals, particularly women, had difficulty achieving an adequate CCD. Previous reports have also highlighted that females weighing < 56 kg had inadequate CCDs.10 Furthermore, the CCD remained shallow even when lightweight rescuers adopted the correct posture. Given this, many researchers have concluded that underweight rescuers require additional attention and specialized training.11., 12.
To increase the CCD achieved by lightweight rescuers, we observed their postures during chest compression. Bucki et al. reported that increasing knee flexion above 90° during chest compressions increased pressure.13 When studying residents’ shoulder positions, Mayrand et al. found that compressions at < 90° resulted in significantly shallow depths.14 Therefore, these studies highlight the effectiveness of focusing on posture in increasing the CCD. However, the optimum angle is unknown, and there have been no reports comparing the effectiveness of chest compressions at different angles. When performing chest compressions, the rescuer’s shoulder acts as the point of effort, the palm placed on the sternum acts as the point of load, and the intersection between the frontal plane of the manikin/patient chest and the extension line of the rescuer’s shoulders and hips acts as the fulcrum point. According to the leverage principle, when a certain amount of force is applied to the point of effort, longer distances between the point of effort and the fulcrum lead to an increase in the force applied to the point of action. Therefore, when the rescuer’s weight is applied to the point of effort, the force of chest compressions can be increased by adopting a forward-leaning posture that places the point of effort anteriorly to the position of the palms, which act as the point of load. Therefore, we attempted to compare the CCD at 90° and 100° in lightweight Asian females. We hypothesized that the CCD would be greater at 100° than at 90° in a simulated cardiac arrest model.
Methods
This study included 35 female students from Shimane University with a standing height of ≤ 165 cm who were in their fifth and sixth year of study at the Department of Medicine and had received basic life support training within a year before participating in this study. The participants performed 30 chest compressions at 90° and 100° from the frontal plane of the chest. Thirty chest compressions were performed at each angle, with the frequency adjusted to that of a metronome set at 110 beats per minute. The participants were classified into three groups according to the depth of the chest compressions at 90°.
How chest compressions were performed
Chest compressions were performed on the floor using a CPR training manikin (Resusci Anne First Aid; Laerdal Medical, Stavanger, Norway), which simulates chest compressions in adults. The manikin’s standard compression spring was used.
Measurement of the CCA
The CCA was measured using Kinect V2 (Microsoft, Redmond, WA), a non-contact motion-capture device that measured each joint’s coordinates in real time and digitizes and converts coordinates into numerical values. In contrast to optical motion-capture systems, this system does not require multiple cameras or reflective markers attached to the body. An image of a protractor was projected onto a wall to set CCAs at 90° and 100° (Fig. 1). Participants were given 5 min of practice time to achieve 90° and 100°. The angle was adjusted using a protractor. After performing chest compressions, the mean CCA used in 30 compressions was calculated based on the angles measured using Kinect. The angle was considered to be 90° when the measured mean angle was 90° ± 3° and 100° when the measured mean angle was 100° ± 3°. Participants whose CCAs deviated from these ranges in either case were excluded from the analysis.
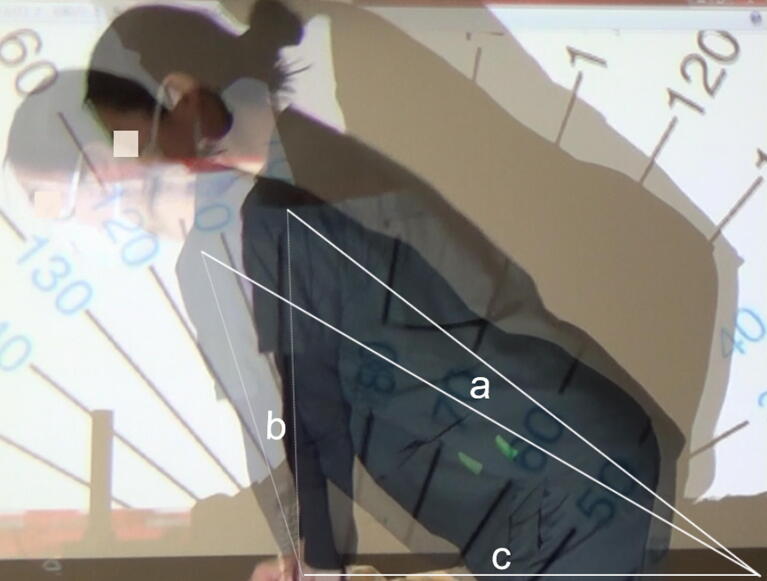
Fig. 1.
The figure shows the protractor image projected onto a wall and chest compressions are performed at the projected angle. a: The distance between the participant’s shoulders and the point of intersection between the extension line of the participant’s hips and the frontal plane of the manikin’s chest. b: The distance between the participant’s shoulders and the location of the participant’s palms placed on the manikin’s chest. c: The distance between the participant’s palms placed on the manikin’s chest and distance “a”.
Measurement of the CCFORCE and CCD
The CCFORCE and CCD for each chest compression were measured using CPRmeter-2 (Laerdal Medical) placed on the manikin’s chest.15 CPRmeter-2 records the CCFORCE and CCD for each compression and the residual force on the chest wall during decompression. The recorded data can be viewed on a smartphone using the downloaded app. The data can also be output in the CSV format. This study was conducted to compare CCDs at two chest compression angles. Therefore, no feedback on the quality of chest compressions was provided during the experiments.
Measurement of the distances (lengths) of the three sides of a triangle during chest compressions at 90° and 100°
To compare the actual and mathematical increase in the elongation of distance “a,” we measured the three sides of the triangle. Based on the CCA determined using Kinect, one participant who performed chest compressions with the most accurate angle was selected. Based on videos captured using Kinect during chest compressions, the distances (lengths) of the three sides of the triangle connecting the participant’s shoulders, palms, and the frontal plane of the manikin’s chest were measured. The distance between the participant’s shoulders and the point of intersection between the extension line of the participants’ hips and the frontal plane of the manikin’s chest was named distance “a,” while the distance between the participant’s shoulders and the location of the participant’s palms placed on the manikin’s chest was referred to as distance “b.” Lastly, distance “c” was defined as the distance between the participant’s palms placed on the manikin’s chest and distance “a” (Fig. 1).
Preliminary calculation
In conventional chest compression, a right triangle is formed following the Pythagorean theorem: . In a forward-leaning posture, which displaces the point of effort anteriorly, the CCA is obtuse; therefore, in accordance with the triangle cosine theorem, the formula is revised to: a2 = b2 + c2 − 2bcCosθ. When Cos100 = −0.17 is used in the formula a2 = b2 + c2 − 2bcCos100, the equation changes as follows: , and distance “a” will be longer by than the right triangle.
According to the type 2 leverage principle, the force applied to the point of action depends on the distance from the fulcrum to the point of force if the distance from the fulcrum to the point of action is similar (Fig. 2). Furthermore, the CCFORCE increases with distance “a.” However, the force at the point of action will cause a reduction of cos10 = 0.98 times when the pressure is applied at 100° to the chest. Therefore, the compression force by a CCA of 100° is enhanced by × 0.98.
Fig. 2.
This figure shows chest compressions with a CPRmeter-2. According to the leverage principle, when a certain amount of force is applied to the point of effort, longer distances between the point of effort and the fulcrum lead to an increase in the force applied to the point of action. : The input force to the effort point. a < á. . .
Measurement of the residual force on the chest wall during recoil
The residual force on the chest wall during recoil was measured using CPRmeter-2. Recoil refers to complete enlargement of the thorax after each chest compression. This ensures that venous blood is pumped back to the heart and helps prepare the systolic output of the following chest compressions. Chest compressions were performed 30 times at 90° and 100°, and the residual force during recoil was measured after each compression.
Statistical analysis
Variables are expressed as mean ± standard deviation. Data were analyzed using the Shapiro–Wilk test to verify the normality of the distribution. A two-sided Student’s t-test was used when the data were normally distributed; otherwise, the Wilcoxon signed-rank test was used to compare CPR performance at 90° and 100°. The relationship between CCFORCE and CCD was evaluated using the Pearson correlation coefficient, and their association was evaluated using univariate linear regression analysis. All statistical analyses were performed using JMP version 14 (SAS Institute, Cary, NC). Statistical significance was set at p < 0.05.
Ethics
The purpose, methods, and ethical considerations of the study were explained to the participants, and written consent was obtained. The explanations specified the following: 1) the data obtained from this study would be managed using coded numbers to prevent identification of the individuals and would not be used for any purpose other than this study; 2) this study was not aimed at evaluating individual skills; and 3) participation was voluntary and participants could withdraw at any time during the study. This study was not considered a human research study by the Shimane University Faculty of Medicine Ethics Committee.
Results
Of the 35 participants, 3 were excluded from analysis because their compression angles deviated from the prescribed angle. The compression angles of the three participants were 90°±3° (considered to be 90°). However, they were excluded because the angles did not reach a range of 100°. The remaining participants were classified into three groups: those who achieved a CCD of ≤ 40 mm at a chest compression angle (CCA) of 90° were assigned to group 1, those who achieved a CCD of 41–49 mm were assigned to group 2, and those who achieved a CCD of ≥ 50 mm were assigned to group 3 (Fig. 3).
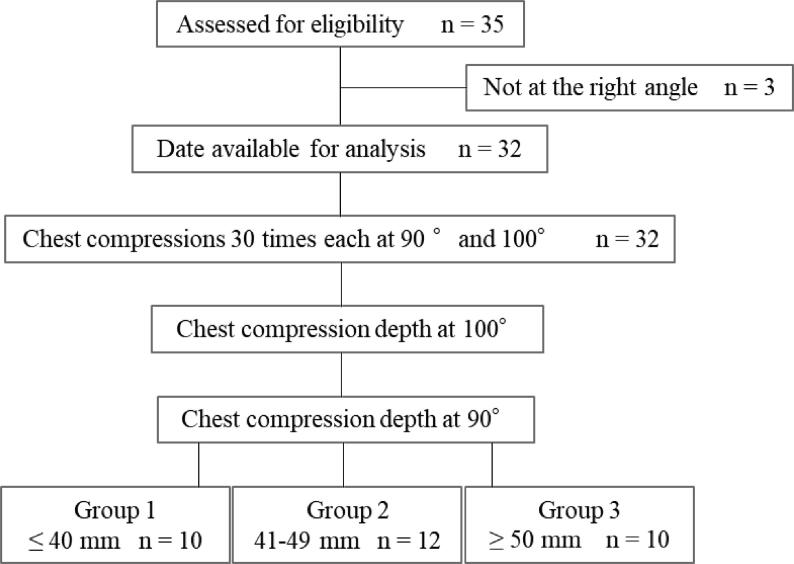
Fig. 3.
Flow diagram of the study subjects. Among the 35 participants, 3 were excluded because their angles deviated from the prescribed angle. Thirty participants were categorized according to the chest compression depth (CCD) at 90°: ≤40 mm (group 1), 41–49 mm (group 2), and ≥ 50 mm (group 3).
Characteristics of the participants
The mean standing height, body weight, and body mass index (BMI) were not significantly different between groups (Table 1).
Table 1.
Comparison of body types and classification of groups according to compression depth.
| All | Group 1 | Group 2 | Group 3 | |
|---|---|---|---|---|
| N | 32 | 10 | 12 | 10 |
| Height (cm) | 157 ± 5 | 156 ± 4 | 156 ± 4 | 158 ± 5 |
| Weight (kg) | 50.0 ± 4.0 | 48.6 ± 3.2 | 49.4 ± 3.9 | 51.1 ± 4.0 |
| BMI (kg/m2) | 20.3 ± 1.4 | 19.9 ± 1.9 | 20.2 ± 1.3 | 20.6 ± 1.5 |
The mean height, body weight, and body mass index (BMI) were not significantly different between the groups.
Changes in CCFORCE due to changes from a CCA of 90° to 100°
With a CCA of 90° and 100°, the 32 participants showed CCFORCEs of 45.7 ± 7.5 kgf and 49.5 ± 7.2 kgf, respectively (p < 0.05). CCFORCE increased with CCA in 28 participants. On average, CCFORCE increased by 5.3 kgf, with a maximum increase of 51%. In group 1, the CCFORCEs at a CCA of 90° and 100° were 37.0 ± 5.5 kgf and 44.0 ± 3.6 kgf, respectively (p < 0.05); 47.3 ± 3.2 kgf and 48.5 ± 4.7 kgf in group 2, respectively (p = 0.45); and 52.1 ± 3.9 kgf and 56.4 ± 6.5 kgf in group 3, respectively (p < 0.05).
Changes in the CCD according to the CCA (90° and 100°)
Overall, the CCD was greater at 100° than at 90° (48.1 ± 7.2 mm vs. 44.3 ± 8.2 mm; p < 0.05). An increase in the CCD was observed in 28 participants, with an average increase of 5.5 mm and a maximum increase of 69%. Fig. 4 presents the changes in the CCD in each group. In groups 1 and 3, the CCD was deeper at 100° than at 90°. In group 2, the CCD was not statistically different between 100° and 90°, but the depth tended to be deeper at a CCA of 100° than at 90° (47.0 ± 4.2 mm vs. 44.9 ± 2.5 mm; p = 0.17). At a CCA of 100°, 6 of the 22 participants in groups 1 and 2 achieved a CCD of 50 mm.
Fig. 4.
Changes in chest compression depth according to chest compression. CCA: chest compression angle.
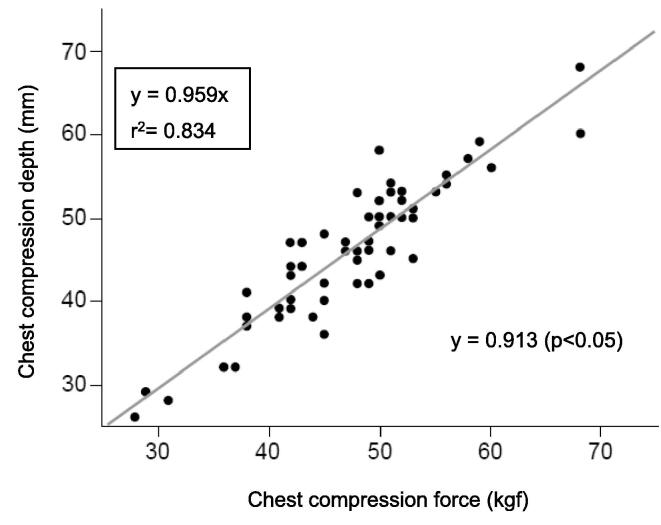
Relationship between the CCFORCE and CCD at 90° and 100°
In a regression equation using CCFORCE as the explanatory variable and CCD as the objective variable, the following formula was derived: y = 0.959x + 0.579 (r = 0.913, p < 0.05), showing a strong correlation between the CCFORCE and CCD in the 32 participants (Fig. 5).
Fig. 5.
Correlation between compression force and depth (n = 64).
Measurement of distances on the three sides of a triangle (shoulder–hip–palms) at 90° and 100°
To compare the actual and the mathematical increase in the CCFORCE due to the elongation of distance “a,” we also measured the three sides of the triangle of the participant who performed chest compressions at the most accurate angle. Distance “a” was 165 mm at 90° and 183 mm at 100°, distance “b” was 110 mm at 90° and 100°, and distance “c” was 120 mm at 90° and 100°.
Changes in the residual force on the chest wall during recoil at 90° and 100°
The residual force on the chest wall during recoil was also measured. Based on the results of the 32 participants, the measured values were 1.9 ± 2.2 kgf and 3.6 ± 3.8 kgf at 90° and 100°, respectively (p < 0.05). In group 1, the residual force at 90° and 100° was 2.5 ± 2.0 kgf and 4.7 ± 3.8 kgf, respectively (p < 0.05). In group 2, the residual force at 90° and 100° was 2.3 ± 2.1 kgf and 4.3 ± 3.2 kgf, respectively (p < 0.05). In group 3, the residual force at 90° and 100° was 0.5 ± 1.0 kgf and 0.7 ± 1.0 kgf, respectively (p < 0.05).
Discussion
This study showed that the CCD was deeper at a CCA of 100° than at 90° in lightweight females. Among them, participants whose CCD was ≤ 40 mm at a CCA of 90° showed a significant increase in CCD at a CCA of 100°. The posture of the rescuer recommended by the American Heart Association guidelines is with the shoulders directly above the compression point and the rescuer's arms forming a 90° angle to the patient's chest. Ten study participants achieved a G2020-recommended CCD of 50–60 mm. However, in the other 22 participants (69%), the CCD was < 50 mm. A rescuer’s small build is associated with a shallow CCD.16., 17. Furthermore, the CCD and body weight are strongly positively correlated, and the following regression equation expresses the predicted CCD: expected CCD (mm) = 0.46 × body weight + 17.59.18 Given this formula, previous studies have indicated that a body weight of at least 70.5 kg is necessary for a CCD of ≥ 50 mm. In our study, the 32 participants had a mean body weight of 50 ± 4 kg; after inputting this into the abovementioned regression equation, the expected CCD would only be 40.6 mm. For the 22 participants with a CCD of < 50 mm, the mean CCD was 40.3 mm, which is consistent with the prediction by the regression equation. In a previous study, individuals from North America had the heaviest average body weight at 80.7 kg, whereas individuals from Asia had the lightest average body weight at 57.7 kg.19 Specifically, Japanese females in their twenties have an average height of 158 cm and an average body weight of 51 kg,20 making it challenging to achieve a sufficient CCD using the guideline-recommended posture.
To increase the CCD of lightweight rescuers, we observed the posture of the chest compression and applied the lever principle. This anterior leaning position leads to an increase in distance “a” and an increase in the CCFORCE. The CCD and CCFORCE are strongly correlated; thus, an increase in the CCFORCE increases the CCD.
To examine the actual magnitude of the elongation of distance “a”, data from one participant at a CCA of 90° and 100° were compared. At a distance “b” of 110 mm and distance “c” of 120 mm, the theoretical length of distance “a” was 162 mm at 90° and 176 mm at 100°. The actual measured values of “a” were 165 mm and 183 mm at 90° and 100°, respectively, with the latter being 1.1 times longer, close to the theoretical value of 1.09 times. Furthermore, the rate of change in the CCD between a CCA of 90° and 100° was examined. At 100°, the CCDs were 42.9 mm, 47.0 mm, and 55.4 mm in groups 1, 2, and 3, respectively. The rates of change were 1.24-fold, 1.04-fold, and 1.05-fold in groups 1, 2, and 3 (respectively), showing that the CCD increased 1.11-fold in all groups. In particular, the changes observed in group 1 exceeded the predicted rate of increase based on the triangular cosine theorem and the leverage principle. Group 3 was able to achieve a CCD of 50 mm at 90°. Therefore, they may have adjusted their CCFORCE so that the CCD would not exceed 60 mm. At 90°, 10 participants could only achieve a CCD of ≤ 40 mm, but at 100°, only 3 participants were not able to achieve a CCD of ≤ 40 mm, with an average increase in CCD of 8.5 mm. This suggests that an increased CCD is associated with an increased distance “a” and the resultant CCFORCE.
To date, several ways have been proposed to increase chest compression depth; leg-foot CPR21., 22. and straddle CPR.23 We believe that the advantage of leg-foot CPR is that the rescuer’s body weight is fully utilized. However, it is difficult to control the force to achieve a depth of 5–6 cm. Straddle chest compression is an alternative technique that can be used in confined spaces. However, straddle CPR is difficult to achieve for larger patients, especially for small lightweight rescuers. We believe that our method is a better alternative to leg-foot CPR and straddle CPR for these reasons. In this study, we devised a method for lightweight rescuers to perform deep sternum compression. However, if the CCA is too large, the recoil may be insufficient. Our study showed that the residual force was higher at a CCA of 100° than at a CCA of 90° in all groups. However, we do not know which is more harmful to the patient, allowing a shallow compression depth of less than 40 mm or an increase in the residual force.
Our study has three main limitations. First, this was a simulation model study, and how this applies to real patients remains unclear. Second, chest compression at a CCA of 100° produced a horizontal force, which may lead to rib fractures. Therefore, additional research is needed on the association between horizontal force and the risk of rib fractures. Third, in group 1, the mean CCD was lower than the recommended value of 50 mm in most participants. However, 7 of the 10 participants with an initial CCD of ≤ 40 mm achieved a great depth at a CCA of 100°. Any improvement in CCD will increase the chances of successful defibrillation.
Conclusion
By setting the CCA at 100°, the CCD was significantly increased in lightweight rescuers in this simulation study. However, the depth was still less than the guideline-recommended depth. Further research using more realistic scenarios (perhaps in combination with feedback systems), longer periods of compression, and clinically relevant models is needed.
Funding source
This work was supported by JSPS KAKENHI (grant number 17K08917).
CRediT authorship contribution statement
Nao Sato: Conceptualization, Methodology, Formal analysis, Writing – original draft, Visualization. Kenji Karino: Conceptualization, Methodology, Project administration, Funding acquisition. Makoto Hirose: Software, Validation. Satoru Okamoto: Conceptualization. Tomoko Osaka: Conceptualization, Software. Hatsue Matsumura: Investigation, Data curation, Methodology. Yoshiaki Iwashita: Writing – review & editing, Visualization, Supervision.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.American Heart Association: Guidelines 2000 for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Part 3. Circulation 2000;102(suppI):122–159.
- 2.Proceedings of the 2005 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendation. Resuscitation 2005;67:157–341. [PubMed]
- 3.Koster R.W., Sayre M.R., Botha M. Part 5: Adult basic life support: 2010 International consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Resuscitation. 2010;81(suppl):e48–e70. doi: 10.1016/j.resuscitation.2010.08.005. [DOI] [PubMed] [Google Scholar]
- 4.Koster R.W., Baubin M.A., Bossaert L.L. European resuscitation council guidelines for resuscitation 2010 section 2. Adult basic life support and use of automated external defibrillators. Resuscitation. 2010;81(10):1277–1292. doi: 10.1016/j.resuscitation.2010.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Perkins G.D., Handley A.J., Koster R.W. Adult basic life support and automated external defibrillation section Collaborators. European resuscitation council guidelines for resuscitation 2015: Section 2. Adult basic life support and automated external defibrillation. Resuscitation. 2015;95:81–99. doi: 10.1016/j.resuscitation.2015.07.015. [DOI] [PubMed] [Google Scholar]
- 6.Stiell I.G., Brown S.P., Christenson J. What is the role of chest compression depth during out of-hospital cardiac arrest resuscitation? Crit Care Med. 2012;40(4):1192–1198. doi: 10.1097/CCM.0b013e31823bc8bb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vadeboncoeur T., Stolz U., Panchal A. Chest compression depth and survival in out-of-hospital cardiac arrest. Resuscitation. 2014;85(2):182–188. doi: 10.1016/j.resuscitation.2013.10.002. [DOI] [PubMed] [Google Scholar]
- 8.Edelson D.P., Abella B.S., Kramer-Johansen J. Effects of compression depth and pre-shock pauses predict defibrillation failure during cardiac arrest. Resuscitation. 2006;71(2):137–145. doi: 10.1016/j.resuscitation.2006.04.008. [DOI] [PubMed] [Google Scholar]
- 9.Wik L., Kramer-Johansen J., Myklebust H. Quality of cardiopulmonary resuscitation during out-of-hospital cardiac arrest. JAMA. 2005;293(3):299–304. doi: 10.1001/jama.293.3.299. [DOI] [PubMed] [Google Scholar]
- 10.Asta K., Kestutis S., Milda D. Can lightweight rescuers adequately perform CPR according to 2010 resuscitation guideline requirements? Emerg Med J. 2013;30(2):159–160. doi: 10.1136/emermed-2011-200634. [DOI] [PubMed] [Google Scholar]
- 11.Asta K., Andrius P., Kestutis S. Magical manoeuvre: a 5-s instructor’s intervention helps lightweight female rescuers achieve the required chest compression depth. Eur J Emerg Med. 2014;21(6):424–428. doi: 10.1097/mej.0000000000000107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Roh Y.S., Lim E.J. Factors influencing quality of chest compression depth in nursing students. Int J Nurs Pract. 2013;19(6):591–595. doi: 10.1111/ijn.12105. [DOI] [PubMed] [Google Scholar]
- 13.Bucki B., Waniczek D., Michnik R. The assessment of the kinematics of the rescuer in continuous chest compression during a 10-min simulation of cardiopulmonary resuscitation. Eur J Med Res. 2019;24(1):9. doi: 10.1186/s40001-019-0369-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mayrand K., Fischer E., Ten Eyck R. A Simulation-based Randomized Controlled Study of Factors Influencing Chest Compression Depth. West J Emerg Med. 2015;16(7):1135–1140. doi: 10.5811/westjem.2015.9.28167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Laerdal Medical. CPR meter 2 measure to improve, Laerdal Med-help save lives. Available: https://laerdal.com/ca/products/simulation-training/resuscitation-training/cprmeter-2/ [Accessed 23 July 23 2021].
- 16.Contri E., Cornara S., Somaschini A. Complete chest recoil during laypersons' CPR: is it a matter of weight? Am J Emerg Med. 2017;35(9):1266–1268. doi: 10.1016/j.ajem.2017.03.060. [DOI] [PubMed] [Google Scholar]
- 17.Hasegawa T., Daikoku R., Saito S., Saito Y. Relationship between weight of rescuer and quality of chest compression during cardiopulmonary resuscitation. J Physiol Anthrop. 2014;33(1)16 doi: 10.1186/1880-6805-33-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Oh J.H., Kim C.H. Relationship between chest compression depth and novice rescuer body weight during cardiopulmonary resuscitation. Am J Emerg Med. 2016;34(12):2411–2413. doi: 10.1016/j.ajem.2016.09.006. [DOI] [PubMed] [Google Scholar]
- 19.Walpole S.C., Prieto-Merino D., Edwards P. The weight of nations: an estimation of adult human biomass. BMC Public Health. 2012;12:439. doi: 10.1186/1471-2458-12-439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.National Health and Nutrition Survey 2017. Portal Site of Official Statistics of Japan. https://www.e-stat.go.jp/stat-search/ files? page =1&toukei=00450171&tstat=000001041744. [Accessed 15 July 23 2020].
- 21.Yoshiaki T., Takeji S., Misaki O. The potential of leg-foot chest compression as an alternative to conventional hands-on compression during cardiopulmonary resuscitation. Hong Kong Journal of Emerg Med. 2019;26(2):106–110. doi: 10.1177/1024907918790068. [DOI] [Google Scholar]
- 22.Otero-Agra M., Santiago-Urgal N., Hermo-Gonzalo M.T. CPR by foot. An alternative in special circumstances? A randomized simulation study. Am J Emerg Med. 2021;43:1–6. doi: 10.1016/j.ajem.2020.12.086. [DOI] [PubMed] [Google Scholar]
- 23.Handley A.J., Handley J.A. Performing chest compressions in a confined space. Resuscitation. 2004;61:55–61. doi: 10.1016/j.resuscitation.2003.11.012. [DOI] [PubMed] [Google Scholar]