Abstract
Background
The burden of urological diseases is rising as the worldwide population ages. Although specialist urological provision is needed, a large proportion of these conditions will be managed in primary care. The importance of including urology in medical education currently remains unclear.
Objective
To provide recommendations on undergraduate medical education for urology in Europe.
Design, setting, and participants
A three-round Delphi process to reach consensus on standardising the undergraduate urology curriculum in Europe was endorsed by the European School of Urology.
Outcome measurements and statistical analysis
The levels of agreement were set using a nine-point scale according to the GRADE grid: 1–3, disagree; 4–6, uncertain; and 7–9, agree. Consensus was defined as at least 70% of the participants scoring within the same 3-point grouping.
Results and limitations
Overall, consensus was reached for 20 of 34 statements (70.5%) across the three Delphi rounds, with agreement for 75% (n = 15) and disagreement for 25% (n = 5). The following main points were agreed. Urological teaching should be introduced before year 5 of medical school, with at least 20 h of theoretical activities and at least 30 h of practical activities. Urology should be taught as a stand-alone subject rather than combined with another surgical specialty or a nephrology programme. The participants agreed that urology should be taught according to symptoms. A urology programme should include the anatomy and physiology of the urinary tract, and students should know how to clinically assess a urological patient.
Conclusions
Our recommended urology pathway will allow European medical schools to provide a more comprehensive undergraduate urology curriculum. It will also help to improve and maintain standards of urology undergraduate teaching across Europe.
Patient summary
Our survey showed that urology in universities should have, at minimum, time for theoretical and practical activities and should be taught as a stand-alone subject on the basis of symptoms. Students should give feedback to facilitate constant improvement and evolution of the teaching programme.
Keywords: Delphi consensus, Education, Undergraduate medical education, Urology
Take Home Message
Our survey shows that urology teaching in universities should have, at minimum, time for theoretical and practical activities and should be taught as a stand-alone subject on the basis of symptomatology. Students should give feedback to facilitate constant improvement and evolution of the teaching programme.
1. Introduction
The burden of urological diseases is increasing as the worldwide population ages. This rise is occurring across both oncological and nononcological services [1]. Although specialist urological provision is needed, a large proportion of these conditions will be managed in primary care. According to recent data, 10% of general practitioner consultations are for urological problems and 30% of human cancers are urological [2], [3]. Hence, it is extremely important that basic urological education is delivered in medical schools and that management of common urological conditions is covered via tutorials, lectures, hands-on training (HOT), and direct patient contact. This would ensure that all medical students are familiar with the presentation and safe initial management of acute and common urological conditions.
Although considered as an important subspecialty of surgical training for undergraduate medical education (UME), only 15% of medical students would consider pursuing a career in urology. There has also been a recent decline in overall competition to enter urological training, with the overall rate of intake into higher surgical training (HST) in urology now the lowest among all surgical specialties [4], [5], [6], [7]. It is plausible that the falling interest in urology at HST level is because of a lack of adequate exposure to and training in urology during UME, as the latter significantly influences the interests and career choices of the future.
A recent snapshot survey by the European School of Urology (ESU) on UME in urology showed huge heterogeneity in urology teaching across medical schools in Europe in terms of the style, content, timing, and duration of teaching as part of the curriculum [6]. Career choices are shaped by clinical exposure and role models during formative years, and a lack of exposure to urology and presumptive lifestyle barriers can lead to further alienation of junior doctors away from urology. With a comprehensive structured urology curriculum, clinical exposure, HOT, and practical skills training, this perception and trend could be reversed and urology could become more appealing again [8], [9].
The importance of the inclusion of urology in UME currently remains unclear and there is wide variation in teaching across medical schools in Europe. Considering that medical student exposure and experience in urology differ between European countries and institutions, and in the absence of any comprehensive study assessing urology-specific education among European universities, we performed a three-round Delphi process with the aim of reaching consensus and providing recommendations on undergraduate education in urology in Europe.
2. Materials and methods
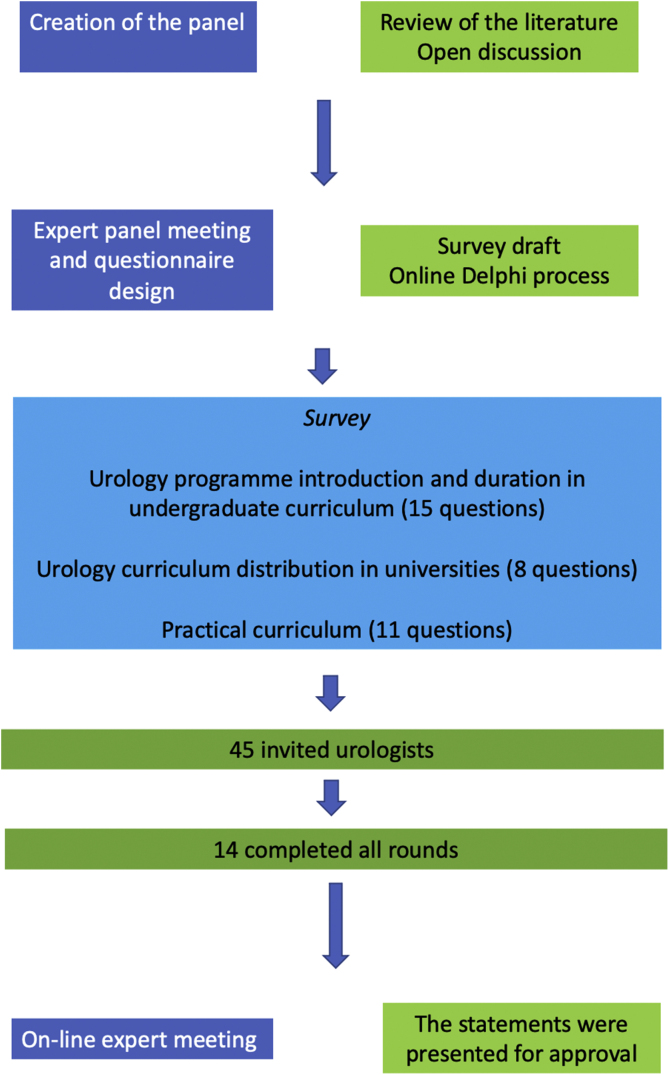
In 2020, a Delphi process to reach consensus on standardising the undergraduate urology curriculum in Europe was endorsed by the ESU. The project was carried out in three phases:
-
(1)
A steering group (J.G.R., M.R.S., B.S., P.Z.) was formed to review the literature and summarise the current evidence on urology UME in Europe.
-
(2)
A larger expert panel (J.G.R., L.H., J.P., I.P., M.R.S., B.S., P.Z.) was convened and discussed important aspects of UME on the basis of the current evidence and personal experience. Following open discussion, a survey was created with input from the panel members.
-
(3)
Panel-based consensus was determined using an online Delphi process to formulate consensus statements and provide recommendations for future UME in urology.
2.1. Phase I: expert panel meeting and questionnaire design
An advisory panel comprising key opinion leaders with a special interest in UME and training in urology was formed (J.G.R., E.L., L.H., J.P., I.P., M.R.S., B.S., H.V.P., P.Z.). The meeting included presentations on the subject matter, clarifications on terminology, and findings from a review of the literature. An overview of the various strategies for UME and urology training was then discussed.
The preliminary survey design and the Delphi methodology were evaluated by the panel. The questionnaire was reviewed, with integration of any other points if necessary and comments on the methodology before starting the consensus rounds. The final version consisted of three parts:
-
(1)
Urology programme introduction and duration in the undergraduate curriculum (15 questions);
-
(2)
Urology curriculum distribution in universities (8 questions); and
-
(3)
Practical curriculum (11 questions).
The survey items in their final form are shown in the Supplementary material. The protocol was then revised and validated by a team of dedicated methodologists (Department of Trials Methodology, Liverpool Clinical Trials Centre, Liverpool University, Liverpool, UK).
2.2. Phase II: internet survey and Delphi process
All of the statements included were entered into DelphiManager (www.comet-initiative.org/delphimanager/), a web-based system designed to facilitate the building and management of Delphi surveys.
The survey was sent to urologists previously selected by different European national urological societies. The levels of agreement were based on a nine-point scale, according to the GRADE grid: 1–3, disagree; 4–6, uncertain; and 7–9, agree. An “Unable to score” option was also added for use in the case of insufficient knowledge/expertise. Consensus was defined as at least 70% of the participants scoring within the same 3-point grouping.
Repeated anonymous voting was performed in three rounds. After the first round, the questions reaching consensus were removed from the subsequent round and the participants were provided with the results from the previous round in the form of histograms plus percentages. Some statements were mutually exclusive, so when consensus was reached for one of them, the others were not included in subsequent rounds.
2.3. Phase III: on-line expert meeting
The last phase included an on-line meeting. The statements for which consensus was reached by the third survey round (agreement or disagreement) were presented for approval but were not rediscussed, whereas all of the statements for which consensus was not reached or the consensus was uncertainty after the three Delphi rounds were rediscussed. The resulting document was distributed for approval to all participants who completed the three Delphi rounds.
3. Results
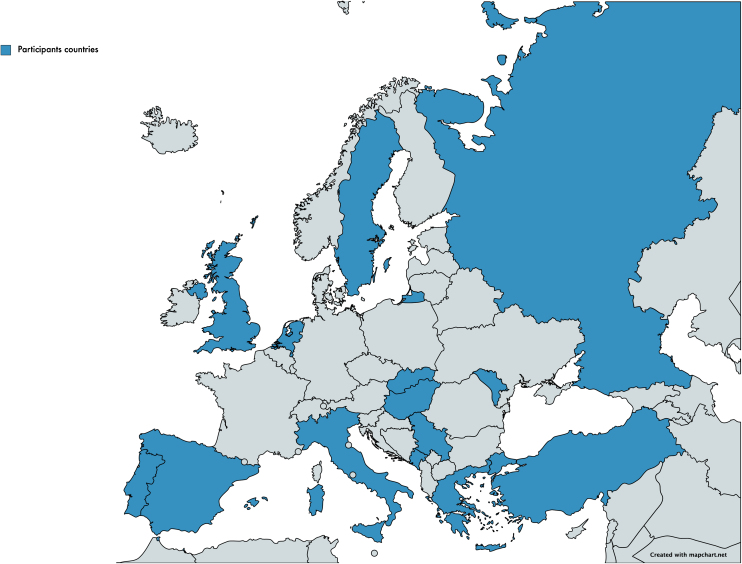
The study flow chart and an overview of the Delphi results are shown in Figure 1. Of the 45 invited urologists representing different European national urological societies, 14 (31.1%), completed all rounds; the respondents were from Greece, Hungary, Italy, Moldova, Montenegro, Portugal, Russia, Serbia, Slovakia, Spain, Sweden, The Netherlands, Turkey, and the UK, with an additional five urologists representing the ESU also completing the three rounds. All respondents were certified urologists with more than 5 yr of experience. The distribution of countries represented in the consensus is shown in Figure 2. Overall, consensus was reached for 20 of 34 statements (70.5%) across the three rounds, with agreement for 75% (n = 15) and disagreement for 25% (n = 5).
Fig. 1.
Study flow chart.
Fig. 2.
European countries from which survey respondents represented different national urological societies.
Consensus was reached for seven, 12, and one questions in the first, second, and third rounds, respectively. The 20 items for which consensus agreement or disagreement was reached during the Delphi process were presented and approved during the on-line meeting without objections or a need for rediscussion (Table 1).
Table 1.
Overview of consensus statements with a final decision
 |
DRE = digital rectal examination; LUTS = lower urinary tract symptoms; TURB = transurethral resection of the bladder; URS = ureteroscopy.
*These statements were excluded as they were mutually exclusive.
3.1. Part I: urology programme introduction and duration in the undergraduate curriculum
Consensus agreement for four of the 15 formulated statements was achieved, with some statements being mutually exclusive (Table 2). It was agreed that urological teaching should be introduced before year 5 of medical school, with at least 20 h of theoretical activities (lectures, classes) and at least 30 h of practical activities (patients, clinical cases, and training models).
Table 2.
Urology programme introduction and duration in the undergraduate curriculum
 |
*Black spaces: results for the 3rd round are not presented as they were mutually exclusive.
For the statements regarding distribution of the urology programme, which ranged from having urology spread throughout all undergraduate medical school years to a 2–4-wk dedicated programme, consensus agreement was not reached.
3.2. Part II: urology curriculum distribution in universities
Statements 16–23 included a list of options on how urology should be taught. For six of the eight items, consensus was reached (Table 3). It was agreed that urology should be taught as a stand-alone subject rather than combined with another surgical specialty or a nephrology programme. While 94% agreed that urology should be mandatory in UME, 72% disagreed that urology should be an optional subject. The participants agreed that urology should be taught by symptoms (haematuria, lower urinary tract symptoms, flank pain) rather than by organ or subspecialty.
Table 3.
Urology curriculum distribution in universities
LUTS = lower urinary tract symptoms.
3.3. Part III: practical curriculum
The practical aspect is important in all medical specialties. The third part of the consensus covered the practical curriculum, with consensus agreement reached for 10 of the 11 statements, including several aspects of physical examination (Table 4).
Table 4.
Practical curriculum
 |
DRE = digital rectal examination; TURB = transurethral resection of the bladder; URS = ureteroscopy.
It was agreed that the urology programme should include the anatomy and physiology of the urinary tract, and students should know how to perform a clinical assessment of a urological patient. In addition, students should be competent in conducting a digital rectal examination (DRE) and abdomen and genital examination, and should be able to perform urethral catheterisation.
While there was no consensus regarding the ability of students to assist in minor urological surgery, there was consensus disagreement with statements suggesting that they should be able to assist in intermediate-complexity or major urological surgery.
Finally, there was agreement that students should rate their time in urology and give feedback to educators, since a positive undergraduate experience has a positive impact on future career choice.
4. Discussion
Our survey shows that the consensus opinion from across Europe is that UME should have at least 20 h of theoretical and 30 h of practical activities in urology, with use of training models to enhance the curriculum. Urology should be taught as a stand-alone subject rather than with another surgical specialty or combined with nephrology. It should be mandatory and taught on the basis of symptomatology. The practical curriculum should include DRE, abdominal and genitourinary examination, and urethral catheterisation. Clinical assessment of patients should be included, and students should have a chance to rate their placement and give feedback to facilitate constant improvement and evolution of the teaching programme.
The current variation in urology training across medical schools leads to inconsistent knowledge and acumen among junior doctors in managing basic urological conditions. This was initially reported in 1966 and has been seen across the world [10]. Junior doctors are likely to meet patients with urological conditions in primary care, emergency departments, and on hospital wards.
Urology is an essential topic in UME. While urology teaching is mandatory in 76% of European medical schools, in the USA, mandatory urology decreased from 99% in 1956 to 48% in 1978 and even further to 17% between 2005 and 2009 [5], [6], [11]. Worse still, a 2001 UK survey suggested that students could graduate without any exposure to urology, a fact also confirmed by 65% of medical school directors in the USA [7]. Our expert panel agreed that urology should be taught as a stand-alone subject and should be mandatory in UME. The urological community must accept that most students will not choose urology as a career, so the typical content for any proposed urology curriculum should emphasise aspects pertinent to surgically minded students and at the same time fulfil the needs required as a primary care physician. A urology curriculum taught by symptoms rather than by organs or subspecialty would fulfil these criteria.
Furthermore, any curriculum should also cover nontechnical skills, as focusing only on the acquisition of technical skills and competence is not enough for the delivery of a modern and safe surgical curriculum. The Royal College of Surgeons of Edinburgh defines nontechnical skills as a collective term describing the skills and behaviours encompassing situational awareness, decision-making, communication, teamwork, and leadership. Others have divided nontechnical skills into interpersonal (eg, communication, teamwork), cognitive (eg, decision-making, situational awareness), and personal resource skills (eg, coping with stress and fatigue) [12], [13].
To date, the relationship between choosing a career in urology and variables such as the year of introduction of urology in medical school and the number of theoretical and practical lessons has not been investigated. Our results show overall agreement that urology teaching should be introduced before year 5 of medical school and should comprise at least 20 h of theoretical activities (lectures, classes) and at least 30 h of practical activities (patients, clinical cases, and training models). Perhaps an early introduction to urology in medical school with content related to anatomy, physiology, and basic clinical examination, along with practical lessons, introduction to new technologies, and simulation, could positively encourage more undergraduates to consider a career in urology [14], [15]. In a previous study from Dundee, a standardised urology curriculum seemed to yield excellent results with good feedback [16].
Current students were born in a digital world and speak the language of technology. They have higher expectations of their education than previous generations; to meet these expectations, medical education has to evolve rapidly with the introduction of technology-based virtual training [17]. This is especially important during and in the aftermath of the COVID-19 pandemic, when teaching via webinars and online media is commonplace [18], [19], [20], [21].
The use of simulation training on models has increased in HST, and perhaps this could also be used for acquisition of practical skills in DRE and scrotal examination during UME [10]. It has been shown that dedicated, focused HOT allows acquisition of skills and builds trainee confidence [12], [16]. Training could also be strengthened via online tutorials, instructional videos on examination and catheter placement, and counselling on intimate examinations. It is much easier for students to learn these skills in a relaxed, stress-free environment under supervision before a real life setting.
Some limitations have to be acknowledged. The study yielded statements based on a panel consensus, which represents the lowest level of evidence. However, with the exception of the present report, the literature review of current evidence on UME in urology in Europe revealed that this is still an unexplored subject. The only data reported at European level come from a recent survey [6] that found that medical students’ exposure to urology during their undergraduate career was heterogeneous, although the quality of urology education in the study was valued from moderate to high, and urology as a specialty did not influence their decision-making on future training.
Another limitation is that the response rate from different European countries was not proportional, which may potentially skew the analysis in favour of the responding nations, and there was no response from some of the largest countries in Europe such as France and Germany. This could limit wider acceptance of the findings in a multistakeholder context. Nevertheless, the present study is the first appraisal among experts in the field of urology UME in Europe. The benefits of an established urology curriculum are likely to improve the medical student experience in the future. This consensus gives the basic requirements for aspects of urology undergraduate education and training in universities and institutions across Europe.
5. Conclusions
Our recommended urology pathway will allow European medical schools to provide a more comprehensive undergraduate urology curriculum. It will also help to improve and maintain standards of urology undergraduate teaching across Europe and ensure that all students receive adequate balanced exposure to theory, HOT, and practical skills in urology. This could standardise teaching, increase the uptake of urology, protect future workforce capacity, and equip trainees with basic knowledge and skills in urology. It is likely that this model will be adopted and followed worldwide in the near future.
Author contributions: Juan Gómez Rivas had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Gómez Rivas, Rodriguez Socarrás, Marra, Palou.
Acquisition of data: Gómez Rivas, Somani, Rodriguez Socarrás, Zondervan.
Analysis and interpretation of data: Gómez Rivas, Somani, Rodriguez Socarrás, Marra, Palou.
Drafting of the manuscript: Gómez Rivas, Somani, Rodriguez Socarrás, Pearce.
Critical revision of the manuscript for important intellectual content: Gómez Rivas, Somani, Rodriguez Socarrás, Marra, Pearce, Henningsohn, Zondervan, van der Poel, Van Poppel, N’Dow, Liatsikos, Palou.
Statistical analysis: None.
Obtaining funding: None.
Administrative, technical, or material support: Gómez Rivas, Rodriguez Socarrás, Marra, Van Poppel, Palou.
Supervision: Gómez Rivas, Somani, Rodriguez Socarrás, Marra, Pearce, Henningsohn, Zondervan, van der Poel, Van Poppel, N’Dow, Liatsikos, Palou.
Other: None.
Financial disclosures: Juan Gómez Rivas certifies that all conflicts of interest, including specific financial interests and relationships and affiliations relevant to the subject matter or materials discussed in the manuscript (eg, employment/affiliation, grants or funding, consultancies, honoraria, stock ownership or options, expert testimony, royalties, or patents filed, received, or pending), are the following: None.
Funding/Support and role of the sponsor: None.
Acknowledgments: We want to acknowledge the European Association of Urology personnel dedicated to keeping this work going during the COVID-19 crisis.
Associate Editor: Silvia Proietti
Footnotes
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.euros.2021.09.003.
Contributor Information
Juan Gómez Rivas, Email: juangomezr@gmail.com.
a European School of Urology collaborative group:
Rade Stanisavljevic, Bojanic Nebojsa, Pavel Banov, Leonid Spivak, Stilianos Giannakopoulos, Mario Álvarez-Maestro, Jan Svihra, Tobias Page, Emrah Yuruk, Miguel Silva-Ramos, Saban Sarikaya, Francesco Porpiglia, and Attila Szendroi
Appendix A. Members of the European School of Urology collaborative group
Rade Stanisavljevic, Urology Department, General Hospital Bar, Bar, Montenegro
Bojanić Nebojsa, Clinic of Urology, Clinical Center of Serbia and School of Medicine, University of Belgrade, Belgrade, Serbia
Pavel Banov, Department of Urology and Surgical Nephrology, Nicolae Testemiceanu State Medical and Pharmaceutical University, Chisinau, Republic of Moldova
Leonid Spivak, Institute for Urology and Reproductive Health, Sechenov University, Moscow, Russia
Stilianos Giannakopoulos, Department of Urology, Democritus University of Thrace, Dragana, Alexandroupolis, Greece
Mario Álvarez-Maestro, Department of Urology, Hospital Universitario La Paz, Madrid, Spain
Jan Svihra, Department of Urology, Hospital Universitario La Paz, Madrid, Spain
Tobias Page, Department of Urology, Freeman Hospital, Newcastle upon Tyne Hospitals NHS Foundation Trust, Newcastle upon Tyne, UK
Emrah Yuruk, Department of Urology, BHT Clinic Istanbul Tema Hospital, Kücükcekmece, Istanbul, Turkey
Miguel Silva-Ramos, Urology Department, Centro Hospitalar e Universitário do Porto, Porto, Portugal
Saban Sarikaya, Department of Urology, Faculty of Medicine, Ondokuz Mayis University, Samsun, Turkey
Francesco Porpiglia, Division of Urology, Department of Oncology, University of Turin, San Luigi Hospital, Orbassano, Italy
Attila Szendroi, Department of Urology, Semmelweis University, Budapest, Hungary
Appendix B. Supplementary data
The following is Supplementary data to this article:
References
- 1.Pietropaolo A., Proietti S., Geraghty R. Trends of ‘urolithiasis: interventions, simulation, and laser technology’ over the last 16 years (2000–2015) as published in the literature (PubMed): a systematic review from European Section of Uro-technology (ESUT) World J Urol. 2017;35:1651–1658. doi: 10.1007/s00345-017-2055-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sung H., Ferlay J., Siegel R.L. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021 doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 3.Browne C., Davis N.F., MacCraith E.D., Lennon G.M., Galvin D.J., Mulvin D.W. Prospective evaluation of a virtual urology outpatient clinic. Ir J Med Sci. 2018;187:251–254. doi: 10.1007/s11845-017-1615-y. [DOI] [PubMed] [Google Scholar]
- 4.Conroy S. Undergraduate urology education: a fundamental pillar in building the next generation of urologists. Eur Urol. 2020;78:385–386. doi: 10.1016/j.eururo.2020.06.050. [DOI] [PubMed] [Google Scholar]
- 5.Casilla-Lennon M., Motamedinia P. Urology in undergraduate medical education. Curr Urol Rep. 2019;20:69. doi: 10.1007/s11934-019-0937-x. [DOI] [PubMed] [Google Scholar]
- 6.Gómez Rivas J., Rodriguez Socarrás M., Somani B. Undergraduate education for urology in Europe. Where do we stand? Eur Urol. 2020;78:381–384. doi: 10.1016/j.eururo.2020.05.037. [DOI] [PubMed] [Google Scholar]
- 7.Scott R., Sinclair A.M., Pearce I. Is there a need for an undergraduate urological curriculum? Br J Med Surg Urol. 2012;5:16–19. doi: 10.1016/j.bjmsu.2011.11.001. [DOI] [Google Scholar]
- 8.Ng A., Light A., Chan V.W.S., Asif A., Bhatt N.R., Kasivisvanathan V. Urology teaching in UK medical schools: does it prepare doctors adequately? Nat Rev Urol. 2020;17:651–652. doi: 10.1038/s41585-020-00393-6. [DOI] [PubMed] [Google Scholar]
- 9.Somani B.K., Van Cleynenbreugel B., Gözen A.S. Outcomes of European Basic Laparoscopic Urological Skills (EBLUS) examinations: results from European School of Urology (ESU) and EAU Section of Uro-Technology (ESUT) over 6 years (2013–2018) Eur Urol Focus. 2020;6:1190–1194. doi: 10.1016/j.euf.2019.01.007. [DOI] [PubMed] [Google Scholar]
- 10.Owen L.E., Byrne D.J., Ker J.S. A learning package for medical students in a busy urology department: design, implementation, and evaluation. Urology. 2008;72:982–986. doi: 10.1016/j.urology.2008.07.037. [DOI] [PubMed] [Google Scholar]
- 11.Burns E., Hotchkiss R.S., Flocks R.H. The present status of undergraduate urologic training: report of the Committee to Study Status of Urology in Medical Schools. J Urol. 1956;76:309–322. doi: 10.1016/S0022-5347(17)66699-0. [DOI] [PubMed] [Google Scholar]
- 12.Yule S., Flin R., Paterson-Brown S., Maran N., Rowley D. Development of a rating system for surgeons’ non-technical skills. Med Educ. 2006;40:1098–1104. doi: 10.1111/j.1365-2929.2006.02610.x. [DOI] [PubMed] [Google Scholar]
- 13.Agha R.A., Fowler A.J., Sevdalis N. The role of non-technical skills in surgery. Ann Med Surg. 2015;4:422–427. doi: 10.1016/j.amsu.2015.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mantica G., Rivas J.G., Carrion D.M. Simulator Availability Index: a novel easy indicator to track training trends. Is Europe currently at a urological training recession risk? Cent Eur J Urol. 2020;73:231–233. doi: 10.5173/ceju.2020.0048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Veneziano D., Cacciamani G., Rivas J.G., Marino N., Somani B.K. VR and machine learning: novel pathways in surgical hands-on training. Curr Opin Urol. 2020;30:817–822. doi: 10.1097/MOU.0000000000000824. [DOI] [PubMed] [Google Scholar]
- 16.Shah J., Billington R., Manson J., Vale J. Undergraduate urology: a survey of current provisions and guidelines for a core curriculum. BJU Int. 2002;89:327–330. doi: 10.1046/j.1464-4096.2001.01534.x. [DOI] [PubMed] [Google Scholar]
- 17.Xia T., Baird C., Jallo G. An integrated system for planning, navigation and robotic assistance for skull base surgery. Int J Med Robot Comput Assist Surg. 2008;4:321–330. doi: 10.1002/rcs.213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ficarra V., Novara G., Abrate A. Urology practice during COVID-19 pandemic. Minerva Urol Nefrol. 2020;72:369–375. doi: 10.23736/S0393-2249.20.03846-1. [DOI] [PubMed] [Google Scholar]
- 19.Campi R., Amparore D., Checcucci E. Exploring the residents’ perspective on smart learning modalities and contents for virtual urology education: lesson learned during the COVID-19 pandemic. Actas Urol Esp. 2021;45:39–48. doi: 10.1016/j.acuro.2020.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pang K.H., Carrion D.M., Rivas J.G. The Impact of COVID-19 on European Health care and urology trainees. Eur Urol. 2020;78:6–8. doi: 10.1016/j.eururo.2020.04.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Teoh J.Y.C., Ong W.L.K., Gonzalez-Padilla D. A global survey on the impact of COVID-19 on urological services. Eur Urol. 2020;78:265–275. doi: 10.1016/j.eururo.2020.05.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.