Summary
This systematic review assessed the progress and barriers towards maternal and neonatal tetanus elimination in the 12 countries that are yet to achieve elimination, globally. Coverage of at least 80% (the coverage level required for elimination) was assessed among women of reproductive age for five factors: (1) at least two doses of tetanus toxoid-containing vaccine, (2) protection at birth, (3) skilled birth attendance, (4) antenatal care visits, and (5) health facility delivery. A scoping review of the literature and data from Demographic and Health Surveys and Multiple Indicator Cluster Surveys provided insights into the barriers to attaining maternal and neonatal tetanus elimination. Findings showed that none of the 12 countries attained at least 80% coverage for women of reproductive age receiving at least two doses of tetanus toxoid-containing vaccine or protection at birth according to the data from Demographic and Health Surveys or Multiple Indicator Cluster Surveys. Barriers to maternal and neonatal tetanus elimination were mostly related to health systems and socioeconomic factors. Modification to existing maternal and neonatal tetanus elimination strategies, including innovations, will be required to accelerate maternal and neonatal tetanus elimination in these countries.
Introduction
In 1989, the World Health Assembly endorsed the global initiative to eliminate neonatal tetanus by 1995. In 1999, the initiative was relaunched as maternal and neonatal tetanus elimination (MNTE) because tetanus also affects mothers, targeting 59 high-risk countries and setting a target date for 2020 after the initial target dates of 2005 and 2015 were missed. Neonatal tetanus elimination, defined as having less than one neonatal tetanus case per 1000 livebirths in every district each year, is also used as a proxy for maternal tetanus elimination.1 Strategies to achieve MNTE include several approaches: vaccinating at least 80% of pregnant women with at least two doses of tetanus toxoid-containing vaccines (TTCV2+) during antenatal care and outreach sessions; doing at least three rounds of tetanus toxoid-containing vaccine (TTCV) supplementary immunisation activities, targeting women of reproductive age in high-risk areas and aiming for at least 80% TTCV2+ coverage; promoting clean births and umbilical cord care by strengthening skilled birth attendance (SBA); and strengthening neonatal tetanus surveillance, including case investigation and response.2
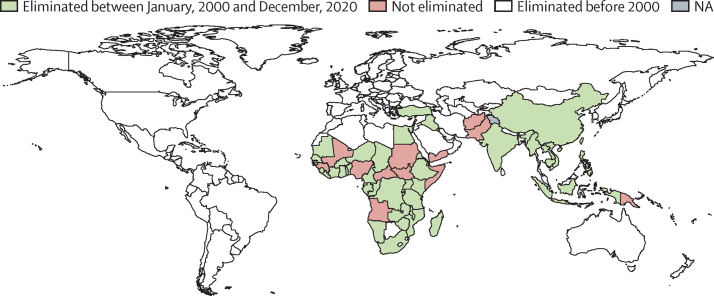
Despite several missed deadlines to achieve MNTE, 47 (80%) of the originally targeted 59 high-risk countries had achieved MNTE as of December, 2020 (figure 1), resulting in an 88% decrease in the annually reported neonatal tetanus deaths from an estimated 200 000 in 2000, to 25 000 in 2018.4 Additionally, partial elimination has been achieved in Nigeria (southeast and southwest geopolitical zones), Pakistan (Punjab province), and Mali (central and southern regions).5 Between 2010 and 2017, the number of targeted countries validated for MNTE increased from 19 to 44, with an average of three countries validated each year, but the number declined to one or two during 2018 and 2020 (figure 2).
Figure 1.
Global progress with maternal and neonatal tetanus elimination, 2000–20
Reproduced with permission from the World Health Organization.3 Progress towards the global goal of eliminating maternal and neonatal tetanus in 59 high-burden countries, with 47 (80%) of 59 countries achieving elimination. Eight (67%) of 12 countries that are yet to eliminate maternal and neonatal tetanus are in the African continent, whereas the remaining four (33%) are in southeast Asia, and in eastern Mediterranean and western Pacific regions. World Health Organization disclaimer: the boundaries and names shown and the designations used on this map do not imply the expression of any opinion whatsoever of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted and dashed lines on maps represent approximate border lines for which there may not yet be full agreement. World Health Organization, WHO. 2020. All rights reserved. NA=not applicable.
Figure 2.
Cumulative number of countries validated for maternal and neonatal tetanus elimination between 2000 and 2020
Number of countries validated out of the total 59 countries targeted for maternal and neonatal tetanus elimination. Although progress has been made towards attaining the global goal, the different global deadlines (2005, 2015, and 2020) set for elimination have been missed.
As of December, 2020, 12 (20%) of the 59 high-risk countries had yet to achieve MNTE: Afghanistan, Angola, Central African Republic, Guinea, Mali, Nigeria, Pakistan, Papua New Guinea, Somalia, South Sudan, Sudan, and Yemen. The slow pace of MNTE implementation indicates the complexities in these countries, which have made it impossible to meet the global deadline of elimination by 2020. This systematic review highlights the progress towards the global goal to eliminate maternal and neonatal tetanus in the remaining 12 countries and the barriers that have delayed elimination.
Methods
Search strategy and selection criteria
We assessed the progress and barriers towards MNTE in each of the 12 countries through compilation of MNTE programmatic performance indicators using different data sources. We assessed the protection of women and infants against tetanus through immunisation via several approaches: compiling the percentage of pregnant women receiving TTCV2+, from official country estimates reported to the WHO/UNICEF Joint Reporting Form between 2015 and 2019,6 and from the most recent Demographic and Health Surveys7 or Multiple Indicator Cluster Surveys8 based on data among women aged 15–49 years who reported a livebirth during the last 5 years preceding the survey; compiling the percentage of infants with protection at birth (PAB) against tetanus, which was assessed on the basis of the timing since the last dose and number of doses of TTCV received by the mother, from WHO estimates between 2015 and 2019,9 and from the most recent Demographic and Health Surveys7 or Multiple Indicator Cluster Surveys;8 and compiling the total number of women of reproductive age who were targeted and received TTCV2+ during TTCV supplementary immunisation activities from the most recent (April, 2021) list of TTCV supplementary immunisation activities available on the WHO website.10
To assess the protection against tetanus through clean delivery in each of the 12 countries, we used estimates reported by the most recent Demographic and Health Surveys7 or Multiple Indicator Cluster Surveys8 among women aged 15–49 years who reported a livebirth during the last 5 years preceding the survey. Data was compiled on three MNTE indicators: the percentage of deliveries assisted by skilled birth attendants (eg, doctors, nurses, and midwives), the percentage of deliveries that occurred in health facilities, and the percentage of pregnancies that had at least one antenatal care (ANC1) visit.
To assess barriers to achievement of MNTE in the 12 countries, we analysed data from the most recent Demographic and Health Surveys7 or Multiple Indicator Cluster Surveys8 to assess the predictors of the last birth being protected against tetanus in each country and the barriers to accessing health care among women aged 15–49 years. A scoping review of the literature provided an insight into health and other systems-wide barriers to achieving MNTE. The impact of the COVID-19 pandemic on the implementation of vaccination and TTCV supplementary immunisation activities was compiled from data available in the WHO repository.10
Data analysis
We compared the percentage coverage of TTCV2+ with the percentage PAB coverage to elucidate the discrepancies in coverage that usually exist between these two methods of computing tetanus protection coverage.2 Although coverage of TTCV2+ considers only vaccination coverage during the last pregnancy, PAB coverage considers the total number of TTCV doses received by the pregnant woman in her lifetime and the date of the last dose to assess if the birth was protected.2 For South Sudan, the coverage of TTCV2+ from the 2010 Demographic and Health Survey was compared with the coverage from the 2013 WHO/UNICEF Joint Reporting Form, the first year WHO/UNICEF Joint Reporting Form data were available for that country. Additionally, the cumulative coverage of TTCV2+ from supplementary immunisation activity rounds targeting women of reproductive age was also analysed with data from the global calendar of TTCV supplementary immunisation activities.10
Although the WHO/UNICEF Joint Reporting Form data allowed for national-level analyses, Demographic and Health Surveys or Multiple Indicator Cluster Surveys also provided data for first subnational level (ie, regions, states, or provinces) and by demographic and socioeconomic factors. For all indicators, we assessed countries’ performances towards attaining at least 80% coverage, the threshold for achieving MNTE.
Results
Demographics and income status of the 12 countries
In 2019, the 12 countries that had yet to eliminate MNTE had a total combined population of 149 million women of reproductive age, with 98 million (66%) of these women living in Nigeria and Pakistan (table 1). Eight (67%; Afghanistan, Central African Republic, Guinea, Mali, Somalia, South Sudan, Sudan, and Yemen) of the 12 countries were classified by the World Bank Group as low-income countries in 2019, whereas the remaining four (33%; Angola, Nigeria, Pakistan, and Papua New Guinea) were classified as lower-middle-income countries.12
Table 1.
Trend of coverage with TTCV2+ and PAB from 2015 to 2019 and TTCV2+ in SIAs in the 12 countries that have not yet achieved maternal and neonatal tetanus elimination
| Population of WRA in 2019 (× 1000)11 |
Year |
TTCV2+ coverage from SIAs among WRA10 |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2015 |
2016 |
2017 |
2018 |
2019 |
WRA targeted (× 1000)10 | WRA vaccinated with TTCV2+ (× 1000)10 | WRA with TTCV2+ coverage | Date of last SIA10 | |||||||
| TTCV2+6 | PAB9 | TTCV2+6 | PAB9 | TTCV2+6 | PAB9 | TTCV2+6 | PAB9 | TTCV2+6 | PAB9 | ||||||
| Afghanistan | 8778 | 91% | 70% | 58% | 70% | 86% | 70% | 85% | 68% | 85% | 68% | 11 472 | 5212 | 45% | February, 2019 |
| Angola | 7327 | 71% | 78% | 70% | 78% | 67% | 78% | 66% | 78% | 54% | 70% | 8452 | 7097 | 84% | December, 2014 |
| Central African Republic | 1150 | 52% | 60% | 54% | 60% | 62% | 60% | 89% | 60% | 64% | 60% | 1033 | 804 | 78% | September, 2011 |
| Guinea | 3161 | 54% | 80% | 60% | 80% | 60% | 80% | 70% | 80% | 80% | 80% | 5643 | 4773 | 85% | March, 2020 |
| Mali | 4391 | 63% | 85% | 75% | 85% | 75% | 85% | 60% | 85% | 46% | 85% | 8462 | 4158 | 49% | June, 2020 |
| Nigeria | 46 238 | 40% | 55% | 47% | 55% | 60% | 55% | 62% | 60% | 40% | 60% | 14 256 | 9365 | 65% | March, 2020 |
| Pakistan | 51 374 | 68% | 75% | 78% | 80% | 62% | 85% | 60% | 85% | 62% | 85% | 30 235 | 25 405 | 84% | March, 2020 |
| Papua New Guinea | 2159 | 46% | 70% | 44% | 70% | 40% | 70% | 25% | 70% | 31% | 70% | 1725 | 450 | 26% | November, 2016 |
| Somalia | 3544 | 67% | 67% | 62% | 67% | 61% | 67% | 59% | 67% | 58% | 67% | 1852 | 497 | 27% | October, 2009 |
| South Sudan | 3190 | 28% | 68% | 38% | 68% | 49% | 68% | 44% | 68% | 40% | 68% | 9399 | 6002 | 64% | January, 2020 |
| Sudan | 10 347 | 53% | 77% | 52% | 77% | 54% | 80% | 51% | 80% | 52% | 80% | 8491 | 7294 | 86% | December, 2019 |
| Yemen | 7497 | 16% | 70% | 19% | 70% | 21% | 70% | 22% | 70% | 25% | 70% | 6650 | 3533 | 53% | March, 2020 |
| Total | 149 156 | .. | .. | .. | .. | .. | .. | .. | .. | .. | .. | 107 670 | 74 590 | 69% | .. |
PAB=protection at birth. SIA=supplementary immunisation activity. TTCV2+=at least two doses of tetanus toxoid-containing vaccine. WRA=women of reproductive age.
Protection against tetanus through immunisation
In 2019, only two (17%; Afghanistan and Guinea) of the 12 countries reported the target of at least 80% TTCV2+ coverage according to their official estimated coverage through the WHO/UNICEF Joint Reporting Form,6 whereas four (33%; Guinea, Mali, Pakistan, and Sudan) countries achieved at least 80% PAB coverage (WHO estimates).9 Yemen reported the lowest coverage of TTCV2+ by the WHO/UNICEF Joint Reporting Form (25%), whereas Central African Republic and Nigeria had the lowest percentage of infants with PAB (60% each). The PAB coverage estimate, a more reliable indicator of the level of tetanus protection than coverage of TTCV2+, maintained a steadier trend and was higher than TTCV2+ coverage in all countries except in Afghanistan and in the Central African Republic. Between 2015 and 2019, there was no or limited improvement in TTCV2+ or PAB coverage in the 12 countries (table 1).
Based on the most recent Demographic and Health Surveys or Multiple Indicator Cluster Surveys data, TTCV2+ and PAB coverage among women that had a livebirth in the 5 years preceding the survey was less than 80% in all 12 countries; however, PAB coverage was higher than TTCV2+ coverage in all countries.7, 8 Pakistan (57%) and Yemen (9%) had the highest and lowest TTCV2+ coverage, respectively, whereas Angola (66%) and Somalia (27%) had the highest and lowest PAB coverage, respectively (table 2).
Table 2.
MNTE performance indicators in the 12 countries that have not achieved MNTE
|
TTCV2+ coverage from the WHO/UNICEF Joint Reporting Form6 |
MNTE indicators from most recent DHS7or MICS8 |
|||||||
|---|---|---|---|---|---|---|---|---|
| TTCV2+ coverage in 2019 | TTCV2+ coverage during the year of most recent DHS or MICS | Year of most recent DHS or MICS | TTCV2+ | PAB | Health facility delivery | SBA | ANC1 | |
| Afghanistan | 85% | 93% | 2015 | 34% | 53% | 48% | 51% | 59% |
| Angola | 54% | 70% | 2016 | 56% | 66% | 46% | 50% | 82% |
| Central African Republic | 86% | 76% | 2010 | ND | ND | 53% | ND | 68% |
| Guinea | 94% | 91% | 2018 | 48% | 59% | 53% | 55% | 81% |
| Mali | 72% | 75% | 2018 | 36% | 50% | 67% | 67% | 80% |
| Nigeria | 40% | 50% | 2018 | 53% | 62% | 39% | 43% | 67% |
| Pakistan | 62% | 60% | 2018 | 57% | 64% | 62% | 64% | 80% |
| Papua New Guinea | 31% | 25% | 2018 | 27% | 38% | 55% | 55% | 76% |
| Somalia | 58% | 58% | 2020 | 17% | 27% | 21% | 32% | 31% |
| South Sudan | 38% | 46% | 2010 | 28% | 37% | 12% | 19% | 62% |
| Sudan | 53% | 53% | 2014 | 32% | 58% | 28% | 78% | 79% |
| Yemen | 25% | 18% | 2013 | 9% | 28% | 30% | 45% | 60% |
ANC1=first antenatal care visit. DHS=Demographic Health Survey. MICS=Multiple Indicator Cluster Survey. MNTE=maternal and neonatal tetanus elimination. ND=no data available. PAB=protection at birth. SBA=skilled birth attendance. TTCV2+=at least two doses of tetanus toxoid-containing vaccine.
As of 2020, 74·5 million (69%) of the estimated cumulative 107·6 million women of reproductive age in the 12 countries that were targeted for TTCV supplementary immunisation activities had received TTCV2+, with coverage varying from as high as 86% in Sudan to as low as 26% in Papua New Guinea (table 1). Many of the 12 countries have done at least one or two rounds of supplementary immunisation activities in a phased manner spread over 1 year or 2 years, but Angola, Papua New Guinea, and Somalia have not done any rounds of supplementary immunisation activities since 2014, 2016, and 2009, respectively. Mali, Guinea, and Sudan have completed their three rounds of supplementary immunisation activities in all high-risk districts and could be ready for MNTE validation in 2021. However, the escalation of the COVID-19 pandemic in the African region might hinder validation in these countries in 2021.
Protection against tetanus through clean delivery
Data from the most recent Demographic and Health Surveys or Multiple Indicator Cluster Surveys showed that only four (33%; Angola, Guinea, Mali, and Pakistan) of the 12 countries achieved at least 80% ANC1 coverage, and none of the 12 countries had at least 80% coverage for health facility delivery or SBA.7, 8 ANC1 coverage was highest in Angola (82%) and lowest in Somalia (31%), SBA coverage was highest in Sudan (78%) and lowest in South Sudan (19%), and coverage for health facility delivery was highest in Mali (67%) and lowest in South Sudan (12%). In all countries, ANC1 coverage was higher than coverage for health facility delivery and SBA, except in Somalia. ANC1 coverage was also higher than TTCV2+ and PAB coverage (table 2).
Barriers to achieving MNTE in the 12 remaining countries
Analysis of the most recent Demographic and Health Surveys and Multiple Indicator Cluster Surveys data showed that children born to educated mothers, residing in urban areas, and from wealthy households were more likely to be protected at birth against tetanus versus infants whose mothers were less educated, whose families lived in rural areas, or whose families were poorer (table 3).7, 8 For example, in Nigeria, infants born to mothers in the highest wealth quintile households (87%) were 2·3 times more likely to be protected at birth compared with infants whose mothers were in the lowest quintile households (38%). Nigerian infants born to mothers from Imo State in the southeast zone (97%) were 4·4 times more likely to be protected at birth compared with infants born in Zamfara State in the northwest zone (22%).
Table 3.
Proportion of women aged 15–49 years whose last livebirth was protected against tetanus according to their background characteristics based on the most recent DHS7 or MICS8 in the 12 countries that are yet to eliminate maternal and neonatal tetanus
| Type and date of survey7, 8 |
Subnational level (province, region, state, or governorate) |
Residence |
Education |
Wealth quintile |
|||||
|---|---|---|---|---|---|---|---|---|---|
| Lowest coverage | Highest coverage | Rural | Urban | No education | At least secondary education | Lowest | Highest | ||
| Afghanistan | DHS 2015 | 3% | 79% | 53% | 55% | 49% | 76% | 53% | 59% |
| Angola | DHS 2015 and 2016 | 39% | 86% | 46% | 77% | 45% | 83% | 42% | 88% |
| Central African Republic | DHS 2010 | ND | ND | ND | ND | ND | ND | ND | ND |
| Guinea | DHS 2018 | 48% | 73% | 53% | 73% | 55% | 76% | 43% | 75% |
| Mali | DHS 2018 | 14% | 67% | 45% | 65% | 45% | 67% | 41% | 68% |
| Nigeria | DHS 2018 | 22% | 97% | 51% | 77% | 40% | 90% | 38% | 87% |
| Pakistan | DHS 2017 and 2018 | 27% | 81% | 63% | 80% | 52% | 91% | 44% | 90% |
| Papua New Guinea | DHS 2016 and 2018 | 15% | 62% | 36% | 50% | 21% | 61% | 25% | 53% |
| Somalia | DHS 2020 | ND | ND | 32% | 43% | 23% | 60% | 10% | 44% |
| South Sudan | HHS 2010 | ND | ND | ND | ND | ND | ND | ND | ND |
| Sudan | MICS 2014 | 42% | 73% | 55% | 68% | 47% | 79% | 44% | 74% |
| Yemen | DHS 2013 | 5% | 53% | 24% | 38% | 21% | 56% | 20% | 40% |
DHS=Demographic Health Survey. HHS=Household Health Survey. MICS=Multiple Indicator Cluster Survey. ND=no data available.
The most commonly reported barriers to accessing health care by women living in eight of the 12 countries according to Demographic and Health Surveys or Multiple Indicator Cluster Surveys were “getting money for treatment” and “distance to health facility” (highest in Afghanistan at 67% each).7, 8 Other barriers reported included “not wanting to go alone” and “getting permission to go for treatment”, which in most cases could mean “getting permission from their husbands” (table 4).7, 8 Affordability, availability, and accessibility of antenatal care providers were cited as hurdles to antenatal care use in Nigeria,13 whereas in rural Mali, scarcity of health facilities, limited availabilty of transportation, and a long distance to health facilities were identified as some of the barriers to antenatal care attendance, and access to SBA and health facility delivery.14
Table 4.
Proportion of women aged 15–49 years who reported that they have serious problems in accessing health care for themselves when they are sick, by type of problem in the 12 countries yet to eliminate maternal and neonatal tetanus7, 8
| Getting permission to go for treatment | Getting money for treatment | Distance to health facility | Not wanting to go alone | At least one problem accessing health care | |
|---|---|---|---|---|---|
| Afghanistan | 51% | 67% | 67% | 70% | 89% |
| Angola | 31% | 63% | 52% | 32% | 70% |
| Central African Republic | ND | ND | ND | ND | ND |
| Guinea | 30% | 60% | 46% | 32% | 68% |
| Mali | 27% | 41% | 29% | 20% | 47% |
| Nigeria | 11% | 46% | 26% | 16% | 52% |
| Pakistan | 21% | 30% | 42% | 58% | 67% |
| Papua New Guinea | 32% | 63% | 56% | 44% | 74% |
| Somalia | 50% | 65% | 62% | 47% | 73% |
| South Sudan | ND | ND | ND | ND | ND |
| Sudan | ND | ND | ND | ND | ND |
| Yemen | ND | ND | ND | ND | ND |
ND=no data available.
MNTE implementation, especially TTCV supplementary immunisation activities, in the 12 remaining countries has been hampered by other competing priorities, scarce funding, and poor focused attention on MNTE. Response to frequent disease outbreaks was the key impediment to implementation of planned MNTE activities and might remain so in the foreseeable future, given the susceptibility of these countries to frequent disease outbreaks.15 Of top priority to most of the 12 countries is the response to ongoing wild poliovirus transmissions in Afghanistan and Pakistan, and the outbreaks of circulating vaccine-derived polioviruses in 23 countries, including Angola, Central African Republic, Guinea, Mali, Nigeria, Somalia, Sudan, and Yemen, as well as measles outbreaks in Angola, Cameroon, Chad, Nigeria, South Sudan, and Sudan.16, 17 Additionally, prolonged outbreaks of yellow fever in Angola and Lassa fever in Nigeria have been reported.18, 19 In the face of frequent and prolonged diseases outbreaks in these countries, the implementation of MNTE becomes of a lower priority as resources (time, financial, and human) become less available.15
Protracted humanitarian crises, including armed conflicts, in parts of Afghanistan, Central African Republic, Mali, Nigeria, Somalia, South Sudan, Sudan, and Yemen have resulted in the destruction of health facilities, displacement of populations, including health workers, have reduced access to health services by populations, and have substantially delayed the implementation of MNTE. A 2018 UN humanitarian crisis report noted that ongoing conflict in Afghanistan continued to hamper maternal and child health, particularly in rural areas where 75% of women live.20 In the Central African Republic, of the total 1010 health facilities, 236 (23%) were not functional because they were completely or partially destroyed.21 In Yemen, an estimated 14·8 million people (>50% of the country's population) had little to no access to basic health care, including 8·8 million living in severely underserved areas. Medical materials were reported to be in chronically short supply, with only 45% of health facilities functioning.22 The United Nations Office for the Coordination of Humanitarian Affairs estimates that 1·2 million people (81% of whom are in Borno State) remain inaccessible to humanitarian agencies in northeast Nigeria as a result of a humanitarian crisis lasting over a decade.23
The COVID-19 pandemic has led to the postponement of TTCV supplementary immunisation activities planned for the first half of 2020 in seven countries (Central African Republic, Guinea, Mali, Nigeria, Pakistan, South Sudan and Yemen) until the second half of the year and into 2021, and TTCV supplementary immunisation activities were cancelled in three countries (Afghanistan, Papua New Guinea, and Sudan). These rounds of supplementary immunisation activities were targeting an estimated 18 million women of reproductive age in the ten countries.10
Discussion
Despite the discrepancies in coverage between the different data sources, analyses show that, except for a few countries, the performance indicators for MNTE in the remaining 12 countries are generally suboptimal, indicating poor implementation of MNTE strategies in these countries. The WHO-recommended approach of targeting women of reproductive age in high-risk districts with three rounds of TTCV supplementary immunisation activities enables a rapid build-up of immunity against tetanus and is the leading MNTE strategy, especially in the countries that have suboptimal routine immunisation programmes.24 This strategy, facilitated by country ownership, technical support from partners (WHO and UNICEF), and funding from donors, has helped to accelerate elimination.
Due mostly to poor technical capacity, health workers in many countries suboptimally adhere to the recommended practice of adequately screening and administering appropriate doses of TTCV to pregnant women during antenatal care visits. These health workers also do not have the skills to adequately and comprehensively record all TTCV doses administered to pregnant women, including those doses provided during previous pregnancies, which leads to an underestimation of livebirths that were protected at birth.2 The WHO recommendation of at least eight antenatal care contacts during each pregnancy increases the opportunity to administer TTCV to pregnant women, but implementation remains a challenge in countries with weak health systems.25 The Maternal Immunization and Antenatal Care Situation Analysis (MIACSA) project noted that countries that recommended at least four antenatal care contacts were more likely to have high PAB coverage (>90%).26 In most of the remaining 12 countries, TTCV2+, PAB, health facility delivery, and SBA coverages were lower than ANC1 coverage, suggesting missed opportunities to administer TTCV and to educate pregnant women about the importance of health facility delivery and SBA. In Angola, despite 82% ANC1 coverage in 2019, TTCV2+, PAB, health facility delivery and SBA coverages were 56%, 66%, 46%, and 50%, respectively—an indication of missed opportunities. A study in Lubumbashi, Democratic Republic of the Congo, showed that despite 93% of women having attended at least one ANC visit, only 61% received at least one dose of TTCV.27 This discrepancy between antenatal care and TTCV2+ coverage can be easily addressed by educating pregnant women and health-care providers, and ensuring availability of TTCV at antenatal care sites.
As reported through Demographic and Health Surveys or Multiple Indicator Cluster Surveys, the socioeconomic barriers to seeking health care could also lower clinic attendance of maternal and newborn services. Barriers to access to essential health services might be particularly worse in the remaining 12 countries, especially among marginalised communities and populations and in rural areas. Given that tetanus affects the poorest and most marginalised populations, deprioritising MNTE might worsen existing health inequities, which could constrain the achievement of the equity goal of universal health coverage. Ensuring that all pregnant women have access to clean deliveries and TTCV could be a path to strengthening the primary health care platform for the integrated delivery of essential maternal, newborn, child, and adolescent health services. Hence, supporting those 12 countries to achieve MNTE would facilitate the implementation of the equity agenda of the Sustainable Development Goals and Immunization Agenda 2030, which has the goal to ensure that everyone has access to immunisation services,28, 29 the 5·0 equity goal from Gavi, the Vaccine Alliance of reducing the number of children that have never been vaccinated in the past (zero dose),30 and the WHO Director-General's report on the Global Strategy for Women's, Children's and Adolescents’ Health (2016–2030).31 Using MNTE as a tracer to promote health equity could help to address the scarce financial and human resources to support MNTE activities in those countries, and would ensure a system-strengthening approach that would be sustainable to maintain MNTE.
The 12 countries that have not achieved MNTE are also facing common barriers to attaining global eradication or elimination goals for polio, measles, rubella, and other diseases preventable by vaccination. Compared with tetanus, countries usually prioritise the control of polio or measles over MNTE implementation, due to their high transmissibility and potential for outbreaks, including spread across borders.15 Given the common challenges across several disease initiatives, MNTE implementation in the remaining countries needs to tap into the experiences of the Global Polio Eradication Initiative and the other interventions delivered in humanitarian settings to reach displaced, nomadic, and conflict-affected populations with strong engagement of civil society and key community stakeholders. Additionally, those 12 countries could accelerate the implementation of TTCV supplementary immunisation activities by integrating the activities with polio, measles, cholera, yellow fever, and other supplementary immunisation activities for vaccine-preventable diseases.
The remaining 12 countries face multiple challenges to achieving MNTE, including poor political will, scarce technical and financial resources, humanitarian crises, and competing priorities.15 Hence, achieving, and documenting, MNTE in those countries would require new tools and methods. In addition to the previously highlighted potential of linking MNTE to health equity, engagement of civil society and communities, and integration of TTCV supplementary immunisation activities with other vaccine-preventable diseases, countries might need to use new methods for delivery of TTCV, such as the easy-to-use, compact, prefilled auto-disable devices, in remote and unsafe areas where low numbers of sufficiently trained health-care workforces might hinder the provision of injectable vaccines.15, 32
Disruptions of essential health services (including immunisation and reproductive, maternal, newborn, and child health) due to the COVID-19 pandemic were reported by many countries and TTCV supplementary immunisation activities were postponed or cancelled in seven (Central African Republic, Guinea, Mali, Nigeria, Pakistan, South Sudan, and Yemen) of the 12 countries.33, 34 A modelling study to estimate the indirect effects of the COVID-19 pandemic on maternal and child mortality in low-income and middle-income countries showed an 8–39% increase in maternal deaths per month, across 118 countries, and reduced coverage of four childbirth interventions, including clean delivery, would account for approximately 60% of the additional maternal deaths.35 The MNTE initiative needs to leverage on the ongoing global efforts to sustain essential health services, to ensure the continued delivery of maternal and neonatal services while countries are responding to the COVID-19 pandemic.
Some limitations were apparent in the current systematic review. Our study data emanate from sources that have known quality issues. With no access to the raw data from the various sources, we were unable to calculate summary statistics, including 95% CI, as the study relied on already calculated percentages for the various indicators. The WHO/UNICEF Joint Reporting Form-reported TTCV2+ underestimates the true tetanus protection among women of reproductive age. Low retention of home-based records by women of reproductive age results in recall biases during Demographic and Health Surveys or Multiple Indicator Cluster Surveys for TTCV2+ and PAB estimates. We were unable to assess the coverage of umbilical cord care practices, given that only two (Nigeria and Pakistan) of the 12 countries had this information in their Demographic and Health Survey or Multiple Indicator Cluster Survey reports. Additionally, because of the known under-reporting of neonatal tetanus cases by surveillance systems that are mostly suboptimal in these countries, our analyses did not include neonatal tetanus incidence. Strengthening neonatal tetanus surveillance and using tetanus seroprevalence data for triangulation of data sources could be used to improve on data quality for the purpose of validation of MNTE.15, 36
Conclusions
Despite the substantial progress towards MNTE, weak health systems, humanitarian and socioeconomic challenges, and more recently the COVID-19 pandemic, are hampering the achievement of MNTE in the remaining 12 countries. To overcome those challenges, countries need to implement innovative approaches, such as integrating MNTE activities with other health activities, using MNTE to promote health equity access, sensitising health-care workers on the vaccination of pregnant women during antenatal care, creating demand for immunisation and clean deliveries from pregnant women, and enabling non-traditional health workers to administer TTCV using simple devices, especially in remote and rural areas.
Data sharing
All data used in this paper are publicly available and can be shared by the corresponding author. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of WHO, UNICEF, and the Centers for Disease Control and Prevention.
Declaration of interests
We declare no competing interests.
Acknowledgments
Contributors
NY conceptualised the idea for this study, collected and analysed the data, and wrote the manuscript. HMS and RAT contributed to data abstraction and the write up and review of the manuscript. All other authors participated in the writing, reviewing, and editing of the manuscript, and have read and agreed to the published version of the manuscript. NY and RAT accessed and verified the data underlying the study.
Editorial note: the Lancet Group takes a neutral position with respect to territorial claims in published maps and institutional affiliations.
This is an Open Access article published under the CC BY-NC-ND 3.0 IGO license which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. In any use of this article, there should be no suggestion that WHO endorses any specific organisation, products or services. The use of the WHO logo is not permitted. This notice should be preserved along with the article's original URL.
References
- 1.WHO Maternal and neonatal tetanus elimination: the strategies. 2020. https://www.who.int/initiatives/maternal-and-neonatal-tetanus-elimination-(mnte)/the-strategies
- 2.WHO . Protecting all against tetanus: guide to sustaining maternal and neonatal tetanus elimination (MNTE) and broadening tetanus protection for all populations. World Health Organization; Geneva: 2019. [Google Scholar]
- 3.WHO Maternal and neonatal tetanus elimination: progress towards global MNT elimination. 2020. https://www.who.int/initiatives/maternal-and-neonatal-tetanus-elimination-(mnte)/progress-towards-global-mnt-elimination
- 4.WHO Maternal and neonatal tetanus elimination. 2020. https://www.who.int/initiatives/maternal-and-neonatal-tetanus-elimination-(mnte)
- 5.WHO Maternal and neonatal tetanus elimination: the partnership. 2020. https://www.who.int/initiatives/maternal-and-neonatal-tetanus-elimination-(mnte)/the-partnership
- 6.WHO Protection at birth (PAB) against neonatal tetanus and tetanus toxoid-containing vaccine (TT2+/Td2+) vaccination coverage. 2020. https://immunizationdata.who.int/pages/coverage/tt2plus.html?GROUP=Countries&YEAR=&CODE=
- 7.The DHS Program Demographic and Health Surveys. https://www.dhsprogram.com/Countries/
- 8.UNICEF Multiple Indicator Cluster Surveys (MICS) https://mics.unicef.org/surveys
- 9.WHO WHO–UNICEF coverage estimates data for protection at birth (PAB) time series. 2020. https://www.who.int/entity/immunization/monitoring_surveillance/data/PAB_estimates.xls
- 10.WHO Maternal and neonatal tetanus elimination: programmatic update. 2021. https://www.who.int/initiatives/maternal-and-neonatal-tetanus-elimination-(mnte)/programmatic-update
- 11.WHO Vaccine-preventable diseases: monitoring system. 2020 global summary. 2020. https://apps.who.int/immunization_monitoring/globalsummary/countries
- 12.World Bank World Bank Country and Lending Group—country classification. 2019. https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups
- 13.Fagbamigbe AF, Idemudia ES. Barriers to antenatal care use in Nigeria: evidences from non-users and implications for maternal health programming. BMC Pregnancy Childbirth. 2015;15:95. doi: 10.1186/s12884-015-0527-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gage AJ. Barriers to the utilization of maternal health care in rural Mali. Soc Sci Med. 2007;65:1666–1682. doi: 10.1016/j.socscimed.2007.06.001. [DOI] [PubMed] [Google Scholar]
- 15.WHO Report of the SAGE Working Group on Maternal and Neonatal Tetanus Elimination and Broader Tetanus Prevention. 2016. https://www.who.int/immunization/sage/meetings/2016/october/1_Report_of_the_SAGE_Working_Group_on_Maternal_and_Neonatal_Tetanus_27Sep2016.pdf
- 16.WHO Circulating vaccine-derived poliovirus type 2—global update. 2021. https://www.who.int/emergencies/disease-outbreak-news/item/circulating-vaccine-derived-poliovirus-type-2-global-update
- 17.I VACCINATE. New measles surveillance data from WHO. 2019. https://ivaccinate.org/new-measles-surveillance-data-from-who/
- 18.Relief Web The yellow fever outbreak in Angola and Democratic Republic of the Congo ends. 2017. https://reliefweb.int/report/democratic-republic-congo/yellow-fever-outbreak-angola-and-democratic-republic-congo-ends
- 19.WHO Emergencies, preparedness, response. Lassa fever—Nigeria disease outbreak news. 2020. https://www.who.int/emergencies/disease-outbreak-news/item/2020-DON245
- 20.Relief Web 2019 Afghanistan humanitarian needs overview. 2018. https://reliefweb.int/report/afghanistan/2019-afghanistan-humanitarian-needs-overview
- 21.Equipe Humanitaire Pays et Partenaires Plan de Réponse Humanitaire, Janvier–Décembre 2019. Republique Centrafricaine. Humanitarian Relief Plan—Central African Republic. 2019. https://reliefweb.int/sites/reliefweb.int/files/resources/2018_hrp_CAR_french-final.pdf
- 22.WHO Yemen humanitarian response plan 2017. 2017. https://www.who.int/emergencies/response-plans/2017/yemen/en/
- 23.United Nations Office for the Coordination of Humanitarian Affairs About OCHA Nigeria. https://www.unocha.org/nigeria/about-ocha-nigeria
- 24.WHO The “high-risk” approach: the WHO-recommended strategy to accelerate elimination of neonatal tetanus. Wkly Epidemiol Rec. 1996;71:33–36. [Google Scholar]
- 25.WHO WHO recommendations on antenatal care for a positive pregnancy experience. 2017. https://www.who.int/publications/i/item/9789241549912 [PubMed]
- 26.Giles ML, Mason E, Muñoz FM. Antenatal care service delivery and factors affecting effective tetanus vaccine coverage in low- and middle-income countries: results of the Maternal Immunisation and Antenatal Care Situational Analysis (MIACSA) project. Vaccine. 2020;38:5278–5285. doi: 10.1016/j.vaccine.2020.05.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Abel Ntambue ML, Françoise Malonga K, Dramaix-Wilmet M, Donnen P. Determinants of maternal health services utilization in urban settings of the Democratic Republic of Congo—a case study of Lubumbashi City. BMC Pregnancy Childbirth. 2012;12:66. doi: 10.1186/1471-2393-12-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.UN The Sustainable Development Goals Report 2016: leaving no one behind. 2016. https://unstats.un.org/sdgs/report/2016/leaving-no-one-behind
- 29.Immunization Agenda 2030: a global strategy to leave no one behind. 2021. http://www.immunizationagenda2030.org/ [DOI] [PubMed]
- 30.Gavi, the Vaccine Alliance Gavi 5·0 strategy: phase V (2021–2025) 2019. https://www.gavi.org/our-alliance/strategy/phase-5-2021-2025
- 31.WHO Global Strategy for Women's, Children's and Adolescents Health (2016–2030) https://www.who.int/life-course/partners/global-strategy/globalstrategyreport2016-2030-lowres.pdf [DOI] [PMC free article] [PubMed]
- 32.Quiroga R, Halkyer P, Gil F, Nelson C, Kristensen D. A prefilled injection device for outreach tetanus immunization by Bolivian traditional birth attendants. Rev Panam Salud Publica. 1998;4:20–25. doi: 10.1590/s1020-49891998000700004. [DOI] [PubMed] [Google Scholar]
- 33.WHO WHO and UNICEF warn of a decline in vaccinations during COVID-19. 2020. https://www.who.int/news/item/15-07-2020-who-and-unicef-warn-of-a-decline-in-vaccinations-during-covid-19
- 34.UNICEF Maternal and newborn health and COVID-19. 2020. https://data.unicef.org/topic/maternal-health/covid-19/
- 35.Roberton T, Carter ED, Chou VB. Early estimates of the indirect effects of the COVID-19 pandemic on maternal and child mortality in low-income and middle-income countries: a modelling study. Lancet Glob Health. 2020;8:e901–e908. doi: 10.1016/S2214-109X(20)30229-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.WHO Vaccine preventable diseases surveillance standards. Annex 2: tetanus serosurveys. 2018. https://www.who.int/immunization/monitoring_surveillance/burden/vpd/WHO_SurveillanceVaccinePreventable_25_Annex2_R2.pdf?ua=1
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data used in this paper are publicly available and can be shared by the corresponding author. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of WHO, UNICEF, and the Centers for Disease Control and Prevention.