Abstract
Aim: Choroid plexus papilloma (CPP) according to the latest WHO classification system in 2016 are an uncommon, benign (WHO grade I) neuroepithelial intraventricular tumor derived from choroid plexus epithelium, which can occur in both the pediatric and adult population. These tumors account for approximately 1% of all brain tumor 2-6% of pediatric brain tumors and 0.5% of adult brain tumors. Case presentation: A 2-year-old female is presented at the Pediatrics Clinic at the University Clinical Center of Kosovo in a febrile, lethargic state and the anterior fontanelle is tense and swollen. The patient’s parents indicate that symptoms such as food refusal, apathy, speechlessness and low mood were presented a week earlier. Conclusion: Choroid plexus papilloma is a rare tumor without specific clinical patterns or imaging findings. In our presentation we have presented the role of symptoms in the detected and diagnostic of choroid plexus papilloma. Not every headache is a symptom of choroid plexus papilloma.
Keywords: Choroid plexus papilloma, MRI, CT, choroid papilloma symptoms
Introduction
Choroid plexus papilloma are benign tumors that grow slowly, originating from the ventricles, from the epithelial cells of the choroid plexuses, most common in children, often accompanied by hydrocephalus.
The incidence of this disease is relatively small and represents 0.4-0.6% of all tumors.
This disease can occur at any age, but most often in children up to 10 years of age and is represented by 3% of all intracranial tumors of children [1,2,3].
A review of the literature shows that 48% of these tumors are found in children under the age of 10, of which 20% in infants under 1 year old.
The incidence is higher in males compared to females (1.6 to 1) [2].
Location varies with age. It is most common in the lateral ventricles in children and in adults in the IV ventricle.
Tumors of the lateral ventricles are mainly localized at the level of the trigonum, as well as in the temporal and frontal horns.
Development in the fossa cranii posterior of the choroid plexus papilloma occurs in the IV ventricle then laterally or outwards from the IV ventricle.
It can also be found at the level of cerebellopontine angles [4,5,6].
Tumor in the third ventricle is very rare.
The tissue of the choroid plexus papilloma as the ectopic embryonic remnant of tumor development is located in the brain convexity.
Clinical symptoms are different, depending on the course of the increase in intracranial pressure and CNS damage.
Most patients have hydrocephalus which is caused by the localization of the tumor in the ventricular system [7].
1. Obstructive hydrocephalus caused by direct obstruction of the CSF.
2. Overproduction of CSF-communicating hydrocephalus.
Patients with clinical signs of increased intracranial pressure-hydrocephalus is directly associated with the development and impact of tumor mass.
Babies show increased intracranial pressure by head enlargement, lethargy or irritation.
In older children and adults, it is manifested by headache, vomiting, papilledema, and in rare cases coma [8,9,10].
Limitation of CNS lesions varies by localization of the tumor mass.
Slight signs of pyramidal lesions are seen in the lateral ventricle.
In the third ventricle it indicates obstruction in vision, imitation of this is the localization in the posterior cranial fossa indicates ataxia, eye movement [9].
Case Presentation
We present the case of a 2-year-old female child, examined and diagnosed with MRI at the Prima Imaging Center, Prishtinë, Kosovo, hospitalized at the Pediatric Clinic of the University Clinical Center of Kosovo. Informed consent was given by the family for publication of the anonymized case data.
A week before admission, she became anorexic, apathetic and unable to speak.
On the day of admission, the child is febrile and lethargic and the anterior fontanelle is tense and inflated.
We have done an initial CT, showing a massive expansive process in right lateral ventricle with calcifications and hyper vascular. Also, we found hydrocephalus with periventricular edema (Figure 1). Examination with MRI presents signs of hyper productive hydrocephalus. The right lateral ventricle is much larger than the left and contains a large lobular mass located in the trigonum. The tumor manifested with low-hypointense signal at T1 generally lower than that of cerebral parenchyma but higher than that of CSF. The images in T2 (Figure 1) showed high signal (microcalcifications are presented with hypo signals). After application of IV contrast they showed pronounced signs of pathological vascularization (Figure 2).
Figure 1.

Choroid plexus papilloma in a 2 years-old female. Brain computed tomography, axial contrast enhanced
Figure 2.



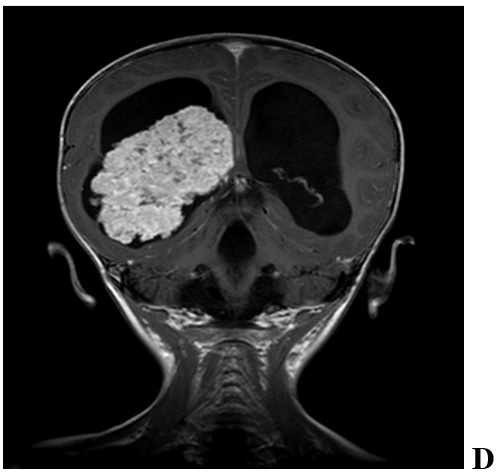


Radiographic features of a pediatric CPP in 2 year old female. We found significant hydrocephalus (A-F) with transependymal flow (F) due to either increased production of CSF or obstruction by tumor debris and blood products. Intraventricular and/or intratumoral hemorrhage are not uncommon. CPPs enhance on T1-weighted MRI with contrast (C,D and E) due to their rich vascular supply. They are generally iso-or hypointense on T1-and T2-weighted MRI (A, B and F) but may demonstrate heterogeneous hyperintensity in some cases. Magnetic resonance angiography may aid in visualizing the tumor’s vascular supply (C, D and F)
Histological findings are shown in Figure 3.
Figure 3.

Regulate, fibro-epithelial papillae without atypical cells, HE, 20x
During the surgery we found that the mass was well vascularized with transverse dimensions 62x60mm.
The pedicle has been identified as bound and removed from the tumor without difficulty.
The histopathological diagnostic confirmed the choroid plexus papilloma:
These tumors feature a single layer of cuboidal and columnar epithelium in a papillary configuration and covering a fibrovascular core.
The child has reached convalescence and the head has returned to nearly its normal size.
Discussion
CCPP is a gradual-developing, benign neoplasm that arises from the choroid plexus epithelium.
Choroid plexus tumors constitute a spectrum of neoplasms starting from well-differentiated papilloma’s (WHO grade I) to enormously aggressive choroid plexus carcinomas (WHO grade III), with uncommon intermediate forms known as “atypical CPP”, for which the biologic conduct is still to be defined [8].
Choroid plexus tumors account for 2%-4% of pediatric brain tumors, 0.5% of adult brain tumors, and up to 20% of pediatric neoplasms taking place within the 1st year of life [9,10].
The fourth ventricle is the most commonplace site of occurrence, followed by the lateral and third ventricles.
In children, it occurs more commonly in the lateral ventricles (80% of cases), whilst the fourth ventricle seems to be the favored site in adults.
Benign tumors are more commonplace in the fourth ventricle, while the anaplastic variety are seen more frequently within the lateral ventricle [11].
Rare cases of extra ventricular choroid plexus tumors have been reported [12,13].
CPP have a papillary or lobulated appearance, which helps differentiate them from other intraventricular neoplasms; conversely, carcinomas tend to have a more irregular contour [14].
Computed tomography (CT) scanning and magnetic resonance imaging (MRI) are the investigative methods of choice in the assessment of choroid plexus papilloma.
The classical CT findings of CPP have been reported as a well-defined, homogeneously enhancing, lobulated mass with an abnormal frond-like pattern, resulting in a cauliflower-like appearance typically seen in instances of intraventricular tumors [11,12,13,14].
Choroid plexus papilloma are very vascular lesions that show off avid enhancement at contrast-enhanced imaging. they are iso-to hyperattenuating at CT.
At MR imaging, these lesions are iso-to hypointense on T1-weighted images and iso-to hyperintense on T2-weighted images; flow voids are commonplace.
CPP have relatively homogeneous MRI signals. In addition, following contrast injection, CPP reveal excellent homogeneous or heterogeneous enhancement on T1-weighted imaging (T1WI) [10,11,12,13,14].
Conclusions
Choroid plexus papilloma is a rare tumor without specific clinical patterns or imaging findings.
In our presentation we have presented the role of symptoms in the detected and diagnostic of choroid plexus papilloma.
Not every headache is a symptom of choroid plexus papilloma.
Conflict of interests
None to declare.
References
- 1.Louis DN, Perry A, Reifenberger G, von Deimling A, Figarella-Branger D, Cavenee WK, Ohgaki H, Wiestler OD, Kleihues P, Ellison DW. The 2016 World Health Organization Classification of Tumors of the Central Nervous System: a summary. Acta Neuropathol. 2016;131(6):803–820. doi: 10.1007/s00401-016-1545-1. [DOI] [PubMed] [Google Scholar]
- 2.Louis DN, Ohgaki H, Wiestler OD, Cavenee WK, Burger PC, Jouvet A, Scheithauer BW, Kleihues P. The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol. 2007;114(2):97–109. doi: 10.1007/s00401-007-0243-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Smith AB, Smirniotopoulos JG, Horkanyne-Szakaly I. From the radiologic pathology archives: intraventricular neoplasms: radiologic-pathologic correlation. Radiographics. 2013;33(1):21–43. doi: 10.1148/rg.331125192. [DOI] [PubMed] [Google Scholar]
- 4.Chen Y, Zhao R, Shi W, Li H. Pediatric atypical choroid plexus papilloma: Clinical features and diagnosis. Clin Neurol Neurosurg. 2021;200:106345–106345. doi: 10.1016/j.clineuro.2020.106345. [DOI] [PubMed] [Google Scholar]
- 5.Glastonbury CM, Osborn AG, Salzman KL. Masses and malformations of the third ventricle: normal anatomic relationships and differential diagnoses. Radiographics. 2011;31(7):1889–1905. doi: 10.1148/rg.317115083. [DOI] [PubMed] [Google Scholar]
- 6.Zhang GB, Huang HW, Li HY, Zhang XK, Wang YG, Lin S. Intracranial chordoid glioma: A clinical, radiological and pathological study of 14 cases. J Clin Neurosci. 2020;80:267–273. doi: 10.1016/j.jocn.2020.09.019. [DOI] [PubMed] [Google Scholar]
- 7.McGirr SJ, Ebersold MJ, Scheithauer BW, Quast LM, Shaw EG. Choroid plexus papillomas: long-term follow-up results in a surgically treated series. J Neurosurg. 1988;69(6):843–849. doi: 10.3171/jns.1988.69.6.0843. [DOI] [PubMed] [Google Scholar]
- 8.Bahar M, Hashem H, Tekautz T, Worley S, Tang A, de Blank P, Wolff J. Choroid plexus tumors in adult and pediatric populations: the Cleveland Clinic and University Hospitals experience. J Neurooncol. 2017;132(3):427–432. doi: 10.1007/s11060-017-2384-1. [DOI] [PubMed] [Google Scholar]
- 9.Stafrace S, Molloy J. Extraventricular choroid plexus papilloma in a neonate. Pediatr Radiol. 2008;38(5):593–593. doi: 10.1007/s00247-007-0737-1. [DOI] [PubMed] [Google Scholar]
- 10.Stevens EA, Stanton CA, Nichols K, Ellis TL. Rare intraparenchymal choroid plexus carcinoma resembling atypical teratoid/rhabdoid tumor diagnosed by immunostaining for INI1 protein. J Neurosurg Pediatr. 2009;4(4):368–371. doi: 10.3171/2009.5.PEDS0955. [DOI] [PubMed] [Google Scholar]
- 11.Jaiswal AK, Jaiswal S, Sahu RN, Das KB, Jain VK, Behari S. Choroid plexus papilloma in children: Diagnostic and surgical considerations. J Pediatr Neurosci. 2009;4(1):10–16. doi: 10.4103/1817-1745.49100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhou WJ, Wang X, Peng JY, Ma SC, Zhang DN, Guan XD, Diao JF, Niu JX, Li CD, Jia W. Clinical Features and Prognostic Risk Factors of Choroid Plexus Tumors in Children. Chin Med J (Engl) 2018;131(24):2938–2946. doi: 10.4103/0366-6999.247195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Menon G, Nair SN, Baldawa SS, Rao RB, Krishnakumar KP, Gopalakrishnan CV. Choroid plexus tumors: an institutional series of 25 patients. Neurol India. 2010;58(3):429–435. doi: 10.4103/0028-3886.66455. [DOI] [PubMed] [Google Scholar]
- 14.Costa JM, Ley L, Claramunt E, Lafuente J. Choroid plexus papillomas of the III ventricle in infants. Report of three cases. Childs Nerv Syst. 1997;13(5):244–249. doi: 10.1007/s003810050077. [DOI] [PubMed] [Google Scholar]


