Abstract
A 70-year-old man with a history of hypertension was evaluated in our dermatology department due to the appearance of a clinical picture compatible with bullous pemphigoid that was confirmed histologically. The lack of response to topical and systemic immunosuppressive treatment resulted in omalizumab being prescribed in a multidisciplinary committee based on the clinical and analytical findings and the patient’s refusal to be treated with rituximab. The evaluation at 3 months showed the absence of blisters on the clinical examination. No associated adverse effects were observed. In the following 3 months the patient was administered medication at home in the absence of an anaphylactic reaction and with prior training by the nursing staff of the Hospital Pharmacy Service. After 6 months the medication was suspended with no relapses for 6 months since the last dose. Omalizumab, an anti-IgE monoclonal drug which has a good safety profile with minimum adverse side effects should be considered when there is a contraindication to the use of intravenous therapies (eg, immunoglobulins, rituximab) or prolonged immunosuppressive treatment (eg, methotrexate, azathioprine).
Keywords: allergy and immunology, clinical medicine, safety, dermatology, social medicine
Background
Bullous pemphigoid (BP) is an autoimmune bullous disease produced by IgG autoantibodies to BP180 or BP230, which clinically manifests as blisters and erosions of the skin and/or mucosa. The classic treatment is based on the use of high-potency topical corticosteroids, systemic corticosteroids and immunosuppressive drugs. However, novel treatments have emerged, some of which are currently being evaluated in clinical trials.
BP is a disease of low incidence and prevalence. This means that treatments must often be selected by case series, clinical practice guidelines and single case reports. Two monoclonal drugs are being used with relative success: rituximab (currently a phase III clinical trial has been completed: NCT00525616) and omalizumab (without planned clinical trials but with a better safety profile due to the experience obtained in severe allergic asthma and spontaneous chronic urticaria, as most of the side effects such as arthralgia or pain at the site of injection do not result in cessation of drug administration).
Case presentation
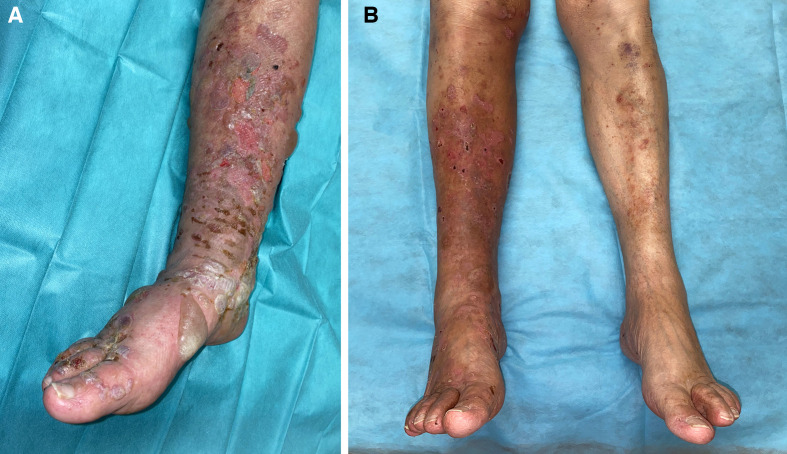
A 70-year-old man with a history of hypertension and dyslipidaemia was referred to our dermatological outpatient clinic with a blistering rash on the trunk and extremities for 3 months (figure 1A). Clinical examination showed tense blisters on an erythematous base in these locations. The blisters did not affect the face, palms and soles. The patient reported itching measured on a visual analogue scale of 9/10.
Figure 1.
(A) Tense blisters on the right leg with erosions. (B) Clinical outcome at 3 months with omalizumab treatment.
Investigations
Requested complementary tests including blood cell count, general biochemistry, thyroid profile, autoantibodies, erythrocyte sedimentation rate (ESR), immunoglobulins, C-reactive protein (CRP), Dimer D and complement showed results within normal except for eosinophils (0.59×10×3 mL, 6.9%), ESR (35 mm/hour) and IgE (7027 UI/mL).
Histological examination showed subepidermal blisters with an inflammatory infiltrate at the base of the blisters which was mainly lymphohistiocytic but rich in eosinophilic granulocytes and the latter dominated in the blisters. Superficial perivascular dermatitis was also present. By direct immunofluorescence, positive C3 (++) and IgG (+++) was identified at the basement membrane/dermo-epidermal limit of the sample with IgA and IgM weakly positive in the same location.
Treatment
Treatment was started with high-potency topical corticosteroids (clobetasol propionate 0.05% in maximum ointment 15 g/day) with no improvement after 30 days. Second-line treatment was prednisone 0.5 mg/day until symptom control and then progressive dose reduction until relapse when the dose fell below 10 mg/day. The addition of azathioprine as a corticosteroid-sparing drug did not achieve improvement with an elevation of ×3 transaminases. Treatment with methotrexate was ruled out because of the liver dysfunction previously reported with azathioprine. The patient was offered treatment with rituximab 2×1 g doses 14 days apart but he refused to sign an informed consent given the potential adverse effects of the drug (progressive multifocal leukoencephalopathy). The patient was fully informed of the relative evidence bases between rituximab and omalizumab.
A multidisciplinary committee consisting of hospital pharmacists and dermatologists approved treatment with omalizumab at a dose of 300 mg every 3 weeks according to the doses published in the literature and review of the patient’s condition. A decision was made to review at 3 months to determine the response and decide whether to continue treatment or not based on a review of the side effects at every visit.
Outcome and follow-up
The evaluation at 3 months showed the absence of blisters in the clinical examination (figure 1B). No associated adverse effects were observed. In the absence of an anaphylactic reaction and with prior training by nursing staff of the Hospital Pharmacy Service, the patient self-administered omalizumab at home for the following 3 months. After 6 months the medication was suspended with no relapse for 6 months since the last dose.
Discussion
BP is an autoimmune bullous disease characterised by the formation of subepidermal blisters due to the action of IgG antibodies against the BP180 and BP230 proteins of the hemidesmosomes of the keratinocytes of the basement membrane. Although they are mostly IgG-type antibodies, IgE-type antibodies have also been described and the participation of eosinophils in the pathophysiology of the disease has been postulated.1 Currently, approximately 25 patients have had a satisfactory BP response to omalizumab with a complete response reported in at least 19 of them. Elevated eosinophil levels and IgE levels have been seen in most of these patients.2 The existence of IgE antibodies against the NC16A domain of the BP180 protein has been demonstrated in 77% of the series of patients with BP studied, as well as linear deposits of IgE in the dermoepidermal junction in 41% of the patients.3 4 However, in the largest series of patients published, the basal levels of IgE and eosinophils did not predict the therapeutic response.5
Omalizumab is a recombinant humanised IgG1 monoclonal antibody against the FcERI receptor for IgE, the dose of which is adjusted according to IgE levels in severe allergic asthma but not in chronic spontaneous urticaria. In the case of BP, by partially blocking IgE it prevents mast cell degranulation and the subsequent release of inflammatory mediators including histamine, cytokines and proteases. Many of these mediators would be involved in the destruction of the dermoepidermal junction that generates the formation of blisters.6
BP is a disease that affects mainly elderly and polymedicated patients. The use of sustained immunosuppressive medication should be carefully evaluated for its potential adverse effects.7 Once the main therapeutic routes have been exhausted, omalizumab is postulated as an interesting therapeutic alternative. As it is an off-label medication, it is the responsibility of the hospital pharmacist to review the patient’s medical history, including previous pathology and possible drug interactions. There is no unanimous opinion on the standardised use of omalizumab in BP. The dose ranges from 300 mg/4 weeks to 300 mg/3 weeks with a clearance time ranging from 1 to 6 months. Concomitant treatment with systemic corticosteroids is normally necessary, which are usually suspended in cases of favourable evolution once at least 50% clearance has occurred.5 Our patient received the dose most commonly reported in the literature by the majority of authors.1 4 5 7 In contrast to most of them, concomitant treatment with systemic corticosteroids was not used in our patient. Although no randomised clinical trials regarding the use of omalizumab in BP have been started, dermatologists and pharmacists have learnt how to use it based on the experience with omalizumab in the management of bronchial asthma and chronic urticaria. One of its main advantages is the versatility of the dosage and individualised adjustment in relation to the clinical response. In most of the reported cases omalizumab was suspended after 6 months of treatment if there was a clinical response.1 4 In our case it was not necessary to reintroduce the medication but, in those cases where it was necessary, the initial response was recovered.
Omalizumab presents a good safety profile with a very low rate of adverse effects including anaphylactic reactions, arthralgia and injection site reactions. In cases where there is a contraindication to the use of intravenous therapies (eg, immunoglobulins, rituximab) or the patient refuses some treatment because of side effects or prolonged immunosuppressive treatment (eg, methotrexate, azathioprine), omalizumab is an alternative to consider.8 9 Prospective studies that allow optimising and defining a therapeutic protocol of consensual use between doctors and pharmacists are needed to determine which patients with BP would benefit from its use.
Patient’s perspective.
Our patient has greatly appreciated the treatment with omalizumab in BP, given the clinical result, and has emphasised the training process by the nursing staff of the hospital’s pharmacy service, which has allowed its home administration with a high score on the TSQM9 test.10
Learning points.
Bullous pemphigoid is an autoimmune bullous disease characterised by the formation of subepidermal blisters due to the action of IgG antibodies against the hemidesmosomes of the keratinocytes of the basement membrane.
Bullous pemphigoid is a disease that affects mainly elderly and polymedicated patients.
With regard to the use of omalizumab in bullous pemphigoid, as it is an off-label medication it is the responsibility of the hospital pharmacist to review the patient’s medical history, including previous pathology and possible drug interactions.
Omalizumab has a good safety profile with minimun adverse side effects. Its use should be considered when there is a contraindication to the use of intravenous therapies (eg, immunoglobulins, rituximab) or prolonged immunosuppressive treatment (eg, methotrexate, azathioprine) as recommended by the European Academy of Dermatology and Venereology.11
Footnotes
Contributors: FJN-T, JML-M, AA-R, BC-D and RR-V contributed equally to this article. RR-V conceptualised the idea of the article. BC-D, FJN-T and RR-V contributed to the evaluation and conclusion of the findings and follow-up of the patient. The survey was conducted by BC-D and RR-V. All authors contributed to the writing of the article.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
All data relevant to the study are included in the article.
Ethics statements
Patient consent for publication
Obtained.
References
- 1. Vico-Alonso C, Calleja-Algarra A, Aragón-Miguel R, et al. Omalizumab as an alternative therapeutic tool in the treatment of bullous pemphigoid: a case report. Dermatol Ther 2019;32:e12829. 10.1111/dth.12829 [DOI] [PubMed] [Google Scholar]
- 2. Yu KK, Crew AB, Messingham KAN, et al. Omalizumab therapy for bullous pemphigoid. J Am Acad Dermatol 2014;71:468–74. 10.1016/j.jaad.2014.04.053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Messingham KN, Pietras TA, Fairley JA. Role of IgE in bullous pemphigoid: a review and rationale for IgE directed therapies. G Ital Dermatol Venereol 2012;147:251–7. [PubMed] [Google Scholar]
- 4. Balakirski G, Alkhateeb A, Merk HF, et al. Successful treatment of bullous pemphigoid with omalizumab as corticosteroid-sparing agent: report of two cases and review of literature. J Eur Acad Dermatol Venereol 2016;30:1778–82. 10.1111/jdv.13758 [DOI] [PubMed] [Google Scholar]
- 5. Lonowski S, Sachsman S, Patel N, et al. Increasing evidence for omalizumab in the treatment of bullous pemphigoid. JAAD Case Rep 2020;6:228–33. 10.1016/j.jdcr.2020.01.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. El-Qutob D. Off-Label uses of omalizumab. Clin Rev Allergy Immunol 2016;50:84–96. 10.1007/s12016-015-8490-y [DOI] [PubMed] [Google Scholar]
- 7. Ewy S, Pham H, Quan K, et al. Successful omalizumab therapy for bullous pemphigoid despite transient reaction. J Drugs Dermatol 2019;18:947–9. [PubMed] [Google Scholar]
- 8. Seyed Jafari SM, Gadaldi K, Feldmeyer L, et al. Effects of omalizumab on FcεRI and IgE expression in lesional skin of bullous pemphigoid. Front Immunol 2019;10:1919. 10.3389/fimmu.2019.01919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Speeckaert R, Lambert J, van Geel N. Learning from success and failure: biologics for non-approved skin diseases. Front Immunol 2019;10:1918. 10.3389/fimmu.2019.01918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Atkinson MJ, Sinha A, Hass SL, et al. Validation of a general measure of treatment satisfaction, the Treatment Satisfaction Questionnaire for Medication (TSQM), using a national panel study of chronic disease. Health Qual Life Outcomes 2004;2:12. 10.1186/1477-7525-2-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Feliciani C, Joly P, Jonkman MF, et al. Management of bullous pemphigoid: the European Dermatology Forum consensus in collaboration with the European Academy of Dermatology and Venereology. Br J Dermatol 2015;172:867–77. 10.1111/bjd.13717 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data relevant to the study are included in the article.