Abstract
Objectives
Clinical pharmacy services in German hospitals appear to be underdeveloped compared with other European countries. However, recent developments have increased the interest in expanding these services. Detailed data about the current state of clinical pharmacy services in Germany are lacking. This survey establishes the current level of pharmacy services in Germany and the barriers to implementation.
Methods
An online survey conducted in 2017 was distributed to directors of all 389 German hospital pharmacies. The survey contained 26 questions addressing hospital and pharmacy characteristics, clinical pharmacy services provided, the number of clinical pharmacists and the frequency as well as the quality assurance of these services.
Results
There were 133 responses (34%). Of these, 84 (63%) pharmacies provided some form of clinical pharmacy services. Based on the 389 contacted pharmacies, a clinical pharmacy service is available in at least 22% of hospital pharmacies in Germany. On average there are 2.4 full-time equivalent (FTE) clinical pharmacists per hospital employed, although there is a wide variation in numbers (0.3–22 FTE) and service provision between hospitals. Clinical pharmacy services are generally provided on a daily or weekly basis, with a principal focus on general surgery, critical care and general medicine wards.
Conclusions
This is the first survey providing a detailed picture of clinical pharmacy services in Germany. There is wide variation in clinical service provision among hospitals, with some hospitals having developed a comprehensive range of clinical services. Compared with other countries, particularly the UK where the focus has shifted to provision of 7-day clinical services, the gap in clinical pharmacy services remains large. The focus should be turned to refining clinical pharmacy services in hospital admissions and discharge planning while also improving Health IT, the opportunities for specialisation and aligning education in accordance with the EAHP common training framework.
Keywords: Germany; surveys and questionnaires; pharmacy service, hospital; clinical pharmacy; hospital pharmacy education
Introduction
Clinical pharmacy services play an important role in providing safe patient care in hospitals and have developed steadily over the last decades.1 Initially, these services began with pharmacists participating on ward rounds or completing chart reviews in the clinical setting.2 The role of the pharmacist has now expanded to clinical specialisation, managing outpatient clinics, and even using prescribing rights within their area of expertise in some countries.3 These advances have raised the profile and recognition of the role of clinical pharmacists worldwide, but there are still large variations in the clinical pharmacy services provided both within and across other countries.4
When compared with other European countries, the German healthcare system provides a reasonable quality of care for a relatively high cost; however, clinical pharmacy services continue to lag behind other countries. In 2010 Germany ranked 25th out of 28 European countries with regard to the number of pharmacists (hospital and community) per 100 000 inhabitants with only 64 pharmacists per 100 000 inhabitants, which is 20 pharmacists per 100 000 inhabitants below the European average and 60 pharmacists per 100 000 inhabitants below the top country.5 Despite low numbers of total pharmacists in comparison with other European countries, there are even fewer pharmacists working in the hospital setting. Only 2000 of the 50 000 pharmacists in Germany work in hospitals.6 The European Association of Hospital Pharmacists (EAHP) survey from 2010 showed that only about 10% of hospital pharmacies in Germany provide daily visits to the wards compared with 85% in the UK.4 The UK has been leading the way when it comes to the development of clinical pharmacy services in Europe, which is reflected by the available pharmacists per 100 hospital beds (UK 4.35, Germany 0.4).4 7 The UK has also developed a comprehensive foundation programme and framework to recognise expert clinical practice by the Royal Pharmaceutical Society.8
The continuing trend of pharmacy department closures within hospitals restricts the further development of clinical services in Germany.6 However, the interest in expanding clinical services within the pharmacy profession remains high. The German Association of Hospital Pharmacists (ADKA) declared the introduction of ‘Closed Loop Medication Management’ as a target for the profession by 2021. In this vision, clinical pharmacists and digitalisation of the medication process play a central role in ensuring the safe and effective use of medicines. The goal is to establish clinical pharmacists in German hospitals by 2021.9
The German efforts to establish clinical pharmacy go back to 2001, when changes were made to the Pharmacy undergraduate degree to include Clinical Pharmacy in the curriculum. However, further changes in education continue to be demanded by pharmacists10 and students alike.11 Additionally, there has been growing political support to move the development forward. In 2018, following a series of murders in two hospitals by a nurse, clinical pharmacy services were identified as a means of strengthening the safe use of medicine in clinical areas. A law was passed obligating hospitals to provide clinical pharmacy services in the federal state of Lower-Saxony, forcing pharmacy departments to begin developing clinical services. Owing to the federal system in Germany, the law is not valid in other federal states. However, the passing of the law promoted discussions about clinical pharmacists in national and federal political committees.12 Furthermore, there is a gap between sufficient healthcare professionals and increasing demands for quality of care.13 This provides opportunities for pharmacists to play a central role within interdisciplinary clinical teams.
The EAHP survey from 2010 provided a benchmark for clinical services across Europe.4 Although the survey gave some insight into clinical services across countries, the statistics date back to 2010 and clinical services were just one aspect among others.4 Given the recent developments in Germany, the aim of our survey was to analyse the current level of clinical pharmacy services in detail and possible barriers.
Methods
A literature review was conducted to identify surveys evaluating clinical pharmacy services on a national and international level. Evaluations of surveys from Poland,14 Switzerland,15 EAHP4 and the American Society of Health-System Pharmacists (ASHP)16 were considered for designing a questionnaire. An online questionnaire was designed using the Tool SoSci Survey (Version 2.6.00-i, questionnaire available as online supplement). The questionnaire was reviewed, tested and approved by the Clinical Pharmacy Services working group of ADKA, referred to as the ADKA Working Group.
An initial screening question was used to determine if pharmacy departments provided clinical services. Only those institutions that stated they had a clinical pharmacy service were guided to the subsequent set of clinical pharmacy questions. The questionnaire contained three main sections with 26 questions in total. The first section focused on the hospital and pharmacy characteristics; the second section assessed the clinical pharmacy services provided, number of clinical pharmacists, clinical areas of services and frequency of these services; and the third section addressed the quality assurance of these services, work experience and pharmacist qualifications. In order to get a comprehensive understanding, some questions allowed additional free-text comments.
Using the ADKA email distribution list, all German hospital pharmacy directors (n=389) were sent an announcement letter with a personalised link to the online survey via email. The survey was conducted over an 8-week period between February 2017 and April 2017. The directors were reminded twice via email. Hospitals that outsourced their pharmacy service were not included.
The results were compiled anonymously by the online survey tool and the data were analysed using Microsoft Excel (Microsoft Office 2010). The results and additional free-text comments were discussed within the ADKA Working Group.
Results
Of the 389 directors contacted, 133 (34%) completed the questionnaire. Of the 133 survey respondents, 84 (63%) departments provided any clinical pharmacy service and 11 (8%) had plans to develop one. Of the survey respondents, 38 (28%) provided no clinical service. Based on all 389 contacted departments, a clinical service is available in at least 22% of pharmacy departments in Germany.
The following results refer to the 84 hospitals who reported having a clinical pharmacy service, unless otherwise stated.
Clinical pharmacy services
Table 1 provides an overview of the available service and staffing levels within different hospital categories. On average, there are 2.4 full-time equivalent (FTE) clinical pharmacists per hospital, ranging from 0.3 to 22.0 FTE. The median FTE clinical pharmacists per hospital is 1.3, which shows that the number of clinical pharmacists are not normally distributed, but there are few hospitals with many clinical pharmacists while the majority of hospitals have few clinical pharmacists.
Table 1.
Staffing levels in pharmacy departments with clinical pharmacy services (n=84)
| Clinical pharmacy services across types of hospitals | ||||||
| University hospitals | Maximum care hospitals | General hospitals | Psychiatric hospitals | Other | Total | |
| Number of pharmacies | 20 | 19 | 30 | 2 | 13 | 84 |
| All pharmacist FTE | 295 | 160 | 127 | 9 | 50 | 641 |
| Clinical pharmacist FTE (% of all pharmacists) | 86 (29%) | 22 (14%) | 72 (57%) | 8 (89%) | 13 (25%) | 201 (31%) |
| Number of clinical pharmacists | 120 | 58 | 108 | 9 | 25 | 320 |
| Average clinical pharmacist FTE per hospital (min–max) | 4.3 (0.8–15.5) | 1.2 (0.3–4.8) | 2.4 (0.3–22.0) | 4.0 (1.0–7.0) | 1.0 (0.5–4.5) | 2.4 (0.3–22.0) |
| Median clinical pharmacist FTE per hospital | 2.7 | 1.0 | 1.0 | 4.0 | 0.5 | 1.3 |
FTE, full-time equivalent.
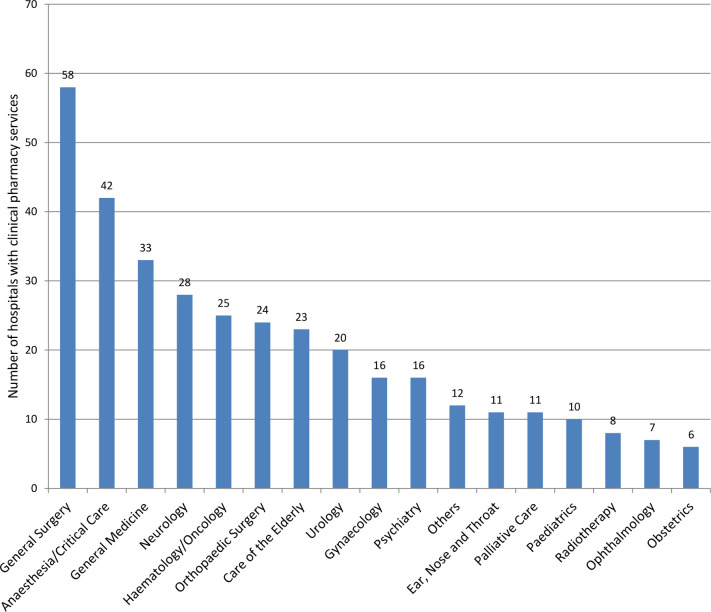
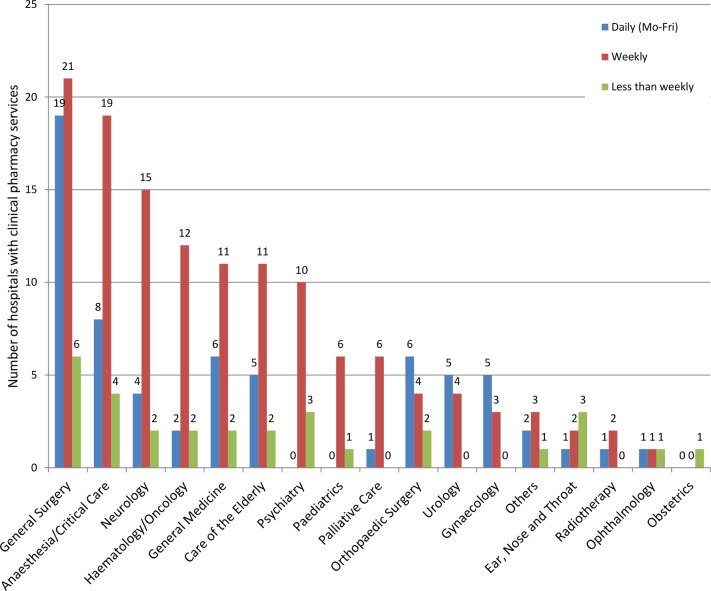
Clinical pharmacy services are generally provided on a daily or weekly basis with a principal focus on general surgery, critical care and general medicine wards (figures 1 and 2). Differences exist between areas of services. Clinical services in general surgery are split nearly evenly between daily (Monday to Friday) and weekly provisions. Almost all other areas (eg, high-risk areas such as critical care, neurology and haematology/oncology) on average only receive weekly provisions. Twenty-eight of the 84 (33%) hospitals with clinical pharmacy services reported having a daily service (Monday to Friday) on at least one ward, 45 (54%) provided clinical services weekly and 17 (20%) less than weekly (multiple answers possible). Based on the 133 completed questionnaires, the quota for a daily clinical service is 21%.
Figure 1.
Clinical pharmacy services provided according to clinical specialty (n=84).
Figure 2.
Frequency of clinical pharmacy services according to clinical specialty (n=84).
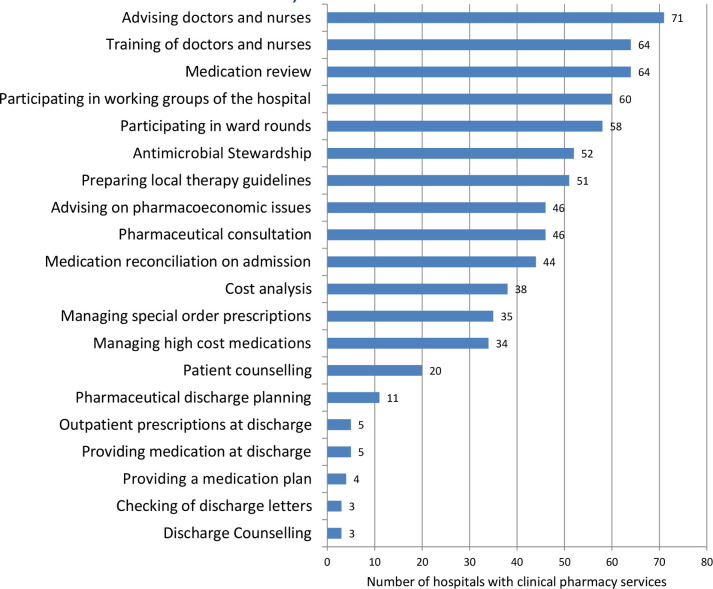
A wide range of services is carried out by pharmacists (figure 3). The most frequent services provided are pharmacy consultations (n=71 departments) and training for nursing and medical staff (n=64). Where services are already established, the major focus is on admission and support during the hospital stay. There is a strong focus on medicines management with 64 pharmacy departments providing medication review, 58 participating in ward rounds and 44 providing comprehensive medication reconciliation on admission.
Figure 3.
Range of clincal pharmacy services covered (multiple answers allowed, n=84).
Only a small number of services focus on medicine management at discharge (dedicated services: 11 departments, provision of medicines for discharge: 5, check and support for medicines in the discharge letter: 3, individualised patient medication list: 4, outpatient prescriptions at discharge: 5). Similarly, patient education is infrequently provided (20 departments counsel patients during their hospital stay and 3 at discharge).
Seventy-two departments (86% of departments with clinical pharmacy services) have at least one pharmacist with a specific qualification for the provision of clinical pharmacy services. Sixty-five departments (77%) have at least one pharmacist who has had experience as a clinical pharmacist for at least 2 years and 55 (65%) employ pharmacists who are undertaking or have completed training in antimicrobial stewardship or infectious diseases. The absolute number of pharmacists with these qualifications was not determined.
Quality assurance
There are currently no standardised quality indicators for the provision of clinical pharmacy services in German hospitals. Nevertheless, half of the departments with clinical pharmacy services provide internal training for clinical pharmacists and clinical standards to which they must adhere (n=44 (52%) and n=43 (51%), respectively). A quarter of all departments conduct regular audits to evaluate the performance of these services.
Documentation of the pharmacists’ interventions are carried out in most of the departments providing clinical pharmacy services, with 58 (69%) recording and evaluating the interventions. Furthermore, 41 (49%) document the pharmacists’ interventions within the medical notes. The central recording tool for medication errors and pharmacists’ interventions of the ADKA (DokuPIK) is used by a third of all departments, another third use Microsoft Excel tables, and another third use individual solutions or an alternative programme.
Electronic prescribing systems are only available in 27 (32%) of the 84 hospitals providing a clinical pharmacy service with another 20 (24%) planning the implementation of a system.
There is a strong focus on qualification, standardisation and internal training in over half of the departments and the majority (n=73 departments, 87%) would be interested in a joined approach to expanding the networking between hospitals.
Discussion
Comparison with other countries
This survey revealed that clinical pharmacy services are available in at least 22% of German hospitals and are still currently developing. There is a gap in services when compared with the UK and USA as outlined in the EAHP4 7 and ASHP surveys.16 One major difference is that, in the UK, the focus is on provision of 7-day clinical services17 and the most frequent mode of clinical service provision in Germany is weekly. The quota for daily clinical service of 21% (out of 133 completed questionnaires) suggests a slight improvement compared with the quota of 10% from the EAHP survey in 2010.4 However, there is a risk of bias as both surveys have response rates of only 30%, and our survey is likely to over-represent respondents with an interest in clinical pharmacy while the EAHP survey covered different aspects of pharmacy services. Therefore, it is not possible to say that there has been an improvement in the quota of daily clinical pharmacy visits in Germany from 2010 to 2017.
Although services in general surgery are provided daily from Monday to Friday or weekly, other areas are still lagging behind. This is particularly worrying in areas like intensive care and haematology/oncology as this includes areas where medication usage is critical and utilisation of high-risk medication is frequent. For example, the PROTECTED study in the UK recorded over 3200 interventions by clinical pharmacists in a 2-week period in 21 critical care units, with 1393 classified as medication errors and 1693 classified as medication optimisations.18 It is unlikely that critical care provisions in Germany are vastly different from the UK and therefore the need for pharmacy services should be similar. Progress has been made in Germany with the initial step of developing clinical specialty areas, but further work is needed to provide a consistent service on a daily basis. This will require both funding and the development of core structural training, as highlighted by the EAHP common training framework, including the provision of specialist training opportunities.19
Clinical pharmacy services
The current services offered by pharmacies mainly focus on support during the hospital stay. However, with resources still limited, medication review and ward rounds are provided by some pharmacy departments but are not yet available by all.
Medication reconciliation on admission has been highlighted by the WHO in the High 5 Project.20 21 Additionally, changes in German legislation in October 2017 mandated comprehensive discharge planning. Despite the focus on admission and discharge, according to our survey, only 52% of pharmacy departments who offer clinical services (n=84) provide services during the admission process and 13% during discharge. Based on the 133 survey respondents, only 33% of departments provide admission services. In contrast, in the UK in May 2017, 76% of all patients in an acute setting received medicine reconciliation within 24 hours of admission.22
The survey results also advocate an interdisciplinary approach. Most pharmacy departments are providing consultation, training for nursing and medical staff, as well as participating in interdisciplinary working groups within the hospital.
Differences between hospital types
The scope of service provision is also variable given the number of clinical pharmacists in each pharmacy department. A difference exists between university, general and maximum care hospitals in the number of pharmacists, both in FTE and percentage of clinical pharmacists; there is also a wide range within each group (table 1). In Germany, the hospital types differ in their range of offered clinical specialties and available beds, with general hospitals offering basic care, and maximum care and university hospitals offering a broad range of clinical specialties. A few pharmacy departments have developed comprehensive clinical services, which is reflected by the current number of pharmacists. One district general hospital employed the highest number of clinical pharmacists in the survey, which shows that opportunities are not only limited to university hospitals.
Workforce education and training
With all these challenges there is a need for a highly skilled workforce to provide these services. The results show there is a minimum of one qualified pharmacist available in the majority of departments with clinical pharmacy services, although absolute numbers of pharmacists with qualifications were not determined in this survey.
The current debate within the profession revolves around what is required to provide clinical pharmacy services, what should be taught at the university level and post-graduation qualifications. The argument for increasing the level of clinical pharmacy education at universities has recently been made by the profession10 and students alike.11
There are currently postgraduate qualifications in infectious diseases, geriatrics and oncology, but there is a lack of training opportunities in other specialty areas such as paediatrics, critical care and mental health.
Health IT
The lack of IT infrastructure is an additional problem affecting efficient clinical services in Germany. In our survey, 32% of the hospitals with clinical pharmacy services had an electronic prescribing system in place and 24% were planning to, compared with 95.6% of US hospitals in the latest survey by the ASHP.23 One important aspect of using electronic health records or electronic prescribing systems is the access outside the boundaries of a clinical service area. As pharmacist resources are already limited and pharmacy departments provide services to numerous sites, access to electronic health records would allow for the prioritisation of patients and reduction of drug-related problems at the transition of care. This would open the opportunity to shift the focus from drug distribution tasks to the evaluation of drug-related therapies and the optimisation of patient care across sectors.
Limitations of study
The response rate of only 34% implies that there is a risk of respondent bias, meaning that mainly departments with an interest in the development of or with current service provision would be over-represented. The EAHP survey from 2010 had a similar response rate for Germany of 31%, meaning that both surveys have the risk of bias. Another limitation is that only hospital pharmacy departments were contacted, so hospitals who receive their medicines from community pharmacies were not included. Another limitation to consider is that in Germany there are numerous projects evaluating the impact of pharmacists in clinical settings, which may or may not have been included in this survey.24 Although these projects help to generate the evidence for clinical services in the German setting, they do not always translate into permanent positions or go beyond the scope after the projects are completed.
The exact number of pharmacists per hospital bed represented was not retrieved in the survey. Bed numbers were clustered according to the German standard classification: <400, 400–800 and >800 beds. This did not permit a detailed analysis of the number of pharmacists per inpatient hospital bed.
There is an ongoing debate in Germany about the definition of ‘clinical pharmacy services’ and the role of a ‘clinical pharmacist’. Despite providing the definition in line with the American College of Clinical Pharmacy,25 some participants may have interpreted the term in a wider context, including any pharmacist working in the hospital setting, even those without direct patient contact. Thus, the current number of clinical pharmacists in this survey could be overestimated.
Conclusion
This survey demonstrates that clinical pharmacy services are currently available in at least 22% of German hospitals, but there is a wide variation of what these clinical service provisions involve. When compared with other countries, particularly the UK where the focus has shifted to the provision of 7-day clinical services, the gap in clinical pharmacy services remains very large. Similar to other countries, we see clinical pharmacy services as one way to minimise patient harm related to medicine. In Germany, public awareness of medication and patient safety and the role of the clinical pharmacist to improve both is needed. The lack of sufficient healthcare professionals, changes in the legal framework for discharge management and mandatory clinical pharmacy services will help reach the goal of establishing clinical pharmacists in German hospitals by 2021. The focus should be turned to refining clinical pharmacy services in hospital admissions and discharge planning, the opportunities for specialisation, aligning education in accordance with the EAHP common training framework and improving Health IT.
What this paper adds.
What is already known on this subject
Clinical pharmacy services in Germany appear to be less developed compared with other European countries.
Detailed and current data are lacking.
What this study adds
A detailed picture of clinical pharmacy services in Germany in 2017.
ejhpharm-2019-001973supp001.pdf (113.7KB, pdf)
Acknowledgments
We would like to thank all participants of the survey, Stephanie Fischer for the technical support designing the online survey and Stephen Bueno for proofreading.
Footnotes
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
No data are available.
Ethics statements
Patient consent for publication
Not required.
References
- 1. Bond CA, Raehl CL. Clinical pharmacy services, pharmacy staffing, and adverse drug reactions in United States hospitals. Pharmacotherapy 2006;26:735–47. 10.1592/phco.26.6.735 [DOI] [PubMed] [Google Scholar]
- 2. Leape LL, Cullen DJ, Clapp MD, et al. Pharmacist participation on physician rounds and adverse drug events in the intensive care unit. JAMA 1999;282:267–70. 10.1001/jama.282.3.267 [DOI] [PubMed] [Google Scholar]
- 3. Viktil KK, Blix HS. The impact of clinical pharmacists on drug-related problems and clinical outcomes. Basic Clin Pharmacol Toxicol 2008;102:275–80. 10.1111/j.1742-7843.2007.00206.x [DOI] [PubMed] [Google Scholar]
- 4. Frontini R, Miharija-Gala T, Sykora J. EAHP survey 2010 on hospital pharmacy in Europe: Parts 4 and 5. Clinical services and patient safety. Eur J Hosp Pharm 2013;20:69–73. 10.1136/ejhpharm-2013-000285 [DOI] [Google Scholar]
- 5. Eurostat . Healthcare personnel in the EU, 2015. Available: https://ec.europa.eu/eurostat/statistics-explained/images/8/84/Healthcare_personnel_in_the_EU-changed.jpg [Accessed Jan 2019].
- 6. ABDA . Die Apotheke - Zahlen, Daten, Fakten ABDA – Bundesvereinigung Deutscher Apothekerverbände e. V 2018.
- 7. Frontini R, Miharija-Gala T, Sykora J. EAHP survey 2010 on hospital pharmacy in Europe: Part 1. General frame and staffing. Eur J Hosp Pharm 2012;19:385–7. 10.1136/ejhpharm-2012-000162 [DOI] [Google Scholar]
- 8. Duggan C. RPS faculty: development opportunities and evidence of progression. Pharmaceutical J 2013;290. [Google Scholar]
- 9. Dörje F, Haber M, Baehr M. Closed loop medication management. Management & Krankenhaus 9/2018, S. 24. Weinheim: WILEY-VCH Verlag GmbH & Co. KGaA, 2018. [Google Scholar]
- 10. ADKA . Grundpositionen der ADKA e. V. zu aktuellen Fragestellungen der pharmazeutischen Ausbildung (Universitätsstudium und PJ) und der Postgraduierten-Weiterbildung. Krankenhauspharmazie 2018;39. [Google Scholar]
- 11. BPhD . Bundesverband der Pharmaziestudierenden in Deutschland e.V. - Thesenpapier zur Bewertung und Überarbeitung der Approbationsordnung und Verbesserung des Pharmaziestudiums 2016.
- 12. https://www.deutsche-apotheker-zeitung.de/news/artikel/2018/10/31/stationsapotheker-allein-laendersache/chapter:2 [Accessed Jun 2019].
- 13. Lauxen O, Bieräugel R. Der Hessische Pflegemonitor. Transparenz über regionale Pflegearbeitsmärkte. Bundesgesundheitsblatt-Gesundheitsforschung-Gesundheitsschutz 2013;8:1056–63. [DOI] [PubMed] [Google Scholar]
- 14. Pawłowska I, Pawłowski L, Kocić I, et al. Clinical and conventional pharmacy services in Polish hospitals: a national survey. Int J Clin Pharm 2016;38:271–9. 10.1007/s11096-015-0234-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Messerli M, Maes KA, Hersberger KE, et al. Mapping clinical pharmacy practice in Swiss hospitals: a cross-sectional study. Eur J Hosp Pharm 2016;23:314–9. 10.1136/ejhpharm-2015-000868 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Pedersen CA, Schneider PJ, Scheckelhoff DJ. ASHP national survey of pharmacy practice in hospital settings: Dispensing and administration—2014. Am J Health Syst Pharm 2015;72:1119–37. 10.2146/ajhp150032 [DOI] [PubMed] [Google Scholar]
- 17. NHS England . Transformation of seven day clinical pharmacy services in acute hospitals. In: Office of the Chief Pharmaceutical Officer MD, ed, 2016: 1–36.
- 18. Shulman R, McKenzie CA, Landa J, et al. Pharmacist’s review and outcomes: treatment-enhancing contributions tallied, evaluated, and documented (PROTECTED-UK). J Crit Care 2015;30:808–13. 10.1016/j.jcrc.2015.04.008 [DOI] [PubMed] [Google Scholar]
- 19. EAHP . The Common Training Framework (CTF) Online: European Association of Hospital Pharmacists, 2017. Available: https://static1.squarespace.com/static/56d2b676746fb93b0ba3e3d8/t/5a6f4b3b53450a84e9ef0e48/1517243196884/CTF+EAHP-Competency+framework.pdf [Accessed Jan 2019].
- 20. ÄZQ . Internationales high 5s-Projekt, SOP medication reconciliation (MedRec) bei Aufnahme: ÄZQ, Aktionsbündnis Patientensicherheit, BMG, 2014. Available: https://www.aezq.de/mdb/edocs/pdf/patientensicherheit/merkblatt-medication-reconciliation.pdf [Accessed Jan 2019].
- 21. WHO . The High 5s Project. Standard Operating Protocol - Assuring Medication Accuracy at Transitions in Care: Medication Reconciliation. Version 3, 2014. Available: https://www.who.int/patientsafety/implementation/solutions/high5s/h5s-sop.pdf [Accessed Jan 2019].
- 22. NHS safety thermometer: medication. Available: https://www.safetythermometer.nhs.uk/index.php?option=com_dashboard&view=dashboard&id=2&Itemid=335 [Accessed Jun 2019].
- 23. Pedersen CA, Schneider PJ, Scheckelhoff DJ. ASHP national survey of pharmacy practice in hospital settings: prescribing and transcribing—2016. Am J Health Syst Pharm 2017;74:1336–52. 10.2146/ajhp170228 [DOI] [PubMed] [Google Scholar]
- 24. ADKA . Kurzvorträge der 8. LAUD-Forschungs- und Doktorandentagung - Abstracts der Kurzvorträge der Tagung am 23. und 24. November 2018 in Dresden. Krankenhauspharmazie 2019;40. [Google Scholar]
- 25. American College of Clinical Pharmacy . The definition of clinical pharmacy. Pharmacotherapy 2008;28:816–7. 10.1592/phco.28.6.816 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
ejhpharm-2019-001973supp001.pdf (113.7KB, pdf)
Data Availability Statement
No data are available.