Abstract
Objective
The risk factors associated with urinary tract infections (UTIs) in patients with SLE remain uncertain. We evaluated the vaginal microbiota pattern and its potential UTI-associated risk factors.
Methods
A pilot cross-sectional study of patients with SLE was conducted at Ramathibodi Hospital, Bangkok, Thailand, during 2019–2020. Patients’ demographic data and relevant information were collected. Vaginal microbiota was assessed in all patients and in 10 healthy volunteers.
Results
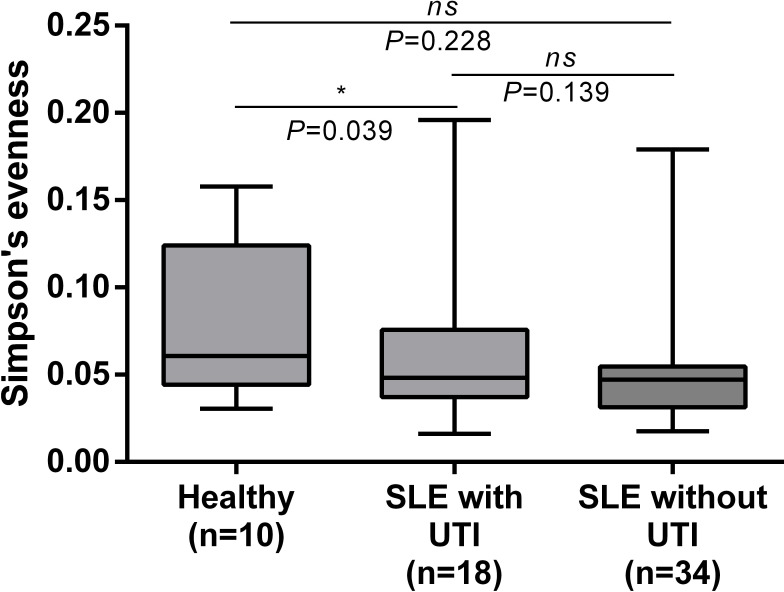
Fifty-two patients were enrolled (mean age: 46.1 years). All patients had SLE that was in low disease activity. As per the Simpson_e index, the within-group alpha diversity of the vaginal microbiota was low in the SLE with UTI and SLE receiving trimethoprim-sulfamethoxazole (TMP-SMX) prophylaxis groups. Multivariate logistic regression analysis revealed that TMP-SMX prophylaxis (adjusted OR (AOR), 30.96; 95% CI 3.63 to 264.11; p=0.002), elevated C3 levels (AOR, 35.33; 95% CI 1.33 to 936.67; p=0.033) and presence of Veillonella dispar in the vaginal microbiota (AOR, 6.68; 95% CI 1.27 to 35.07; p=0.025) were associated with UTI.
Conclusions
The vaginal microbiota diversity differed between patients with lupus with and without UTI, and unnecessary administration of TMP-SMX prophylaxis may affect the alpha diversity of the vaginal microbiota.
Keywords: therapeutics, lupus erythematosus, systemic, inflammation
Key messages.
What is already known about this subject?
Urinary tract infections (UTIs) in patients with SLE remain a critical infectious complication that increases patients’ morbidity and mortality.
Comprehensive potential risk factors and vaginal microbiota patterns associated with UTI are unreported in this population.
What does this study add?
Vaginal microbiota diversity differs between patients with SLE with UTI and those without UTI.
Unnecessary use of trimethoprim-sulfamethoxazole prophylaxis may affect the alpha diversity of the vaginal microbiota.
How might this impact on clinical practice or future developments?
This study reflects unnecessary treatment and provides evidence to support discontinuing trimethoprim-sulfamethoxazole prophylaxis in patients with SLE who are receiving low-level immunosuppressive agents.
Introduction
SLE is a chronic autoimmune disease involving multiple organ systems.1 Infections can trigger the body’s immune response, which aggravate the SLE disease activity and result in morbidity and mortality in these patients.2 Urinary tract infections (UTIs) are among the most common infections in patients with SLE and have a 36% prevalence compared with an approximately 12% prevalence among the general population.3 4
Several risk factors can lead to UTI development, including defects in the host immune response either secondary to immunosuppressive drugs or patients’ medical conditions; uncontrolled diabetes; anatomical abnormalities of the genitourinary system; imbalances of specific cytokines, such as interleukin 1β and interleukin 1β antagonists, which are reported to play roles in controlling Escherichia coli colonisation in the genitourinary tract; and altered vaginal microbiota.5–7 Kirjavainen et al8 found that the vaginal microbiota in UTI-prone women exhibited diminished Lactobacillus compositions compared with those in the control group (p=0.003).
One of the first large-scale, non-culture-dependent studies of vaginal microbial communities assessed approximately 400 asymptomatic North American women and revealed that most vaginal microbial flora (73%) were dominated by one or more species of Lactobacillus.9 Proposed mechanisms by which Lactobacillus may prevent UTI include preventing E. coli from colonising the vagina via competitive mechanisms in which Lactobacillus spp adhere to uroepithelial cells, lowering the vaginal pH by producing lactic acid, and producing bacteriocins, surfactants and hydrogen peroxide.10 Lactic acid concentrations are high in a Lactobacillus-dominated vaginal microbiota, and these conditions produce a potently antimicrobial environment in vitro.11
Many factors affect the vaginal microbiota, including a natural or treatment-associated lack of oestrogen, especially during menopause, receiving antimicrobial treatment or contraceptive pills, and having bacterial vaginosis, especially when lacking Lactobacillus spp.10 Women lacking vaginal Lactobacillus are at an increased risk of various urogenital disease conditions, including bacterial vaginosis, HIV infection, Neisseria gonorrhoeae infections and vaginal colonisation by E. coli.12 13
Nielsen et al14 compared the E. coli faecal flora characteristics in patients with UTI with those of healthy controls who had never had a UTI and discovered that 87% of patients with UTI carried the infecting strain in their faecal flora. Additionally, faecal clones causing the UTI were more often dominant in the faecal flora. These findings support the UTI pathogenesis in which the gut microbiota colonising the vaginal introitus and periurethra may cause an ascending infection via the urethra to the bladder and sometimes the kidneys.10 Thus, many patients with SLE may be at risk of UTI after receiving immunosuppressive therapy, treatments affecting normal ovarian function, or antibiotics or if they have altered vaginal microbiota patterns either from impaired ovarian function or imbalanced glucose homeostasis. However, knowledge is lacking regarding patients with SLE and the associated risk factors for UTI considering that these individuals are immunocompromised. Moreover, the vaginal microbiota compositions in women with UTI-associated SLE are unreported. Here, we assessed the associated risk factors for UTI in this population.
Objectives
The primary objective of this work was to study the potential characteristics of the vaginal microbiota associated with UTI in women with SLE. The secondary objectives were to evaluate the associated risk factors for UTI in women with SLE and explore whether SLE-related treatment affects UTI development in this population.
Methods
Study design
A pilot cross-sectional study of patients with SLE was conducted at Ramathibodi Hospital, a university hospital in Bangkok, Thailand. Women with SLE, according to the Systemic Lupus International Collaborating Clinics 2012 classification criteria, aged >18 years visiting the rheumatology or infectious disease clinics from March 2019 to March 2020 were screened for enrolment regardless of their SLE disease activity, age and immunosuppressive therapy.
Patients were excluded if they had at least one of the following conditions at screening:
History of antibiotic use within 2 weeks before enrolment for any reason other than a UTI or suspected UTI.
Receipt of hormone replacement therapy, oral contraceptive pills or an intrauterine device.
History of vaginal douching within 4 weeks before enrolment.
Diagnoses of gynaecological infections within 1 month before enrolment.
Known or newly diagnosed non-infectious renal conditions resulting in an abnormal urinalysis at baseline (eg, IgA nephropathy, lupus nephritis).
Need for routine urinary catheterisation or indwelling urinary catheter.
Pregnancy.
No gynaecological examination was performed for any reason.
Diagnoses of any malignancies.
Known abnormal genitourinary tract structure.
Definitions
Urinary tract infection
Diagnosis of UTI was adapted from the Infectious Diseases Society of America and the European Society for Microbiology and Infectious Diseases using the following criteria15 16:
Relevant clinical presentations: participants with acute dysuria alone or with fever (>37.9°C or 1.5°C increase above baseline temperature) plus at least one symptom or new or worsening symptoms associated with urination, including urgency, frequency, suprapubic pain, gross haematuria, costovertebral tenderness and/or urinary incontinence.
-
Laboratory diagnostic criteria:
2.1. Presence of >10 white cell count per 109/L/high-power field on urinalysis.
2.2. Evidence of bacteriuria (≥105 colony-forming units (CFU)/mL in self-voided urine or ≥102 CFU/mL in single catheterised urine).
Culture-confirmed UTI was defined as those from individuals who met criteria 1, 2.1 and 2.2.
Probable UTI was defined as those from individuals who met only criteria 1 and 2.1.
High-level immunosuppression
High-level immunosuppression was defined as at least one of the following17 18:
Receipt of corticosteroid therapy of ≥20 mg/day of prednisolone or equivalent for ≥14 days.
Receipt of methotrexate (MTX) >0.4 mg/kg/week or azathioprine >2 mg/kg/day or 6-mercaptopurine (6-MP) >1.5 mg/kg/day.
Receipt of biological immune modulators, including tumour necrosis factor-alpha blockers and rituximab.
Receipt of mycophenolate mofetil >1.5 g/day or Myfortic >1080 mg/day.
Receipt of cyclophosphamide.
Receipt of a combination of three of more immunosuppressive agents, including prednisolone, MTX, azathioprine, 6-MP, mycophenolate mofetil and Myfortic, at any doses.
Low-level immunosuppression
Low-level immunosuppression was defined as at least one of the following17 18:
Receipt of systemic corticosteroid therapy of <20 mg/day of prednisolone or equivalent for ≤14 days or receiving alternate-day corticosteroid therapy.
Receipt of MTX ≤0.4 mg/kg/week, azathioprine ≤2 mg/kg/day or 6-MP ≤1.5 mg/kg/day.
Receipt of mycophenolate mofetil <1.5 g/day or Myfortic <1080 mg/day.
Receipt of a combination of two immunosuppressive drugs, including MTX, azathioprine, mycophenolate mofetil and Myfortic, or combined prednisolone with one immunosuppressive drug including MTX, azathioprine, 6-MP, mycophenolate mofetil and Myfortic.
Active SLE
Active SLE was defined as SLE in patients with a modified Systemic Lupus Erythematosus Disease Activity Index 2000 (SLEDAI-2K) score ≥4.19 20
Alpha diversity
Alpha diversity represents bacterial richness, evenness or both within a single sample.21
Simpson_e index
Simpson_e index is one of the most commonly used alpha diversity measures.22
Data and sample collection
Patients’ demographic data, menstrual status, cause of menopause, vaginal pH, coexisting medical conditions, modified SLEDAI-2K scores, use of trimethoprim-sulfamethoxazole (TMP-SMX) and/or acyclovir as prophylactic agents for opportunistic infections, complete blood count, glycosylated haemoglobin (HbA1C), and fasting plasma glucose, C3 and C4 levels were collected at enrolment. The immunosuppressive drug type and data on the 3-month cumulative dose of each drug were recorded.
On the day of enrolment, vaginal swabs were taken at the posterior fornix to assess the vaginal microbiota and urinalyses were performed on all participants. Five healthy menopausal and five healthy non-menopausal women agreed to participate in the study and were used as controls to compare with the enrolled study population on their menstrual status. All healthy controls were screened for the same inclusion/exclusion criteria as were the patients with SLE. The vaginal swabs were stored at −80°C until DNA extraction. Blank swabs and blank buffer controls were also included.
Sample processing and DNA extraction
Total DNA was extracted using the GenUP gDNA Extraction Kit (Biotechrabbit, Berlin, Germany) with additional mechanical lysis steps. First, 1 mL of swab suspension was transferred to a 2 mL lysis tube and centrifuged at 2000 revolutions per minute (rpm) for 5 min to pellet the bacterial cells. After removing the supernatant, the sample was added to 200 µL of lysis buffer from the extraction kit and lysed using a TissueLyser LT with a 5 mm stainless steel bead (Qiagen, Hilden, Germany) at 50 Hz for 5 min. The unlysed residue was pelleted again by centrifuging at 12 000 rpm for 2 min. The lysate was then processed following the standard protocol from the extraction kit.
16S rDNA amplification
The amplification method for next-generation sequencing was modified from a previous publication.23 Briefly, the V4 region of the bacterial 16S rDNA was amplified using four phasing primer sets (spacers 1–4) containing the target primer sequences 515F: 5′-GTGCCAGCMGCCGCGGTAA-3′ and 806R: 5′-GGACTACHVGGGTWTCTAAT-3′. Each 20 µL PCR consisted of 20 ng of DNA template, 0.2 µM of each primer, 0.2 mM of deoxynucleoside triphosphate, 1× Phusion Green HF Buffer and 0.4 U of Phusion DNA Polymerase (2 U/µL) (Thermo Scientific, Waltham, Massachusetts, USA). The thermal profile included the following:
Initial denaturation at 98°C for 30 s.
Twenty-five cycles of amplification (98°C for 10 s, 53°C for 25 s, 72°C for 25 s).
A final extension at 72°C for 10 min was done.
Library preparation and next-generation sequencing
The PCR product was reamplified using another set of primers composed of a dual multiplexing index set and Illumina adapters. The PCR reaction was prepared using the same protocol as the first PCR in a total volume of 40 µL. For the second PCR, DNA was amplified under the following conditions: 98°C for 30 s, 25 amplification cycles (98°C for 10 s, 60°C for 30 s, 72°C for 30 s) and a final extension at 72°C for 10 min. The PCR product was examined using 2% agarose gel electrophoresis. The expected band (~440 bp) was purified using the QIAquick Gel Extraction Kit (Qiagen, Germany). Purified DNA was quantified via quantitative PCR using KAPA Library Quantification Kits for Illumina platforms (Kapa Biosystems, USA). The DNA libraries were pooled at equal amounts. The pooled library was spiked with 20% PhiX and subsequently pair-end sequenced at 2×250 bp using a MiSeq V.2 reagent kit on the MiSeq sequencing platform (Illumina, San Diego, California, USA).
Data analysis
Raw data were demultiplexed using MiSeq Reporter Software (V.2.6.2.3). Paired-end FASTQ sequences were analysed using the QIIME2 pipeline (V.2018.8).24 Briefly, paired-end reads were merged and trimmed based on quality score (<Q30). Joined reads were deduplicated and clustered with 97% similarity using VSEARCH.25 Chimeric sequences were also filtered out by the UCHIME algorithm.26 The filtered reads were classified based on 99% operational taxonomic units clustered in the 16S Greengene database (V.2013.8)27 using the VSEARCH algorithm.
Statistical analyses
Categorical variables are presented as frequencies and percentages. Continuous variables are presented as mean and SD or median and IQR for data with and without a normal distribution, respectively. Characteristics between patients with and without UTI were compared via χ2 or Fisher’s exact tests for categorical variables and Mann-Whitney U test or Student’s t-test for continuous variables. ORs and their 95% CIs were calculated. Two-tailed tests were used to determine statistical significance, and p<0.05 was considered significant. All variables with p<0.05 in the univariate analysis were considered for inclusion in the multivariate analysis. All statistical analyses were performed using SPSS V.17.0 statistical software.
Results
Baseline characteristics
Among 1500 patients with SLE in the rheumatology clinic, 104 female patients were screened for enrolment and 52 patients agreed to participate in the study; 18 (34.6%) were diagnosed with UTI (17 with probable UTI and one with confirmed UTI). The mean age of all patients was 46.1±12.7 years, and 33 of 52 (63.5%) were in menopause. Among those in menopause, 29 (87.9%) were undergoing natural menopause (table 1). The proportion of menopausal patients was higher in the SLE without UTI group (24 of 34 patients, 70.6%) than in the SLE with UTI group (9 of 18 patients, 50%; p=0.226). Of the 52 patients, 23 (44.2%) had coexisting conditions: 9 (17.3%) had hypertension, 5 (9.6%) had hyperlipidaemia, 4 (7.7%) had well-controlled diabetes (mean HbA1C of 5.85%±0.87%), 3 (5.8%) had myoma uteri, 1 (1.9%) had undergone kidney transplantation and 1 (1.9%) had HIV. No patients in the SLE without UTI group had myoma uteri, whereas 3 of 18 (16.7%) in the SLE with UTI group had myoma uteri (p=0.037). All patients were in remission or low disease activity with a median modified SLEDAI-2K of 0 (range, 0–1). None of these developed active SLE necessitating treatment modification during the study period. The common immunosuppressive drug prescribed was prednisolone (44 of 52 patients, 84.6%; table 1). The drug type and 3-month cumulative immunosuppressive drug doses did not differ between the SLE with UTI and SLE without UTI groups (tables 1 and 2). Of 52 patients, 11 (21.2%) received TMP-SMX as a prophylactic agent, whereas 18 (34.6%) patients received acyclovir for prophylaxis. Nine of 18 (50%) patients receiving TMP-SMX prophylaxis developed UTI compared with 2 of 34 (5.9%) patients in the SLE without UTI group (p<0.001). Baseline laboratory values did not differ between the groups, as shown in online supplemental data, except for the UTI group which had a higher mean C3 level (1.1±0.2 g/L vs 0.9±0.3 g/L; p=0.027). The mean age among healthy menopausal individuals was 61±6.36 years old and 39.6±10.5 years old among healthy non-menopausal women. All healthy volunteers did not have any significant medical conditions and reported no regular medications at enrolment.
Table 1.
Demographic and baseline characteristics
| Variables | Total (N=52) | SLE with UTI (n=18) | SLE without UTI (n=34) | P value |
| Age (years), mean (SD) | 46.1 (12.7) | 43.5 (10.6) | 47.4 (13.7) | 0.296 |
| Menstrual status, n (%) | ||||
| Non-menopausal | 19 (36.5) | 9 (50) | 10 (29.4) | 0.226 |
| Menopausal | 33 (63.5) | 9 (50) | 24 (70.6) | |
| Cause of menopause, n (%) | ||||
| Natural menopause | 29 (87.9) | 7 (77.8) | 22 (91.7) | 0.555 |
| Treatment-associated | 4 (12.1) | 2 (22.2) | 2 (8.3) | |
| Duration of menopause prior to enrolment, years, median (IQR) | 7 (4.5–15) | 7 (4.5–11.0) | 8 (2.8–16.5) | 0.254 |
| Vaginal pH, median (IQR) | 5.5 (5–5.5) | 5.3 (5–5.5) | 5.5 (4.4–5.5) | 0.633 |
| Coexisting conditions, n (%) | ||||
| None | 33 (63.5) | 10 (55.6) | 23 (67.6) | |
| Well-controlled diabetes | 4 (7.7) | 2 (11.1) | 2 (5.9) | 0.602 |
| Hypertension | 9 (17.3) | 2 (11.1) | 7 (20.6) | 0.47 |
| Hyperlipidaemia | 5 (9.6) | 2 (11.1) | 3 (8.8) | 1 |
| Myoma uteri | 3 (5.8) | 3 (16.7) | 0 (0) | 0.037 |
| Kidney transplantation | 1 (1.9) | 1 (5.6) | 0 (0) | 0.346 |
| HIV | 1 (1.9) | 0 (0) | 1 (2.9) | 1 |
| Immunosuppressive drugs, n (%) | ||||
| Prednisolone | 44 (84.6) | 16 (88.9) | 28 (82.4) | 0.698 |
| HCQ | 39 (75) | 14 (77.8) | 25 (73.5) | 1 |
| Azathioprine | 28 (53.8) | 12 (66.7) | 16 (47.1) | 0.245 |
| Cyclophosphamide | 2 (3.8) | 0 (0) | 2 (5.9) | 0.538 |
| MTX | 6 (11.5) | 2 (11.1) | 4 (11.8) | 1 |
| MMF | 9 (17.3) | 2 (11.1) | 7 (20.6) | 0.47 |
| Ciclosporin A | 2 (3.8) | 1 (5.6) | 1 (2.9) | 1 |
| Tacrolimus | 3 (5.8) | 2 (11.1) | 1 (2.9) | 0.543 |
| Sulfasalazine | 1 (1.9) | 0 (0) | 1 (2.9) | 1 |
| Leflunomide | 5 (9.6) | 1 (5.6) | 4 (11.8) | 0.648 |
| Everolimus | 1 (1.9) | 1 (5.6) | 0 (0) | 0.346 |
| Level of immunosuppression, n (%) | ||||
| High level | 3 (5.8) | 0 (0) | 3 (8.8) | 0.308 |
| Low level | 49 (94.2) | 18 (100) | 31 (91.2) | |
| TMP-SMX prophylaxis, n (%) | 11 (21.2) | 9 (50) | 2 (5.9) | <0.001 |
| Acyclovir prophylaxis, n (%) | 18 (34.6) | 9 (50) | 9 (26.5) | 0.127 |
| Vaginal microbiota, n (%) | ||||
| Enterococcus spp | 19 (36.5) | 10 (55.6) | 9 (26.5) | 0.038 |
| Peptostreptococcus spp | 22 (42.3) | 11 (61.1) | 11 (32.4) | 0.046 |
| Veillonella dispar | 20 (38.5) | 11 (61.1) | 9 (26.5) | 0.015 |
HCQ, hydroxychloroquine; MMF, mycophenolate mofetil; MTX, methotrexate; TMP-SMX, trimethoprim-sulfamethoxazole; UTI, urinary tract infection.
Table 2.
Three-month cumulative dose of immunosuppressive drugs
| Immunosuppressive drugs | SLE with UTI (n=18) | SLE without UTI (n=34) | P value |
| Prednisolone, mg/day, median (IQR) | 6.3 (5.0–10.0) | 7.5 (3.13–10.0) | 0.611 |
| HCQ, mg/day, mean±SD | 173.5±53.1 | 173.5±53.8 | 0.960 |
| Azathioprine, mg/day, mean±SD | 67.9±31.9 | 58.7±24.0 | 0.393 |
| MTX, mg/day, median (IQR) | 13.8 (5.6–24.0) | 8.8 (7.5–10.0) | 0.617 |
| MMF, mg/day, mean±SD | 1000±0 | 1351.4±623.7 | 0.667 |
HCQ, hydroxychloroquine; MMF, mycophenolate mofetil; MTX, methotrexate; UTI, urinary tract infection.
lupus-2021-000551supp001.pdf (87.7KB, pdf)
Vaginal microbiota
The median vaginal pH in the SLE with and without UTI groups did not statistically differ (5.3 (5–5.5) vs 5.5 (4.4–5.5); p=0.633). Of 52 patients, 15 (28.8 %) were discovered to have at least 50% of the sequences belonging to the Lactobacillus spp, and this proportion of patients was similar to that of the healthy volunteers (3 of 10, 30%; figures 1 and 2). Thus, Lactobacillus spp were considered the predominant organisms in all participants. The proportions of Enterococcus spp, Peptostreptococcus spp and Veillonella dispar were higher in the SLE with UTI group than in the SLE without UTI group (p=0.038, p=0.046 and p=0.015, respectively; table 1). Alpha diversity among all patients was determined via the Simpson_e index, and patients in the SLE with UTI group and SLE patients taking TMP-SMX prophylaxis had relatively low diversities compared with those of the controls (p=0.039 and p=0.041, respectively; figures 3 and 4). Patients’ menstrual status did not affect the alpha diversity.
Figure 1.
Relative abundance of taxa in vaginal samples from healthy controls, patients with SLE without UTI and patients with SLE with UTI. UTI, urinary tract infection.
Figure 2.
Relative abundance taxa bar plot of vaginal samples from healthy controls, patients with SLE taking TMP-SMX prophylaxis and patients with SLE not taking TMP-SMX prophylaxis. TMP-SMX, trimethoprim-sulfamethoxazole.
Figure 3.
Distribution of alpha diversity within groups as measured by the Simpson_e index among healthy controls and patients with and without urinary tract infection (UTI). *lower alpha diversity among SLE with UTI and patients taking TMP-SMX prophylaxis compared with healthy controls.
Figure 4.
Distribution of alpha diversity within groups as measured by the Simpson_e index among healthy controls, patients with SLE taking TMP-SMX and patients with SLE not taking TMP-SMX prophylaxis. *lower alpha diversity among SLE with UTI and patients taking TMP-SMX prophylaxis compared with healthy controls. TMP-SMX, trimethoprim-sulfamethoxazole.
Potential associated risk factors for UTI in this population
TMP-SMX prophylaxis (OR: 16, 95% CI 2.92 to 8.70; p=0.001), elevated plasma C3 levels (OR: 12.75, 95% CI 1.21 to 133.83; p=0.034), and presence of Enterococcus spp (OR: 3.472, 95% CI 1.04 to 11.55; p=0.042), V. dispar (OR: 4.37, 95% CI 1.29 to 14.73; p=0.018) and Peptostreptococcus spp (OR: 3.29, 95% CI 1.00 to 10.79; p=0.05) in the vaginal microbiota were associated with an increased risk of UTI in the univariate analysis. In the multivariate logistic regression analysis, only three factors reached statistical significance: TMP-SMX prophylaxis (adjusted OR (AOR): 30.96, 95% CI 3.63 to 264.11; p=0.002), elevated plasma C3 levels (AOR: 35.33, 95% CI 1.33 to 936.67; p=0.033) and presence of V. dispar (AOR: 6.68, 95% CI 1.27 to 35.07; p=0.025; table 3).
Table 3.
Potential associated risk factors of urinary tract infection in female patients with SLE
| Variables | Univariate analysis OR (95% CI) |
P value | Multivariate analysis OR (95% CI) |
P value |
| TMP-SMX prophylaxis | 16 (2.92 to 87.70) | 0.001 | 30.96 (3.63 to 264.11) | 0.002 |
| Serum C3 level | 12.75 (1.21 to 133.83) | 0.034 | 35.33 (1.33 to 936.67) | 0.033 |
| Vaginal microbiota | ||||
| Enterococcus spp | 3.472 (1.04 to 11.55) | 0.042 | 5.53 (0.93 to 32.96) | 0.060 |
| Veillonella dispar | 4.37 (1.29 to 14.73) | 0.018 | 6.68 (1.27 to 35.07) | 0.025 |
| Peptostreptococcus spp | 3.29 (1.00 to 10.79) | 0.05 | – | – |
TMP-SMX, trimethoprim-sulfamethoxazole.
Discussion
Several factors affect UTI development in women.28 The unidirectional urine flow resulting from ureteric and bladder peristalsis helps reduce bacterial adhesion to epithelial cells.29 Another local mechanism is glycosaminoglycan secretion by bladder transitional cells, which acts as an antiadherence factor and traps bacteria.30 If the innate immune system fails to respond to the invading bacteria, the complement system and other complex mechanisms will occur next. C3 is one of the essential factors that promote opsonisation to speed up bacterial elimination. Deficient C3 may result in ineffective bacterial clearance, thus resulting in severe infection.30 31
Syukri et al31 noticed that serum C3 levels were significantly lower in patients with recurrent UTIs than in healthy younger women (mean 42.08 µg/mL ±1.20 vs 42.75 µg/mL ±0.71, p=0.008). However, Springall et al32 used a mouse model to demonstrate conflicting results in which C3 deficiency prevented an ascending renal infection. These authors postulated that the bacteria used C3 to enter renal epithelial cells, thus resulting in low C3 levels. In our study, the mean serum C3 levels were higher in the SLE with UTI group than in the SLE without UTI group, possibly because C3 acts as an acute-phase protein and may be elevated during infectious episodes such as UTIs.33 However, determining the serum C3 level at one time point may not explain the entire clinical course but may be used to monitor dynamic changes in the complement. The vaginal microbiota is no less critical than the intact host immune responses. These microbes help maintain a healthy environment in the birth canal by hindering excessive growth of colonising uropathogens, thus reducing the risk of UTI.10 34–37 The vaginal microbiota responds to uropathogens by competitive exclusion. Lactobacillus adheres to uroepithelial cells and produces lactic acid and other substances that alter the vaginal canal environment for excessive growth of specific pathogens.38–44
Prolonged antibiotic use may affect the vaginal microbiota, mostly reducing the microbial diversity. This effect triggers abnormal multiplication of the uropathogens, eventually altering the vaginal colonisation pattern. One animal study supported this theory: the researchers flushed cefadroxil into monkeys’ vaginas and found predominant E. coli colonisation in 9 of 10 monkeys. Conversely, another group found no E. coli colonisation in the vaginal canals despite flushing them with P-fimbriated E. coli.45 46 Consistently, in the current study, Enterococcus spp, Peptostreptococcus spp and V. dispar proportions were higher in the SLE with UTI group than in the SLE without UTI group (p=0.038, p=0.046 and p=0.015, respectively). Additionally, the alpha diversity was low in the SLE with UTI group and in those who received TMP-SMX prophylaxis. Thus, prolonged use of a TMP-SMX prophylaxis may affect the vaginal microbiota, but consequent UTI development requires additional clinical information to conclude.
Smith et al46 examined whether prior antimicrobial use influenced the subsequent relative risk of UTI in premenopausal women. These authors concluded that previous antibiotic use within 28 days as well as TMP-SMX were associated with an increased risk of UTI (relative risk: 5.83, 95% CI 3.17 to 10.70 and relative risk: 4.56, 95% CI 2.10 to 9.87, respectively). Another retrospective study conducted at the University Student Health Center of the University of Florida between 2006 and 2014 revealed that TMP-SMX use as an initial agent in cystitis increased the risk of subsequent UTI events (AOR: 2.14, 95% CI 1.23 to 4.09).47 This finding may be explained in that increasingly resistant bacteria caused the UTI, which could only be partially treated with TMP-SMX. Unknown effects on the vaginal microbiota may also cause recurrent infections. In our study, TMP-SMX prophylaxis was a potent associated risk factor of UTI (AOR: 30.96, 95% CI 3.63 to 264.11; p=0.002). Thus, prolonged use of TMP-SMX prophylaxis may cause unrecognised harm in patients with SLE.
TMP-SMX is considered an effective treatment for uncomplicated UTIs; therefore, some clinicians acknowledge that patients may benefit from reduced risk of UTI, pneumocystis pneumonia and toxoplasmosis. However, one extensive clinical survey conducted at 28 hospitals across Thailand from 2000 to 2005, focusing on the susceptibility patterns of E. coli to TMP-SMX among non-critically ill individuals, demonstrated that 62.6% of the isolates were resistant to TMP-SMX.48 Therefore, routinely prescribing TMP-SMX to prevent UTI should be discouraged in Thailand.
TMP-SMX is indicated for opportunistic infection prophylaxis when CD4 counts are low or the patient is receiving high-dose corticosteroid therapy.49 However, to date, no consensus has been reached regarding when TMP-SMX should be provided to patients with SLE. Therefore, TMP-SMX for opportunistic infection prophylaxis as part of SLE treatment is solely individualised. Interestingly, most patients in our study were treated with only low-level immunosuppressive drugs, but a large proportion of them received TMP-SMX prophylaxis. Our data may reflect unnecessary treatment and provide evidence to support discontinuing TMP-SMX prophylaxis in patients with SLE who are receiving low-level immunosuppressive agents.
To further analyse whether TMP-SMX affects Lactobacillus proportions, Melkumyan et al50 conducted a clinical study assessing the sensitivity patterns of 123 vaginal Lactobacillus strains to a variety of antibiotic types and noticed that all strains were resistant to TMP-SMX. Hence, TMP-SMX should not directly affect the proportion of the main vaginal micro-organisms but rather affect the overall microbes in the vagina, causing reduced microbial diversity.
Our study had several limitations. First, the study population was small, and other essential risk factors of UTI may have been missed. Second, the nature of the cross-sectional study did not allow comparing the vaginal microbiota patterns among individuals prior to and after TMP-SMX prophylaxis and prior to and after UTI events. Third, the results may not apply to active patients with SLE requiring a higher level of immunosuppressive therapy. A final limitation was that we lacked patients’ histories of sexual activity. However, this study highlighted some significant findings as follows. First, vaginal microbiota diversity differs between patients with SLE with and without UTI. Second, unnecessary use of TMP-SMX prophylaxis may affect the alpha diversity of the vaginal microbiota.
In conclusion, UTI in patients with SLE remains a critical infectious complication that can increase patients’ morbidity and mortality. In addition to comprehensively assessing the anatomical abnormalities of the genitourinary system, prophylactic agents must be carefully prescribed to help maintain a healthy and diverse vaginal microbiota and help prevent future UTI events. Further studies on a larger scale and with higher modified SLEDAI-2K scores are encouraged.
Acknowledgments
We thank our colleagues at the Division of Allergy, Immunology and Rheumatology, Department of Medicine, Faculty of Medicine Ramathibodi Hospital, Mahidol University, and the staff at Ramathibodi Hospital for enrolling and caring for the participants and assisting in data collection.
Footnotes
Contributors: PR and AJ conceived the study question and design and drafted the manuscript. AJ extracted the data and performed the statistical analysis. PR, PP, PN, JM, VS, PC and SP reviewed the analysis for accuracy. VS, PC and SP processed the samples and performed the DNA extraction, DNA sequencing and analysis. PR takes responsibility for the integrity of the data and the accuracy of the analysis. All authors had full access to the data (including statistical reports and tables) in the study and approved the final manuscript. PR was the principal investigator in this study and is also responsible for the overall content as the gurantor.
Funding: This study was supported by the Faculty of Medicine Ramathibodi Hospital (RF_63040 and CF_61004) and Mahidol University (2563).
Disclaimer: The funder had no role in the study design, data collection, analysis, decision to publish or manuscript preparation.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available in a public, open access repository.
Ethics statements
Patient consent for publication
Consent obtained directly from patient(s).
Ethics approval
This study was conducted in accordance with the Declaration of Helsinki. Ethical approval was granted by the Research Ethics Committee of the Faculty of Medicine Ramathibodi Hospital, Mahidol University (approval no ID 01-62-06). The committee approved the use of patient samples and data for publishing this study. All patients provided written informed consent.
References
- 1.La Paglia GMC, Leone MC, Lepri G, et al. One year in review 2017: systemic lupus erythematosus. Clin Exp Rheumatol 2017;35:551–61. [PubMed] [Google Scholar]
- 2.Esposito S, Bosis S, Semino M, et al. Infections and systemic lupus erythematosus. Eur J Clin Microbiol Infect Dis 2014;33:1467–75. 10.1007/s10096-014-2098-7 [DOI] [PubMed] [Google Scholar]
- 3.Hidalgo-Tenorio C, Jiménez-Alonso J, de Dios Luna J, et al. Urinary tract infections and lupus erythematosus. Ann Rheum Dis 2004;63:431–7. 10.1136/ard.2003.006346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Foxman B. The epidemiology of urinary tract infection. Nat Rev Urol 2010;7:653–60. 10.1038/nrurol.2010.190 [DOI] [PubMed] [Google Scholar]
- 5.Minardi D, d'Anzeo G, Cantoro D, et al. Urinary tract infections in women: etiology and treatment options. Int J Gen Med 2011;4:333. 10.2147/IJGM.S11767 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.John AS, Mboto CI, Agbo B. A review on the prevalence and predisposing factors responsible for urinary tract infection among adults. Euro J Exp Bio 2016;6:7–11. [Google Scholar]
- 7.Lindblad A, Persson K, Demirel I. Il-1Ra is part of the inflammasome-regulated immune response in bladder epithelial cells and influences colonization of uropathogenic E. coli. Cytokine 2019;123:154772–9. 10.1016/j.cyto.2019.154772 [DOI] [PubMed] [Google Scholar]
- 8.Kirjavainen PV, Pautler S, Baroja ML, et al. Abnormal immunological profile and vaginal microbiota in women prone to urinary tract infections. Clin Vaccine Immunol 2009;16:29–36. 10.1128/CVI.00323-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ravel J, Gajer P, Abdo Z, et al. Vaginal microbiome of reproductive-age women. Proc Natl Acad Sci U S A 2011;108:4680–7. 10.1073/pnas.1002611107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stapleton AE. The vaginal microbiota and urinary tract infection. Microbiol Spectr 2016;4. 10.1128/microbiolspec.UTI-0025-2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.O'Hanlon DE, Moench TR, Cone RA. Vaginal pH and microbicidal lactic acid when lactobacilli dominate the microbiota. PLoS One 2013;8:e80074. 10.1371/journal.pone.0080074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hawes SE, Hillier SL, Benedetti J, et al. Hydrogen peroxide-producing lactobacilli and acquisition of vaginal infections. J Infect Dis 1996;174:1058–63. 10.1093/infdis/174.5.1058 [DOI] [PubMed] [Google Scholar]
- 13.Martin HL, Richardson BA, Nyange PM, et al. Vaginal lactobacilli, microbial flora, and risk of human immunodeficiency virus type 1 and sexually transmitted disease acquisition. J Infect Dis 1999;180:1863–8. 10.1086/315127 [DOI] [PubMed] [Google Scholar]
- 14.Nielsen KL, Dynesen P, Larsen P, et al. Faecal Escherichia coli from patients with E. coli urinary tract infection and healthy controls who have never had a urinary tract infection. J Med Microbiol 2014;63:582–9. 10.1099/jmm.0.068783-0 [DOI] [PubMed] [Google Scholar]
- 15.Nicolle LE, Bradley S, Colgan R, et al. Infectious diseases Society of America guidelines for the diagnosis and treatment of asymptomatic bacteriuria in adults. Clin Infect Dis 2005;40:643–54. 10.1086/427507 [DOI] [PubMed] [Google Scholar]
- 16.Gupta K, Hooton TM, Naber KG, et al. International clinical practice guidelines for the treatment of acute uncomplicated cystitis and pyelonephritis in women: a 2010 update by the infectious diseases Society of America and the European Society for microbiology and infectious diseases. Clin Infect Dis 2011;52:e103–20. 10.1093/cid/ciq257 [DOI] [PubMed] [Google Scholar]
- 17.America IDSo. . IDSA clinical practice guideline for vaccination of the immunocompromised host, 2013. [Google Scholar]
- 18.Yong PF, D'Cruz DP, D’Cruz DP. Mycophenolate mofetil in the treatment of lupus nephritis. Biologics 2008;2:297. 10.2147/btt.s2266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gladman DD, Ibañez D, Urowitz MB. Systemic lupus erythematosus disease activity index 2000. J Rheumatol 2002;29:288–91. [PubMed] [Google Scholar]
- 20.Mikdashi J, Nived O. Measuring disease activity in adults with systemic lupus erythematosus: the challenges of administrative burden and responsiveness to patient concerns in clinical research. Arthritis Res Ther 2015;17:183. 10.1186/s13075-015-0702-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Walters KE, Martiny JBH, Kendra E. Alpha-, beta-, and gamma-diversity of bacteria varies across habitats. PLoS One 2020;15:e0233872–17. 10.1371/journal.pone.0233872 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wagner BD, Grunwald GK, Zerbe GO, et al. On the use of diversity measures in longitudinal sequencing studies of microbial communities. Front Microbiol 2018;9:1–11. 10.3389/fmicb.2018.01037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wu L, Wen C, Qin Y, et al. Phasing amplicon sequencing on Illumina Miseq for robust environmental microbial community analysis. BMC Microbiol 2015;15:125. 10.1186/s12866-015-0450-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bolyen E, Rideout JR, Dillon MR, et al. Reproducible, interactive, scalable and extensible microbiome data science using QIIME 2. Nat Biotechnol 2019;37:852–7. 10.1038/s41587-019-0209-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rognes T, Flouri T, Nichols B, et al. VSEARCH: a versatile open source tool for metagenomics. PeerJ 2016;4:e2584. 10.7717/peerj.2584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Edgar RC, Haas BJ, Clemente JC, et al. UCHIME improves sensitivity and speed of chimera detection. Bioinformatics 2011;27:2194–200. 10.1093/bioinformatics/btr381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.DeSantis TZ, Hugenholtz P, Larsen N, et al. Greengenes, a chimera-checked 16S rRNA gene database and workbench compatible with ARB. Appl Environ Microbiol 2006;72:5069–72. 10.1128/AEM.03006-05 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Scholes D, Hooton TM, Roberts PL, et al. Risk factors for recurrent urinary tract infection in young women. J Infect Dis 2000;182:1177–82. 10.1086/315827 [DOI] [PubMed] [Google Scholar]
- 29.Cox CE, Hinman F. Experiments with induced bacteriuria, vesical emptying and bacterial growth on the mechanism of bladder defense to infection. J Urol 1961;86:739–48. 10.1016/S0022-5347(17)65257-1 [DOI] [PubMed] [Google Scholar]
- 30.Springall T, Sheerin NS, Sacks SH. Breaching host defenses in the urinary tract. Hong Kong J Nephrol 2002;4:13–21. 10.1016/S1561-5413(09)60070-3 [DOI] [Google Scholar]
- 31.Syukri M, Imran I, Harapan H, et al. Comparison of serum C3 complement levels between young women with recurrent urinary tract infection and healthy women. Alexandria J Med 2015;51:35–9. 10.1016/j.ajme.2014.04.006 [DOI] [Google Scholar]
- 32.Springall T, Sheerin NS, Abe K, et al. Epithelial secretion of C3 promotes colonization of the upper urinary tract by Escherichia coli. Nat Med 2001;7:801–6. 10.1038/89923 [DOI] [PubMed] [Google Scholar]
- 33.Alava MA, González-Ramón N, Heegaard P, et al. Pig-MAP, porcine acute phase proteins and standardisation of assays in Europe. Comp Haematol Int 1997;7:208–13. 10.1007/BF02658691 [DOI] [Google Scholar]
- 34.Czaja CA, Stamm WE, Stapleton AE, et al. Prospective cohort study of microbial and inflammatory events immediately preceding Escherichia coli recurrent urinary tract infection in women. J Infect Dis 2009;200:528–36. 10.1086/600385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Russo TA, Stapleton A, Wenderoth S, et al. Chromosomal restriction fragment length polymorphism analysis of Escherichia coli strains causing recurrent urinary tract infections in young women. J Infect Dis 1995;172:440–5. 10.1093/infdis/172.2.440 [DOI] [PubMed] [Google Scholar]
- 36.Beerepoot M, Geerlings S. Non-Antibiotic prophylaxis for urinary tract infections. Pathogens 2016;5:36. 10.3390/pathogens5020036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mulvey MA, Klumpp DJ, Stapleton AE. Urinary tract infections: molecular pathogenesis and clinical management. John Wiley & Sons, 2017. [Google Scholar]
- 38.Boris S, Barbés C. Role played by lactobacilli in controlling the population of vaginal pathogens. Microbes Infect 2000;2:543–6. 10.1016/S1286-4579(00)00313-0 [DOI] [PubMed] [Google Scholar]
- 39.Herthelius M, Gorbach SL, Möllby R, et al. Elimination of vaginal colonization with Escherichia coli by administration of Indigenous flora. Infect Immun 1989;57:2447–51. 10.1128/iai.57.8.2447-2451.1989 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.McGroarty JA, Reid G. Detection of a Lactobacillus substance that inhibits Escherichia coli. Can J Microbiol 1988;34:974–8. 10.1139/m88-171 [DOI] [PubMed] [Google Scholar]
- 41.McGroarty JA, Tomeczek L, Pond DG, et al. Hydrogen peroxide production by Lactobacillus species: correlation with susceptibility to the spermicidal compound nonoxynol-9. J Infect Dis 1992;165:1142–4. 10.1093/infdis/165.6.1142 [DOI] [PubMed] [Google Scholar]
- 42.Osset J, Bartolomé RM, García E, et al. Assessment of the capacity of Lactobacillus to inhibit the growth of uropathogens and block their adhesion to vaginal epithelial cells. J Infect Dis 2001;183:485–91. 10.1086/318070 [DOI] [PubMed] [Google Scholar]
- 43.Reid G, Cook RL, Bruce AW. Examination of strains of lactobacilli for properties that may influence bacterial interference in the urinary tract. J Urol 1987;138:330–5. 10.1016/S0022-5347(17)43137-5 [DOI] [PubMed] [Google Scholar]
- 44.Reid G, Heinemann C, Velraeds M. Biosurfactants produced by Lactobacillus. In: Methods in enzymology. 310. Elsevier, 1999: 426–33. [DOI] [PubMed] [Google Scholar]
- 45.Winberg J, Gezelius L, Guldevall L, et al. Cephadroxil promotes vaginal colonization with Escherichia coli. Infection 1993;21:201–5. 10.1007/BF01728887 [DOI] [PubMed] [Google Scholar]
- 46.Smith HS, Hughes JP, Hooton TM, et al. Antecedent antimicrobial use increases the risk of uncomplicated cystitis in young women. Clin Infect Dis 1997;25:63–8. 10.1086/514502 [DOI] [PubMed] [Google Scholar]
- 47.Rich SN, Klann EM, Almond CR, et al. Associations between antibiotic prescriptions and recurrent urinary tract infections in female college students. Epidemiol Infect 2019;147:e119. 10.1017/S0950268818003369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Polwichai P, Dejsirilert S, Panpetch S. Antimicrobial resistance of Escherichia coli isolated from urine in Thailand from 2000 to 2005. J Med Assoc Thai 2011;92:S59–67. [PubMed] [Google Scholar]
- 49.Maertens J, Cesaro S, Maschmeyer G, et al. ECIL guidelines for preventing Pneumocystis jirovecii pneumonia in patients with haematological malignancies and stem cell transplant recipients. J Antimicrob Chemother 2016;71:2397–404. 10.1093/jac/dkw157 [DOI] [PubMed] [Google Scholar]
- 50.Melkumyan AR, Priputnevich TV, Ankirskaya AS, et al. Effects of antibiotic treatment on the Lactobacillus composition of vaginal microbiota. Bull Exp Biol Med 2015;158:766–8. 10.1007/s10517-015-2857-1 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
lupus-2021-000551supp001.pdf (87.7KB, pdf)
Data Availability Statement
Data are available in a public, open access repository.