Abstract
Background
The impact of public health policy to reduce the spread of COVID-19 on access to surgical care is poorly defined. We aim to quantify the surgical backlog during the COVID-19 pandemic in the Brazilian public health system and determine the relationship between state-level policy response and the degree of state-level delays in public surgical care.
Methods
Monthly estimates of surgical procedures performed per state from January 2016 to December 2020 were obtained from Brazil's Unified Health System Informatics Department. Forecasting models using historical surgical volume data before March 2020 (first reported COVID-19 case) were constructed to predict expected monthly operations from March through December 2020. Total, emergency, and elective surgical monthly backlogs were calculated by comparing reported volume to forecasted volume. Linear mixed effects models were used to model the relationship between public surgical delivery and two measures of health policy response: the COVID-19 Stringency Index (SI) and the Containment & Health Index (CHI) by state.
Findings
Between March and December 2020, the total surgical backlog included 1,119,433 (95% Confidence Interval 762,663–1,523,995) total operations, 161,321 (95%CI 37,468–395,478) emergent operations, and 928,758 (95%CI 675,202–1,208,769) elective operations. Increased SI and CHI scores were associated with reductions in emergent surgical delays but increases in elective surgical backlogs. The maximum government stringency (score = 100) reduced emergency delays to nearly zero but tripled the elective surgical backlog.
Interpretation
Strong health policy efforts to contain COVID-19 ensure minimal reductions in delivery of emergent surgery, but dramatically increase elective backlogs. Additional coordinated government efforts will be necessary to specifically address the increased elective backlogs that accompany stringent responses.
Keywords: COVID-19, Global health, Health policy, Surgery, Elective surgery, Emergency surgery, Pandemics
Research in context.
Evidence before this study
The COVID-19 pandemic has significantly disrupted surgical care systems worldwide, causing a growing backlog of surgical procedures at national level. In many countries, including Brazil, access to emergent surgery was reduced due to shifts in health system capacity and elective surgeries were postponed in order to increase medical resources available for COVID-19 patients. Previous work has demonstrated increased surgical mortality among patients with COVID-19 and guided international consensus to delay elective surgery, however, the impact of strong government policy on access to emergent care has not been studied. Models of global surgical backlog have been published; nonetheless more robust subnational estimates on surgical backlogs that identify the reductions in both emergent and elective surgery may be useful for guiding government policy to expand surgical care during a surge.
Added value of this study
Our research utilizes subnational data combined with a modeling approach to quantify the backlog of surgical operations in public Brazilian hospitals at the state level. We found broad variation in surgical backlogs at the subnational level. Furthermore, increased Stringency Index and Containment and Health Index scores were associated with reductions in emergent surgical delays, while maximum government stringency ensured minimal delays in emergent surgery but results in a tripling of elective surgical backlog compared with minimal stringency.
Implications of all available evidence
As a result of the pandemic, over a million surgical procedures have been delayed or canceled in Brazil's public health system with the elective surgical backlog reaching over 900,000 cases. Stricter government policy responses are associated with reductions in delayed emergent surgery, but large increases in elective surgical backlogs. Our findings suggest that stringent efforts to reduce COVID-19 spread will be associated with reduced delays and cancellations for emergent surgery but will require coordinated government efforts to expand surgical care to overcome elective backlogs. Future work is needed to understand if stricter implementation of policy measures results in a more rapid return to expected surgical volume.
Alt-text: Unlabelled box
1. Introduction
The Coronavirus Disease (COVID-19) pandemic has significantly disrupted surgical care systems worldwide, with an estimated 28 million surgical procedures canceled within the first 12 weeks of the pandemic,[1] and caused a dramatic reduction in surgical services, but further investigation is required to study the effects of these delays on population health.[2,3] As healthcare systems prepare to tackle the backlog of surgical cases generated by the pandemic, more data is needed to understand the extent of the backlog, guide the formulation of robust recovery plans, and minimize the potential public health impacts of canceled and postponed surgeries.[4] Previous studies indicated that upper-middle-income countries are expected to sustain the highest cancelation numbers.[1]
Government policy responses to the pandemic have been varied across the globe.[5] Robust governmental policy interventions have been shown to significantly reduce the incidence of COVID-19 cases and mortality.[6] The Oxford COVID-19 Government Response Tracker was designed to track government response through two core indicators: Containment and Health Index, a combination of lockdown restrictions with measures such as testing policies, vaccines, health care investments, and contact tracing; and Stringency Index, which expresses the strictness of lockdown policies.[7]
In Brazil, the high number of cases has contributed to the emergence of novel strains that further complicated public health measures to control the outbreak, while vaccination rates continued at a slow pace.[8] The Brazilian unified health system (Sistema Único de Saúde - SUS) is decentralized, following a tri-level administration at municipality, statal, and national. In April 25, 2020, despite an attempt of the federal government to centralize power during the pandemic, the Brazilian Supreme Court ruled that healthcare delivery would remain decentralized which has resulted in wide variation in local policy towards the pandemic.[9] The wide regional variation in responses to the pandemic offers an opportunity to better understand how local strategies adopted to contain COVID-19 incidence impacts the delivery of surgical care.
Although several national and international studies have highlighted the large number of canceled elective surgical operations and growing surgical backlog, few studies focused on examining the association of the surgical backlog with COVID-19 national policies or impact of local resources for monitoring, assessment, and self-evaluation, and other context-related confounders.[1,[10], [11], [12]] Granular understanding of the extent of unperformed surgical cases at subnational level is necessary to guide policymakers as they plan for the surgical system expansion in order to respond to backlogs. Furthermore, an improved understanding of the impact of strategies to control COVID-19 on surgical backlogs may assist countries to direct future responses to surgical system changes.
This study aims to quantify the surgical backlog as a result of the COVID-19 pandemic in the Brazilian public health system and determine the relationship between both the COVID-19 Stringency Index and the Containment and Health Index and the degree of state-level delays in emergency and elective public surgical care.
2. Methods
2.1. Data sources
Monthly data on the number of operations performed in Brazilian public hospitals by state between January 2016 and December 2020 was obtained from Brazil's SUS Health System Informatics Department, known as DATASUS. This database-reporting system requires hospitals funded under Brazil's Federal health plan, which represents 60–70% of all hospital admissions, to submit monthly reports on various diagnostic and procedural statistics, including information on procedures performed. Regarding data validity, the quality of the SUS database has been found to have good and accurate representative reporting of public health settings, and has been used in numerous previous studies [13], [14], [15]. Any procedure coded as procedure group 04: Surgical procedures, was included in the study. Further classification codes in DATASUS for elective or emergent procedures were used to further subset surgical operations.
Data on the daily number of confirmed COVID-19 cases, as well as daily Stringency Index and Containment and Health Index were obtained from the Oxford COVID-19 Government Response Tracker (OxCGRT). The OxCGRT is a large, multi-country collaboration that includes 19 policy indicators covering closure and containment, health and economic policies. The Stringency Index records the strictness of ‘lockdown style’ policies that primarily restrict people's behavior, while the Containment and Health Index combines ‘lockdown’ restrictions and closures with measures such as testing policy and contact tracing, short term investment in healthcare, as well investments in vaccine[7]. Daily data for each state were obtained from the Oxford COVID-19 Government Response Tracker (OxCGRT) and monthly averages for each Index were calculated. See Appendix 1 for a complete list of data used in this study.
2.2. Estimate of surgical backlog
To estimate the surgical backlog for each state, we first estimated the expected number of monthly operations that would be performed for each state in Brazil's public hospitals between March 2020 and December 2020. We used March 1, 2020, as the start date for impact from the COVID-19 pandemic based on the first reported cases in late February [16]. We used historical data on surgical volume from January 2016 through March 2020 to construct Autoregressive Integrated Moving Average (ARIMA) models for each state. ARIMA models use time series data to predict future trends based on the historical trend. For each model, we determined the optimal specification and parameter estimation using an automated selection process that optimizes for the lowest Akaike information criterion (AIC) score [17]. We then utilized each model to forecast the number of monthly operations that would be expected to be performed for each month between March and December 2020 and finally, we compared these numbers to the reported number of operations in DATASUS. Point estimates and 95% confidence intervals were reported. We repeated this procedure for both emergent operations and elective operations. We defined emergent surgical delays as reductions in the number of emergent operations as these represent emergent operations that were not performed due to fewer patients able to seek surgical care or lack of operative capacity for those who do. We defined the elective surgical backlog as the total decrease in elective surgical operations as these operations represent those that may be performed in the future. Relationship of Surgical Volume and COVID-19 Health Policy.
We used Poisson generalized linear mixed models with random state and month level effects to model the longitudinal relationship between delays in emergent surgical care and the size of the elective surgical backlog and each of the policy indices (Stringency Index and the Containment and Health Index). The primary outcome was the total surgical backlog (number of cases). Two models were constructed for each type of surgical backlog (total, emergent and elective). For each of these outcomes, one of the two indexes was included (Stringency and Containment and Health Index).Each index is a scaled unitless score from 0 to 100. Each model included the log transformed index with an offset term for the total number of operations performed in each state. We also adjusted for the population adjusted number of confirmed COVID-19 cases (cases per 100k population) as reported by the OxCGRT in order to account for differences in the effectiveness of the government policies introduced to reduce transmission. The final models were checked for overdispersion based on the residual deviance and degrees of freedom. We then calculated estimated marginal means in order to estimate the degree of backlog associated with each index score.
All analyses were conducted in R v4•03. Linear mixed-effects models were fitted using the “lme4” package. Maps were constructed using the program ArcGIS Pro (version 2•6). The country shapefile was obtained from the ArcGIS online repository. Equal quantiles were used to subdivide the population-adjusted surgical backlog per state.
This study was not considered human subject research and was exempt from requiring IRB approval. All data used for this study is open source country-level data. All estimates were summarized according to the Guidelines for Accurate and Transparent Health Estimates Reporting (GATHER) statement [18].
Role of the Funding Source: All authors had full access to all the data and accepted responsibility to submit for publication. There was no sponsor or funding for this research.
3. Results
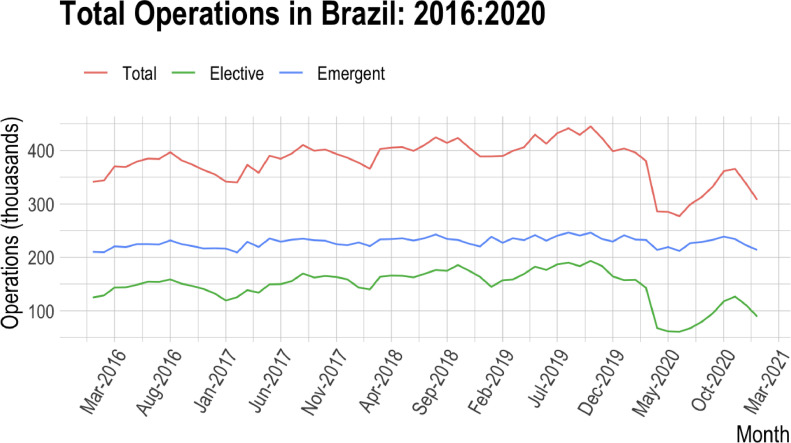
A total of 4996,963 operations were performed in Brazil's SUS system in 2019 compared to a total of 4038,321 in 2020. In 2019, the total number of emergent operations performed was 2844,255 which dropped to a total of 2736,264 in 2020. A total of 2089,807 elective procedures were performed in 2019 which dropped to 1244,433 in 2020 (Fig. 1). This corresponds to a 19% reduction in total surgical volume, 4% reduction in emergency volume, and 40% reduction in elective volume.
Fig. 1.
The monthly total, emergent, and elective operations performed in Brazil from January 2016 to January 2021. The monthly total, emergent, and elective operations performed in Brazil from January 2016 to January 2021. This Figure. depicts the number of operations over time and shows a dramatic decrease in operations in 2020.
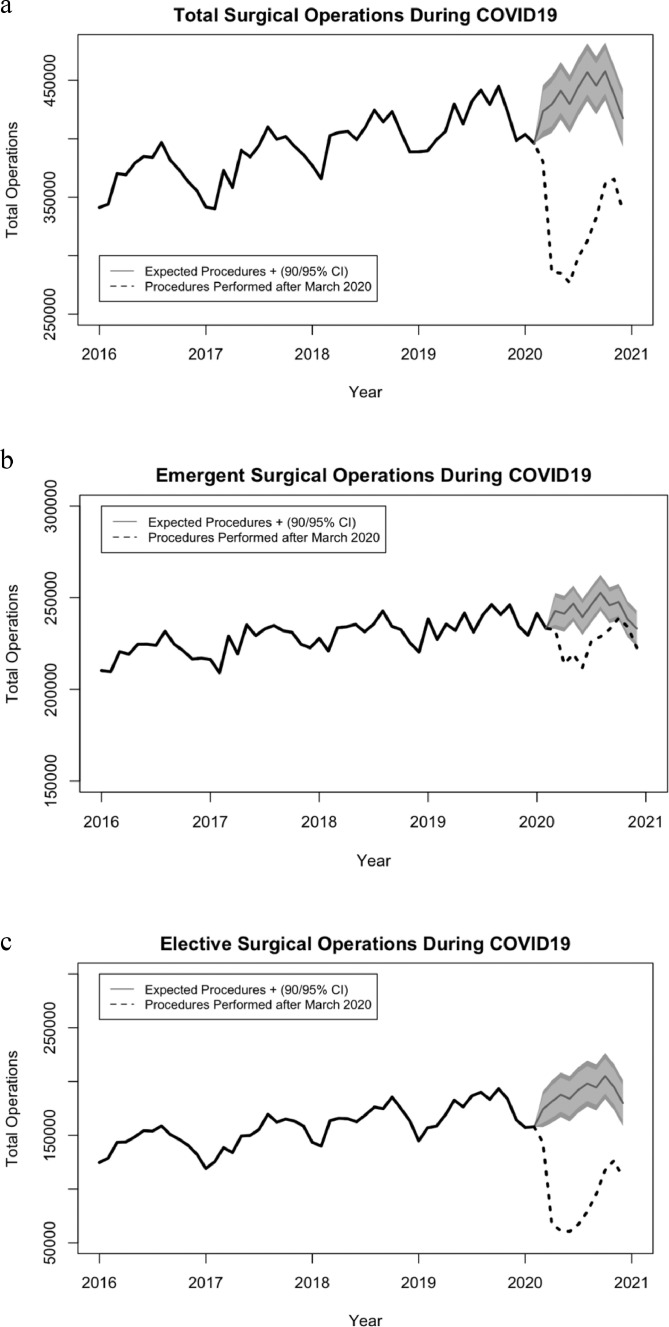
Between March 2020 and December 2020, the total surgical backlog included 1119,433 (95% Confidence Interval 762,663–1523,995) total operations, 161,321 (95% CI 37,468- 395,478) emergent operations and 928,758 (95% CI 675,202–1208,769) elective operations. The total backlog of 1119,433 cases represents 22% of total cases, 6% of emergent cases and 69% of elective cases that were expected to be performed in 2020 (Fig. 2).
Fig. 2.
Expected vs performed operations during the COVID-19 pandemic in Brazil for A) total, B) emergent, and C) elective operations. ARIMA models of surgical procedures in Brazil for A) total, B) emergent, and C) elective operations. Solid black represents historical data, dashed line represents true surgical operations between January 2016 and January 2021. Light grey (90%), and dark grey (95%) represent confidence intervals for predicted number of operations based on historical trends. All panels show a reduction in operations compared to expected rates based on historical data, however this decrease is mainly driven by elective procedures as seen in Panel C.
All five regions developed surgical backlogs in 2020. Regionally the total surgical backlog ranged from 492,746 (95% CI 374,603–611,560) to 281,355 (95% CI 177,829–411,413). The Northeast and Southeast regions experienced the largest number of delayed or canceled emergent surgeries: 47,693 (95% CI 9585–123,875) in the Northeast region and 47,110 (95% CI 10,737–107,799) in the Southeast region (Table 1).
Table 1.
Brazilian Surgical Population-Adjusted Backlog per 100,000 by Region.
| Region | Total Backlog |
||
|---|---|---|---|
| Total | Emergent | Elective | |
| Midwest | 65,705(30,472–114,123) | 15,803(1097–47,846) | 49,327(30,017–69,979) |
| North | 70,398(32,588–115,454) | 25,118(10,985–53,901) | 34,774(11,236–69,508) |
| Northeast | 281,355(177,829–411,413) | 47,693(9585–123,875) | 224,120(145,164–315,719) |
| South | 209,229(147,171–271,446) | 25,596(5064–62,057) | 186,373(145,549–228,113) |
| Southeast | 492,746(374,603–611,560) | 47,110(10,737–107,799) | 434,164(343,237–525,449) |
| Total | 1119,432 (762,663 - 1523,996 | 161,329(37,468–395,478) | 928,758(675,203–1208,768) |
Backlog = Delayed surgical interventions (or cases). Data are presented in number (95% Confidence Interval).
Population adjusted backlogs were highest in the South at 693 (95% CI 147,171–271,446) procedures per 100,000 followed by Southeast 554 (95% CI 374,603–611,560), Northeast 490 (95% CI 177,829–411,413), Midwest 398 (95% CI 30,472–114,123), and North 377 (95% CI 32,588–115,454) (Fig. 3).
Fig. 3.
Brazilian population-adjusted surgical backlog per 100,000 by state for A) total, B) emergent, and C) elective delayed procedures This series of maps shows Brazilian population-adjusted surgical backlog per 100,000 population by state for A) total, B) emergent, and C) elective delayed procedures. The map displays the population-adjusted backlog using the equal quantile distribution in four groups.
At the state level, the mean backlog was 41,460 (SD 55,052) total cases. The mean emergent backlog was 5975 (SD 5250), and mean elective backlog was 34,398 (SD 49,955). The total number of canceled operations ranged from 740 (0–3973) in Acre to 265,641 (211,202–320,081) in São Paulo (Table 2; Appendix 2).
Table 2.
Brazilian surgical backlog and population-adjusted backlog (per 100,000) by State.
| State | Estimated Population in 2020 | Number of Delayed Cases (95% CI) |
|||||
|---|---|---|---|---|---|---|---|
| Total |
Emergent |
Elective |
|||||
| Backlog | Population Adjusted Backlog (per 100k population) | Backlog | Population Adjusted Backlog (per 100k population) | Backlog | Population Adjusted Backlog (per 100k population) | ||
| Acre | 894,470 | 740 (0–3973) | 83 (0–444) | 291 (0–1603) | 33 (0–179) | 478 (0–3236) | 53 (0–361) |
| Alagoas | 3351,543 | 15,806 (9014–24,482) | 472 (268–730) | 3370 (1039–6968) | 101 (31–207) | 15,560 (10,974–20,517) | 464 (327–612) |
| Amapá | 861,773 | 2997 (817–5834) | 348 (94–677) | 1277 (117–3518) | 148 (13–408) | 2109 (966–3287) | 245 (112–381) |
| Amazonas | 4207,714 | 12,279 (5231–20,031) | 292 (124–476) | 3567 (471–9242) | 85 (11–219) | 8389 (4190–12,764) | 199 (99–303) |
| Bahia | 14,930,634 | 95,874 (71,540–120,207) | 642 (479–805) | 10,191 (378–27,823) | 68 (2–186) | 75,025 (54,935–95,116) | 502 (367–637) |
| Ceará | 9187,103 | 29,589 (12,432–52,438) | 322 (135–570) | 7501 (839–17,717) | 82 (9–192) | 22,779 (7991–39,209) | 248 (86–426) |
| Distrito Federal | 3055,149 | 9600 (0–32,035) | 314 (0–1048) | 4886 (0–19,726) | 160 (0–645) | 6956 (2320–12,726) | 228 (75–416) |
| Espírito Santo | 4064,052 | 34,319 (21,507–47,802) | 844 (529–1176) | 447 (0–5083) | 11 (0–125) | 28,173 (21,209–35,496) | 693 (521–873) |
| Goiás | 7113,540 | 25,115 (13,878–36,352) | 353 (195–511) | 5347 (29–15,065) | 75 (0.407–211) | 13,481 (6864–20,305) | 190 (96–285) |
| Maranhão | 7114,598 | 20,592 (6270–50,385) | 289 (88–708) | 8467 (1363–24,166) | 119 (19–339) | 12,558 (3988–29,868) | 177 (56–419) |
| Mato Grosso | 3526,220 | 14,575 (8740–20,410) | 413 (247–578) | 4185 (750–9015) | 119 (21–255) | 12,054 (8339–15,768) | 342 (236–447) |
| Mato Grosso Do Sul | 2809,394 | 16,414 (7853–25,326) | 584 (279–901) | 1385 (318–4039) | 49 (11–143) | 16,837 (12,493–21,180) | 599 (444–753) |
| Minas Gerais | 21,292,666 | 113,936 (86,684–141,188) | 535 (407–663) | 13,235 (5652–24,305) | 62 (26–114) | 102,958 (78,946–126,970) | 484 (370–596) |
| Pará | 8690,745 | 33,320 (17,718–49,696) | 383 (203–571) | 10,500 (5351–19,889) | 121 (61–228) | 13,651 (4256–26,910) | 157 (48–309) |
| Paraíba | 4039,277 | 17,161 (11,657–22,665) | 425 (288–561) | 94 (0–5163) | 2 (0–127) | 13,869 (9214–18,523) | 343 (228–458) |
| Paraná | 11,516,840 | 102,255 (78,906–125,603) | 888 (685–1090) | 14,529 (5064–26,578) | 126 (43–230) | 91,529 (75,477–107,581) | 795 (655–934) |
| Pernambuco | 9616,621 | 60,100 (48,155–72,044) | 625 (500–749) | 12,120 (4657–20,568) | 126 (48–213) | 47,536 (37,314–57,758) | 494 (388–600) |
| Piauí | 3281,480 | 21,292 (10,246–32,344) | 649 (312–985) | 4415 (1309–8588) | 135 (39–261) | 15,270 (8611–21,929) | 465 (262–668) |
| Rio de Janeiro | 17,366,189 | 78,850 (55,211–102,489) | 454 (317–590) | 13,503 (1021–34,624) | 78 (5–199) | 61,471 (46,128–76,815) | 354 (265–442) |
| Rio Grande do Norte | 3534,165 | 14,662 (6911–23,789) | 415 (195–673) | 1102 (0–7983) | 31 (0–225) | 12,374 (6475–19,609) | 350 (183–554) |
| Rio Grande do Sul | 11,422,973 | 48,040 (28,279–67,960) | 421 (247–594) | 5585 (0–17,906) | 49 (0–156) | 46,779 (36,796–57,678) | 410 (322–504) |
| Rondônia | 1796,460 | 6638 (1857–12,263) | 370 (103–682) | 2481 (342–6699) | 138 (19–372) | 3940 (0–12,396) | 219 (0–690) |
| Roraima | 631,181 | 1950 (22–4932) | 309 (3–781) | 737 (0–2887) | 117 (0–457) | 1243 (0–2715) | 197 (0–430) |
| Santa Catarina | 7252,502 | 58,934 (39,986–77,882) | 813 (551–1073) | 5481 (0–17,573) | 76 (0–242) | 48,064 (33,276–62,853) | 663 (458–866) |
| São Paulo | 46,289,333 | 265,641 (211,202–320,081) | 574 (456–691) | 19,925(4064–43,787) | 43 (8–94) | 241,562(196,955–286,169) | 522 (425–618) |
| Sergipe | 2318,822 | 6280 (1604–13,059) | 271 (69–563) | 433 (0–4899) | 19 (0–211) | 9149 (5662–13,191) | 395 (244–568) |
| Tocantins | 1590,248 | 12,473 (6944–18,725) | 784 (436–1177) | 6265 (4704–10,064) | 394 (295–632) | 4965 (1824–8199) | 312 (114–515) |
Backlog = Delayed surgical interventions (or cases). Data are presented in number (95% Confidence Interval).
Increases in the Stringency Index were associated with reduced total surgical backlogs [incident rate 0•84 (95% CI 0•82–0•87), P < 0•001], and reduced delays in emergent surgical delivery [IRR 0•52 (0•48–0•56), P < 0•001], but increased elective surgical backlogs [1•22 (95% CI 1•17–1•27), P< 0•001]. Increases in the Containment and Health Index were also associated with reduced total surgical backlogs [0•97 (95% CI 0•94–1•01), P = 0•141], reduced emergent surgical backlog [0•64 (95% CI 0•59–0•69), P < 0•001], and increased elective backlogs [1•11 (95% CI 1•07–1•16), P < 0•001]. Increasing number of COVID-19 cases was associated with increases in both delayed emergent surgical care and elective backlogs (Table 3).
Table 3.
Linear mixed models.
| Stringency Index |
Containment and Health Index |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| All Operations |
Emergent Operations |
Elective Operations |
All Operations |
Emergent Operations |
Elective Operations |
|||||||
| Predictors | Incidence Rate Ratios | p | Incidence Rate Ratios | p | Incidence Rate Ratios | P | Incidence Rate Ratios | p | Incidence Rate Ratios | p | Incidence Rate Ratios | p |
| Intercept | 26•79(16•45–43•62) | < 0•001 | 69•20(25•13–190•58) | < 0•001 | 3•80(2•54–5•69) | < 0•001 | 17•54(11•10–27•71) | < 0•001 | 36•99(14•45–94•68) | < 0•001 | 5•94(3•92–8•99) | < 0•001 |
| Stringency Index | 0•75(0•73–0•78) | < 0•001 | 0•33(0•31–0•36) | < 0•001 | 1•16(1•12–1•21) | < 0•001 | ||||||
| Confirmed COVID-19 Cases (per 100k pop) | 1•29(1•28–1•30) | < 0•001 | 1•46(1•45–1•48) | < 0•001 | 1•24(1•24–1•25) | < 0•001 | 1•27(1•27–1•28) | < 0•001 | 1•44(1•42–1•45) | < 0•001 | 1•25(1•25–1•26) | < 0•001 |
| Containment and Health Index | 0•84(0•81–0•87) | < 0•001 | 0•38(0•35–0•41) | < 0•001 | 1•04(1•00–1•08) | 0•060 | ||||||
| Random Effects | ||||||||||||
| σ[2] | 0•00 | 0•00 | 0•00 | 0•00 | 0•00 | 0•00 | ||||||
| τ00 | 0•23 State | 1•06 State | 0•34 State | 0•24 State | 1•07 State | 0•34 State | ||||||
| 0•48 Month | 1•99 Month | 0•23 Month | 0•41 Month | 1•62 Month | 0•26 Month | |||||||
| ICC | 1•00 | 1•00 | 1•00 | 1•00 | 1•00 | 1•00 | ||||||
| N | 10 Month | 10 Month | 10 Month | 10 Month | 10 Month | 10 Month | ||||||
| 25 State | 25 State | 25 State | 25 State | 25 State | 25 State | |||||||
At the maximal Stringency Index (score = 100) or maximal Containment and Health Index (score = 100) there are nearly zero delays in emergent surgical care, but an average increase in 3000 state-level elective operations per month (Fig. 4).
Fig. 4.
Relationship between total surgical backlog and government policy response Estimated marginal means were performed to plot the relationship of the stringency index and containment and health index and the A) total surgical backlog B) emergent surgical backlog and C) elective surgical backlog. As stringency increases, the total backlog and emergent backlog decreases, while the elective backlog increases for both COVID-19 policy indices.
A sensitivity analysis was performed using historical data from 2016 through 2018 to predict total monthly surgical volume for 2019 using the same Arima methodology used for surgical backlog estimation. Predicted values had an average error of 1.7% and all months were within the 95% confidence interval of our predictive interval (Appendix 3).
4. Discussion
The COVID-19 pandemic has resulted in a global reduction in surgical delivery due to significant delays and cancellations of both elective and emergent surgical procedures leading to a large backlog of cases. Our findings suggest that since March 2020, when the first case of COVID-19 was reported, 1119,433 fewer total operations were performed than expected across Brazil's public health system. The 161,321 fewer emergent operations performed represent potential reductions in access to emergent surgical care, and the 928,758 fewer elective operations make up a considerable backlog that may take years to resolve and likely will result in delayed treatment for a variety of surgically amenable conditions. Furthermore, increases in COVID-containment policies increased the delivery of emergent surgical procedures, but nearly tripled elective backlogs. This suggests that these local policies may allow emergent surgical care to remain available, but also drive larger elective backlogs. These results highlight the importance of maintaining COVID-19 management policies that are evidence-driven and in accordance with local resources in order to ensure optimal access to emergent surgical care while also preparing for larger elective surgical backlogs.
At the beginning of the pandemic, multinational collaborative studies offered guidance on how countries’ surgical backlogs would be managed, in an attempt to coordinate systemic and interdisciplinary strategies to mitigate the burden of this public health emergency [10]. High income countries such as England, Canada, and the United States have been forecasting on the building backlog and sharing possible plans to tackle this crisis. In England for instance they calculate a backlog of 1 200 000 cases over a 3 month period [12]. In Ontario, Canada, they calculated between March 15th and June 13th of 2020, resulting in an estimated backlog of 148 364 surgeries [19]. In the United States looking into elective orthopedic surgery lenses, they estimate a cumulative backlog of approximately 1 million orthopedic surgical cases. In addition, they speculate that it would take around 7 to 16 months for the system to be able to perform 90% of the expected pre-pandemic forecasted volume [20]. Despite this joint effort, few studies have focused on the current surgical backlog in LMICs, a group of countries that, prior to the pandemic, were most affected by lack of access to timely and safe surgical, obstetric, anesthesia, and trauma care. Understanding that each nation's response to the surgical backlog will be tailored to their specific needs and regional differences, our study exemplifies how local data coupled with modeling can be used to identify gaps, provide comprehensive analysis, and allow for policy recommendations for developing a plan to begin to address the surgical backlog caused by the pandemic.
In Brazil, the National Health Agency, with the support of the country's surgical societies, recommended postponing elective surgeries on March 25th, [21] authorizing resuming procedures on June 7th, 2020 [22]. These measures were necessary to increase medical resources available for COVID-19 infected patients and reduce infection rates among elective patients, visitors, and health professionals [10]. Concurrently, emergency surgical care was also hampered, as access to operating rooms became increasingly limited, and surgeons were encouraged to consider non-operative treatments when feasible and safe for the patient [10]. In Brazil, estimates of cancelation rates for cancer, benign and obstetric surgeries were 43•6%, 81•2%, and 26•1% respectively, with an estimated 46 weeks required to clear the backlog if an additional 20% operations were performed above baseline surgical volume [1].
We found that while there were reductions in the number of both emergent and elective surgical cases performed across Brazil, the majority of canceled or delayed cases were elective. This aligns with international consensus guidelines on handling surgical care during the pandemic which have typically advised postponing elective surgery while continuing any necessary emergent surgical care [23]. Work by the COVIDSURG collaborative found that perioperative outcomes were worse for those with COVID-19 infections and further supports that avoiding operations on infected individuals improves outcomes and recommended delaying surgery up to seven weeks following infection [24,25]. Another study by the COVIDSURG collaborative observed that previous SARS-CoV-2 infection was associated with increased odds of pulmonary complications and mortality compared to no infection, with the lowest rates occurring at least 4 weeks after notification of a positive swab test [26]. Elective surgical cancellations represent a reasonable approach to limiting additional stress on health systems, preserving hospital capacity and supplies, especially personal protective equipment (PPE), avoiding hospital-acquired infection, and reducing the potential for increased postoperative complications among infected individuals. Moreover, reduction of elective surgeries was an alternative to further diminish social interaction, spread of COVID-19, and mobility in the community, as preventive measures to combat the pandemic, entail a health system stress and an increased backlog. Previous estimates obtained through a mixed-methods approach suggest that as many as 28,404,603 elective operations were canceled globally due to the pandemic during the 12 weeks of peak disruption [1]. Our results represent the first Latin American country to quantify its surgical backlog. The large elective backlog likely comprises surgical interventions for the treatment of cancer or other conditions where worse patient outcomes can be expected after significant delays [27]. The impact of these practices has yet to be quantified in most countries; nevertheless, there is a considerable concern for a large surgical backlog [28]. Our findings support these concerns as over 900,000 fewer elective operations were performed in 2020 alone, a trend that will likely continue through 2021 as COVID-19 continues to have a significant impact in the country.
Our findings also showed that stronger government responses as measured by the Stringency Index and Containment and Health Index were associated with reduced delays in emergent surgery, but significantly larger elective surgical backlogs. Brazilian states where measures were more rigorous had fewer elective surgeries, which could be explained by the population's higher compliance with lockdown measures, political support for adopting social distancing rather than against it and for hospital support to cancel surgery [29]. At the pandemic's onset, the mortality index for COVID-19 was higher in socioeconomically vulnerable states, particularly in the North and Northeast regions. However, owing to these states' capacity to produce stricter measures and populations' higher adherence to physical distancing, mortality index was reverted, while states with higher HDI reported more deaths. Stringent policies were effective against the increase of COVID-19 cases and that the socioeconomic vulnerability was balanced with population level behaviors, policy implementation, better primary healthcare programs, and coverage of social assistance [30]. These results support the idea that a well-coordinated governmental response to COVID-19 aligned with recommendations for public health organizations and medical societies may have mitigated poor surgical outcomes. Further studies are needed to assess how these measures will affect the speed at which countries will recover from the backlog. These indexes may be valuable in other LMICs to identity regions where subnational surgical backlogs may be largest, and guide policymakers to promote a controlled openness of cities, increasing health-system preparedness to resolve the backlog [5].
The six percent reduction in emergent operations is particularly concerning given that we expect emergent surgical need to remain unchanged during the pandemic and the lower numbers likely reflect patients who did not receive a necessary operation. Although the decrease in emergent procedures was smaller in comparison to elective procedures, the consequences for not performing emergent surgeries are larger in terms of morbidity, mortality, disability, and costs since they are essential to treat acute and life-threatening conditions, including obstetric complications, traumatic injuries, communicable and non-communicable diseases [31]. Concentrating efforts in strengthening and improving access to emergent surgical and anesthesia is essential to the health of a population. Further research is necessary, however, to better understand how the pandemic has changed case mix and the need for emergent operations. Reductions in road traffic accidents, gunshots, stab wounds, and interpersonal violence, may have contributed to the decline of emergency operations is the overall trauma cases during the period of lockdown [32].
Furthermore, our study demonstrated that increased COVID-19 case rates are independently associated with increased surgical backlogs across Brazil's 27 states despite broad differences in public health policy and health system strength. This may imply that local COVID-19 case control will directly impact surgical backlogs. Many LMICs do not have coordinated subnational monitoring of surgical cases, and thus our results suggest that the number of COVID-19 cases may be used to identify regions where surgical backlogs are highest. Preparedness for health outbreaks requires a systemic and continuous process of planning and implementation at national and international levels. Therefore, strengthening health systems is pivotal through the development and maintenance of core capacities for surveillance and response, a process that demands the involvement of different stakeholders, including countries’ surgical workforce. It is imperative that surgeons be involved in public health and advocacy to minimize COVID-19 transmission, ultimately aiming to reduce the backlog and ensure access to surgical services. Such efforts comprise the development of strategies to disseminate and translate knowledge to the local community, which includes protocols, evidence-based information, and active involvement of civil society in managing the current health emergency. To decrease the risk of surgical team contamination with SARS-CoV-2 during surgical procedures, it is essential that the appropriate use of PPE, including face shields, N95 masks, gloves, waterproof gowns, and shoe covers be available [33]. A strategy that has been used to avoid contamination during PPE replacement is the “Buddy System”, in which someone oversees and assists in the process [30]. Moreover, usage of devices such as aerosol boxes has been noticed as a reliable protective resource to surgical staff that minimizes contagion during open suctioning of airways and endotracheal intubation or extubation [34].
Given the enormous number of delayed operative cases in regions of high COVID-19 prevalence, along with factors such as health workforce exhaustion and resources depletion, strategies to overcome the increasing surgical backlog will become critical over the next several years which should be staged and prioritize essential needs. Hospital preparedness and national guidelines are necessary in order to guide how and when surgery is resumed and which procedures will have the highest impact on morbidity associated with operative delays [35]. Additionally, it is vital to expand and equip the surgical workforce, including training on using PPE and funding for surgery in low-resource settings [36]. Hospitals must consider expanding surgical hours and performing elective surgeries over the weekends in order to expand their surgical capacity to address the backlog [35]. In addition, surgical system inventory and supply chain management as well as the safety of all patients and hospital staff must be taken into consideration when planning for the scheduling of the backlog of elective cases [35]. Emergent operations have also been affected which suggests that additional measures must be taken to minimize the patient risk of exposure to SARS-CoV-2 while weighing the morbidity of the primary diagnosis, and the accumulated morbidity that the delay in the procedure has caused [35]. Existing criteria and practice recommendations for patient selection to emergency and elective surgeries have been revised in some countries in order to lessen the burden on medical resources, maximizing, when possible, the use of non-operative treatments and ambulatory or minimally invasive surgery, and the referral of patients to sub-specialty trained, high-volume surgeons [37]. In this instance, one must acknowledge the advantages of telemedicine, which consists of the healthcare delivered remotely to a patient through information and communication technology, including the provision of diagnosis, monitoring, and treatment services [38]. Telemedicine practices in outpatient follow-up or in non-operative treatments can also play an important role in high demand settings and for very common conditions such as management of appendicitis by reducing the number of hospital admissions, providing an alternative to triage, and facilitating peer-to-peer exchange between healthcare providers [37,39,40]. Protocols must be put in place to allow patients who have been recently diagnosed with COVID-19 to safely undergo surgery when needed. Equipping surgeons to safely perform emergent surgery when needed is necessary to reduce the number of delayed or canceled emergent options. Finally, continuous guidance and provision of proper information to the community, along with societal accountability and commitment, is vital to effectively control COVID-19 cases and enable surgical systems’ recovery.
4.1. Limitations
Our study has several limitations. Data on surgical volume does not include private healthcare facilities, used by approximately 24% of the population. Therefore, as our study focuses on Brazil's public health sector, it underestimates canceled surgeries in the private health sector, which may have also absorbed some cases from the public health sector. Reporting in DATASUS can lag up to six months, and the impact of the pandemic on reporting to the national reporting system has not been studied, however, we only used data through December 2020 in order to minimize this possible bias. Furthermore, data quality within DATASUS has been criticized as lacking reliability from a hospital reporting perspective, in particular about surgical volume which may have led to underreporting. Differences in socioeconomic factors between states may also impact surgical backlogs and may not be completely captured by our models, however we used hierarchical linear mixed models and adjusted for COVID-19 cases in an attempt to bluntly capture these potential differences among states which each administer health care independently. The composite metrics used to measure policy response are broad and do not capture how well the policies are enforced or implemented. We adjusted for population adjusted COVID-19 case rates in order to bluntly capture response success however access to testing in Brazil has been varied and thus introduced bias when using case rates. Lastly, our results are based on a single country and may not apply to other settings; however, Brazil's states represent broad socioeconomic diversity that is similar to several LMIC countries.
5. Conclusion
As a result of the pandemic, over a million surgical procedures have been delayed or canceled in Brazil and the elective surgical backlog is over 900,000 cases. Stricter government policy responses are associated with reductions in delayed emergent surgery, but large increases in elective surgical backlogs. Our findings suggest that stringent efforts to reduce COVID-19 spread will be associated with reduced delays and cancellations for emergent surgery but will require coordinated government efforts to expand surgical care to overcome elective backlogs. Future work is needed to understand if stricter implementation of policy measures results in a more rapid return to expected surgical volume, and if there is an association between numbers of COVID-19 cases and speed that regions and states reopened. Future directions should also investigate if outcomes of procedures will improve as the surgical backlog resumes, as well as which state-level backlog resumed the fastest. Higher local case rates are independently associated with increased numbers of delayed operations, suggesting that local efforts to reduce COVID-19 spread can reduce delays and cancellations of both emergent and elective surgical operations. These results also highlight the need for surgeons to take an active role in local public health measures.
Our findings emphasize the crucial demand for appropriate public health policies and timely governmental action plans to overcome such a crisis. To adequately handle the current surgical backlog, guidance on establishing criteria to prioritize procedures must be acknowledged and suit the local context. Moreover, attention should be given to patients who had COVID-19 infection to schedule surgeries, resources and guarantee optimal outcomes. Several national and international organizations have designed protocols on triage of surgical care during the pandemic in order to provide some guidance, however national level policies may help surgeons decide which operations should be delayed and which should take precedence in the face of limited resources [10,12]. Studies examining conservative management of surgically amenable such as appendicitis have raised the possibility of adjusting surgical management to conservative approaches during the pandemic [40]. Robust telemedicine systems may help to provide outpatient follow-up for these types of management and may be a worthwhile investment for Brazil from a surgical standpoint. Additionally, it is pivotal to keep transport networks and supply chains open to facilitate timely, equitable, and affordable access to medical products, including PPE.
Achieving resilient surgical health systems as an essential foundation for effective preparedness and response to health emergencies. Policymakers must look to strengthen several aspects of the Brazilian surgical system. Expansion of the surgical workforce is critical, not only in terms of absolute numbers, but also the distribution of surgeons across the country. Second, investment in hospital capacity ensures availability of operations rooms, ICU and beds. Third, investment in innovative strategies such as telemedicine consultation to support remote postoperative care or conservative non-surgical treatment of surgical conditions. Lastly, local and regional, evidence-based guidelines in order to guide hospital systems and allow the continuation of emergent and urgent surgery while appropriately triaging and tracking elective surgical patients.
Acknowledgments
Contributors
Paul Truche: Conceptualization, Data curation, Validation, Visualization, Writing original draft, Formal analysis, Writing review & editing, Investigation. Letícia Nunes Campos: Conceptualization, Data curation, Writing original draft, Writing review & editing, Investigation. Enzzo Barrozo Marrazzo: Conceptualization, Data curation, Writing original draft, Writing review & editing, Investigation. Ayla Gerk Rangel: Conceptualization, Data curation, Writing original draft, Writing review & editing, Investigation. Ramon Bernardino: Conceptualization, Data curation, Writing original draft, Writing review & editing, Investigation. Alexis N Bowder: Validation, Writing review & editing, Investigation. Alexandra M Buda: Conceptualization, Data curation, Visualization, Writing original draft, Writing review & editing, Investigation. Isabella Faria: Writing original draft, Writing review & editing, Investigation. Laura Pompermaier: Writing review & editing, Investigation. Henry E. Rice: Writing review & editing, Investigation. David Watters: Conceptualization, Writing review & editing. Fernanda Lage Lima Dantas: Writing review & editing, Investigation. David P. Mooney: Writing review & editing, Investigation. Fabio Botelho: Validation, Writing review & editing, Investigation. Rodrigo Vaz Ferreira: Validation, Conceptualization, Formal analysis, Writing review & editing, Investigation. Nivaldo Alonso: Conceptualization, Data curation, Validation, Writing review & editing, Investigation.
Declaration of Competing Interests
None.
Data Sharing
All data used in these analyses are publicly available from Brazil's SUS Health System Informatics Department and the Oxford COVID-19 Government Response Tracker. For further details on the data included, please see Appendix 1.
Acknowledgements
None.
Editor Disclaimer
The Lancet Group takes a neutral position with respect to territorial claims in published maps and institutional affiliations.
Funding
None.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.lana.2021.100056.
Appendix. Supplementary materials
References
- 1.COVIDSurg Collaborative Elective surgery cancellations due to the COVID-19 pandemic: global predictive modelling to inform surgical recovery plans. Br J Surg. 2020;107:1440–1449. doi: 10.1002/bjs.11746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stöß C., Steffani M., Kohlhaw K., et al. The COVID-19 pandemic: impact on surgical departments of non-university hospitals. BMC Surg. 2020;20:313. doi: 10.1186/s12893-020-00970-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Meredith J.W., High K.P., Freischlag J.A. Preserving elective surgeries in the COVID-19 pandemic and the future. JAMA. 2020 doi: 10.1001/jama.2020.19594. published online Oct 5. [DOI] [PubMed] [Google Scholar]
- 4.Sharma D., Agrawal V., Agarwal P. Roadmap for restarting elective surgery during/after COVID-19 pandemic. Indian J Surg. 2020:1–5. doi: 10.1007/s12262-020-02468-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hale, Thomas, Thomas Boby, Noam Angrist, Emily Cameron-Blake, Laura Hallas, Beatriz Kira, Saptarshi Majumdar, Anna Petherick, Toby Phillips, Helen Tatlow, Samuel Webster (2020). Oxford COVID-19 government response tracker, Blavatnik School of Government. Available: www.bsg.ox.ac.uk/covidtracker. . [DOI] [PubMed]
- 6.Piovani D., Christodoulou M.N., Hadjidemetriou A., et al. Effect of early application of social distancing interventions on COVID-19 mortality over the first pandemic wave: an analysis of longitudinal data from 37 countries. J Infect. 2021;82:133–142. doi: 10.1016/j.jinf.2020.11.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hale T., Angrist N., Goldszmidt R., et al. A global panel database of pandemic policies (Oxford COVID-19 government response tracker) Nat Hum Behav. 2021;5:529–538. doi: 10.1038/s41562-021-01079-8. [DOI] [PubMed] [Google Scholar]
- 8.Taylor L. Covid-19: Brazil breaks record daily death toll as crisis spreads through South America. BMJ. 2021;373:n930. doi: 10.1136/bmj.n930. [DOI] [PubMed] [Google Scholar]
- 9.Supremo decide que estados e municípios têm poder para definir regras sobre isolamento. 2020; published online April 15. https://g1.globo.com/politica/noticia/2020/04/15/maioria-do-supremo-vota-a-favor-de-que-estados-e-municipios-editem-normas-sobre-isolamento.ghtml (accessed May 13, 2021).
- 10.COVIDSurg Collaborative Global guidance for surgical care during the COVID-19 pandemic. Br J Surg. 2020;107:1097–1103. doi: 10.1002/bjs.11646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Clarke J., Murray A., Markar S.R., Barahona M., Kinross J., PanSurg Collaborative New geographic model of care to manage the post-COVID-19 elective surgery aftershock in England: a retrospective observational study. BMJ Open. 2020;10 doi: 10.1136/bmjopen-2020-042392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Macdonald N., Clements C., Sobti A., Rossiter D., Unnithan A., Bosanquet N. Tackling the elective case backlog generated by COVID-19: the scale of the problem and solutions. J Public Health. 2020;42:712–716. doi: 10.1093/pubmed/fdaa155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Machado J.P., Martins M., Leite I da C. Quality of hospital databases in Brazil: some elements. Rev Bras Epidemiol. 2016;19:567–581. doi: 10.1590/1980-5497201600030008. [DOI] [PubMed] [Google Scholar]
- 14.Bittencourt S.A., Camacho L.A.B., Leal M do C. Hospital information systems and their application in public health. Cad Saude Publica. 2006;22:19–30. doi: 10.1590/s0102-311x2006000100003. [DOI] [PubMed] [Google Scholar]
- 15.Massenburg B.B., Saluja S., Jenny H.E., et al. Assessing the Brazilian surgical system with six surgical indicators: a descriptive and modelling study. BMJ Glob Health. 2017;2 doi: 10.1136/bmjgh-2016-000226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Serdan T.D.A., Masi L.N., Gorjao R., Pithon-Curi T.C., Curi R., Hirabara S.M. COVID-19 in Brazil: historical cases, disease milestones, and estimated outbreak peak. Travel Med Infect Dis. 2020;38 doi: 10.1016/j.tmaid.2020.101733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hyndman R.J., Khandakar Y. Others. automatic time series forecasting: the forecast package for R. J Stat Softw. 2008;27:1–22. [Google Scholar]
- 18.Stevens G.A., Alkema L., Black R.E., et al. Guidelines for accurate and transparent health estimates reporting: the gather statement. Lancet. 2016;388:e19–e23. doi: 10.1016/S0140-6736(16)30388-9. [DOI] [PubMed] [Google Scholar]
- 19.Wang J., Vahid S., Eberg M., et al. Clearing the surgical backlog caused by COVID-19 in Ontario: a time series modelling study. CMAJ. 2020;192:E1347–E1356. doi: 10.1503/cmaj.201521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jain A., Jain P., Aggarwal S. SARS-CoV-2 impact on elective orthopaedic surgery: implications for post-pandemic recovery. J Bone Joint Surg Am. 2020;102:e68. doi: 10.2106/JBJS.20.00602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.COVID-19: Nota do CBC/SBCO/SBOT sobre suspensão de cirurgias eletivas - CBC. 2020; published online March 29. https://cbc.org.br/covid-19-nota-do-cbc-sbco-sbot/ (accessed April 9, 2021).
- 22.Abib A.R., Soares C de F., Rodrigues T.J.M., Tanaka F.H.R., Martins A.C.M. PROCESSO no: 33910.007111/2020-95. Nota técnica no 10/2020/ASSNT-DIPRO/DIRAD-DIPRO/DIPRO. Agência Nacional de Saúde Suplementar 2020. http://www.ans.gov.br/images/Nota_T%C3%A9cnica_10.pdf (accessed April 9, 2021).
- 23.De Simone B., Chouillard E., Di Saverio S., et al. Emergency surgery during the COVID-19 pandemic: what you need to know for practice. Ann R Coll Surg Engl. 2020;102:323–332. doi: 10.1308/rcsann.2020.0097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.COVID Surg Collaborative. Global Surg Collaborative Timing of surgery following SARS-CoV-2 infection: an international prospective cohort study. Anaesthesia. 2021 doi: 10.1111/anae.15458. published online March 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nepogodiev D., Glasbey J.C., Li E., et al. Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: an international cohort study. Lancet. 2020 doi: 10.1016/S0140-6736(20)31182-X. published online May 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.COVID Surg Collaborative Delaying surgery for patients with a previous SARS-CoV-2 infection. Br J Surg. 2020;107:e601–e602. doi: 10.1002/bjs.12050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Al-Jabir A., Kerwan A., Nicola M., et al. Impact of the coronavirus (COVID-19) pandemic on surgical practice - Part 2 (surgical prioritisation) Int J Surg. 2020;79:233–248. doi: 10.1016/j.ijsu.2020.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Glauser W. Surgery backlog crisis looming. CMAJ. 2020;192:E593–E594. doi: 10.1503/cmaj.1095870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Centre for Economic Policy Research. https://cepr.org/active/publications/discussion_papers/dp.php?dpno=14707 (accessed May 18, 2021).
- 30.Rocha R., Atun R., Massuda A., et al. Effect of socioeconomic inequalities and vulnerabilities on health-system preparedness and response to COVID-19 in Brazil: a comprehensive analysis. Lancet Glob Health. 2021 doi: 10.1016/S2214-109X(21)00081-4. published online April 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Reynolds T.A., Sawe H., Rubiano A.M., Do Shin S., Wallis L., Mock C.N. Disease control priorities: improving health and reducing poverty. 3rd edition. The International Bank for Reconstruction and Development /The World Bank; 2017. Strengthening health systems to provide emergency care. [PubMed] [Google Scholar]
- 32.Ribeiro-Junior M.A.F., NÉder P.R., Augusto S.D.E.S., Elias Y.G.B., Hluchan K., Santo-Rosa O.M. Current state of trauma and violence in São Paulo - Brazil during the covid-19 pandemic. Rev Col Bras Cir. 2021;48 doi: 10.1590/0100-6991e-20202875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yánez Benítez C., Güemes A., Aranda J., et al. Impact of personal protective equipment on surgical performance during the COVID-19 pandemic. World J Surg. 2020;44:2842–2847. doi: 10.1007/s00268-020-05648-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bianco F., Incollingo P., Grossi U., Gallo G. Preventing transmission among operating room staff during COVID-19 pandemic: the role of the aerosol box and other personal protective equipment. Updates Surg. 2020;72:907–910. doi: 10.1007/s13304-020-00818-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Moawad G.N., Klebanoff J.S., Tyan P., Einarsson J.I. COVID-19: a surgical perspective for when the curve flattens. Facts Views Vis Obgyn. 2020;12:129–131. [PMC free article] [PubMed] [Google Scholar]
- 36.Brat G.A., Hersey S., Chhabra K., Gupta A., Scott J. Protecting surgical teams during the COVID-19 outbreak: a narrative review and clinical considerations. Ann Surg. 2020 doi: 10.1097/SLA.0000000000003926. published online April 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Di Saverio S., Pata F., Gallo G., et al. Coronavirus pandemic and colorectal surgery: practical advice based on the Italian experience. Colorectal Dis. 2020;22:625–634. doi: 10.1111/codi.15056. [DOI] [PubMed] [Google Scholar]
- 38.Gallo G., Picciariello A., Di Tanna G.L., et al. E-consensus on telemedicine in colorectal surgery: a RAND/UCLA-modified study. Updates Surg. 2021 doi: 10.1007/s13304-021-01139-8. published online July 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lurie N., Carr B.G. The role of telehealth in the medical response to disasters. JAMA Intern Med. 2018;178:745–746. doi: 10.1001/jamainternmed.2018.1314. [DOI] [PubMed] [Google Scholar]
- 40.Ielpo B., Podda M., Pellino G., et al. Global attitudes in the management of acute appendicitis during COVID-19 pandemic: acie appy study. Br J Surg. 2020 doi: 10.1002/bjs.11999. published online Oct 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.