Abstract
The sense of coherence (SOC) is defined as a personal orientation to life. People with higher SOC are better at dealing with stressful situations, psychological stress, and problems and are more able to manage them, leading to better general health. The purpose of this study was to evaluate the effect of SOC on the oral health status of people in different age groups. A systematic search up to May 2019 was carried out in PubMed,Scopus, Psycho info, and Persian sources. Studies were included if they evaluated the relationship between SOC and oral health behaviors (OHBs) or oral health status including dental caries. The Newcastle-Ottawa checklist was used to appraise the selected articles and meta-analysis of included studies were performed using Comprehensive Meta-Analysis software. Value of P < 0.05 was considered to be statistically significant. Odds ratio (OR) was used to measure effect size with 95% confidence interval (CI). The random-effects model was chosen in the presence of heterogenicity. I2 index and Q index were used to measure the heterogeneity present between the studies. Fifteen articles received the minimum score of criticism. In general, SOC could significantly affect the oral health and OHBs of adults independently of the underlying factors. There was a significant relationship between SOC and tooth decay in adolescents, but this association was poor after adjusting for the underlying factors. In children, only one article revealed an association with OHBs. Meta-analysis revealed that SOC was significantly associated with the caries rate (OR = 0.78, CI 95% = 0.9–0.67, P = 0.001) and tooth brushing frequency (OR = 1.22, CI 95% = 1.1–1.31 and P < 0.001). Sense of coherence appears to be one of the effective factors in predicting oral health behaviors and ultimately oral health, especially in adults. The number of articles available for children and adolescents was not sufficient in this regard.
Keywords: Behavior change, oral health, sense of coherence, systematic review
Introduction
Sense of coherence (SOC) is a health-promoting psychological resource that enhances a person's ability to cope with environmental stress and life tensions.[1] SOC indicates how individuals exhibit inner resistance to maintaining their health in stressful situations.[2] It consists of three dimensions of comprehensibility, manageability, and meaningfulness. Comprehensibility refers to defining events as being less stressful, manageability refers to mobilizing resources to deal with stressors, and meaningfulness refers to having motivation, willingness, and commitment to cope with stressors.[3] The SOC is defined as a personal orientation to life.[4] People with higher SOC are better at dealing with stressful situations, psychological stress, and problems and are more able to manage them, leading to better general health.[5,6]
Strong evidence is available indicating a positive correlation between SOC and chronic diseases such as insulin-dependent diabetes, cancer, and rheumatoid arthritis.[7] In addition, the SOC has been reported to be correlated with health behaviors such as dietary habits and alcohol consumption.[8] The correlation between SOC and oral health behavior (OHB) has been assessed in recent years. Freire et al. stated that people with higher SOC undertake more regular dental visits, even when they do not feel the need.[9] It has been reported that healthier OHBs and more knowledge about oral hygiene resulting in a lower incidence of dental caries.[10] In a cluster-randomized trial study, Nammontri et al. stated that increased SOC has a significant impact on the improvement of OHBs as well as the quality of life-related health behaviors.[11] Other studies have reported that people with higher SOC might have a greater number of filled teeth and lower rates of dental plaque and periodontal disease,[12] healthier eating habits,[13] and more tooth and lower daily smoking rate.[14] Savolainen et al. also confirmed a direct relationship between SOC and OHB and argued that the effects of the environment and mental health on health promotion should not be overlooked.[15]
Antonovsky argued that SOC is an age-related process that evolves during life, so children have lower SOC than adults. Although the exact relationship between age and SOC has not been established yet, studies have shown no direct relationship between age and SOC.[8]
Although there are some studies indicating an association between SOC and oral health in children and adolescents, there are limited systematic reviews evaluating this association among different age groups. Therefore, the purpose of this study was to evaluate the correlation of SOC in children, adolescents, and adults and oral health or oral health-related behaviors.
Materials and Methods
This systematic review and meta-analysis study was approved by the Deputy of Research at Isfahan University of Medical Sciences (No: 398032, Code of Ethics: IR. MUI. RESEARCH. REC.1398.070).
Inclusion and exclusion criteria
The cross-sectional and cohort studies written in Persian and English that assessed the relationship between SOC and OHB and status and were conducted on one of the age groups of children, adolescents, or adults were recruited. PECO was considered as P: children, adolescent, adult; E: SOC; O: OHB, oral health status including dental caries and plaque index. The manuscripts that were not available or had assessed the effect of oral health status/behavior on SOC were excluded. SOC index in the studies had to be investigated based on Antonovsky's short-form questionnaire (13 questions). The Antonovsky's Questionnaire with 29 closed questions, each with a score of 1–7, was developed to operationalize the construct in 1983 and has been approved to have validity and reliability for measuring SOC.[16]
Primary outcomes
The status of dental caries measured by indices such as DMFT and ICDAS and/or hygiene status measured by plaque index were considered primary outcomes.
Secondary outcomes
OHBs, including frequency of tooth brushing, using dental floss, nutrition pattern, and dental visit patterns were considered secondary outcomes.
Search protocol
To retrieve the required Persian language articles in this study, Persian databases, including Jihad Academic, Civilica, Iranian Medical Library, and Iranian Theses of Medical Sciences were searched. To elicit the relevant English language articles, Medline (PubMed), Embase, and ERIC databases were searched up to May 2019 without time restrict using relevant keywords, including SOC, oral health status, OHB, children, adolescents, and adults. Table 1 presents the keywords and search protocols for each database.
Table 1.
Search protocols in PubMed and Embase
| PubMed |
| 1. Search “Dental Caries”[Mesh] |
| 2. Search (tooth OR teeth OR enamel OR dentin) AND (cavity OR caries OR decay) |
| 3. Search “Oral Hygiene”[Mesh] |
| 4. Search “Tooth brushing”[Mesh] |
| 5. Search “Office Visits”[Mesh] |
| 6. Search “dental visit” OR “dental attendance” OR “dental attending” |
| 7. Search “oral health behavior” |
| 8. Search “Sense of Coherence”[Mesh] |
| 9. Search “Dental Plaque”[Mesh] |
| 10. Search “Diet, Cariogenic”[Mesh] |
| 11. Search (((((((“Diet, Cariogenic”[Mesh]) OR “Dental Plaque”[Mesh]) OR “oral health behavior”) OR (“dental visit” OR “dental attendance” OR “dental attending”)) OR “Toothbrushing”[Mesh]) OR “Oral Hygiene”[Mesh]) OR ((tooth OR teeth OR enamel OR dentin) AND (cavity OR caries OR decay))) OR “Dental Caries”[Mesh] |
| 12. Search (((((((((“Diet, Cariogenic”[Mesh]) OR “Dental Plaque”[Mesh]) OR “oral health behavior”) OR (“dental visit” OR “dental attendance” OR “dental attending”)) OR “Toothbrushing”[Mesh]) OR “Oral Hygiene”[Mesh]) OR ((tooth OR teeth OR enamel OR dentin) AND (cavity OR caries OR decay))) OR “Dental Caries”[Mesh])) AND “Sense of Coherence”[Mesh] |
| Embase |
| #1. ‘sense of coherence’ |
| #2. ‘sense of coherence’/exp OR ‘sense of coherence’ |
| #3. ‘dental visit’ OR ‘dental attendance’ OR ‘dental attending’ |
| #4. ‘oral health behavior’ |
| #5. (tooth OR teeth OR enamel OR dentin) AND (cavity OR caries OR decay) |
| #6. ‘oral health’ AND status |
| #7. ‘dental caries’ |
| #8. ‘dental plaque’ |
| #9. ‘tooth brushing’ OR ‘flossing’ |
| #10. ‘cariogenic diet’ OR ‘sugar intake’ |
| #11. #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 |
| #12. #1 AND #11 |
Selection of studies
Studies were selected firstly according to their title and abstract, following which the full texts of the relevant articles were retrieved. Details of each selected article encompassing the author's name, year of publication, country, study design, participants’ characteristics, primary and secondary outcomes, statistical analyses, and results were reported in evidence tables. The articles obtained were reviewed and critically appraised by two of the main reviewers (BT and RP) separately based on the Newcastle-Ottawa checklists for cross-sectional and cohort studies.[17] The risk of bias was evaluated by a relevant checklist.[18] In case of disagreement between the two reviewers (score difference more than 2 points), the third reviewer (AN) was referred for scoring. The Newcastle-Ottawa checklist consists of 7 items and a maximum of 10 scores for cross-sectional studies and 8 items and a maximum of 8 scores for cohort studies. A cut-off point of 5 was considered to determine the qualified studies.
Statistical analysis
All included studies were summarized descriptively and categorized based on the main outcome measured (number of decayed teeth, perceived oral health, and oral hygiene behavior) before carrying out statistical analyses with Comprehensive Meta-Analysis (CMA) version 3 software. P < 0.05 was considered to be statistically significant. Odds ratio (OR) was used to measure effect size with a 95% confidence interval (CI). Fixed or random-effects models were used to estimate pooled OR.[19] The random-effects model was chosen in the presence of heterogenicity. I2 index and Q index were used to measure the heterogeneity present between the studies. I2 is a ratio of variation among point estimates that is attributable to heterogeneity. Its values lie on a scale from 0 to 100 and based on the current guidelines, thresholds of 25% was considered for low, 50% for medium, and 75% for high heterogeneity.[20]
Results
Searching in the PubMed search engine yielded 21 relevant articles, of which 13 met the inclusion criteria, 5 were excluded due to different hypotheses, type of intervention, etc., and the rest were critically evaluated. One article was removed due to the appraisal score lower than 5. Out of 59 articles obtained from the search in the EMBASE database, 21 met the inclusion criteria, 9 of these articles were excluded due to different hypotheses, type of intervention, etc., and the rest were evaluated critically. One article was excluded based on a score under 5. The search in the SID (Persian database) with the keywords “sense” and “coherence” yielded 40 articles, of which one article met the inclusion criteria. However, it was finally excluded due to the low appraisal score. In the psychology database of ProQuest, 102 articles were found relevant and one was critically appraised and excluded because of low quality. Details of search results are summarized in the PRISMA flow diagram [Figure 1]. The scores given to the selected articles by two authors based on the Newcastle-Ottawa checklist are given in Table 2. Details of each selected article are presented in Table 3.
Figure 1.
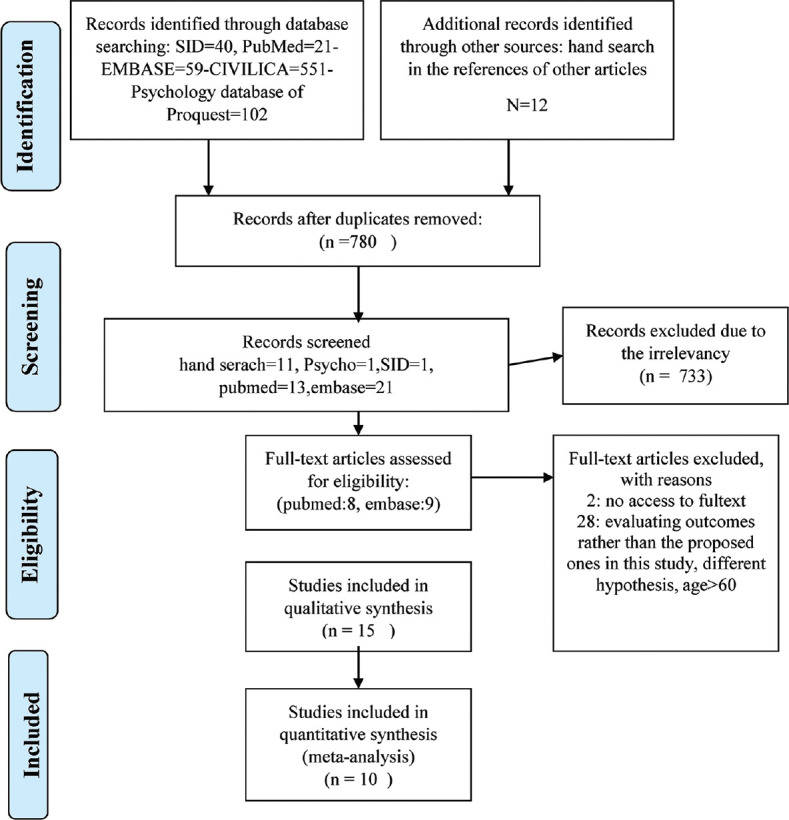
The PRISMA chart of searched articles
Table 2.
The results of critical appraising of studies by the two reviewers
| Author/years | Freire MCM 2001 | Bernabe´E 2010 | Kadriye Peker 2011 | Dorri M 2010 (pae) | Jarno J. Savolainen 2005 | Dorri M 2010 | ULRIKA LINDMARK2011 | Ayo-Yusuf OA 2009 | Bernabe´E 2009 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||||||||
| BT | RP | BT | RP | BT | RP | BT | RP | BT | RP | BT | RP | BT | RP | BT | RP | BT | RP | |
| Selection | ||||||||||||||||||
| 1) Representativeness of the sample | ||||||||||||||||||
| a) Truly representative of the average in the target population* (all subjects or random sampling) b) Somewhat representative of the average in the target population* (nonrandom sampling) c) Selected group of users d) No description of the sampling strategy |
a* | a* | a* | a* | c | c | a* | a* | a* | a* | a* | a* | a* | a* | a* | a* | a* | a* |
| 2) Sample size | ||||||||||||||||||
| a) Justified and satisfactory* b) Not justified |
a* | a* | b | b | b | b | a* | b | b | b | a* | b | a* | B | b | b | b | b |
| 3) Nonrespondents | ||||||||||||||||||
| a) Comparability between respondents and nonrespondents characteristics is established, and the response rate is satisfactory* b) The response rate is unsatisfactory, or the comparability between respondents and nonrespondents is unsatisfactory c) No description of the response rate or the characteristics of the responders and the non-responders |
a* | a* | a* | b | b | b | b | a* | b | b | b | a* | a* | a* | a* | a* | b | b |
| 4) Ascertainment of the exposure (risk factor) | ||||||||||||||||||
| a) Validated measurement tool** b) Nonvalidated measurement tool, but the tool is available or described* c) No description of the measurement tool |
a** | a** | a** | a** | a** | b* | a** | a** | a** | a ** | a** | a** | a** | a** | b* | b* | a** | a** |
| Comparability: Maximum 2 stars | ||||||||||||||||||
| 1) The subjects in different outcome groups are comparable, based on the study design or analysis. Confounding factors are controlled | ||||||||||||||||||
| a) The study controls for the most important factor (select one)** b) The study control for any additional factor* |
a** | a** | a** | a** | b* | b* | a** | a** | a** | a** | b* | a** | a** | a** | a** | a** | a** | a** |
| Outcome: Maximum 3 stars | ||||||||||||||||||
| 1) Assessment of the outcome | ||||||||||||||||||
| a) Independent blind assessment** b) Self-report* c) No description |
a** | a** | a** | a** | b* | b* | b* | b* | a** | a** | b* | b* | a** | a** | b* | b* | b* | b* |
| 2) Statistical test | ||||||||||||||||||
| a) The statistical test used to analyze the data is clearly described* b) The statistical test is not appropriate, not described or incomplete |
a* | a* | a* | a* | a* | a* | a* | a* | a* | a* | a* | a* | a* | a* | a* | a* | a* | a* |
| Scores | 10/10 | 10/10 | 9/10 | 8/10 | 5/10 | 4/10 | 8/10 | 8/10 | 8/10 | 8/10 | 7/10 | 8/10 | 10/10 | 9/10 | 7/10 | 7/10 | 7/10 | 7/10 |
| Risk of bias | - | - | Reject | Detection bias | Attrition bias | Detection bias | - | Detection bias | Detection bias, attrition bias | |||||||||
|
| ||||||||||||||||||
| Author/years | Deepak Viswanath 2015 | Lindmark U2011 | Renata Magalhães Cyrino2016 | Bernabe´E2011 | A. Wennstrom 2013 | CAROLINA FREITAS LAGE 2016 | A. Neiva da silva2016 | Bernabe´E2012 | ||||||||||
|
| ||||||||||||||||||
| BT | RP | BT | RP | BT | RP | BT | RP | BT | RP | BT | RP | BT | RP | BT | RP | |||
|
| ||||||||||||||||||
| Selection | ||||||||||||||||||
| 1) Representativeness of the sample | ||||||||||||||||||
| a) Truly representative of the average in the target population* (all subjects or random sampling) b) Somewhat representative of the average in the target population.* (non-random sampling) c) Selected group of users d) No description of the sampling strategy |
d | c | a* | a* | a* | a* | a* | a* | a* | a* | b* | a* | b* | b* | a* | a* | ||
| 2) Sample size | ||||||||||||||||||
| A) Justified and satisfactory* b) Not justified |
b | b | a* | a* | a* | a* | b* | b | b | b | a* | a* | a* | a* | a* | a* | ||
| 3) Non-respondents | ||||||||||||||||||
| A) Comparability between respondents and non-respondents characteristics is established, and the response rate is satisfactory* b) The response rate is unsatisfactory, or the comparability between respondents and non-respondents is unsatisfactory c) No description of the response rate or the characteristics of the responders and the nonresponders |
c | b | a* | a* | a* | a* | a* | b | b | a* | B | a* | c | c | a* | b | ||
| 4) Ascertainment of the exposure (risk factor) | ||||||||||||||||||
| A) Validated measurement tool** b) Non-validated measurement tool, but the tool is available or described* c) No description of the measurement tool |
b* | b* | a** | a** | a** | a** | a** | a** | a** | a** | b* | a ** | a** | a** | a** | a** | ||
| Comparability: Maximum 2 stars | ||||||||||||||||||
| 1) The subjects in different outcome groups are comparable, based on the study design or analysis. Confounding factors are controlled | ||||||||||||||||||
| a) The study controls for the most important factor (select one)** b) The study control for any additional factor* |
c | c | a** | a** | a* | a* | a** | a** | a** | a** | b* | b* | a** | a** | a** | a** | ||
| Outcome: Maximum 3 stars | ||||||||||||||||||
| 1) Assessment of the outcome | ||||||||||||||||||
| A) Independent blind assessment** b) Self report* c) No description |
a** | a** | b* | b* | a** | a** | a** | a** | b* | b* | a** | a** | a** | a** | a** | a** | ||
| 2) Statistical test | ||||||||||||||||||
| a) The statistical test used to analyze the data is clearly described* b) The statistical test is not appropriate, not described or incomplete |
a* | a* | a* | a* | a* | a* | a* | a* | a* | a* | a* | a* | a* | a* | a* | a* | ||
| Scores | 4/10 | 4/10 | 9/10 | 9/10 | 9/10 | 9/10 | 9/10 | 8/10 | 7/10 | 8/10 | 7/10 | 9/10 | 9/10 | 9/10 | 10/10 | 9/10 | ||
| Risk of bias | Reject | - | - | - | Detection bias | Selection bias | - | - | ||||||||||
BT=Bahareh tahani, RP=Roksana poursalehi
Table 3.
The evidence table of the included studies. Note-the coloured boxes are the studies that evaluate the effect of SOC as mediator
| Author Year | Country | Participants Age/sex/number | Scale of SOC | Primary outcome | Secondary outcome | Results | Conclusion |
|---|---|---|---|---|---|---|---|
| E. Bernabé1 2012 | Finland | 944 dentate adults (426 men and 518 women) Mean age: 48.6 years (SD: 11.9, range: 30-89) |
SOC-13 scale, 7-point (1=very often and 7=very seldom or never | DT, DT increment | - | Dependent: DT Baseline: Unadjusted (RR: 0.74 [0.6-0.91], P<0.01). After adjustment for age, sex (Model 1): RR: 0.72, 95% CI: 0.59-0.87, P<0.01 After adjustment for age, sex, education (Model 2): RR: 0.72, 95% CI: 0.59-0.87, P<0.01 After adjustment for age, sex, education, oral health behavior (Model 3): 0.81 (0.68-0.97) P<0.05 |
The number of decayed teeth decreased by 28% for every unit increase in SOC |
| E. Bernabé1 2012 | Finland | 944 dentate adults (426 men and 518 women) mean age: 48.6 years (SD: 11.9, range: 30-89) | SOC-13 scale, 7-point (1=very often and 7=very seldom or never) | DT, DT increment | - | After 4 years Dependent: DT unadjusted (RR: 0.81 [0.65-1.01], NS). After adjustment for age, sex (Model 1), (RR: 0.78, 95% CI: 0.63-0.97, P<0.05) After adjustment for age, sex, education (Model 2): (RR: 0.79, 95% CI: 0.63-0.98, P<0.05) After adjustment for age, sex, education, oral health behavior (Model 3): (0.81 [0.64-1.02] NS) |
SOC was a predictor of 4-year incidence of tooth decay, irrespective of subjects’ sociodemographic background. Each higher point in the SOC score was associated with around 20% decrease in the risk of having tooth decay |
| Renata Magalh~aes Cyrino 2016 | Brazil | 202 Brazilian males and 74 females mean age: 37.36±12.05 years | SOC-13 (5-point Likert scale) sum from 13 to 65, (weak=24-46), moderate (47-51), strong (52-65) | PI, perceived oral health | - | Logistic reg: Dependent: General perceived oral health Weak SOC OR (4.63; 95% CI: 1.59-3.51, P=0.005) Moderate SOC OR (1.31; 95% CI: 0.34-5.04, P=NS) Strong SOC reference, P=0.001 |
Weak SOC was significantly associated with poor perceived general oral health, But not associated with Clinical periodontal health outcomes such as PI |
| Bernabe´E2011 | Finland | 5401 dentate adults (2538 men and 2863 women) mean age=49.6 years (SD: 12.8, range: 30-99 | SOC-13 scale | Role of adult SOC as a mediator of the relationship between childhood SEP (parental education), and tooth retention | Adult oral health behavior | Childhood SEP with tooth retention directly: (standardized path: 0.06, P: <0.001) indirectly via adulthood SEP: (0.07, P: <0.001), via adulthood SEP and oral health-related behaviors (0.10, P<0.001), and via SOC and oral health-related behaviors (0.01, P=0.001). indirect effects via SOC (−0.002, P=0.081) and via oral health-related behaviors (−0.004, P=0.692) SOC with oral health-related behavior: (0.18, P<0.0001) SOC with tooth retention only indirectly via oral health-related behaviors (0.06, P: <0.001) |
SOC is associated only indirectly with tooth retention through oral health-related behaviours, but may contribute little to the relationship between childhood SEP and tooth retention in adult life. These findings were consistent across sexes and age groups |
| Lindmark U2011 | Sweden | 525 individuals, 261 men and 264 women, aged 20-80 years | SOC-13 levels of SOC (low<66, intermediate: 67-75, high: >76) | . | Oral health-related behaviour | Sweat drinks SOC low (ref) SOC intermediate (OR=1.25; 95% CI: 0.62-2.54, P=NS) SOC high (OR=0.88; 95% CI: 0.42-1.8, P=NS) Frequency of snacks between meals SOC low (ref) SOC intermediate (OR=2; 95% CI: 1.17-3.43, P=0.011) SOC high (OR=1.9 95% CI: 1.1-3.29, P=0.021) Tooth brushing Frequency SOC low (ref) SOC intermediate (OR=2.62 95% CI: 1.01-6.82, P=0.048) SOC high (OR=1.24 95% CI: 0.55-2.82, P=NS) |
Subjects with High SOC 1.90 times more chance of having fewer snacks and drinks between meals and 2.62 times more chance of being included in the group who brushed their teeth twice a day or more, compared with individuals with lower SOC scores |
| A. WENNSTRÖM2013 | Sweden | Women in Gothenburg, aged 38 and 50 years, from the survey in 2004 to 2005 n=493 | SOC-13 | Oral health status (number of teeth, self-reported oral health) | - | Regressions Model I: Number of teeth as dependent (0-25/26-32) and SOC, education, marriage independent: Odds of SOC: 1.02 (1.00-1.04, P=0.018) Model 2: Self-rated oral health (poor/good) as dependent and SOC, education, marriage independent: Odds of SOC: 1.03 (1.01-1.05, P=0.001) |
An increase by 10 SOC points predicts a 20% and 30% greater likelihood of having more teeth and better perceived oral health, respectively |
| CAROLINA FREITAS LAGE 2016 | South eastern Brazil | 1195 adolescents and their mothers The female gender: 55.9% mean age: 13.84 years (SD: 0.717 years) | SOC-13, 5-likert SOC>46 SOC≤46 |
Dental caries experience | - | Dependent: Dental caries Unadjusted bivariate adolescent’s SOC (≤46 as reference,>46 OR: 0.38 (0.32-0.46, P<0.001) Multivariate model: Adjusted for age, economic status SOC>46 versus≤46: OR 0.46 (0.39-0.55, P<0.001) |
SOC is associated with dental caries in adolescents; adolescents with high frequency of dental caries had a lower SOC |
| Neiva da Silva2016 | Brazil | 190 women age 26-63 years (mean 37.5, SD 7.2) | SOC-13 | Dental caries | Tooth brushing frequency, dental floss use | SOC scores with number of decayed teeth (ρ=−0.003, P>0.05) | SOC moderates the relationshipbetween untreated dental caries and dental pain |
| Freire MCM 2001 | middle west Brazil | 664 adolescent 15 years | SOC-13 | DMFS, plaque index, and dental caries | Pattern of dental attendance, Daily frequency of sugar intake, Daily between meals frequency of sugar intake, daily tooth brushing frequency | Simple regression DMFS (OR=0.98; CI: 0.87-1.15, NS; P=0.795) Plaque index (OR=0.98; CI: 0.8-1.19, NS, P=0.810) Cries experience anterior teeth (OR=0.81 scale; 95% CI=0.66-0.98, P: 0.029). Pattern of dental attendance (OR=0.83; CI: 0.71-0.98, P=0.020) Sugar intake (OR=0.89; CI: 0.67-1.19, NS P=0.425) |
Adolescents with higher SOC were less likely to have caries experience in anterior teeth than those with lower SOC scores (after adjusting for all important variables, caries experience in anterior teeth was not associated with SOC) |
| Between meals frequency of sugar intake (OR=0.86 CI: 0.71-1.02, NS P=0.074) Tooth brushing frequency (OR=0.91 CI: 0.76-1.09, NS P: 0.304 Multiple regression Dependent (caries experience in anterior teeth) when adjusted just for social class (OR=0.81; 0.66-0.99, P=0.03), adjusted for all variable (above+dental attendance, sport, mothers dental health, mothers education) OR=0.88 (CI: 0.7-1.09, NS, P=0.22) Dependent (pattern of dental attendance) when adjusted just for social class (OR=0.84, CI: 0.84-1.04, P=0.02), adjusted for above+mothers education): OR=0.85 (CI 0.73-1, NS, P=0.04) |
In the final model, adolescents with higher SOC scores had less probability of attending the dentist when in trouble and were therefore more likely to attend for check-ups than those with lower SOC scores | ||||||
| Bernabe´E2010 | Finland | 5401 dentate adults (2538 men and 2863 women) mean age: 49.6 years (range: 30-99 years) | Slightly abbreviated version of the Finnish SOC-13 scale | Dental plaque and decayed teeth, perceived oral health | - | Linear reg Dependant (number of teeth) when adjusted just for age, sex, marriage and urbanization SOC was significant estimate=0.68, 95% CI: 0.44-0.92, P<0.001 when adjusted just for above and education and income SOC was significant estimate=0.46; 95% CI: 0.23-0.68, P<0.001 when adjusted just for above and oral health behavior SOC was significant estimate=0.29; 95% CI: 0.08-0.51, P=0.007 Dependant (number of decayed teeth) when adjusted just for age, sex, marriage and urbanization SOC was significant estimate=−0.22; 95% CI: −0.3-−0.14, P<0.001 when adjusted just for above and education and income SOC was significant estimate=−0.19; 95% CI: −0.27-−0.11, P<0.001 when adjusted just for above and oral health behavior SOC was significant estimate=−0.13 95% CI: −0.2-−0.06, P<0.001 Logistic reg: Dependant (poor perceived oral health) when adjusted just for age, sex, marriage and urbanization SOC was significant estimate=0.73; 95% CI: 0.67-0.79, P<0.001 when adjusted just for above and education and income SOC was significant estimate=0.76; 95% CI: 0.7-0.83, P<0.001 when adjusted just for above and oral health behavior SOC was significant estimate=0.8; 95% CI: 0.73-0.87, P<0.001 |
SOC was positively associated with various aspects of adult oral health such that adults with a strong SOC had more teeth, fewer decayed teeth, less periodontal pockets and better perceived oral health |
| Mojtaba Dorri 2010 | Iran | 1054 grade 6 Iranian student age 11-16 mean age: 12.4 (SD=0.7) | SOC-13 | - | Frequency of toothbrushing behaviours | Dependent: Frequencies of tooth brushing Univaraite: OR 1.022; 95% CI: 1.001-1.031 (P=0.01) Multivariate: OR 1.021; 95% CI: 1.001-1.032 (P=0.01) adjusted for sex, fathers education |
This study highlights the importance of SOC as a factor influencing toothbrushing behaviours in adolescents |
| Mojtaba Dorri 2010 (paediatric) | Iran | 1132 sixth grade students average age: 12.4 (SD=0.8) | SOC-13 | - | Oral hygiene behaviors | Structural SOC and peer social networks were positively associated with oral hygiene behaviors. B: 0.144, P<0.01 and B: 0.175, P<0.01 |
Sociodemographic factors, sex and education influence hygiene behaviours in adolescents through their impact on sense of coherence and peer social networks |
| ULRIKA LINDMARK2011 | Sweden | 525 individuals, 261 men and 264 women, aged 20, 30, 40, 50, 60, 70 and 80 years | SOC-13, low<66, intermediate 67-75, high>76 | Oral health status | - | Model I linear Reg: Unadjusted, dependent Frequency of DFS (r2=0.026, B=0.167, P<0.000), DS (r2=0.020, B=−0.14, P=0.008), FS (r2=0.010, B=0.177, P=0.053) and teeth with calculus (r2=0.008, B=−0.1 P=0.00). Number of teeth (r2=0.001, B=−0.027, P=NS) After adjusting for age, gender, marital ststus, income, education, occupation level (Model II), dependent Frequency of DFS (r2=0.584, B=0.013 P=NS), DS (r2=0.135, B=−0.051, P=NS), FS (r2=0.608, B=−0.038, P=NS) and teeth with calculus (r2=0.012, B=−0.089, P=NS). number of teeth (r2=0.42, B=-0.015, P=NS) logistic Regression adjusting for age, gender, marital status, income, education, occupation level DFS low (one third low/one third high) intermediate SOC: OR: 053; 95% CI; 0.13-2.22 P=NS, high SOC: OR: 0.85 (95% CI: 0.24-2.97 P=NS), DS(<6/>6 sites) (intermediate SOC: OR: 1.61 (95% CI: 0.71-3.61 P=NS, High SOC : OR: 1.6 (95% CI: 0.65-3.92, P=NS), FS (one third low/one third high) (intermediate SOC: OR : 0.52 (95% CI: 0.09-2.98, P=NS, High SOC: OR: 0.77 (95% CI: 0.16-3.82 P=NS) and teeth with Calculus (<20%/>20%) (intermediate SOC: OR: 0.79; 95% CI 0.45-1.39 P=NS, High SOC: OR: 0.72; 95% CI: 0.4-1.27 P=NS) Number of teeth (>20/<20) (intermediate SOC: OR: 1.02; 95% CI: 0.42-2.5, P=NS, high SOC: OR: 0.67; 95% CI: 0.27-1.66 P=NS) PLI (<20%/>20%) (intermediate SOC: OR: 0.67; 95% CI: 0.4-1.12 P=NS, high SOC: OR: 0.58; 95% CI: 0.34-0.98 P=04) |
Higher mean SOC scores were statistically significantly associated with more decayed and filled tooth surfaces and filled tooth surfaces, fewer decayed tooth surfaces, fewer teeth with calculus and periodontal health |
| Ayo-Yusuf OA-2009 | Limpopo Province, South Africa | Between 12 and 19 years old, mean (SD) age: 14.4 (SD 1.5) years (n=1025) | SOC-13 At baseline and 18 months later |
- | Tooth-brushing frequency, dental attendance, change brushing behaviour | Logistic reg: Dependent: Frequent brushing Model 2 Adjusted for smoking (NS)/depression/live with mother: SOC development OR: 1.02 (CI: 1.01-1.04, P<0.05) SOC baseline OR 1.03 (0.99-1.06, P=NS) Model 3 adjusted for above plus dental visit and reason for brushing: SOC development OR: 1.03 (CI: 1.01-1.05, P<0.05) SOC baseline OR 1.03 (CI: 1-1.06, P<0.05) Model 4 adjusted for above plus stage of change: SOC development OR: 1.03 (CI: 1.01-1.05, P<0.05) SOC baseline OR 1.02 (CI: 0.99-1.06, P=NS) |
Children’s psychological predispositions (SOC, depression) and family environment (living with mother) might significantly influence their tooth-brushing behaviour, and subsequently their oral health (in model 2, 3, 4 beside other factors. SOC was significantly effective with almost the same OR) |
| Jarno J. Savolainen-2005 | Finland | 4131 30-64-year-old individuals (1928 males and 2203 females) | SOC-13 SOC2=low=58.8-64.8) SOC5=high=74.2-84 |
Oral hygiene: PLI | Tooth brushing frequency | Logistic reg: (1) Independent: SOC Dependent: Tooth brushing frequency Model A (unadjusted): SOC2, OR: 1.3 (95% CI: 101-107) SOC5, OR 2.2 (1.7-207) Model B (adjusted for gender, age, education, marital status, smoking, number of teeth): SOC2, OR 1.3 (1-1.6) SOC5, OR 1.9 (1.5-2.5) (2) Independent: SOC Dependant: Level of oral hygiene Model A: SOC2: OR 1.5 (1.2-1.9) SOC5: OR 1.9 (1.6-2.4) >Model B (adjusted for gender, age, education, marital status, smoking, number of teeth): SOC2: OR 1.4 (1.2-1.8) SOC5: OR 1.7 (1.4-2.1) |
A weak sense of coherence increases both the probability of having a poorer level of oral hygiene and a tooth brushing frequency of less than once a day. A strong sense of coherence seems to associate with both higher frequency and quality of toothbrushing |
| Bernabe´2009 | Finland | 8028 subjects, 30 years of age and over | Abbreviated version of the Finnish SOC-13 scale | - | Pattern of dental attendance, tooth brushing frequency, sugar intake frequency, their intake frequency of six di?erent sweets and snacks | Logistic reg: Dependent: Dental attendance adjusted for income and education: OR 1.2 (95% CI: 1.11-1.28, P<0.001) Dependent: Tooth brushing frequency adjusted for income and education: OR 1.22 (95% CI: 1.12-1.32, P<0.001) Dependent: Sugar intake frequency adjusted for income and education: OR 0.9 (95% CI: 0.83-0.97, P=0.006) |
SOC was positively associated with visiting a dentist regularly for check-ups and brushing teeth twice or more often a day as well as being negatively associated with daily smoking and sugar-intake frequency |
SD=Standard deviation, SOC=Sense of coherence, PI=Plaque Index, SEP=socioeconomic position, DMFS=Decayed- Missed-Filled surfaces , PLI=Plaque Index
Of the 15 articles that received the minimum score of criticism, 10, 3, and 2 were conducted among adults aged over 20-year-old, adolescents aged 15–19, and children, respectively. Six articles received score 9 or higher and two articles got score 7 [Table 2]. Ten articles investigated primary outcomes, including dental caries, plaque index, and oral health index. Nine articles (in some articles both outcomes were measured) studied OHBs, including visiting a dentist, using a toothbrush and dental floss, and consuming sugars. The clinical results of the articles were categorized based on the age group of their participants and the assessed outcomes, which are presented in the following sections.
Adult age group articles
Sense of coherence and dental caries
The study of Bernabé et al. on an adult population with a mean age of 48.6 ± 11.9 in Finland revealed that in the multivariate regression model, SOC along with other factors such as age, sex, education level, and OHBs were factors affecting the number of decayed teeth; each increase in SOC caused 28% decrease in the number of decayed teeth. Further, the same study showed similar results after 4 years of follow-up, with 20% drop in caries rate as a result of the increase in SOC.[21] The study of Bernabé et al. on a Finnish population aged 30–99 years, with a mean age of 49.6 years, showed that SOC was significantly associated with oral health. Accordingly, individuals with higher SOC (adjusted for factors such as education, income, marriage, gender, and age) had fewer decayed teeth.[22] The research by Lindmark et al. on a Swedish adult population aged 20–80 years showed that individuals with higher SOC, after adjustment for age, sex, marital status, income, education, and occupation, had a higher number of filled teeth, a lower number of decayed teeth, and a lower rate of dental calculus.[12]
Sense of coherence and plaque index
The study of Cyrino et al. on Brazilian adults (mean age: 37.36 ± 12.05) showed no relationship between SOC and plaque index with respect to low, medium, and strong SOC.[23] Savolainen et al. (2005) concluded that adults aged 30–64 years old in Finland (considering scores under 64 as weak and over 74 as strong SOC), adjusted for age, sex, education, marital status, smoking, and tooth number, reported that weak SOC could significantly increase the likelihood of poorer oral health, as measured by the plaque index.[3]
Sense of coherence and oral health behaviors
The study of Lindmark et al. on a Swedish adult population of 20–80–year–old with low, medium, and high SOC showed a significant association between SOC and reduced snack consumption and toothbrush behavior. People with high SOC were 1.4 times more likely to have a lower snack consumption and two times more likely to brush twice daily than those with low SOC.[24] Savolainen et al. concluded that poor SOC could significantly cause irregular brushing behavior.[4] The research of Bernabé et al. on adults aged ≥30 years in Finland indicated that, after adjustment for education and income, SOC was significantly and positively associated with regular dental visits and brushing twice daily. Moreover, there was a negative relationship between SOC and consumption of sugars.[25]
Sense of coherence and other oral health indicators
A study by Cyrino et al. in Brazilian adults showed a relationship between poor SOC and poor perceived oral health.[23] Wennstrom et al. (2013) conducted a study in a Swedish 38–50-year-old population and concluded that, along with factors such as education and marriage, an increase of 10 points in SOC could lead to 20% and 30% increase in the number of remaining teeth and perceived oral health status, respectively.[26] Bernabé et al. showed that individuals with higher SOC (adjusted for factors such as education, age, marital status, gender, and age) had better perceived oral health.[22]
Adolescent age group articles
Sense of coherence and dental caries
Lage et al. (2017) carried out a study among a group of Brazilian adolescents with a mean age of 13.8 ± 0.7. Considering the cut-off point of 46, they found high SOC was significantly (along with factors such as age and economic status) correlated with the experience of tooth decay; adolescents with lower SOC had a higher number of decayed teeth.[27]
Freire et al. performed a study on a 15-year-old Brazilian adolescent population and showed that adolescents with higher SOC were less likely to develop dental caries in the anterior teeth. After adjusting the results for social class, the same results were obtained. However, this relationship was not significant after adjustment for additional factors such as maternal education, maternal oral health, physical exercise, and dental referral.[9]
Sense of coherence and plaque index
The study of Freire et al. showed no significant association between SOC and plaque index.[9]
Sense of coherence and oral health behaviors
The research by Freire et al. showed no significant relationship between SOC and tooth brushing and sweet snack consumption.[9] In the same study, adolescents with a higher SOC were more likely to visit a dentist for regular examinations even after adjusting for other factors.[9] Ayo-Yusuf et al. performed a study on 12-year-old adolescents (mean age: 14.4 ± 1.5) and found that SOC with factors such as depression, living with mother, smoking, referring to a dentist, and stage of change influenced their brushing behavior after 18 months of follow-up.[28]
Children age group articles
Sense of coherence and oral health behaviors
The study of Dorri et al. on Iranian children aged 11–16 years (mean age: 12.4 years) indicated that SOC, after adjustment for gender and paternal education, was significantly associated with the brushing behavior; the higher the SOC, the higher the frequency of tooth brushing.[29]
Sense of coherence as a mediator among other variables
In three studies, the role of SOC as a mediator over other factors was measured. A study by Bernabé et al. among adults with a mean age of 49.6 ± 12.8 years showed that SOC could affect the number of the remaining teeth after adjusting for gender and age. However, it had a mediating effect on the OHBs.[30] In a study by Vettore MV et al.(2016) among Brazilian adults aged 26–63 years (mean age: 37.5 ± 7.2), it was found that SOC could be a mediator of the association between untreated decayed teeth and dental pain.[31] In a study on children, Dorri et al. found that social factors, gender, and education could influence the children's OHBs through SOC.[32]
Meta-analysis of the data
Considering the inclusion criteria of at least 3 studies per subdivision (by type of outcome and age group) and accuracy of studies using CMA3 software, the number of decayed teeth in adults, perceived oral health, and oral hygiene behavior (brushing) were eligible for meta-analysis.
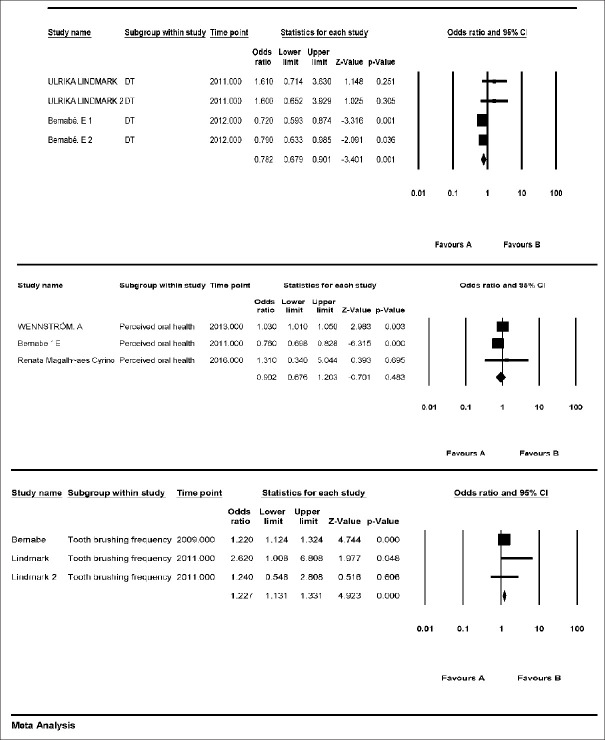
Dental caries in adults
Only 4 studies, which were almost homogenous using homogeneity analysis (Q = 6.7, P = 0.1, I2 = 51%), were eligible for inclusion. Therefore, the Fixed model revealed SOC was significantly associated with the caries rate (OR = 0.78, CI 95% = 0.9–0.67, P = 0.001) [Figure 2].
Figure 2.
The meta-analysis of data: Dental caries, perceived oral health and tooth brushing frequency in adults as the outcome
Perceived oral health in adults
Only 3 studies were eligible for analysis. Homogeneity analysis (Q-value = 46.6, P < 0.001, I2 = 95%) showed that studies were not homogeneous. Thus, random effects model was applied, which indicated no significant relationship between overall SOC and this outcome (OR = 0.9, CI 95% = 1.2–0.67, P = 0.4) [Figure 2].
Tooth brushing frequency
Only 3 studies were eligible for inclusion. Homogeneity analysis showed that studies were homogeneous (Q-value = 2.4, P = 0.2, I2 = 18%). Therefore, using the fixed effects model, the tooth brushing frequency was significantly influenced by SOC (OR = 1.22, CI 95%. = 1.1-1.31 and P < 0.001). Lindmark's study compared a group of participants with high and moderate SOC with another group of participants with low SOC. According to the results of his study, only moderate SOC affected the frequency of tooth brushing [Figure 2].
Discussion
Health is defined as continuous repetition of comfort and illness. Salutogenic theory, a health-related theory, indicates the relationship between stress, health, and dealing with stress.[33] It also emphasizes the higher impact of psychological factors on the continuity and maintenance of human health rather than pathological factors.[16] A central component of this theory is the SOC, which is defined as the ability to understand the general conditions and the capacity to use the existing resources to deal with stressful situations and promote health.[16,33] This capacity is defined as the ability of people to evaluate and understand their situation, to motivate them to move towards health promotion, and to have the resources needed for these actions, which are defined as comprehensibility, meaningfulness, and manageability, respectively.[2]
Various factors reported in many studies affect the SOC. Research has shown that gender does not have a significant effect on SOC but, social support, education, working conditions, and living conditions in childhood can influence SOC. Age has also been suggested to be an influential factor; an increase in SOC has been observed with a rise in age.[34]
SOC affects health promotion in three ways; through regulation of the emotions in the face of stressors, through the choice of health-promoting behaviors, and through the direct physiological impact of the central nervous-immune pathway and the endocrine system.[22] Research in the medical field has shown that SOC is related to the emotional status and health biomarkers. Yet, further research is needed to confirm the influence of each of these factors on oral health and well-being.[22]
Oral health is an important part of general health. To promote oral health, it is essential to establish effective OHBs and have adequate knowledge.[35] Oral health status is clearly related to the OHBs. Studies have shown that people who have better oral hygiene behaviors such as brushing and flossing exhibit better oral health status, including plaque index, etc.[35] In a study conducted on Iranian children, it was found that oral hygiene behaviors, including tooth brushing and regular dental visiting, were significantly positively correlated with the children's oral health status; the higher the frequency of tooth brushing and dental visits, the better the oral health status.[36] A study on Asian students also found a significant relationship between poor oral health status and poor oral hygiene behavior so that social factors, lack of belief and knowledge about the importance of brushing might cause this weakness.[37]
In the current systematic review, a significant relationship was observed between SOC and caries and plaque indexes. This relationship might be due to the influence of SOC on OHBs and consequently on oral health status. Overall, it appears that SOC could have affected tooth decay, plaque index, and oral hygiene behaviors such as tooth brushing, sweet snack consumption, and regular dental visits in adults independent of the underlying factors. In adolescents, this association was significant for tooth decay; however, it faded away after adjusting for the underlying factors. In one study, there was a significantly positive correlation between SOC and tooth brushing. The total number of articles in adolescence is limited. In children, only one article was found to show an association between SOC and OHBs. The results of the meta-analysis also showed a significant relationship between adults’ SOC and dental caries.
The impact of SOC on OHBs has also been investigated in various studies, both by the reports of individuals studied and by clinical examinations. A systematic review by Elyasi et al. found a significant association between SOC and OHBs in adults so that the higher the SOC, the higher the tooth brushing frequency and dental visiting and the fewer the sugar intake. This association has been less frequently observed in adolescents, which may be attributed to the role of parents in these behaviors.[14] The above study recruited articles conducted in 2015 and no primary outcomes, including decay and number of teeth, were included. Ayo-Yusuf et al. measured the SOC of adolescents identifying the stage of change of twice-daily tooth brushing. After 18 months, the individuals who successfully acquired this behavior were those who had higher SOC at baseline.[28] In the meta-analysis section of the present study, the SOC in adults was significantly associated with their frequency of tooth brushing. It was not possible to perform a meta-analysis in adolescents due to the scarcity of studies.
However, a critical evaluation shows the relationship between SOC and the frequency of tooth brushing can be influenced by other factors. For example, people with higher SOC may report their OHBs unrealistically; hence, a stronger relationship is reported.[4] People with higher SOC are more optimistic and have greater confidence and ability to control and perform tooth brushing, so this may also be a factor involved in the association between SOC and tooth brushing frequency.[31] Clinical examinations including observation of tooth brushing practice in people or recording their plaque index instead of self-reported behaviors might be helpful to overcome this bias.
Furthermore, the present study indicated no correlation between perceived oral health and SOC. In the meta-analysis in adults the heterogeneity of studies was also very high that might be partly due to the different methods or indices to measure perceived status. However, his result was also seen in other studies examining the relationship between perceived oral health and clinical measures, including dental caries. In the study mentioned, there was only a relationship between perceived oral health and the number of un-replaced teeth in adults.[38,39] This may be due to the underlying problems caused by edentulousness, including inelegant appearance, chewing problems, and the need for dentures.[38]
There have been a lot of efforts to promote health behaviors but, currently, they are mostly in accordance with behavior (change) models such as the Theory of Planned Behavior or the Health Belief Model[40,41] In these models, the main focus is on the beliefs, social norms, self-efficacy to perform the behavior, perceived risk, and benefits that, according to the salutogenic model, are resources that exist within the individual and can not necessarily result in behavior change.[42]
Antonovsky considered SOC to be formed in young ages and stabilizes around the age of 30, forming a personality character that influences the way in which people see the world, use the required resources to respond to demands, and feel that these responses are meaningful and make sense emotionally.[16] The biological, material, and psychosocial resources used to respond to stimuli are called “General Resistance Resources” (GRRs) that are within an individual (e.g. attitudes, self-efficacy beliefs, knowledge) or in their environment (e.g., social support, cultural stability)[43] To enable people to identify and use their resources to move to healthier status, through empowerment and reflection, they should perceive the situation comprehensible and manageable. Therefore, health professionals interested in oral health promotion, moreover than attempting to promote the knowledge and beliefs of their patients, need to concentrate on empowering people to identify and mobilize appropriate GRRs to solve stressful situations and reflect on the resources they already have available.[44,45]
Limitations
The number of articles available for children and adolescents was insufficient, so more high-quality research is recommended to be conducted on these critical age groups.
Conclusion
SOC seems to be an important factor involved in predicting oral hygiene behaviors and ultimately oral health status, especially in adults. Oral Health professionals who concern about promotion should concentrate on empowering people to identify and mobilize appropriate resistance resources to solve stressful situations and reflect on the resources they already have available.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
we would like to thank the vice chancellery of research at Isfahan University of Medical Sciences for their support. The current study is based on the results of a thesis conducted at Isfahan University of Medical Sciences with the code of ethics of IR. MUI. RESEARCH. REC.1398.070.
References
- 1.Chu JJ, Khan MH, Jahn HJ, Kraemer A. Sense of coherence and associated factors among university students in China: Cross-sectional evidence. BMC Public Health. 2016;16:336. doi: 10.1186/s12889-016-3003-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Eriksson M, Lindström B. Antonovsky's sense of coherence scale and the relation with health: A systematic review. J Epidemiol Community Health. 2006;60:376–81. doi: 10.1136/jech.2005.041616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Savolainen JJ, Suominen-Taipale AL, Uutela AK, Martelin TP, Niskanen MC, Knuuttila ML. Sense of coherence as a determinant of toothbrushing frequency and level of oral hygiene. J Periodont. 2005;76:1006–12. doi: 10.1902/jop.2005.76.6.1006. [DOI] [PubMed] [Google Scholar]
- 4.Mohamamdirizi S, Mohamadirizi M, Mohamadirizi S. The comparison of fear of childbirth and sense of coherence among low-risk and high-risk pregnancy women. J Educ Health Promot. 2018;7:143. doi: 10.4103/jehp.jehp_179_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wiseman J, McLeod J, Zubrick SR. Promoting mental health and well-being: Integrating individual, organisational and community-level indicators. Health Promot J Austr. 2007;18:198–207. doi: 10.1071/he07198. [DOI] [PubMed] [Google Scholar]
- 6.Patrick DL, Lee RS, Nucci M, Grembowski D, Jolles CZ, Milgrom P. Reducing oral health disparities: A focus on social and cultural determinants. BMC Oral Health. 2006;6(Suppl 1):S4. doi: 10.1186/1472-6831-6-S1-S4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lundman B, Norberg A. The significance of a sense of coherence for subjective health in persons with insulin dependent diabetes. J Adv Nurs. 1993;18:381–6. doi: 10.1046/j.1365-2648.1993.18030381.x. [DOI] [PubMed] [Google Scholar]
- 8.Wainwright NW, Surtees PG, Welch AA, Luben RN, Khaw KT, Bingham SA. Healthy lifestyle choices: Could sense of coherence aid health promotion? J Epidemiol Community Health. 2007;61:871–6. doi: 10.1136/jech.2006.056275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Freire M, Sheiham A, Hardy R. Adolescents’ sense of coherence, oral health status, and oral health-related behaviours. Community Dent Oral Epidemiol. 2001;29:204–12. doi: 10.1034/j.1600-0528.2001.290306.x. [DOI] [PubMed] [Google Scholar]
- 10.Hall-Scullin E, Goldthorpe J, Milsom K, Tickle M. A qualitative study of the views of adolescents on their caries risk and prevention behaviors. BMC Oral Health. 2015;15:141. doi: 10.1186/s12903-015-0128-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nammontri O, Robinson P, Baker S. Enhancing oral health via sense of coherence: A cluster-randomized trial. J Dent Res. 2013;92:26–31. doi: 10.1177/0022034512459757. [DOI] [PubMed] [Google Scholar]
- 12.Lindmark U, Hakeberg M, Hugoson A. Sense of coherence and oral health status in an adult Swedish population. Acta Odontol Scand. 2011;69:12–20. doi: 10.3109/00016357.2010.517553. [DOI] [PubMed] [Google Scholar]
- 13.Lindmark U, Stegmayr B, Nilsson B, Lindahl B, Johansson I. Food selection associated with sense of coherence in adults. Nutr J. 2005;4:9. doi: 10.1186/1475-2891-4-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Elyasi M, Abreu LG, Badri P, Saltaji H, Flores-Mir C, Amin M. Impact of sense of coherence on oral health behaviors: A systematic review? PLoS One. 2015;10:e0133918. doi: 10.1371/journal.pone.0133918. doi: 10.1371/journal.pone. 0133918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Savolainen J, Suominen-Taipale A, Uutela A, Aromaa A, Härkänen T, Knuuttila M. Sense of coherence associates with oral and general health behaviours. Community Dent Health. 2009;26:197–203. [PubMed] [Google Scholar]
- 16.Antonovsky A. The structure and properties of the sense of coherence scale. Soc Sci Med. 1993;36:725–33. doi: 10.1016/0277-9536(93)90033-z. [DOI] [PubMed] [Google Scholar]
- 17.Wells GA, Shea B, O'Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Score for Non-Randomized Studies. 2013. [Accessed June 2019]. Available at: http://www.ohri.ca .
- 18.Viswanathan M, Ansari MT, Berkman ND, Chang S, Hartling L, McPheeters LM, et al. Assessing the Risk of Bias of Individual Studies in Systematic Reviews of Health Care Interventions. Agency for Healthcare Research and Quality Methods Guide for Comparative Effectiveness Reviews. AHRQ Publication No. 12-EHC047-EF. 2012. [Last accessed on 2019 Jun]. Available from: http//www.effectivehealthcare.ahrq.gov/ [PubMed]
- 19.Zhang J, Yu KF. What's the relative risk? A method of correcting the odds ratio in cohort studies of common outcomes. JAMA. 1998;280:1690–91. doi: 10.1001/jama.280.19.1690. [DOI] [PubMed] [Google Scholar]
- 20.Dersimonian R, Laird N. Meta-analysis in clinical trailas. Contemp Clin Trials. 2015;45:139–45. doi: 10.1016/j.cct.2015.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bernabé E, Newton JT, Uutela A, Aromaa A, Suominen AL. Sense of coherence and four-year caries incidence in Finnish adults. Caries Res. 2012;46:523–9. doi: 10.1159/000341219. [DOI] [PubMed] [Google Scholar]
- 22.Bernabé E, Watt RG, Sheiham A, Suominen-Taipale AL, Uutela A, Vehkalahti MM, et al. Sense of coherence and oral health in dentate adults: Findings from the Finnish health 2000 survey. J Clin Periodontol. 2010;37:981–7. doi: 10.1111/j.1600-051X.2010.01604.x. [DOI] [PubMed] [Google Scholar]
- 23.Cyrino RM, Costa FO, Cortelli JR, Cortelli SC, Cota LO. Sense of coherence and periodontal health outcomes. Acta Odontol Scand. 2016;74:368–73. doi: 10.3109/00016357.2016.1154601. [DOI] [PubMed] [Google Scholar]
- 24.Lindmark U, Hakeberg M, Hugoson A. Sense of coherence and its relationship with oral health-related behaviour and knowledge of and attitudes towards oral health. Community Dent Oral Epidemiol. 2011;39:542–53. doi: 10.1111/j.1600-0528.2011.00627.x. [DOI] [PubMed] [Google Scholar]
- 25.Bernabé E, Kivimäki M, Tsakos G, Suominen-Taipale AL, Nordblad A, Savolainen J, et al. The relationship among sense of coherence, socio-economic status, and oral health-related behaviours among Finnish dentate adults. Eur J Oral Sci. 2009;117:413–8. doi: 10.1111/j.1600-0722.2009.00655.x. [DOI] [PubMed] [Google Scholar]
- 26.Wennström A, Wide Boman U, Stenman U, Ahlqwist M, Hakeberg M. Oral health, sense of coherence and dental anxiety among middle-aged women. Acta Odontol Scand. 2013;71:256–62. doi: 10.3109/00016357.2012.671362. [DOI] [PubMed] [Google Scholar]
- 27.Lage CF, Fulgencio LB, Corrêa-Faria P, Serra-Negra JM, Paiva SM, Pordeus IA. Association between dental caries experience and sense of coherence among adolescents and mothers. Int J Paediatr Dent. 2017;27:412–9. doi: 10.1111/ipd.12275. [DOI] [PubMed] [Google Scholar]
- 28.Ayo-Yusuf OA, Reddy PS, Van Den Borne BW. Longitudinal association of adolescents’ sense of coherence with tooth-brushing using an integrated behaviour change model. Community Dent Oral Epidemiol. 2009;37:68–77. doi: 10.1111/j.1600-0528.2008.00444.x. [DOI] [PubMed] [Google Scholar]
- 29.Dorri M, Sheiham A, Hardy R, Watt R. The relationship between sense of coherence and tooth brushing behaviours in Iranian adolescents in Mashhad. J Clin Periodontol. 2010;37:46–52. doi: 10.1111/j.1600-051X.2009.01497.x. [DOI] [PubMed] [Google Scholar]
- 30.Bernabé E, Watt RG, Sheiham A, Suominen AL, Vehkalahti MM, Nordblad A, et al. Childhood socioeconomic position, adult sense of coherence and tooth retention. Community Dent Oral Epidemiol. 2012;40:46–52. doi: 10.1111/j.1600-0528.2011.00633.x. [DOI] [PubMed] [Google Scholar]
- 31.Vettore MV. Sense of coherence modifies the association between untreated dental caries and dental pain in low-social status women. Community Dent Health. 2016;33:54–9. 29. [PubMed] [Google Scholar]
- 32.Dorri M, Sheiham A, Watt RG. Modelling the factors influencing general and oral hygiene behaviours in adolescents. Int J Paediatr Dent. 2010;20:261–9. doi: 10.1111/j.1365-263X.2010.01048.x. [DOI] [PubMed] [Google Scholar]
- 33.Antonovsky A. Unraveling the Mystery of Health: How People Manage Stress and Stay Well. New Jersey: Jossey-Bass; 1987. [Google Scholar]
- 34.Volanen SM, Lahelma E, Silventoinen K, Suominen S. Factors contributing to sense of coherence among men and women. Eur J Public Health. 2004;14:322–30. doi: 10.1093/eurpub/14.3.322. [DOI] [PubMed] [Google Scholar]
- 35.Lalani A, Dasar PL, Sandesh N, Mishra P, Kumar S, Balsaraf S. Assessment of relationship between oral health behavior, oral hygiene and gingival status of dental students. Indian J Dent Res. 2015;26:592. doi: 10.4103/0970-9290.176922. [DOI] [PubMed] [Google Scholar]
- 36.Rad AB, Joulaei H, Vossoughi M, Golkari A. Assessing oral health status and behaviors in 6-year-old school children in rural and urban areas of Shiraz, Southern Iran. Int J School Health. 2016;3(1):e33036. [Google Scholar]
- 37.Peltzer K, Pengpid S. Dental health status and oral health behavior among university students from five ASEAN countries. Nagoya J Med Sci. 2017;79:123. doi: 10.18999/nagjms.79.2.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Schützhold S, Holtfreter B, Schiffner U, Hoffmann T, Kocher T, Micheelis W. Clinical factors and self-perceived oral health. Eur J Oral Sci. 2014;122:134–41. doi: 10.1111/eos.12117. [DOI] [PubMed] [Google Scholar]
- 39.Locker D, Wexler EW, Jokovic A. What do older adults’ global self-ratings of oral health measure? J Public Health Dent. 2005;65:146–52. doi: 10.1111/j.1752-7325.2005.tb02804.x. [DOI] [PubMed] [Google Scholar]
- 40.Goodarzi A, Heidarnia A, Tavafian SS, Eslami M. Predicting oral health behaviors among Iranian students by using health belief model. J Educ Health Promot. 2019;8:10. doi: 10.4103/jehp.jehp_10_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Tahani B, Yadegarfar G, Ahmadi A. Knowledge, attitude, and practice of parents of 7-12-year-old children regarding fissure sealant therapy and professional fluoride therapy. J Educ Health Promot. 2017;6:106. doi: 10.4103/jehp.jehp_17_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Van Woerkum C, Bouwman L. Getting things done: An everyday-life perspective towards bridging the gap between intentions and practices in health-related behavior. Health Promot Int. 2014;29:278–86. doi: 10.1093/heapro/das059. [DOI] [PubMed] [Google Scholar]
- 43.Lindström B, Eriksson M. Contextualizing salutogenesis and antonovsky in public health development. Health Promot Int. 2006;21:238–44. doi: 10.1093/heapro/dal016. [DOI] [PubMed] [Google Scholar]
- 44.Silva AN, Mendonça MH, Vettore MV. A salutogenic approach to oral health promotion. Cad Saude Publica. 2008;24(Suppl 4):s521–30. doi: 10.1590/s0102-311x2008001600005. [DOI] [PubMed] [Google Scholar]
- 45.Super S, Wagemakers MA, Picavet HS, Verkooijen KT, Koelen MA. Strengthening sense of coherence: Opportunities for theory building in health promotion. Health Promot Int. 2016;31:869–78. doi: 10.1093/heapro/dav071. [DOI] [PubMed] [Google Scholar]