Abstract
BACKGROUND:
Diabetes self-management (DSM) is the cornerstone in diabetes mellitus (DM) management. Unfortunately, the practice of DSM by Iraqi type 2 DM (T2DM) patients is poor that mainly resulted from their poor knowledge about the required DSM behaviors. This lack of knowledge may be attributed to the lack of DSM education and support (DSMES) program in Iraq. Thus, this study was conducted with aim of developing and validating a culturally specific DSMES program for Iraqi T2DM patients.
MATERIALS AND METHODS:
The development and validation of the DSMES program was done according to the Hilda Taba model. Content validity of the program was done by a panel of 6 health-care experts in management of Iraqi DM patients. Face validity was confirmed by conducting a pilot study for six adults with uncontrolled T2DM at the National Diabetes Center, Baghdad, Iraq. Both the experts and patients were asked to evaluate the developed program in regard to its contents, design, and supporting material (booklet). The evaluation was done by filling in a questionnaire that based on a 5-point scale. Items with a score ≥4 by <70% of the experts and patients were subjected to revision and further assessment.
RESULTS:
No total disagreement for any item was expressed by all participants (experts and patients). Content and face validity was ensured through obtaining a positive feedback from all participants at which all items about the program had scores of ≥4 by at least 75% of participants.
CONCLUSION:
The developed culturally based DSMES program is highly suitable for educating Iraqi T2DM patients.
Keywords: Diabetes self-management education, Iraq, type 2 diabetes
Introduction
Diabetes mellitus (DM) is a chronic metabolic disease with a world prevalence of 8.4%.[1] The prevalence of DM in Iraq is very high and approaching 20% which is comparable to that in some other Middle East countries.[2] Uncontrolled hyperglycemia is associated with the development of DM microvascular (neuropathy, retinopathy, and nephropathy) and macrovascular (stroke, ischemic heart disease, and peripheral vascular disease) complications.[3] Diabetes self-management (DSM) is the cornerstone in the management of diabetes and controlling hyperglycemia; however, it is not a simple task.[4] Unfortunately, the practice of DSM by Iraqi type 2 DM (T2DM) patients is poor and lower than that reported in other countries. The main reason behind poor DSM practice includes poor patient knowledge not only about the required DSM behaviors but also about diabetes and its complications. This lack of knowledge may be attributed to the lack of DSM education (DSME) and support programs in Iraq.[5,6] Despite the presence of dozens of DSME studies which showed a positive effect on glycemic control.[7] Many of these studies provide limited details about the educational program,[8,9] which make replication is not possible;[10] besides that, all of these programs are not specific for Iraqi DM patients since they were designed and validated in countries with different health-care systems and their DM patients have different perceptions, health beliefs, and ethnic structures. Hence, direct adoption of such programs in Iraq is not a good idea, and thus, this study was conducted with aim of developing and validating a DSME and support (DSMES) program that is culturally specific for Iraqi T2DM patients.
Materials and Methods
The development and validation of the DSMES program was done in accordance with the Hilda Taba model [Figure 1].[11]
Figure 1.
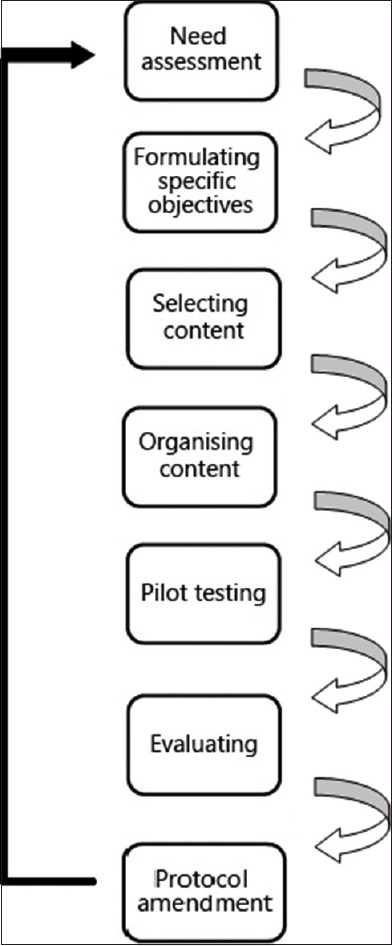
Steps of diabetes self-management educational program development according to Hilda-Taba model
Need assessment
According to the American Diabetes Association (ADA) and Association of Diabetes Care and Education Specialists (ADCES) guidelines, management of DM must involve medications and education about the seven self-care behaviors.[12,13] The current care and management of DM patients in all Iraqi hospitals and clinics (including the National diabetes center) involves prescribing of medications and brief education about the use of medications besides a piece of general advice about the need for dietary restrictions and doing self-monitoring of blood glucose level (SMBG). In general, DM management was performed through a multidisciplinary team approach involving physicians and pharmacists only. Meanwhile, the National Diabetes Center is the only center in Baghdad that has trained diabetes educators that can assist in educating patients about insulin injecting techniques (especially for insulin naïve patients and for those who face problems while injecting insulin) and also about the use of a glucometer. Laboratory tests and physical examination are generally performed at each checkup visit (usually once every 3 months) to the National Diabetes Center. Based on the results of these tests and examinations, the addition and/or deletion in prescribed medications besides medication dose adjustment are done at these checkup visits. The characteristics of the usual care to DM patients are presented in Table 1. According to all of the above, a big gap in the DSMES for Iraqi DM patients is obvious. Thus, the present study was conducted to fill this gap by designing a culturally based DSMES program. To design such a program, analysis of general knowledge, practice, and needs of Iraqi patients with T2DM regarding DSM was performed through a qualitative study.[14] Besides that, a systematic review for all DSMES programs in Middle East countries was conducted[15] to know the used materials for DSMES and to determine factors that result in achieving maximum benefit on glycemic control by such programs.
Table 1.
Care provided to type 2 diabetes mellitus patients in the National Diabetes Center
| Domain | Characteristic |
|---|---|
| Timing | Monitoring at 3-4 month interval |
| Mode of delivery | Individualized through face-to-face interview |
| Theoretical basis | None |
| Materials | Medications and on limited occasions brochures |
| Duration | 5-10 min |
| Care approach | Team of health-care providers: physician, pharmacist, and diabetes educator |
| Educational topics | Diabetes complications |
| How to use the prescribed medications | |
| How to use the glucometer (at the time of dispensing the glucometer only) | |
| Dietary restriction: Need to avoid sugars and reduce carbohydrate and fat consumption | |
| The necessity of adherence to prescribed medications | |
| Management of hypoglycemia (only for those who suffer from recurrent hypoglycemia) | |
| Laboratory tests | FBG |
| RBG | |
| HbA1c (not routinely done) | |
| Lipid profile | |
| Renal function tests | |
| Liver function tests (not routinely done) | |
| General urine examination | |
| Hemoglobin (not routinely done) | |
| ESR (not routinely done) | |
| Examinations | Blood pressure |
| ECG (only for those with chest pain or confirmed IHD) | |
| Eye examination (on limited occasions and only for those with sight problems) | |
| Ultrasound (for those with abdominal pain and/or abnormal laboratory tests) |
FBG=Fasting blood glucose, RBG=Random blood glucose, HbA1c=Glycosylated hemoglobin, ESR=Erythrocyte sedimentation rate, ECG=Electrocardiography, IHD=Ischemic heart disease
Specific objectives
Develop a pharmacist-led DSMES program that can improve knowledge and skills to motivate Iraqi adults with T2DM to perform DSM behaviors, based on health belief theory
Validate the developed program for Iraqi adults with T2DM.
Selection of the contents for the diabetes self-management education and support program
The contents of the DSMES program were selected by the main researcher and they were designed to cover all aspects of the ADCES 7 self-care behaviors (healthy eating, physical activity, medication taken, self-monitoring of blood glucose, solving problems, reducing risks, and healthy coping).[12] The information about DSM in the Iraqi guideline for DM management[16] was limited and based on somewhat old dated references; therefore, educational information in this program was mainly based on the last ADA[13] and ADCES guidelines.[12] Besides that, additional information about healthy diet and antidiabetic medications that are specific for Iraqi T2DM patients was also added to the program. The contents of the program are shown in Table 2. The overall educational material (for “Educational Material,” please contact the corresponding author) had 61 pages including the cover page and content page. It also contains 42 illustrating pictures and 9 tables. Educational material was prepared in the Arabic Language.
Table 2.
Contents of the developed diabetes self-management education and support program
| Topic | Contents |
|---|---|
| General information about diabetes | Definition of diabetes |
| Diabetes symptoms and complications | |
| Healthy eating | Types of major nutrients and their effect on blood glucose level |
| Planning for a meal with a focus on the use of modified plate method | |
| Application of plate method on different foods from the Iraqi cuisine | |
| Physical activity | Benefits of physical activity |
| Main types of physical activity | |
| Recommended physical activity for diabetic patients | |
| Strategies to overcome barriers for physical activity | |
| Prevention of hypoglycemia during physical activity | |
| Medication taken | Importance of antidiabetic medications |
| Importance of medications adherence | |
| How to take the anti-diabetic medication in a correct way | |
| Correct storage of medications (taking into account the weather and lack of electricity in Iraq) | |
| SMBG | Target values for blood glucose level |
| How to measure the blood glucose level | |
| When to measure blood glucose level (recommended measuring times) | |
| Techniques to reduce pain of blood glucose testing | |
| Solving problems | Skills to diagnose and manage hyperglycemia |
| Skills to diagnose and manage hypoglycemia | |
| Skills to manage diabetes during sick days | |
| Skills to reduce the possibility of missing a medication dose | |
| Reducing diabetes risks | Benefits of regular physician visit |
| Recommended schedule for physicians visit | |
| Effect of diabetes on foot and risk of gangrene | |
| Foot care | |
| The danger of smoking and the benefits of smoking cessation | |
| Barriers to quit smoking and how to overcome these barriers | |
| Healthy coping | Negative effects of stress on diabetes |
| Negative and positive ways to cope with stress |
SMBG=Self-monitoring of blood glucose
The educational material was intended for six different groups of T2DM patients: smokers on insulin therapy (51 pages); nonsmokers on insulin therapy (49 pages); smokers on noninsulin antidiabetic therapy (50 pages); and nonsmokers on noninsulin antidiabetic therapy (48 pages); smokers on mixed (insulin with non-insulin) antidiabetic therapy (60 pages); non-smokers on mixed anti-diabetic therapy (58 pages).
Organizing the contents of the diabetes self-management education and support program
The findings of the previously conducted systematic review[15] and qualitative study[14] were used to guide the design of the developed DSMES program. The main obtained findings include:
The educational material of the DSMES program that covers all of the ADCES 7 self-care behaviors is more effective than those covering only some of the ADCES 7 self-care behaviors
Individualized-based education through face-face interview was found to be more effective to improve glycemic control for T2DM patients in Middle East countries[15] and highly recommended by the participants of the qualitative study[14]
The DSMES program should be designed to be patient specific and delivered through few sessions to prevent wasting of the patient's time
A combination of different approaches to deliver information/education (interactive and didactic) was found to be more effective than any single approach to improve patients’ DSM behavior and thus glycemic control
Supporting DSMES program through booklet and telephone call not only highly recommended by Iraqi T2DM patients but also can result in greater benefit from the program
Theory-based interventions may result in improved outcomes.[17] Health belief model was expected to be the most suitable theory for interventions to Iraqi DM patients.
Therefore, the DSMES program was designed to be conducted by a clinical pharmacist with a certificate in diabetes education through two individualized educational sessions over 1 week period. The first session was designed to be conducted at the same time of the checkup visit of the T2DM patient to the National Diabetes Center and the other one within 3–7 days from the first visit according to the participant schedule to give him/her some flexibility. Each session was designed to last for about 80–100 min. These two sessions aimed to build participant's self-management knowledge and skills besides enhancing his/her confidence to perform DSM. The main DSM behaviors (healthy diet, physical activity, medication taken, and SMBG) will be explained at the first visit. At the end of the first visit, individualized goals will be set and each participant will be given a written summary of self-selected behavioral goals besides the educational booklet. Additionally, each participant will be asked to do intensive blood glucose testing (before and after each main meal) for 2–3 days while writing the type and amount of food in each meal, the type, the duration, and the time for exercise, and the time for taking each medication and to bring these notes in the second visit. This strategy may further motivate participants to do DSM by allowing them to monitor their progress[18] and also enable the educator to assess the behavior of each participant and thus to educate him/her about the mistaken behaviors through the use of nonjudgmental language[19] while re-enforcing correct behaviors.
At the beginning of the second educational session, an open discussion will be conducted with each participant to find out the achievement of the set goals at the first educational session and also to assess the presence of any barriers that face the participant during performing the already explained DSM behaviors during the period between these two visits. Other DSM behaviors such as solving diabetes problems, healthy coping with stress, and reducing risks will be explained in the second educational session. At the end of the second educational session, individualized goals will be also set and a written summary of these goals will be shared with each participant.
A phone number will be shared between the participant and the educator to help the educator to follow-up the participant twice (once after 1.5 and the other after 4.5 months from the program start) and to allow the participant to call the educator in case of facing any difficulties or problems with the intervention. The outlines of the developed DSMES program are presented in Table 3.
Table 3.
Outlines of the developed diabetes self-management education and support program
| Parameter | Details |
|---|---|
| Framework for program modules | ADCES 7 self-care behaviors (healthy eating, physical activity (exercise), medications, SMBG level (SMBG), reducing diabetes risks, resolving problems, and health coping with stress) |
| Delivery format | Face-to-face individual-based educational sessions (two sessions; 80-100 min in each session) |
| Lectures with open discussions, posters, and real demonstrations with training | |
| Giving an educational booklet to each participant at the end of the first educational session | |
| Goal setting is established at the end of each educational session and reviewed at the next visit | |
| Two follow-up phone calls and reminder messages | |
| Resolving urgent problems through an emergency mobile phone number | |
| Follow-up visit 3 months after the first educational visit to reinforce good behaviors and correct poor behaviors | |
| Theoretical framework | Health belief model |
ADCES=Association of Diabetes Care and Education Specialists, SMBG=Self-monitoring of blood glucose
Content validity of the developed program
Before pilot testing of the developed DSMES program, content validity of the program was done during May 2018 by a panel of 6 health-care experts in management of Iraqi patients with T2DM including 1 internist, 1 nutritionist, 2 clinical pharmacists, 1 biochemist, and 1 diabetes educator.
Data collection tool and technique
Health-care experts were given the educational materials and the design of the developed DSMES program and then asked to evaluate this program in regard to its design (number of sessions, duration of sessions, educational approach, and delivery format); educational contents (adequacy of information, quality of information, adequacy of demonstrations, and suitability of information to the Iraqi DM patients); and its supporting (booklet) material (font size, easy to understand, adequacy of information, and adequacy of photos). The evaluation was done by filling in a questionnaire [Appendix 1] that based on a 5-point scale ranging from 1 (totally disagree) to 5 (totally agree). Experts were able to add their comments and suggestions to improve the program at the end of the questionnaire. Items with a score ≥4 by <70% of the health care experts[20] were subjected to revision (according to the given comments and suggestions) and further assessment.
Study design and study participants
To determine the face validity of the final version (experts approved version) of the developed DSMES program, a pilot cross-sectional study was conducted in an outpatient clinic of the National Diabetes Center in Baghdad, Iraq. Six adults with T2DM from the National Diabetes Center were recruited as the study sample. Patients were eligible for the study if they were (1) adults who are able to speak and read the Arabic language; (2) had been diagnosed with T2DM at least 1 year ago; (3) on the same antidiabetic medication(s) and dose for at least 3 months; (4) had uncontrolled hyperglycemia (glycosylated hemoglobin ≥7% and/or fasting blood glucose >126 mg/dl at two consecutive visits to the National Diabetes Center); (5) had no any mental or psychological illness; and (6) had no end-organ damage. Recruitment of participants to this study was through a physician who works in the National Diabetes Center clinic. Participant's eligibility to this study was assessed by the main researcher. All eligible patients were instructed about the study objective and the confidentiality of obtained data. Only those who gave their consent were included in the pilot cross-sectional study.
Ethical considerations
Ethical approval for this pilot cross-sectional study was obtained from the ethical committee at the National Diabetes Center.
Pilot testing of the developed diabetes self-management education and support program
The pilot testing of the developed DSMES program was conducted according to the study protocol [Table 3]. At the end of the second educational session, all participants were asked to assess the educational program and its materials by filling in a questionnaire [Appendix 1]. Participants were able to add their comments and suggestions to improve the program at the end of the questionnaire. Items with a score ≥4 by <70% of the participants[20] were subjected to revision (according to the given comments and suggestions) and further assessment.
Results (Evaluation and Program Amendment)
The experts’ responses were analyzed, and the followings were obtained: No total disagreement for any item was expressed by all of the experts. All items about the educational program had scores of ≥4 by at least 83.3% of experts; further details are given in Table 4. One expert suggested reducing the time and the number of educational sessions.
Table 4.
Assessment of the diabetes self-management education and support program by the panel of experts
| Parameter | Totally agree (%) | Agree (%) | Neutral (%) | Disagree (%) | Totally disagree (%) |
|---|---|---|---|---|---|
| Educational contents of the program | |||||
| Adequacy of information | 6 (100) | 0 | 0 | 0 | 0 |
| Adequacy of demonstrations | 6 (100) | 0 | 0 | 0 | 0 |
| Quality of information | 6 (100) | 0 | 0 | 0 | 0 |
| Suitability of information to Iraqi T2DM patients | 4 (66.7) | 1 (16.7) | 1 (16.7) | 0 | 0 |
| The program design | |||||
| Number of educational sessions | 3 (50) | 2 (33.3) | 1 (16.7) | 0 | 0 |
| Time of each educational session | 3 (50) | 3 (50) | 0 | 0 | 0 |
| Approach of education (didactic and interactive approach) | 6 (100) | 0 | 0 | 0 | 0 |
| Method of delivering information (individual based face to face interview) | 3 (50) | 3 (50) | 0 | 0 | 0 |
| The educational booklet | |||||
| Adequacy of information | 6 (100) | 0 | 0 | 0 | 0 |
| Adequacy of figures and pictures | 6 (100) | 0 | 0 | 0 | 0 |
| Font size | 4 (66.7) | 2 (33.3) | 0 | 0 | 0 |
| Easy to understand | 2 (33.3) | 3 (50) | 1 (16.7) | 0 | 0 |
T2DM=Type 2 diabetes mellitus
On the other hand, responses from T2DM patients were also analyzed. All participants totally agreed on all items of the educational contents of the program, while at least 83.3% of participants agreed on the suitability of the program design. Regarding the booklet, two participants did not read the booklet in the period between the two educational sessions; therefore, the contents of the booklet were evaluated by four participants only. At least 75% of participants gave positive feedback on the design and content of the booklet; further details were given in Table 5. One participant suggested reducing the amount of information in the booklet. Since most of the obtained experts and patients comments had a negative effect on the quality of the program and besides that, the positive responses for most experts and T2DM patients were sufficient to confirm content and face validity of the developed program, so the program was left as it is without any further revisions.
Table 5.
Assessment of the diabetes self-management education and support program by type 2 diabetes mellitus patients
| Parameter | Totally agree (%) | Agree (%) | Neutral (%) | Disagree (%) | Totally disagree (%) |
|---|---|---|---|---|---|
| Educational contents of the program | |||||
| Adequacy of information | 6 (100) | 0 | 0 | 0 | 0 |
| Adequacy of demonstrations | 6 (100) | 0 | 0 | 0 | 0 |
| Quality of information | 6 (100) | 0 | 0 | 0 | 0 |
| Suitability of information to Iraqi T2DM patients | 6 (100) | 0 | 0 | 0 | 0 |
| The program design | |||||
| Number of educational sessions | 2 (33.3) | 4 (66.7) | 0 | 0 | 0 |
| Time of each educational session | 2 (33.3) | 3 (50) | 1 (16.7) | 0 | 0 |
| Approach of education (didactic and interactive approach) | 6 (100) | 0 | 0 | 0 | 0 |
| Method of delivering information (individual-based face-to-face interview) | 6 (100) | 0 | 0 | 0 | 0 |
| The educational booklet | |||||
| Adequacy of information | 4 (100) | 0 | 0 | 0 | 0 |
| Adequacy of figures and pictures | 4 (100) | 0 | 0 | 0 | 0 |
| Font size | 2 (50) | 1 (25) | 0 | 1 (25) | 0 |
| Easy to understand | 3 (75) | 0 | 0 | 1 (25) | 0 |
T2DM=Type 2 diabetes mellitus
Discussion
There is a robust need to enhance DSM among Iraqi T2DM patients through the development of a culturally specific program for DSMES. One of the most important challenges during the development of any educational program is the choice of suitable materials that can help in achieving the program goals.
The results of this study showed a high agreement on the educational contents of the developed DSMES program by most health-care experts and participant T2DM patients. A similar finding was also obtained in studies that conducted in other developing countries.[20,21,22] In addition, this good agreement on the educational contents of the program may be attributed to its coverage for all of the seven self-care behaviors. Furthermore, the lack of previous culturally specific DSMES program in Iraq[5,6] may also positively influence choices of raters about the content of this program.
This study also showed a good agreement on the design of the current DSMES program by the panel of experts and participant T2DM patients. There are many reasons behind the agreement on the design of the developed program including the interactive mode of delivering information to the patient which can increase patient satisfaction;[23] and training of participants can improve their skills and confidence in themselves to perform the DSM behaviors,[24,25] besides taking into account needs, perceptions, and attitudes of Iraqi T2DM patients[26] to design a comprehensive, short, and flexible DSMES program. Similarly, positive feedback on the design of the developed educational program was also obtained in many other studies.[20,21,22]
On the other hand, the panel of experts and T2DM patients were highly persuaded by the prepared educational booklet in regard to its adequacy of information and illustrations and its easiness to be read and understood. This finding was similar to the finding of a study that evaluated a nurse-led DSME program among Iranian adults with T2DM patients.[20]
Limitations and recommendations
There are some limitations in the current study: the first one is the small sample size, the second one is the assessment of the booklet was done by only two-third of the participants, and the last limitation is the pilot testing of the developed program on educated T2DM patients only. Despite these limitations, it is expected that the program is suitable even for illiterate patients because the intervention is based on patient's needs through an interactive way of education with demonstrations and pictorial illustration of most information in the program and the booklet. Anyhow, further studies are needed to confirm suitability of the current program among larger sample of T2DM patients including illiterate patients and those with low educational level.
Conclusion
The currently developed culturally based DSMES program is suitable for educating Iraqi adults with T2DM. Thus, it is highly recommended to adopt such a program by the Iraqi Ministry of Health to assess the effectiveness of the current program to improve DSM behaviors and glycemic control among T2DM patients in different regions of Iraq.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors express their gratitude to the staff of the National Diabetes Center.
Appendix
Appendix 1.
The questionnaire for the assessment of the diabetes self-management education and support program
| Parameter | Totally agree | Agree | Neutral | Disagree | Totally disagree |
|---|---|---|---|---|---|
| Educational contents of the program | |||||
| Adequacy of information | |||||
| Adequacy of demonstrations | |||||
| Quality of information | |||||
| Suitability of information to Iraqi T2DM patients | |||||
| The program design | |||||
| Number of educational sessions | |||||
| Time of each educational session | |||||
| Approach of education (didactic and interactive approach) | |||||
| Method of delivering information (individual-based face-to-face interview) | |||||
| The educational booklet | |||||
| Adequacy of information | |||||
| Adequacy of figures and pictures | |||||
| Font size | |||||
| Easy to understand |
T2DM=Type 2 diabetes mellitus
References
- 1.Cho NH, Shaw JE, Karuranga S, Huang Y, da Rocha Fernandes JD, Ohlrogge AW, et al. IDF diabetes atlas: Global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract. 2018;138:271–81. doi: 10.1016/j.diabres.2018.02.023. [DOI] [PubMed] [Google Scholar]
- 2.Mansour AA, Al-Maliky AA, Kasem B, Jabar A, Mosbeh KA. Prevalence of diagnosed and undiagnosed diabetes mellitus in adults aged 19 years and older in Basrah, Iraq. Diabetes Metab Syndr Obes. 2014;7:139–44. doi: 10.2147/DMSO.S59652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Balaji R, Duraisamy R, Kumar MP. Complications of diabetes mellitus: A review. Drug Invent Today. 2019;12:98–103. [Google Scholar]
- 4.Shrivastava SR, Shrivastava PS, Ramasamy J. Role of self-care in management of diabetes mellitus. J Diabetes Metab Disord. 2013;12:14. doi: 10.1186/2251-6581-12-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fadhil AM, Khalifa MF. Evaluation of diabetes self-management among patients in Baghdad City: A comparative study. Iraqi Natl J Nurs Spec. 2018;31:101–9. [Google Scholar]
- 6.Abbas SK, Al-Tukmagi HF, AL-Auqbi TF. Assessment of knowledge, attitude and practice in a sample of Iraqi type 2 diabetic patients. Al Qadisiya Med J. 2015;11:100–6. [Google Scholar]
- 7.Chrvala CA, Sherr D, Lipman RD. Diabetes self-management education for adults with type 2 diabetes mellitus: A systematic review of the effect on glycemic control. Patient Educ Couns. 2016;99:926–43. doi: 10.1016/j.pec.2015.11.003. [DOI] [PubMed] [Google Scholar]
- 8.Farsaei S, Sabzghabaee AM, Zargarzadeh AH, Amini M. Effect of pharmacist-led patient education on glycemic control of type 2 diabetics: A randomized controlled trial. J Res Med Sci. 2011;16:43–9. [PMC free article] [PubMed] [Google Scholar]
- 9.Jarab AS, Alqudah SG, Mukattash TL, Shattat G, Al-Qirim T. Randomized controlled trial of clinical pharmacy management of patients with type 2 diabetes in an outpatient diabetes clinic in Jordan. J Manag Care Pharm. 2012;18:516–26. doi: 10.18553/jmcp.2012.18.7.516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: Template for intervention description and replication (TIDieR) checklist and guide. BMJ. 2014;348:g1687. doi: 10.1136/bmj.g1687. [DOI] [PubMed] [Google Scholar]
- 11.Taba H. Curriculum Development: Theory and Practice. New York: Harcourt, Brace and World; 1962. [Google Scholar]
- 12.American Association of Diabetes Educators. AADE guidelines for the practice of diabetes self-management education & training. Diabetes Educ. 2009;35:85–107. [Google Scholar]
- 13.American Diabetes Association. Standards of medical care in diabetes 2018. Diabetes Care. 2018;41(Suppl 1):S7–125. doi: 10.2337/dc18-S001. [DOI] [PubMed] [Google Scholar]
- 14.Mikhael EM, Hassali MA, Hussain SA, Shawky N. Self-management knowledge and practice of type 2 diabetes mellitus patients in Baghdad, Iraq: A qualitative study. Diabetes Metab Syndr Obes. 2019;12:1–7. doi: 10.2147/DMSO.S183776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mikhael EM, Hassali MA, Hussain SA. Effectiveness of diabetes self-management educational programs for type 2 diabetes mellitus patients in Middle East countries: A systematic review. Diabetes Metab Syndr Obes. 2020;13:117–38. doi: 10.2147/DMSO.S232958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Iraqi Ministry of Health. Guideline for Diabetes Mellitus and Metabolic Syndrome Management. 2012. Available from: http://phd.iq/LionImages/PDFStore/1Diabetes%20and%20Metabolic%20Syndrome-MOH-Revised%20Final%20May%2015%20docs.pdf .
- 17.Mohebbi B, Tol A, Sadeghi R, Mohtarami SF, Shamshiri A. Self-management intervention program based on the Health Belief Model (HBM) among women with gestational diabetes mellitus: A Quazi-Experimental study. Arch Iran Med. 2019;22:168–73. [PubMed] [Google Scholar]
- 18.Zheng Y, Mancino J, Burke LE, Glanz K. Nutrition in the Prevention and Treatment of Disease. 4th ed. 9. India: Academic Press; 2017. Current Theoretical Bases for Nutrition Intervention and Their Uses; p. 189. Available from: http://www.sciencedirect.com/science/article/pii/B9780128029282000096 . [Google Scholar]
- 19.Dickinson JK, Guzman SJ, Maryniuk MD, O'Brian CA, Kadohiro JK, Jackson RA, et al. The use of language in diabetes care and education. Diabetes Care. 2017;40:1790–9. doi: 10.2337/dci17-0041. [DOI] [PubMed] [Google Scholar]
- 20.Azami G, Soh KL, Sazlina SG, Salmiah MS, Aazami S, Mozafari M, et al. Developing and validating the educational materials for a nurse-led self-management education in adults with type 2 diabetes. Int J Diabetes Metab. 2019;25:1–10. [Google Scholar]
- 21.Malan Z, Mash B, Everett-Murphy K. Development of a training programme for primary care providers to counsel patients with risky lifestyle behaviours in South Africa. Afr J Prim Health Care Fam Med. 2015;7:819. doi: 10.4102/phcfm.v7i1.819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kisokanth G, Prathapan S, Indrakumar J, Ilankoon IM. Validation of educational material for diabetes self-management education: Judgemental and criterion validity. Biomed Res. 2018;29:2290–5. [Google Scholar]
- 23.Heinrich E, de Nooijer J, Schaper NC, Schoonus-Spit MH, Janssen MA, de Vries NK. Evaluation of the web-based Diabetes Interactive Education Programme (DIEP) for patients with type 2 diabetes. Patient Educ Couns. 2012;86:172–8. doi: 10.1016/j.pec.2011.04.032. [DOI] [PubMed] [Google Scholar]
- 24.Winkley K, Upsher R, Stahl D, Pollard D, Kasera A, Brennan A, et al. Psychological interventions to improve self-management of type 1 and type 2 diabetes: A systematic review. Health Technol Assess. 2020;24:1–232. doi: 10.3310/hta24280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tol A, Baghbanian A, Mohebbi B, Shojaeizadeh D, Azam K, Shahmirzadi SE, et al. Empowerment assessment and influential factors among patients with type 2 diabetes. J Diabetes Metab Disord. 2013;12:6. doi: 10.1186/2251-6581-12-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mandalia PK, Stone MA, Davies MJ, Khunti K, Carey ME. Diabetes self-management education: Acceptability of using trained lay educators. Postgrad Med J. 2014;90:638–42. doi: 10.1136/postgradmedj-2014-132865. [DOI] [PubMed] [Google Scholar]


