Abstract
BACKGROUND:
Anemia is a major public health problem among reproductive-aged women in India. Despite many programs implemented for decades to fight anemia, still the prevalence of anemia is high because its associated factors vary among different regions. This exploratory study was carried out to find the prevalence of anemia and factors influencing it among nonpregnant reproductive-aged women (15–49 years) in a rural area of Coimbatore.
MATERIALS AND METHODS:
The study was conducted in the field practice area of Rural Health Training Centre, PSG IMSR, Coimbatore, during March 2016 to August 2016. Participants were recruited by two-staged random sampling method and 426 participants were enrolled. A predesigned semi-structured questionnaire was used to collect the data pertaining to the factors influencing the prevalence of anemia, and their hemoglobin level was measured using a hemoglobin photometer. The data were analyzed using SPSS-24. (IBM Corporation, SPSS Inc., Chicago, IL, USA) Univariate analysis was done using Chi-square test and the strength of association was estimated by odds ratio. Those factors which were found to be significant by univariate analysis were further subjected to multivariate logistic regression analysis. P < 0.05 was considered statistically significant.
RESULTS:
The prevalence of anemia was estimated as 64.8% (95% confidence interval: 60%–69%). Significant predictors for anemia among the study participants were less frequent intake of green leafy vegetables (adjusted odds ratio [AOR] = 3.65, confidence interval [CI]: 2.17–6.12), low socioeconomic status (AOR = 3.36, CI: 1.93–5.84), illiteracy (AOR = 3.09, CI: 1.09–5.24), birth spacing <2 years (AOR = 2.49, CI: 1.19–5.25), excessive menstrual bleeding (AOR = 2.27, CI: 1.09–4.76), and inadequate knowledge regarding anemia (AOR = 2.03, CI: 1.19–3.44).
CONCLUSION:
Anemia is still prevalent in high magnitude in reproductive-aged women, and measures to prevent and control it are not optimum. Hence, its multifactorial determinants have to be addressed to alleviate its burden.
Keywords: Anemia, nonpregnant reproductive-aged women, risk factors for anemia
Introduction
Anemia is a major public health problem, affecting 24.8% of the global population. The prevalence of anemia is disproportionately high in developing countries compared to developed countries due to poverty, illiteracy, inadequate dietary intake, certain infectious diseases, frequent pregnancy, and poor access to health services. The most vulnerable groups affected by anemia are children, adolescent girls, and women in the reproductive age, especially pregnant women.[1] Anemia can reduce the quality of life, leading to a substantial economic burden on the affected individuals and their families, communities, and societies.[2] According to the Fourth National Family Health Survey (NFHS-4), 54.4% and 56.9% of women of reproductive age are found to be anemic in rural areas of India and in Tamil Nadu, respectively.[3] Anemia is found to be more prevalent among reproductive-aged women in India, and it poses a significant morbidity risk, particularly among reproductive-aged women. Despite the fact that anemia is largely preventable and easily treatable if detected in time, it still continues to be a common cause of morbidity and mortality and is considered a silent killer.[4] This nutritional disability in the life of women will have adverse consequences on the developmental stages of the next generation and can have long-term impact and thus leave a perpetual effect.[5] The WHO recommends local studies for each region to provide baseline information for designing prophylactic and therapeutic strategies to control this problem.[4] Most of the studies carried out in different parts of the country are either hospital-based studies done among pregnant and lactating mothers or college/school-based studies done among adolescent girls, there is a scarcity of community-based studies among nonpregnant reproductive-aged women. Social, cultural, economic, and dietary features vary widely across India and hence the factors influencing anemia also vary based on the geographical location. Though the accurate data on the prevalence of anemia is essential to determine public health measures, in reality, accurate data are scarce in the study area, which impedes anemia preventive strategies. Identifying the local determinants and risk factors of anemia will help to plan for appropriate package of services to reduce the risks of morbidity and mortality associated with anemia and is one of the priorities for safe motherhood initiative.
Materials and Methods
Study design and setting
A community-based cross-sectional study was done in the rural field practice area of PSG Institute of Medical Science and Research, Coimbatore, during March 2016 to August 2016. The conceptual framework adopted in this study explains the possible causes of anemia and the interconnectedness of these factors in predisposing a woman to become anemic [Figure 1].[6]
Figure 1.

Conceptual framework for anemia among reproductive age women
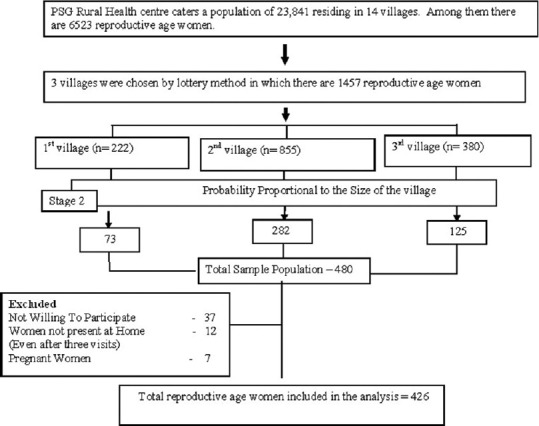
Study participants and sampling
With an estimated prevalence of 55.4% from NFHS-4[3] study and 5% allowable error, and 20% nonresponse rate, the sample size was estimated as 480. The study participants were selected by two-staged random sampling method [Figure 2]. In the first stage, three villages were selected randomly from 14 villages. In the second stage, the required sample numbers were selected from three villages by probability proportional to the size of the villages. Individual participants from each village were chosen by SPSS-generated random numbers. Women in reproductive age group (15–49 years) who are permanent residents for at least 1 year were included, whereas pregnant women, those not willing to participate in the study, and absence at home on three visits were excluded from the study.
Figure 2.
Flow diagram showing the sampling procedure
Data collection tool and technique
After obtaining informed consent, a predesigned semi-structured questionnaire was used to collect the data pertaining to the factors influencing the prevalence of anemia namely demographic factors, socioeconomic, environmental factors, reproductive, and menstrual factors. Socio-economic status was assessed using Modified Prasad Classification. Knowledge was assessed by a series of twelve questions on causes, symptoms, complication, and prevention methods, and a scoring system was given and those who scored more than 50% were considered having adequate knowledge on anemia. Sixteen iron-rich food items were considered in our study based on the iron content given by the National Institute of Nutrition.[7] Height and weight were measured according to the WHO standard procedure,[8] and confidentiality of the study participants was ensured. Hemoglobin level was measured from capillary blood obtained by finger prick using a hemoglobin photometer, which is a reliable method in field surveys.[9] The sensitivity and specificity for the hemoglobin estimation by this photometer is 94.1% and 95.2%, respectively.[10] The Haemoglobin photometer was checked each day morning prior to data collection with the control microcuvette given along with the instrument by the manufacturer for the purpose of internal validation of the instrument. After every seventy samples examined by the photometer, the instrument was tested for reliability using same blood samples, and it was also externally validated in the Pathology Laboratory of PSGIMSR using the Beckman Coulter LH 450 method. Difference in the value of hemoglobin was found to be in the range of 0.3–0.6 g/dL.
Ethical consideration
The study was carried out in accordance with the ethical standards of PSGIMSR Institutional Human Ethics Committee (IHEC – Proposal Code – 14/075), and the Ethical Principles for Medical Research was followed.
Operational definition
The WHO criteria for diagnosis of anemia in nonpregnant women with hemoglobin level <12 g/dL were used in this study. Grading of anemia was done on the basis of cutoff values: mild anemic (hemoglobin [Hb]: 11–11.9 g/dL), moderate anemic (Hb: 8–10.9 g/dL), and severe anemic (Hb: <8 g/dL).
Statistical analysis
Data were analyzed using SPSS-24. The prevalence of anemia was estimated with 95% confidence interval (CI). The associations between independent variables and hemoglobin level were tested using Chi-square test and the strength of associations was obtained using odds ratio. The variables which were found to be statistically significant in univariate analysis were further subjected to multivariate logistic regression analysis. P < 0.05 was considered statistically significant.
Results
Of the selected 480 women of reproductive age, 37 of them did not participate due to fear of finger prick, 7 of them were pregnant, and 12 of them were not present in their house during three visits and hence excluded from the study. A total of 426 nonpregnant women in the reproductive age group were enrolled in the study.
The demographic profile of the study participants is shown in Table 1. 18.8% of the study participants were in the age group of 25-29 years, 26.7% had education up to high School, higher proportion (63.8%) of the study participants were not working and majority of them (92.7%) belonged to Hindu religion. 71.6% of the participants were residing in a nuclear family and 37% of them belonged to low-socio-economic class (Class IV and V).
Table 1.
Demographic profile of the study participants (n=426)
| Variable | Frequency, n (%) |
|---|---|
| Age (years) | |
| 15-19 | 51 (12.0) |
| 20-24 | 75 (17.6) |
| 25-29 | 80 (18.8) |
| 30-34 | 66 (15.5) |
| 35-39 | 59 (13.8) |
| 40-44 | 48 (11.3) |
| 45-49 | 47 (11.0) |
| Education | |
| Illiterate | 64 (16.2) |
| Primary | 29 (6.8) |
| Middle | 63 (14.8) |
| High school | 114 (26.7) |
| Higher secondary | 68 (16.0) |
| Graduate | 83 (19.5) |
| Occupation | |
| Working | 154 (36.2) |
| Not working | 272 (63.8) |
| Religion | |
| Hinduism | 395 (92.7) |
| Christianity | 27 (6.3) |
| Islam | 4 (1.0) |
| Type of family | |
| Nuclear | 305 (71.6) |
| Extended | 121 (28.4) |
| Socioeconomic status | |
| Class I | 22 (5.2) |
| Class II | 102 (23.9) |
| Class III | 144 (33.8) |
| Class IV | 111 (26.1) |
| Class V | 47 (11.0) |
Table 2 shows the reproductive characteristics of the study participants. Nearly 75.6% of them have attained menarche before the age of 14 years, and 79.6% of the participants were married. Among those who were married, 25.7% of them got married before the age of 18 years, 9.6 % of them have more than 2 children, 28.6% have a history of abortion, and 8.3% of the individuals are currently using IUD. Among 218 people having two children and more, 45.4% had birth spacing <2 years. 10 participants had hysterectomy done, and 19 of them have attained menopause. Of the remaining 397 participants, 21.2% of them had irregular menstrual cycle and 19.5% of the individuals had excessive menstrual bleeding.
Table 2.
Reproductive and menstrual characteristics of the study participants
| Variable | Frequency, n (%) |
|---|---|
| Age at the time of menarche (years) (n=426) | |
| <14 | 322 (75.6) |
| ≥14 | 104 (24.4) |
| Marital status (n=426) | |
| Unmarried | 70 (16.4) |
| Married | 339 (79.6) |
| Widowed | 15 (3.5) |
| Divorced | 2 (0.5) |
| Age at the time of marriage (years) (n=339) | |
| <18 | 87 (25.7) |
| >18 | 252 (74.3) |
| Number of children (n=339) | |
| 0 | 22 (6.4) |
| 1 | 99 (29.2) |
| 2 | 185 (54.6) |
| 3 | 24 (7.1) |
| >3 | 9 (2.7) |
| Age at the time of first child birth (years) (n=317) | |
| <19 | 35 (11) |
| ≥19 | 282 (89) |
| Birth spacing (n=218) | |
| <2 | 99 (45.4) |
| ≥2 | 119 (54.6) |
| History of abortion (n=339) | |
| Yes | 97 (28.6) |
| No | 242 (71.4) |
| Current IUD usage (n=339) | |
| Yes | 28 (8.3) |
| No | 311 (91.7) |
| Menstrual cycle (n=397) | |
| Regular | 313 (78.8) |
| Irregular | 84 (21.2) |
| Excessive menstrual bleeding (n=397) | |
| Yes | 83 (20.9) |
| No | 314 (79.1) |
IUD=Intrauterine device
Regarding the environmental factors, only 64.3% of them were having toilet facility in their homes, 20.4% of them were having the practice of open-air defecation, and the rest were using community toilets. Almost 5.9% of the participants had the habit of barefoot walking, 8.2% of them had a history of passing worms in the stool, and 20% of them did not have the habit of washing hands with soap after defecation.
Regarding knowledge, 49.1% of them had adequate knowledge regarding anemia – its cause, symptoms, methods to prevent anemia – and knowledge regarding iron-rich foods. Almost 87.3% of the participants were on mixed diet and 40.1 of them have the habit of taking coffee along with food. Nearly half (48.6%) of them were having normal body mass index (BMI), while 19% of them were undernourished and 32.4% were overweight/obese. The mean BMI of the study participants was 23.03 ± 4.71 kg/m2.
Prevalence of anemia
The prevalence of anemia among the study population was 64.8% (95% CI: 60–69). The mean hemoglobin of the study participants was 11.34 ± 1.63 g/dL. Out of the 276 anemic women, 55.07% of them were mildly anemic, 35.15% were moderately anemic, and 9.78% of them were severely anemic.
Factors influencing prevalence of anemia
The contributing factors associated with anemia in descending order as revealed by multivariate logistic regression [Table 3] were intake of green leafy vegetables (GLVs) (<2 times weekly), socioeconomic status (class IV and V), illiteracy, birth spacing <2 years between last two pregnancies, excessive menstrual bleeding, and inadequate knowledge regarding anemia. Factors such as open air defecation habit, history of passing worms in stool, not washing hands with soap after defecation, attained menarche <14 years of age, irregular menstrual cycle, following vegetarian diet, those having the habit of drinking coffee along with food, those having low BMI, intake of whole grains and mutton less frequently, which were found to have a significant association on univariate analysis did not show a significant association with anemia in the multivariate logistic regression analysis. There was no significant association between anemia and type of family, habit of barefoot walking, marital status, age at marriage <18 years, age at first child birth <19 years, having more than two children, current IUD usage, and other iron-rich foods.
Table 3.
Multivariate logistic regression analysis of factors influencing anemia
| Variable | AOR | CI | P |
|---|---|---|---|
| Education | |||
| Illiterate | 3.09 | 1.09-8.81 | <0.05 |
| Literate | 1 | ||
| Socioeconomic status | |||
| Classes IV, V | 1.38 | 1.93-5.84 | <0.001 |
| Classes I, II, III | 1 | ||
| Practice open-air defecation | |||
| Present | 1.84 | 0.97-5.57 | 0.09 |
| Absent | 1 | ||
| History of passing worms in stools | |||
| Present | 2.83 | 0.88-9.04 | 0.08 |
| Absent | 1 | ||
| Washing hands with soap after defecation | |||
| Present | 0.89 | 0.44-1.21 | 0.75 |
| Absent | 1 | ||
| Menarche attained (years) | |||
| <14 | 2.35 | 0.78-4.22 | 0.09 |
| ≥14 | 1 | ||
| Birth spacing (<2 years) | |||
| Present | 2.49 | 1.19-5.25 | <0.05 |
| Absent | 1 | ||
| Regularity of menstrual cycle | |||
| Regular | 0.78 | 0.42-1.47 | 0.44 |
| Irregular | 1 | ||
| Excessive menstrual bleeding | |||
| Present | 2.27 | 1.09-4.76 | <0.05 |
| Absent | 1 | ||
| Knowledge regarding anemia | |||
| Inadequate | 2.03 | 1.19-3.44 | <0.05 |
| adequate | 1 | ||
| Nature of diet | |||
| Vegetarian | 2.57 | 0.89-6.29 | 0.10 |
| Mixed | 1 | ||
| Taking coffee along with food | |||
| Yes | 1.60 | 0.92-2.78 | 0.09 |
| No | 1 | ||
| BMI (Kg/m2) | |||
| <25 | 2.46 | 0.94-5.01 | 0.57 |
| ≥25 | 1 | ||
| Intake of whole grains (times/week) | |||
| <2 | 2.36 | 0.89-8.44 | 0.102 |
| ≥2 | 1 | ||
| Intake of GLVs (times/week) | |||
| <2 | 3.65 | 2.17-6.12 | <0.001 |
| ≥2 | 1 | ||
| Intake of heme iron (time/week) (meat, poultry, and fish) | |||
| <1 | 2.79 | 0.88-8.91 | 0.08 |
| ≥1 | 1 |
AOR=Adjusted odds ratio, CI=Confidence interval, BMI=Body mass index, GLVs=Green leafy vegetables
Discussion
Anemia is largely preventable and easily treatable if the local determinants are identified. The WHO and UNICEF therefore reemphasize the urgent need to combat anemia and stress the importance of recognizing its multifactorial etiology for developing effective control programs.[11] Our study showed the prevalence of anemia to be 65% (95% CI: 60%–69%), which is 10% higher compared to NFHS-4[3] survey. According to the WHO, if the prevalence of anemia at community levels is more than 40%,[1] it is considered a problem of high magnitude.
Out of the 276 anemic women, majority of them were mild to moderately anemic and only few of them were severely anemic, which was consistent with that of other studies.[12,13] Hence, its prevention is essential for child survival and safe motherhood.[14] The identified anemic women were referred to the Rural Health Training Centre for further management. Data from the National Nutritional Monitoring Bureau Surveys[5] show that Indian women have a sustained low intake of iron, which may be due to various reasons such as economic, social, and lack of empowerment.
In our study, we identified six factors which had a significant association with anemia. The mean hemoglobin level of significant predictors for anemia in the current study is shown in Figure 3. The first risk factor which was found to have statistical significant association with higher risk of anaemia was the intake of GLV. The study participants who took GLV less than twice a week had three times higher risk of becoming anaemic and this finding was also observed in other studies.[15,16] GLV is a good source of iron, and inadequate intake of GLV is one of the important causes of anemia. It is followed by socioeconomic status which had an inverse relationship with anemia. This finding is consistent with that of other studies.[17,18,19] Poor socioeconomic status is known to be associated with a number of factors such as high parity; short birth interval; poor diet, both in quantity and quality; lack of awareness regarding health and nutrition; a high rate of infectious diseases and parasitic infestations; as well as limited access to medical attention.[12]
Figure 3.

Mean hemoglobin levels of significant predictors for anemia in the current study
The current study reveals the fact that illiterates have about three times higher risk of becoming anemic. Similar findings have been observed in other studies.[20,21] Better educated women enjoy the privilege of higher paying jobs and live in better environment, which will have a positive influence on their nutritional status. In our study, another factor associated with anemia is birth spacing, which is a similar observation in other studies also.[22,23] Repeated pregnancies at short interval deplete the iron stores, thereby leading to anemia, which depict the need for contraception education.[24]
Excessive menstrual bleeding is said to be present when a woman has long duration of menstruation (>5 days) or if there is passage of clots during the menstrual period. In the present study, those with excessive menstrual bleeding had two times higher risk of anemia. Similar findings have been observed in other studies.[19,23,25] We also observed that there was a significant association between inadequate knowledge regarding anemia and risk of anemia, which was similar to the findings of other studies.[26,27] Due to lack of adequate knowledge on anemic causes, ill effects, and preventive measures, incorrect choice of food can lead to nutritional deficiency, making them more prone to become anemic. No significant association was found between hemoglobin concentrations and anthropometric measurements, which was similar to that of another study.[28] Other demographic, reproductive, and socioenvironmental factors did not show a significant association with anemia.
India was the first developing country to commence a National Anaemia Prophylaxis Programme during the 4th five-year plan in 1970, providing iron and folic acid supplementation to all pregnant women and children with an aim to reduce the prevalence of anemia to below 25%.[29] The current study highlights that anemia still remains a public health issue of great magnitude among nonpregnant reproductive-aged women, even after nearly 50 years into the program. Women of childbearing age are at risk of anemia not only throughout their reproductive years but also during pregnancy. Measures to prevent and control anemia so far have largely been ineffective, hence strategies to combat anemia, therefore, should address all the causal factors and focusing our thrust on iron supplementation alone may not be able to provide the much-desired effect because the pathogenesis of anemia is multifactorial. First, the system of periodic screening for anemia among women of childbearing age should be developed and it should be considered one of the important primary healthcare activities at the center. Second, an IEC program to change knowledge, attitudes, household dietary practices, and kitchen garden activities is required to effect positive changes in consumption patterns, thereby improving the nutritional status. Economic empowerment of women can be attempted by organizing the women to form a self help group in order to carry out small scale business and thereby paving a way for small income. Optimal birth spacing (Minimum two years) should be enforced and the reproductive aged women should be made assertive to it.
Further studies are needed to determine the specific types of anemia and the quantum of dietary intake of iron, thereby giving a better insight into the situation.
Limitation
The study has few limitations. Because it is a cross-sectional study, cause–effect relationship cannot be determined. Dietary history was limited to self-reported food frequency, hence the quantum of dietary intake of iron could not be ascertained and confirmation of worm infestation by stool examination was not possible due to operational difficulty.
Conclusion
Anemia has been recognized as a public health problem for many years, but only little progress has been made in its control. The best predictors of anemia in descending order are intake of GLVs (<2 times weekly), socioeconomic status (class IV and V by the Modified Prasad classification), illiteracy, birth spacing <2 years between last two pregnancies, excessive menstrual bleeding, and inadequate knowledge regarding anemia. Hence, to alleviate anemia burden, measures such as economic empowerment, improvement in awareness regarding anemia, dietary practice of taking frequent GLVs and making it easily available, and contraceptive education should be provided by an integrated multifactorial and multi-sectorial approach.
Financial support and sponsorship
This study was supported by PSGIMSR.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The authors would like to thank PSG Institute of Medical Sciences and Research (PSGIMSRIHEC – Proposal Code – 14/075) as well as the study participants for their support. Furthermore, the authors acknowledge the very helpful contributions of the reviewers to the quality of the final manuscript.
References
- 1.McLean E, Cogswell M, Egli I, Wojdyla D, de Benoist B. Worldwide prevalence of anaemia, WHO Vitamin and Mineral Nutrition Information System, 1993-2005. Public Health Nutr. 2009;12:444–54. doi: 10.1017/S1368980008002401. [DOI] [PubMed] [Google Scholar]
- 2.Kaur K. Anaemia 'A Silent Killer’ among women in India: Present scenario. Eur J Zoolog Res. 2014;3:32–6. [Google Scholar]
- 3.International Institute for Population Sciences (IIPS) and ICF National Family Health Survey (NFHS-4), 2015–16: India. [Last accessed on 2020 Sep 02]. Available from: http://mohfwnicin/nfhsfactsheethtm .
- 4.DeMaeyer E, Adiels-Tegman M. The prevalence of anaemia in the World. World Health Stat Q. 1985;38:302–16. [PubMed] [Google Scholar]
- 5.National Nutrition Monitoring Bureau. Hyderabad NNMB. Diet & nutritional status of population and prevalence of hypertension among adults in rural areas. National Institute of Nutrition; 2006. [Last accessed on 2021 Mar 26]. Available from: https://www.nin.res.in/downloads/NNMBReport06Nov20.pdf . [Google Scholar]
- 6.USAID. United States Agency International Development. Geneva, Switzerland: Health Report, USAID; 2013. [Google Scholar]
- 7.Gopalan C, Rama S, Balasubramanian S. Nutritive Value of Indian. Foods-Revised ed. Hyderabad, India: National Institute of Nutrition, Indian Council of Medical Research. 1989:50. [Google Scholar]
- 8.World Health Organization. Physical Status: The Use of and Interpretation of Anthropometry, Report of a WHO Expert Committee. Geneva, Switzerland: World Health Organization; 1995. [PubMed] [Google Scholar]
- 9.Johns W, Lewis SM. Primary health screening by haemoglobinometry in a tropical community. Bull World Health Organ. 1989;67:627. [PMC free article] [PubMed] [Google Scholar]
- 10.Akhtar K, Sherwani RK, Rahman K, Hasan J, Shahid M. HemoCue photometer: A better alternative of hemoglobin estimation in blood donors? Indian J Hematol Blood Transfus. 2008;24:170–2. doi: 10.1007/s12288-008-0041-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.World Health Organization. United Nations Children's Fund (2004) Focusing on Anaemia: Towards an Integrated Approach for Effective Anaemia Control. Joint Statement by the World Health Organization and the United Nations Children's Fund. Geneva: World Health Organization; 2011. [Google Scholar]
- 12.Yip R. Forging effective strategies to combat iron deficiency-plenary papers-prevention and control of Iron deficiency: Policy and Strategy Issues. J Nutr. 2002;132:802S. doi: 10.1093/jn/132.4.802S. [DOI] [PubMed] [Google Scholar]
- 13.Thankachan P, Muthayya S, Walczyk T, Kurpad AV, Hurrell RF. An analysis of the etiology of anemia and iron deficiency in young women of low socioeconomic status in Bangalore, India. Food Nutr Bull. 2007;28:328–36. doi: 10.1177/156482650702800309. [DOI] [PubMed] [Google Scholar]
- 14.Ramachandran P. Food fortification: A public health approach to bridge the gap between requirement and intake of micronutrients. Proceed Indian Natl Sci Acad. 2018;84:913–22. [Google Scholar]
- 15.Rao S, Joshi S, Bhide P, Puranik B, Kanade A. Social dimensions related to anaemia among women of childbearing age from rural India. Public Health Nutr. 2011;14:365–72. doi: 10.1017/S1368980010002776. [DOI] [PubMed] [Google Scholar]
- 16.Ramachandran P. Nutrition in Pregnancy. In: Gopalan C, Kaur S, editors. Women and nutrition in India, Special Publication No. 5. New Delhi: Nutrition Foundation of India; 1989. pp. 153–93. 19. [Google Scholar]
- 17.Balarajan YS, Fawzi WW, Subramanian SV. Changing patterns of social inequalities in anaemia among women in India: Cross-sectional study using nationally representative data. BMJ Open. 2013;3:e002233. doi: 10.1136/bmjopen-2012-002233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rajaratnam J, Abel R, Ganesan C, Jayaseelan SA. Maternal anaemia: A persistent problem in rural Tamil Nadu. Natl Med J India. 2000;13:242–5. [PubMed] [Google Scholar]
- 19.Venkatachalam J, Muthu R, Singh Z, Madhanraj K, Sathya G. Determinants of anemia among women in the age group of 11-49-A case control study in a rural area of Kancheepuram district, Tamil Nadu. EXCEL Int J Multidisci Manage Stud. 2014;4:218–23. [Google Scholar]
- 20.Gebremedhin S, Enquselassie F. Correlates of anemia among women of reproductive age in Ethiopia: Evidence from Ethiopian DHS 2005. Ethiop J Health Dev. 2011;25:22–30. [Google Scholar]
- 21.Ngnie-Teta I, Kuate-Defo B, Receveur O. Multilevel modelling of sociodemographic predictors of various levels of anaemia among women in Mali. Public Health Nutr. 2009;12:1462–9. doi: 10.1017/S1368980008004400. [DOI] [PubMed] [Google Scholar]
- 22.Swarnlatha N. Prevalence of anaemia and its socio demographic determinants among pregnant women attending government maternity hospital, Tirupati, AP. Sudan J Public Health. 2013;8:104–6. [Google Scholar]
- 23.Alquaiz AM, Gad Mohamed A, Khoja TA, Alsharif A, Shaikh SA, Al Mane H, et al. Prevalence of anemia and associated factors in child bearing age women in Riyadh, Saudi Arabia. J Nutr Metab. 2013:1–7. doi: 10.1155/2013/636585. https://doi.org/10.1155/2013/636585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Asghari S, Mohammadzadegan-Tabrizi R, Rafraf M, Sarbakhsh P, Babaie J. Prevalence and predictors of iron-deficiency anemia: Women's health perspective at reproductive age in the suburb of dried Urmia Lake, Northwest of Iran. J Educ Health Promot. 2020;9:332. doi: 10.4103/jehp.jehp_166_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kaur S, Deshmukh P, Garg B. Epidemiological correlates of nutritional anemia in adolescent girls of rural Wardha. Indian J Commun Med. 2006;31:255–8. [Google Scholar]
- 26.Ahmad N, Kalakoti P, Bano R, Syed MMA. The prevalence of anaemia and associated factors in pregnant women in a rural Indian community. AMJ. 2010;3:276–280. Doi 10.4066/ AMJ.2010.286. [Google Scholar]
- 27.Mamta K, Vibha B. Anaemia: Impact assessment of dietary intervention on iron status of college going girls. Food Sci Res J. 2011;2:76–9. [Google Scholar]
- 28.Adib Rad H, Sefidgar SA, Tamadoni A, Sedaghat S, Bakouei F, Bijani A, et al. Obesity and iron-deficiency anemia in women of reproductive age in northern Iran. J Educ Health Promot. 2019;8:115. doi: 10.4103/jehp.jehp_371_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Agarwal DK, Agarwal KN, Roychoudhry S. Targets in National Anemia Prophylaxis Programme for pregnant women. Indian Pediatr. 1988;25:319–22. [PubMed] [Google Scholar]


