Abstract
BACKGROUND:
The outbreak of coronavirus disease 2019 (COVID-19) has turned attention to the essential competencies needed to confront pandemics for a physician. However, medical students, as future physicians, are not adequately trained for such a situation. This study aimed to determine the essential competencies for a medical student to face the COVID-19 pandemic.
MATERIALS AND METHODS:
We performed this mixed-method needs assessment study at Shiraz University of Medical Sciences in May–June 2020 in three steps: the first step was a brainstorming session followed by a nominal group technique with the experts’ participation. The second step was determining the validity of competencies by calculating the content validity ratio. In the third and last step, three rounds of the modified Delphi technique were held with the participation of 22 medical faculty members and 45 undergraduate medical students to reach a consensus about the competencies utilizing quantitative analysis.
RESULTS:
A total of 30 key competencies essential for a medical student were obtained through the current study. They were categorized into four major themes: (1) developing knowledge and abilities for effective diagnosis and treatment of COVID-19, (2) demonstrating safety principles correctly, (3) demonstrating effective behavior, and (4) determining the meta-competencies.
CONCLUSIONS:
Although medical students will be the frontline physicians in the future pandemics, they are not prepared to display the diversity of requisite skills to practice effectively and safely. This study provides essential competencies for medical students during the COVID-19 pandemic and underlines the importance of a paradigm shift from traditional time-based to competency-based education.
Keywords: Competency-based education, COVID-19, curriculum, medical education, medical students, needs assessment, pandemics
Introduction
Recent crises, especially the coronavirus disease 2019 (COVID-19) pandemic, have brought considerable attention to physicians’ preparedness during these periods.[1] Medical students, as future health-care workers, will be frontline soldiers in this battle. It is well established that better results can be reached by properly preparing health workers for health-care emergencies.[2] Education and training play a vital role in preparing health-care workers to face pandemics. Appropriate education can improve medical students’ knowledge, competencies, and preparedness to cope with pandemics. However, it should be considered that factual knowledge is not enough, and meta-competencies such as critical thinking and decision-making should be defined for dealing with a crisis.[3]
Traditional training cannot meet all students’ educational needs in a critical period.[4] According to students’ educational demands during a pandemic, designing a precise curriculum is essential, and curriculum developers should design and develop a new modified curriculum for an unprecedented situation like the COVID-19 pandemic.[5] They can use experiences gained during prior pandemics, such as the severe acute respiratory syndrome (SARS) outbreak, to reach this purpose more straightforwardly.[6]
Frank et al. defined competency as “An observable ability of a health professional, integrating multiple components such as knowledge, skills, value and attitudes.”[7] Competency-based education needs to be oriented to graduate outcomes and meet societal and patient demands.[8] Therefore, in order to adapt to the new situations, faculties must implement a plan for needs assessment, which can be defined as collecting and analyzing information of the students to identify their educational needs.[9]
After the beginning of the COVID-19 pandemic, medical education has undergone many changes. The risk of disease transmission has led to the cancelation of in-person clinical courses, and it has changed the methods of teaching students to online and virtual methods.[10,11] Since faculties have never encountered such a situation, consequently, they have faced many problems in educating students.[12] This issue emphasizes the importance of identifying the educational needs of students at these unprecedented times.
In the literature review, few studies were found about the methods of empowering medical students during pandemics. In 2019, Rezaee et al. described the students’ educational needs in crisis through conducting a needs assessment. In the mentioned study, having critical competencies in four major areas has been considered necessary for medical students. These areas include the basic concepts of crisis, the ability to control the disease, managing patients properly, and demonstrating acceptable health-care skills.[13] In another study, Tabari et al. asserted that students need to be more competent in public health education, crisis management, and mental health care in an anomalous situation.[14] Since 1999, when Harden et al. introduced outcome-based education in medical education, it has been deemed essential that medical students must have a set of competencies such as the ability to accomplish duties and the ability to perform tasks in the right manner. They suggested a three-circle model for medical student competencies, which contains three parts: the tasks performed by them in the inner circle, the way of doing the tasks in the middle, and individual growth in practice in the outer area.[15]
Considering inevitable medical education changes during the COVID-19 pandemic, comprehensive and accurate needs assessment is required in designing a new medical curriculum for training medical students during this outbreak. In the current study, we aimed to provide an overview of essential competencies for medical students to deal with the COVID-19 pandemic by conducting a comprehensive needs assessment through a mixed-method technique with medical experts and students’ participation.
Materials and Methods
Study design and setting
The process of the study was held in May–June 2020 at Shiraz University of Medical Sciences in three steps: (1) developing the competency framework, (2) determining the validity of the competencies, and (3) three rounds of the modified Delphi technique [Figure 1].
Figure 1.
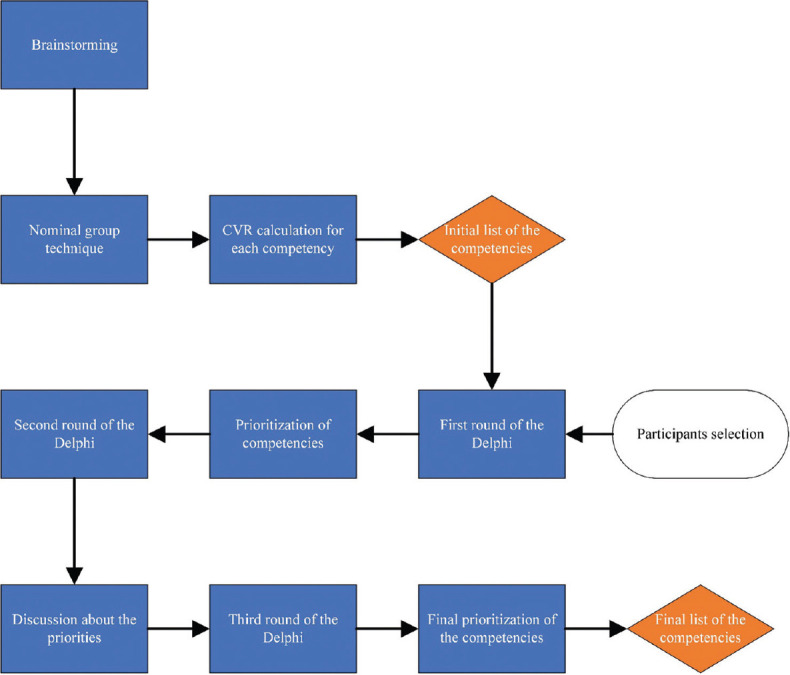
An overview of the needs assessment process
Study participants and sampling
All faculty members and undergraduate medical students who participated in this study were selected using stratified purposive sampling.
Data collection tool and technique
Developing the competency framework
To determine the competencies essential for medical students to cope with the COVID-19 pandemic, we held an online brainstorming session followed by a nominal group technique. The participants were ten clinical faculty members who had expertise in medical education. We used Skype to hold the brainstorming session. We asked all members to write down any competency they think is essential, silently on a paper. Then, we asked the participants to state one competency that they previously had written down to perform the nominal group technique. This process continued until no new competencies were available to be mentioned by the participants. The coordinator of the session, who was a medical education expert, recorded the competencies on paper, as mentioned by the participants. The session coordinator then merged all the duplicates and removable competencies by group consensus. Eventually, we reached 33 competencies essential for medical students to face the COVID-19 pandemic.
Determining validity of the competencies
The session members, who were 22 clinical faculty members, assessed 33 competencies in terms of validity. An online questionnaire was developed based on the results of the nominal group technique, and faculty members marked each competency as “essential,” “useful but nonessential,” or “unnecessary.” They were also asked to add any comments on the competencies and determine competencies that could be necessary but were not mentioned in the primary list. Then, the content validity ratio (CVR) was calculated for each competency. According to Lawshe's table, competencies with CVR > 0.45 were acceptable.[16] Then, competencies were undergone a qualitative content analysis approach, which resulted in four major themes.
Three rounds of the modified Delphi technique
To date, various methods have been employed to achieve the group agreement on an issue. The Delphi technique is one of the most practical ways of doing this process. This method was developed to turn the participants’ ideas into group consensus.[17] In the third step, three rounds of the modified Delphi technique were utilized for making a uniform decision about the priority of the competencies. In the first round, the new list of competencies was sent to 45 medical students and 22 faculty members to conduct the modified Delphi survey. They were asked to score each competency from 1 (completely unnecessary) to 5 (completely necessary) according to the degree these items were essential for a medical student in confronting the COVID-19 pandemic. All members of the expert panel confirmed the validity of the competencies in the second step. Then, the mean score for each competency and each person was calculated. One faculty member's score and eight students’ scores were significantly lower than the participants’ mean score. In the second round, they were contacted via social networks or phone calls and asked to express the reasons for their choices. Furthermore, they had the right to keep their previous scores. All participants changed their ratings following the discussion. Then, we recalculated the scores of each competency and listed them in the order of priority. In the third round, we sent the new list to all participants (n = 67) for any further comments on the competencies’ prioritization. All participants approved the final list. All mean scores and standard deviations were calculated with SPSS, version 21 software (IBM Corp., Armonk, NY, USA).
Ethical consideration
Prior to undertaking this mixed-method needs assessment process, ethical approval (IR.SUMS.REC.1399.401) was obtained from ethics committee of Shiraz University of Medical Sciences. Informed consent was obtained from all participants. Participants took part in this research study voluntarily, and their names were not mentioned in the scripts.
Results
Three competencies had CVR <0.45 were removed from the list. Finally, the modified Delphi survey was conducted with the participation of 45 medical students and 22 faculty members [The demographic features are illustrated in Table 1].
Table 1.
The demographic features of the Delphi survey participants
| Variables | Categories | n (%) |
|---|---|---|
| Gender (n=67) | Male | 34 (50.8) |
| Female | 33 (49.2) | |
| Age (years) (n=67) | 20-30 | 45 (67.1) |
| 31-40 | 8 (12) | |
| 41-50 | 6 (9) | |
| 51-60 | 7 (10.5) | |
| 60< | 1 (1.4) | |
| Medical students (years) (n=45) | 5th | 21 (46.6) |
| 6th | 12 (26.7) | |
| 7th | 12 (26.7) | |
| Faculty members’ specialties (n=22) | Infectious Disease | 2 (9.1) |
| Internal Medicine | 3 (13.6) | |
| Community Medicine | 1 (4.5) | |
| General surgery | 1 (4.5) | |
| Pediatrics | 1 (4.5) | |
| OB and GYN | 1 (4.5) | |
| Pathology | 2 (9.1) | |
| Physiatry | 1 (4.5) | |
| Cardiology | 2 (9.1) | |
| Dermatology | 2 (9.1) | |
| Psychiatry | 2 (9.1) | |
| MD-MPH | 1 (4.5) | |
| Medical education | 3 (13.6) | |
| Years of professional practice among faculty members (n=22) | <10 | 6 (27.3) |
| 10-20 | 6 (27.3) | |
| 20-30 | 5 (22.7) | |
| <30 | 5 (22.7) |
Thirty competencies were agreed upon and prioritized by all participants and divided into four themes: (1) developing knowledge and abilities for effective diagnosis and treatment of COVID-19, (2) demonstrating safety principles correctly, (3) demonstrating effective behavior, and (4) determining the meta-competencies. The priority of competencies, according to the mean scores given by the faculty members and medical students at the end of the Delphi survey, is shown in Table 2.
Table 2.
Medical students’ competencies as identified by participants in the Delphi survey
| Theme (mean score of the competencies within each theme) | Competencies | Mean±SD | Competencies | Mean±SD |
|---|---|---|---|---|
| Theme 1: Developing knowledge and abilities for effective diagnosis and treatment of COVID-19 (4.44) | Proper triage of patients with presentations of COVID-19 (deciding which patient to go where) | 4.78±0.42 | Determining the absence or presence of physical signs that are indicative of COVID-19 | 4.40±0.71 |
| Determining the absence or presence of signs or symptoms that are indicative of COVID-19 | 4.66±0.56 | Interpreting the results of the medical history, physical examination, and using the latest evidence-based diagnostic measures to confirm the diagnosis | 4.33±0.72 | |
| Knowledge of prevention and control | 4.58±0.63 | Knowledge of drug interactions, especially in patients with other medications | 4.30±0.87 | |
| Managing people exposed to a COVID-19 patient | 4.51±0.68 | Knowledge and ability to choose proper ventilation methods by mask, bag, or ventilator for each patient | 4.03±0.95 | |
| Cardiopulmonary resuscitation in COVID-19 patients | 4.43±0.67 | |||
| Theme 2: Demonstrating safety principles correctly (4.84) | PPE using skills | 4.91±0.28 | Knowing how to wash hands properly | 4.82±0.49 |
| Decontamination skills | 4.88±0.32 | Knowing how to take off contaminated clothes and shoes | 4.78±0.42 | |
| Theme 3: Demonstrating effective behavior (4.15) | The ability to inform people correctly about COVID-19 | 4.37±0.81 | Knowing how to tell bad news, especially when young patients died | 4.12±0.78 |
| The ability of teamwork to better serve patients | 4.28±0.81 | Attention to mental health concerns | 4.01±0.91 | |
| Learn when to consult with colleagues | 4.18±0.86 | Leadership skills | 3.93±0.94 | |
| The ability to communicate efficiently with patients, colleagues, etc. | 4.16±0.82 | |||
| Theme 4: Determining the meta-competencies (4.17) | The ability to manage herself or himself emotionally if infected with SARS-CoV-2 | 4.54±0.65 | Identifying the role of a student within the health system in a pandemic | 4.03±1.07 |
| Learn to solve the conflict of risk of being infected and the duty to treat | 4.43±0.83 | Ability to manage human and material resources available | 4.01±0.99 | |
| The ability to adapt to the current situation with personal life | 4.39±0.77 | Managing legal and ethical issues that may happen in pandemics | 3.94±1.08 | |
| Reflection on and in action | 4.34±0.82 | Understanding the role of the health system in preparedness, planning, and response for the pandemic | 3.94±0.88 | |
| Understanding of social accountability in addition to responsibility for each patient | 4.24±0.92 | Recognizing opportunities for further development in the field of pandemics | 3.93±0.89 |
SD=Standard deviation
In theme 1, the competencies are scored by the participants in the following order: (1) proper triage of patients with presentations of COVID-19; (2) determining the absence or presence of signs or symptoms that are indicative of COVID-19; (3) knowledge of prevention and control; (4) managing people exposed to a COVID-19 patient; (5) cardiopulmonary resuscitation in COVID-19 patients; (6) determining the absence or presence of physical signs that are indicative of COVID-19; (7) interpreting the results of the medical history, physical examination, and using the latest evidence-based diagnostic measures to confirm the diagnosis; (8) knowledge of drug interactions, especially in patients with other medications; and (9) knowledge and ability to choose proper ventilation methods by mask, bag, or ventilator for each patient.
Within theme 2, (1) personal protective equipment (PPE) using skills, (2) decontamination Skills, (3) knowing how to wash hands properly, and (4) knowing how to take off contaminated clothes and shoes have the highest score, respectively.
In theme 3, (1) the ability to inform people correctly about COVID-19; (2) the ability of teamwork to better serve patients; (3) learn when to consult with colleagues; (4) the ability to communicate efficiently with patients, colleagues, etc.; (5) knowing how to tell bad news, especially when young patients died; (6) attention to mental health concerns; and (7) leadership skills and in theme 4, (1) the ability to manage herself or himself emotionally if infected with SARS-CoV-2; (2) learn to solve the conflict of risk of being infected and the duty to treat; (3) the ability to adapt to the current situation with personal life; (4) reflection on and in action; (5) understanding of social accountability in addition to responsibility for each patient; (6) identifying the role of a student within the health system in a pandemic; (7) ability to manage human and material resources available; (8) managing legal and ethical issues that may happen in pandemics; (9) understanding the role of the health system in preparedness, planning, and response for the pandemic; and (10) recognizing opportunities for further development in the field of pandemics have the highest score, respectively.
Discussion
Our study has provided 30 essential competencies in 4 major domains regarding medical students’ competencies to face COVID-19 pandemic. In themes 1 and 2, competencies represent basic requirements of becoming a physician, while themes 3 and 4 go beyond the basic requirements and focus on behaviors and meta-competencies that have received increasing attention in recent years. Empowering health-care workers to confront crises is one of the most critical medical education issues in recent years.[18,19] Various studies have been conducted to adapt the educational curriculum to the new conditions during a crisis. It is mentioned in the studies that health-care workers should be educated not only on the knowledge but also on how to use knowledge properly and how to adapt knowledge to new situations.[3,13] Previous studies have shown that the knowledge and preparedness to face a crisis among medical staff is low; this issue emphasizes the importance of training students to be prepared for such a situation.[20,21] In general, in reviewing the literature, none of the writers had investigated the identification of competencies necessary to make students competent in the COVID-19 pandemic. As mentioned earlier, the competencies as the results of this study were classified into four major themes:
Theme 1: Developing knowledge and abilities for effective diagnosis and treatment of COVID-19
This theme includes competencies concerning proper triage, diagnosis, treatment, and prevention of the disease. Obviously, without having sufficient knowledge about COVID-19, providing adequate service to the patients is not possible. The worldwide spread of the COVID-19 has led to ceasing in-person clinical courses;[10,22] as a result universities are striving to use online methods to solve the educational shortcomings.[23] Considering the high pace of knowledge expanding on COVID-19, new therapies and diagnostic methods are rapidly replacing the previous methods in the guidelines. Therefore, health workers should always update their knowledge with new information.[24] A majority of previous studies that have attempted to provide a curriculum for health-care emergencies built concrete evidence on the essence of having updated knowledge and abilities to manage the situation. Despite the fact that there is no specific study about a physician's competencies in a pandemic, many of the provided competencies in relevant studies about competencies in health-care emergencies were comparable to our study.
Theme 2: Demonstrating safety principles correctly
The highest mean score of competencies among a theme belonged to “Demonstrate safety principles correctly.” Personal protection has been one of the main concerns of medical students and faculty members while dealing with the COVID-19 pandemic. Although, it should be borne in mind that proper and timely use of PPE is indispensable to forestall overuse and misuse of the equipment and comprehensive education is vital in order to achieve this goal.[25,26] Therefore, it is necessary to instruct the students to prevent the shortage of PPE. In other words, they should learn to properly select, don, and doff PPE.[26] Rezaee et al. also mentioned the importance of controlling infectious diseases as a competency for medical students in disaster management.[13]
Theme 3 and 4: Demonstrating effective behavior and determining the meta-competencies
According to the scores, the third and fourth themes were “demonstrating effective behavior” and “determining the meta-competencies,” respectively. Since competency-based medical education has been put on the agenda, re-evaluation of the traditional curriculum has been of paramount concern for many medical universities.[27] This paradigm emphasizes competency achievement rather than fixed-time education and also underlines the importance of re-examining the curriculum in order to meet population health needs.[28] Many competency-based frameworks have been proposed since the representation of outcome-based education in 1999 by Harden et al. However, what they all have in common is the emphasis on meta-competencies and appropriate behavior of a physician in addition to medical knowledge.[28,29,30] Our study has provided 17 competencies related to the second and third circles in Dundee's three-circle model.[15] Therefore, according to experts’ opinion, students as future physicians should have abilities beyond diagnosing and treating the disease during the current pandemic. For instance, the ability to inform people with accurate information about COVID-19, the ability to manage patients infected with SARS-CoV-2, and the ability to solve the conflict of risk of being infected with the virus and the duty to treat patients are vital competencies which should be acquired by medical students.
Many medical centers around the world depend on medical students and residents to provide services to patients. In fact, they are at the forefront of combat against the COVID-19. Thus, they have to be competent in order to fight against pandemics. Faculty members should use diverse educational methods to teach undergraduate students and prepare them for effective practice. It should also be considered that if medical students are adequately trained, they can help the health-care system in times of crisis.
Limitations and implications
As a limitation, this study did not provide detailed courses and required teaching contents. An issue that emerges from the findings in participants’ viewpoints is that expanding the number of critical competencies to be learned by medical students during the pandemic may inhibit them from learning more requisite ones. Therefore, although all of these competencies can be beneficial, considering all of them as a core competency may distract us from teaching more critical competencies, and it may make students less prepared to face the pandemic. We suggest that further research should address the determination of phase, course, and lecture outcomes precisely to build a rigorous framework for curriculum development. Furthermore, after the curriculum implementation, a comprehensive evaluation should be done with all stakeholders’ participation to investigate the efficacy and eliminate the shortcomings of the training program.
Conclusions
This study was conducted to identify the required competencies for medical students to confront a pandemic. These competencies should be included in the educational curriculum to empower them to practice effectively and safely. It is essential to teach the students a diversity of competencies, not only the knowledge required to diagnose and treat the patients, but also the way to perform the tasks effectively. We encourage medical faculties to look at the present situation as a unique opportunity of transition from traditional time-based education toward competency-based education. Especially after the cancellation of in-person training and online training utilization, it is critical to ensure their future practice competency by taking advantage of “assessment for learning” where assessment goes hand in hand with education.[31,32] This research can enhance our understanding of the medical students’ role and the essence of paradigm shift from time-based to competency-based training.
Financial support and sponsorship
Vice-Chancellor of research at Shiraz University of Medical Sciences financially supported this study (grant no: 20045).
Conflicts of interest
There are no conflicts of interest to declare.
Acknowledgment
The authors would like to thank all of the faculty members and students who participated in this study and also Center for Development of Clinical Research of Nemazi Hospital and Dr. Nasrin Shokrpour for editorial assistance.
References
- 1.Mian A, Khan S. Medical education during pandemics: A UK perspective. BMC Med. 2020;18:100. doi: 10.1186/s12916-020-01577-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bhaumik S, Moola S, Tyagi J, Nambiar D, Kakoti M. Community health workers for pandemic response: A rapid evidence synthesis. BMJ Glob Health. 2020;5:e002769. doi: 10.1136/bmjgh-2020-002769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hsu EB, Thomas TL, Bass EB, Whyne D, Kelen GD, Green GB. Healthcare worker competencies for disaster training. BMC Med Educ. 2006;6:19. doi: 10.1186/1472-6920-6-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Frank JR, Snell L, Englander R, Holmboe ES ICBME Collaborators. Implementing competency-based medical education: Moving forward. Med Teach. 2017;39:568–73. doi: 10.1080/0142159X.2017.1315069. [DOI] [PubMed] [Google Scholar]
- 5.Aslan D, Sayek İ. We need to rethink on medical education for pandemic preparedness: Lessons learnt from COVID-19. Balkan Med J. 2020;37:178–9. doi: 10.4274/balkanmedj.galenos.2020.2020.4.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Emanuel EJ. The lessons of SARS. Ann Intern Med. 2003;139:589–91. doi: 10.7326/0003-4819-139-7-200310070-00011. [DOI] [PubMed] [Google Scholar]
- 7.Frank JR, Snell LS, Cate OT, Holmboe ES, Carraccio C, Swing SR, et al. Competency-based medical education: Theory to practice. Med Teach. 2010;32:638–45. doi: 10.3109/0142159X.2010.501190. [DOI] [PubMed] [Google Scholar]
- 8.Frank JR, Mungroo R, Ahmad Y, Wang M, De Rossi S, Horsley T. Toward a definition of competency-based education in medicine: A systematic review of published definitions. Med Teach. 2010;32:631–7. doi: 10.3109/0142159X.2010.500898. [DOI] [PubMed] [Google Scholar]
- 9.Thomas PA, Kern DE, Hughes MT, Chen BY. Curriculum Development for Medical Education: A Six-Step Approach. Baltimore, USA: JHU Press; 2016. [DOI] [PubMed] [Google Scholar]
- 10.Rose S. Medical student education in the time of COVID-19. JAMA. 2020;323:2131–2. doi: 10.1001/jama.2020.5227. [DOI] [PubMed] [Google Scholar]
- 11.Sani I, Hamza Y, Chedid Y, Amalendran J, Hamza N. Understanding the consequence of COVID-19 on undergraduate medical education: Medical students’ perspective. Ann Med Surg. 2020;58:117–9. doi: 10.1016/j.amsu.2020.08.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gill D, Whitehead C, Wondimagegn D. Challenges to medical education at a time of physical distancing. Lancet. 2020;396:77–9. doi: 10.1016/S0140-6736(20)31368-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rezaee R, Peyravi M, Ahmadi Marzaleh M, Khorram-Manesh A. Needs assessment for standardized educational program for Iranian medical students in crisis and disaster management. J Adv Med Educ Prof. 2019;7:95–102. doi: 10.30476/JAMP.2019.44713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tabari P, Amini M, Moosavi M. Lessons learned from COVID-19 epidemic in Iran: The role of medical education. Med Teach. 2020;42:833. doi: 10.1080/0142159X.2020.1754376. [DOI] [PubMed] [Google Scholar]
- 15.Harden RM. AMEE Guide No.14: Outcome-based education: Part 1-An introduction to outcome-based education. Med Teach. 1999;21:7–14. doi: 10.1080/01421599978951. [DOI] [PubMed] [Google Scholar]
- 16.Ayre C, Scally AJ. Critical values for Lawshe's content validity ratio: Revisiting the original methods of calculation. Meas Eval Couns Dev. 2013;47:79–86. [Google Scholar]
- 17.Keeney S, McKenna H, Hasson F. The Delphi Technique in Nursing and Health Research. West Sussex, UK: Wiley-Black-well; 2011. [Google Scholar]
- 18.Jasper EH, Wanner GK, Berg D, Berg K. Implementing a disaster preparedness curriculum for medical students. South Med J. 2017;110:523–7. doi: 10.14423/SMJ.0000000000000681. [DOI] [PubMed] [Google Scholar]
- 19.Ingrassia PL, Foletti M, Djalali A, Scarone P, Ragazzoni L, Corte FD, et al. Education and training initiatives for crisis management in the European Union: A web-based analysis of available programs. Prehosp Disaster Med. 2014;29:115–26. doi: 10.1017/S1049023X14000235. [DOI] [PubMed] [Google Scholar]
- 20.Su T, Han X, Chen F, Du Y, Zhang H, Yin J, et al. Knowledge levels and training needs of disaster medicine among health professionals, medical students, and local residents in Shanghai, China. PLoS One. 2013 Jun 24;8(6):e67041. doi: 10.1371/journal.pone.0067041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Barrimah I, Adam I, Al-Mohaimeed A. Disaster medicine education for medical students: Is it a real need? Med Teach. 2016;38(Suppl 1):S60–5. doi: 10.3109/0142159X.2016.1142515. [DOI] [PubMed] [Google Scholar]
- 22.Ravi RC. Lockdown of colleges and universities due to COVID-19: Any impact on the educational system in India? J Educ Health Promot. 2020;9:209. doi: 10.4103/jehp.jehp_327_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Goh PS, Sandars J. A vision of the use of technology in medical education after the COVID-19 pandemic. MedEdPublish. 2020;9:49. doi: 10.15694/mep.2020.000049.1. doi: 10.15694/mep. 2020.000049.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Alipour F, Shahvari Z, Asghari F, Samadi S, Amini H. Educational system defects and observing professional behavior: A qualitative study. J Educ Health Promot. 2019;8:162. doi: 10.4103/jehp.jehp_22_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cook TM. Personal protective equipment during the coronavirus disease (COVID) 2019 pandemic – A narrative review. Anaesthesia. 2020;75:920–7. doi: 10.1111/anae.15071. [DOI] [PubMed] [Google Scholar]
- 26.Organization WH. Rational Use of Personal Protective Equipment for Coronavirus Disease (COVID-19) and Considerations During Severe Shortages: Interim Guidance, 6 April 2020. World Health Organization; 2020. [Google Scholar]
- 27.Nousiainen MT, Caverzagie KJ, Ferguson PC, Frank JR ICBME Collaborators. Implementing competency-based medical education: What changes in curricular structure and processes are needed? Med Teach. 2017;39:594–8. doi: 10.1080/0142159X.2017.1315077. [DOI] [PubMed] [Google Scholar]
- 28.Park YS, Hodges BD, Tekian A. Evaluating the paradigm shift from time-based toward competency-based medical education: Implications for curriculum and assessment. In: Wimmers PF, Mentkowski M, editors. Assessing Competence in Professional Performance across Disciplines and Professions. Cham: Springer International Publishing; 2016. pp. 411–25. [Google Scholar]
- 29.Swing SR. The ACGME outcome project: Retrospective and prospective. Med Teach. 2007;29:648–54. doi: 10.1080/01421590701392903. [DOI] [PubMed] [Google Scholar]
- 30.Frank JR, Danoff D. The CanMEDS initiative: Implementing an outcomes-based framework of physician competencies. Med Teach. 2007;29:642–7. doi: 10.1080/01421590701746983. [DOI] [PubMed] [Google Scholar]
- 31.Lockyer J, Carraccio C, Chan MK, Hart D, Smee S, Touchie C, et al. Core principles of assessment in competency-based medical education. Med Teach. 2017;39:609–16. doi: 10.1080/0142159X.2017.1315082. [DOI] [PubMed] [Google Scholar]
- 32.Santen SA, Ryan MS, Coates WC. What can a pandemic teach Us about competency-based medical education? AEM Educ Train. 2020;4:301–5. doi: 10.1002/aet2.10473. [DOI] [PMC free article] [PubMed] [Google Scholar]


