Abstract
Background:
Patients with kidney failure are exposed to a surfeit of new information about their disease and treatment, often resulting in ineffective communication between patients and providers. Improving the amount, timing, and individualization of information received has been identified as a priority in in-center hemodialysis care.
Objective:
To describe and explicate patient, caregiver, and health care provider perspectives regarding challenges and solutions to information transfer in clinical hemodialysis care.
Design:
In this multicenter qualitative study, we gathered perspectives of patients, their caregivers, and health care providers conducted through focus groups and interviews.
Setting:
Five Canadian hemodialysis centers: Calgary, Edmonton, Winnipeg, Ottawa, and Halifax.
Participants:
English-speaking adults receiving in-center hemodialysis for longer than 6 months, their caregivers, and hemodialysis health care providers.
Methods:
Between May 24, 2017, and August 16, 2018, data collected through focus groups and interviews with hemodialysis patients and their caregivers subsequently informed semi-structured interviews with health care providers. For this secondary analysis, data were analyzed through an inductive thematic analysis using grounded theory, to examine the data more deeply for overarching themes.
Results:
Among 82 patients/caregivers and 31 healthcare providers, 6 main themes emerged. Themes identified from patients/caregivers were (1) overwhelmed at initiation of hemodialysis care, (2) need for peer support, and (3) improving comprehension of hemodialysis processes. Themes identified from providers were (1) time constraints with patients, (2) relevance of information provided, and (3) technological innovations to improve patient engagement.
Limitations:
Findings were limited to Canadian context, English speakers, and individuals receiving hemodialysis in urban centers.
Conclusions:
Participants identified challenges and potential solutions to improve the amount, timing, and individualization of information provided regarding in-center hemodialysis care, which included peer support, technological innovations, and improved knowledge translation activities. Findings may inform the development of interventions and strategies aimed at improving information delivery to facilitate patient-centered hemodialysis care.
Keywords: hemodialysis, quality of care, information, qualitative research, patient-oriented research
Abrégé
Contexte:
Les patients atteints d’insuffisance rénale reçoivent beaucoup de nouvelles informations sur leur maladie et leurs traitements, ce qui engendre de fréquents problèmes de communication avec leurs fournisseurs de soins. Parmi les priorités des soins d’hémodialyse en centre hospitalier, on compte notamment des améliorations quant au volume et à la personnalisation des informations reçues, de même qu’en regard du moment de leur transmission.
Objectifs:
Présenter le point de vue des patients, de leurs aidants et des fournisseurs de soins sur les enjeux liés au transfert de l’information entourant les soins cliniques d’hémodialyse, et sur de possibles solutions pour y remédier.
Type d’étude:
Étude qualitative multicentrique. Des entrevues et des groupes de discussion ont permis de recueillir les points de vue des patients, de leurs aidants et des fournisseurs de soins.
Cadre:
Cinq centres canadiens d’hémodialyse: Calgary, Edmonton, Winnipeg, Ottawa et Halifax.
Participants:
Des adultes anglophones recevant des traitements d’hémodialyse en centre hospitalier depuis au moins six mois, leurs aidants et les fournisseurs de soins des centres d’hémodialyse participants.
Méthodologie:
Entre le 24 mai 2017 et le 16 août 2018, des entrevues et groupes de discussion impliquant des patients et leurs aidants ont permis de recueillir des données qui ont ensuite informé des entrevues semi-structurées avec les fournisseurs de soins. Une méthode d’analyse thématique inductive reposant sur les faits a été employée pour procéder à une analyse secondaire des données afin de les examiner plus en profondeur et d’en tirer des thèmes généraux.
Résultats:
Les entretiens et groupes de discussion, qui ont impliqué 82 patients/aidants et 31 fournisseurs de soins, ont permis de dégager six thèmes principaux. Les thèmes dégagés par les patients/aidants étaient les suivants: (i) le sentiment d’être submergé au début des soins d’hémodialyse; (ii) le besoin de soutien des pairs; et (iii) le besoin de mieux comprendre les processus d’hémodialyse. Les fournisseurs de soins ont quant à eux souligné (i) des contraintes de temps avec les patients; (ii) la pertinence de l’information fournie; et (iii) les innovations technologiques pouvant améliorer l’engagement des patients.
Limites:
Les résultats se limitent au contexte canadien, aux locuteurs anglophones et aux personnes recevant des traitements d’hémodialyse en centre urbain.
Conclusion:
Les participants ont exposé des enjeux liés à la transmission d’informations sur les soins d’hémodialyse en centre hospitalier; notamment en ce qui concerne la quantité d’informations reçues, la personnalisation de celles-ci et le moment opportun pour les transmettre. Ils ont également énoncé de possibles solutions à ces enjeux, notamment des améliorations en matière de soutien des pairs, d’innovations technologiques et d’activités d’application des connaissances. Ces résultats pourraient guider l’élaboration de stratégies et d’interventions visant à mieux transmettre l’information et à faciliter la prestation de soins d’hémodialyse centrés sur le patient.
Introduction
A focus on patient-centered care in chronic disease management has prompted clinical research to improve outcomes that align with the priorities of patients with kidney failure requiring kidney replacement therapy. 1 Hemodialysis care requires patients and their caregivers to make complex decisions regarding their treatment based on their individual health and social circumstances. In previous studies, individuals with kidney disease undergoing renal replacement therapy perceived existing educational resources to be incompatible with their needs as the material did not meet their health literacy levels2,3 and did not effectively prepare them for the realities of being on dialysis.4-6 Individuals with kidney disease have also previously identified the need for research to answer the following question: “How can I get more information about my health, so that I can better manage my condition?” 7 highlighting that knowledge is a tool of empowerment that encourages greater patient involvement in care pathways. 8 Thus, improving information transfer is integral to improving in-center hemodialysis care.
As part of Canada’s strategy for Patient-Oriented Research (SPOR), the Can-SOLVE CKD (Canadians Seeking Solutions to Overcome Chronic Kidney Disease Network) was established to further participatory action research in the field and promote the implementation of findings into clinical practice. 9 The Can-SOLVE CKD Triple I project is a mixed-methods study in which researchers, clinicians, and patient partners work collaboratively in multiple sites across Canada to advance the quality of care and health outcomes for individuals receiving in-center hemodialysis. 10 The 3 “I’s” in the study title refer to the original framework for the Triple I study that aims to improve in-center hemodialysis care by addressing key challenges to information provided to patients about their health and health care, interactions with health providers, and individualization of care in in-center hemodialysis.10,11 The objective of this article is to identify challenges and potential solutions to accessing and delivering information in in-center hemodialysis as identified by patients, caregivers, and health providers.
Methods
This qualitative study was conducted using focus groups and interviews with individuals receiving in-center hemodialysis, their caregivers, and health care providers in 5 academic centers across Canada (Calgary, Edmonton, Winnipeg, Ottawa, and Halifax) between May 24, 2017, and August 16, 2018. Detailed methodology, participant selection, and data collection for phase 1 of the Triple I project have been previously described by Rossum et al and Sass et al.10,11 This planned secondary analysis was undertaken in 2020 by the same researchers involved in the original study to focus on data from the parent study that appeared important and warranted further analysis. 12 In our primary analysis, we summarized and organized the data into the 3 Triple I categories (Information, Individualization, Interaction), which fit study objectives in previous phases of the study using qualitative description and content analysis. 10 For this secondary data analysis, we used the same data set but chose a different methodological approach, grounded theory, as we looked at the data more deeply for overarching themes that spoke to information transfer in hemodialysis care. With grounded theory, the data inform new concepts and theories, rather than fitting within an existing theoretical framework. 13 Our goal using grounded theory was not to situate the findings within a theoretical framework, but rather to stay as close as possible to the data to identify and describe overarching challenges and solutions to information transfer as identified by patients, caregivers, and health providers.
The study protocol was approved by research ethics boards at the University of Manitoba for the main site and at the 4 other participating institutions (University of Calgary, University of Alberta, University of Ottawa, and Nova Scotia Health Authority, Halifax). We followed the consolidated criteria for reporting qualitative research (COREQ) checklist. 14
Patient Engagement
Patient partners form an integral part of the research team. A patient advisory group of 4 patient partners was established at the project’s inception, providing guidance and insight throughout all stages of the research, from proposal development and study design, through to interview guide development and data analysis. 10 In addition, 2 of the patient partners are members of the Can-SOLVE Indigenous Peoples’ Engagement and Research Council (IPERC), ensuring the project identifies issues and solutions that are relevant to Indigenous peoples.
Participant Selection
Individuals receiving in-center hemodialysis for at least 6 months were eligible for inclusion if they were aged 18 years and older and able to provide written informed consent. Participants were excluded if they were unable to communicate effectively in English. Patients were initially approached to participate in the study by hemodialysis unit staff. A study information letter was also distributed and posted at participating hemodialysis clinics.
At the patient recruitment visit, consenting patients were asked by study staff whether they have a caregiver who may also be interested in participating. If so, these caregivers were approached to participate. Caregivers were defined as a family member or significant person in the patient’s life who is aware of the patient’s illness and assists with care provision.
Health care providers, including nephrologists, nurses, and allied health professionals with experience in hemodialysis, were recruited by email or in person to participate in semi-structured interviews. To promote diversity in health care roles, we used a combination of purposive and snowball sampling by asking recruited health care providers to recommend colleagues who may be interested in participating.
Data Collection
Interview and focus group guides were developed with input from patient partners, existing literature, and the Ottawa Hospital Research Institute needs assessment guidelines. 15 In-person focus groups ranging from 90 to 120 min in duration were conducted with consenting patients and caregivers. Individual semi-structured interviews lasting 30 to 60 min took place in person at hemodialysis units with patients who were unable to participate in focus groups. 11 The challenges and solutions to hemodialysis care identified by patients and caregivers in the focus groups informed the development of interview questions for the semi-structured interviews with health care providers. Providers were asked to identify barriers or facilitators to the implementation of solutions identified by the patients/caregivers. Health care provider interviews lasted 30 to 40 min and were conducted face to face or by telephone. Focus groups and interviews were moderated by 2 members of the study team with training and experience in qualitative research methods (K.S., research assistant and J.F., senior study member with expertise in qualitative methodology) with no preexisting relationships with participants. Audio recordings from all focus groups and interviews were transcribed verbatim. Field notes taken by the interviewer and/or a second member of the study team (for focus groups) supplemented the transcripts.
Data Analysis
In phase 1 of the Triple I project, the data were divided into the 3 “I” categories, delineated by whether it related to interaction, information, or individualization; in addition, the data were divided to distinguish the perspectives of patients and their caregivers, from that of health care providers. 11 For ease of reading, these perspectives are presented in this article as “patients” (identified as P in quotes) and “providers” (identified as HCP in quotes). A qualitative inductive thematic analysis using a grounded theory methodology 13 was conducted by 2 researchers with training and experience in qualitative research methods (P.F.T. and M.D.T.). Themes were derived inductively out of a systematic familiarization with the data. Researchers read through the transcripts while simultaneously taking notes, highlighting and flagging passages that were recurrent in content. 13 From these points, it became possible to tease out how the ideas are connected and extract common themes among the narratives. As the themes began to emerge, overarching themes and subthemes were identified, as well as how the themes interacted and intersected with one another from the 2 perspectives (of both patients and providers). The themes were agreed upon with the investigative team, including patient partners. The data were further analyzed to elicit challenges and solutions identified by patients and providers relating specifically to the themes.
Results
Across all sites, 113 individuals participated in 44 interviews and 8 focus groups. Detailed participant demographics have been previously reported (see Table 1). 11 A total of 47 patients and 18 caregivers participated in focus groups in Winnipeg, Halifax, Ottawa, and Edmonton. In Calgary (n = 13) and Edmonton (n = 4), patient interviews supplemented focus groups. The mean age of participating patients was 60 (interquartile range [IQR]: 51-74) years and caregiver age was 64.5 (IQR: 56-68) years. About 33% of patients and 72% of caregivers were women Participating health care providers (n = 31) were 77% women and had been in practice for a median of 13 (IQR: 6-16) years.
Table 1.
Participant Demographic Characteristics (N = 113).
| Patients | Caregivers | Health care providers | |
|---|---|---|---|
| Overall participation, n (%) | 64 (57) | 18 (16) | 31 (27) |
| Sex | |||
| Female | 21 (33) | 13 (72) | 24 (77) |
| Male | 43 (67) | 5 (28) | 7 (23) |
| Age (years) | |||
| Median (IQR) | 60 (51-74) | 65 (56-68) | — |
| Location, n (%) | |||
| Calgary | 13 (20) | 0 (0) | 8 (26) |
| Edmonton | 14 (22) | 3 (17) | 3 (10) |
| Winnipeg | 22 (34) | 7 (39) | 13 (42) |
| Ottawa | 3 (5) | 1 (6) | 3 (10) |
| Halifax | 12 (19) | 7 (39) | 4 (13) |
| Time since initiating in-center hemodialysis (years) | |||
| Median (IQR) | 13 (1-6) | — | — |
| Years in clinical practice | |||
| Median (IQR) | — | — | 13 (6-16) |
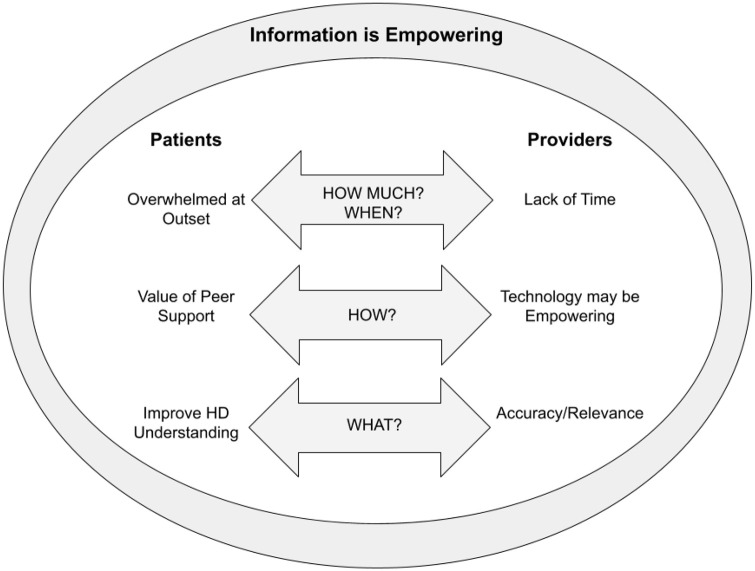
The overarching theme revealed in the data is the concept that knowledge is empowering for patients and their caregivers. It is generally agreed that improved knowledge of one’s health condition and treatment facilitates an improvement in health literacy levels, leading to a greater sense of autonomy, independence, and control over one’s health. Three major patient/caregiver-related themes emerged from the data: (1) feeling overwhelmed at the outset of hemodialysis care, (2) the need for peer support/education, and (3) improving patient understanding of the hemodialysis process. Three major provider-related themes emerged from the data: (1) lack of time to spend with patients, (2) ensuring accuracy and relevance of information provided, and (3) the use of technology may improve patient engagement. Additional key topic areas, along with respective challenges and solutions to improve information in hemodialysis care that were identified by participants as well as selected examples, are presented in Table 2.
Table 2.
Key Topic Areas and Identified Challenges and Solutions in Hemodialysis Information Delivery.
| Topic | Challenge | Solution |
|---|---|---|
| Nutrition | Lack of information about the implications of one’s potassium, sodium, and phosphorus levels being abnormal. Information about nutrition and diet is designed in a one size-fits-all manner: “I’m a vegetarian, they said, ‘Your protein is low.’ So I said, ‘What should I take in protein?’ If I take lentils the phosphorus gets high. So they have no solution for that.” (ID P20) |
- Recipe books - Personalized cooking classes and videos - Nutrition and diet apps - Update diet charts to consider ethnicity and dietary diversity |
| Medication | Insufficient details about the side effects of prescribed medications: “I mean, I’d like to know the side effects of the medication that’s going to be anti-rejection.” (ID P22) |
- Verbal and written information about the side effects of medications - Share database of medications that interact with, are contraindicated, or need to be modified for dialysis with family doctors |
| Dialysis modalities | Lack of education on the pros and cons of each modality and the care involved in looking after one’s access: “They were pushing me towards peritoneal and I never even knew what both [modalities] were. I didn’t know anything about them, so I just, ok, I’ll do peritoneal.” (ID P2) |
- Information on the most suitable type of dialysis based on a person’s values and lifestyle - Connect with patients who have been through the decision-making process |
| Travel aid | The amount of preparation involved in arranging out-of-town dialysis both within and across provinces is perceived as lengthy and bureaucratic: “It’s extremely difficult to arrange that. You have to get so much bloodwork and sometimes they can say no, and that ruins your whole vacation and even going there, it’s hard. It would be nice if it was easier, definitely.” (ID P11) |
- Reserved spot for travelers in units - Better support from social workers to coordinate travel arrangements between patients and units - Better patient histories from physicians to determine medical stability to travel |
| Symptom and pain management | Possible symptoms, side effects, and pain management of dialysis treatment is not adequate: “My first dialysis treatment, nobody said not to stand up . . . Well what’s the first thing you do when you get a cramp in your stomach? You stand up. Well, I stood up. Nobody said, sit down, so I passed out cold, in my chair.” (ID P4) |
- Distribute a fact sheet to patients with Frequently Asked Questions - Information on common symptoms and how to manage them, for example, cramps, pruritus, fatigue, nausea, altered taste, restless legs, fluid restriction, and so on. - Information tailored for patients with diabetes and other underlying conditions |
| Transplant | Lack of transparency about how the transplant list works and lack of updates regarding where individuals are on the list and how to prepare for transplant: “I had a close friend and two other donors willing to donate a live donor . . . he had phoned and they didn’t get back to him for weeks on end and apparently they didn’t have staffing to return calls and they were very, very slow with the process and all the tests.” (ID P10) |
- Clear information on eligibility criteria to be on transplant list - A road map informing individuals of how long they should expect to be on the list based on blood type along with nutrition tips to prepare for transplant - Timely assessments of potential donors - More information about the national Kidney Paired Donation (KPD) program |
Overwhelmed at outset
Challenges
Patients expressed the importance of feeling as prepared as possible to begin hemodialysis treatments. Many patients described the amount of information provided to them on handouts, binders, and through one-on-one interactions as overwhelming, while other patients reported receiving insufficient information. A lack of familiarity with treatment procedures, coping with major life changes, and new clinical terminology makes many patients unable to retain the information they receive when initiating hemodialysis. As one patient described, “We were kind of shell-shocked. So, we didn’t know the questions to ask, and then down the road there was no kind of follow-up . . . which would have been helpful” (ID P5).
Providers shared the concern of overloading patients with information at initiation of hemodialysis therapy, and note they are cautious to not convey information all at once. A provider explained a recurrent barrier in reaching patients: “often we are seeing patients who are really quite uremic and feeling unwell . . . they are not in a headspace where they can take in that information” (ID HCP 5). Providers explained that hemodialysis education programs are well established at various sites, but existing resources must be modified to be more patient-friendly.
Solutions
Many patients expressed that they would prefer to receive information in a gradual manner accounting for their circumstances and learning preferences. In addition to one-on-one appointments with providers, patients suggested that units offer more group activities to ease overwhelm such as facility tours, meet and greet events explaining the process and unit setup, orientation sessions with “welcome to the unit” packages, and the availability of videos in multiple languages. As one patient suggested, “We need a classroom . . . We have the time to come, they should give us a one hour or half hour class, any doctor or any nurse, they can tell you how the dialysis works” (ID P6).
Providers suggested designing an introduction to hemodialysis information package for patients according to their individual needs and co-morbidities. A provider shared,
It needs to be simple and appropriate to where the patients are at . . . we were talking about a patient care map, a road map . . . if things are going smooth on dialysis, it’s pretty simple, but if a patient, they have trouble with a foot ulcer or they are struggling with their access . . . What is the map of their care? What can they expect? (ID HCP6)
Need for peer support/education and ensuring accuracy and relevance of information
Challenges
Patients and caregivers describe the critical value to learning and sharing with their peers in various forms and capacities. “I learn more from the patients in the waiting room than I do from my team. That’s the truth, and everybody that sits in that waiting room will tell you the same thing” (ID P7). From the providers’ perspective, the concept of peer support and peer education is a valuable resource for patients and their families. However, many providers deem that information must be “filtered” to ensure accuracy and relevance to the specific needs of the patient. Providers express concern that patients and caregivers could share information that is not accurate for all hemodialysis patients, potentially causing harm or confusion. Patient confidentiality was also identified as a barrier as providers are limited in their ability to connect patients with each other.
Solutions
Peer-based support may take many forms and must be adaptable to various settings and levels of accessibility. Patients provided numerous examples of ways that peer support can meet their needs, including one-on-one sharing, a buddy system, group support, online, in person, literature written by patients for patients, group meetings, family support, health advocates, videos, phone calls, monthly newsletters, and patient forums. Noticing that peer-to-peer education already occurs in waiting rooms and the hemodialysis unit, providers also recognize the necessity of this form of support and knowledge sharing. Both providers and patients identified that some level of oversight and formalization is useful as it has the potential to have a greater reach, better accuracy of information, and is more likely to have better uptake and promotion by providers. As one provider explains,
You want them to be [paired] with a patient that’s had a holistic experience. They’ve tried different dialysis modalities, different accesses . . . you’ve got to make sure that whatever they are providing, the information, not all of it is subjective, and some of it is objective. (ID HCP8)
Improving understanding of hemodialysis process and machine
Challenges
A patient described how the machine sounds may trigger stress: “Because when the machine alarms, we say, oh something wrong is happening because we are not educated” (ID P20). The physiology of hemodialysis is complex and many patients may not be interested in learning about all of the details; however, there is a common sense of feeling disempowered by the unknown aspects of the machine that they are connected to:
All people coming here, sitting on the chairs, doing their dialysis, going home, don’t know what is happening. (ID P16)
Solutions
Patients wanted more training to understand the hemodialysis process, including the significance of the machine displays and alarms. Patients specifically highlighted the importance of understanding how the machine works, how vascular access is connected to the machine, how it removes fluid, and how hemodialysis impacts blood pressure. By tracking and monitoring body changes and understanding hemodialysis machine displays and function, patients may become more engaged in their health. A patient suggested,
Have that brand new patient that is not on the machine . . . to come at the same time as the dialysis patients and have them sit with you and watch you get connected, watch you go through your run. (ID HCP16)
The use of technology to enhance information delivery
Challenges
Providers pointed out several barriers to implementing information resources through the use of computers, tablets, and smartphones. Providers linked socioeconomic factors to technological accessibility and use, thus disadvantaging patients with lower socioeconomic status. Considering the large proportion of elderly patients on dialysis, providers identified lower technology literacy among this population as a challenge. Providers acknowledged that patients may gain a sense of independence accessing information on the Internet, but that it will not benefit all patients. A provider said, “You shouldn’t necessarily assume using technology will improve people’s outcomes, but you could imagine that there may be specific things that technology could be useful for” (ID HCP19). Patients did not extensively discuss challenges to accessing technological devices. Some individuals pointed out not being tech proficient and feeling leery to access information on the Internet due to the unknown reliability of the information: “You need to filter on the internet . . . you have to be really, really careful what website you are going into” (ID P7).
Another vital aspect to consider when developing educational content in both low- and high-tech delivery modalities is ensuring that the information is suitable and responsive to the culturally diverse dialysis populations. A provider reiterated a pressing challenge,
One is language . . . In [this unit] we have a very large Aboriginal population . . . so trying to make sure that we have things, let’s say in Cree for example . . . also trying to make sure that they are culturally appropriate . . . there might be some traditional healing that might be better incorporated into our pamphlets. (ID HCP17)
Solutions
Providers identified solutions to mitigate any disparity in access to online information among patients. There are ways to make the content more versatile, such as adjusting font size, adding voice command capabilities, and embedding videos. As a provider highlighted, “Just because someone is disabled doesn’t mean they can’t use technology” (ID HCP14). Patients indicated that while some individuals may not be well versed in technology, the use of technology plays a crucial role in information delivery. Training sessions could be offered to individuals who are unfamiliar with tablet/computer use to fill the gaps in accessibility. A patient suggested, “I don’t know too much about computers, and if you could get a group session . . . where someone teaches us about computers” (ID P25).
Time constraints
Challenges
The issue of time was a recurrent theme among providers, who pointed out that they must be efficient with the delivery of care to fulfill their duties and see all of their patients. As a result, providers felt that they must sacrifice getting to know their patients’ individual backgrounds, acknowledging their cultural context and adapting to language barriers. Nephrologists indicated that when patients ask questions or bring up issues that could be better directed to their GP or other health care providers, they find it time-consuming and unnecessarily taking up resources:
I think the problem is that we don’t have the time to spend. There isn’t that longitudinal relationship with the average patient you are rounding on and as a consequence you don’t know them well enough to really know what’s going on and get at those issues. (ID HCP3)
Concerns were raised about initiating and delivering new educational programs in the unit, due to the training and time required. Patients also recognized the time constraints faced by their providers; however, for patients who must spend extended periods of time receiving hemodialysis treatment, usually 4 hours/day 3 days/week, they would have ample time to participate in education/training.
Solutions
Patients and providers discussed possible solutions to providing adequate information to patients under the existing time constraints, such as improving patient advocacy with the support of a patient care coordinator and/or patient advocate. Coordinating care between providers may also alleviate time constraints by ensuring the patient’s voice is heard and questions are answered by the appropriate health care provider. Despite facing strict time constraints, it is critical for providers to introduce themselves, what their role in the patients’ care is, and to ensure they are providing culturally sensitive and culturally/linguistically appropriate care: “I think the time constraints put on us as we go around are such that we are going to focus on urgent medical issues and not so much on things I would assume are more important to patients” (ID HCP9).
Discussion
This multicenter study revealed 3 key opportunities to improve information for patients receiving in-center hemodialysis in Canada: refining the method of information delivery (ie, how), the quantity/quality of information (ie, how much/what), and the timing (ie, when) of when information is provided. Using these thematic analysis findings, we extrapolated this concept of information delivery to identify how provider and patient themes intersect with one another, as depicted in Figure 1.
Figure 1.
Thematic schema.
The overarching theme that knowledge of one’s health is empowering is consistent with existing literature on patient-centered care and patient engagement. Arming patients with information regarding their treatment holds transformative power to improve care experiences for overall health and well-being.2,16,17 Our study identified the need for educational resources to be more patient-friendly, interactive, culturally appropriate, and available in multiple languages, supporting previous studies indicating a disconnect between patients’ health literacy levels and the readability of end-stage kidney disease (ESKD) material in the United States, United Kingdom, and Australia. 3 Health educators must prioritize the accessibility and readability of health educational material.
Patients generally pointed out that they felt ill prepared to begin hemodialysis. They were overwhelmed due to the large volume of information provided at outset while also processing their diagnosis and need for renal replacement therapy. Researchers have previously identified the difficulties involved with the transition to dialysis in view of the level of complexity involved in decision-making combined with a struggle to accept the diagnosis and an inability to uptake information due to fear and anxiety related to hemodialysis. 18 Patients in our study suggested hemodialysis unit tours, a roadmap, or a “what to expect” handbook/website/video as helpful solutions in preparing for their treatment pathways and relieving the initial fear and uncertainty that follow the diagnosis. Recent tools to assess key psychological and interpersonal factors in patients transitioning to dialysis may help to further individualize educational needs.19,20
In addition, self-management strategies encourage patients to take an active role in their care. A self-management program that focused on self-efficacy through improving problem-solving skills, building partnerships between patients and providers, mental health and lifestyle support, and coping with challenges related to hemodialysis has been shown to improve quality of life. 21 The program had no effect on cognitive abilities nor social interactions in 53 individuals on maintenance hemodialysis. 21 In another study, a WeChat program designed for patients to communicate with nurses through text, video, and audio messages showed positive outcomes on self-management, self-efficacy, and treatment knowledge. 22 A systematic review of CKD educational randomized control trials RCTs involving dialysis patients indicated most studies focused on fluid intake, diet, exercise, and psychological adaptation. 23 Although some interventions have shown successful and promising results, studies largely lacked the required level of rigor.23,24 From a patient perspective, an integrative review underscored the urgency of participatory processes in the development of self-management strategies as existing programs were found to be largely incompatible with the needs and preferences of patients. 25
We identified that peer-led learning is viewed by patients as critical to the flow of information and the development of social supports. Previous studies have also identified that patients value the opportunity to obtain relevant information from those who have experienced similar physical and psychological challenges23,26 and have demonstrated the effectiveness of peer-led education in chronic disease self-management and improving patient experience.27-29 In a quasi-experimental pilot project that provided peer mentors with 5 hours of training in the domains of ESKD knowledge, leadership, communication, distinguishing between medical information and advice, and confidentiality, mentees (n = 23) demonstrated increased knowledge, self-efficacy, perceived social support, and less missed hemodialysis treatments after 3 months. Knowledge, self-management, and social support also increased in peer mentors (n = 23). 30
In our study, providers agreed with the value of peer education, but cautioned that it must be considered in terms of the quality of information that is shared. Moderated peer support systems or support groups with nurse educators and care coordinators are potential solutions that address this concern. In a pilot study with culturally appropriate peer navigators (PNs), a Latina PN assisted Latino patients to navigate hemodialysis services, such as advance care planning, care coordination, dietary support, and mental health support. 31 Most individuals reported that PN guidance improved quality of life, enhanced emotional support, and assisted in key steps of the decision-making process. 31 Such programs could be tailored to specific ethnic groups in various geographical locations who face disproportionate rates of CKD and ESKD stemming from racial inequities.32-34 In another pilot program involving CKD patients, transplant referral rates substantially increased when a health care advocate such as a care coordinator provided transplant education and acted as a liaison. 35
The time constraints that providers perceive are a barrier to patient-centered care, as patients have stated that feeling appreciated by providers was a key aspect of receiving and retaining information.36,37 Although physicians agreed that an electronic platform where patients can access individualized information and health reports may reduce these constraints, some physicians were reluctant to adopt new systems. A recent pilot study highlighted the efficiency and effectiveness of an app to facilitate communication between nephrologists and hemodialysis patients. 38 In this study, despite demonstrated patient acceptance and utility of the app, nephrologists felt that the tool interrupted workflow, which was a barrier to adoption into clinical care. 38 Only 20% of patient participants used web-based technology prior to the study, thus emphasizing the need for technological literacy training and the possibility that such solutions may not be relevant to all persons receiving hemodialysis.38-40
Limitations of this study include that all participants were English-speaking and from urban in-center hemodialysis units in Canada. Thus, perspectives from diverse non-English-speaking ethnic groups were not captured in this analysis and findings may not be applicable in other cultures and settings. Importantly, in Canada, ESKD disproportionately affects Indigenous peoples, 41 who also experience systemic barriers, such as lack of clean water, housing insecurity, 42 lack of transportation options, and complex health coverage. 43 Further studies, working with Indigenous patient partners for insight and direction, are needed to understand the ways these factors intersect with information delivery in dialysis. In addition, the median dialysis vintage of study participants was 13 (IQR: 1-6) years. As such, study findings may not represent the perspectives of individuals who have recently initiated hemodialysis. As this is a secondary analysis, possible limitations which could not be avoided include the vintage of the data, the lack of detailed demographic data, and the combined analysis of patient focus group and interview data. However, we believe that conducting and analyzing interviews with individuals who were unwilling or unable to attend focus groups allowed us to include perspectives that may be different from that of patients and caregivers who attended focus groups. In addition, there has been little change in in-center hemodialysis practices and patterns over the time period as these data were initially collected. Findings still reflect common practices in in-center hemodialysis clinics as changes to health care delivery happen very slowly. 44
Strengths of our study include meaningful consultation with patient partners throughout all project stages from study design, development of interview and focus group guides, to analysis and implementation.10,11 The multicenter pan-Canadian participant sampling provides diverse perspectives from across the country.
Conclusions
Our findings reveal that information is a multifaceted concept and solutions aimed at improving hemodialysis information must be relevant and address the specific context of each patient to facilitate patient empowerment and engagement in their care. We identified challenges and potential solutions to improve information translation and delivery in hemodialysis care, including technological tools, care navigators, peer support programs, and orientation sessions. In subsequent phases of this project, we plan to test these solutions to address key challenges.10,11 In addition, we will use these results to develop a diverse catalog of information resources that in-center hemodialysis populations can access.
Acknowledgments
We thank patients, caregivers, and health care providers who participated in the study, hemodialysis in-center units, and their staff across the country and our patient partners for their valuable input and reflections.
Footnotes
Authors’ Note: All authors have contributed to the manuscript, provided critical revisions, and approved this submission. The results presented in this paper have not been published in whole or in part elsewhere.
Ethics Approval and Consent to Participate: The study protocol was approved by the research ethics board at the University of Manitoba for the main Winnipeg site (HS20494 [H2017:049]), as well as the research ethics boards at the 4 other participating institutions (University of Calgary, University of Alberta, University of Ottawa, and Dalhousie University). Informed consent was obtained from all participants.
Consent for Publication: All authors consent to publication.
Availability of Data and Materials: The data and materials are available from corresponding author upon reasonable request.
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: R.S, M.D.T., K.R., J.F., M.M., A.D., H.V., G.F., P.F.D.S., K.S., M.J., A.T., N.P., S.T., M.T., and C.B. declare that they have no relevant financial interests. Dr. Sood has received speaker fees from AstraZeneca. Dr. Tennankore has received advisory board and/or consulting fees from AstraZeneca, Otsuka, Jansen, and Baxter and unrestricted investigator-initiated grant funding from Astellas and Otsuka.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work is a project of the Canadians Seeking Solutions and Innovations to Overcome Chronic Kidney Disease (Can-SOLVE CKD) Network, which is supported by the Canadian Institutes of Health Research (CIHR) under Canada’s Strategy for Patient-Oriented Research Grant 20R26070. Dr. Tonelli is supported by a Foundation grant from the CIHR. Dr. Bohm is supported by the Manitoba Medical Services Foundation F.W. Du Val Clinical Research Professorship.
ORCID iDs: Matthew James  https://orcid.org/0000-0002-1876-3917
https://orcid.org/0000-0002-1876-3917
Karthik Tennankore  https://orcid.org/0000-0002-7919-6709
https://orcid.org/0000-0002-7919-6709
Stephanie Thompson  https://orcid.org/0000-0003-3109-6837
https://orcid.org/0000-0003-3109-6837
Clara Bohm  https://orcid.org/0000-0001-7710-7162
https://orcid.org/0000-0001-7710-7162
References
- 1. Molnar AO, Barua M, Konvalinka A, Schick-Makaroff K. Patient engagement in kidney research: opportunities and challenges ahead. Can J Kidney Health Dis. 2017;4:2054358117740583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bear RA, Stockie S. Patient engagement and patient-centred care in the management of advanced chronic kidney disease and chronic kidney failure. Can J Kidney Health Dis. 2014;1:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Morony S, Flynn M, McCaffery KJ, Jansen J, Webster AC. Readability of written materials for CKD patients: a systematic review. Am J Kidney Dis. 2015;65(6):842-850. [DOI] [PubMed] [Google Scholar]
- 4. Davis JL, Davison SN. Hard choices, better outcomes: a review of shared decision-making and patient decision aids around dialysis initiation and conservative kidney management. Curr Opin Nephrol Hypertens. 2017;26(3):205-213. [DOI] [PubMed] [Google Scholar]
- 5. Verberne WR, Konijn WS, Prantl K, et al. Older patients’ experiences with a shared decision-making process on choosing dialysis or conservative care for advanced chronic kidney disease: a survey study. BMC Nephrol. 2019;20(1):264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Finkelstein FO, Story K, Firanek C, et al. Perceived knowledge among patients cared for by nephrologists about chronic kidney disease and end-stage renal disease therapies. Kidney Int. 2008;74(9):1178-1184. [DOI] [PubMed] [Google Scholar]
- 7. Listening, Learning and Leading: A Strategic Planning Meeting to Identify Priorities for Research for Canadians With Kidney Disease. Canadians Seeking Solutions and Innovation to Overcome Chronic Kidney Disease Network. Montreal: Canadian Society of Nephrology; 2014. [Google Scholar]
- 8. Kalantar -Zadeh K, Kam-Tao Li P, Tantisattamo E, et al. Living well with kidney disease by patient and care-partner empowerment: kidney health for everyone everywhere. Clin Nephrol. 2021;95(3):115-122. [DOI] [PubMed] [Google Scholar]
- 9. Levin A, Adams E, Barrett BJ, et al. Canadians seeking solutions and innovations to overcome chronic kidney disease (Can-SOLVE CKD): form and function. Can J Kidney Health Dis. 2018;5:2054358117749530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Rossum KA, Finlay J, McCormick M, et al. A mixed method investigation to determine priorities for improving information, interaction and individualization of care among individuals on in-center hemodialysis: the triple I study. Can J Kidney Health Dis. 2020;7. doi: 10.1177/2054358120953284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Sass R, Finlay J, Rossum K, et al. Patient, caregiver and provider perspectives on challenges and solutions to individualization of care in hemodialysis: a qualitative study. Can J Kidney Health Dis. 2020;7:2054358120970715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ruggliano N, Perry EP. Conducting secondary analysis of qualitative data: should we, can we, and how? Qual Soc Work. 2019;18(1):81-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Chapman AL, Hadfield M, Chapman CJ. Qualitative research in healthcare: an introduction to grounded theory using thematic analysis. J R Coll Physicians Edinb. 2015;45(3):201-205. [DOI] [PubMed] [Google Scholar]
- 14. Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349-357. [DOI] [PubMed] [Google Scholar]
- 15. Jacobsen M, O’Connor A, Stacey D. Decisional needs assessment in populations: a workbook for assessing patients’ and practitioners’ decision making needs. Ottawa, ON, Canada: University of Ottawa Google Scholar, 2013. [Google Scholar]
- 16. Wilkie M, Barnes T. Shared hemodialysis care: increasing patient involvement in center-based dialysis. Clin J Am Soc Nephrol. 2019;14(9):1402-1404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hibbard JH, Greene J. What the evidence shows about patient activation: better health outcomes. Health Aff (Millwood). 2013;32(2):207-214. [DOI] [PubMed] [Google Scholar]
- 18. Loiselle MC, Michaud C, O’Connor A. Decisional needs assessment to help patients with advanced chronic kidney disease make better dialysis choices. Nephrol Nurs J. 2016;43(6):463-493. [PubMed] [Google Scholar]
- 19. Moore C, Wearden A, Carter L, et al. Development of a measure for patients preparing to start dialysis and their partners: the Starting Dialysis Questionnaire (SDQ). Health Qual. Life Outcomes. 2020;18:358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Nair D, Cavanaugh K. Measuring patient activation as part of kidney disease policy: are we there yet? J. Am. Soc. Nephrol. 2020;31(7):1435-1443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Ahmadzadeh S, Matlabi H, Allahverdipour H, et al. The effectiveness of self-management program on quality of life among haemodialysis patients. Prog Palliat Care. 2017;25(4):177-184. [Google Scholar]
- 22. Ren Q, Lian M, Liu Y, Thomas-Hawkins C, Zhu L, Shen Q. Effects of a transtheoretical model-based WeChat health education programme on self-management among haemodialysis patients: a longitudinal experimental intervention study. J Adv Nurs. 2019;75(12):3554-3565. [DOI] [PubMed] [Google Scholar]
- 23. Mason J, Khunti K, Stone M, Farooqi A, Carr S. Educational interventions in kidney disease care: a systematic review of randomized trials. Am J Kidney Dis. 2008;51(6):933-951. [DOI] [PubMed] [Google Scholar]
- 24. Griva K, Nandakumar M, Ng JA, Lam KFY, McBain H, Newman SP. Hemodialysis self-management intervention randomized trial (HED-SMART): a practical low-intensity intervention to improve adherence and clinical markers in patients receiving hemodialysis. Am J Kidney Dis. 2018;71(3):371-381. [DOI] [PubMed] [Google Scholar]
- 25. Havas K, Bonner A, Douglas C. Self-management support for people with chronic kidney disease: patient perspectives. J Ren Care. 2015;42(1):7-14. [DOI] [PubMed] [Google Scholar]
- 26. Taylor F, Gutteridge R, Willis C. Peer support for CKD patients and carers: overcoming barriers and facilitating access. Health Expect. 2016;19(3):617-630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Heisler M. Building peer support programs to manage chronic disease: seven models for success. Oakland: California Health Care Foundation. 2006. [Google Scholar]
- 28. Knox L, Huff J, Graham D, et al. What peer mentoring adds to already good patient care: implementing the Carpeta Roja peer mentoring program in a well-resourced health care system. Ann Fam Med. 2015;13(suppl 1):S59-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Sandhu S, Veinot P, Embuldeniya G, et al. Peer-to-peer mentoring for individuals with early inflammatory arthritis: feasibility pilot. BMJ Open. 2013;3(3):1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. St Clair Russell J, Southerland S, Huff ED, et al. A peer-to-peer mentoring program for in-centre hemodialysis: a patient-centered quality improvement program. Nephrol Nurs J. 2017;44(6):481496-481489. [PubMed] [Google Scholar]
- 31. Cervantes L, Chonchol M, Hasnain-Wynia R, et al. Peer navigator intervention for Latinos on hemodialysis: a single-arm clinical trial. J Palliat Med. 2019;22(7):838-843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Garcia-Garcia G, Jha V.On behalf of the World Kidney Day Steering Committee. CKD in disadvantaged populations. Can J Kidney Health Dis. 2015;2(18). 10.1186/s40697-015-0050-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. McDonald SP, Russ GR. Burden of end-stage renal disease among Indigenous peoples in Australia and New Zealand. Kidney Int Suppl. 2003(83):S123-S127. [DOI] [PubMed] [Google Scholar]
- 34. Norris K, Agodoa L. Unraveling the racial disparities associated with kidney disease. Kidney Int. 2005;68(3):914-924. [DOI] [PubMed] [Google Scholar]
- 35. Johnson DS, Kapoian T, Taylor R, Meyer KB. Going upstream: coordination to improve CKD care. Semin Dial. 2016;29(2):125-134. [DOI] [PubMed] [Google Scholar]
- 36. Cassidy BP, Harwood L, Getchell LE, et al. Educational support around dialysis modality decision making in patients with chronic kidney disease: a qualitative Study. Can J Kidney Health Dis. 2018;5:1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Cramm JM, Leensvaart L, Berghout M, et al. Exploring views on what is important for patient-centred care in end-stage renal disease using Q methodology. BMC Nephrol. 2015;16(74):1-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Thompson S, Schick-Makaroff K, Bello A, et al. Voicing individual concerns for engagement in hemodialysis (VOICE-HD): a mixed method, randomized pilot trial of digital health in dialysis care delivery. Canadian Journal of Kidney Health and Disease. January2021. doi:10.1177/20543581211032857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Diamantidis CJ, Becker S. Health information technology (IT) to improve the care of patients with chronic kidney disease (CKD). BMC Nephrol. 2014;15(7). https://pubmed.ncbi.nlm.nih.gov/24405907/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Min Y, Park M. Effects of a mobile-app-based self-management support program for elderly hemodialysis patients. Healthc Inform Res. 2020;26(2):93-103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Canadian Institute for Health Information (CIHI). Ottawa, Ontario: end-stage renal disease among Aboriginal peoples in Canada: treatment and outcomes. Ottawa, ON, Canada: Canadian Institute for Health Information, 2013. [Google Scholar]
- 42. Zacharias J, Komenda P, Olson J, Bourne A, Franklin D, Bernstein K. Home hemodialysis in the remote Canadian north: treatment in Manitoba fly-in communities. Semin Dial. 2011;24(6):653-657. [DOI] [PubMed] [Google Scholar]
- 43. Anderson K, Yeates K, Cunningham J, Devitt J, Cass A. They really want to go back home, they hate it here: the importance of place in Canadian health professionals’ views on the barriers facing Aboriginal patients accessing kidney transplants. Health Place. 2009;15(1):390-393. [DOI] [PubMed] [Google Scholar]
- 44. Morris ZS, Wooding S, Grant J. The answer is 17 years, what is the question: understanding time lags in translational research. J R Soc Med. 2011;104(12):510-520. [DOI] [PMC free article] [PubMed] [Google Scholar]