Abstract
Male infertility presents a public health concern. As most men wish to become fathers, it is important to increase men’s awareness of infertility risk factors. We developed a mobile health application (mHealth app), Infotility XY, to promote men’s reproductive health. This study evaluates whether use of the app led to increased knowledge of infertility risk factors, and whether knowledge change was associated with participants’ sociodemographic characteristics and/or app usage. Participants were recruited between August and October 2020. Eligibility criteria included: identified as male; 18–45 years old; childless; no infertility history; able to read and write in English/French; had internet access. We assessed participants’ fertility knowledge before and after app use. App usage data were captured during the 2-week intervention period. Our sample included 49 men aged 18–45. Seventy-eight percent of participants had not previously sought fertility information. Participants viewed on average 75% of the app’s articles, and 96% of participants said the app increased their fertility knowledge. Before app use, 55% of men said they were aware of infertility risk factors, compared to 96% after app use. Men correctly identified more risk factors after app use compared to before, t(48) = 8.28, p < .001. Participants’ sociodemographic characteristics and amount of app usage were not associated with knowledge change. This study provides evidence of the feasibility of an mHealth app to improve men’s awareness of infertility risk factors. Given the positive relationship between male reproductive health and overall health, increased awareness of infertility risk factors may lead to men’s improved overall health.
Keywords: male infertility, fertility knowledge, infertility risk factors, mHealth, app intervention
Male infertility presents a public health concern (Barratt et al., 2021). Up to 6% of men in North America and up to 12% worldwide experience infertility (Agarwal et al., 2015), which is defined as the failure to achieve a clinical pregnancy after 1 year of regular unprotected sexual intercourse or due to a person’s inability to reproduce as an individual or with a partner (Zegers-Hochschild et al., 2017). Clinical guidelines recommend that an initial evaluation of a man’s fertility status includes a reproductive history and at least one semen analysis (Schlegel et al., 2021), which assesses multiple parameters such as sperm concentration, motility, and morphology (Baskaran et al., 2020).
Men should be aware of factors that can affect their semen quality, and thus their fertility, as most men consider parenthood to be an important aspect of their lives and express a desire to become a father (Hammarberg et al., 2017). However, men tend to have limited fertility awareness (Hammarberg et al., 2017; Pedro et al., 2018). For example, in a survey of Canadian men aged 18–50 years old, participants were only able to identify half of the risk factors for male infertility on average (Daumler et al., 2016).
Evidence points to declining sperm counts among men in North America, Europe, Australia, and New Zealand (Levine et al., 2017). Several factors have been associated with impaired semen parameters. Older age has been linked to declines in semen volume, sperm motility, and morphology (Eisenberg & Meldrum, 2017). Male infertility can be a result of sperm DNA damage caused by common medical conditions such as cancer, diabetes mellitus, obesity, varicocele, and untreated reproductive tract infections (Panner Selvam et al., 2021). Impaired semen parameters, including sperm concentration, motility, and morphology, have been associated with tobacco smoking, excessive alcohol consumption, the use of drugs such as cannabis, and the use of anabolic steroids (Leisegang & Dutta, 2021). Psychological stress may lead to impaired testicular function, thus negatively affecting sperm quality (Dissanayake et al., 2019; Leisegang & Dutta, 2021). Male infertility can result from other environmental and lifestyle activities including exposure to environmental toxins such as pesticides, radiation from cell phones and Wi-Fi (Leisegang & Dutta, 2021; Panner Selvam et al., 2021), and prolonged exposure to heat, for example through wearing tight underwear, frequent sauna use, and intensive cycling (Leisegang & Dutta, 2021; Sharma et al., 2021).
Compared to women, men are more likely to engage in risky behaviors, such as smoking and drug use, and are more likely to have an unhealthy diet (Baker, 2019). Men also tend to have lower health literacy levels and are less likely than women to seek health information and use health-care services (Baker, 2019). This reluctance to engage in self-care can in part be explained by the feelings of vulnerability to one’s masculinity, whereby help-seeking is viewed as a sign of dependency and weakness (Baker, 2019; De Jonge & Barratt, 2019; Mahalik & Backus Dagirmanjian, 2018).
Seeking fertility information can be perceived as threatening to a man’s sense of masculinity due to the feelings of worthlessness and inadequacy that infertility can produce (Hanna & Gough, 2020). The stigma attached to male infertility may prevent men from seeking fertility information directly from health professionals (Grace et al., 2019). Online sources of information can appeal to men due to their anonymity and accessibility (Lohan et al., 2015) and can be effective in increasing men’s fertility knowledge (Grace et al., 2019), potentially motivating them to address modifiable risk factors to improve reproductive health (Buckworth, 2017). A cross-sectional study of websites conducted by our research team revealed a lack of high-quality online information on male fertility that was appropriate for men in the general public (Robins et al., 2016). This informed our decision to develop a mobile health application (mHealth app), Infotility XY, to promote men’s reproductive health.
Only a few research studies assessed the effectiveness of online interventions in increasing fertility awareness, but these were not exclusively focused on male fertility, their samples consisted of both women and men, and participants were exposed to fertility information for a very brief amount of time (Boivin et al., 2018; Conceição et al., 2017; Daniluk & Koert, 2015; Maeda et al., 2016; Wojcieszek & Thompson, 2013).
The current study contributes to the existing literature by evaluating the feasibility of an mHealth app (Infotility XY) geared exclusively toward men in increasing men’s knowledge of factors affecting their fertility. Compared to previous studies that employed very brief exposures to fertility information, participants in the current study had access to Infotility XY for two weeks and were able to absorb the information at their own pace. In addition, Infotility XY contained a wide range of fertility topics and included interactive features such as videos and quizzes to help participants better understand the material. The present study aims to determine whether men’s knowledge of risk factors for male infertility increased after using the Infotility XY app, and whether the change in fertility knowledge was associated with participants’ sociodemographic characteristics and/or amount of app usage.
Methods
App Development
Our research team developed the mHealth app Infotility XY/Infotilité XY as part of a larger research program funded by the Canadian Institutes of Health Research to address the need for innovative modalities of promoting reproductive health among men. The overarching aim of the study was to assess the feasibility of recruiting men and the mHealth app’s acceptability as a source of fertility information. This would inform a future randomized controlled trial to evaluate whether app use would result in increased fertility awareness and reproductive health behavior. With the assistance of an app development company, we developed three distinct versions of the app for three populations: (1) men in the general public; (2) male infertile patients; and (3) male oncology patients. For the purposes of this paper, only data from the subsample of men in the general public were analyzed and presented.
The content for the three versions of the app was developed by our research team and informed by reviews of fertility literature and needs assessment surveys with stakeholders. Pertaining to the population of men in the general public, a web-based survey of 701 Canadian men aged 18–50 revealed men’s limited fertility awareness as participants were only able to identify 51% of the risk factors and 45% of the health issues associated with male infertility on average (Daumler et al., 2016). The survey also pointed to men’s interest in obtaining information on male reproductive health, with preferred sources being medical professionals and the internet.
Content was vetted for accuracy and relevance by physicians, nurses, psychologists, and experts in patient-centered care. Content was written in accessible language and available in both English and French. The Infotility XY app for men in the general public included 18 articles grouped into four categories: (1) reproduction 101; (2) risks to male fertility; (3) promoting male fertility; and (4) sperm banking 101 (see Appendix A for an overview of articles). Each article had an illustration, the option to give a thumbs-up or thumbs-down indicating that the article was useful (or not), and most articles included links to additional resources. To keep users engaged, the app featured infographics, interactive quizzes, animations, pop-up glossary definitions, and the My Fertility Checklist (referred to as “checklist”), which allowed participants to keep track of items to improve fertility included in articles (e.g., “Feed your nuts more brazil nuts,” “Wash your produce, those pesticides don’t just harm insects”). See Appendix B for examples of the app’s design and features.
Recruitment
The study was approved by the Medical/Biomedical Research Ethics Committee of CIUSSS West-Central Montreal Research Ethics Board (MP-05-2016-344). Participants were recruited between August 31 and October 29, 2020, by a market research firm (referred to as “recruitment company”), which adheres to the highest standards in research methodology, ethical practices, respondent rights, and personal privacy. Interested individuals were screened for eligibility based on the following criteria: (1) identified as male; (2) 18–45 years old; (3) had no children; (4) had no history of infertility; (5) were able to read and write in English or French; (6) had internet access. The recruitment company ensured that participants met eligibility requirements and represented a demographically diverse sample. To maintain confidentiality throughout the study, only unique participant codes were used in communication between our research team and the recruitment company.
Participants
Guidelines for the pilot stage of the evaluation of web-based interventions suggest that a sample of 20 users is required (Usability.gov, n.d.). To account for possible attrition, our research team set a recruitment target of 50 men. All participants were drawn from the recruitment company’s database of men who had previously indicated an interest in participating in research in general. Of the 3303 men who responded to the recruitment screener, 54 men met the eligibility criteria and were recruited, four dropped out due to loss of interest, and 50 completed the study.
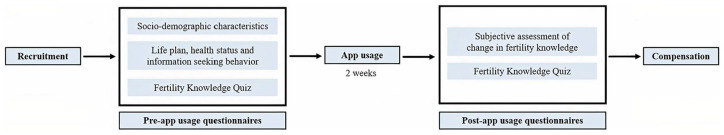
Procedures
A summary of the study’s procedures and measures is displayed in Figure 1. Informed consent was obtained online from each participant. Participants received instructions on how to use the app and were asked to create an account and complete a set of pre-app usage questionnaires. After completing these questionnaires, participants gained access to the Infotility XY app. Participants were able to use the app as little or as much as they wished during the 2-week study period. This time period was selected based on our previous experience with app usage (Kruglova et al., forthcoming), where we found that app usage tended to drop off after 2 weeks, suggesting that a study period of 2 weeks may be sufficient to obtain app usage data, while helping to reduce attrition, which is common in studies of mHealth interventions (Linardon & Fuller-Tyszkiewicz, 2020). After the study period, participants were temporarily blocked from accessing the app and prompted to complete a set of post-app usage questionnaires. After completing these questionnaires, participants regained access to the app. To reduce attrition and delays in study completion, participants received up to three automatic reminder emails to complete the questionnaires and to use the app. Participants who completed the study were compensated $150 CAD by the recruitment company.
Figure 1.
Flowchart of study procedures and measures.
Data Security
To access the app, participants were required to create a username that did not use their full name and a password. Collected data (responses to questionnaires, app usage) were stored on a server located in Canada and then exported to a secure folder of the institution’s network drive using only participants’ usernames, each associated with a unique code. Neither the recruitment company nor the app development company had access to these data. The key linking the codes to participants’ personal information was kept separate on a password-protected computer and was only available to the Principal Investigator and the research coordinator. All collected information was backed up nightly to prevent data loss.
Measures
Sociodemographic Characteristics
Before using the app, participants’ sociodemographic characteristics were collected. Men were asked to specify their age, relationship status, immigrant status, household income, level of education, ethnic origin, and religious affiliation.
Life Plan, Health Status, and Information-Seeking Behavior
Before using the app, participants were asked if they were currently trying to have a child and if they planned to have children in the future. Men also reported if they had ever been diagnosed with cancer or conditions that can affect fertility, whether they ever sought information on fertility and/or fertility preservation, and if so, whether they received all the information that they needed.
Fertility Knowledge Quiz
To assess whether using the Infotility XY app might increase men’s fertility knowledge, participants were asked to complete the Fertility Knowledge Quiz (referred to as “Quiz”) both before and after app use. The Quiz was developed by our research team, including two male fertility specialists, for our 2015 population-based survey (Daumler et al., 2016). In the present study, we used an adapted version of the original measure which included: (1) an open-ended question asking participants if they were aware of any factors that can affect their fertility, and if they responded “yes,” they were asked to list up to 15 factors; and (2) a list of 33 items to endorse if participants considered them to be risk factors for male infertility (see Table 1). Of these 33 items, 24 were actual risk factors such as smoking and diabetes, and nine items were factors not associated with male fertility such as dental cavity fillings and migraines. These nine decoy items were used to reduce response set bias (i.e., responding “yes” to questionnaire items).
Table 1.
Items on the Fertility Knowledge Quiz.
| # | Quiz Item |
|---|---|
| Risk factors | |
| 1 | Age (more than 45 years old) |
| 2 | Delayed puberty |
| 3 | Exposure to pesticides or environmental toxins such as paint, solvents |
| 4 | Use of drugs such as marijuana, narcotics, cocaine |
| 5 | Smoking cigarettes |
| 6 | Alcohol consumption (more than 10 drinks a week) |
| 7 | Long term use of steroids |
| 8 | Sexually transmitted infections such as chlamydia, gonorrhea |
| 9 | Pain or injury to the testicles or scrotum |
| 10 | Size of testicles |
| 11 | X-rays |
| 12 | Diabetes |
| 13 | High cholesterol |
| 14 | Cancer treatment such as radiation or chemotherapy |
| 15 | Stress |
| 16 | Overweight/obesity |
| 17 | Frequent hot tub use |
| 18 | Wearing tight pants |
| 19 | Frequent bicycling or riding horses |
| 20 | Overuse of electronic devices such as cellphones or computers |
| 21 | Frequent use of a laptop on your lap |
| 22 | Urinary tract (bladder) infection |
| 23 | Hernia repair |
| 24 | Genetic abnormality |
| Decoy items | |
| 1 | Belonging to a specific ethnic group |
| 2 | Frequent sexual relations |
| 3 | Frequent masturbation |
| 4 | Long term use of antibiotics |
| 5 | Dental cavity fillings |
| 6 | Migraines |
| 7 | Poor diet |
| 8 | Lack of regular exercise |
| 9 | Work-out supplements such as creatine, protein |
App Usage
Participants’ app usage patterns were tracked over the two-week study period. The following key performance indicators (KPIs) were collected: (1) number of unique pageviews; (2) thumbs-up assessments; (3) thumbs-down assessments; and (4) number of checklist items the participant endorsed.
Subjective Assessment of Change in Fertility Knowledge
After using the app, participants were asked to report on their subjective change in fertility knowledge. It was assessed with the question “Did using the app increase your knowledge of fertility?” on a Likert scale where 0 = No, not at all, 1 = No, not very much, 2 = Yes, a bit, and 3 = Yes, quite a lot.
Statistical Analyses
The app development company provided the metrics on participants’ app usage. All analyses were performed using IBM SPSS Statistics, Version 23.0 Armonk, NY: IBM Corp. Descriptive statistics (e.g., frequencies, means) were used to examine participants’ sociodemographic characteristics, responses to the questions about life plan, health status, and information-seeking behavior, their responses to the Quiz, and app usage. The threshold for significance was set at p < .05. There were 4.08% missing app usage data. No data were missing from the pre- or post-app usage questionnaires.
App Usage
For each participant, we extracted the total number of unique pages viewed. All thumbs-up and thumbs-down were totaled separately. Articles and thumbs-up/down assessments were further classified into two categories: “medical” (11 articles) or “lifestyle” (7 articles; see Appendix A). These categories were developed for analytic purposes only and were not visible to participants. For pageviews and thumbs-up/down assessments, total numbers as well as numbers per category were used in the analyses. If a participant visited a particular article in a category more than once, it was only counted once. Of the 11 possible checklist items, all items endorsed by the participant were summed. For checklist items, only total numbers were used.
Fertility Knowledge Quiz
To quantify participants’ knowledge of infertility risk factors, we collapsed similar responses to the open-ended question of the Quiz (e.g., “drinking,” “drinking alcohol,” and “alcohol” were all collapsed into “alcohol”). We then calculated frequencies for each set of responses (e.g., “alcohol”) by dividing the number of participants who listed each item by the total number of participants.
Percentage change values were estimated for the 24 risk factors to examine change in the number of correct responses after using the app compared to before. These values were obtained by dividing the difference in the number of correct responses before and after app use by the number of correct responses before app use and multiplying the result by 100%. To create continuous scores, items that participants selected were coded as “1” and non-selected items as “0.” We summed each participant’s responses (either 0 or 1) to obtain continuous scores that could range from zero to 24, with higher scores representing higher fertility knowledge. The continuous scores for the risk factors before and after app use demonstrated good internal consistency with Cronbach’s alphas of 0.81 and 0.84, respectively. A Kolmogorov-Smirnov (K-S) test indicated that the continuous scores both before (D[49] = .13, p = .06) and after (D[49] = .10, p = .20) app use followed a normal distribution. Therefore, a paired samples t-test was used to determine if there was a change in mean scores.
Fertility Knowledge, Sociodemographics, and App usage
A fertility knowledge change score was created for each participant by subtracting the pre-app usage continuous score from the post-app usage continuous score. Pearson’s correlations were used to assess the relationship between fertility knowledge change scores and participants’ ages, as both variables were normally distributed. Point-biserial correlations were used to assess the relationship between fertility knowledge change scores and dichotomous sociodemographic characteristics (e.g., ethnicity, immigrant status). Spearman’s correlations were used to assess the relationship between fertility knowledge change scores and ordinal level sociodemographic characteristics (e.g., income, education). According to the K-S test, all app usage variables deviated from a normal distribution. Therefore, Spearman’s correlations were used to assess the relationship between fertility knowledge change scores and the app usage variables.
Results
Sample Characteristics
One participant, who selected all Quiz items—including the nine decoy items—both before and after app use, was considered a careless responder, and his data were removed from analyses. Therefore, the final sample included 49 men between the ages of 18 and 45 years old (M = 31.5 years, SD = 6.0). Data on participants’ sociodemographics, life plan, health status, and information-seeking behavior are presented in Table 2. The majority of participants were Anglophones (93.9%, 46/49), Canadian-born (81.6%, 40/49), either single (46.9%, 23/49), or in a heterosexual relationship (44.9%, 22/49), had at least a bachelor’s degree (61.2%, 30/49), and identified as White (59.2%, 29/49). The majority (93.9%, 46/49) of men indicated that they were not currently trying to have a child; however, most said that they would like to have children in the future (65.3%, 32/49) while 28.6% (14/49) were uncertain. The majority of participants (77.6%, 38/49) indicated that they had not previously sought information on fertility and/or fertility preservation. Of the 11 men who had sought fertility-related information, 10 (90.9%) said that the information came from the internet, six (54.5%) from a family physician, and two (18.2%) from friends/family. Of these 11 men, only three (27.3%) said that they received all the information that they needed.
Table 2.
Participants’ Sociodemographics, Life Plan, Health Status, and Information-Seeking Behavior.
| n | Valid % or M (SD) (Range) | |
|---|---|---|
| Age (years) | 49 | 31.5 (6.0) (18–45) |
| Language | ||
| English | 46 | 93.9 |
| French | 3 | 6.1 |
| Household income (CAD) | ||
| ≤$50,000 | 8 | 16.3 |
| $50,000–89,999 | 19 | 38.8 |
| $90,000–129,999 | 10 | 20.4 |
| $130,000 and above | 12 | 24.5 |
| Relationship status | ||
| Single | 23 | 46.9 |
| In a heterosexual relationship | 22 | 44.9 |
| In a non-heterosexual relationship | 4 | 8.2 |
| Relationship status (dichotomous) | ||
| Single | 23 | 46.9 |
| In a relationship | 26 | 53.1 |
| Highest level of education | ||
| High school diploma | 9 | 18.4 |
| CEGEP a , trade, vocational | 10 | 20.4 |
| Undergraduate/Bachelor’s degree | 25 | 51.0 |
| Graduate or other professional degree | 5 | 10.2 |
| Immigrant status | ||
| Immigrant | 9 | 18.4 |
| Born in Canada | 40 | 81.6 |
| Ethnicity | ||
| Indigenous | 1 | 2.0 |
| White | 29 | 59.2 |
| Black | 1 | 2.0 |
| Latin, Central and South American | 1 | 2.0 |
| South Asian | 8 | 16.3 |
| East and Southeast Asian | 6 | 12.2 |
| Mixed ethnicity | 3 | 6.1 |
| Ethnicity (dichotomous) | ||
| White | 29 | 59.2 |
| BIPOC b | 20 | 40.8 |
| Do you consider yourself a religious person? | ||
| Yes | 9 | 18.4 |
| No | 40 | 81.6 |
| Are you currently trying to have a child? | ||
| Yes | 3 | 6.1 |
| No | 46 | 93.9 |
| Would you like to have any children in the future? | ||
| Yes | 32 | 65.3 |
| No | 3 | 6.1 |
| I don’t know | 14 | 28.6 |
| Have you ever been diagnosed with cancer or other conditions that might affect fertility? | ||
| Yes | 1 | 2.0 |
| No | 48 | 98.0 |
| Have you ever sought information on fertility and/or fertility preservation? | ||
| Yes | 11 | 22.4 |
| No | 38 | 77.6 |
Note. aCEGEP is a 2-year college preparatory program or 3-year technical program following high school and preceding post-secondary education in Quebec, Canada.
BIPOC = black, Indigenous and people of color.
App Usage
Participants viewed on average 13.45 (74.7%, SD = 6.17, range = 1–18) of the 18 articles on the app, specifically, 8.02 (72.9%, SD = 3.98, range = 0–11) of the 11 medical articles and 5.43 (77.6%, SD = 2.35, range = 1–7) of the 7 lifestyle articles. Men gave a thumbs-up to an average of 5.11/18 (28.4%, SD = 5.76, range = 0–18) articles, specifically, to 2.91/11 (26.5%, SD = 3.62, range = 0–11) medical articles and 2.19/7 (31.3%, SD = 2.37, range = 0–7) lifestyle articles. The articles that received the most thumbs-up were “Heat” (42.9%, 21/49), “Nutrition” (34.7%, 17/49), and “The what, why and how of sperm banking” (32.7%, 16/49). Men gave a thumbs-down to an average of 0.13/18 (0.7%, SD = 0.54, range = 0–3) articles, specifically, to 0.11/11 (1.0%, SD = 0.43, range = 0–2) medical articles and 0.02/7 (0.3%, SD = 0.15, range = 0–1) lifestyle articles. Of the 11 checklist items, participants checked an average of 5.26 (47.8%, SD = 4.62, range = 0–11) items.
Subjective Evaluation of Fertility Knowledge
In response to the question whether using the Infotility XY app increased their fertility knowledge, the majority of participants (95.9%, 47/49) indicated “Yes, a bit” or “Yes, quite a bit.” Only 4.1% (2/49) responded “No, not very much.”
Fertility Knowledge Quiz
Before app use, 55.1% (27/49) of men indicated that they were aware of risk factors for male infertility and listed 2.2 items on average. The most commonly listed items were age (26.5%, 13/49), smoking (20.4%, 10/49), genetics (18.4%, 9/49), use of drugs (14.3%, 7/49), alcohol consumption (14.3%, 7/49), and radiation (14.3%, 7/49). After using the app, 95.9% (47/49) of men indicated that they were aware of risk factors for male infertility and listed 6.9 items on average. The most commonly listed items were age (63.3%, 31/49), diet/nutrition (63.3%, 31/49), exercise/physical activity (63.3%, 31/49), clothing/underwear (51.0%, 25/49), heat/temperature (46.9%, 23/49), and smoking (46.9%, 23/49).
Before app use, the mean percentage of men who correctly identified the 24 risk factors for male infertility was 46.3% (Table 3). Percentage of correct responses ranged from 6.1% to 79.6%. Over 70% of participants were aware of the fertility risk associated with advanced male age (79.6%, 39/49), long-term use of steroids (79.6%, 39/49), use of drugs (77.6%, 38/49), smoking cigarettes (73.5%, 36/49), pain or injury to the testicles or scrotum (73.5%, 36/49), alcohol consumption (71.4%, 35/49), and cancer treatment (71.4%, 35/49). On the other hand, less than 30% of men identified the fertility risk associated with frequent bicycling or riding horses (22.4%, 11/49), overuse of electronic devices (18.4%, 9/49), frequent hot tub use (16.3%, 8/49), delayed puberty (16.3%, 8/49), size of testicles (10.2%, 5/49), and hernia repair (6.1%, 3/49).
Table 3.
Percentage of Men Who Correctly Identified Fertility Risk Factors and Percentage Change in the Number of Correct Responses.
| Risk Factors | Pre-App Usage | Post-App Usage | % Change | ||
|---|---|---|---|---|---|
| N * | Valid % | N * | Valid % | ||
| Hernia repair | 3 | 6.1% | 15 | 30.6% | 400.0% |
| Frequent hot tub use | 8 | 16.3% | 33 | 67.3% | 312.5% |
| Frequent bicycling or riding horses | 11 | 22.4% | 42 | 85.7% | 281.8% |
| Size of testicles | 5 | 10.2% | 19 | 38.8% | 280.0% |
| Overuse of electronic devices such as cell phones or computers | 9 | 18.4% | 28 | 57.1% | 211.1% |
| Frequent use of a laptop on your lap | 15 | 30.6% | 43 | 87.8% | 186.7% |
| Wearing tight pants | 17 | 34.7% | 45 | 91.8% | 164.7% |
| Delayed puberty | 8 | 16.3% | 19 | 38.8% | 137.5% |
| Sexually transmitted infections such as chlamydia, gonorrhea | 25 | 51.0% | 43 | 87.8% | 72.0% |
| Diabetes | 16 | 32.7% | 25 | 51.0% | 56.3% |
| X-rays | 17 | 34.7% | 26 | 53.1% | 52.9% |
| Urinary tract (bladder) infection | 15 | 30.6% | 22 | 44.9% | 46.7% |
| High cholesterol | 16 | 32.7% | 23 | 46.9% | 43.8% |
| Overweight/obesity | 31 | 63.3% | 44 | 89.8% | 41.9% |
| Alcohol consumption (more than 10 drinks a week) | 35 | 71.4% | 49 | 100.0% | 40.0% |
| Exposure to pesticides or environmental toxins such as paint, solvents | 32 | 65.3% | 44 | 89.8% | 37.5% |
| Smoking cigarettes | 36 | 73.5% | 47 | 95.9% | 30.6% |
| Stress | 29 | 59.2% | 37 | 75.5% | 27.6% |
| Use of drugs such as marijuana, narcotics, cocaine | 38 | 77.6% | 47 | 95.9% | 23.7% |
| Age (more than 45 years old) | 39 | 79.6% | 47 | 95.9% | 20.5% |
| Pain or injury to the testicles or scrotum | 36 | 73.5% | 41 | 83.7% | 13.9% |
| Long term use of steroids | 39 | 79.6% | 43 | 87.8% | 10.3% |
| Cancer treatment such as radiation or chemotherapy | 35 | 71.4% | 38 | 77.6% | 8.6% |
| Genetic abnormality | 30 | 61.2% | 30 | 61.2% | No change |
| Mean | 23 | 46.3% | 35 | 72.3% | 104.2% |
Note. *Number of participants that correctly identified the item as a risk factor for male infertility.
After app use, the mean percentage of men who correctly identified the risk factors increased from 46.3% to 72.3% (Table 3). Percentages increased for all risk factors except for the factor genetic abnormality. Mean percentage change was 104.2% with the values ranging from 0% to 400%. The percentage change for the following eight risk factors was over 100%: hernia repair (400.0%); two factors associated with reproductive development—size of testicles (280.0%) and delayed puberty (137.5%); and five factors linked to heat exposure—frequent hot tub use (312.5%), frequent bicycling or riding horses (281.8%), overuse of electronic devices (211.1%), frequent use of a laptop on one’s lap (186.7%), and wearing tight pants (164.7%). On the other hand, the percentage change was below 30% for the following six risk factors: stress (27.6%); use of drugs (23.7%); age (20.5%); pain or injury to the testicles or scrotum (13.9%); long-term use of steroids (10.3%); and cancer treatment (8.6%).
Participants’ continuous scores were compared before and after using the Infotility XY app. On average, men correctly identified more risk factors after using the app (M = 17.14, SD = 4.32) compared to before (M = 11.12, SD = 4.53). A paired samples t-test indicated that this difference was statistically significant, t(48) = 8.28, p < .001. The majority of participants (81.6%, 40/49) demonstrated higher knowledge of risk factors for male infertility after the intervention, with an average increase of 7.6 risk factors (SD = 4.21, range 2–21). Continuous scores did not change for 4/49 (8.2%) men and decreased for 5/49 (10.2%) men, with an average decrease of 1.8 factors (SD = 0.84, range 1–3).
Fertility Knowledge, Sociodemographics, and App Usage
None of the participants’ sociodemographic characteristics were related to their fertility knowledge change scores. There was also no association between men’s fertility knowledge change scores and their amount of app usage.
Discussion
To the best of our knowledge, our study is the first to develop a 2-week mHealth intervention geared specifically toward men in the general public and evaluate its feasibility in increasing men’s fertility knowledge. Our results demonstrate that participants’ knowledge of risk factors for male infertility improved after using the Infotility XY app. Though the change in the number of correct responses varied across the factors, the mean percentage change was over 100% improvement. The greatest change was observed for the eight factors that can be broadly categorized as either medical or lifestyle. The three medical risk factors—hernia repair, size of testicles, and delayed puberty—were known to only three, five and eight participants, respectively, before the intervention. This is not surprising as these medical conditions are relevant for only a small group of men, and those not directly affected are unlikely to seek information on these conditions (Lee et al., 2014), let alone be aware of their impact on male fertility. Given the low baseline levels of awareness of these factors, even a short exposure to information may be effective in communicating the fertility risk associated with these factors, thus leading to a relatively large increase in knowledge. For example, only three men were aware of the fertility risk associated with hernia repair before using Infotility XY compared to 15 men after, which corresponds to a 400% increase in knowledge. The lifestyle factors with the greatest change in knowledge were the five items related to heat exposure, which were covered in the app’s article “Heat” and the interactive quizzes. This finding may suggest that the app’s information on these factors was clear and sufficient and presented in an engaging way. App usage data support this conclusion: the article “Heat” received the largest number of thumbs-up. The information on lifestyle activities, such as using a laptop on one’s lap, is relatable and applicable to a man’s daily life, which can make it easier to understand and remember.
Participants’ change in fertility knowledge was not associated with their amount of app usage. Regardless of whether men viewed all app articles or only a few articles of personal interest, their knowledge of risk factors still increased on average. It is also interesting to note that there was no variation in fertility knowledge according to participants’ sociodemographic characteristics, which suggests that our findings can be generalized to diverse groups of men in the general public.
There are several limitations to the present study. First, our results could have been influenced by self-selection bias since all participants were recruited from the recruitment company’s database of individuals with an interest in participating in research. Participants were also compensated for their involvement in the study. Therefore, our sample may not fully reflect the interest in or knowledge of fertility issues of men in the general public who would not have chosen to participate in this research project. Second, our sample was relatively small, which may limit generalizability of results. Third, because change in fertility knowledge was only assessed once immediately after the intervention, long-term retention of knowledge cannot be measured. Current evidence is insufficient to determine the effectiveness of online interventions in producing a long-term increase in fertility awareness among men. In a Japanese RCT, though still higher than the pre-intervention levels, men’s fertility knowledge after 2 years was lower than immediately after the intervention (Maeda et al., 2018). In a Canadian study by Daniluk and Koert (2015), the increase in knowledge was not sustained at 6-month follow-up, particularly in men. More longitudinal studies are needed to determine if mHealth app interventions can result in long-term improvements in fertility knowledge. Fourth, because our study did not include a control group, it is not possible to account for any external factors that might have influenced participants’ change in knowledge. In addition, as research on factors affecting male fertility is ongoing, there can be some question about our choice of Quiz items. For example, both lack of sleep and excessive sleep have been associated with low sperm concentration and poor fertility outcomes (Kohn et al., 2020). Despite these limitations, our study has notable strengths. The pre–post study design allowed the assessment of change in fertility knowledge from before to after the app intervention. Furthermore, the level of participant engagement was high, as demonstrated by the app usage data showing that on average men viewed over 70% of app articles.
Conclusion
The present study provides novel evidence of the feasibility of an mHealth app to improve men’s knowledge of factors that can affect their fertility. Despite men’s reluctance to seek health information, particularly through direct contact with health professionals, our study demonstrates the feasibility of engaging men in learning about their reproductive health. Educational programs and public health campaigns are needed to inform men about factors affecting their fertility and ways to improve it (Ravitsky & Kimmins, 2019). This is particularly relevant given the growing evidence that male fertility can be a biomarker of men’s overall health (Kasman et al., 2020). Compared to their fertile counterparts, infertile men tend to be at a higher risk for mortality and morbidity including cancer, cardiovascular disease, hypertension, and diabetes (Choy & Eisenberg, 2018; Del Giudice et al., 2020; Kasman et al., 2020). A fertility-related mHealth app designed specifically for men, which presents succinct information in an interactive format, can help keep men engaged and motivated to improve their fertility knowledge. As more health initiatives specifically for men are developed (De Jonge & Barratt, 2019), there is an excellent opportunity to reach men in the general public by providing them with evidence-based and accessible online resources on male fertility. Given the positive relationship between male reproductive health and overall health, increased awareness of factors that can affect a man’s fertility may lead to men’s better overall health and quality of life.
Supplemental Material
Supplemental material, sj-docx-1-jmh-10.1177_15579883211049027 for Risky Business: Increasing Fertility Knowledge of Men in the General Public Using the Mobile Health Application Infotility XY by Katya Kruglova, Eden Noah Gelgoot, Peter Chan, Kirk Lo, Zeev Rosberger, Emilie Bélanger, Jordana Kazdan, Stephanie Robins and Phyllis Zelkowitz in American Journal of Men’s Health
Supplemental material, sj-docx-2-jmh-10.1177_15579883211049027 for Risky Business: Increasing Fertility Knowledge of Men in the General Public Using the Mobile Health Application Infotility XY by Katya Kruglova, Eden Noah Gelgoot, Peter Chan, Kirk Lo, Zeev Rosberger, Emilie Bélanger, Jordana Kazdan, Stephanie Robins and Phyllis Zelkowitz in American Journal of Men’s Health
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was funded by the Canadian Institutes of Health Research Grant [MOP – 138296].
ORCID iDs: Phyllis Zelkowitz  https://orcid.org/0000-0002-1965-5731
https://orcid.org/0000-0002-1965-5731
Supplemental Material: Supplemental material for this article is available online.
References
- Agarwal A., Mulgund A., Hamada A., Chyatte M. R. (2015). A unique view on male infertility around the globe. Reproductive Biology and Endocrinology, 13, Article 37. 10.1186/s12958-015-0032-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker P. (2019). Who self-cares wins: An updated perspective on men and self-care. Trends in Urology and Men’s Health, 10(3), 19–22. 10.1002/tre.694 [DOI] [Google Scholar]
- Barratt C. L., De Jonge C. J., Anderson R. A., Eisenberg M. L., Garrido N., Rautakallio Hokkanen S., Krausz C., Kimmins S., O’Bryan M. K., Pacey A. A., Tüttelmann, F., & Veltman, J. A. (2021). A global approach to addressing the policy, research and social challenges of male reproductive health. Human Reproduction Open, 2021(1), hoab009. 10.1093/hropen/hoab009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baskaran S., Finelli R., Agarwal A., Henkel R. (2020). Diagnostic value of routine semen analysis in clinical andrology. Andrologia, 53(2), e13614. 10.1111/and.13614 [DOI] [PubMed]
- Boivin J., Koert E., Harris T., O’Shea L., Perryman A., Parker K., Harrison C. (2018). An experimental evaluation of the benefits and costs of providing fertility information to adolescents and emerging adults. Human Reproduction, 33(7), 1247–1253. 10.1093/humrep/dey107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckworth J. (2017). Promoting self-efficacy for healthy behaviors. ACSM’s Health and Fitness Journal, 21(5), 40–42. 10.1249/FIT.0000000000000318 [DOI] [Google Scholar]
- Choy J. T., Eisenberg M. L. (2018). Male infertility as a window to health. Fertility and Sterility, 110(5), 810–814. 10.1016/j.fertnstert.2018.08.015 [DOI] [PubMed] [Google Scholar]
- Conceição C., Pedro J., Martins M. V. (2017). Effectiveness of a video intervention on fertility knowledge among university students: A randomised pre-test/post-test study. The European Journal of Contraception and Reproductive Health Care, 22(2), 107–113. 10.1080/13625187.2017.1288903 [DOI] [PubMed] [Google Scholar]
- Daniluk J., Koert E. (2015). Fertility awareness online: The efficacy of a fertility education website in increasing knowledge and changing fertility beliefs. Human Reproduction, 30(2), 353–363. 10.1093/humrep/deu328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daumler D., Chan P., Lo K., Takefman J., Zelkowitz P. (2016). Men’s knowledge of their own fertility: A population-based survey examining the awareness of factors that are associated with male infertility. Human Reproduction, 31(12), 2781–2790. 10.1093/humrep/dew265 [DOI] [PMC free article] [PubMed]
- De Jonge C., Barratt C. (2019). The present crisis in male reproductive health: An urgent need for a political, social, and research roadmap. Andrology, 7(6), 762–768. 10.1111/andr.12673 [DOI] [PubMed] [Google Scholar]
- Del Giudice F., Kasman A. M., Ferro M., Sciarra A., De Berardinis E., Belladelli F., Salonia A., Eisenberg M. L. (2020). Clinical correlation among male infertility and overall male health: A systematic review of the literature. Investigative and Clinical Urology, 61(4), 355–371. 10.4111/icu.2020.61.4.355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dissanayake D., Keerthirathna W., Peiris L. D. C. (2019). Male infertility problem: A contemporary review on present status and future perspective. Gender and the Genome, 3, 10.1177/2470289719868240 [DOI] [Google Scholar]
- Eisenberg M. L., Meldrum D. (2017). Effects of age on fertility and sexual function. Fertiluty and Sterility, 107(2), 301–304. 10.1016/j.fertnstert.2016.12.018 [DOI] [PubMed] [Google Scholar]
- Grace B., Shawe J., Johnson S., Stephenson J. (2019). You did not turn up. . . I did not realise I was invited. . .: Understanding male attitudes towards engagement in fertility and reproductive health discussions. Human Reproduction Open, 2019(3)3. 10.1093/hropen/hoz014 [DOI] [PMC free article] [PubMed]
- Hammarberg K., Collins V., Holden C., Young K., McLachlan R. (2017). Men’s knowledge, attitudes and behaviours relating to fertility. Human Reproduction Update, 23(4), 458–480. 10.1093/humupd/dmx005 [DOI] [PubMed] [Google Scholar]
- Hanna E., Gough B. (2020). The social construction of male infertility: A qualitative questionnaire study of men with a male factor infertility diagnosis. Sociology of Health and Illness, 42(3), 465–480. 10.1111/1467-9566.13038 [DOI] [PubMed] [Google Scholar]
- Kasman A. M., Del Giudice F., Eisenberg M. L. (2020). New insights to guide patient care: The bidirectional relationship between male infertility and male health. Fertility and Sterility, 113(3), 469–477. 10.1016/j.fertnstert.2020.01.002 [DOI] [PubMed] [Google Scholar]
- Kohn T. P., Kohn J. R., Haney N. M., Pastuszak A. W., Lipshultz L. I. (2020). The effect of sleep on men’s health. Translational Andrology and Urology, 9(Suppl 2), S178–S185. 10.21037/tau.2019.11.07 [DOI] [PMC free article] [PubMed]
- Kruglova K., O’Connell S. B. L., Dawadi S., Gelgoot E. N., Miner S. A., Robins S., Schinazi J., Zelkowitz P. An mHealth app Infotility, a mobile health application to support fertility patients navigating the world of infertility (Infotility): Development and usability study. JMIR Formative Research (forthcoming). 10.2196/28136 [DOI] [PMC free article] [PubMed]
- Lee K., Hoti K., Hughes J. D., Emmerton L. (2014). Dr Google and the consumer: A qualitative study exploring the navigational needs and online health information-seeking behaviors of consumers with chronic health conditions. Journal of Medical Internet Research, 16(12), e262. 10.2196/jmir.3706 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leisegang K., Dutta S. (2021). Do lifestyle practices impede male fertility? Andrologia, 53(1), e13595. 10.1111/and.13595 [DOI] [PubMed] [Google Scholar]
- Levine H., Jørgensen N., Martino-Andrade A., Mendiola J., Weksler-Derri D., Mindlis I., Pinotti R., Swan S. H. (2017). Temporal trends in sperm count: A systematic review and meta-regression analysis. Human Reproduction Update, 23(6), 646–659. 10.1093/humupd/dmx022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linardon J., Fuller-Tyszkiewicz M. (2020). Attrition and adherence in smartphone-delivered interventions for mental health problems: A systematic and meta-analytic review. Journal of Consulting and Clinical Psychology, 88(1), 1–13. 10.1037/ccp0000459 [DOI] [PubMed] [Google Scholar]
- Lohan M., Aventin Á., Oliffe J. L., Han C. S., Bottorff J. L. (2015). Knowledge translation in men’s health research: Development and delivery of content for use online. Journal of Medical Internet Research, 17(1), e31. 10.2196/jmir.3881 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maeda E., Boivin J., Toyokawa S., Murata K., Saito H. (2018). Two-year follow-up of a randomized controlled trial: Knowledge and reproductive outcome after online fertility education. Human Reproduction, 33(11), 2035–2042. 10.1093/humrep/dey293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maeda E., Nakamura F., Kobayashi Y., Boivin J., Sugimori H., Murata K., Saito H. (2016). Effects of fertility education on knowledge, desires and anxiety among the reproductive-aged population: Findings from a randomized controlled trial. Human Reproduction, 31(9), 2051–2060. 10.1093/humrep/dew133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahalik J. R., Backus Dagirmanjian F. R. (2018). Working men’s constructions of visiting the doctor. American Journal of Men’s Health, 12(5), 1582–1592. 10.1177/1557988318777351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panner Selvam M. K., Ambar R. F., Agarwal A., Henkel R. (2021). Etiologies of sperm DNA damage and its impact on male infertility. Andrologia, 53(1), e13706. 10.1111/and.13706 [DOI] [PubMed] [Google Scholar]
- Pedro J., Brandão T., Schmidt L., Costa M. E., Martins M. V. (2018). What do people know about fertility? A systematic review on fertility awareness and its associated factors. Upsala Journal of Medical Sciences, 123(2), 71–81. 10.1080/03009734.2018.1480186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ravitsky V., Kimmins S. (2019). The forgotten men: Rising rates of male infertility urgently require new approaches for its prevention, diagnosis and treatment. Biology of Reproduction, 101(5), 872–874. 10.1093/biolre/ioz161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robins S., Barr H. J., Idelson R., Lambert S., Zelkowitz P. (2016). Online health information regarding male infertility: An evaluation of readability, suitability, and quality. Interactive Journal of Medical Research, 5(4), e6440. 10.2196/ijmr.6440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schlegel P. N., Sigman M., Collura B., De Jonge C. J., Eisenberg M. L., Lamb D. J., Mulhall J. P., Niederberger C., Sandlow J. I., Sokol R. Z., Spandorfer S. D., Tanrikut C., Treadwell J. R., Oristaglio J. T., Zini A. (2021). Diagnosis and treatment of infertility in men: AUA/ASRM guideline part I. Fertility and Sterility, 115(1), 54–61. 10.1016/j.fertnstert.2020.11.015 [DOI] [PubMed] [Google Scholar]
- Sharma A., Minhas S., Dhillo W. S., Jayasena C. N. (2021). Male infertility due to testicular disorders. The Journal of Clinical Endocrinology and Metabolism, 106(2), e442–e459. 10.1210/clinem/dgaa781 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Usability.gov. (n.d.). Recruiting Usability Test Participants. Retrieved March 1, 2021 from https://www.usability.gov/how-to-and-tools/methods/recruiting-usability-test-participants.html
- Wojcieszek A. M., Thompson R. (2013). Conceiving of change: A brief intervention increases young adults’ knowledge of fertility and the effectiveness of in vitro fertilization. Fertility and Sterility, 100(2), 523–529. 10.1016/j.fertnstert.2013.03.050 [DOI] [PubMed] [Google Scholar]
- Zegers-Hochschild F., Adamson G. D., Dyer S., Racowsky C., De Mouzon J., Sokol R., Rienzi L., Sunde A., Schmidt L., Cooke I. D., Simpson, J. L., & van der Poel, S. (2017). The international glossary on infertility and fertility care, 2017. Human Reproduction, 32(9), 1786–1801. 10.1093/humrep/dex234 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-jmh-10.1177_15579883211049027 for Risky Business: Increasing Fertility Knowledge of Men in the General Public Using the Mobile Health Application Infotility XY by Katya Kruglova, Eden Noah Gelgoot, Peter Chan, Kirk Lo, Zeev Rosberger, Emilie Bélanger, Jordana Kazdan, Stephanie Robins and Phyllis Zelkowitz in American Journal of Men’s Health
Supplemental material, sj-docx-2-jmh-10.1177_15579883211049027 for Risky Business: Increasing Fertility Knowledge of Men in the General Public Using the Mobile Health Application Infotility XY by Katya Kruglova, Eden Noah Gelgoot, Peter Chan, Kirk Lo, Zeev Rosberger, Emilie Bélanger, Jordana Kazdan, Stephanie Robins and Phyllis Zelkowitz in American Journal of Men’s Health