Abstract
Ophthalmic emergencies are invariably challenging for the non-specialist to identify and evaluate, and may be complicated by occult but vision threatening raised intraocular pressure. We present a case of hypertensive uveitis accompanied by the finding of retinal arterial pulsation, which when visualised by direct ophthalmoscopy allows the non-specialist to identify significantly raised intraocular pressure requiring urgent evaluation by an ophthalmologist.
Keywords: Retinal artery pulsation, arterial, raised intraocular pressure
Introduction
Ophthalmic emergencies are notable for being inherently challenging to identify and evaluate in the absence of specialist equipment. They can pose particular difficulties when they present to primary care physicians with limited ophthalmic experience, as is often the case.
Some of these emergencies are characterised by an acute rise in intraocular pressure (IOP). Chief among ocular hypertensive emergencies is acute angle closure (AAC), which can cause irreversible visual loss via damage to the optic nerve head, while presenting with often vague or non-localising symptoms. While ocular pain, ocular redness, visual loss and a fixed, mid-dilated pupil are textbook presenting features, the initial presentation may be as vague as ‘headache’, ‘off legs’ or ‘vomiting’. Furthermore, IOP spikes not attributable to AAC may also occur, again without the textbook features of AAC.
We present a case of acutely raised IOP not attributable to AAC, where the sparsely documented finding of retinal arterial pulsation was noted at the time of presentation. This finding implies an acutely raised IOP, may be visualised with a direct ophthalmoscope and should alert the non-specialist to the presence of acute ocular hypertension and the need for emergency ophthalmic referral.
Case
An 18-year-old male presented to the Eye Emergency Department at a tertiary eye centre complaining of a 2-day history of blurred vision in the left eye accompanied by mild redness and aching. There was no watering, discharge, photophobia, floaters or flashes, and he was asymptomatic with respect to his right eye. The patient denied any foreign body or other recent ocular injury, nor any similar preceding episodes. Review of systems was unrevealing, in particular he denied rashes, cold sores, malaise or recent intercurrent illness. His past ocular history and past medical history were similarly unremarkable.
The best-corrected visual acuity was measured at 6/5 in both eyes despite subjectively blurred vision on the left. A slit-lamp biomicroscopy showed the right eye was normal. The left eye had ciliary injection with signs of anterior chamber inflammation. 1 + cells with minimal flare was observed, as were numerous fine keratic precipitates (KPs) on the inferior corneal endothelium of the left eye. Both anterior chambers were deep and no notable abnormalities of iris or vitreous were observed in either eye. The IOPs were recorded as 18 mmHg in the right eye and 35 mmHg in the left (normal range < 21 mmHg) by Goldman applanation tonometry.
On funduscopy, spontaneous retinal arterial pulsation could be seen at the disc in the left eye, as per the Supplementary Material. There was no corresponding pulsatile activity in the right eye, and no spontaneous venous pulsation (SVP) could be seen in either eye.
The clinical impression was of acute anterior uveitis with relatively modest anterior chamber inflammation, complicated by raised IOP. There were no signs clearly indicating any underlying aetiology to the uveitis, and it was therefore presumed to be viral in nature, viral uveitis being a frequent cause of uni-ocular hyptertensive uveitis. The patient responded well to topical pressure lowering agents, with an IOP measuring 18 mmHg 1 hour after administration. Typically, these cases are highly responsive to topical steroids, and therefore, prednisolone acetate 1% drops were given four times daily. Antiviral agents were not given in the absence of granulomatous or severe inflammation or corneal involvement. The patient was discharged with regular Dorzolamide + Timolol drops to the left eye to control the IOP, a tapering course of topical steroid and a short course of topical cycloplegic therapy for comfort. Review was scheduled in clinic over the following weeks.
The patient did not attend initially scheduled follow-up; however, he was seen some months later in clinic. At this point, he reported rapid resolution of his symptoms with complete return to subjective normality of his eyes. Clinical examination confirmed entirely normal findings with full visual function. He was subsequently discharged and has not re-presented to our eye service.
Discussion
The present case illustrates the potential clinical subtlety of presentations of raised IOP. This gentleman had only mild redness; he complained of no photophobia and retained 6/5 vision in the affected eye in spite of subjective visual blur. Specific diagnostic clinical signs in this case of low to moderate level anterior segment inflammation are impossible to detect without the use of a slit lamp. Despite this, his IOP was elevated to a level capable of causing irreversible damage to the optic nerve. Typical symptoms of raised IOP such as headache, nausea and vomiting, and typical signs such as corneal clouding, a mid-dilated non-reactive pupil and significantly reduced vision were notably absent in this case. These may not occur until the IOP is far higher and optic nerve damage is inevitable or has already occurred.
Acute rises in IOP are most commonly caused by AAC, although hypertensive uveitis and other entities may infrequently be responsible. In AAC, the most common pathological process is of enlarging cataract progressively narrowing the drainage angle for aqueous humour in an already susceptible eye (usually hypermetropes with an already narrow angle) which then closes precipitously, resulting in a dramatic elevation of IOP. The burden of this condition is likely to increase over the coming years as the population ages and cataract prevalence increases. This may be further exacerbated by pandemic-related delays in elective cataract surgery provision and advanced presentation. For these reasons, diagnostic signs available to the front-line practitioner will be increasingly valuable.
On funduscopy, the retinal vasculature is clearly visible in a healthy eye, and arteries can be distinguished from veins by their smaller calibre, lighter colour, more prominent light reflexes, general tendency to cross over the veins (roughly 70% of crossings 1 ), and to arise nasally to the vein in the optic nerve head – as can be seen in Figure 1.
Figure 1.
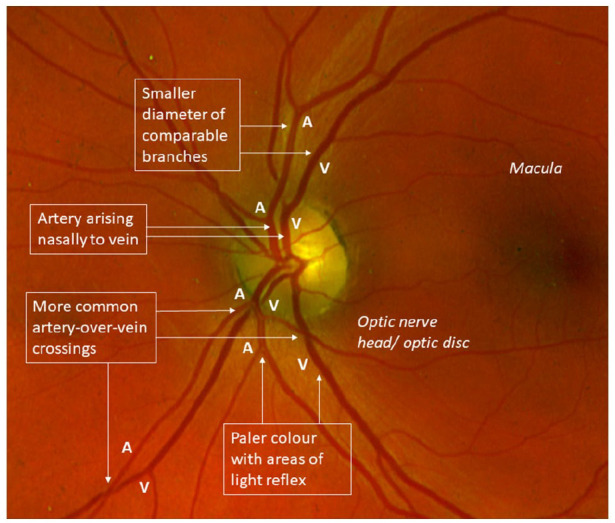
Annotated false colour image of a left eye of a healthy subject showing characteristics of retinal arteries versus that of veins.
Pulsations in this vasculature, generally at the point of leaving the optic nerve head, have been of interest to ophthalmologists for over a century. 2 SVP can be seen in around 70% of healthy individuals, is well characterised and has considerable diagnostic utility in the non-invasive exclusion of raised intracranial pressure (ICP) – that is, if SVP present, then having a raised ICP is very unlikely. 3 An example of SVP is shown in the Supplementary Material.
Arterial pulsation in contrast is much less frequently observed clinically and is less well recognised as a useful sign for the non-specialist practitioner, though it has seen application in the past in the form of ophthalmodynamometry, where the retinal vessels are observed while IOP is manipulated in order to ascertain the pressure in these vessels. 4 Visible retinal artery pulsation arises from a pathological state (as opposed to SVP which is physiologic) in which IOP greater than diastolic retinal arterial pressure causes partial or complete collapse of the vessel during part of the cardiac cycle. This is followed by re-filling of the artery as systolic arterial pressure once more exceeds IOP during cardiac systole. From calculations derived from animal studies, this occurs when IOP reaches roughly 33 mmHg in a person with normal blood pressure. 5 Consequently, this sign indicates that there is an IOP rise sufficient to cause significant optic nerve compromise and merits urgent investigation and aggressive management. It is worth noting that clinically significant IOP rises may not produce this pulsation, hence lack of pulsation is not indicative of a normal IOP.
Retinal arterial pulsation may be observed with a direct ophthalmoscope, if present, and would be most easily visible with moderate IOP rise of recent onset. Prolonged or higher pressure rises are likely to precipitate corneal oedema, obscuring the fundus view. Funduscopy may in any case be challenging, particularly in AAC where lens opacity is often a factor. While mydriatic drops are contraindicated in AAC, the mid-dilated pupil unresponsive to light may present a fundoscopic advantage.
Given the very different clinical significance of arterial pulsation and venous pulsation, it is important to differentiate the two, and this is done largely by clarifying which vessel is pulsating based on features mentioned previously.
Arterial pulsation – takes place in a vessel which is thinner, lighter, with greater light reflex, which is more likely to cross over and to arise nasally compared to its venous counterparts, and is more likely to be unilateral on the side of symptoms. This is a pathological finding, but may not be present even if the IOP is significantly raised.
Venous pulsation – takes place in a vessel which is larger, darker and more red, with lesser light reflex, which is more likely to be crossed over and to arise temporally compared to its arterial counterparts. It may be present bilaterally, or in affected or unaffected eyes. This is a physiological finding, but is not always present in healthy individuals.
Conclusion
To summarise, we have described a case of acutely raised IOP due to hypertensive uveitis; discussed the importance and difficulty of identifying raised IOPs in the non-specialist care setting; discussed the appearance of normal retinal vasculature and the differing features of venous versus arterial pulsation; and presented the utility of retinal arterial pulsation as an indicator of acutely and dangerously raised IOP.
In general practice or acute settings where there is likely to be no capacity for measuring IOP, a sign visible by direct ophthalmoscopy may be invaluable. While retinal arterial pulsation may not reveal the aetiology of the problem in the absence of slit-lamp examination, it would definitively inform the nature and urgency of onward referral and may allow the receiving specialist to more accurately triage the patient. It is our opinion that this sign should be actively sought by the non-ophthalmic specialist faced with acute uni-ocular pain with or without visual loss.
Supplemental Material
Supplemental material, sj-pdf-1-sco-10.1177_2050313X211054633 for Retinal arterial pulsation as an indicator of raised intraocular pressure by George Benjamin Berrett, Jeffry Hogg and William Innes in SAGE Open Medical Case Reports
Acknowledgments
There are no other contributors listed as authors.
Footnotes
Author contributions: G.B.B. contributed to literature review and research, drafting of the manuscript, manuscript editing in response to comments and final approval of the manuscript. J.H. contributed to data collection, obtaining appropriate consent, manuscript review and comments, and final approval of the manuscript. W.I. contributed to supervision, manuscript review and comments, and final approval of the manuscript.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: Our institution does not require ethical approval for reporting individual cases or case series.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed consent: Written informed consent was obtained from the patient(s) for their anonymised information to be published in this article.
Patient consent: Patient consent has been received and may be produced if required.
ORCID iD: George Benjamin Berrett  https://orcid.org/0000-0003-0080-9507
https://orcid.org/0000-0003-0080-9507
Supplemental material: Supplemental material for this article is available online.
References
- 1. Weinberg D, Dodwell DG, Fern SA. Anatomy of arteriovenous crossings in branch retinal vein occlusion. Am J Ophthalmol 1990; 109(3): 298–302. [DOI] [PubMed] [Google Scholar]
- 2. Elliot RH. The retinal pulse. Br J Ophthalmol 1921; 5(11): 481–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Morgan WH, Hazelton ML, Yu DY. Retinal venous pulsation: expanding our understanding and use of this enigmatic phenomenon. Prog Retin Eye Res 2016; 55: 82–107. [DOI] [PubMed] [Google Scholar]
- 4. Morgan WH, Yu DY, Alder VA, et al. Relation between pressure determined by ophthalmodynamometry and aortic pressure in the dog. Br J Ophthalmol 1998; 82(7): 821–825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Morgan WH, Yu DY, Cooper RL, et al. Retinal artery and vein pressures in the dog and their relationship to aortic, intraocular, and cerebrospinal fluid pressures. Microvasc Res 1997; 53(3): 211–221. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-sco-10.1177_2050313X211054633 for Retinal arterial pulsation as an indicator of raised intraocular pressure by George Benjamin Berrett, Jeffry Hogg and William Innes in SAGE Open Medical Case Reports


