Abstract
Health equity is attained when everyone has the opportunity achieve the health they envision; however, health disparities are a barrier to health equity. As health disparities specific to urogynecology exist, it is critical to examine and contextualize them in a framework that improves understanding of what factors may drive these disparities to craft effective solutions. This article will review what we currently know about urinary incontinence (UI) disparities and provide a framework for evaluation as well as a framework for advancing health equity in the care of diverse patient populations with UI.
Introduction
Health Equity is “the absence of unfair and unavoidable or remediable differences in health among population groups defined socially, economically, demographically and geographically.”1 Health care disparities are a barrier to health equity for all populations and pose a significant economic burden on society. The role that social determinants of health play in driving health disparities are well established. Racial/ethnic disparities in health and health care in particular are driven by the influence of systemic racism on social, political and structural determinants of health,2 and these health inequities pose a significant economic burden on society. A 2009 study found that between 2003 and 2006, 30.6% of direct medical care expenditure for African-Americans, Hispanics, and Asians were excess costs due to health inequities.3 Furthermore, that study showed that eliminating health disparities for minorities would have reduced direct medical care by $229.4 billion between 2003–2006. Beyond the economic impact of health disparities, there is a moral case to evaluate root causes in all medical fields and craft solutions to address these disparities.
In the field of urogynecology, where care centers on improving quality of life, equity must be at the forefront of our care delivery and health outcomes. There is currently a paucity of robust data on health disparities related to UI and strategies to address observed disparities, which then lead to potential suboptimal prevention, diagnosis, and treatment of UI. An additional challenge in capturing disparities lies in the fact the women of color are underrepresented in most studies on UI.4 This article will review what we currently know about health and health care disparities specific to UI and provide a framework for understanding disparities and advancing health equity in our care of persons with UI.
Terminology
Health Disparity/ Health Inequity:
Healthy People 2020 defines a health disparity as a “particular type of health difference that is closely linked with economic, social, and environmental disadvantage. Health disparities adversely affect groups of people who have systematically experienced greater social or economic obstacles to health based on their racial or ethnic group, religion, socioeconomic -status, gender, age, or mental health; cognitive, sensory, or physical disability; sexual orientation or gender identity; geographic location; or other characteristics historically linked to discrimination or exclusion.”5 Concisely, health disparities are systemic and avoidable health differences that adversely affect populations that experience marginalization in society.6 The predominant cause of racial and ethnic health disparities is structural racism.7,8 As a result, health disparity does not refer to all health differences9,10 and not all health differences are health disparities. For example, if we observed that basketball athletes have higher rates of anterior cruciate ligament (ACL) injuries than non-athletes, this would be a health difference and not a health disparity. However, if athletes from a disadvantaged group experience worse outcome after ACL injury than athletes from a different group, this would be a disparity. In this article, we will often use the term health inequity when referring to gaps in health and health outcomes between populations.
Social Determinants of Health:
The World Health Organization (WHO) defines social determinants of health as the conditions in which persons are born, grow, live, work, and age, including the healthcare system. 1 They are non-biologic determinants of health.
Structural/Systemic Racism:
Structural racism according to Bailey et al refers to the “totality of ways in which societies foster racial discrimination via mutually reinforcing inequitable systems (housing, education, employment, earnings, benefits, credit, media, healthcare, criminal justice, etc.), that in turn reinforce discriminatory beliefs, values and distribution of resources.” 8
Equity:
The concept of equity is distinct from equality. While both concepts promote fairness, equality aims to achieve this by treating everyone the same regardless of need, and equity emphasizes that people should receive what they need to achieve optimal outcomes. Equity as a framework is essential in health care because it acknowledges a justice-oriented framework that different groups may require different resources to achieve optimal health. Inherent in the definitions of health disparity and health equity is the notion of social disadvantage and the concern for social justice6,9, which is at the heart of these concepts and why they demand attention.
Disparities specific to urinary incontinence. What we currently know
The available literature on disparities among patients with pelvic floor disorders is lacking relative to the body of literature on this topic for gynecologic conditions. While a systematic review of publications addressing outcome differences and disparities specific to UI is beyond this article’s scope, this section will provide an overview of what is currently known about UI disparities. As a significant portion of the disparity literature is related to race/ethnicity, it is essential to note that the relationship between race/ethnicity and UI is poorly understood. Race is a social construct, but as earlier stated, systemic racism plays a root-cause role in health disparities. Some studies suggest that there are differences in the prevalence of UI by race/ethnicity, with White women having a higher prevalence of UI compared to Black or Hispanic women.11–13 Other studies also suggest racial/ethnic differences in the prevalence of UI subtypes with a higher prevalence of urgency urinary incontinence (UUI) observed in Black women than White women, and a higher prevalence of stress urinary incontinence (SUI) in White and Mexican American women than Black women.14,15 While these studies suggest differences that are not necessarily disparities, the etiology of these differences are unknown and the following must be considered while incorporating the data from these studies. First, racial minority groups are underrepresented in many prevalence studies relative to their demographic representation in general population, making the estimates unreliable for these groups. In addition, one must consider the impact of reporting bias, where many racial/ethnic minority women may not disclose their UI symptoms. Risk factors for UI, such as some medical comorbidities such as obesity, 16 are experienced disproportionately among specific racial/ethnic populations, which also confounds this relationship.
Knowledge about urinary incontinence
While differences in UI prevalence and perceptions of UI do not indicate disparities, some studies suggest that disparities in knowledge about UI exist. Shah et al found that among care-seeking women, knowledge of UI was higher among White women than non-White women.17 White women and women with higher education levels were also more likely to demonstrate knowledge of treatment options for UI than non-White women and women with lower education levels.17 However, Kubik et al demonstrated that White women had greater knowledge about UI compared to non-White women; this finding was no longer significant when controlling for socioeconomic status.18 Another analysis of community-dwelling women found racial/ethnic disparities in knowledge proficiency about modifiable risk factors and treatment options for UI and pelvic organ prolapse (POP).19 Specifically, non-Black women of color demonstrated the most significant knowledge disparities and showed a lack of proficiency regarding any effective treatment options for both UI and POP. 19 Non-Black women of color were more likely to assume that surgery is the only treatment option for both UI and POP. Black women were less likely to recognize childbirth as a risk factor for UI, less likely to know that pelvic floor exercises could help control leakage, less likely to recognize pessaries as a treatment for UI.19
These studies highlight that the reasons behind observed racial differences in knowledge about UI are not well defined and may be explained by factors such as education level and socioeconomic status. Disparities in knowledge about pelvic floor disorders (PFD) and misbeliefs could influence care-seeking and apprehension to pursue treatment for PFDs, underscoring the importance of curating culturally competent interventions and resources to enhance knowledge about UI effectively.
Care seeking and Barriers to care and treatment seeking
Studies estimate that at least 50% of women do not seek care for UI.20,21 Understanding barriers to care can improve care-seeking in various populations. A study by Berger et al suggests that there are no racial differences in care-seeking for UI and showed no differences in care-seeking for UI between Black and White women (53% Black, 50.6% White, P = 0.64).21 However for Black women, having regular pelvic exams, which implied having regular access to health care, was associated with care seeking.21 Thus, one must consider the role of regular access to care in interpreting these results as regular access to a health care provider is associated with increased care seeking for UI22 and thus results may differ in populations with limited health care access. Another recent qualitative study found that while experiences related to UI were similar between Black, White, and Latina women, there were different perceptions about care seeking among women of different racial backgrounds.23 Specifically Latina women maintained more secrecy about UI and reported longer delays in seeking care, while White and Black women described discussing their UI symptoms with close friends and family, which normalized the symptoms and prevented care-seeking suggesting a cultural impact on care-seeking for UI. 23 Similarly Waetjen et al found that race or ethnicity, socioeconomic measures, and education were not significantly related to seeking treatment for UI.22
Several studies also suggest that when care-seeking barriers are present, they may differ across racial groups. A study of barriers to UI care among White, Black, and Latina women found that Latina women faced significantly higher barriers to care for UI than White and Black women, including cost, inconvenience, fear, and site-related factors.24 Another study examining treatment for women with SUI in a racially diverse population found that Black women were likely to consult with a specialist to address UI and were less likely to undergo active treatment.25 Dunivan et al found that elder American Indian women reported more barriers to care-seeking than historic gynecology controls. In particular, the most significant barriers to care were related to cost and inconvenience.26 In this study, the most frequently cited barriers in this cohort of American Indian women were long delays before co-pay reimbursement, with 29.7% reporting that this prevented them from seeking care and prolonged wait times for appointments, with 19.7% reporting this prevented them from seeking care.26 Almost half of the women in this study reported an annual household income less than $10,000 highlighting that socioeconomic status impacts care-seeking, although it is not solely responsible for barriers to care-seeking.26
The relationship between socioeconomic status and care-seeking barriers is demonstrated in a study that found that lower household income was associated with a decreased likelihood of discussing UI with any provider or with a specialist.27 Also, women with only a high school education were less likely to report discussing UI compared to women with graduate school education or higher.27 However, even among racial minority women from higher socioeconomic backgrounds, care-seeking barriers exist. A study of community-dwelling insured Professional African-American women found that the attitudes that PFDs are a normal part of aging and concern about insurance complexity were significant barriers to care-seeking (aOR, 5.56; 95% CI 1.46–21.23 and aOR,3.80; 95% CI, 1.39–10.33 respectively).28
Treatment for urinary incontinence
It is currently unknown if there are disparities in the rates of surgeries performed for UI, and no recent population-based studies examine the current epidemiology of surgical procedures performed for UI in the US. Boyles et al, using a federal database of outpatient surgery in the US, found 76% of women undergoing surgery between 1994 and 1996 for SUI were White compared to the 0.3% who were African-American.29 Shah et al in 2003 suggested that White women underwent surgery for SUI at higher rates than African-American women.30 The data from these studies are, however, over 20 years old and do not adjust for the incidence of UI in these populations.
Nonetheless, there are a few studies that suggest that inequities in treatment for UI exist. Washington el al found that women with Medicaid and no insurance coverage were less to participate in pelvic floor physical therapy,31 highlighting a possible inequity in access to this treatment modality. Self-pay cost of pelvic floor physical therapy are high and costs and inadequate coverage poses a barrier to this treatment, thus further studies are needed to evaluate the impact of insurance type on coverage for pelvic floor physical therapy and subsequent access to this treatment. Duralde et al reported that Black and Asian women were less likely to report being offered surgical/invasive treatments for UI.27 Among women who underwent surgery for SUI in a study of Medicare beneficiaries age 65 and older, non-White women were twice as likely to have a non-urologic complication.32 A recent study examined disparities in use of sacral neuromodulation over a 10-year period and found that minority patients (non-White) were less likely to undergo treatment than White patients (aOR 0.38, p <0.0001) as were patients who lived in the West compared to other regions of the US (aOR 0.52, p <0.0001).33 In this study the most common diagnosis for sacral neuromodulation was overactive bladder. 33
Model for understanding disparities
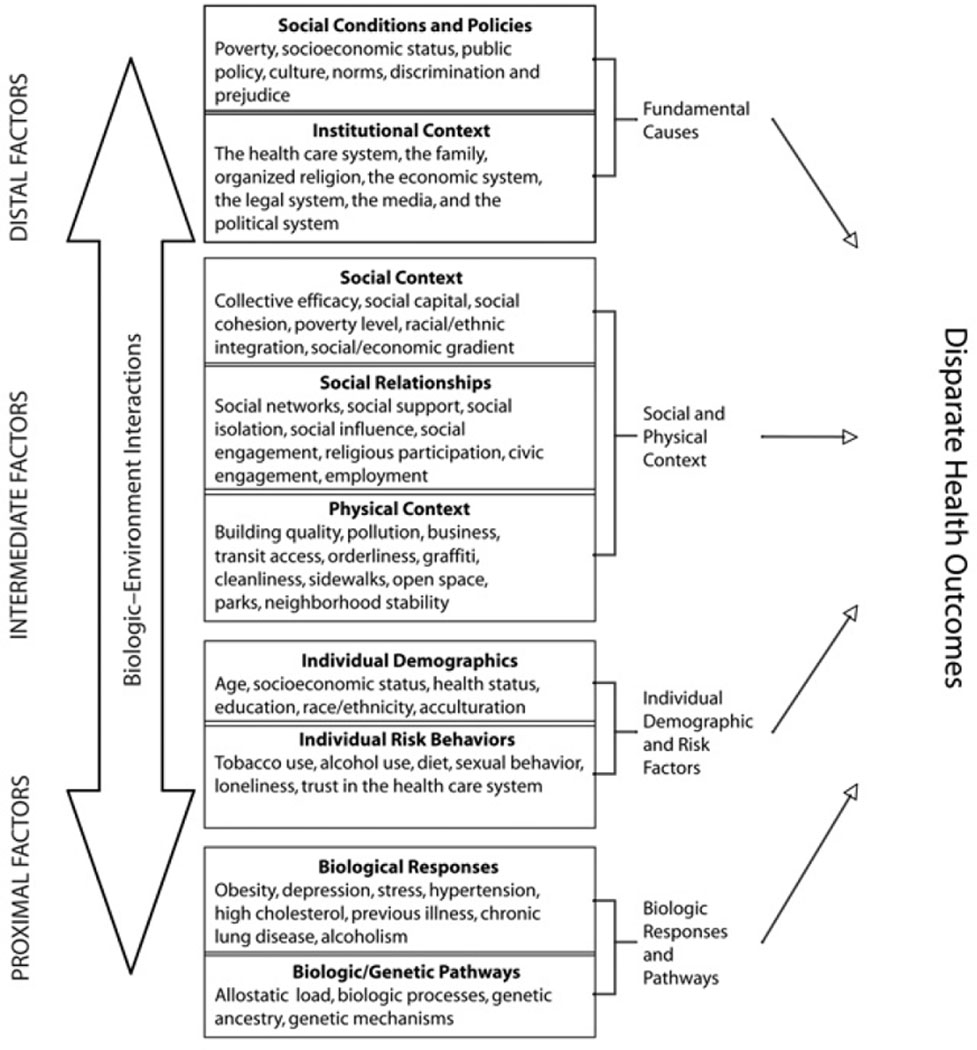
To begin to understand the drivers of the disparities discussed above and craft solutions to address health disparities, we must focus on the interplay between the multiple factors, including individual and population-level determinants of health. Disparate health outcomes are typically a result of inequities in the distribution of resources, often driven by systemic racism, that promote optimal health outcomes.10 However, a common pitfall is to reflexively attribute disparities solely to inherent differences in the groups affected, which implies a sole biologic basis for the disparity and ultimately disregards the complex relationship of several external factors that places individuals and populations at risk for disparate health outcomes. Warnecke et al present a model for analyzing health disparities shown in Figure 1. In Figure 1, three levels of health determinants are shown: distal, intermediate, and proximal factors.
Figure 1: Model For Evaluating Health Disparities.
Figure adapted with permission from Warnecke et al. Approaching Health Disparities From a Population Perspective: The National Institutes of Health Centers for Population Health and Health Disparities. American journal of public health. 2008
The distal factors are the social conditions, the policies, and policy-making bodies that impact social conditions and the healthcare system and are considered fundamental causes of disparate health outcomes at a population level. Distal factors also include legislation and governance that facilitate neighborhood-level segregation, systemic racism (which is not explicitly stated in the Warnecke et al model, but is an integral piece of the framework), inadequate health care and quality of health care, state-sanctioned violence, and political exclusion. The distal factors can impose downstream barriers that limit individuals at a population level from attaining optimal healthcare. Research evaluating how these distal social determinants of health impact care for women with UI is absent and needed. The intermediate factors are the link between the distal factors and in the individual-level factors. They are the social and physical contexts and social relationship structures that impact health. The proximal factors represent the individual demographics and risk behaviors as well as biologic responses and the environment and to disease states.
This framework assumes that health inequities do not occur as a result of one isolated factor and instead result from an interplay between multiple levels of determinants of health and underlying systemic racism. Also inherent in the framework above is the concept that certain populations may be structurally vulnerable to disparate health outcomes because of these groups experience individual patient and system mismatches; a concept highlighted in a recent publication describing a framework for health equity in gynecology oncology.34
Structural vulnerability for Native and Black women
For example, American Indian/Alaska Native (AIAN) tribes in the US have a unique history experiencing racist policies and practices that encompass genocide, marginalization and displacement from their land, which has resulted in treaties and policies to provide services to these groups. The Indian Health Service (IHS) is the agency within the Department of Health and Human Services responsible for providing federal health services to federally recognized American Indian tribes in the US. However not all Native tribes are federally recognized, thus potentially excluding some Native tribes from coverage under the IHS. The capacity for adequate coverage is also impacted by underfunding of the IHS.35 Reluctance for some tribes and AIAN people to enroll in Centers for Medicare and Medicaid Services programs has also been described for many reasons, including trust concerns about sharing personal information with non-Indian government agencies.35 These system and individual level factors can create issues with access to care, particularly subspecialized care like urogynecology for AIAN populations, and undoubtedly would contribute to health inequities in this population.
The history of slavery and the system level policies that allow neighborhood level and residential segregation, racism, economic injustice and social deprivation impact the experience of health and healthcare for many Black women in the US.8 For example, residential segregation impacts health care access, utilization, and quality of neighborhood health care and providers. The chronic divestment that results from residential segregation also worsens economic disadvantage, and creates barriers to attracting specialist care for example to facilities that are in some neighborhoods that end up being predominantly Black. 8
Structural vulnerability due to language proficiency
Many groups are impacted by the unique challenges that arise in interfacing with the US health care system with low English proficiency. Often parallel, is the experience of immigrants and the challenges and marginalization this creates and its impact on health. There are challenges in communication described in the urogynecology literature for persons with low English proficiency that impact patient knowledge of conditions and the provider-patient relationship, both of which place patients at risk for disparate outcomes. A recent study that analyzed the readability of patient information materials in Spanish for pelvic floor disorders including UI available through organizations, professional societies, government and industry found that these materials were at a range of average to difficult reading level. 36 Also, none of the analyzed materials met the sixth-grade reading level criteria suggested by the National Institutes of Health and American Medical Association.36
Another study evaluating communication between Spanish-speaking Latin-American women with pelvic floor disorders and physicians found that physicians commonly avoided medical terminology and instead used simple words when describing the patient’s diagnosis.37 Also, a common theme identified in the study was a lack of Spanish proficiency among physicians, with physicians commonly using inadequate Spanish during counseling of patients, in addition to speaking for several minutes at a time without pausing to elicit patient feedback and understanding.37 In this study, the researchers found that the patients had poor understanding of their diagnosis even at the end of the physician-patient encounter and often felt overwhelmed during the clinical encounter. 37 The communication barriers that patients with limited English proficiency meet extend beyond physician encounters and often are present at many points of interface with the health care system from office staff to interpreters,38 which can create a marginalized experience as these patients seek care. Communication deficits and barriers put patients at a disadvantage in understanding their conditions, decision making, and can place patients at risk for disparities.
Structural vulnerability for rural populations
Finally, prolonged travel to access care and limited availability of subspecialty care in some rural areas present barriers to obtaining treatment, seeking care, adherence to care, and can limit the presence of patient-chosen advocates during healthcare encounters, all of which can place persons from rural populations at risk for health inequities.
Applying a health equity framework to urinary incontinence to reduce disparities
First, it is vital to address challenges in capturing disparities related to UI. Measurement of variables presents a challenge in elucidating disparities. While not all disparities are based on race/ethnicity, the majority of the disparity studies specific to UI report on racial/ethnic disparities. However, the research describing racial differences in UI prevalence offers no etiology for these differences. Some studies that have attempted to elucidate the etiology for these differences have approached this question from a perspective that assumes inherent biologic (anatomic and physiologic) differences by race. However, we know that the race categories are flawed. Traditional race/ethnicity categories, particularly in research, do not accurately identify populations. Race is a social construct, and these categories embody significant ancestral heterogeneity, and thus are a poor proxy for genetics and ancestry. In research, race/ethnicity is not always self-identified and does not capture mixed ancestry, and the genesis of the classification criteria linking individuals in race categories is rooted in skin color.
Focusing on the “race” variable as a risk factor in disparities research models as opposed to racism and social determinants commonly experienced by the groups lumped by race, limits our ability to identify the drivers of observed racial differences and protective factors and mechanisms of resilience against adverse social determinants of health. Complex modeling systems that can consider multiple social determinants of health, bias, and cumulative risk with exposures to these determinants are needed. This sort of complex modeling would require us to craft relevant variables and objective measures to thoroughly evaluate disparities and move beyond convenient variables typically found in large databases such as annual household income, education level, and zip code that reflect deeply rooted patterns of privilege, power, and exclusion.
Another challenge in evaluating disparities in the use of treatment modalities for UI is that there are multiple treatment options for UI, and there isn’t one treatment modality that is the standard of care. As a result, when there are racial differences in the use of surgical modalities, it is difficult to discern if this results from patient preference, provider bias, or access issues. Furthermore, the data on utilization is often from administrative databases that lack information on important sociodemographic variables that could account for observed differences.
How do we move forward?
In our delivery of care, we should aim to deliver care that is free from racism and discrimination, which requires acknowledging the structural vulnerability and marginalization of certain communities, addressing systemic racism and discrimination, provider-level implicit and explicit bias. We should individualize care and leverage culture and community. Diversifying our workforce is also integral to ensuring health equity in our care. Adopting innovative solutions such as telemedicine and patient navigators offers an avenue to advance equity and address barriers to care. For example, telemedicine allows us to offer early morning and evening appointments to accommodate patients who do not have flexibility in work schedules and can overcome access and travel challenges. We acknowledge that there are equity challenges with telemedicine, such as limited internet and phone access, which need to be considered when implementing new care approaches and technology in healthcare delivery. At our individual institutions, we can advance equity by having an equity focus in our quality improvement process, by reviewing our outcomes and treatment utility for different groups to identify gaps in care provision and areas of bias. In our research, we can strive for inclusive research practices and recruitment of diverse study populations. Finally, we should incorporate equity competency in trainee and provider education.
Advancing equity must be intentional and should be central to our patient care, research, and education for UI.
References
- 1.The World Health Organization. Social determinants of Health. https://www.who.int/health-topics/social-determinants-of-health#tab=tab_1. Accessed December 1, 2020.
- 2.Williams DR, Lawrence JA, Davis BA, Vu C. Understanding how discrimination can affect health. Health services research. 2019;54(6):1374–1388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.LaVeist TA GD, Richard P. Estimating the economic burden of racial health inequalities in the United States. Int J Health Serv. 2011;41(2):231–238. [DOI] [PubMed] [Google Scholar]
- 4.Brown O, Siddique M, Mou T, Boniface ER, Volpe KA, Cichowski S. Disparity of Racial/Ethnic Representation in Publications Contributing to Overactive Bladder Diagnosis and Treatment Guidelines. Female pelvic medicine & reconstructive surgery. 2020;Publish Ahead of Print. [DOI] [PubMed] [Google Scholar]
- 5.HealthyPeople.gov. Disparities. http://www.healthypeople.gov/2020/about/disparitiesAbout.aspx. Accessed Dcemeber 1, 2020.
- 6.Braveman P. What are Health Disparities and Health Equity? We Need to Be Clear. Public health reports (1974). 2014;129(1_suppl2):5–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jones CP. Levels of racism: a theoretic framework and a gardener’s tale. American journal of public health (1971). 2000;90(8):1212–1215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bailey ZD, Krieger N, Agénor M, Graves J, Linos N, Bassett MT. Structural racism and health inequities in the USA: evidence and interventions. The Lancet (British edition). 2017;389(10077):1453–1463. [DOI] [PubMed] [Google Scholar]
- 9.Braveman PA, Kumanyika S, Fielding J, et al. Health Disparities and Health Equity: The Issue Is Justice. American journal of public health (1971). 2011;101(S1):S149–S155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Warnecke RB, Oh A, Breen N, et al. Approaching Health Disparities From a Population Perspective: The National Institutes of Health Centers for Population Health and Health Disparities. American journal of public health (1971). 2008;98(9):1608–1615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Anger JT, Saigal CS, Litwin MS. The Prevalence of Urinary Incontinence Among Community Dwelling Adult Women: Results From the National Health and Nutrition Examination Survey. The Journal of urology. 2006;175(2):601–604. [DOI] [PubMed] [Google Scholar]
- 12.Thom DH, van den Eeden SK, Ragins AI, et al. Differences in Prevalence of Urinary Incontinence by Race/Ethnicity. The Journal of urology. 2006;175(1):259–264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dooley Y, Kenton K, Cao G, et al. Urinary Incontinence Prevalence: Results From the National Health and Nutrition Examination Survey. The Journal of urology. 2008;179(2):656–661. [DOI] [PubMed] [Google Scholar]
- 14.Shah ADMD Kohli NMDMBA, Rajan SSMD Hoyte LMDM. Racial characteristics of women undergoing surgery for pelvic organ prolapse in the United States. American journal of obstetrics and gynecology. 2007;197(1):70.e71–70.e78. [DOI] [PubMed] [Google Scholar]
- 15.Sears CLG, Wright J, O’Brien J, et al. The Racial Distribution of Female Pelvic Floor Disorders in an Equal Access Health Care System. The Journal of urology. 2009;181(1):187–192. [DOI] [PubMed] [Google Scholar]
- 16.Wu JM, Vaughan CP, Goode PS, et al. Prevalence and Trends of Symptomatic Pelvic Floor Disorders in U.S. Women. Obstetrics and gynecology (New York 1953). 2014;123(1):141–148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shah AD, Shott S, Kohli N, Wu JM, Catlin S, Hoyte L. Do racial differences in knowledge about urogynecologic issues exist? International urogynecology journal and pelvic floor dysfunction. 2008;19(10):1371–1378. [DOI] [PubMed] [Google Scholar]
- 18.Kubik K, Blackwell L, Heit M. Does socioeconomic status explain racial differences in urinary incontinence knowledge? American journal of obstetrics and gynecology. 2004;191(1):188–193. [DOI] [PubMed] [Google Scholar]
- 19.Mandimika CL, Murk W, McPencow AM, et al. Racial Disparities in Knowledge of Pelvic Floor Disorders Among Community-Dwelling Women. Female pelvic medicine & reconstructive surgery. 2015;21(5):287–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Morrill MMD, Lukacz ESMD, Lawrence JMMPHS, Nager CWMD, Contreras RMS, Luber KMMD. Seeking healthcare for pelvic floor disorders: a population-based study. American journal of obstetrics and gynecology. 2007;197(1):86.e81–86.e86. [DOI] [PubMed] [Google Scholar]
- 21.Berger MB, Patel DA, Miller JM, DeLancey JO, Fenner DE. Racial differences in self-reported healthcare seeking and treatment for urinary incontinence in community-dwelling women from the EPI study. Neurourology and urodynamics. 2011;30(8):1442–1447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Waetjen LE, Xing G, Johnson WO, Melnikow J, Gold EB. Factors Associated With Seeking Treatment for Urinary Incontinence During the Menopausal Transition. Obstetrics and gynecology (New York 1953). 2015;125(5):1071–1079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Siddiqui NY, Ammarell N, Wu JM, Sandoval JS, Bosworth HB. Urinary Incontinence and Health-Seeking Behavior Among White, Black, and Latina Women. Female pelvic medicine & reconstructive surgery. 2016;22(5):340–345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Willis-Gray MG, Sandoval JS, Maynor J, Bosworth HB, Siddiqui NY. Barriers to Urinary Incontinence Care Seeking in White, Black, and Latina Women. Female pelvic medicine & reconstructive surgery. 2015;21(2):83–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McKellar K, Abraham N. Prevalence, risk factors, and treatment for women with stress urinary incontinence in a racially and ethnically diverse population. Neurourology and urodynamics. 2019;38(3):934–940. [DOI] [PubMed] [Google Scholar]
- 26.Dunivan GC, Komesu YM, Cichowski SB, Lowery C, Anger JT, Rogers RG. Elder American Indian Women’s Knowledge of Pelvic Floor Disorders and Barriers to Seeking Care. Female pelvic medicine & reconstructive surgery. 2015;21(1):34–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Duralde ER, Walter LC, Van Den Eeden SK, et al. Bridging the gap: determinants of undiagnosed or untreated urinary incontinence in women. American journal of obstetrics and gynecology. 2016;214(2):266.e261–266.e269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Washington BB, Raker CA, Mishra K, Sung VW. Variables impacting care-seeking for pelvic floor disorders among African American women. Female pelvic medicine & reconstructive surgery.19(2):98–102. [DOI] [PubMed] [Google Scholar]
- 29.Boyles SH, Weber AM, Meyn L. Ambulatory procedures for urinary incontinence in the United States, 1994–1996. American journal of obstetrics and gynecology. 2004;190(1):33–36. [DOI] [PubMed] [Google Scholar]
- 30.Shah AD, Kohli N, Rajan SS, Hoyte L. Surgery for stress urinary incontinence in the United States: does race play a role? International urogynecology journal and pelvic floor dysfunction. 2008;19(8):1085–1092. [DOI] [PubMed] [Google Scholar]
- 31.Washington BBMDMHA, Raker CAS, Sung VWMDMPH. Barriers to pelvic floor physical therapy utilization for treatment of female urinary incontinence. American journal of obstetrics and gynecology. 2011;205(2):152.e151–152.e159. [DOI] [PubMed] [Google Scholar]
- 32.Anger JT, Rodríguez LV, Wang Q, Chen E, Pashos CL, Litwin MS. Racial disparities in the surgical management of stress incontinence among female Medicare beneficiaries. The Journal of urology. 2007;177(5):1846–1850. [DOI] [PubMed] [Google Scholar]
- 33.Laudano MA, Seklehner S, Sandhu J, et al. Disparities in the Use of Sacral Neuromodulation among Medicare Beneficiaries. The Journal of urology. 2015;194(2):449–453. [DOI] [PubMed] [Google Scholar]
- 34.Temkin SM, Rimel BJ, Bruegl AS, Gunderson CC, Beavis AL, Doll KM. A contemporary framework of health equity applied to gynecologic cancer care: A Society of Gynecologic Oncology evidenced-based review. Gynecologic oncology. 2018;149(1):70–77. [DOI] [PubMed] [Google Scholar]
- 35.Warne D, Frizzell LB. American Indian Health Policy: Historical Trends and Contemporary Issues. American journal of public health (1971). 2014;104(S3):S263–S267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Robb J, Mackay A, Rondeau N, et al. Spanish Language Pelvic Floor Disorders Patient Information Handouts: How Readable Are They? Female pelvic medicine & reconstructive surgery. 2019;25(1):72–75. [DOI] [PubMed] [Google Scholar]
- 37.Sevilla C, Wieslander CK, Alas AN, et al. Communication Between Physicians and Spanish-Speaking Latin American Women With Pelvic Floor Disorders: A Cycle of Misunderstanding? Female pelvic medicine & reconstructive surgery. 2013;19(2):90–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Khan AA, Sevilla C, Wieslander CK, et al. Communication Barriers Among Spanish-Speaking Women With Pelvic Floor Disorders: Lost in Translation? Female pelvic medicine & reconstructive surgery. 2013;19(3):157–164. [DOI] [PMC free article] [PubMed] [Google Scholar]