Abstract
Many disasters that have happened in the last decades, including the latest COVID-19 pandemic, have caused a shortage of healthcare resources and change in healthcare operations. Given these impacts, the Operational Research (OR) community has applied various approaches to improve the emergency medical responses. Coordination of healthcare facilities is one of the emergency medical response strategies to ensure the continued provision of medical services during disasters. Although the existing literature reviews of OR approaches have included the perspective of healthcare management, they focused mostly on the application of OR in disaster operations and logistics management. The importance of coordination in healthcare systems during disasters is well recognised in the literature, but to the best of our knowledge there has been no review of the published research in this area. This study provides a focused literature review of the OR contributions in the coordination in healthcare systems during disasters. Definitions of the terms in use in this field are provided. An overall descriptive statistics of the reviewed articles is given, followed by the review of the presented research problems, disaster types, and developed methodologies. The main characteristics of models for the coordination in the healthcare system are described. Measures of coordination effectiveness that denote healthcare resilience are discussed. Based on our findings, we suggest future research directions in the context of existing models extension, and application and development of other methodologies with the aim to provide a solid basis for OR research in the healthcare disaster management.
Keywords: OR in health services, Disasters management, Coordination, Healthcare resilience, Emergency medical response
1. Introduction
According to the records from the UN Office for Disaster Risk Reduction, 7255 disaster events took place between 1998 and 2017 (Wallemacq, 2018). Natural disasters, technology-related incidents, terrorism events and epidemics formed the majority of these disasters. These disasters caused more than 1.3 million deaths and affected 2.5 billion of people. Some of the world's disaster events include the World Trade Centre attack in 2001, the Indian Ocean Tsunami in 2004, the earthquake in Haiti in 2010, and the latest COVID-19 pandemic in 2020, to mention just a few.
One of the most prominent systems in disaster response is the healthcare system. Healthcare systems have encountered extreme pressures from disasters (Yi, George, Paul & Lin, 2010). One of the critical organisations in the healthcare system are hospitals, which are generally recognised as a centre of medical services during disasters (Achour, Miyajima, Pascale & Price, 2014; Cimellaro, Reinhorn & Bruneau, 2010; Kruk, Myers, Varpilah & Dahn, 2015; Vanvactor, 2011). Their roles in providing timely and good quality treatments to both existing and new patients affected by a disaster become even more critical during disasters (McDaniels, Chang, Cole, Mikawoz & Longstaff, 2008). Disasters have an impact on both healthcare resources and healthcare operations as follows. First, hospitals are required to allocate some medical staff to the shelters in order to provide the initial treatments (Lodree, Altay & Cook, 2017). Hospitals, thus, need to ensure a sufficiency of medical staff at their settings in order to maintain the healthcare capability during disasters (Becker, Steenweg & Werners, 2018; Yi et al., 2010). Second, hospitals are usually required to provide an evacuation service, especially during natural disasters. Due to a limited number of available ambulances, they need to make multiple trips during such events (Repoussis, Paraskevopoulos, Vazacopoulos & Hupert, 2016). Third, a sudden surge of emergency patients causes a shortage of healthcare resources, resulting in a lower healthcare capability for a period of time (Achour & Price, 2010). Especially, a shortage of emergency beds creates bottleneck operations, resulting in higher waiting times for severe-injured patients (Xiang & Zhuang, 2016). Lastly, disasters change healthcare operations. The admission and discharge protocols are modified in order to increase the ability to accept new patients who require emergency medical services (Zhang & Howard, 2015). To better respond to future disasters, healthcare providers and institutions for social care, in both private and public sectors, need to prepare contingency plans for medical response (Boyd et al., 2012; Starr & Matinrad, 2016). For instance, after the Indian Ocean Tsunami in 2004 with more than 225,000 casualties, hospitals around the world started planning the emergency medical response for the natural disaster (Altay & Green, 2006).
Operational Research (OR) has been employed to a variety of problems to support decision making in the healthcare systems during disasters. A reasonably large number of literature reviews of disaster management have been offered by numerous OR scholars. Altay and Green (2006) reviewed the articles on disaster operations management (DOM) which covered all stages of DOM. Simpson and Hancock (2009) reviewed the articles on emergency responses in both urban and disaster services. They defined urban services as municipal services that can be provided by a single organisation, whereas disaster services referred to large-scale emergency services. Caunhye, Nie and Pokharel (2012) reviewed the optimisation models proposed for the emergency logistics problems, which included the facility location, stock pre-positioning, relief distribution and casualty transportation. Galindo and Batta (2013) analysed the trend of articles in DOM and compared them with the review by Altay and Green (2006). Their review also identified the most frequent assumptions presented in the reviewed articles. Anaya-Arenas, Renaud and Ruiz (2014) reviewed the articles in the relief distribution network focusing on logistics perspectives. Gul and Guneri (2015) reviewed the application of simulation methods in an emergency department (ED) in their normal functioning and during disaster events. The review mainly presented the frequency of use of simulation methods. Key performance indices and simulation software used in the reviewed articles were presented. Özdamar and Ertem (2015) provided a comprehensive review of the mathematical models for mass evacuation, casualty transportation, and relief distribution. Gutjahr and Nolz (2016) provided an in-depth review of articles which addressed multi-criteria optimisation for humanitarian aid. The multicriteria deterministic and stochastic optimisation models for different stages of DOM were presented. Ahmadi-Javid, Seyedi and Syam (2017) reviewed the articles on the healthcare facility location in both non-emergency and emergency situations. The review presented the main characteristics of the models and optimisation methods for the healthcare facility location. Esposito Amideo, Scaparra and Kotiadis (2019) reviewed the optimisation models developed for shelter locations and evacuation routing. The review also discussed the challenges in developing realistic optimisation models by considering the applicability of models in real-world cases. Mishra, Kumar and Hassini (2019) reviewed the applications of simulation methods in disaster management. The review mainly presented a broad analysis of different simulation methods in the context of disaster management. Recently, Farahani, Lotfi, Baghaian, Ruiz and Rezapour (2020) reviewed the articles in the casualty management in humanitarian operations which included resource dispatching, search and rescue, on-site medical operations and patient transportation. Sabbaghtorkan, Batta and He (2020) reviewed articles which investigated prepositioning and allocations of healthcare supplies.
Table 1 presents a summary of exiting reviews of OR applications in disaster management and positions our review. The columns in the table show the authors, the review focus, the stages of DOM, the disaster types, and the time period of articles covered in the review. The last column shows the level of details presented in the review. The existing reviews covered some parts of disaster management. Most of them consider only the logistics management in their review including facility locations, stock pre-positioning, relief distribution network, evacuation routing, and casualty transportation. Only a few of them considered the operations management of entire activities in different stages of DOM. Most of them covered all types of disasters, whereas a few reviews covered only natural disasters.
Table 1.
Literature reviews of OR applications in disaster management.
| Author(s) | Focus of literature review | Scope of study |
Review includes | ||
|---|---|---|---|---|---|
| Stages of DOM | Types of disaster | Period surveyed | |||
| Altay and Green (2006) | - DOM | Mit, Pre, Res, Rec | Nat, Man | 1980 – 2004 | Sol |
| Simpson and Hancock (2009) | - Emergency response in urban services and disaster services | Res | Nat, Man | 1965 – 2007 | Sol |
| Caunhye et al. (2012) | - Optimisation models for emergency logistics | Mit, Pre, Res | Nat, Man | 1980 – 2010 | Par, Var, Obj, Cons |
| Galindo and Batta (2013) | - Evaluation of the trend of articles on DOM and comparison with the review by Altay and Green (2006) | Mit, Pre, Res, Rec | Nat, Man | 2005 – 2010 | Assump, Sol |
| Anaya-Arenas et al. (2014) | - Relief distribution network focusing on logistics perspective - Models for location-network design and humanitarian aid transportation |
Res | Nat, Man | 1990 – 2013 | Obj, Cons, Sol |
| Gul and Guneri (2015) | - Simulation models in an ED | N/A | Nat, Man | 1968 – 2013 | Obj |
| Özdamar and Ertem (2015) | - Models for mass evacuation, casualty transportation, and relief distribution | Res, Rec | N/A | 1998 – 2014 | Obj, Cons, Sol |
| Gutjahr and Nolz (2016) | - Multicriteria optimisation in humanitarian aid - Optimisation criteria in humanitarian aid |
Mit, Pre, Res, Rec | Nat | 2007 – 2015 | Par, Obj, Sol |
| Ahmadi-Javid et al. (2017) | - Healthcare facility location in both non-emergency and emergency situations - Models for healthcare facility location |
N/A | N/A | 2004 – 2015 | Par, Var, Obj, Cons, Sol |
| Esposito Amideo et al. (2019) | - Optimisation models developed for shelter location and evacuation routing - Challenges in developing applicable optimisation models for these problems |
Res | Nat, Man | 1980 – 2016 | Par, Obj, Cons, Sol |
| Mishra (2019) | - Simulation models in disaster management | Mit, Pre, Res, Rec | Nat, Man | 2000 – 2016 | Sol |
| Farahani et al. (2020) | - Casualty management | Res | Nat, Man | 1977 – 2019 | Assump, Par, Var, Obj, Cons, Sol |
| Sabbaghtorkan et al. (2020) | - Prepositioning and allocation of healthcare supplies | Mit, Pre | Nat | 2000 – 2018 | Var, Obj, Cons |
| This review | - Coordination in the healthcare systems - Measures of healthcare resilience |
Res | Nat, Man | 2005 – 2020 | Par, Var, Obj, Cons |
Note: Mit - Mitigation, Pre - Preparedness, Res - Response, Rec - Recovery, Nat - Natural, Man - Man-made, Assump - Main assumptions, Par - Parameters, Var - Key decision variables, Obj - Objective functions, Cons - Main constraints, Sol - Solution approach, N/A - Not applicable.
The importance of coordination in the healthcare systems during disasters is well recognised in the literature. The coordination allows pooling of healthcare resources to ensure the continued provision of medical services in the healthcare network during disasters (Kruk et al., 2015; Rolland, Patterson, Ward & Dodin, 2010). The lack of coordination of multiple healthcare facilities for emergency medical response results in the managerial confusions and ambiguity of authority in the collective response during disasters (Espíndola, Albores & Brewster, 2018). The practice of the coordination in the healthcare system proved to be very useful during the COVID-19 outbreak. When the medical supplies at Wuhan Red Cross were in shortage, Red Cross in other cities in China shared with them respirator masks, medical protective suits, and some medicine in order to enhance the healthcare capability in the city and to reduce the spread of COVID-19 in China (CNN.com, 2020). The healthcare providers in Italy have shared their testing kits, beds, and ventilators in response to a surge of infected patients and coordinated the development of protocols and procedures of healthcare operations and medical treatments in order to mitigate the impacts of COVID-19 on the healthcare system (Carenzo et al., 2020). When the United States experienced an increase in the number of infected patients, there was a need to manage the ventilator allocation at the national level, resulting in a sharing of ventilators between states (covidanalytics.io, 2020). States which had available ventilators were required to allocate some ventilators to the states that were expected to have the ventilator shortage in the upcoming weeks.
Studies on disaster management claim that a highly proactive and functioning healthcare-network delivery is needed. Disaster response plans require a collective effort such as healthcare-network actions, rather than an individual effort from a single hospital (Kruk et al., 2015; Ogawa, Kaneko, Kajihara, Sano & Munechika, 2016; Rolland et al., 2010; Vanvactor, 2011). The National Health Service (NHS) in the UK claims that the coordination with other agencies to provide emergency medical response enhances the ability to respond to disasters (GOV.uk, 2019). There is a limit to what any individual institution can achieve without support from other institutions. For instance, disaster responses that assess each hospital facility in isolation fail to account for patients reallocation from one facility to another (Zhang & Howard, 2015). It affects the ability of the healthcare system to admit new patients. Independent participation of different organisations during two major floods in Mexico and their independent decision-making caused an ineffective response and an inefficient use of resources (Espíndola et al., 2018). The lack of coordination amongst humanitarian organisations during natural disasters can cause higher operational costs, response times, and inefficient emergency resource allocation (Pazirandeh & Maghsoudi, 2018).
However, to the best of our knowledge, there has been no comprehensive review of OR methodologies applied in the healthcare management with focus on coordination in the healthcare system during disasters. The interviews that we conducted with the health authorities and medical staff in Thailand, who experienced the Tsunami disaster in 2004, proved the importance of coordination of healthcare services in such events. Hospitals in the affected areas were disorganised while allocating the disaster victims because there was no coordination agreement in response to Tsunami. This provided further motivation for our review.
The contributions of this review are as follows. First, this is the first review of OR articles that discusses the coordination of the integrative and collaborative care in the healthcare systems during disasters. We classify the articles by the research problems they addressed, disaster types, and the methodologies they developed/used. The main characteristics of mathematical models for the coordination are analysed. Second, the review analyses the proposed measures of coordination effectiveness. Third, we provide the clarification of the terminology that has been in use across the published articles. A part of this terminology, which originated in a medical field, has to be precisely defined to be consistently used in the OR fields. Finally, we highlight the possible future research directions deriving from our findings.
The remainder of the article is organised as follows. The scope of the study is presented in Section 2. Section 3 explains the search process used in the review. Section 4 presents an analysis of OR articles on coordination in the healthcare systems. A review of measures of coordination effectiveness is given in Section 5. Section 6 suggests future research directions followed by Section 7 which presents our remarks and conclusions.
2. Terminology and scope of the study
The first step in our literature review is to define and explain the terminology which is in use in the reviewed articles. This helps in highlighting precisely the scope of our study.
2.1. Disasters
This study is not limited to any particular type of disasters because healthcare systems have encountered extreme pressures from different types of disasters, including natural disasters and man-made disasters (Yi et al., 2010). All these disasters have created a surge of demands for medical services and caused a shortage of healthcare resources in the affected areas. We adopt the term disasters defined by Galindo and Batta (2013) to establish the scope of our study. Their definition encompasses other definitions. They define disasters as “a shocking event that seriously disrupt the functioning of a community or society, by causing human, material, economic or environmental damage that cannot be handled by local agencies through standard procedures”.
2.2. Stages of DOM
There are four stages of DOM, including mitigation, preparedness, response, and recovery (Altay & Green, 2006). The mitigation stage aims to predict potential dangers as well as to develop necessary action plans in order to alleviate the effects of upcoming disaster events. The goal of the preparedness stage is to reduce the potential economic, social and physical impacts of a disaster as well as to facilitate the use of resources for response and disaster relief. In the response stage, available resources are allocated, coordinated and managed, with the efforts to enhance the post-disaster survival rates and economic growth. The recovery stage aims to restore some resemblance of normality after a disaster. Interested readers can refer to Altay and Green (2006) for more details about objectives and activities of different stages.
Our review is focused on the response stage of DOM. When disasters happen there is often a shortage of healthcare resources even if some emergency medical plans have been developed in advance. The healthcare environment during disasters is characterised by high level of variations which drive the need for adaptation plans (Fairbanks et al., 2014). For instance, a surge of patient demand, and an inappropriate staffing are common variations in the conditions of work and require adaptation. The changes in clinical pathway to meet a surge of demands as well as the flexible medical staff assignment to perform medical services have to be implemented for a better disaster response (GOV.uk, 2019). Therefore, devastating impacts of disasters on the healthcare systems require an efficient emergency medical response and the adaptation of healthcare operations to meet a surge of disaster victims.
2.3. Emergency medical response
Altay and Green (2006) define the term emergency response as “response to catastrophic and disaster events and do not consider daily response of ambulance, police, or fire departments”. They claim that the emergency response is needed when the event is more harmful; for example, when resources are in shortage, when non-standard procedures have to be implemented to save lives, or when special authorities have to be appealed to manage the event. Therefore, we adapt their definition and define the term emergency medical response to refer to either non-standard operations of medical services that are implemented, or standard operations of medical services that need to be adjusted to save victims in the events where healthcare resources become stressed. In this study, healthcare resources include medical staff, beds, medical equipment and medical supplies. In this definition, daily responses to routine emergency calls are excluded.
2.4. Coordination
The term coordination in the healthcare system is defined by Boon, Mior, Barnsley, Ashbury and Haig (2009) who examine the coordination of interdisciplinary healthcare teams for the good of patients. They define two different terms, namely integrative care (IC) and collaborative care (CC), to describe the corresponding coordination by considering the characteristics of workforce sharing and work dependency. Both terms are originally described as an interaction amongst medical staff working together in order to deliver medical services. IC emphasises a closer interaction on a regular basis, which is subsumed into a single entity. Medical staff from different disciplines work dependently under a common governance structure resulting in less autonomy. In contrast, CC allows medical staff to work together for a specific purpose during a period of time in order to deliver medical services. However, medical staff under CC still work independently because they have their own administrative structures. Consequently, they maintain their autonomy while working together. CC is perceived as a precondition for IC. We believe that a strong collaboration is likely to be a stepping stone towards an integration because an integration requires greater inter-dependency. However, the difference remains unclear since only workforce sharing and work dependency are considered. The sharing of other healthcare resources including medical equipment and beds as well as the decision making processes in IC and CC are not defined. Thus, we introduce additional characteristics as follows. The sharing of medical equipment and beds in IC normally occurs under a common governance structure to enable better medical service quality. In contrast, in CC these are usually implemented across governance structures. Such sharing will only be implemented for a period of time, especially during disasters, in order to improve the healthcare capability of the whole healthcare network. The decision on providing medical services during disasters should be made in a timely manner. All members under IC generally design both practice guidelines and treatment plans in advance since they work dependently under a common governance structure. Consequently, such guidelines and plans are perceived as a common agreement amongst members when decision making on provision of medical services is required. Conversely, the decision on provision of medical services under CC is made on demand basis since medical staff only work together for a specific purpose. It requires a sharing of information amongst medical staff in the decision making in order to provide proper medical services. The clear characteristics of IC and CC aid in classification of the current literature. They are summarised in Table 2 .
Table 2.
Characteristics of IC versus CC.
| Characteristics | Integrative care | Collaborative care |
|---|---|---|
| Sharing of healthcare resources | Interdisciplinary team of medical staff working together on a regular basis as part of a single entity | Interdisciplinary team of medical staff working together for a specific issue/goal during a period of time |
| Sharing of medical equipment and beds for a better allocation within the common governance structure | Sharing of medical equipment and beds to increase the healthcare capability across governance structures | |
| Dependency | Common governance structure | Independent administrative structure |
| Work dependency | Work independency | |
| Less autonomous while working together | Maintain autonomy while working together | |
| Requires collaboration | Precondition for integration | |
| Decision making | Cooperative sharing of information | Cooperative sharing of information |
| Decision on medical services is planned in advance | Decision on medical services is made on a demand basis | |
| Decision making follows common practice guidelines and treatment plans | Requires a sharing of information in the decision making |
Note: Adapted from Boon et al. (2009).
2.5. Healthcare resilience
In our study, we also review the measures of coordination effectiveness in the healthcare systems during disasters proposed in the literature. Some studies use the term healthcare resilience to describe the coordination effectiveness in the healthcare system and address different stages of DOM in their definitions. We will use the term resilience to refer to healthcare resilience in the remaining part of the article. For instance, Crowe et al. (2014) define resilience as the ability of the healthcare system to reduce the potential impact of disasters and to meet the needs of population. These measures of resilience served as objectives in the preparedness stage. Liu and Zhao (2015) define resilience as the ability of multi-hospitals network to recover its operational state, as well as the ability of sustaining its medical services to save people during disasters by the use of available healthcare resources of the network. A coordination of hospitals and the management of available resources in the network are the activities carried out in the response stage. Kruk et al. (2015) define resilience as the capacity of healthcare organisations to prepare for and effectively respond to disasters; to maintain core functions during disasters, and to reorganise functions if required. This definition includes both preparedness and response stage of DOM. It is apparent that the resilience can be perceived at the network level where the coordination of hospitals is required during disasters (J. E. Anderson et al., 2016). Interested readers can refer to Holling (1996) for an original conceptual framework for resilience in adaptive systems during disasters and to Bruneau et al. (2003) for a broad concept of seismic resilience in community system. Both studies include the healthcare system in their analysis.
As our review focuses on the response stage, we thus define the resilience as the ability of a healthcare network to respond to the impact of disasters and to adapt its emergency medical operations in order to meet better the patient demands during disasters.
Given the provided definitions of disasters, emergency medical response, coordination, and resilience, we have established the boundaries of our review.
3. Literature search and selection of articles
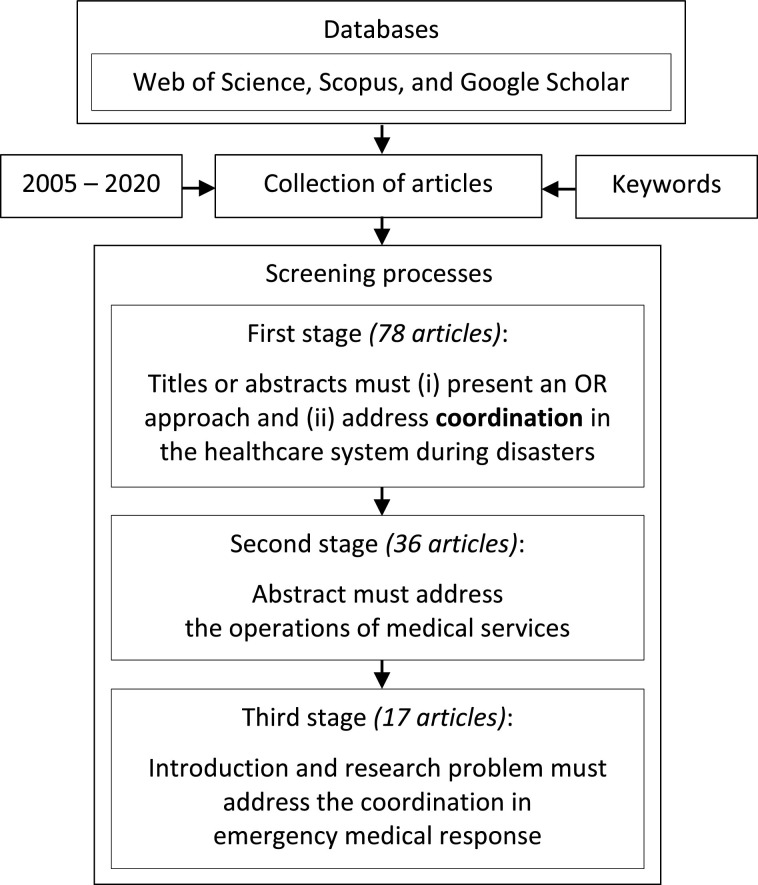
Our study focuses on articles published in OR and OR-related journals, which presented research into coordination in the healthcare system during disasters. We refer to OR-related journals as the journals that do not focus on OR in their scope, but they present articles describing OR approaches. The utilised databases include Web of Science, Scopus, and Google Scholar. Conference proceedings, book chapters, books, working papers, theses, conceptual frameworks, and practitioner magazines are not included in our review. Only publications in English are considered. Our study covers the timeframe 2005 – 2020, because prior to 2005, OR articles address mostly the mitigation phase of disaster management. Only after 2005, there have been more research interests and advancements in the response phase of disaster management. We believe that Tsunami in 2004 caused an increase in OR articles in the healthcare management. In the initial stage of our article selection, we considered articles where the following keywords were used in any place of the articles: “integrated”, “collaboration”, “coordination”, “sharing”, “allocation”, “resilience” or “resiliency”, together with one of the terms “emergency”, “disasters”, “hospital” or “healthcare”. We proceed to select the candidate articles, which fit into our scope. Our screening process is divided into three stages, which is similar to the review by Gutjahr and Nolz (2016); and Mishra et al. (2019). First, the titles and their abstracts are checked if they present an OR approach to the coordination in the healthcare system during disasters. Second, the articles that pass the first screening test are kept if they address the operations of medical services in their abstracts. Third, the last filtering is done based on the introduction and the problem description of articles, which have to address the coordination in emergency medical response. The steps taken in the review methodology are given in Fig. 1 .
Fig. 1.
Search conducted in the literature review.
Our search reveals that it is not always straightforward to determine whether the subject of an article should be classified as a disaster. For instance, the terms “disruption”, “overcrowding events”, and “crowded demand” are used in the literature to address different issues. In these situations, the following questions are considered: (1) Does the event cause a surge in patient demands? (2) Are the healthcare resources of single department or organisation in shortage during the event? The articles are retained if research problems address the surge in patient demand and the shortage of healthcare resources. In addition, articles have to address the healthcare management of the response stage of DOM. This aspect is sometimes difficult to evaluate precisely because some models presented in the articles could be applied in either the preparedness stage or the response stage of DOM. In the latter case, they are included in our list.
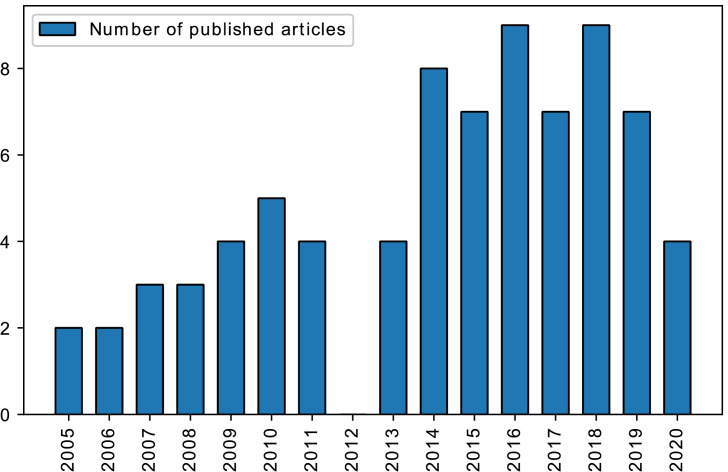
The first stage resulted in 78 articles. Fig. 2 shows the number of published articles based on the year of the publication. It can be noticed that research interests in coordination in the healthcare system during disasters have increased gradually in the last decade. The number of articles published between 2014 and 2020 almost doubled. However, the number is still relatively small taking into account the breadth and depth of research potentials in this topic as well as the complexity of the healthcare system.
Fig. 2.
Number of articles published between 2005 and 2020.
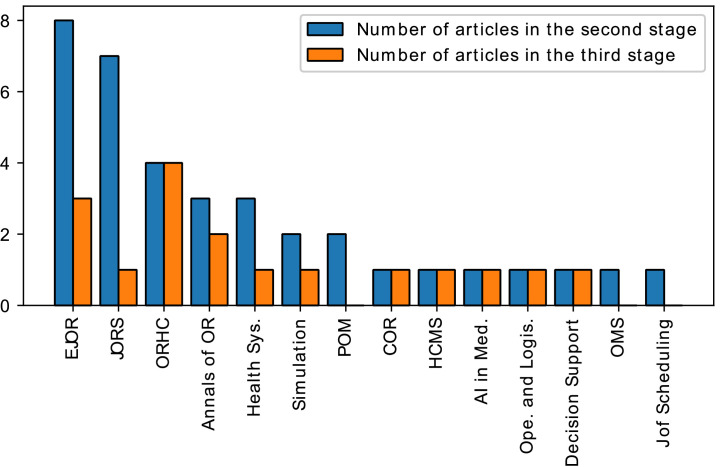
Only 36 of the retrieved articles address the operations of medical services in the abstract. They are published in European Journal of Operational Research (EJOR), Journal of the Operational Research Society (JORS), Operations Research for Health Care (ORHC), Annals of Operations Research, Health Systems, Journal of Simulation, Production and Operations Management Journal (POM), Computers and Operations Research (COR), Journal of Scheduling, Health Care Management Science (HCMS), Artificial Intelligence in Medicine, Operations and Logistics, Decision Support Systems, and Operations Management Research (OMS). Fig. 3 illustrates the distribution of published articles across these journals. There are 42 articles published in non-OR journals, mostly in medicine and engineering related journals, including Journal of Prehospital, Disaster Medicine and Earthquake Spectra. Their focus is on physical space sharing. In all of them, the research into how the undamaged hospitals can support the damaged ones by allocating their free space during disasters was reported. These articles do not fit into our scope, i.e. do not address the operations of medical services. Thus, we exclude these 42 articles.
Fig. 3.
Distribution of articles across journals.
In total, 17 articles in which the introduction and research problem address the coordination of emergency medical responses are kept to be reviewed. Fig. 3 shows the number of reviewed articles across journals. ORHC published the largest number of papers followed by EJOR and Annals of OR. In the third stage, we exclude 19 articles because all of them investigate the provision of medical services under the coordination of healthcare infrastructure during the collapse of buildings and the failure of information technology network. Collapsed buildings and failed information technology network are out of the scope of our study, which address insufficient healthcare resources where the resources include medical staff, beds, medical equipment and medical supplies.
4. OR approaches to coordination in the healthcare system
The characteristics of the reviewed articles are given in Table 3 and are discussed in detail in the remainder of this section.
Table 3.
Reviewed articles and their characteristics.
| Article | Journal | Type | Boundary | Resource | Disaster | Model/Method |
|---|---|---|---|---|---|---|
| Yi and Özdamar (2007) | EJOR | CC | Across | Staff | Nat, Man | DeterOpt (MIP) / Simple split algorithm |
| Lameris et al. (2008) | AI in Med. | IC | Within | Staff, Bed, Equip | Nat, Man | Sim (MCS) and DynOpt (IP) |
| Arora et al. (2010) | Decision Support | CC | Across | Equip | Nat | DeterOpt (IP) |
| Konrad et al. (2013) | ORHC | IC | Within | Staff | Nat, Man | Sim (DES) |
| Crowe et al. (2014) | JORS | IC | Within | Staff, Equip | Nat | DeterOpt (IP) |
| Sun et al. (2014) | COR | CC | Across | Pat | Nat | DeterOpt (MIP) |
| Lei et al. (2015) | Annals of OR | CC | Across | Staff | Nat, Man | DeterOpt (MIP) / Greedy heuristic |
| Liu and Zhao (2015) | Ope. and Logis. | CC | Across | Equip | Nat, Man | DeterOpt (MIP) |
| Zhang and Howard (2015) | Health Sys. | CC | Across | Pat | Nat | DeterOpt (MIP) |
| Chen and Wang (2016) | Simulation | IC | Within | Staff, Equip | Nat, Man | Sim (DES) and StochOpt (IP) / Multiobjective swarm optimisation |
| El-Rifai et al. (2016) | ORHC | IC | Within | Staff | Nat | StochOpt (MIP) |
| Repoussis et al. (2016) | EJOR | CC | Across | Pat | Nat, Man | DeterOpt (MIP) / Hybrid multi-start local search |
| Sung and Lee (2016) | EJOR | CC | Across | Pat | Nat, Man | DeterOpt (MIP) / Column generation |
| Yang et al. (2016) | ORHC | IC | Within | Staff | Nat, Man | Sim (DES) |
| Lodree et al. (2017) | Annals of OR | IC | Within | Staff | Nat, Man | Sim (MCS) |
| Becker et al. (2018) | HCMS | IC | Within | Staff | Nat, Man | DeterOpt (IP) |
| Niessner et al. (2018) | ORHC | CC | Across | Staff | Nat, Man | Sim (DES) and DynOpt (IP) |
Note: IC - integrative care, CC - collaborative care, Within - within a hospital, Across - across hospitals, Staff - Medical staff allocation/scheduling, Bed - emergency bed allocation, Equip – medical equipment/supplies allocation, Pat - patient flow/allocation, Nat - natural disasters, Man - man-made disasters, DeterOpt - deterministic optimisation, DynOpt - dynamic optimisation, StochOpt - stochastic optimisation, MIP - mixed integer programming, IP - integer programming, Sim - simulation method, MCS - Monte Carlo simulation, DES - discrete event simulation.
4.1. Research problem
The reviewed articles are classified into groups based on their research problems. Each article is presented in some detail. Overall, the IC articles mainly examine the sharing of healthcare resources within a hospital setting, whereas the CC articles primarily investigate the sharing of healthcare resources across hospitals to address a surge of demands for emergency medical services in the network. The common purpose of coordination is to ensure the continuity of medical services and to improve the healthcare capability during disasters. The healthcare resources that are commonly found in the reviewed articles include medical staff, emergency beds, medical equipment, and medical supplies such as syringes, antibiotics, surgical blades, vaccines, and bandages.
4.1.1. Integrative care
The literature on IC dealt with the workforce allocation to ensure a sufficient coverage within a hospital. Some reviewed articles proposed models for workforce scheduling with on-call duty to respond to disasters. Becker et al. (2018) developed a cyclic workforce scheduling with on-call duties for emergency events. Two sets of medical staff were allocated for the period of time. First set of medical staff was assigned to provide medical services on a regular basis, while the second set was assigned to perform on-call duties. When patient demand reached the usually available healthcare capability, the second set of medical staff was called in order to increase the healthcare capability during disasters. El-Rifai, Garaix and Xie (2016) also optimised the workforce scheduling with on-call duty during a seasonal epidemic. They concluded that such scheduling can save 10% of the total wage cost compared to the workforce scheduling without on-calls. Additionally, some reviewed articles presented the allocation of extra staff to respond to disasters. Lodree et al. (2017) presented the allocation of separate medical staff teams to serve different patient classes simultaneously, opposite to the normal approach where medical staff treated all patients. They found that this strategy can minimise waiting time and patients’ queue in an ED during mass casualty incidents. Yang, Lam, Low and Ong (2016) also presented the allocation of extra nurses to the triage station in order to improve the ED performance during a demand peak while considering the utilisation rate of medical staff. Konrad et al. (2013) investigated a hospital which has encountered the ED crowding caused by a surge of patient volume. They introduced the concept of split patient flow with an addition of medical staff to improve the Door-to-Doctor time. The split-flow concept classified patients considering their severity and created parallel processes. The severe-injured patients were treated using a normal ED process flow, whereas the minor-injured patients were treated in an intake area where emergency beds were not required. This study addressed the coordination by sharing the medical staff in a hospital setting and the emergency medical response by adjusting the patient flow process. This research is useful in the disaster management when the healthcare resources become stressed and the hospitals in the affected areas need to adjust the ED operations in response to a surge of victims affected by a disaster. The definition of Door-to-Doctor time will be presented in Section 5.
Some IC studies developed models for resource integration within a hospital in order to improve the healthcare capability during disasters. Crowe et al. (2014) investigated the reallocation of medical staff and medical equipment within a hospital in order to minimise unmet demand and improve the resilience during flooding. To improve resilience, the availability of care service levels for different patient classes was determined within a hospital in order to estimate the shortage levels. Both medical staff and medical equipment were allocated between departments subject to their availability of resources and the shortage levels. A few studies developed a dynamic allocation approach to improve the healthcare capability when responding to disasters. In general, the dynamic allocation refers to the adaptive allocation of healthcare resources considering the current situations such as patient demands. Lameris et al. (2008) proposed a model of dynamic resource allocation in order to achieve high service levels for all patient classes during disasters. They claimed that such allocation should be adjusted considering patient arrivals, the current and expected situations. Chen and Wang (2016) also investigated the dynamic allocation of healthcare resources in order to improve an average patient length of stay and healthcare resource wasted costs in an ED during overcrowding events. The healthcare resource wasted costs were measured by a surplus of healthcare resources in the department.
4.1.2. Collaborative care
The main focus of CC literature was on the sharing of medical staff amongst hospitals. Lei, Wang, Pinedo, Yang and Qi (2015) developed models for the allocation of medical staff to different hospitals. Medical teams from home hospitals were allocated to carry out treatments at affected hospitals. Once the treatment operations were completed, the medical teams could proceed to the next assigned hospitals. Travelling of medical teams was taken into consideration in order to minimise the total tardiness of the service operations across all hospitals in the network. Medical supplies were included in the model. However, the medical supplies were shipped from multiple distribution centres to hospitals to support medical treatments, rather than being shared between the hospitals in the network. In addition, a dynamic allocation of medical staff to affected areas was proposed in a number of articles. Such allocation aimed to enable fast-relief access and improve survivor rates in the affected areas (Altay & Green, 2006), as well as to reduce congestion at the hospitals (Galindo & Batta, 2013). Niessner, Rauner and Gutjahr (2018) investigated the physician assignment to treatment stations in a shelter. The physicians were reallocated amongst treatment stations by considering the queue lengths and the number of physicians already working at the treatment stations. Yi and Özdamar (2007) optimised the allocation of medical staff to the shelters in order to maximise the response service level and reduce congestion in the hospitals during an earthquake. The allocation concerned a trade-off between patient demands at the shelters and healthcare capacity at the hospitals. Medical staff can also be shifted from shelter to shelter considering the patient demand at the shelters.
Apart from sharing of staff, some of the reported CC approaches included sharing of medical supplies to enable resource collaboration across hospitals. Arora, Raghu and Vinze (2010) examined the regional aid by sharing the redundant amount of antiviral drugs during a pandemic flu. They employed the strategy of matching capacity to fluctuant demands in order to minimise the negative health outcomes such as number of deaths, etc. A proportion of antiviral drugs was allocated to each region for the treatment of the expected infected population, while the rest was retained in the stockpile for the later use. The pandemic might affect one region more than others, thereby leaving some regions with a shortage of antiviral drugs, and others with an excess. The regions with a shortage could therefore receive mutual aids from regions with surplus. Costs of transferring antiviral drugs between regions and the delay in transfer were to be minimised. Liu and Zhao (2015) examined the collaborative scheduling strategy across hospitals to improve the resilience in the healthcare network. Under this strategy, one hospital referred to as the main hospital providing medical services, whereas others transferred their medical supplies to it. Sung and Lee (2016) proposed a resource-constrained triage for patient allocation in the network. The priority of patients was considered while deploying the limited healthcare resources in the healthcare network. The priority was dynamically determined considering the change in the patients’ chance of survival in order to maximise the number of expected survivals.
Another purpose of CC across hospitals is to create a surge capacity between hospitals during disasters. In general, healthcare surge capacity is defined in terms of resources necessary to care for a surge of patient demands that exceeds the routine capacity (Morton, DeAugustinis, Velasquez, Singh & Kelen, 2015). Creating a surge capacity amongst nearby hospitals requires the consideration of their current availability of healthcare resources during disasters (Gutjahr & Nolz, 2016; Repoussis et al., 2016; Starr & Matinrad, 2016; Sun, Depuy & Evans, 2014). The CC allows hospitals in affected areas to share their healthcare resources in order to respond to disasters by allocating patients to hospitals where healthcare resources are available (Bayram & Zuabi, 2012). Thus, the creating of a surge capacity aims to enhance the effectiveness of patient allocation in the healthcare network, as well as to improve the ability to admit new severe-injured patients at hospitals, the number of expected survivals, and the utilisation of healthcare resources as a whole. Zhang and Howard (2015) used the skilled nursing facilities to expand the healthcare system and create a surge capacity at the hospitals during natural disasters. Minor-injured patients were allocated to the skilled nursing facilities, thus relieving the pressure on hospitals, and improving their ability to admit new severe-injured patients.
Some reviewed articles discussed a trade-off between sending patients to closest hospitals and to remote hospitals with the aim to smooth the demand. Sun et al. (2014) optimised the patient allocation by considering the total travel distance to hospitals. Repoussis et al. (2016) argued that the patient allocation to the closest hospital may cause a congestion resulting in long waiting times. Although sending patients to remote hospitals caused longer travel times, the patient allocation was more balanced and the healthcare network capacity as a whole was more effectively utilised. The patient allocation was optimised by considering the efficient use of healthcare network capacity instead of the total travel distance to hospitals.
4.1.3. Types of disaster
The reviewed articles presented in Table 3 are concerned with all types of disasters. Several disasters including Spanish influenza pandemic in 1918, Asian influenza pandemic in 1957, and in Hong Kong in 1968, Swine influenza in 1976, the World Trade Centre bombing in 2001, Tsunami in Indonesia in 2004, Hurricane Katrina in 2005, and Haiti earthquake in 2010 have drawn OR scholars’ attention to use and/or develop models and methods for disaster management. Articles that developed general models/methods and evaluated them on a specific real-world disaster are of particular interest to the OR community. For instance, Repoussis et al. (2016) developed a response model for ambulance dispatching and patient assignment for all disaster situations. They then illustrated the application of the proposed model in the terror attack on the New York Stock Exchange in Lower Manhattan in 2001. The response efficiency was examined by varying the availability of resources including ambulances and emergency beds. The models were developed to support decision making responding to events with many causalities.
4.2. Methodology and model development
Table 3 shows that development of deterministic optimisation models together with heuristic algorithms to solve larger problems is the dominant approach in the reviewed articles (Arora et al., 2010; Becker et al., 2018; Crowe et al., 2014; Lei et al., 2015; Liu & Zhao, 2015; Repoussis et al., 2016; Sun et al., 2014; Sung & Lee, 2016; Yi & Özdamar, 2007; Zhang & Howard, 2015). We would like to emphasise that a classification of an article to deterministic optimisation does not imply that the underlying problem itself is fully deterministic. Several reviewed articles included the components in the model to handle uncertainties, then solved the problem using a deterministic optimisation approach. This is mainly because, in general, deterministic optimisation methods consume less computational time and hence are able to handle larger instances. Crowe et al. (2014) advised that a simple model must be built in the first instance to reduce the computational burden. Then a more complex model with more realistic assumptions and input data to address stochastic behaviour of the problems in disasters management should be developed.
Due to the nature of the problems, developing a mixed integer programming (MIP) model was a common approach to find the optimal solutions. In these problems, decisions often involved, the selection of hospitals for patient allocation and the patient assignment to ambulances. Some reviewed articles presenting the MIP models provided the computational costs associated with the approaches used to solve the problems. Yi and Özdamar (2007) developed an MIP model to allocate medical staff to the shelters during an earthquake. They included 20 shelters and solved the problem using a two-stage procedure. In the first stage, they treated vehicles as integer commodity flows rather than binary variables. In the second stage, they used a simple vehicle splitting algorithm to generate detailed vehicle routes and pick up/delivery locations. All instances were solved in the MIP solver CPLEX 7.5 within 2 s. They also illustrated the applicability of a two-stage procedure in larger size scenarios with up to 60 nodes for which optimal solutions were obtained within 140 s. Sun et al. (2014) developed an MIP model to allocate patients to hospitals during the pandemic influenza. They divided the long planning horizon into several short planning horizons in order to shorten the run time. For example, a 2-month pandemic outbreak was divided into consecutive weekly planning horizons. The output from the previous planning horizon was used as input to the next planning horizon. Specifically, the number of patients who were admitted and the available resources from the previous planning horizon were fed in the new planning horizon as the starting condition. This approach allowed decision makers to update the system state in each weekly planning horizons. The model was solved using LINGO 11.0. Unfortunately, no data about runtime was reported. Lei et al. (2015) developed an MIP model for the allocation of medical staff to different hospitals. They used a rolling-horizon based greedy heuristic to find near optimal solutions. The search process started with a hospital sequence in which hospitals were sorted based on the starting time of their services. In each iteration, a sub-problem focused on the hospitals on the top of the list that needed the additional medical staff was solved, which in turn reduced the size of the problem. This heuristic allowed them to solve the problem with a short time horizon and to quickly obtain a solution for a given group of waiting hospitals. The best feasible solution was obtained within 2 min for 40 hospitals and within 12 min for 80 hospitals. Repoussis et al. (2016) developed an MIP model for ambulance dispatching and patient assignment during disasters and solved the model using a hybrid multi-start local search. They initially used a greedy randomised algorithm to generate the upper bound of initial solutions. Then, these initial solutions served as the starting points for an iterated Tabu search algorithm. The application of the proposed model was illustrated on large scale problem instances with up to 150 patients. The conclusion was that the iterated Tabu search algorithm considerably improved the initial solutions. Unfortunately, no CPU time required for solving the large-scale instances was given. Sung and Lee (2016) developed an MIP model for patient allocation in the network. They modelled the defined problems as a set-partitioning problem and evaluated the model on 900 instances. A column generation approach was developed which obtained near optimal solutions within a short computation time (but the exact time was not reported).
Simulation was used relatively frequently as well. Simulation was used to investigate the outcomes of a change in strategy, and to evaluate the implementation of alternative plans (Katsaliaki & Mustafee, 2011). Discrete event simulation (DES) was most widely used. Konrad et al. (2013) and Yang et al. (2016) developed DES models to examine the patient flows under IC strategy in an ED during the higher patient demands. In addition, Lodree et al. (2017) developed a Monte Carlo simulation model to simultaneously allocate different teams of medical staff to serve different patient classes in an ED during mass casualty incidents.
There was a number of research works which employed a combination of simulation and optimisation methods. Lameris et al. (2008) implemented a patient scheduling using Monte Carlo simulation, then used the optimisation method to allocate healthcare resources to patients. These methods were employed sequentially. Chen and Wang (2016) developed a multi-objective stochastic optimisation model to identify the optimal number of healthcare resources at EDs. This served as input to DES model to examine potential solutions to healthcare resource allocation problems. Different resource allocations obtained by DES were analysed by comparing performance indicators including the average patient length of stay and healthcare resource wasted cost.
More details of the developed models for IC and CC are given in Table 4 . In the medical management field, the coordination has been implemented for two main purposes: clinical integration/collaboration and resource integration/collaboration. The former can be achieved by sharing of medical staff, the latter by sharing of key resources such as medical staff, emergency beds, medical equipment and medical supplies (Bender, Connelly & Brown, 2013; Chong, Aslani & Chen, 2013; Gould et al., 2000; Johnson & Mahan, 2019; Karam, Brault, Van Durme & Macq, 2018; Lockhart-Wood, 2000). Therefore, the models proposed in the reviewed articles are classified into two categories considering the purpose of coordination: sharing of medical staff for clinical integration and clinical collaboration (second and fourth column respectively); and sharing of healthcare resources for resource integration and resource collaboration (third and fifth column respectively). The table shows the relevant objectives, parameters, decision variables, and model constraints. The models for clinical integration in IC (second column) aimed to improve the healthcare performance in an ED by sharing staff within a hospital. Objectives used in IC for clinical integration included minimisation of waiting times (Konrad et al., 2013; Yang et al., 2016), and minimisation of total costs (El-Rifai et al., 2016) in an ED. Treatment processes in an ED, service times for different processes, and patient arrival rates were taken into account in the models. Service time was defined as the total estimated time for each treatment process. The decision variables included the number of staff allocated to a particular time period. The required number of staff for a shift or a treatment process, the number of available staff and total available working times were normally perceived as model constraints for the allocation of staff. In contrast, the models for clinical collaboration in CC (fourth column) aimed to improve performance of healthcare facilities as a whole by sharing staff across hospitals. The examples of objectives included the minimisation of response times across facilities in the network (Lei et al., 2015), minimisation of number of patients waiting for medical services in the network (Yi & Özdamar, 2007), as well as the maximisation of number of treated patients in the network (Niessner et al., 2018). Characteristics of healthcare facilities in the network, travel times between healthcare facilities, and patient demands in the network were typically considered as model parameters. The decision variables included the number of staff allocated to different facilities, and the number of patients assigned to facilities after implementing the clinical collaboration. The number of staff available in different facilities, the total number of vehicles available and their load capacities were normally modelled constraints.
Table 4.
Main characteristics of the models for IC and CC.
| Integrative care (within a hospital) |
Collaborative care (in the network) |
|||
|---|---|---|---|---|
| Sharing of medical staff forclinical integration | Sharing of healthcare resourcesfor resource integration | Sharing of medical staff forclinical collaboration | Sharing of healthcare resourcesfor resource collaboration | |
| Objectives | - Minimisation of the waiting times in an ED (Konrad et al., 2013; Yang et al., 2016) - Minimisation of total cost in an ED (El-Rifai et al., 2016; Lodree et al., 2017) |
- Minimisation of the length of stay in an ED (Chen & Wang, 2016) - Minimisation of total cost in an ED (Chen & Wang, 2016; Güneş & Yaman, 2010; Lameris et al., 2008; Li, Beullens, Jones & Tamiz, 2009) - Minimisation of untreated patients in an ED (Crowe et al., 2014) |
- Minimisation of the times of service operations across healthcare facilities in the network (Lei et al., 2015) - Minimisation of number of patients waiting for medical services in the network (Yi & Özdamar, 2007) - Maximisation of number of treated patients in the network (Niessner et al., 2018) |
- Minimisation of maximum completion times of treatment (Repoussis et al., 2016) - Minimisation of travel times of all patients (Sun et al., 2014; Sung & Lee, 2016) |
| Main parameters | - Treatment processes in an ED (Konrad et al., 2013; Yang et al., 2016) - Service times for different treatment processes in an ED (Konrad et al., 2013) - Patient arrival rate (Yang et al., 2016; Lodree et al., 2017) |
- Treatment processes in an ED (Chen & Wang, 2016) - Amount of resources required to serve different patient classes (Chen & Wang, 2016; Lameris et al., 2008) - Number of patients (Crowe et al., 2014; Chen & Wang, 2016) |
- Number of healthcare facilities in the network (Lei et al., 2015) - Travel times between healthcare facilities (Lei et al., 2015) - Number of patients (Yi & Özdamar, 2007; Niessner et al., 2018) |
- Number of healthcare facilities in the network (Liu & Zhao, 2015) - Travel times between healthcare facilities or incident scene-healthcare facilities (Liu & Zhao, 2015; Repoussis et al., 2016; Sun et al., 2014; Sung & Lee, 2016) - Number of patients (Repoussis et al., 2016; Sun et al., 2014; Sung & Lee, 2016) |
| Decision variables | - Number of medical staff allocated to a particular period of time (El-Rifai et al., 2016; Konrad et al., 2013; Lodree et al., 2017; Yang et al., 2016) | - Number of healthcare resources allocated to an ED (Lameris et al., 2008; Crowe et al., 2014; Chen & Wang, 2016) | - Number of medical staff allocated to different facilities in the network (Lei et al., 2015; Niessner et al., 2018) Number of patients assigned to facilities in the network (Yi & Özdamar, 2007) | - Number of healthcare resources transferred from one facility to other (Liu & Zhao, 2015; Repoussis et al., 2016) - Number of patients assigned to facilitates (Repoussis et al., 2016; Sun et al., 2014; Sung & Lee, 2016) |
| Main constraints | - Medical staff capacity in an ED (El-Rifai et al., 2016; Konrad et al., 2013; Lodree et al., 2017; Yang et al., 2016) - Total working times in an ED (Becker et al., 2018; El-Rifai et al., 2016) - Staff requirement for a shift or a treatment process in an ED (Becker et al., 2018) |
- Healthcare resource availability in different departments (Chen & Wang, 2016; Crowe et al., 2014) - Minimum number of healthcare resources required in an ED (Lameris et al., 2008; Chen & Wang, 2016) |
- Medical staff capacity in different facilities (Lei et al., 2015; Niessner et al., 2018) - Total number of vehicles available in the network (Yi & Özdamar, 2007) - Load vehicle capacity (Yi & Özdamar, 2007) |
- Healthcare capacity in different facilities (Liu & Zhao, 2015; Repoussis et al., 2016; Sun et al., 2014; Sung & Lee, 2016) - Patient demand (Liu & Zhao, 2015; Sun et al., 2014) - Load vehicle capacity (Repoussis et al., 2016) |
Similarly to the models for clinical integration, the models for resource integration in IC (third column) aimed to improve the healthcare performance in an ED by sharing healthcare resources within a hospital. These models usually considered emergency beds, medical equipment and also medical staff. The examples of objectives were the minimisation of length of stay and costs in an ED (Chen & Wang, 2016) and minimisation of unmet demands in an ED (Crowe et al., 2014). Again, the models had treatment processes in an ED, the resources required to serve different patient classes, and patient demands as model parameters. Decision variables included the number of healthcare resources (staff, emergency beds, medical equipment, and medical supplies) allocated to an ED. These models mainly took into consideration healthcare resource availability in different departments as model constraints. On the other hand, the models for resource collaboration in CC (fifth column) were only concerned with the time improvement by sharing of healthcare resources in the whole network. Healthcare resources in different hospitals were pooled together in order to allocate patients to hospitals where healthcare resources were available, instead of assessing the resources in isolation. The examples of objectives were the minimisation of maximum completion time of treatment (Repoussis et al., 2016), and of total travel times between incident scene and healthcare facilities (Sun et al., 2014; Sung & Lee, 2016). The number of healthcare facilities, travel times between healthcare facilities or incident scene-healthcare facilities, and patient demands in the network were usually considered as model parameters. The optimal solution usually showed the number of healthcare resources transferred from one facility to other; or the number of patients assigned to facilities. The models generally took into account the healthcare capacity in different facilities, demand, and vehicle load capacity as model constraints.
To summarise, the models for clinical integration/collaboration include staff only, whereas the models for resource integration/collaboration include the key resources such as staff, beds, medical equipment, and medical supplies. The main difference between IC and CC models is that the former are mainly concerned with the allocation and resource sharing within a hospital to accomplish treatment tasks, ensure the continuity of medical services and provide the required capacity in a hospital, while the latter deal with the sharing of healthcare resources across hospitals, and take into account the capacity of healthcare resources in different healthcare facilities, and travel times between facilities to enable an efficient use of healthcare resources in the whole network.
5. Healthcare resilience measures
The primary concern of resilience is to maximise the provision of emergency medical services as well as to minimise negative healthcare outcomes (Bruneau et al., 2003). It is advocated that the resilience measures should be outcome-based describing the reduction in morbidity and mortality of the survivors (Rådestad et al., 2013). The measures are sometimes referred to as patient outcome because they are used to evaluate the improvement of population's health during disasters (Fitzpatrick, Davey, Buxton & Jones, 1998; Fries, Spitz, Kraines & Holman, 1980).
We define the characteristics of resilience measures based on the framework proposed by Kruk et al. (2017). The framework included a set of resilience indices for the healthcare system during disasters. The framework specified that the resilience measures should reveal the population health, reveal the quality of healthcare-network performance, serve as a benchmark for resilience that is comparable across different strategies of emergency medical response, and provide the information for decision makers on the required actions to improve emergency medical responses. Berg, Akerjordet, Ekstedt and Aase (2018) suggested that the resilience measures should concern the system performance as a whole rather than the performance of individual components. The characteristics of resilience measures are summarised in Table 5 .
Table 5.
Characteristics of resilience measures.
| Characteristics | Description |
|---|---|
| Population health | - Reveal the health conditions of population in the affected area. |
| Quality of healthcare-network performance | - Reveal the quality of medical services during a particular time. - Evaluate the effectiveness of collective medical response during disasters. - Concern the system performance as a whole rather than performance of individual components. |
| Benchmark | - Enable the comparison of different strategies for medical response during a particular disaster. |
| Information for decision maker | - Provide information for the decision maker or policy maker on patients’ outcome as well as the required actions of collective medical response to improve it during disasters. |
The measures found in the literature can be classified into four different categories: time-based, based on number of patients, costs, and utilisation rate.
5.1. Time-based
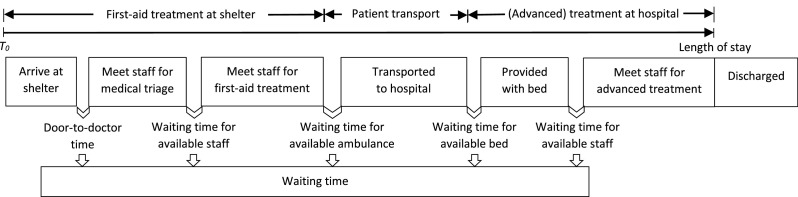
A considerable volume of literature has measured the resilience considering time including waiting time, Door-to-doctor time, and length of stay. Rolland et al. (2010) claimed that time was becoming a critical factor during disasters.
Waiting time is usually identified as the measure of medical service quality related to the availability of healthcare resources (Dansky & Miles, 1997). Waiting time is generally defined as the time elapsed between the received demand for medical service by the healthcare provider and the provision of medical service to the patient. Some studies measured the resilience during disasters using average patients’ waiting times. For example, Cimellaro and Piqué (2016) assigned weights to different patient classes where higher weight was assigned to severe-injured patient class. The sum of average weighted waiting times was then used to measure the resilience in an ED after an earthquake event. In contrast, Yang et al. (2016) measured the resilience using average waiting time for different classes, where all patient classes were assigned equal weights.
The waiting time is sometimes measured in terms of Door-to-Doctor time in order to assess the effectiveness of medical staff allocation. The Door-to-Doctor time is duration of time from a patient arriving at a healthcare facility until patient being seen by medical staff (Konrad et al., 2013). The Door-to-Doctor time is affected by the availability of medical staff, whereas the waiting time can be also affected by the availability of healthcare resources such as emergency beds, laboratory rooms, and medical staff.
The length of stay measures the total time that patient spent in the healthcare system and indicates the effectiveness of healthcare resource allocation (Chen & Wang, 2016). The length of stay includes both waiting times for healthcare resources and times spent for treatments at all stations.
The time-based measures associated with the emergency medical response during disasters are illustrated in Fig. 4 . Patients are moved from shelters to hospitals through a series of ordered medical services. The ordered services are defined in the boxes.
Fig. 4.
Time-based measures during disasters.
5.2. Based on number of patients
Several studies measured the number of patients rather than the waiting time. Ogawa et al. (2016) and J. E. Anderson et al. (2016) claimed that the goal of medical services during disasters is altered from providing the best medical services to each patient, to providing medical services to the maximum number of patients. Both number of treated patients and untreated patients were used in the literature. The number of treated patients (Bruneau & Reinhorn, 2007; Jerić & Figueira, 2012) and the minimum service level (Lameris et al., 2008) were used to represent the effectiveness of healthcare resource allocation during disasters. The minimum service level is measured as a minimum percentage of patients who received allocated healthcare resources within an acceptable waiting time. In contrast, the number of untreated patients can indicate the shortage level of healthcare resources during disasters and can be used in the capacity planning of the emergency medical response. This measure was evaluated in terms of expected death rate (Arora et al., 2010; Xiang & Zhuang, 2016), unmet demand level (Crowe et al., 2014), and loss level (Cimellaro et al., 2010). The expected death rate is the estimated number of deaths when healthcare resources become stressed. The unmet demand level is measured as a number of patients who wait for a treatment due to a shortage of healthcare resources until the healthcare resources are available. The loss level is measured as the ratio of the number of untreated patients to treated patients.
5.3. Cost-based
Studies by Chen and Wang (2016), El-Rifai et al. (2016), and Lodree et al. (2017) measured the resilience using costs. Deprivation cost represents the shortage level of healthcare resources during disasters. The deprivation cost can occur when the patient demands exceed the availability of healthcare resources. Patients need to wait until the resources are available, resulting in a delay in the treatment. The deprivation cost is thus measured as the total cost of delay for the treatment for untreated patients. The planning of resource allocation takes into account the deprivation cost when all resources are almost utilised (i.e. utilised up to a pre-determined level), especially in mass casualty incidents. The limited resources should be effectively allocated to patient classes in order to minimise the delay in treatments, so that the deprivation cost could be minimised. In addition, the deprivation cost and labour cost were sometimes simultaneously considered when staff was assigned to the shifts while trying to meet the expected patient demands.
5.4. Utilisation rate
A few studies have measured the resilience in terms of the utilisation rate. These studies stated that the utilisation rate reflected the effective use of healthcare resources during disasters. The nurse utilisation was measured when additional nurses were allocated to the treatment operations while considering the total wage cost for nurses (Griffiths, Price-Lloyd, Smithies & Williams, 2005). The utilisation rate was sometimes measured as the shortage level of healthcare resources during disasters. For instance, Harper and Shahani (2007) used the refusal rate to reflect the bed utilisation. The refusal occurred when no bed was available for an arriving patient. An increase in patient demand caused the higher refusal rate. This implied that the bed utilisation was higher because more beds were efficiently allocated to patients.
Table 6 presents a list of resilience measures proposed in the literature. The columns in the table show the characteristics of resilience measures.
Table 6.
Healthcare resilience measures.
| Category | Quantitative measures found in literature | Characteristics of healthcare resilience measurement |
|||
|---|---|---|---|---|---|
| Population health | Quality of healthcare-network performance | Benchmark | Information for decision maker | ||
| Time-based | Waiting time for different patient classes (Cimellaro & Piqué, 2016; Yang et al., 2016) | ✓ | ✓ | ✓ | ✓ |
| Door-to-Doctor time (Konrad et al., 2013) | ✓ | ✓ | ✓ | ✓ | |
| Expected length of stay (Chen & Wang, 2016) | ✓ | ✓ | ✓ | ✓ | |
| Based on number of patients | Number of treated patients (Bruneau & Reinhorn, 2007; Jerić & Figueira, 2012) | ✓ | ✓ | ✓ | ✓ |
| Minimum service level (Lameris et al., 2008) | ✓ | ✓ | ✓ | ✓ | |
| Number of expected deaths (Arora et al., 2010; Xiang & Zhuang, 2016) | ✓ | ✓ | ✓ | ✓ | |
| Unmet demand level (Crowe et al., 2014) | ✓ | ✓ | ✓ | ✓ | |
| Loss level (Cimellaro et al., 2010) | ✓ | ✓ | ✓ | ✓ | |
| Cost-based | Deprivation cost (Chen & Wang, 2016; El-Rifai et al., 2016; Lodree et al., 2017) | ✓ | ✓ | ✓ | ✓ |
| Utilisation rate | Nurse utilisation (Griffiths et al., 2005) | Ignores patient's health condition | ✓ | Limited to the medical staff allocation | Only concerns with the use of resources |
| Refusal rate (Harper & Shahani, 2007) | ✓ | ✓ | ✓ | ✓ | |
We found that the time-based measures, measures based on number of patients, and costs are the comprehensive resilience measures since they can be used to evaluate the health conditions of population in. the affected area, to reveal the quality of healthcare-network performance during disasters, and to compare the effectiveness of different strategies for medical response. The information on the patients’ health conditions at the network level reveals the effectiveness of current collective medical response, which is useful for the decisions on the required actions during disasters.
We note that the nurse utilisation rate can be used to evaluate the effectiveness of collective medical response when nurses are shared between hospitals during disasters. However, this measure mainly assesses the efficient use of medical staff and is therefore of interest for staff allocation, but it does not reveal the patients’ health conditions during disasters. In contrast, the refusal rate can reflect the population health when healthcare resources are in shortage. However, in the literature, the refusal rate refers only to the use of beds, although the refusal occurs when other resource such as medical staff, medical equipment, and medical supplies is not available for an arriving patient.
6. Future research directions
In our review, we are particularly interested in the applicability of the developed approaches to real-world disasters, COVID-19 pandemic being the most recent one. We identify possible extensions to the existing models, in the view to better address issues that appear in real-world disasters. Also, we notice that the current advancements of OR in solving other related problems have not been exploited in the coordination in the healthcare systems. We also propose additional resilience measures.
6.1. Extensions of the current models
In our review, we focus on OR studies on IC and CC and their differences in dealing with the challenges of the healthcare system during disasters. However, there are still many research avenues to be explored by the OR community to increase the applicability of the OR methodologies and methods to the coordination in the healthcare systems in real-world disaster management.
6.1.1. Simultaneous allocation of patient and staff
The existing literature is either concerned with the allocation of patients (Sung & Lee, 2016; Zhang & Howard, 2015) or medical staff (Lei et al., 2015; Yi & Özdamar, 2007) during disasters, but does not consider them simultaneously. In fact, in practice, the hospitals are required to allocate medical staff to shelters in affected areas. At the same time, patients at the shelters are allocated to hospitals. It would provide an important opportunity to advance the understanding of real-world healthcare management in disasters by developing CC models for simultaneous allocation of patients and medical staff and analyse how this affects the resilience measures.
6.1.2. Design of new network structures
In real-world, different hospitals have different healthcare capacities to respond to disasters. The capacity depends on the availability of healthcare resources such as medical staff and beds, as well as the capability to provide emergency medical services for severe injuries. The high-capacity hospitals are more likely to admit the severe-injured patients. To the best of our knowledge, none of the reviewed articles has proposed a design of healthcare network for emergency medical response during disasters considering the differences in healthcare capacities amongst hospitals in the network. Therefore, it is unclear what hospitals’ responsibilities for CC are with respect to the emergency medical services they can offer during disasters. It may cause the managerial confusions and ambiguity of authority in the collective medical response. It would be very useful to classify hospitals into groups considering their capacities, which would inform the design of more realistic healthcare networks.
6.1.3. IC across hospital setting
According to our findings, the models for IC included only one hospital, but they should be extended and applied to a larger healthcare network. For instance, models for IC -between different hospital branches operating under the common governance structure could be developed to investigate the impact of IC on the response to the surge of patient demands during disasters. Please note that if the current IC studies that focus on a single hospital setting are extended to cover multiple hospital branches operating under the common governance structure, they would still fall into the category of IC by the definition given in Table 2. In addition, the extended models may cause a considerably heavier computational burden, but would be very beneficial to the real-world disaster management.
6.1.4. Addition of resources from outside the area affected by a disaster
The reviewed articles have not addressed the healthcare resources in the facilities which were not affected by disaster from outside network. In real-world, the external medical staff from outside the affected area are generally allocated to the affected healthcare network in order to enhance the healthcare capability during disasters, especially natural disasters. The future research efforts could go into the improvement of healthcare capability with resources outside the affected network. OR scholars could approach to the coordination in the healthcare system by investigating the external resource allocation in the network problem. The internal healthcare facilities would be perceived as nodes with the required medical services. The external resources would be shared between the facilities and be allocated to the facilities regarding their required medical services. The external resources could be shifted between the facilities in order to improve the state of the affected healthcare network. The travel times from one network to another and between the facilities would play an important role in models for allocation decision support.
6.1.5. Coordination of ambulance sharing
Interestingly, the reviewed articles have not paid attention to the coordination of ambulance sharing. The literature on patient transportation so far has always assumed that only one patient could be dispatched in one ambulance trip, but has not considered sharing of an ambulance between multiple-patients. However, this would increase the efficiency of the dispatching strategy of emergency vehicles during disasters. There has been a recognition of the importance of ambulance sharing in real-word DOM. For instance, WHO.int (2008) reported that one of ambulance types, called patient transport ambulances, was suitable for transportation of one or more patient(s) on stretcher(s) and/or chair(s), particularly in post-disaster logistics when fast transportation of patients to medical facilities was of utmost importance. Boness and Mayes (2018) stated that Australia developed a plan for sharing an ambulance to carry out the transportation requests. An ambulance picks all the patients for the common route before dropping them off. BBC.com (2018) reported that an increase in demand for ambulances required the ambulance sharing. However, the constraints that an ambulance could stop for an additional patient only if it is clinically safe for the patient on board should be carefully modelled. In addition, the health authorities and medical staff in Thailand, whom we interviewed advocate the practice of ambulance sharing in response to a surge of patient volume and a shortage of ambulances during the Tsunami disaster in 2004. Ambulances transported different categories of patients to a hospital in one trip. This provides further motivation for future research direction.
6.1.6. Creating a surge capacity for patient allocation
Creating a surge capacity for patient allocation aims to enhance the effectiveness of collaboration in the healthcare network, and the utilisation of healthcare resources as a whole during disasters (Bayram & Zuabi, 2012). However, we only found one study by Zhang and Howard (2015) which addressed this issue. Zhang and Howard (2015) aimed to increase the healthcare capacity at hospitals under CC by involving the skilled nursing facilities which could provide treatment to less severe-injured patients in response to a surge of patients affected by natural disasters. As a result, hospitals were able to admit more severe-injured patients (an increase of 20%) during natural disasters. We would like to remark that this issue is very important in real-world disaster management. For example, apart from hospitals the use of other healthcare facilities such as primary healthcare centres and temporary medical units was recommended (WHO.int, 2020). The involvement of other facilities for creating surge capacity should be further investigated. Inevitably, their coordination would pose additional challenge in the modelling efforts.
6.1.7. Deployment in real-world
The majority of reviewed articles used randomly generated data based on the relevant data from real-world and described general approaches to emergency medical response designed for all types of disasters. However, two articles utilised the real-world data and illustrated the application of proposed model to the real-world case study. Repoussis et al. (2016), which introduced a response model for ambulance dispatching and patient assignment for all disaster situations and evaluated it in a case study of a terror attack on the New York Stock Exchange. Niessner et al. (2018) proposed a response model for physician assignment to treatment stations in a shelter and applied it to a case of a gas explosion in Austria. In this respect, it would be of value to have more articles like these.
6.2. Methodologies and models
Although many OR methods have been applied to address the coordination of healthcare resources in disaster management, there are still methodologies and models to be investigated. Particularly, we identify modelling of uncertainties, mixed models-methods, data-driven optimisation, and online optimisation to be of great interest.
6.2.1. Modelling of uncertainties
Generally, most emergency response to disasters encounter a high level of uncertainties (Arora et al., 2010). However, little efforts have been made to understand the nature and uncertainties of the problems. The disasters usually cause a high level of uncertainty in the healthcare systems. Deterministic models often fail to address appropriately the nature of the uncertainties in the healthcare systems during disasters. Some reviewed articles used unrealistic assumptions in order to reduce the complexity of the problem. Typically, a known deterministic demand for emergency medical services, and deterministic duration of medical treatment during disasters were used in the models. There are only a few articles which modelled uncertainties and thus increased the applicability of the model/method to real-world disaster management. Niessner et al. (2018)) investigated the dynamic staff reallocation in a stochastic environment. The model considered the queue length and the number of physicians already working at the treatment stations. Chen and Wang (2016) considered uncertain patient arrivals and service time, and included as parameters the minimum and maximum number of medical resources required in an ED to model the uncertain availability of resources. Sung and Lee (2016) used the survival probability to represent the deterioration in a patient's chance of survival as a function of elapsed time. They advocated that the patients’ chance of survival could be changed over time until patients were transported and treated at the hospitals. El-Rifai et al. (2016)) scheduled staff by considering the evolution of the epidemic in order to better cover the demand.
6.2.2. Mixed models/methods
In many complex real-world problems, decisions at the strategic level have an impact on the decisions at the operational level, and vice versa. Modelling approaches traditionally cover only some aspects of decision making at a certain level. The benefits of combining different modelling approaches and consequently different methods have been discussed in the OR community for more than a decade (Morgan, Howick & Belton, 2017). Particularly, the mixing of Discrete Event Simulation (DES), which is often employed in healthcare simulation, and Systems Dynamics (SD) has attracted the most interest in the healthcare simulation community, because these two modelling approaches offer complementary views of the system. SD methodology provides a macro perspective of the system, aiming at capturing dynamic (causal) relationships between entities in a system. On the other hand, DES provides a picture of the system at a micro level, usually sampling arrivals of entities in the system and their required service time from probability distributions. Changes of the state of the system occur at discrete points of time. There have been studies of combining SD and DES in healthcare in different healthcare settings (Ahmad, Ghani, Kamil & Tahar, 2012; Brailsford, Desai & Viana, 2010; Viana, Brailsford, Harindra & Harper, 2014). However, in spite of the growing number of publications, it seems that this approach to modelling has still not reach its momentum. As pointed out by Brailsford, Eldabi, Kunc, Mustafee and Osorio (2019) there is a need for the development of a new rigorous methodology, which should focus on the modelling of links between different models. So far, the research into the healthcare coordination in disaster management has resorted mostly to DES but not to SD. We argue that the combination of these two complementary approaches would considerably strengthen the healthcare coordination in disaster management. DES would provide insights into detailed interactions of individual entities (such as patients, ambulance, staff, etc.), which affect the overall behaviour of the system and determines its performance. SD would interact with DES and would be particularly useful in the investigation of relations between separate components in the healthcare network and how they affect each other. It would enable the identification of potential bottlenecks in the network. Ultimately, it would give a tool to the policy makers to evaluate different policies and choose appropriate one to implement in disaster management. Particularly, we recommend the use of the framework for assisting in the design of mixed methods by Morgan et al. (2017). Based on the insights from practice, the authors introduced a framework consisting of a series of questions to assist in OR modelling in choosing suitable methods and suggesting the design of mixed methods.
6.2.3. Data-driven optimisation
It is very difficult to define uncertain parameters and variables in OR models because their accurate probabilistic descriptions of randomness is often unavailable in practice (Mandelbaum et al., 2020). Recent years have seen an increased interest in application of data-driven optimisation to resource allocation problems in healthcare, especially to real-time epidemic control (Du, Sai & Kong, 2020; Han, Preciado, Nowzari & Pappas, 2015). In these applications, data-driven optimisation aims to use analysis of data collected periodically (progressively) in order to refine the decisions over time. This is opposite to classical approaches to dealing with uncertainty, which assume that all probability distributions are known at the beginning of the planning horizon. There has been no reported research yet into data-driven optimisation in the healthcare coordination. We strongly believe that data-driven optimisation could serve as an excellent tool for handling uncertainties that arise in the healthcare coordination during disasters. For example, the routing of ambulances for patient transportation with uncertain travel times, the calculation of healthcare resources capacity with uncertain time of treatment durations, etc., would be improved by using data-driven optimisation. As more and more data about the type and scale of disaster gradually become available, decision making process could be improved over time leading to better i.e. often called fact-based decisions.
6.2.4. Online optimisation
Online optimization is a rather overlooked method to address real-world uncertainties in healthcare coordination in disaster management. Online algorithms receive their input piece by piece upon making certain actions and have to react with respect to each piece of input. The goal of online algorithms is to guarantee a performance which is as close as possible to the optimal performance achievable if the entire input is known in advance. Different from stochastic optimisation, in online optimisation, no prior probabilistic knowledge is required. In a real world disaster setting, some information might be revealed over time and upon taking particular actions. Online optimisation has been successfully used in some post-disaster DOM problems. Shiri, Akbari and Salman (2020) is one of these studies in which routing and allocation of search-and-rescue teams to areas with trapped victims was addressed. In that study, the number of casualties in a post-disaster emergency assembly location and the status of the roads that were damaged after a disaster could only be revealed by close observation of the search-and-rescue teams on the scene. In another recent study, Akbari and Shiri (2021), addressed the post-disaster relief distribution problem in which some of the road segments were blocked. The blockage of these roads was not known in advance and had an online nature. It could only be revealed when the relief distribution team observed them. Online optimisation would provide a robust tool for handling uncertainties and providing algorithms that can address real aspects of coordination in healthcare systems of disaster management. An example of online parameters in our context is the triage categories for each patient. While in most of the studies, the triage category of each patient is determined by either a stochastic or deterministic approach, it is plausible to identify it after a nurse or doctor observes the conditions of a patient for the first time. Another example of online information is the required time for emergency treatment of a patient. This time can only be assessed after an initial monitoring of the patient by the medical staff on the scene. These online parameters have a direct impact on the obtained input information and hence can have a direct influence on the performance of a solution approach. Instead of making assumptions to enable deterministic or stochastic modelling, which are often unrealistic, the adoption of an online approach would facilitate the development of more accurate models of different real-world conditions in the healthcare coordination.
6.3. Healthcare resilience measures
In this section, we propose the future research directions related to resilience measures including standardisation of measures, additional cost-based measures, and application of existing resilience metrics.
6.3.1. Standardisation of measures
Different resilience measures have been proposed in the OR literature. It has to be further investigated which of these can best reflect the resilience in the healthcare system during disasters. The resilience measures should be standardised to enable the OR researchers to compare and evaluate their models and algorithms.
6.3.2. Additional cost-based measures
In the disaster management the aim is to minimise the response time, rather than to minimise costs (Rolland et al., 2010). Considering only the cost minimisation may be a threat to resilience because the resilient healthcare system requires the redundant capacity of healthcare resources to respond to a surge of demand during disasters (Fairbanks et al., 2014). The redundant capacity can be perceived as unnecessary healthcare resources when the total cost has to be minimised. However, we argue that costs should be also measured in terms of a probability of deaths and social disturbances due to the time delay which is caused by the shortage of healthcare resources. More research into deprivation costs and how to properly quantify them should be carried out. Also, instead of using only cost-based measures a trade-off between cost and other healthcare performances has to be made, such as the number of treated patients. Multi-objective decision making methods could be a useful tool to provide insights into such a trade-off that reflect the effectiveness of the healthcare network.
6.3.3. Application of existing resilience metrics proposed in other disciplines
Resilience measures have been investigated in other disciplines. For example, Henry and Ramirez-Marquez (2012) proposed a generic resilience metric not specific for a particular discipline. Their metric incorporates loss and recovery estimation. To adopt their metric in the field of healthcare management, loss estimation should be included, for example, loss of healthcare performance, deaths, and untreated patients. These measures are based on the fact that the healthcare resources are often short during disasters even if some emergency medical plans have been developed in advance. A shortage of resources can cause ‘losses’ which are unfavourable for the healthcare providers. Recovery estimation includes recovery rate and recovery time. These measures are in agreement with the basic definition of resilience by Bruneau et al. (2003) that is the ability of a system to recover and return to the normal condition. The future research efforts could estimate ‘loss’ and ‘recovery’ based on a measure of, for example, waiting time and number of treated/untreated patients.
7. Conclusions
In this review, we have provided insights into the OR literature on the coordination of emergency medical response and on the measures of resilience during disasters. We categorise the reviewed articles into two different types of coordination of emergency medical response, namely IC and CC. IC mainly investigates the resource allocation within a common governance, whereas CC is mainly focused on the sharing of healthcare resources across governances. Both types of coordination aim to improve the emergency medical response by ensuring the continuity of medical services and improving the healthcare capability during disasters. Resilience is used to evaluate the coordination effectiveness during disasters. Measures based on time and number of patients (treated or untreated) are commonly used.
Based on our findings, we have identified a number of future research directions. First, we suggest some extensions to the existing models which would address better real-world issues including: (1) simultaneous allocation of patients and medical staff in the network; (2) design of new network structures; (3) IC models across hospitals; (4) addition of resources from outside the area affected by a disaster; (5) coordination of ambulance sharing; (6) creating a surge capacity for patient allocation; and (7) considering the deployment of the models/methods in real-world disasters. In addition, we identified OR methodologies that have not been used in this field yet, but could be very beneficial. Of particular interest are: (8) modelling of uncertainties; (9) mixed models/methods (particularly SD and DES); (10) data-driven optimisation; and (11) online optimisation. We also invite researchers to work on (12) the standardisation of resilience measures; (13) further cost-based resilience measures, and (14) the application of existing resilience metrics in other disciplines.
We believe that our review will provide a solid basis for the future OR research in the coordination of emergency medical response. We hope that our findings and recommendations will contribute to the advancement of the healthcare management in disasters. We trust that this review will motivate the OR community to make further effective contributions in actual disaster responses.
ncited references
J. E. Anderson et al., 2016, Banomyong, Varadejsatitwong & Oloruntoba, 2019, Cimellaro, Fumo, Reinhorn & Bruneau, 2008, Ferrand, Magazine, Rao & Glass, 2018, Konrad, Tang, Shiner & Watts, 2017, Luscombe & Kozan, 2016, Maliapen & Dangerfield, 2010, Nilsson, Vikström & Jonson, 2012, Ozkaynak & Brennan, 2012, Perry & Lindell, 2003, Rüter, Nilsson & Vilkström, 2006, Veenema, Rains, Casey-Lockyer, Springer & Kowal, 2015, Zhong, Clark, Hou, Zang & Fitzgerald, 2014a, Zhong, Clark, Hou, Zang & Fitzgerald, 2014b.
References
- Achour N., Miyajima M., Pascale F., Price A.D.F. Vol. 23. Disaster Prevention and Management; 2014. pp. 40–52. (Hospital resilience to natural hazards: Classification and performance of utilities). [Google Scholar]
- Achour N., Price A.D.F. Resilience strategies of healthcare facilities: Present and future. International Journal of Disaster Resilience in the Built Environment. 2010;1(3):264–276. [Google Scholar]
- Ahmad N., Ghani N.A., Kamil A.A., Tahar R.M. Emergency department problems: A call for hybrid simulation. In: Ao S.I., Gelman L., Hukins D.W.L., Hunter A., Korsunsky A.M., editors. Proceedings of the world congress on engineering; London, UK: Imperial College London; 2012. pp. 1470–1474. 4–6 July 2012. [Google Scholar]
- Ahmadi-Javid A., Seyedi P., Syam S.S. A survey of healthcare facility location. Computers and Operations Research. 2017;79:223–263. [Google Scholar]
- Akbari V., Shiri D. Weighted online minimum latency problem with edge uncertainty. European Journal of Operational Research. 2021;295(1):51–65. [Google Scholar]
- Altay N., Green W.G. OR/MS research in disaster operations management. European Journal of Operational Research. 2006;175(1):475–493. [Google Scholar]
- Anaya-Arenas A.M., Renaud J., Ruiz A. Relief distribution networks: A systematic review. Annals of Operations Research. 2014;223(1):53–79. [Google Scholar]
- Anderson J.E., Ross A.J., Back J., Duncan M., Snell P., Walsh K. Implementing resilience engineering for healthcare quality improvement using the CARE model: A feasibility study protocol. Pilot and Feasibility Studies. 2016;2(1):1–9. doi: 10.1186/s40814-016-0103-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson J.E., Ross A., Back J., Duncan M., Hopper A., Snell P. Springer International Publishing; 2016. Resilience engineering as a quality improvement method: Insights from a research programme. [Google Scholar]
- Arora H., Raghu T.S., Vinze A. Resource allocation for demand surge mitigation during disaster response. Decision Support Systems. 2010;50(1):304–315. [Google Scholar]
- Banomyong R., Varadejsatitwong P., Oloruntoba R. A systematic review of humanitarian operations, humanitarian logistics and humanitarian supply chain performance literature 2005 to 2016. Annals of Operations Research. 2019;283(1):71–86. [Google Scholar]
- Bayram J.D., Zuabi S. Disaster metrics: Quantification of acute medical disasters in trauma-related multiple casualty events through modeling of the acute medical severity index. Prehospital and Disaster Medicine. 2012;27(2):130–135. doi: 10.1017/S1049023X12000428. [DOI] [PubMed] [Google Scholar]
- BBC.com (2018). Ambulances to stop for additional emergency patients. Retrieved from https://www.bbc.co.uk/news/uk-england-norfolk-45550841. Accessed February 2, 2021
- Becker T., Steenweg P.M., Werners B. Cyclic shift scheduling with on-call duties for emergency medical services. Health Care Management Science. 2018;22(4):676–690. doi: 10.1007/s10729-018-9451-9. [DOI] [PubMed] [Google Scholar]
- Bender M., Connelly C.D., Brown C. Interdisciplinary collaboration: The role of the clinical nurse leader. Journal of Nursing Management. 2013;21(1):165–174. doi: 10.1111/j.1365-2834.2012.01385.x. [DOI] [PubMed] [Google Scholar]
- Berg S.H., Akerjordet K., Ekstedt M., Aase K. Methodological strategies in resilient health care studies: An integrative review. Safety Science. 2018;110:300–312. [Google Scholar]
- Boness T., Mayes H. Vol. 2018. Impact; 2018. pp. 42–45. (Improving patient transport in new south wales). [Google Scholar]
- Boon H.S., Mior S.A., Barnsley J., Ashbury F.D., Haig R. The Difference Between Integration and Collaboration in Patient Care: Results From Key Informant Interviews Working in Multiprofessional Health Care Teams. Journal of Manipulative and Physiological Therapeutics. 2009;32(9):715–722. doi: 10.1016/j.jmpt.2009.10.005. [DOI] [PubMed] [Google Scholar]
- Boyd A., Chambers N., French S., King R., Shaw D., Whitehead A.S. Final report. NIHR Health Services and Delivery Research programme; 2012. A scoping study of emergency planning and management in health care: What further research is needed. [Google Scholar]
- Brailsford S.C., Desai S.M., Viana J. Towards the holy grail: Combining system dynamics and discrete-event simulation in healthcare. In: Johansson B., Jain S., Montoya-Torres J., Hugan J., Yucesan E., editors. Proceedings of the 42nd winter simulation conference; Baltimore, MD; 2010. [Google Scholar]
- Brailsford S.C., Eldabi T., Kunc M., Mustafee N., Osorio A.F. Hybrid simulation modelling in operational research: A state-of-the-art review. European Journal of Operational Research. 2019;278:721–737. [Google Scholar]
- Bruneau M., Chang S.E., Eguchi R.T., Lee G.C., O'Rourke T.D. A Framework to Quantitatively Assess and Enhance the Seismic Resilience of Communities. Earthquake Spectra. 2003;19(4):733–752. [Google Scholar]
- Bruneau M., Reinhorn A. Exploring the concept of seismic resilience for acute care facilities. Earthquake Spectra. 2007;23(1):41–62. [Google Scholar]
- Carenzo L., Costantini E., Greco M., Barra F.L., Rendiniello V., Mainetti M. Hospital surge capacity in a tertiary emergency referral centre during the COVID-19 outbreak in Italy. Anaesthesia. 2020;75(7):928–934. doi: 10.1111/anae.15072. [DOI] [PubMed] [Google Scholar]
- Caunhye A.M., Nie X., Pokharel S. Optimization models in emergency logistics: A literature review. Socio-Economic Planning Sciences. 2012;46(1):4–13. [Google Scholar]
- Chen T.L., Wang C.C. Multi-objective simulation optimization for medical capacity allocation in emergency department. Journal of Simulation. 2016;10(1):50–68. [Google Scholar]
- Chong W.W., Aslani P., Chen T.F. Shared decision-making and interprofessional collaboration in mental healthcare: A qualitative study exploring perceptions of barriers and facilitators. Journal of Interprofessional Care. 2013;27(5):373–379. doi: 10.3109/13561820.2013.785503. [DOI] [PubMed] [Google Scholar]
- Cimellaro G.P., Fumo C., Reinhorn A., Bruneau M. Seismic resilience of health care facilities. 14th World Conference on Earthquake Engineering (14WCEE); Beijing, China; 2008. Oct (12-17) [Google Scholar]
- Cimellaro G.P., Piqué M. Resilience of a hospital emergency department under seismic event. Advances in Structural Engineering. 2016;19(5):825–836. [Google Scholar]
- Cimellaro G.P., Reinhorn A.M., Bruneau M. Seismic resilience of a hospital system. Structure and Infrastructure Engineering. 2010;6(1–2):127–144. [Google Scholar]
- CNN.com . That's a problem for the government; 2020. China's red cross is under fire for not getting supplies to hospitals fighting coronavirus.https://edition.cnn.com/2020/02/06/asia/red-cross-china-donations-intl-hnk/index.html Retrieved from. Accessed February 2, 2021. [Google Scholar]
- covidanalytics.io (2020). Optimization can solve the ventilator shortage. Retrieved from https://www.covidanalytics.io/ventilator_allocation. Accessed February 2, 2021
- Crowe S., Vasilakis C., Skeen A., Storr P., Grove P., Gallivan S. Examining the feasibility of using a modelling tool to assess resilience across a health-care system and assist with decisions concerning service reconfiguration. Journal of the Operational Research Society. 2014;65(10):1522–1532. [Google Scholar]
- Dansky K.H., Miles J. Patient satisfaction with ambulatory healthcare services: Waiting time and filling time. Hospital and Health Services Administration. 1997;42(2):165–177. [PubMed] [Google Scholar]
- Du M., Sai A., Kong N. A data-driven optimization approach for multi-period resource allocation in cholera outbreak control. European Journal of Operational Research. 2020;291(3):1106–1116. [Google Scholar]
- El-Rifai O., Garaix T., Xie X. Proactive on-call scheduling during a seasonal epidemic. Operations Research for Health Care. 2016;8:53–61. [Google Scholar]
- Espíndola O.R., Albores P., Brewster C. Disaster preparedness in humanitarian logistics: A collaborative approach for resource management in floods. European Journal of Operational Research. 2018;264(3):978–993. [Google Scholar]
- Esposito Amideo A., Scaparra M.P., Kotiadis K. Optimising shelter location and evacuation routing operations: The critical issues. European Journal of Operational Research. 2019;279(2):279–295. [Google Scholar]
- Fairbanks R.J., Wears R.L., Plsek P., Woods D.D., Hollnagel E., Cook R.I. Resilience and Resilience Engineering in Health Care. The Joint Commission Journal on Quality and Patient Safety. 2014;40(8):376–383. doi: 10.1016/s1553-7250(14)40049-7. [DOI] [PubMed] [Google Scholar]
- Farahani R.Z., Lotfi M.M., Baghaian A., Ruiz R., Rezapour S. Mass casualty management in disaster scene: A systematic review of OR&MS research in humanitarian operations. European Journal of Operational Research. 2020;287(3):787–819. [Google Scholar]
- Ferrand Y.B., Magazine M.J., Rao U.S., Glass T.F. Managing responsiveness in the emergency department: Comparing dynamic priority queue with fast track. Journal of Operations Management. 2018;58–59:15–26. [Google Scholar]
- Fitzpatrick R., Davey C., Buxton M.J., Jones D.R. Evaluating patient-based outcome measures for use in clinical trials. Health Technology Assessment. 1998;2(14):1–74. i-ivPMID: 9812244. [PubMed] [Google Scholar]
- Fries J.F., Spitz P., Kraines R.G., Holman H.R. Section of T H E Arthritis Foijndation Measurement of Patient Outcome in Arthritis. Arthritis & Rheumatism. 1980;23(2):137–145. doi: 10.1002/art.1780230202. [DOI] [PubMed] [Google Scholar]
- Galindo G., Batta R. Review of recent developments in OR/MS research in disaster operations management. European Journal of Operational Research. 2013;230(2):201–211. [Google Scholar]
- Gould D., Gammon J., Donnelly M., Batiste L., Ball E., Carneiro De Melo A.M.S. Improving hand hygiene in community healthcare settings: The impact of research and clinical collaboration. Journal of Clinical Nursing. 2000;9(1):95–102. doi: 10.1046/j.1365-2702.2000.00334.x. [DOI] [PubMed] [Google Scholar]
- GOV.uk (2019). NHS Emergency Planning Guidance. Retreived from https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/215643/dh_125842.pdf. Accessed February 2, 2021
- Griffiths J.D., Price-Lloyd N., Smithies M., Williams J.E. Modelling the requirement for supplementary nurses in an intensive care unit. Journal of the Operational Research Society. 2005;56(2):126–133. [Google Scholar]
- Gul M., Guneri A.F. A comprehensive review of emergency department simulation applications for normal and disaster conditions. Computers and Industrial Engineering. 2015;83:327–344. [Google Scholar]
- Güneş E.D., Yaman H. Health network mergers and hospital re-planning. Journal of the Operational Research Society. 2010;61(2):275–283. [Google Scholar]
- Gutjahr W.J., Nolz P.C. Multicriteria optimization in humanitarian aid. European Journal of Operational Research. 2016;252(2):351–366. [Google Scholar]
- Han S., Preciado V., Nowzari C., Pappas G. IEEE Transactions on Network Sci- ence and Engineering. Vol. 2. 2015. Data-driven network resource allocation for controlling spreading processes; pp. 127–138. [Google Scholar]
- Harper P.R., Shahani A.K. Modelling for the planning and management of bed capacities in hospitals. Journal of the Operational Research Society. 2007;53(1):11–18. [Google Scholar]
- Henry D., Ramirez-Marquez J.E. Generic metrics and quantitative approaches for system resilience as a function of time. Reliability Engineering and System Safety. 2012;99:114–122. [Google Scholar]
- Holling C.S. In: Engineering within ecological constraints. Ed. Schulze P., editor. National Academy of Engineering; 1996. Engineering resilience versus ecological resilience; pp. 31–44. [Google Scholar]
- Jerić S.V., Figueira J.R. Multi-objective scheduling and a resource allocation problem in hospitals. Journal of Scheduling. 2012;15(5):513–535. [Google Scholar]
- Johnson K.F., Mahan L.A. A Qualitative Investigation into Behavioral Health Providers Attitudes Toward Interprofessional Clinical Collaboration. The Journal of Behavioral Health Services & Research. 2019;46:636–647. doi: 10.1007/s11414-019-09661-9. [DOI] [PubMed] [Google Scholar]
- Karam M., Brault I., Van Durme T., Macq J. Comparing interprofessional and interorganizational collaboration in healthcare: A systematic review of the qualitative research. International Journal of Nursing Studies. 2018;79:70–83. doi: 10.1016/j.ijnurstu.2017.11.002. [DOI] [PubMed] [Google Scholar]
- Katsaliaki K., Mustafee N. Applications of simulation within the healthcare context. Journal of the Operational Research Society. 2011;62(8):1431–1451. doi: 10.1057/jors.2010.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Konrad R., DeSotto K., Grocela A., McAuley P., Wang J., Lyons J. Modeling the impact of changing patient flow processes in an emergency department: Insights from a computer simulation study. Operations Research for Health Care. 2013;2(4):66–74. [Google Scholar]
- Konrad R., Tang C., Shiner B., Watts B.V. Workforce design in primary care-mental health integration: A case study at one Veterans affairs medical centre. Health Systems. 2017;6(2):112–121. [Google Scholar]
- Kruk M.E., Ling E.J., Bitton A., Cammett M., Cavanaugh K. Building resilient health systems: A proposal for a resilience index. British medical journal. 2017;357:2323. doi: 10.1136/bmj.j2323. J. [DOI] [PubMed] [Google Scholar]
- Kruk M.E., Myers M., Varpilah S.T., Dahn B.T. What is a resilient health system? Lessons from Ebola. The Lancet. 2015;385(9980):1910–1912. doi: 10.1016/S0140-6736(15)60755-3. [DOI] [PubMed] [Google Scholar]
- Lameris H., Bakker P.J.M., Elkhuizen S.G., Vermeulen I.B., Poutré H.La, Bohte S.M. Adaptive resource allocation for efficient patient scheduling. Artificial Intelligence in Medicine. 2008;46(1):67–80. doi: 10.1016/j.artmed.2008.07.019. [DOI] [PubMed] [Google Scholar]
- Lei L., Wang S., Pinedo M., Yang J., Qi L. Personnel scheduling and supplies provisioning in emergency relief operations. Annals of Operations Research. 2015;235(1):487–515. [Google Scholar]
- Li X., Beullens P., Jones D., Tamiz M. An integrated queuing and multi-objective bed allocation model with application to a hospital in China. Journal of the Operational Research Society. 2009;60(3):330–338. [Google Scholar]
- Liu F., Zhao L. Resilience of multi-hospitals network based on the collaborative scheduling. International Journal of Systems Science: Operations and Logistics. 2015;2(3):135–143. [Google Scholar]
- Lockhart-Wood K. Collaboration between nurses and doctors in clinical practice. British Journal of Nursing. 2000;9(5):276–280. doi: 10.12968/bjon.2000.9.5.6363. [DOI] [PubMed] [Google Scholar]
- Lodree E.J., Altay N., Cook R.A. Staff assignment policies for a mass casualty event queuing network. Annals of Operations Research. 2017;283:411–442. [Google Scholar]
- Luscombe R., Kozan E. Dynamic resource allocation to improve emergency department efficiency in real time. European Journal of Operational Research. 2016;255(2):593–603. [Google Scholar]
- Maliapen M., Dangerfield B.C. A system dynamics-based simulation study for managing clinical governance and pathways in a hospital. Journal of the Operational Research Society. 2010;61(2):255–264. [Google Scholar]
- Mandelbaum A., Momčilović P., Trichakis N., Kadish S., Leib R., Bunnell C.A. Data-driven appointment-scheduling under uncertainty: The case of an infusion unit in a cancer center. Management Science. 2020;66(1):243–270. [Google Scholar]
- McDaniels T., Chang S., Cole D., Mikawoz J., Longstaff H. Fostering resilience to extreme events within infrastructure systems: Characterizing decision contexts for mitigation and adaptation. Global Environmental Change. 2008;18(2):310–318. [Google Scholar]
- Mishra D., Kumar S., Hassini E. Current trends in disaster management simulation modelling research. Annals of Operations Research. 2019;283(1–2):1387–1411. [Google Scholar]
- Morgan J.S., Howick S., Belton V. A toolkit of designs for mixing Discrete Event Simulation and System Dynamics. European Journal of Operational Research. 2017;257:907–918. [Google Scholar]
- Morton M.J., DeAugustinis M.L., Velasquez C.A., Singh S., Kelen G.D. Developments in surge research priorities: A systematic review of the literature following the academic emergency medicine consensus conference, 2007–2015. Academic Emergency Medicine. 2015;22(11):1235–1252. doi: 10.1111/acem.12815. [DOI] [PubMed] [Google Scholar]
- Niessner H., Rauner M.S., Gutjahr W.J. A dynamic simulation–optimization approach for managing mass casualty incidents. Operations Research for Health Care. 2018;17:82–100. [Google Scholar]
- Nilsson H., Vikström T., Jonson C.O. Performance indicators for initial regional medical response to major incidents: A possible quality control tool. Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine. 2012;20:1–8. doi: 10.1186/1757-7241-20-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogawa K., Kaneko M., Kajihara C., Sano M., Munechika M. Systematization of countermeasures to improve business continuity of regional healthcare in a disaster. Total Quality Science. 2016;2(2):60–69. [Google Scholar]
- Özdamar L., Ertem M.A. Models, solutions and enabling technologies in humanitarian logistics. European Journal of Operational Research. 2015;244(1):55–65. [Google Scholar]
- Ozkaynak M., Brennan P.F. Characterizing patient care in hospital emergency departments. Health Systems. 2012;1(2):104–117. [Google Scholar]
- Pazirandeh A., Maghsoudi A. Improved coordination during disaster relief operations through sharing of resources. Journal of the Operational Research Society. 2018;69(8):1227–1241. [Google Scholar]
- Perry R.W., Lindell M.K. Preparedness for Emergency Response: Guidelines for the Emergency Planning Process. Disasters. 2003;27(4):336–350. doi: 10.1111/j.0361-3666.2003.00237.x. [DOI] [PubMed] [Google Scholar]
- Rådestad M., Jirwe M., Castrén M., Svensson L., Gryth D., Rüter A. Essential key indicators for disaster medical response suggested to be included in a national uniform protocol for documentation of major incidents: A Delphi study. Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine. 2013;21(1):1–11. doi: 10.1186/1757-7241-21-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Repoussis P.P., Paraskevopoulos D.C., Vazacopoulos A., Hupert N. Optimizing emergency preparedness and resource utilization in mass-casualty incidents. European Journal of Operational Research. 2016;255(2):531–544. [Google Scholar]
- Rolland E., Patterson R.A., Ward K., Dodin B. Decision support for disaster management. Operations Management Research. 2010;3(1):68–79. [Google Scholar]
- Rüter A., Nilsson H., Vilkström T. Performance indicators as quality control for testing and evaluating hospital management groups: A pilot study. Prehospital and Disaster Medicine. 2006;21(6):423–426. doi: 10.1017/s1049023x00004131. [DOI] [PubMed] [Google Scholar]
- Sabbaghtorkan M., Batta R., He Q. Prepositioning of assets and supplies in disaster operations management: Review and research gap identification. European Journal of Operational Research. 2020;284(1):1–19. [Google Scholar]
- Shiri D., Akbari V., Salman F.S. Online routing and scheduling of search-and-rescue teams. OR Spectrum. 2020;42(3):755–784. [Google Scholar]
- Simpson N.C., Hancock P.G. Fifty years of operational research and emergency response. Journal of the Operational Research Society. 2009;60(sup 1):126–139. [Google Scholar]
- Starr M.K., Matinrad N. Vol. 25. Production and Operations Management Society; 2016. pp. 1611–1637. (Disaster management from a pom perspective : Mapping a new domain). [Google Scholar]
- Sun L., Depuy G.W., Evans G.W. Multi-objective optimization models for patient allocation during a pandemic influenza outbreak. Computers and Operations Research. 2014;51:350–359. [Google Scholar]
- Sung I., Lee T. Optimal allocation of emergency medical resources in a mass casualty incident: Patient prioritization by column generation. European Journal of Operational Research. 2016;252(2):623–634. [Google Scholar]
- Vanvactor J.D. Cognizant healthcare logistics management: Ensuring resilience during crisis. International Journal of Disaster Resilience in the Built Environment. 2011;2(3):245–255. [Google Scholar]
- Veenema T.G., Rains A.B., Casey-Lockyer M., Springer J., Kowal M. Quality of healthcare services provided in disaster shelters: An integrative literature review. International Emergency Nursing. 2015;23(3):225–231. doi: 10.1016/j.ienj.2015.01.004. [DOI] [PubMed] [Google Scholar]
- Viana J., Brailsford S.C., Harindra V., Harper P.R. Combining discrete-event simulation and system dynamics in a healthcare setting: A composite model for Chlamydia infection. European Journal of Operational Research. 2014;237(1):196–206. [Google Scholar]
- Wallemacq P. Centre for Research on the Epidemiology of Disasters, CRED; 2018. Economic losses, poverty & disasters: 1998-2017. [DOI] [Google Scholar]
- WHO.int . WHO Regional Office for Europe; 2008. Emergency medical services systems in the European Union: Report of an assessment project co-ordinated by the world health organization.https://apps.who.int/iris/bitstream/handle/10665/107916/E92038.pdf?sequence=1&isAllowed=y Retrieved from. Accessed February 2, 2021. [Google Scholar]
- WHO.int (2020). Health-care facilities. Retrieved from https://www.who.int/environmental_health_emergencies/services/en/ Accessed February 2, 2021
- Xiang Y., Zhuang J. A medical resource allocation model for serving emergency victims with deteriorating health conditions. Annals of Operations Research. 2016;236(1):177–196. [Google Scholar]
- Yang K.K., Lam S.S.W., Low J.M.W., Ong M.E.H. Managing emergency department crowding through improved triaging and resource allocation. Operations Research for Health Care. 2016;10:13–22. [Google Scholar]
- Yi P., George S.K., Paul J.A., Lin L. Hospital capacity planning for disaster emergency management. Socio-Economic Planning Sciences. 2010;44(3):151–160. [Google Scholar]
- Yi W., Özdamar L. A dynamic logistics coordination model for evacuation and support in disaster response activities. European Journal of Operational Research. 2007;179(3):1177–1193. [Google Scholar]
- Zhang K., Howard D.H. Hospital and skilled nursing facility patient flows during Hurricane Katrina and the Midwest floods of 2008. Health Systems. 2015;4(1):29–40. [Google Scholar]
- Zhong S., Clark M., Hou X.Y., Zang Y., Fitzgerald G. Development of hospital disaster resilience: Conceptual framework and potential measurement. Emergency Medicine Journal. 2014;31(11):930–938. doi: 10.1136/emermed-2012-202282. [DOI] [PubMed] [Google Scholar]
- Zhong S., Clark M., Hou X.Y., Zang Y., Fitzgerald G. Validation of a framework for measuring hospital disaster resilience using factor analysis. International Journal of Environmental Research and Public Health. 2014;11(6):6335–6353. doi: 10.3390/ijerph110606335. [DOI] [PMC free article] [PubMed] [Google Scholar]