Abstract
Individuals with a comorbid diagnosis of Down syndrome (DS) and autism spectrum disorder (ASD) have been found to exhibit greater deficits in expressive communication than individuals with DS only. We hypothesized that individuals with a comorbid diagnosis (n = 430) would have significantly lower Communication Matrix scores and specifically social communication scores than individuals with DS alone (n = 4,352). In a sample of 4,782 individuals with DS, scores for individuals with a comorbid diagnosis were on average 18.01 points and 7.26 points lower for total score and social score respectively as compared to individuals with DS. Comorbid diagnosis accounted for 10.5% of the variance in communication scores. Between-group differences in referential gestures and symbolic communication behaviors were also observed.
Keywords: Down syndrome, autism spectrum disorder, intellectual disability, language, communication
Down syndrome (DS), with a prevalence of almost one in 700 births in the United States, is the most commonly occurring chromosomal cause of intellectual disability (ID; Parker et al., 2010). Individuals with DS experience characteristic spoken language deficits and their expressive language skills vary greatly ranging from minimal verbal skills, to single word utterances, and syntactically complex utterances (Abbeduto et al., 2016; Finestack & Abbeduto, 2010; Finestack et al., 2012). Although research has begun to identify a DS behavioral phenotype (Chapman & Hesketh, 2000), less is known about individuals with DS who communicate using prelinguistic and early symbolic communication behaviors.
Another gap in the literature is research describing expressive communication skills in individuals with comorbid DS and autism spectrum disorders (DS/ASD). The prevalence of ASD is higher in children with DS compared to the general population, with estimates ranging from 1%–19% (DisGuiseppi et al., 2010; Moss et al., 2013). Individuals with DS/ASD have greater deficits in cognition and communication and exhibit more stereotypic behavior, anxiety, conduct problems, hyperactivity, and social withdrawal than individuals with DS alone (Capone et al., 2005; Carter et al., 2007; Molloy et al., 2009; Warner et al., 2014). Importantly, they need customized treatment and educational approaches distinct from intervention strategies for individuals with DS alone (Moss & Howling, 2009; Reilly, 2009). A greater understanding of early communication behaviors can lead to interventions that are tailored for individuals with DS/ASD.
Focusing on the development of early expressive communication skills is important because the frequency of prelinguistic and early symbolic behaviors significantly predicts language growth in children with and without DS (Brady et al., 2004; Calandrella & Wilcox, 2000; Yoder & Warren, 2004; Zampini & D’Odorico, 2009, 2013). Expanding research on individuals with DS and DS/ASD is a critical first step toward developing interventions that optimize spoken language outcomes. In the current study, we used an expressive communication measure, the Communication Matrix (Rowland, 2011, 2020), to provide novel insights on prelinguistic and early symbolic behaviors in individuals with DS as compared to individuals with DS/ASD.
Prelinguistic and Early Symbolic Communication Skills in Individuals With DS
Prelinguistic communication behaviors emerge prior to the development of spoken language and include gestures, facial expressions, eye-gaze, physical body movements, and vocalizations (Spencer, 2011). Early symbolic behaviors include spoken words, manual signs, and picture symbols which represent specific referents (Adamson et al., 2004, 2012). Children with DS show differences in gestures, and vocalizations when compared to typically developing children and children with other neurodevelopmental disabilities (Abbeduto et al., 2016; Romano et al., 2019). They have relative strengths in gesture use and maintain high rates whereas typically developing children’s gestures decrease as they begin to use and combine words (Kat-van den Os et al., 2017; Vandereet et al., 2011). During infancy and toddlerhood, children with DS show lower rates of vocalizations than their typically developing peers (Romano et al., 2019; Thiemann-Bourque et al., 2014). For children with DS, vocabulary growth is slow with wide variability, and they have difficulty transitioning to multiple-word combinations and early sentences (Abbeduto et al., 2016). Berglund et al. (2001) found that by 60 months, 78% of children with DS acquired 50 words, but 10%–20% had fewer than 10 words and some had no words in their spoken vocabularies. Although most individuals with DS learn to communicate with spoken language, little is known about the subgroup of individuals who do not develop sufficient natural speech to meet their daily communication needs.
Most research on prelinguistic and early symbolic communication was conducted with relatively small samples of young children with DS (ages 1–7 years) and there are important gaps in describing expressive communication skills across broader age ranges. Individuals with DS may continue to communicate using these behaviors for multiple years or for their lifetime if they experience severe motor speech disorders (Roberts et al., 2007). Severe motor speech disorders are common in individuals with DS. For example, in a recent study of children and adolescents with DS (Wilson et al., 2019), 97.8% met criteria for motor speech disorders. Additional descriptive data is needed to understand individuals with DS who continue to use prelinguistic and early symbolic behaviors.
Expressive Communication Skills in Individuals With DS and ASD
Some studies have closely examined social communication and expressive language skills in individuals with DS/ASD compared to individuals with DS alone. Capone et al. (2005) found that individuals with DS/ASD have greater communication impairments than individuals with DS, as measured by the Diagnostic and Statistical Manual of Mental Disorders, Fourth edition (DSM-IV; Bell, 1994). They hypothesized that the deficit was related to the greater cognitive impairments they observed in individuals with DS/ASD. However, Molloy et al. (2009) found that greater deficits in communication observed in children with DS/ASD, as measured by the Mullen Scales of Early Learning (Mullen, 1995), were not completely explained by the difference in cognitive ability. Using the Autism Diagnostic Interview–Revised (Rutter, Le Couteur, & Lord, 2003) and the Mullen (1995), Godfrey et al. (2019) explored social and expressive communication to find that individuals with DS/ASD had significantly more social-communicative impairments than individuals with DS. The severity of these impairments was related to verbal cognition in individuals with DS/ASD, but not individuals with DS. Warner et al. (2014) used parent-reported results from a general questionnaire and the Social Communication Questionnaire (Rutter, Bailey, & Lord, 2003) to measure communication. They found that individuals with DS/ASD were significantly less likely to communicate using phrases and sentences than individuals with DS. Of those who developed verbal skills, individuals with DS/ASD acquired developmental skills later and were more likely to have lost skills than individuals with DS. In Moss et al. (2013), researchers identified differences in language use among individuals with DS and DS/ASD. They found that 29% of individuals with DS/ASD used fewer than 30 words as compared to 12% of individuals with DS. These studies show a pattern of increased difficulty with expressive communication, and specifically social communication, in individuals with DS/ASD as compared to individuals with DS.
Although there is emerging research on social communication and language skills in individuals with DS/ASD, there are gaps describing prelinguistic and early symbolic communication skills. None of the studies found have used sample sizes larger than 200 individuals with each diagnosis. Replicating the results of these studies with a larger sample size would benefit the body of literature. Previous studies used tools that evaluated multiple developmental domains or were instruments developed for screening and diagnosing ASD. These tools have few test items on expressive communication, especially at the earliest developmental stages. Many developmental assessments have limitations for describing expressive communication skills because they have floor effects for individuals with IDD and often require spoken responses that exclude individuals who do not use natural speech (Brady et al., 2012; Esbensen et al., 2017; Mervis & Robinson, 2005). Measures developed for the purpose of diagnosing ASD were not designed to describe prelinguistic and early symbolic communication behaviors in individuals with other intellectual and developmental disabilities and may have limited sensitivity and specificity when applied to individuals with DS (Moss et al., 2013). Additional research is needed to expand knowledge of the DS/ASD phenotype by focusing specifically on prelinguistic communication in individuals with DS/ASD as compared to individuals with DS.
Purpose and Research Questions
In this study, we used the Communication Matrix (Rowland, 2020), an assessment of early prelinguistic and symbolic behaviors, to explore expressive communication skills of children and adolescents with DS and those with DS/ASD. We selected this measure because it provides comprehensive information regarding the communication level and communication behaviors used to express a variety of early messages and the associated data repository provides access to a large sample size. The outcome measure describes early communication skills including pre-intentional, presymbolic, and early symbolic behaviors, both typical (e.g., spoken words) and atypical (e.g., picture symbols), and is robust to floor effects. The following research questions are explored:
Are expressive communication scores of individuals with a diagnosis of DS/ASD significantly lower than scores of individuals with DS?
Are social communication scores of individuals with a diagnosis of DS/ASD significantly lower than scores of individuals with DS?
What specific referential and conventional gestures and early symbolic behaviors do individuals with DS and DS/ASD use to communicate?
To answer these questions, we explored data collected through the online version of the Communication Matrix assessment (www.communicationmatrix.org). We hypothesized that individuals with DS would have significantly higher total and social communication scores and would use a greater number of and more complex communication behaviors than individuals with DS/ASD.
Method
Study Design
A retrospective cross-sectional design was conducted to analyze a subset of data from the Communication Matrix data repository (IRB0001517), which as of April 2019, contained over 185,370 assessments of expressive communication in individuals with IDD. A data-mining approach was used to extract samples from the repository including participants with a diagnosis of DS and DS/ASD. The repository was queried on October 1, 2019.
First, the repository was queried using the following inclusion criteria: (a) age between 0–21 years, (b) diagnosis of DS confirmed by one or more professionals, (c) assessment administered by an educational professional (e.g., speech-language pathologist, teacher, or therapist), and (d) the assessment was completed in the United States. This age range was chosen to limit the sample to ages that cover language development in typically developing children and through the school years, when educational programs would be expected to influence communication development. Data from individuals whose diagnosis was scored as suspected by a family member or a professional were not included. The assessments that were administered by educational professionals were selected to increase the homogeneity of the results and to prevent the inclusion of repeated measures on some individuals who were assessed by both parents and professionals. Based on this criterion, 231 assessments administered by family members were not included. Only assessments from the United States were included to increase the homogeneity of the sample. If the database included more than one assessment meeting the previous criteria for the same individual, only the most recent assessment results were used to avoid repeated measures on any participants. Using this criterion, 5,060 participants with DS were extracted from the database.
Next, the dataset was cleaned to eliminate assessments that were test or example assessments, incomplete, or repeated measures of the same individual conducted by different assessors. Specifically, individuals were removed when their (a) personal identifier included the following words test, example, class, training, or sample (n = 43); (b) assessment scores were 0 (n = 4); or (c) demographic information matched exactly on the following characteristics birth month, birth year, state, country, race, gender, language, and personal ID (e.g., initials, pseudonym; n = 231).
Last, individuals with DS/ASD were identified from the sample of individuals with DS. A diagnosis of ASD was operationalized by the assessor either answering yes to the question, “Does the primary diagnosis of the person you are assessing involve Autism?” OR choosing “Autism Spectrum Disorder” from a list of diagnoses, OR both. The source of the diagnosis had to be from at least one professional. Using the previous criteria, 430 participants with DS/ASD were extracted from the database.
Participants
The resulting sample of participants formed two groups: (a) individuals with DS (n = 4,352), and (b) individuals with DS/ASD (n = 430). Participants with comorbid DS/ASD constituted 9.0% of the initial sample, consistent with reported estimates of prevalence (Moss et al., 2013; Reilly, 2009). Table 1 describes demographic characteristics of the two samples of participants.
Table 1.
Participant Demographics
| Diagnosis | ||||
|---|---|---|---|---|
| Measure | DS | DS/ASD | Total | p |
| N | 4352 | 430 | 4782 | |
| Mean Age (years) | 8.58 (4.78) | 10.60 (4.77) | 8.76 (4.82) | .764 |
| Sex | .002* | |||
| Female | 1561 (36%) | 122 (28%) | 1683 (35%) | |
| Male | 2791 (64%) | 308 (72%) | 3099 (65%) | |
| Race | .150 | |||
| American Indian or Alaska Native | 57 (1%) | 3 (0.7%) | 60 (1%) | |
| Asian | 175 (4%) | 14 (3%) | 189 (4%) | |
| Black or African American | 415 (10%) | 33 (8%) | 448 (9%) | |
| Native Hawaiian or other Pacific Islander | 21 (0.5%) | 2 (0.5%) | 23 (0.5%) | |
| White | 2361 (54%) | 262 (61%) | 2623 (55%) | |
| More than One Race | 294 (7%) | 34 (8%) | 328 (7%) | |
| Unknown | 1029 (24%) | 82 (19%) | 1111 (23%) | |
| Profession of the Assessor | .742 | |||
| Speech-Language Pathologist | 3454 (80%) | 336 (78%) | 3790 (80%) | |
| Teacher | 727 (17%) | 78 (18%) | 805 (17%) | |
| Other Educator or Therapist | 171 (4%) | 16 (4%) | 187 (4%) | |
| Primary Language of Familya | .007* | |||
| English | 3186 (73%) | 377 (88%) | 3563 (75%) | |
| Spanish | 895 (21%) | 37 (9%) | 932 (20%) | |
| Cognitive Impairment | .000* | |||
| None | 447 (10%) | 22 (5%) | 469 (10%) | |
| Mild | 244 (6%) | 12 (3%) | 256 (5%) | |
| Moderate | 1830 (42%) | 119 (28%) | 1949 (41%) | |
| Severe | 1831 (42%) | 277 (64%) | 2108 (44%) | |
| Hearing Impairment | .235 | |||
| None | 3525 (81%) | 345 (80%) | 3870 (81%) | |
| Mild | 452 (10%) | 47 (11%) | 499 (10%) | |
| Moderate | 283 (7%) | 23 (5%) | 306 (6%) | |
| Severe | 92 (2%) | 15 (4%) | 107 (2%) | |
| Vision Impairment | .002* | |||
| None | 3059 (70%) | 265 (62%) | 3324 (70%) | |
| Mild | 782 (18%) | 97 (23%) | 879 (18%) | |
| Moderate | 428 (10%) | 55 (13%) | 483 (10%) | |
| Severe | 83 (2%) | 13 (3%) | 96 (2%) | |
| Physical Impairment | .026* | |||
| None | 2857 (66%) | 263 (61%) | 3120 (65%) | |
| Mild | 866 (20%) | 105 (24%) | 971 (20%) | |
| Moderate | 476 (11%) | 54 (13%) | 530 (11%) | |
| Severe | 153 (4%) | 8 (2%) | 161 (3%) | |
| Other Health Impairment | .006* | |||
| None | 336 (77%) | 304 (71%) | 3670 (77%) | |
| Mild | 309 (7%) | 32 (7%) | 341 (7%) | |
| Moderate | 422 (10%) | 55 (13%) | 477 (10%) | |
| Severe | 255 (6%) | 39 (9%) | 294 (6%) | |
| Other Impairment | .001* | |||
| None | 4096 (94%) | 386 (90%) | 4482 (94%) | |
| Mild | 77 (2%) | 10 (2%) | 87 (2%) | |
| Moderate | 115 (3%) | 18 (4%) | 133 (3%) | |
| Severe | 64 (2%) | 16 (4%) | 80 (2%) | |
Note. Count data are presented as n (%). Correlations are between demographics variables and ASD diagnosis. DS = Down syndrome; DS/ASD = Down syndrome/Autism spectrum disorder.
Only above 100 total shown.
p < .05.
Measures
The Communication Matrix (Rowland, 2020) is an online assessment of early expressive communication skills. It can be used to assess individuals with any type or degree of disability. The assessment is organized by four major reasons to communicate: (a) refusing things, (b) obtaining things, (c) engaging in social interaction, and (d) providing or seeking information (Light, 1988). It is comprised of seven levels: (1) Pre-Intentional Behavior, (2) Intentional Behavior, (3) Unconventional Communication, (4) Conventional Communication, (5) Concrete Symbols, (6) Abstract Symbols, and (7) Language. These levels are based on the pragmatic approach to communication development first discussed by Bates et al. (1979) that promotes the importance of acknowledging the communicative intent of prelinguistic behaviors in young children (Rice, 1989). Levels 1–4 involves presymbolic communication through motor and vocal behaviors such as body movements, facial expressions, vocalizations, and simple gestures (hand guiding or touching a person). Referential and conventional gestures begin at Level 4 and include pointing and waving. Levels 5–7 consist of symbolic communication behaviors such as spoken words, picture exchange systems, manual signs, and using a mobile device to indicate symbols. The assessment spans the communication development of typically developing children ages 0–24 months.
The Communication Matrix is conducted by answering a series of 24 questions about early communication skills. For instance, Can you tell that this individual doesn’t want some specific thing, such as a certain food or a toy or a game you’re playing, like tickling? If yes, What does your child do to refuse or reject something?, followed by a list of communication categories and specific behaviors that might be used to convey this message. Users choose not used (0), emerging (1), or mastered (2) for each behavior. After assessments are completed, the information is encrypted in a secure server and stored as part of the Communication Matrix data repository.
Communication Matrix Total Score and Social Score
The Communication Matrix total score represents the degree of mastery on 24 questions. Total scores range from 0–160 possible points. The social communication score represents a subset of the 24 questions related to engaging in social interactions. Scores range from 0–56 possible points.
Referential Gestures and Early Symbolic Behaviors
The assessment covers nine categories of communicative behavior ranging from body movement (such as arm, head movements) to language (combining symbols into multisymbol utterances). Categories of behavior were compared starting at Level 4 with referential and conventional gestures because referential gestures used at early stages of communication are associated with the development of symbolic communication and future expressive language skills (Brady et al., 2004, 2013; Calandrella & Wilcox, 2000; Crais et al., 2004). The percentage of each sample that used specific referential gestures (e.g., pointing, alternating gaze) and types of symbolic communication behaviors (e.g., picture symbols, manual signs, spoken words) was calculated.
Control Variables: Demographics and Functional Impairments
Each assessor is required to complete a brief series of demographic questions before beginning the Communication Matrix assessment. These include a question regarding the profession of the assessor as well as questions about the demographics of the individual being assessed including the diagnosis, source of diagnosis, age, sex, race, state, primary language spoken in the home, and country. The following functional impairments are rated by assessors on a scale of none, moderate, mild, or severe: autism, cognition, hearing, learning, speech/language, vision, physical impairments, other health impairments, and other impairments.
Analytic Approach
Prior to testing our primary research questions, we conducted a preliminary analysis to provide a broad view of communication in the two groups. First, we generated a composite portrait of each group representing the percentage of individuals who expressed each message across the seven levels of communication as represented in each of the 80 cells on the Matrix profile. Due to the number of items on the Communication Matrix assessment (80 questions), running correlations on the items, control variables, and outcome measures may have resulted in false positives or other statistical errors that would not be relevant to the research questions. For this reason we chose not to run correlations on each item. Correlations were run on all demographic variables, functional impairments, and administration date compared to total score and social score to remove any influence of these variables on outcome measures in the regression model (see Table 2). Correlations of p < .05 were included as covariates. Multiple linear regression models were estimated to evaluate our primary research questions of whether individuals with a DS/ASD have significantly lower total scores and lower social scores on the Communication Matrix as compared to individuals with DS. Separate multiple linear regressions adjusted for the covariates and including a dummy variable for diagnosis (DS or DS/ASD) were conducted to determine if diagnosis was a significant predictor of scores. The assumptions for multiple regression were tested and the data met assumptions of normality, linearity, homoscedasticity, multicollinearity.
Table 2.
Pearson Correlations
| ASD | S | A | AD | PA | PL | R | CI | HI | LD | OHI | PI | LI | VI | OI | TS | SS | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Autism Spectrum Disorder | 1 | ||||||||||||||||
| Sex | .045** | 1 | |||||||||||||||
| Age (years) | .119** | .001 | 1 | ||||||||||||||
| Administration Date | .022 | −.015 | .084** | 1 | |||||||||||||
| Profession of Assessor | −.011 | −.033* | −.114** | .068** | 1 | ||||||||||||
| Primary Language | −.034* | −.009 | −.008 | .014 | −.008 | 1 | |||||||||||
| Race | .013 | .002 | −.005 | −.044** | −.005 | −.005 | 1 | ||||||||||
| Cognitive Impairment | .110** | .018 | −.032* | .158** | −.032* | −.032* | −.027 | 1 | |||||||||
| Hearing Impairment | .010 | .010 | .008 | .039** | .008 | .008 | .012 | .036* | 1 | ||||||||
| Learning Disability | .069** | −.013 | .045** | .329** | .045** | .045** | −.011 | .321** | .052** | 1 | |||||||
| Other Health Impairment | .051** | −.018 | −.001 | .157** | −.001 | −.001 | −.009 | .124** | .137** | .204** | 1 | ||||||
| Physical Impairment | .010 | −.015 | .026 | .165** | .026 | .026 | −.011 | .179** | .091** | .253** | .368** | 1 | |||||
| Language Impairment | .069** | .003 | .131** | 199** | .131** | .131** | −.009 | .385** | .059** | .287** | .130** | .188** | 1 | ||||
| Vision Impairment | .052** | −.033* | −.007 | .079** | −.007 | −.007 | .000 | .125** | .213** | .133** | .191** | .208** | .077** | 1 | |||
| Other Impairment | .058** | −.016 | −.033* | .110** | −.033* | −.033* | −.004 | .088** | .088** | .150** | .310** | .258** | .070** | .123** | 1 | ||
| Total Score | −.137** | −.039** | −.026 | .035* | −.026 | −.026 | .013 | −.110** | −.021 | −.037* | −.123** | −.195** | −.062** | −.076** | −.089** | 1 | |
| Social Score | −.162** | −.050** | −.043** | .020 | −.043** | −.043** | .012 | −.118** | −.023 | −.044** | −.115** | −.179** | −.073** | −.073** | −.081** | .946** | 1 |
Correlation is significant at p < .05, two tailed.
Correlation is significant at p < .01, two tailed.
Chi-squared tests were performed to determine if there were significant differences in the proportion of individuals with DS and DS/ASD using specific referential gestures and symbolic communication behaviors (Levels 4–7 on the Communication Matrix). These specific behaviors were chosen because they relate to future expressive communication skills. Analyses were conducted with IBM SPSS Statistics Version 24.
Results
Preliminary Results
Figures 1 and 2 show that individuals with DS expressed more messages than individuals with DS/ASD. Preliminary descriptive statistics revealed between group differences in referential behaviors used to communicate, characterized by fewer participants with DS/ASD communicating using referential gestures (Level 4), concrete symbols (Level 5), abstract symbols (Level 6), and language (Level 7).
Figure 1.
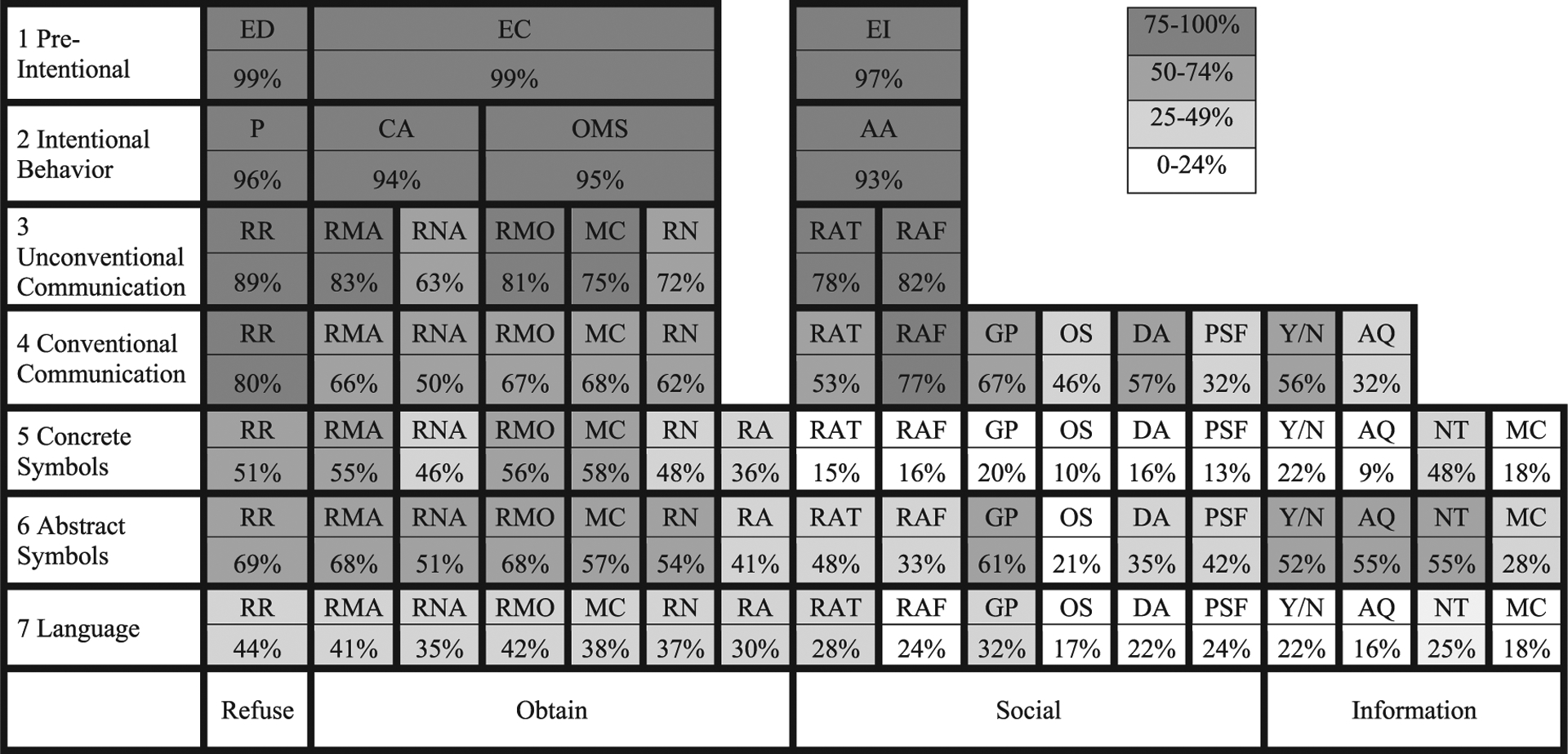
Composite Profile for Individuals With Down Syndrome. Composite profile showing the percentage of individuals with Down syndrome who expressed each communication message. Level 1: ED = Expresses Discomfort; EC = Expresses Comfort; EI = Expresses Interest in Other People; Level 2: P = Protests; CA = Continues Action; OMS = Obtains More of Something; AA = Attracts Attentions; Levels 3–7: RR = Refuses, Rejects; RMA = Requests More Actions; RNA = Requests New Actions; RMO = Requests More Objects; MC = Makes Choices; RN = Requests New Object; RA = Requests Absent Object; RAT = Requests Attention; RAF = Requests Affections; GP = Greets People; OS = Offers, Shares; DA = Directs Attentions; PSF = Polite Social Forms; Y/N = Answers Yes/No Answers; AQ = Answers Questions; NT = Names Things/People; MC = Makes Comments.
Figure 2.
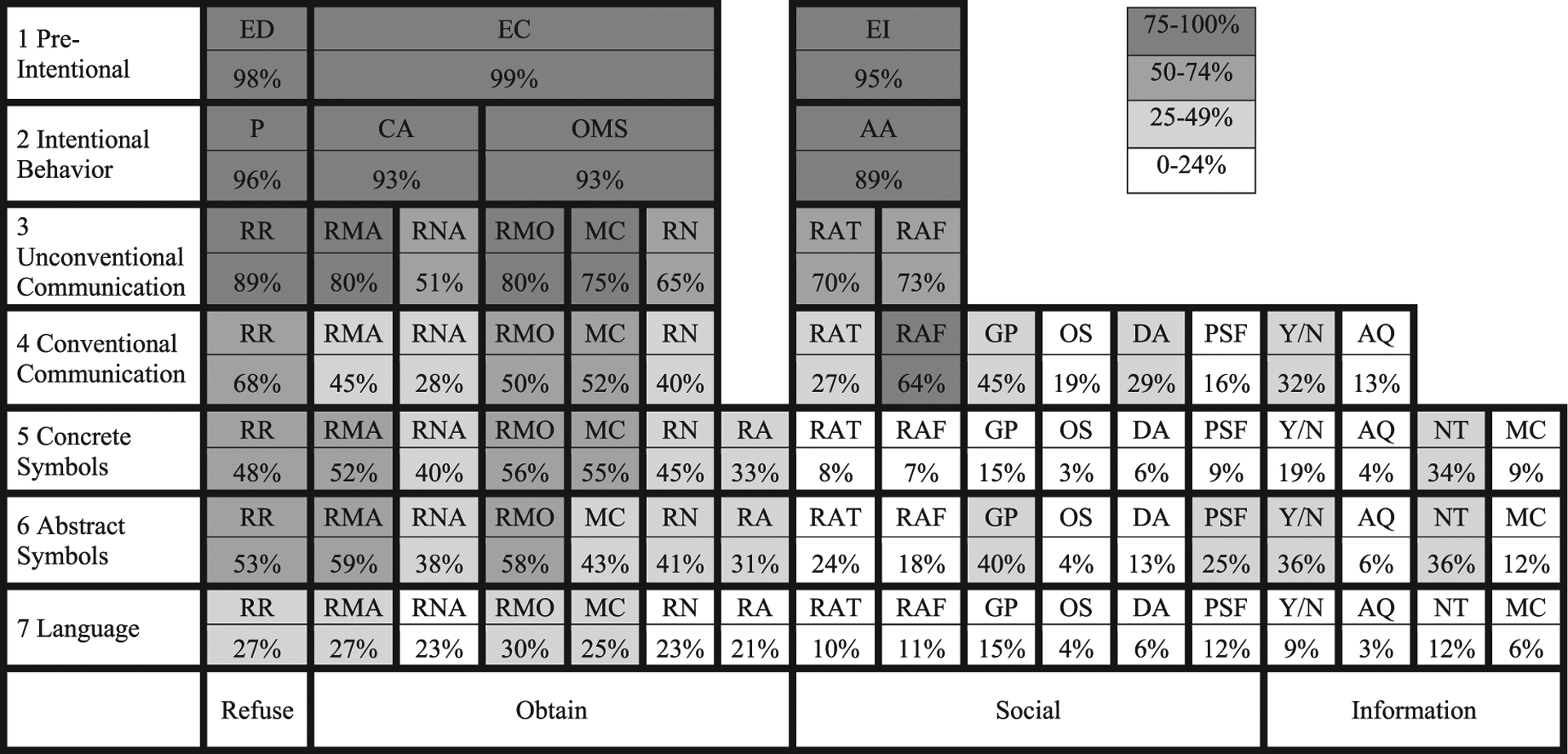
Composite Profile for Individuals With Comorbid Down Syndrome and Autism Spectrum Disorder. Composite profile showing the percentage of individuals with comorbid Down syndrome and Autism spectrum disorder who expressed each communication message. Level 1: ED = Expresses Discomfort; EC = Expresses Comfort; EI = Expresses Interest in Other People; Level 2: P = Protests; CA = Continues Action; OMS = Obtains More of Something; AA = Attracts Attentions; Levels 3–7: RR = Refuses, Rejects; RMA = Requests More Actions; RNA = Requests New Actions; RMO = Requests More Objects; MC = Makes Choices; RN = Requests New Object; RA = Requests Absent Object; RAT = Requests Attention; RAF = Requests Affections; GP = Greets People; OS = Offers, Shares; DA = Directs Attentions; PSF = Polite Social Forms; Y/N = Answers Yes/No Answers; AQ = Answers Questions; NT = Names Things/People; MC = Makes Comments.
Communication Matrix Scores
Multiple linear regressions were conducted to determine if a comorbid diagnosis of DS and ASD was a significant predictor of total score and social score on the Communication Matrix after adjusting for significant covariates. Comorbid diagnosis was a significant predictor of total score, F(10, 4771) = 56.029, p < .001, adjusted R2 = .103 (see Table 3). Adjusting for the covariates, the estimated marginal means for individuals with DS and DS/ASD were 67.386 (SE = 0.525), 95% CI [66.357, 68.4115] and 49.376 (SE = 1.693), 95% CI [46.058, 52.694] respectively. Comorbid diagnosis was a significant predictor of social score, F(10, 4771) = 52.740, p < .001, adjusted R2 = .098 (see Table 4). Adjusting for the covariates, the estimated marginal means for individuals with DS and DS/ASD were 16.159 (SE = 0.182), 95% CI [15.82, 16.515], and 8.901 (SE = 0.587), 95% CI [7.751, 10.052] respectively.
Table 3.
Summary of Regression Analysis for Study Group Predicting the Communication Matrix Total Score
| Measure | B | SE | p values |
|---|---|---|---|
| Constant (Total Score) | 19.80 | 105.72 | .85 |
| Comorbid diagnosis | −17.45* | 1.93* | .00* |
| Age | 1.28* | 0.11* | .00* |
| Administration date | 0.00 | 0.00 | .66 |
| Sex | −2.72* | 1.02* | .01* |
| Profession of assessor | −0.37 | 0.75 | .63 |
| Primary language | −0.09* | 0.03* | .01* |
| Race | 0.89* | 0.19* | .00* |
| Cognitive impairment | −3.86* | 0.57* | .00* |
| Physical impairment | −5.68 | 0.72* | .006* |
| Hearing impairment | −2.03* | 0.73* | .00* |
| Speech-language impairment | −0.25 | 0.53 | .63 |
| Vision impairment | −0.28 | 0.71 | .70 |
| Other impairment | −0.43 | 1.20 | .72 |
| Other Health Impairment | −1.94* | 0.70* | .006* |
p < 0.05.
Table 4.
Summary of Regression Analysis for Study Group Predicting the Communication Matrix Social Score
| Measure | B | SE | p values |
|---|---|---|---|
| Constant (Social Score) | 11.97 | 38.60 | .76 |
| Comorbid diagnosis | −7.40* | 0.71* | .00* |
| Age | .44* | 0.038* | .00* |
| Administration date | 0.00 | 0.00 | .79 |
| Sex | −1.20* | 0.37* | .001* |
| Profession of assessor | −0.11 | 0.27 | .69 |
| Primary language | −0.03 | 0.01 | .04 |
| Race | 0.22* | 0.07* | .001* |
| Cognitive impairment | −1.45* | 0.21v | .00* |
| Physical impairment | −1.80* | 0.26 | .004* |
| Hearing impairment | −0.78 | 0.27* | .00* |
| Speech-language impairment | −0.29 | 0.19 | .13 |
| Vision impairment | −0.13 | 0.26 | .61 |
| Other impairment | −0.09 | 0.44 | .84* |
| Other Health Impairment | −0.71 | 0.26 | .006* |
p < 0.05.
Communication Behaviors Used to Express Messages/Intents
To further explore between-group differences in performance on the Communication Matrix, we conducted an analysis of expressive communication behaviors including referential gestures and symbolic communication. Chi-squared tests were conducted to explore whether the proportion of participants with DS/ASD using specific expressive communication behaviors was significantly smaller than the proportion of participants with DS. Table 5 presents the percentage of participants who used specific referential gestures, conventional gestures, and symbolic behaviors. Findings from individual contrasts controlling for multiple comparisons with a Bonferroni correction (p < 0.003) indicated there were significant differences between groups, with the DS group using more referential and conventional gestures, including alternating gaze, beckoning, giving/showing, head nodding, pointing, head shaking “no,” pointing, head shaking, shrugging shoulders, waving “hello” and “goodbye,” two dimensional concrete symbols (e.g., photo of a pretzel), three dimensional concrete symbols (e.g., pretzel shape glued to paper), manual signs, spoken words, and combining two or more symbols. There were no significant differences between groups on some symbolic behaviors, including the use of two dimensional abstract symbols (e.g., line drawing of “playground”), three dimensional abstract symbols (e.g., an abstract 3-dimensional shape to represent going outside to the playground), or written words.
Table 5.
Percentage of Individuals Who Used Referential and Conventional Gestures and Symbolic Behavior by Diagnosis
| Behavior | DS | DS/ASD | p value |
|---|---|---|---|
| Referential and Conventional Gestures | |||
| Alternating Gaze | 70.5 | 51.6 | 0.00* |
| Beckons | 58.4 | 29.1 | 0.00* |
| Give/show item | 75.3 | 61.2 | 0.00* |
| Nods head | 59.8 | 29.1 | 0.00* |
| Point | 72.8 | 50.0 | 0.00* |
| Shake head “no” | 51.9 | 26.0 | 0.00* |
| Shrug shoulders | 34.6 | 10.2 | 0.00* |
| Wave “hi,” “bye” | 67.2 | 44.7 | 0.00* |
| Concrete Symbols | |||
| 2-D symbol | 72.2 | 71.9 | 0.00* |
| 3-D symbol | 63.0 | 58.6 | 0.00* |
| Abstract Symbols | |||
| Abstract 2-D symbols | 30.1 | 34.9 | 0.06 |
| Abstract 3-D symbols | 12.2 | 11.4 | 0.73 |
| Manual signs | 62.8 | 51.2 | 0.00* |
| Spoken word | 70.7 | 46.5 | 0.00* |
| Written word | 13.9 | 10.5 | 0.05 |
| Language | |||
| Combine 2+ symbols | 56.6 | 40.7 | 0.00* |
Note. N = 4,352 for DS and N = 430 for DS/ASD. Chi-squared tests were performed to investigate between group differences in communication behavior. The p value was adjusted for multiple significance testing using a Bonferroni correction, the critical value for this series of Chi-squared tests is p < 0.003. DS = Down syndrome; DS/ASD = Down syndrome/Autism spectrum disorder.
p < 0.003.
Discussion
This is the first study to extract data from the Communication Matrix registry and generate a composite profile of early expressive communication skills for individuals with DS (n = 4,352) and individuals with DS/ASD (n = 430). The composite profiles show a detailed view of how individuals with DS and DS/ASD express 24 communication behaviors which depict greater abstract symbol and language use in individuals with DS when compared to individuals with DS/ASD.
Prelinguistic and Early Symbolic Communication in Individuals With DS and DS/ASD
Findings from this study are consistent with our research hypotheses and results of prior research on individuals with DS and DS/ASD, indicating individuals with DS/ASD have significantly lower expressive communication skills than individuals with a diagnosis of DS alone (Capone et al., 2005; Godfrey et al., 2019; Molloy et al., 2009). Individuals with comorbid DS/ASD had significantly lower total and social scores on the Communication Matrix. Total scores for individuals with DS/ASD were on average 18.01 points lower than scores for individuals with DS. The average difference in total score is clinically significant, because it is equivalent to the expression of 9–18 messages or intents. In other words, individuals with a dual diagnosis have on average 9–18 fewer ways to communicate their thoughts, desires, and feelings using vocalizations, gestures, manual signs, symbols, and spoken words. For an individual with beginning communication skills, these differences may have implications for language growth (Brady et al., 2004; Calandrella & Wilcox, 2000; Yoder & Warren, 2004; Zampini & D’Odorico, 2009, 2013). Social scores for individuals with a comorbid diagnosis were on average 7.26 points lower than scores for individuals with DS. This finding replicates Godfrey et al.’s (2019) finding that individuals with DS/ASD had greater social communication impairments than individuals with DS. This difference on the social subscale is equivalent of individuals with DS using on average 3–7 more social communication behaviors than individuals with DS/ASD. This finding is significant, because social communication skills predict language outcomes (Wetherby et al., 2007).
Both multiple linear regression models accounted for a small amount of the variance in total expressive communication scores (10%) which suggested there is a high amount of within-syndrome variability in expressive communication skills as measured by the Communication Matrix. This finding was consistent with prior research demonstrating large within-syndrome variability in expressive communication skills (Abbeduto et al., 2016; Finestack & Abbeduto, 2010; Finestack et al., 2012).
Referential and conventional gestures, spoken words, and symbol combinations were significantly higher in individuals with DS. But, individuals with DS and DS/ASD both used abstract symbols (e.g., line drawings, objects) and written words at a similarly low frequency. More investigation is required to determine the significance of these findings. It is possible that both populations would benefit from increased access to abstract symbols.
Many communication assessments are limited due to floor effects for individuals with presymbolic and early symbolic communication skills, and for individuals who use nonspoken responses (Brady et al., 2012; Esbensen et al., 2017; Mervis & Robinson, 2005). The current study adds to research on individuals with comorbid DS/ASD by providing a detailed profile of early expressive communication skills.
Influence of Demographic and Individual Characteristics
Importantly, the current study showed in a large sample of individuals with DS/ASD and DS that between-group differences in early expressive communication skills persist after controlling for potential confounding variables including age, administration date, sex, cognitive impairment, physical impairment, speech and language impairment, vision impairment, other health impairment, and other impairment. These findings replicate the results of many smaller studies of communication in individuals with DS/ASD as compared to individuals with DS. (Capone et al., 2005; Molloy et al., 2009; Moss et al., 2013; Warner et al., 2014). Many factors contribute to communication skills in addition to dual diagnosis. Controlling for demographic information and functional impairments were important to our findings and has implication for practice when determining the tools an individual has for their learning process. Although the measure of cognitive impairment in this study is rated on a scale of none, mild, moderate, and severe instead of tested directly, the main findings are in line with other studies showing behavior and communication differences remain between groups of individuals with DS and DS/ASD even after controlling for cognitive ability (Capone et al., 2005; Molloy et al., 2009; Moss et al., 2013). These results indicate a meaningful significant difference in the expressive communication skills of individuals with DS and DS/ASD even when controlling for cognition.
Benefits of Large Data
This study was innovative because it was the first to use an existing clinical repository with a large sample of individuals with DS and DS/ASD to describe pre-intentional and early symbolic communication behaviors. Online databases, repositories, or registries have potential to inform diagnostic assessment and intervention for individuals with physical, intellectual, or developmental disabilities (Iezzoni, 2002), and more specifically children with DS (McCabe & McCabe, 2011). Large sample sizes are essential in achieving sufficient statistical power to potentially identify common corollaries, effects, behaviors, symptoms, and biological markers with small effect sizes that may not be discovered through research with smaller samples. Research registries and online databases are especially important for individuals with IDD because researchers may not have access to a large, diverse sample in their own community or through their own research network. Registries have been created for IDD including ASD (Feliciano et al., 2018), cerebral palsy (Hurley et al., 2011), and DS (Peprah et al., 2015). The Communication Matrix repository complements these existing patient registries by providing detailed information on early communication skills including presymbolic and symbolic behaviors.
Limitations
This study is limited by sampling bias because data was from a repository of assessments conducted by professionals. The Communication Matrix is designed for individuals who are in the early stages of communication and may include individuals with more severe impairments relative to the larger population of individuals with DS and DS/ASD. Consequently, our data may reflect an underestimation of expressive communication skills and our findings should be viewed in light of this limitation. It is also possible that these assessors and the people they are assessing have important differences from the typical populations of individuals with DS, such as access to speech and language services and professionals who have time and technology literacy sufficient to complete an online assessment.
A second limitation of this research includes the use of third-party report. The Communication Matrix is conducted using informant report instead of systematic observation or direct assessment of early communication skills. This measurement approach allowed for a much larger sample size, but did not allow for direct assessment or independent validation of expressive communication skills, demographic characteristics such as cognitive ability, or ASD diagnosis and severity. Although assessors marked that diagnosis was confirmed by at least one professional, there was no independent ASD or DS diagnosis by the researchers themselves. This population of individuals with a comorbid diagnosis of DS/ASD in particular may be sensitive to false positives (Channell et al., 2015). Due to the third party nature of collecting the data, we cleaned the data of duplicate entries based on demographic data and personal identifier. A fraction of assessment matched on demographic data, but not personal identifier (n = 760) and were included in the sample. Although unlikely, it is possible that some of these assessments were completed about the same individual and remain in the sample used for analysis thus skewing the results. Assessors indicated cognitive impairments were mild, moderate, or severe, however it is difficult to interpret these categorical assessments and relate these categories to extent research. For individuals with DS, there is a large range in cognitive ability with IQs ranging from 30 to 70 and an average IQ of 50 which corresponds with a moderate impairment (Chapman & Hesketh, 2000). In this study 42% of individuals with DS had moderate cognitive impairments and 42% had severe cognitive impairments whereas 28% of individuals with DS/ASD had moderate cognitive impairments and 64% had severe cognitive impairments. In a recent study examining the risks associated with ASD in individuals with DS, Channel et al. (2019) found that 35% of individuals with DS scored at the floor of the Kaufman Brief Intelligence Test, Second Edition (Kaufman & Kaufman, 2004), and 75% of those with a high risk for ASD scored at the floor. This suggests individuals with DS have wide variability in IQ and individuals with DS/ASD are more likely to have severe cognitive impairments. Replication of this study is necessary to mitigate the previous limitations and strengthen its conclusions.
Future Research
Next steps in this area of research include a replication and expansion of the current study. Future studies should describe the early expressive communication skills of individuals with DS and DS/ASD using a variety of measurement systems. For example, investigators may apply direct assessment procedures using (a) standardized assessments of language, cognition, and communication; (b) observational assessments of language and communication skills; and (c) informant report measures of language and communication skills. Additionally, future studies should confirm the diagnosis of the sample of individuals with DS/ASD using the Autism Diagnostic Interview (Rutter, Le Couteur, & Lord, 2003) and the Autism Diagnostic Observation Schedule – 2nd edition (Lord et al., 2012). An exploration of moderating factors would contribute to our knowledge of phenotypical differences and inform policy and intervention. If the covariates were more precise, the expectation would be that this study would result in a greater amount of the variance being accounted for by a dual diagnosis. The research would also benefit from a longitudinal study investigating communication skill growth in a large sample. This addition would provide more information on the average trajectory of individuals with DS and DS/ASD.
Research describing the behavioral phenotype of individuals with DS and DS/ASD can support the design and implementation of interventions optimized for their specific needs (McDaniel & Yoder, 2016). Within-syndrome variability has important implications for designing future studies on the efficacy of early language and communication interventions. Designing language interventions for individuals with DS and DS/ASD with variations in dosage, instructional strategy, communication partner, and communication modality may optimize language interventions for individuals with a wide range of expressive communication skills (e.g., presymbolic, early symbolic, and emergent language). Tailoring interventions based on the individual’s pretreatment expressive communication skills may be critically important for maximizing spoken language outcomes for individuals with DS and DS/ASD.
Previous research highlighted the potential for “diagnostic overshadowing” in individuals with IDD, the idea that characteristics of one diagnosis may make it easier to miss characteristics of another syndrome or disorder (Dykens, 2007). In children with DS, symptoms of comorbid ASD are frequently attributed to the DS behavioral phenotype or to overall cognitive ability. Although the Communication Matrix is not developed for the purposes of differential diagnosis, results from the current study suggest that some referential, conventional gestures and symbolic communication skills vary by diagnostic group, and this knowledge may contribute to screening measures or diagnostic measures adapted for individuals with comorbid DS/ASD. Continued research on the development of early communication behaviors in individuals with DS and DS/ASD may minimize the potential for diagnostic overshadowing.
Conclusions
It is clear from this research and previous studies (Godfrey et al., 2019; Molloy et al., 2009; Moss et al., 2013; Warner et al., 2014) that individuals with a comorbid diagnosis of DS/ASD have measurable differences in expressive communication as compared to individuals with DS. This large scale study confirms DS/ASD phenotype is distinct from individuals with DS. The small amount of variance that was accounted for by a comorbid diagnosis when controlling for other factors associated with expressive communication suggests a wide variability in this population of individuals with DS and complex communication needs. Practitioners and family members may improve intervention and assessment effectiveness by considering the comorbid diagnosis as some-what separate from a diagnosis of DS and recognizing the unique strengths and challenges associated with such a diagnosis. Research would benefit the IDD community by concentrating on this subpopulation that has a distinct set of symptoms and behaviors and analyzing other factors that may help to explain the large variability observed.
Acknowledgments
The authors would like to thank the many individuals with complex communication needs, their family members, and professionals who have participated in this research. This research was supported in part by Grants H327A110010 and H327S130010 from the U.S. Department of Education and 1013200 from the U.S. Department of Health and Human Services Agency for Healthcare Research and Quality.
References
- Abbeduto L, McDuffie A, Thurman AJ, & Kover ST (2016). Chapter Three - Language development in individuals with intellectual and developmental disabilities: From phenotypes to treatments. In Hodapp RM & Fidler DJ (Eds.), International review of research in developmental disabilities (pp. 71–118). Academic Press. 10.1016/bs.irrdd.2016.05.006 [DOI] [Google Scholar]
- Adamson L, Bakeman R, & Deckner D (2004). The development of symbol infused joint engagement. Child Development, 75(4), 1171–1187. [DOI] [PubMed] [Google Scholar]
- Adamson LB, Bakeman R, Deckner DF, & Nelson PB (2012). Rating parent–child interactions: Joint engagement, communication dynamics, and shared topics in autism, Down syndrome, and typical development. Journal of Autism and Developmental Disorders, 42(12), 2622–2635. 10.1007/s10803-012-1520-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bates E, Benigni L, Bretherton I, Camaioni L, & Volterra V (1979). The emergence of symbols: Cognition and communication in infancy. Academic Press. [Google Scholar]
- Bell CC (1994). DSM-IV: Diagnostic and Statistical Manual of Mental Disorders. JAMA: The Journal of the American Medical Association, 272(10), 828–829. 10.1001/jama.1994.03520100096046 [DOI] [Google Scholar]
- Berglund E, Eriksson M, & Johansson I (2001). Parental reports of spoken language skills in children with Down syndrome. Journal of Speech, Language, and Hearing Research, 44(1), 179–191. 10.1044/1092-4388(2001/016) [DOI] [PubMed] [Google Scholar]
- Brady NC, Fleming K, Thiemann-Bourque K, Olswang L, Dowden P, Saunders MD, & Marquis J (2012). Development of the communication complexity scale. American Journal of Speech-Language Pathology, 21(1), 16–28. 10.1044/1058-0360(2011/10-0099) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brady NC, Marquis J, Fleming K, & McLean L (2004). Pre-linguistic predictors of language growth in children with developmental disabilities. Journal of Speech, Language, and Hearing Research, 47(3), 663–677. [DOI] [PubMed] [Google Scholar]
- Brady NC, Thiemann-Bourque K, Fleming K, & Matthews K (2013). Predicting language outcomes for children learning augmentative and alternative communication: Child and environmental factors. Journal of Speech, Language, and Hearing Research, 56(5), 1595–1612. 10.1044/1092-4388(2013/12-0102) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calandrella AM, & Wilcox MJ (2000). Predicting language outcomes for young prelinguistic children with developmental delay. Journal of Speech, Language, and Hearing Research, 43(5), 1061–1071. 10.1044/jslhr.4305.1061 [DOI] [PubMed] [Google Scholar]
- Capone G, Grados MA, Kaufmann WE, Bernad-Ripoll S, & Jewell A (2005). Down syndrome and comorbid autism-spectrum disorder: Characterization using the aberrant behavior checklist. American Journal of Medical Genetics Part A, 134A(4), 373–380. 10.1002/ajmg.a.30622 [DOI] [PubMed] [Google Scholar]
- Carter JC, Capone GT, Gray RM, Cox CS, & Kaufmann WE (2007). Autistic-spectrum disorders in Down syndrome: Further delineation and distinction from other behavioral abnormalities. American Journal of Medical Genetics Part B: Neuropsychiatric Genetics, 144B(1), 87–94. 10.1002/ajmg.b.30407 [DOI] [PubMed] [Google Scholar]
- Channell MM, Hahn LJ, Rosser TC, Hamilton D, Frank-Crawford MA, Capone GT, Sherman SL, & The Down Syndrome Cognition Project. (2019). Characteristics associated with autism spectrum disorder risk in individuals with Down syndrome. Journal of Autism and Developmental Disorders, 49(9), 3543–3556. 10.1007/s10803-019-04074-1 [DOI] [PubMed] [Google Scholar]
- Channell MM, Phillips BA, Loveall SJ, Conners FA, Bussanich PM, & Klinger LG (2015). Patterns of autism spectrum symptomatology in individuals with Down syndrome without comorbid autism spectrum disorder. Journal of Neurodevelopmental Disorders, 7(1), 1–9. 10.1186/1866-1955-7-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapman RS, & Hesketh LJ (2000). Behavioral phenotype of individuals with Down syndrome. Mental Retardation and Developmental Disabilities Research Reviews, 6(2), 84–95. [DOI] [PubMed] [Google Scholar]
- Crais E, Douglas DD, & Campbell CC (2004). The intersection of the development of gestures and intentionality. Journal of Speech, Language, and Hearing Research, 47(3), 678–694. 10.1044/1092-4388(2004/052). [DOI] [PubMed] [Google Scholar]
- DiGuiseppi C, Hepburn S, Davis JM, Fidler DJ, Hartway S, Lee NR, Miller L, Ruttenber M, & Robinson C (2010). Screening for autism spectrum disorders in children with Down syndrome: Population prevalence and screening test characteristics. Journal of Developmental & Behavioral Pediatrics, 31(3), 181–191. 10.1097/DBP.0b013e3181d5aa6d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dykens EM (2007). Psychiatric and behavioral disorders in persons with Down syndrome. Mental Retardation and Developmental Disabilities Research Reviews, 13(3), 272–278. 10.1002/mrdd.20159 [DOI] [PubMed] [Google Scholar]
- Esbensen AJ, Hooper SR, Fidler D, Hartley SL, Edgin J, d’Ardhuy XL, Capone G, Conners FA, Mervis CB, Abbeduto L, Rafii M, Krinsky-McHale SJ, Urv T, & Outcomes Measures Working Group. (2017). Outcome measures for clinical trials in Down syndrome. American Journal on Intellectual and Developmental Disabilities, 122(3), 247–281. 10.1352/1944-7558-122.3.247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feliciano P, Daniels AM, Green Snyder L, Beaumont A, Camba A, Esler A, Gulsrud AG, Mason A, Gutierrez A, Nicholson A, Paolicelli AM, McKenzie AP, Rachubinski AL, Stephens AN, Simon AR, Stedman A, Shocklee AD, Swanson A, Finucane B, & Chung WK (2018). SPARK: A U.S. cohort of 50,000 families to accelerate autism research. Neuron, 97(3), 488–493. 10.1016/j.neuron.2018.01.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finestack LH, & Abbeduto L (2010). Expressive language profiles of verbally expressive adolescents and young adults with Down syndrome or fragile X syndrome. Journal of Speech, Language, and Hearing Research, 53(5), 1334–1348. 10.1044/1092-4388(2010/09-0125) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finestack LH, Palmer M, & Abbeduto L (2012). Macrostructural Narrative language of adolescents and young adults with Down syndrome or fragile X syndrome. American Journal of Speech-Language Pathology, 21(1), 29–46. 10.1044/1058-0360(2011/10-0095) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Godfrey M, Hepburn S, Fidler DJ, Tapera T, Zhang F, Rosenberg CR, & Raitano Lee N (2019). Autism spectrum disorder (ASD) symptom profiles of children with comorbid Down syndrome (DS) and ASD: A comparison with children with DS-only and ASD-only. Research in Developmental Disabilities, 89, 83–93. 10.1016/j.ridd.2019.03.003 [DOI] [PubMed] [Google Scholar]
- Hurley DS, Sukal-Moulton T, Msall ME, Gaebler-Spira D, Krosschell KJ, & Dewald JP (2011). The Cerebral palsy research registry: Development and progress toward national collaboration in the United States. Journal of Child Neurology, 26(12), 1534–1541. 10.1177/0883073811408903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iezzoni LI (2002). 4. Using administrative data to study persons with disabilities. The Milbank Quarterly, 80(2), 347–379. 10.1111/1468-0009.t01-1-00007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaat-van den Os DT, Volman C, Jongmans M, & Lauteslager P (2017). Expressive vocabulary development in children with Down syndrome: A longitudinal study. Journal of Policy and Practice in Intellectual Disabilities, 14(4), 311–318. 10.1111/jppi.12212 [DOI] [Google Scholar]
- Kaufman AS, & Kaufman NL (2004). Kaufman Brief Intelligence Test (2nd ed.). AGS Publishing. [Google Scholar]
- Light J (1988). Interaction involving individuals using augmentative and alternative communication systems: State of the art and future directions. Augmentative and Alternative Communication, 4(2), 66–82. 10.1080/07434618812331274657 [DOI] [Google Scholar]
- Lord C, Rutter M, DiLavore PC, Risi S, Gotham K, & Bishop SL (2012). Autism Diagnostic Observation Schedule, (ADOS-2) modules 1–4. Western Psychological Services. [Google Scholar]
- McCabe LL, & McCabe ERB (2011). Down syndrome: Issues to consider in a national registry, research database and biobank. Molecular Genetics and Metabolism, 104(1–2), 10–12. 10.1016/j.ymgme.2011.03.018 [DOI] [PubMed] [Google Scholar]
- McDaniel J, & Yoder PJ (2016). Pursuing precision speech-language therapy services for children with Down syndrome. Seminars in Speech and Language, 37, 239–251. https://doi.org/10.1055s_0036-1587708 [DOI] [PubMed] [Google Scholar]
- Mervis CB, & Robinson BF (2005). Designing measures for profiling and genotype/phenotype studies of individuals with genetic syndromes and developmental language disorders. Applied Psycholinguistics, 26, 41–64. https://doi.org/10.1017.S0142716405050058 [Google Scholar]
- Molloy CA, Murray DS, Kinsman A, Castillo H, Mitchell T, Hickey FJ, & Patterson B (2009). Differences in the clinical presentation of Trisomy 21 with and without autism. Journal of Intellectual Disability Research, 53(2), 143–151. 10.1111/j.1365-2788.2008.01138.x [DOI] [PubMed] [Google Scholar]
- Moss J, & Howlin P (2009). Autism spectrum disorders in genetic syndromes: Implications for diagnosis, intervention and understanding the wider autism spectrum disorder population. Journal of Intellectual Disability Research, 53(10), 852–873. 10.1111/j.1365-2788.2009.01197.x [DOI] [PubMed] [Google Scholar]
- Moss J, Richards C, Nelson L, & Oliver C (2013). Prevalence of autism spectrum disorder symptomatology and related behavioural characteristics in individuals with Down syndrome. Autism, 17(4), 390–404. 10.1177/1362361312442790 [DOI] [PubMed] [Google Scholar]
- Mullen EM (1995). Mullen Scales of Early Learning. Circle Pines. [Google Scholar]
- Parker SE, Mai CT, Canfield MA, Rickard R, Wang Y, Meyer RE, Anderson P, Mason CA, Collins JS, Kirby RS, Correa A, for the National Birth Defects Prevention Network. (2010). Updated national birth prevalence estimates for selected birth defects in the United States, 2004–2006. Birth Defects Research Part A: Clinical and Molecular Teratology, 88(12), 1008–1016. 10.1002/bdra.20735 [DOI] [PubMed] [Google Scholar]
- Peprah EK, Parisi MA, Kaeser L, Bardhan S, Oster-Granite M, & Maddox YT (2015). DS-Connect. Global Heart, 10(4), 337–340. 10.1016/j.gheart.2015.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reilly C (2009). Autism spectrum disorders in Down syndrome: A review. Research in Autism Spectrum Disorders, 3(4), 829–839. 10.1016/j.rasd.2009.01.012 [DOI] [Google Scholar]
- Rice RE (1989). Issues and concepts in research on computer-mediated communication systems. Annals of the International Communication Association, 12(1), 436–476. 10.1080/23808985.1989.11678731 [DOI] [Google Scholar]
- Roberts JE, Price J, & Malkin C (2007). Language and communication development in Down syndrome. Mental Retardation & Developmental Disabilities Research Reviews, 13(1), 26–35. 10.1002/mrdd.20136 [DOI] [PubMed] [Google Scholar]
- Romano M, Kaiser A, Lounds-Taylor J, & Woods J (2019). Rates of prelinguistic communication and early symbol use in young children with Down syndrome: Using a progress-monitoring tool to model growth. American Journal of Speech-Language Pathology, 29(1), 49–62. 10.1044/2019_AJSLP-19-0016 [DOI] [PubMed] [Google Scholar]
- Rowland C (2011). Using the Communication Matrix to assess expressive skills in early communicators. Communication Disorders Quarterly, 32(3), 190–201. 10.1177/1525740110394651 [DOI] [Google Scholar]
- Rowland C (2020). Communication Matrix. Communication Matrix Foundation. https://communicationmatrix.org/ [Google Scholar]
- Rutter M, Bailey A, & Lord C (2003). Social Communication Questionnaire (SCQ). Western Psychological Services. [Google Scholar]
- Rutter M, Le Couteur A, & Lord C (2003). Autism Diagnostic Interview-Revised. Western Psychological Services. [Google Scholar]
- Spencer PE (2011). Prelinguistic communication. In Goldstein S & Naglieri JA (Eds.), Encyclopedia of Child Behavior and Development, (pp. 1145–1146). Springer. 10.1007/978-0-387-79061-9_2218 [DOI] [Google Scholar]
- Thiemann-Bourque KS, Warren SF, Brady N, Gilkerson J, & Richards JA (2014). Vocal interaction between children with Down syndrome and their parents. American Journal of Speech-Language Pathology, 23(3), 474–485. 10.1044/2014_AJSLP-12-0010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vandereet J, Maes B, Lembrechts D, & Zink I (2011). The role of gestures in the transition from one to two-word speech in a variety of children with intellectual disabilities. International Journal of Language & Communication Disorders, 46(6), 714–727. 10.1111/j.1460-6984.2011.00050.x [DOI] [PubMed] [Google Scholar]
- Warner G, Moss J, Smith P, & Howlin P (2014). Autism characteristics and behavioural disturbances in ~ 500 children with Down’s syndrome in England and Wales: Autism features in Down’s syndrome. Autism Research, 7(4), 433–441. 10.1002/aur.1371 [DOI] [PubMed] [Google Scholar]
- Wetherby AM, Watt N, Morgan L, & Shumway S (2007). Social communication profiles of children with autism spectrum disorders late in the second year of life. Journal of Autism and Developmental Disorders, 37(5), 960–975. 10.1007/s10803-006-0237-4 [DOI] [PubMed] [Google Scholar]
- Wilson EM, Abbeduto L, Camarata SM, & Shriberg LD (2019). Estimates of the prevalence of speech and motor speech disorders in adolescents with Down syndrome. Clinical Linguistics & Phonetics, 33(8), 772–789. 10.1080/02699206.2019.1595735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoder PJ, & Warren SF (2004). Early predictors of language in children with and without Down syndrome. American Journal on Mental Retardation, 109(4), 285–300 [DOI] [PubMed] [Google Scholar]
- Zampini L, & D’Ordorico L (2009). Communicative gestures and vocabulary development in 36 month old children with Down’s syndrome. International Journal of Language & Communication Disorders, 44(6), 1063–1073. 10.3109/13682820802398288. [DOI] [PubMed] [Google Scholar]
- Zampini L, & D’Ordorico L (2013). Vocabulary development in children with Down syndrome: Longitudinal and cross sectional data. Journal of Intellectual and Developmental Disability, 38(4), 310–317. 10.3109/13668250.2013.828833 [DOI] [PubMed] [Google Scholar]


