Abstract
Introduction
Given the fragility of reusable ureterorenoscopes, many single use instruments have appeared on the market. Unfortunately, reuse of these scopes occurs in undeveloped countries in order to cut costs. This raises safety concerns for the patient.
The aim of this article was to macroscopically evaluate the changes that single use flexible ureterorenoscopes (su-fURS) suffer after a retrograde intrarenal surgery (RIRS), and to compare them to reusable fURS.
Material and methods
Pre and post-operative images of the instruments used in 23 RIRS were obtained. All the cases had renal calculi of the inferior calix between 10–15 mm, and all of them were treated with Holmium laser. The ureterorenoscopes used were: Storz® Flex X2, Storz® Flex XC, Pusen® 3022, OTU® Wiscope, AnQIng® Innovex and Boston Scientific® LithoVue. Qualitative comparisons of these were made.
Results
After su-fURS usage, significant damage was observed, especially on the distal tip. Deflection was not compromised. Reusable fURS did not sustain any damage after their use.
Conclusions
fURS are delicate equipment, especially if they are of single use. The considerable damage sustained by single use scopes could mean that reuse of these instruments is dangerous and should be avoided.
Keywords: disposable equipment, ureteroscopes, ureteroscopy, urolithiasis
INTRODUCTION
During the last decades, the evolution of endourologic equipment has allowed a considerable growth in the number of available treatments for urinary calculi and urothelial tumors. With the appearance of the first flexible ureteroscopes (fURS), the development of Holmium laser and evermore finer quartz fibers that could be introduced through the working channel, endourologic treatment of stones became widespread across the world.
With time, smaller equipment has been developed, with far better resolution, deflection and resistance compared to previous instruments, significantly improving their performance. However, the increased cost of acquisition and maintenance, summed to their frailness under repeated use and sterilization, were important limitations for the technique application, since only some centers could afford the technology.
In view of the above, cautious manipulation of fURS is of the utmost importance. Many tips and tricks for handling these instruments and to extend their lifespan have been reported in literature [1, 2]. One of the most relevant points is to maintain a prudent distance between the distal tip of the fURS and the laser fiber at the moment of firing (1/4 of the screen) [3].
Over time, two things allowed the diffusion of the fURS use: first, the prices decreased, and second, the appearance of the single use flexible ureteroscope (su-fURS).
Numerous publications have demonstrated that su-fURS are comparable to reusable fURS on image quality, maneuverability, deflection and flow, and they have the advantage of being lighter, not needing maintenance nor sterilization [4, 5, 6].
However, there is no evidence on the economic superiority of su-fURS over reusable fURS.
The cost-effectiveness of a flexible ureteroscopy program is dependent of several aspects [7–11]. In a cost-benefit analysis, the acquisition cost would be the most important factor to determine whether purchasing a su-fURS is convenient or not [12]. Also, environmental concerns have been raised with respect to the use of disposable material [13].
It can be argued that many su-fURS appear to maintain their deflection and visibility after surgery, similarly to their reusable counterparts. The following question arises: can a single use scope be reused?
It is an undocumented reality that reuse of single use ureteroscopes occurs in undeveloped countries, mainly to cut costs on an economically adverse setting. The development of limited use time systems such as with Pusen 3022 and LithoVue scopes seem to be a response from the industry to fight this improper use.
The reuse of this material raises concerns over patient safety, more specifically, over the effectiveness of the removal of biological material from a damaged ureteroscope tip.
The objective of this study was to evaluate macroscopic changes on su-fURS and reusable fURS post-retrograde intrarenal surgery (RIRS) for comparison.
MATERIAL AND METHODS
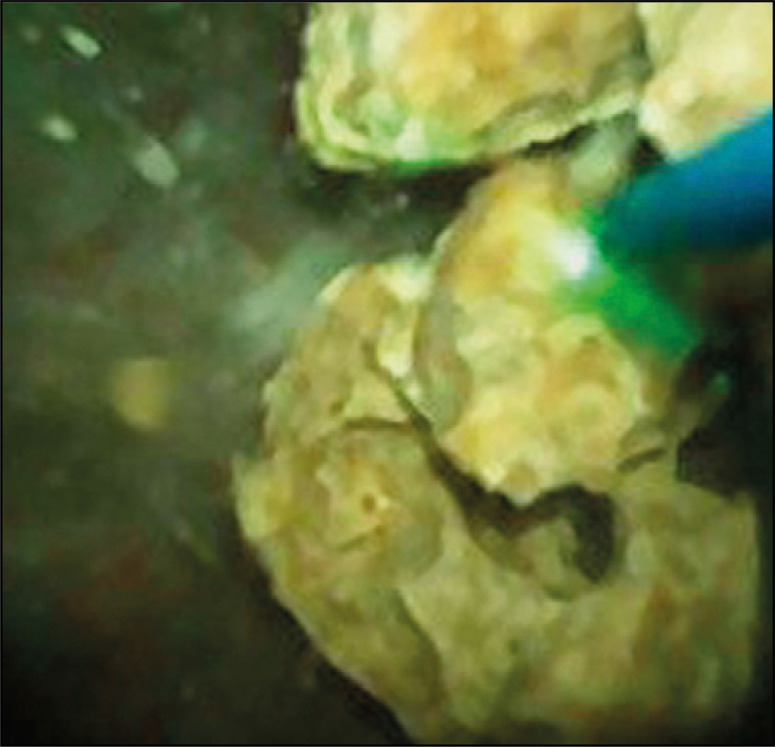
During the period between July and December 2019 we performed 33 RIRS, both with reusable and single use fURS. Of those, 23 patients had lower pole renal calculi between 10-15 mm that required Holmium laser lithotripsy, which were included in the analysis. The procedures were carried in two tertiary centers by two experienced urologists, and in all the cases there was a ureteral exploration with a semirigid ureteroscope done previously to discard the presence of ureteral calculi and to assist in dilation. We used access sheaths from 10–12 Fr or 12–14 Fr depending on the ureteroscope being used. There were no stone relocations, always treating the calculi on the original lower calix. A minimal distance was kept between the laser fiber and the tip of the scope, using as reference at least 1/4 of the image (Figure 1) [3]. All the calculi were treated with a 30 W holmium laser on pulverization settings (0.5 J, 15–20 Hz and between 7.5–10 W), with a 200 nm reusable fiber. For irrigation, normal saline was used, and an assistant could provide extra flow by manually pressing the serum drop. Procedures lasted between 45 to 90 minutes since the start of the anesthesia. There were no intraoperative complications, and all patients presented a favorable outcome.
Figure 1.
Pusen 3022 with the laser fiber placed on the safety zone.
Digital photographs of the distal tips of the instruments were obtained before and after surgery with the Canon® EOS Rebel XS camera, with a 35 mm macro Canon® EFS lens.
The fURS models used were the optic fiber Storz® Flex X2, and the digital Storz® Flex XC. Both had 25 previous procedures each. The su-fURS models used were: Pusen® 3022, OTU® Wiscope, AnQIng® Innovex and Boston Scientific® LithoVue. Technical specifications are shown in Table 1.
Table 1.
Technical specifications of the examined ureteroscopes
| Pusen Uscope 3022 | WiScope® | Innovex | LithoVue™ | Flex X2 | Flex XC | |
|---|---|---|---|---|---|---|
| Manufacturer | Clairon Medical | OTU® | AnQIng | Boston Scientific | Storz | Storz |
| Type of use | Single use | Single use | Single use | Single use | Reusable | Reusable |
| Image system | Digital | Digital | Digital | Digital | Optic fiber | Digital |
| Length [mm] | 650 | 670 | n/a | 680 | 670 | 700 |
| Working channel | 1 | 1 | 1 | 1 | 1 | 1 |
| Working channel diameter [Fr] | 3.6 | 3.6 | 3.6 | 3.6 | 3.6 | 3.6 |
| Distal tip diameter [Fr] | 9 | 7.4 | 9.3 | 7.7 | 7.5 | 8.5 |
| Deflection | Bidirectional 270°/270° | Bidirectional 275°/275° | Bidirectional 275°/275° | Bidirectional 270°/270° | Bidirectional 270°/270° | Bidirectional 270°/270° |
| Usage time | 4 hours | Unlimited | Unlimited | 4 hours | Unlimited | Unlimited |
| Resolution | n/a | 160K | 160K | 62K | n/a | 1920 x 1080 |
| Field Depth [mm] | 3–50 | 2–50 | 3–50 | 2–50 | – | – |
We qualitatively compared the pre- and post-use photographs between every model to determine how much damage each one sustained.
RESULTS
From the 23 total cases, 2 cases for every scope model were included. Thus, a total of 12 ureteroscopes were photographed, analyzed and compared. Photographs are shown in Figures 2–7.
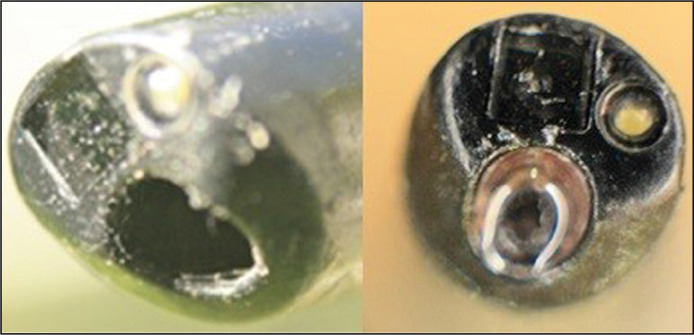
Figure 2.
Storz Flex X2.
Figure 7.
LithoVue before and after use.
Figure 3.
Storz Flex XC.
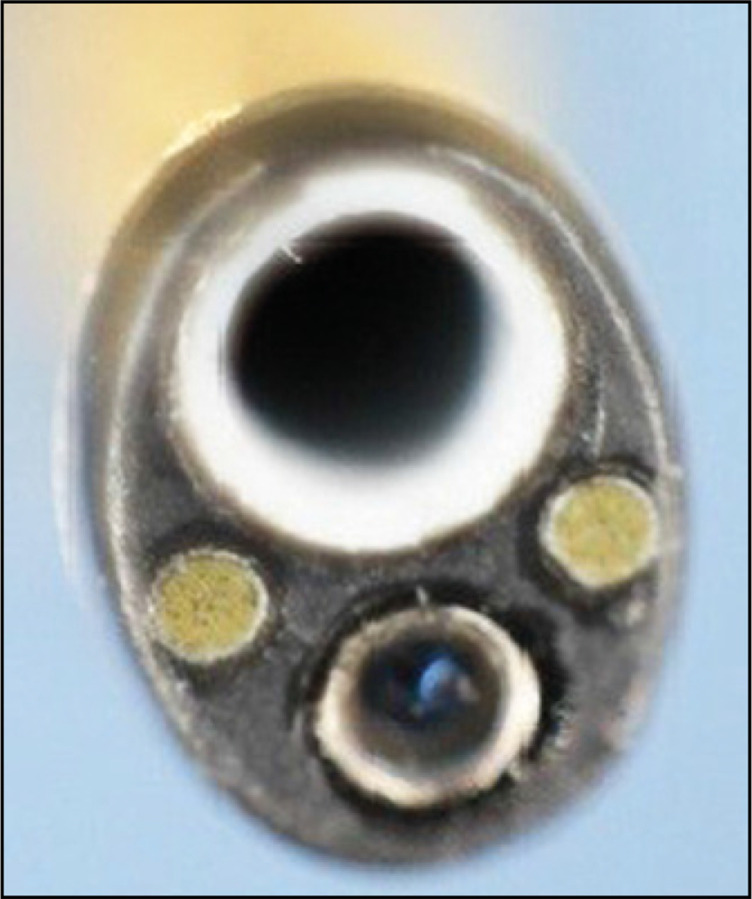
Figure 4.
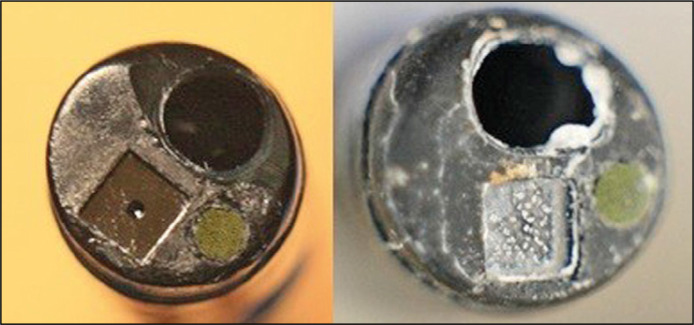
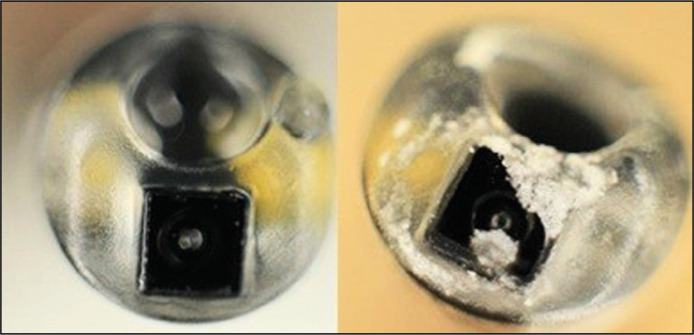
Pusen 3022 before and after use.
Figure 5.
OTU Wiscope before and after use.
Figure 6.
AnQIng Innovex before and after use.
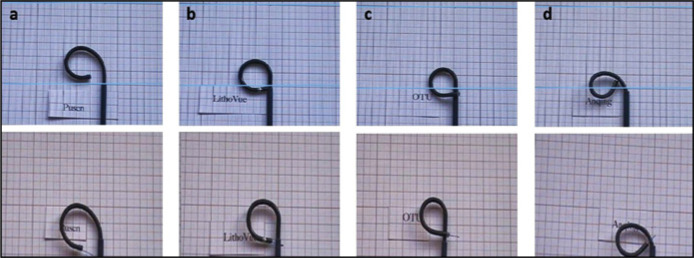
When comparison of the pictures was made, all the su-fURS presented more damage on the distal tip versus reusable fURS. The su-fURS that presented less damage where the LithoVue and the AnQIng Innovex. There was no alteration of the deflection mechanism after usage in any model. Figure 8 shows how deflection is compromised when the working channel is occupied with a 270 nm fiber. The reusable fURS showed no signs of damage.
Figure 8.
Deflection of different su-fURS. On the first row the working channel is free, on the second row a 270 nm fiber. has been placed. A. Pusen; B. LithoVue; C. OTU; D. Anqing.
DISCUSSION
In spite of the technological progress that has been achieved with fURS, they are still a delicate and expensive tool with an important risk of being damaged during their operation and sterilization/storage process. Sung et al. demonstrated that the most common place of damage is the working channel (52%), followed by the body of the instrument (27%), deflection mechanism (15%) and optical components (8%). The laser fiber was the main cause of burn and perforation damage. Ninety percent of the time the damage was found on the last 3–4 mm of the working channel [14].
In this study, we found no evident changes on the distal tip of reusable fURS. Both of the reusable fURS examined were previously used in 25 procedures each. This was not the case with single use equipment, since important damage was noted.
The fragility of the reusable fURS and the risk of damaging them are inconveniences of great importance. In response to this, the market developed su-fURS, trying to overcome these problems. However, the cost/benefit superiority of single use versus reusable scopes hasn’t been proved. The most certain indication of the su-fURS appears to be cases where the risk of damage of the instrument is high (long estimated operative time, inferior calix calculi with acute infundibulopelvic angle).
In the present study, we performed a qualitative assessment of the images of the distal tip of reusable and single use fURS before and after use. As expected, su-fURS presented important damage, even when appropriate safety measures where respected. Meanwhile, no changes were noted on the reusable fURS. This outcome disparity is accentuated, since all the cases implied a high stress setting for the instruments (medium sized lower pole stones).
It is also worth noting that both the deflection mechanism and the image quality of the su-fURS were intact at the end of the procedures, although, this last characteristic was not objectively measured.
As it was stated above, the reuse of single use ureteroscopes is an undocumented phenomenon that occurs in undeveloped countries to cut costs. The apparent indemnity of the scope’s deflection system and image quality after it has been used has created the notion that the material is suitable for reuse. In our study we demonstrated that considerable damage to the distal tip should warn against this practice, as it could preclude appropriate sterilization.
Because of the observational and qualitative nature of this study, it has important limitations. Further research should determine how deflection and image quality is affected before and after surgery.
CONCLUSIONS
Flexible ureteroscopes are delicate equipment, especially if they are of single use. We observed that single use scopes sustain significant damage compared to reusable ones, especially on the distal tip. The reuse of these instruments is an undocumented real-life issue that takes place in undeveloped countries. As shown in our findings, this questionable practice could compromise adequate sterilization and thus patient safety.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
References
- 1.Legemate JD, Kamphuis GM, et al. Durability of Flexible Ureteroscopes : A Prospective Evaluation of Longevity , the Factors that Affect it , and Damage Mechanisms. Eur Urol Focus. 2018:1–7. doi: 10.1016/j.euf.2018.03.001. [DOI] [PubMed] [Google Scholar]
- 2.Doizi S, Traxer O. Flexible ureteroscopy: technique, tips and tricks. Urolithiasis. 2018;46:47–58. doi: 10.1007/s00240-017-1030-x. [DOI] [PubMed] [Google Scholar]
- 3.Talso M, Emiliani E, Haddad M, et al. Laser Fiber and Flexible Uretero renoscopy: The ‘Safety Distance’ Concept. J Endourol. 2016;30:1269–1274. doi: 10.1089/end.2016.0209. [DOI] [PubMed] [Google Scholar]
- 4.Ventimiglia E, Somani BK, Traxer O. Flexible ureteroscopy: reuse? Or is single use the new direction? Curr Opin Urol. 2020;30:113–119. doi: 10.1097/MOU.0000000000000700. [DOI] [PubMed] [Google Scholar]
- 5.Deininger S, Haberstock L, Kruck S, et al. Single - use versus reusable ureterorenoscopes for retrograde intrarenal surgery (RIRS): systematic comparative analysis of physical and optical properties in three different devices. World J Urol. 2018;36:2059–2063. doi: 10.1007/s00345-018-2365-9. [DOI] [PubMed] [Google Scholar]
- 6.Scotland KB, Chew BH, Chew BH. Single - use flexible ureteroscopes: How do they compare to reusable ureteroscopes? J Endourol. 2019;33:71–78. doi: 10.1089/end.2018.0785. [DOI] [PubMed] [Google Scholar]
- 7.Emiliani E, Traxer O. Single use and disposable flexible ureteroscopes. Curr Opin Urol. 2017;27:176–181. doi: 10.1097/MOU.0000000000000371. [DOI] [PubMed] [Google Scholar]
- 8.Martin CJ, Mcadams SB, Abdul-muhsin H, et al. The Economic Implications of a Reusable Flexible Digital Ureteroscope: A Cost- Benefit Analysis. J Urol. 2017;197(3Pt1):730–735. doi: 10.1016/j.juro.2016.09.085. [DOI] [PubMed] [Google Scholar]
- 9.Proietti S, Somani B, Sofer M, Pietropaolo A, Rosso M. The ‘Body mass index’ of flexible ureteroscopes. J Endourol. 2017;31:1090–1095. doi: 10.1089/end.2017.0438. [DOI] [PubMed] [Google Scholar]
- 10.Usawanchintachit M, Isaacson DS, Taguchi K, Tzou TD, His RS, Sherer BA, Stoller ML, Chi T. A. Prospective Case Control Study Comparing LithoVueTM, a Single-Use Flexible Disposable Ureteroscope, to Flexible Reusable Fiber-optic Ureteroscopes. J Endourol. 2017;31:468–475. doi: 10.1089/end.2017.0027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Marchini GS, Torricelli FC, Batagello CA, et al. A comprehensive literature-based equation to compare cost-effectiveness of a flexible ureteroscopy program with single-use versus reusable devices. Int Braz J Urol. 2019;45:658–670. doi: 10.1590/S1677-5538.IBJU.2018.0880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hennessey DB, Fojecki GL, Papa NP, Lawrentschuk N, Bolton D. Single-use disposable digital flexible ureteroscopes: an ex vivo assessment and cost analysis. BJU Int. 2018;121(Suppl 3):55–61. doi: 10.1111/bju.14235. [DOI] [PubMed] [Google Scholar]
- 13.Moore B, Proietti S, Giusti G, Eisner BH. Single - Use Ureteroscopes. Urol Clin NA. 2019;46:165–174. doi: 10.1016/j.ucl.2018.12.002. [DOI] [PubMed] [Google Scholar]
- 14.Sung JC, Springhart WP, Marguet CG, et al. Location and etiology of flexible and semirigid ureteroscope damage. Urology. 2005;66:958–963. doi: 10.1016/j.urology.2005.05.033. [DOI] [PubMed] [Google Scholar]