Abstract
Introduction
Male reproductive health is rapidly declining during the past decades and it is well known that scrotal temperature is linked to male infertility.
Material and methods
We performed a prospective data evaluation within a counterfactual analysis study design. Scrotal cooling was performed using Snowballs™ underwear, scrotal temperature was monitored using a wireless temperature sensor (SensorPush, Brooklyn, NY, 11215)
Results
Overall, scrotal skin temperatures were monitored for 1008 hours. Median scrotal skin temperature was 34.6°C (IQR 33.1 to 35.3) and 35.3°C (IQR 34.4 to 35.9) in the experimental (SnowWedge™) period and control period, respectively, which was significantly different (P <0.001).
Conclusions
Cyclic scrotal skin cooling using specialized underwear is feasible and efficacious without impairing the activities of daily living and reduces median scrotal skin temperature significantly by 0.7°C. Given the proven association of scrotal skin temperature and semen quality, cyclic scrotal skin cooling by a device such as Snowballs™ underwear may eventually increase semen quality and fertility.
Keywords: semen quality, fertility, cooling underwear
INTRODUCTION
Over the past decades, male reproductive health has rapidly declined with unequivocal signs of deteriorated sperm concentration and total sperm count [1]. Regarding this worrisome fact, its implications for further generations, and public healthcare systems, strategies to stop this trend are urgently needed.
Several modifiable risk factors for poor sperm morphology were identified [2], of which lifestyle and behavioral factors such as type of underwear, profession, and environmental temperature are directly linked to scrotal temperature. It is well known that elevated scrotal temperature is linked to male infertility [3]. The range of physiological scrotal skin temperature has been described between roughly 33°C and 35°C [3, 4]. Even a moderate temperature elevation of only 0.7°C has been shown to significantly decrease sperm counts and subsequently impact paternity rates [3]. Although some pathophysiological mechanisms still might remain unclear, the association between varicocele and semen quality is well known and impaired scrotal temperature regulation is sought to play a fundamental role [5]. A study using scrotal temperature monitoring proved the temperature reductive effect of varicocelectomy leading to almost normal postoperative values [5].
Regarding feasible and practicable strategies to improve semen quality, a different approach seems promising. Taking the same line, Zorgniotti et al. [6] and Jung et al. [7] described a pragmatic approach of cyclic intermittent scrotal cooling leading to significantly increased semen quality [6, 7]. However, the lack of suitability for daily use of testicular cooling devices based on external air pumps and fluid reservoirs limited a widespread utilization [6]. Recently, the idea of scrotal cooling to improve fertility was taken up to investigate improvement of semen quality in mice after cisplatin-induced spermatogenesis toxicity and confirmed a significant positive effect [8]. In 2013, a novel cooling underwear (Snowballs™, Under Ice LLC, Richmond, VA, USA) was introduced to markets. To set a foundation for further studies on the impact of scrotal cooling on sperm quality and subsequent paternal rates, we aimed to prospectively investigate the cooling effect of Snowballs™ underwear on scrotal skin in a proof-of-concept study.
MATERIAL AND METHODS
Three urologists (VZ, AP, and PB, 32–33 years old) made themselves available for the prospective data evaluation within a counterfactual analysis study design. The participants signed an informed consent and were aware that the data was going to be published. Scrotal cooling was performed using Snowballs™ underwear (http://www.snowballsunderwear.com). An ergonomic cooling device (SnowWedge™) contained a freezable gel (sodium carboxymethyl cellulose) and was stored for five hours in the -20°C freezer prior to application. Scrotal temperature was documented using a wireless temperature sensor (SensorPush, Brooklyn, NY, USA). The sensor was centrally placed on the scrotum and data were continuously received on a smart phone using the appropriate software application (http://www.sensorpush.com/apps), resulting in one data log per testing minute. The three participants were instructed to wear the underwear with the sensor for one week without cooling and subsequently for one week using the SnowWedge™ device. The SnowWedge™ was changed every 12 h (7 am and 7 pm). Over the study period, the participants worked on a regular base at a hospital. There were no restrictions regarding the other clothes worn during the data acquisition.
In descriptive analyses, the three subjects’ documented scrotal skin temperatures were cumulated and their distribution was tested for normality by the Shapiro-Wilk test. Consecutively, medians and interquartile ranges (IQRs) of scrotal skin temperature were reported for cooling and corresponding non-cooling strata and compared by the Wilcoxon matched-pairs signed-ranks test, given that scrotal skin temperatures were not normally distributed.
RESULTS
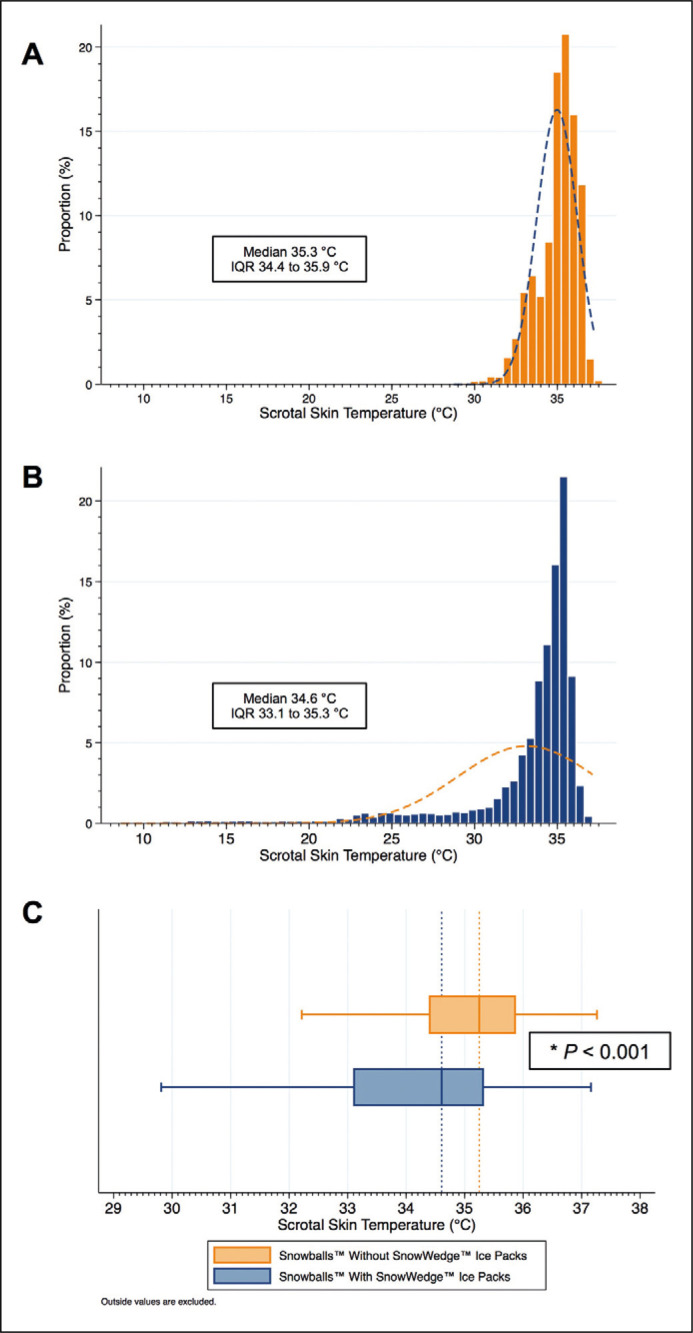
Overall, scrotal skin temperatures were monitored for 1008 hours corresponding to 30,240 documented temperature values in each of the experimental (cooling) and control (non-cooling) period. Median scrotal skin temperature was 34.6°C (IQR 33.1 to 35.3) and 35.3°C (IQR 34.4 to 35.9) in the experimental (SnowWedge™) period and control period, respectively, which was significantly different (p <0.001, Figure 1). All three study subjects did not report any problems nor discomfort regarding the cooling device and during the study period there were no adverse events reported.
Figure 1.
Histograms of the distribution of scrotal skin temperature A in the control period without the SnowWedge™ cooling device and B in the experimental period with the SnowWedge™ cooling device. The box-and-whisker diagram in C depicts the counterfactual analysis comparing the distribution of scrotal skin temperature between the study periods.
DISCUSSION
Although it has been shown that cyclic intermittent scrotal cooling leads to significantly increased semen quality [6], the ideal cooling period in such a setting remains unclear. Our setting with a cooling period twice daily confirmed the feasibility and efficacy of scrotal skin cooling and already lead to an overall temperature decrease of 0.7°C. A more intensive cooling rhythm might lead to even better temperature reduction without impairing the activities of daily living. In summary, we were able to confirm the feasibility and efficacy of cyclic scrotal skin cooling using specialized underwear. Given the proven association of scrotal skin temperature and semen quality, cyclic scrotal skin cooling by a device such as Snowballs™ underwear may eventually increase semen quality and fertility. This hypothesis should be tested by a clinical trial including different settings for cooling periods
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
References
- 1.Levine H, Jorgensen N, Martino-Andrade A, et al. Temporal trends in sperm count: a systematic review and meta-regression analysis. Hum Reprod Update. 2017;23:646–659. doi: 10.1093/humupd/dmx022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pacey AA, Povey AC, Clyma JA, et al. Modifiable and non-modifiable risk factors for poor sperm morphology. Hum Reprod. 2014;29:1629–1636. doi: 10.1093/humrep/deu116. [DOI] [PubMed] [Google Scholar]
- 3.Hjollund NH, Bonde JP, Jensen TK, Olsen J. Diurnal scrotal skin temperature and semen quality. The Danish First Pregnancy Planner Study Team. Int J Androl. 2000;23:309–318. doi: 10.1046/j.1365-2605.2000.00245.x. [DOI] [PubMed] [Google Scholar]
- 4.Nikolopoulos I, Osman W, Haoula Z, Jayaprakasan K, Atiomo W. Scrotal cooling and its benefits to male fertility: a systematic review. J Obstet Gynaecol. 2013;33:338–342. doi: 10.3109/01443615.2012.758088. [DOI] [PubMed] [Google Scholar]
- 5.Wright EJ, Young GP, Goldstein M. Reduction in testicular temperature after varicocelectomy in infertile men. Urology. 1997;50:257–259. doi: 10.1016/s0090-4295(97)00191-x. [DOI] [PubMed] [Google Scholar]
- 6.Zorgniotti AW, Sealfon AI, Toth A. Chronic scrotal hypothermia as a treatment for poor semen quality. Lancet. 1980;1:904–906. doi: 10.1016/s0140-6736(80)90839-9. [DOI] [PubMed] [Google Scholar]
- 7.Jung A, Schill WB, Schuppe HC. Improvement of semen quality by nocturnal scrotal cooling in oligozoospermic men with a history of testicular maldescent. Int J Androl. 2005;28:93–98. doi: 10.1111/j.1365-2605.2004.00517.x. [DOI] [PubMed] [Google Scholar]
- 8.Aminsharifi A, Hekmati P, Noorafshan A, et al. Scrotal Cooling to Protect Against Cisplatin-induced Spermatogenesis Toxicity: Preliminary Outcome of an Experimental Controlled Trial. Urology. 2016;91:90–98. doi: 10.1016/j.urology.2015.12.062. [DOI] [PubMed] [Google Scholar]