Abstract
Introduction
Racial disparities in COVID-19 morbidity and mortality have been well-documented. However, there may also be racial disparities in COVID-19 vaccination rates which, if present, would further exacerbate the existing disparities. No previously published articles have identified and quantified potential racial disparities in vaccination throughout the USA at any geography lower than the national level.
Methods
Using data compiled from state health departments, we calculated racial disparities in COVID-19 vaccination for the Black and Hispanic populations compared to the White population in each state. We explored the relationship between a state-level index of structural racism and the observed differences in the racial disparities in COVID-19 vaccination across states for both the Black and Hispanic populations by conducting linear regression analyses.
Results
Racial disparities in COVID-19 vaccination were present for both the Black and Hispanic populations in the overwhelming majority of states. There were vast differences between the states in the magnitude of the racial disparity in race-specific vaccination rates. These differences were largely explained by differences in the level of structural racism in each state. The relationship between structural racism and the racial disparities in vaccination was not entirely explained by racial differences in vaccine hesitancy or political affiliation.
Conclusions
There are marked racial disparities in COVID-19 vaccination throughout the USA, and structural racism is strongly associated with the magnitude of these disparities. Efforts to reduce these disparities must address not only individual behavior but must also confront the structural barriers that are inhibiting equitable vaccine distribution.
Keywords: COVID-19 (coronavirus disease 2019), COVID-19 vaccination, Health disparities, Structural racism, African American populations, Hispanic/Latinx populations, Vaccination
Introduction
It is no secret that there exist blatant disparities in COVID-19 infection, hospitalization, and mortality between Black and Hispanic compared to White populations within the USA [1]. Previous studies have shown strong associations of these disparities with numerous forms of structural racism, such as economic inequality, residential segregation, and disproportionate incarceration [2, 3]. However, racial disparities may not end with the initial morbidity and mortality from COVID-19, and several articles in this Journal have asked whether or not there are also disparities in COVID-19 vaccination rates between Black and Hispanic compared to White populations in the USA, which would further exacerbate the existing racial disparities [4–6]. If so, it is important not only to identify the existence of these disparities, but to also determine their magnitude, how they differ across states, and if they share an association with structural racism. Our research seeks to explore these questions by quantifying racial disparities in COVID-19 vaccination rates between non-Hispanic Black and Hispanic compared to non-Hispanic-White populations at the state level, examining the differences between the magnitude of those disparities across states, and investigating the relationship between structural racism and any observed racial disparities in vaccination rates.
Despite the importance of potential racial disparities in COVID-19 vaccination, we are not aware of any published articles that have actually quantified these disparities throughout the USA at any geography lower than the national level. For example, the Centers for Disease Control and Prevention (CDC) has reported on racial disparities in COVID-19 vaccination nationally [7] and in one state (North Carolina) [8], but not at the state or county level. There is one published article that measures the association between components of structural racism and the Black-White COVID-19 vaccination disparity across US counties, although it does not provide the level of disparity for each county [9]. The study measures the impact of economic stability, education access and quality, health care access and quality, neighborhood and built environment, and social and community context on racial disparities in COVID-19 vaccination rates at the county level. While the data, this study produces, is extremely important, it is also important to analyze these disparities at the state level because the vaccine rollout and the priorities for vaccination are mainly at the discretion of the state powers. There are a number of web sites that provide race-specific vaccination rates at the state level [10–12], but because they are not published in the peer-reviewed literature, it is not clear how widely this information has been disseminated. In addition, these web sites do not provide any analysis of potential reasons for the observed differences in racial disparities across states. In short, we believe this is the first published paper to quantify race-based disparities in COVID-19 vaccination rates at the state level and to examine potential explanations for the observed differences in the magnitude of the observed disparities across states.
There are conceptual reasons to believe that the Black and Hispanic populations may be subject to disparities in COVID-19 vaccination. Laurencin et al. have pointed to vaccine hesitancy in the Black community—deriving from vaccine misconceptions, the spread of misinformation, and mistrust—that may prevent individuals from being willing to get vaccinated [4]. A survey investigating vaccine hesitancy reported that Black participants had a higher general medical mistrust than White and White-Hispanic participants, but there were no significant differences for Black-Hispanic participants [13]. Many factors influence the high vaccine hesitancy in these groups, some of them being past experiences of discrimination, political ideology, and sociodemographic factors [13]. The same survey found that experiences of everyday discrimination, structural discrimination, and healthcare discrimination were significantly and positively correlated with vaccine hesitancy [13]. In addition, political beliefs seem to affect the likelihood of getting vaccinated as one study found that Republicans tend to be more hesitant to become vaccinated than people of other political affiliations [14]. Lastly, findings of a survey demonstrated that sociodemographic factors have a correlation with vaccine hesitancy, particularly lower levels of education, which are significantly associated with higher degrees of medical mistrust [15].
Beyond individual-level factors, there is reason to believe that institutional and systemic factors—structural racism—may also contribute to racial inequity in COVID-19 vaccine distribution. This could include factors such as increased distance to vaccination sites as a result of residential segregation, lack of health insurance to provide easy access at medical settings, difficulty taking time off work due to much higher economic instability, transportation costs, difficulty obtaining child care, and fear of deportation if citizenship status is ascertained.
In this paper, we explore the relationship between structural racism and the Black-White disparity and Hispanic-White disparity in COVID-19 vaccination rates across 45 US states. We use racially stratified vaccination data, as recent as May 19, 2021, from the APM Research Lab, Kaiser Family Foundation, and Bloomberg, allowing for a detailed exploration of vaccination disparities within the USA for both the non-Hispanic Black and Hispanic populations compared to the non-Hispanic-White population. We work to “name racism” and “figure out the levers on which we can intervene,” as called for by many, like by Dr. Camara Jones in a recent webinar that explored vaccine hesitancy in the Black community [4]. Quantifying the magnitude of multiple components of structural racism and their association with vaccination disparities may allow us to pinpoint the most effective means to intervene and create effective change.
Methods
Design Overview
Using data compiled from state health departments by the Kaiser Family Foundation [10], American Public Media [11], and Bloomberg [12], we calculated racial disparities in COVID-19 vaccination for the Black and Hispanic populations compared to the White population in each state. The racial disparity was defined as the difference in the proportion of the Black (or Hispanic) population vaccinated compared to that of the White population in that state. Some states categorized White- or Black-Hispanic people as White or Black, while others separated these populations into Hispanic-White and Hispanic Black. The denominator in each case was the relevant population from the 2019 American Community Survey. Using a previously developed state-level index of structural racism, we explored the relationship between this state racism index and the observed differences in the racial disparities in COVID-19 vaccination across states by conducting linear regression analyses.
Measures and Data Sources
Outcome Variable
The outcome variable was the Black-White or Hispanic-White racial disparity in the proportion of the population that received at least one COVID-19 vaccination as of May 17, 2021, defined as the difference (in percentage points) between the proportion of Black or Hispanic people vaccinated and the proportion of White people vaccinated in a given state. It is important to note that in some cases, the disparity being measured is between non-Hispanic Black people and non-Hispanic-White people, while in other cases, the disparity being measured is between Black people of all ethnicities and White people of all ethnicities. It is also important to remember that race is a social and political construct without biological significance; thus, there are inherent complexities in attempting to measure these constructs.
COVID-19 vaccination data are collected by each state health department. Although these data are reported to the Centers for Disease Control and Prevention (CDC) and some are made available on the CDC web site, race-specific vaccination rates by state are not. However, three health/media organizations have conducted and made available their own analyses of the state department web sites in order to provide weekly estimates of state-specific, race-specific COVID-19 vaccination rates. We obtained data from each of these sites covering vaccination rates as of May 17, 2021.
Because the racial disparity was defined as the proportion of vaccinated Black or Hispanic residents minus the proportion of vaccinated White residents, a negative number indicates the presence of a racial disparity, meaning that the proportion of Black or Hispanic people who are vaccinated is less than the proportion of White people who are vaccinated. A positive number would indicate the absence of any disparity, meaning that the proportion of vaccinated Black or Hispanic people is greater than the proportion of vaccinated White people. The more negative the number, the greater the disparity that is present.
Kaiser Family Foundation (KFF)
KFF continuously analyzes data from publicly available state health department web sites to estimate race-specific vaccination rates in 43 states [10]. States that do not report percentages of racial groups that received at least one dose of a vaccine are excluded, as are states that do not present the data in a format allowing for the calculation of the percentage of each racial group that were vaccinated. Because some states report data by race and ethnicity alone, while others report by race/ethnicity, KFF matches the population data to reflect the states’ racial/ethnic characterization in order to calculate the correct vaccination rate. Population data are obtained from the 2019 American Community Survey, 1-year estimate. Because of separate reporting, vaccination rates for Pennsylvania exclude Philadelphia.
American Public Media (APM)
The APM Research Lab conducts a variety of demographic analyses and, as part of that work, has been periodically tracking race-specific rates of COVID-19 vaccination in the states based on its own monitoring and analysis of state health department web sites [11]. Its most recent data update covers the period through May 17, 2021. As with KFF, the denominators used for vaccination rate calculations are from the U.S. Census Bureau’s 2019 American Community Survey, 1-year estimate, and are matched to each state’s method of data collection for race and ethnicity. Also, as with KFF, states are omitted if they do not allow calculation of the proportion of each racial group that has received at least one dose of a vaccine. The reported data cover at total of 33 states. APM considered reporting from both Philadelphia and the rest of the state so its estimates for Pennsylvania do include the entire state.
Bloomberg
The Bloomberg Vaccine Tracker analyzes state web sites to report race-specific vaccination rates for 45 states, claiming to account for 93.8% of all COVID-19 doses administered in the USA [12]. Its methods are similar to those of KFF and APM, except that it uses the 5-year American Community Survey estimates to derive the population denominators for each racial group. As with KFF, Bloomberg’s estimates for Pennsylvania exclude Philadelphia.
Using the combined data from these sources, we were able to generate race-specific COVID-19 vaccination rates for the White population in 45 states, the Black population in 45 states, and the Hispanic population in 42 states. The 45-state sample excluded Arkansas, Montana, New Hampshire, New Jersey, and Wyoming. It accounted for 313 million people, or 95.4% of the population and for 40.0 million Black people, or 95.9% of the Black population. The 42-state sample additionally excluded Hawaii, Kentucky, and West Virginia. It accounted for 305 million people, or 93.0% of the population and for 57.8 million Hispanic people, or 95.7% of the Hispanic population.
Validity Checks and Sensitivity Analyses for Outcome Variable
Vaccination rate estimates from the KFF and Bloomberg sources were the most highly correlated, with correlation coefficients ranging from 0.88 to 0.92 (Table 1). Because of variability in the estimates, we conducted a sensitivity analysis to test the dependence of our findings on the data source. We conducted four different analyses: one for each data source and one for the average of the estimates across all three data sources. Associations were deemed valid only if they were present in all four analyses. The main findings presented are based on taking an average of the estimates from the three data sources.
Table 1.
Correlation matrix for three data sources for race-specific vaccination rates
| Data sources | White vaccination rates | Black vaccination rates | Hispanic vaccination rates |
|---|---|---|---|
| KFF-APM | 0.95 | 0.79 | 0.69 |
| KFF-Bloomberg | 0.92 | 0.90 | 0.88 |
| APM-Bloomberg | 0.86 | 0.74 | 0.72 |
Main Predictor Variable
The main predictor variable was the state racism index, which we originally developed in previous research exploring the relationship between structural racism and racial disparities in fatal police shootings [16, 17]. In that work, we found that the state racism index was significantly related to differences in the Black-White racial disparity in fatal police shooting rates of unarmed victims across states. More recently, we showed that the state racism index is a robust predictor of the magnitude of the Black-White disparity in COVID-19 mortality rates across states [2].
The state racism index measures structural racism at the state level across five dimensions: (1) economic indicators; (2) employment indicators; (3) incarceration; (4) educational attainment; and (5) residential segregation. The economic dimension consists of (a) the ratio of the proportion of Black people in rental housing to that of White people in rental housing; (b) the ratio of the Black poverty rate to the White poverty rate; and (c) the ratio of median household income for the White population to median household income for the Black population. The employment dimension consists of (a) the ratio of the Black unemployment rate to the White unemployment rate and (b) the ratio of the Black labor non-participation rate to the White labor non-participation rate. The incarceration dimension is the ratio of the incarceration rate of Black people to the incarceration rate of White people. The educational attainment dimension is the ratio of the proportion of Black people without a college education to the proportion of White people without a college education. The residential segregation dimension consists of (a) the index of dissimilarity, a measure of the differential distribution of two population groups and (b) the isolation index, a measure of the spatial isolation of one racial group from another. For each measure, the values across the 50 states are converted into a scale from 0 to 100. The components are then averaged to obtain a dimension score for each state. The scores for the five dimensions are averaged to yield the final state racism index. We constructed the state racism index using data from the 2019 American Community Survey (education, economics, employment), 2019 national prisoner data from the Bureau of Justice Statistics (incarceration rates) [18], and the 2010 Decennial Census (segregation measures). The index of dissimilarity and the isolation index were calculated for the non-Hispanic-White and non-Hispanic Black populations using the Census block as the lower-level geographic unit. Details are shown in Table 2.
Table 2.
Definitions, data sources, and methods for calculation of the state racism index, 2019
| Dimension | Measure | Description | Data source |
|---|---|---|---|
| Exposure risk | Dissimilarity Index | D = 1/2 SUM [blackpct—Whitepct] * 100, where blackpct is the proportion of the state’s Black population living in each block and Whitepct is the proportion of the state’s White population living in that block. Values are on a scale from 0 to100 with 100 being the most spacially segregated by race. It represents the percentage of Black people who would have to move in order to achieve an equal distribution of White and Black people across all blocks within a state | US Decennial Census, 2010 |
| Isolation Index | I = 100—(SUM((blackpct)*(proportionblack)) * 100), where blackpct is the proportion of the state’s Black population living in each block and proportion black is the proportion of people in that block who are Black. Values are on a scale from 0 to 100 with higher values representing higher levels of segregation. It can be interpreted as the probability a Black person does not share a block area with a White person or as the extent to which Black members of a block are exposed only to one another | US Decennial Census, 2010 | |
| Segregation Index | Average of Dissimilarity Index and Segregation Index | ||
| Incarceration | Incarceration Index | Ratio of Black incarceration rate to White incarceration rate for each state. Converted to 0–100 scale | US Bureau of Justice Statistics, National Prisoner Statistics |
| Education | Education Index | Ratio of proportion of Black adults ages 25 + without a college degree to the proportion of White adults ages 25 + without a college degree for each state. Converted to 0–100 scale | 2019 American Community Survey |
| Economic | Poverty Index | Ratio of proportion of Black people living under the poverty level to the proportion of White people living under the poverty level for each state. Converted to 0–100 scale | 2019 American Community Survey |
| Income Index | Ratio of White median annual household income to Black median annual household income for each state. Converted to 0–100 scale | 2019 American Community Survey | |
| Rental Index | Ratio of proportion of Black people in rental housing to proportion of White people in rental housing for each state. Converted to 0–100 scale | 2019 American Community Survey | |
| Economic Index | Average of Poverty Index, Income Index, and Rental Index | ||
| Employment | Labor Force Participation Index | Ratio of proportion of Black people not participating in the labor force to proportion of White people not participating in the labor force for each state. Converted to 0–100 scale | 2019 American Community Survey |
| Unemployment Index | Ratio of proportion of unemployment rate among Black people to the unemployment rate among White people for each state. Converted to 0–100 scale | 2019 American Community Survey | |
| Employment Index | Average of Labor Force Participation Index and Unemployment Index | ||
| Overall State Structural Racism Index | Racism Index | Average of Segregation Index, Incarceration Index, Education Index, Economic Index, and Employment Index |
Hispanic state racism index is calculated identically, except Hispanic population is substituted for non-Hispanic Black population
We constructed a Hispanic state racism index using the identical procedure as above, except substituting the Hispanic population for the non-Hispanic Black population in each of the measures. We are not aware of any previous use of the Hispanic state racism index to examine the relationship between structural racism and adverse health outcomes among the Hispanic population.
Potential Mediating Variables
Differences Between Racial Groups in COVID-19 Vaccine Hesitancy
One might hypothesize that racial differences in vaccine hesitancy could explain observed racial disparities in actual vaccination rates. We used data from the U.S. Bureau of the Census Household Pulse Survey, a periodic national survey conducted by the Census Bureau during the COVID-19 pandemic beginning on April 23, 2020, to measure race-specific vaccine hesitancy [19]. The first pulse survey to measure COVID-19 vaccine hesitancy was the week 22 survey, which was conducted between January 6 and January 18, 2021. We used these data to calculate, for each state, the ratio of the proportions of the non-Hispanic Black population to non-Hispanic-White population expressing vaccine hesitancy and the same ratio for the Hispanic compared to the White, non-Hispanic population. Respondents were considered vaccine hesitant if they reported that they would “definitely not” or “probably not” get a vaccine or if they refused to answer the question about whether they were vaccinated. Our rationale for including refusal to answer the question as being vaccine hesitant is that we suspect refusal to answer the question reflects some level of hostility toward the issue which is itself likely a manifestation of vaccine hesitancy. As we operationalize it, then, vaccine hesitancy is the failure to indicate that one is definitely or probably going to get the vaccine. The adjustment for vaccine hesitancy was computed by dividing the percentage of the Black population that was vaccine hesitant by the percentage of the White population that was vaccine hesitant. We acknowledge that there are complexities in measuring the construct of “vaccine hesitancy” and that in some cases, a person classified as “vaccine hesitant” may actually be “vaccine deliberate,” or waiting for a longer period of time before seeking vaccination.
Support for President Donald Trump in 2020 Election
For each state, we included the proportion of presidential voters who cast ballots for President Trump [20]. One might hypothesize that states with stronger support for President Trump might have greater vaccine hesitancy and that this support might be differential with respect to race. In fact, an analysis by the Kaiser Family Foundation documented that Trump voters are significantly less likely to be vaccinated for COVID-19 than those that voted for Biden [21].
Data Analysis
We began by calculating the difference (in percentage points) between the proportion of Black or Hispanic people vaccinated and the proportion of White people vaccinated in each state. Next, we conducted linear regression analyses to examine the relationship between the state racism index and differences in the magnitude of the Black-White and Hispanic-White disparities in COVID-19 vaccination rates across states. Finally, we explored whether including the mediating variables in the same linear regression altered the relationship between the state racism index and any observed racial disparities in COVID-19 vaccination. To ease interpretation of the regression coefficients, we standardized the independent variables so that the coefficient represents the change in the magnitude of the vaccination rate difference for each one standard deviation increase in the relevant structural racism index.
Results
Descriptive Results
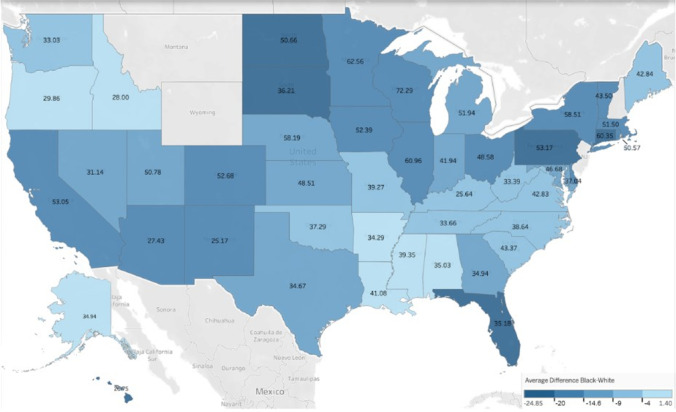
Of the 50 states analyzed, we were able to collect reliable Black-to-White vaccination rate difference data from 45 states (Table 3). There was a widespread Black racial disparity in vaccination rates in 43 states (96% of reporting states), in which the proportion of Black people who were vaccinated minus the proportion of White people who were vaccinated was negative. Only two states did not have a Black racial disparity: Alaska (+ 1.4%) and Oregon (+ 0.1%).The five states with the highest Black racial disparity were Pennsylvania (− 24.9%), South Dakota (− 24.0%), North Dakota (− 22.9%), Connecticut (− 21.3%), and Florida (− 20.5%). The five states with the lowest Black racial disparity (other than Alaska and Oregon) were Idaho (− 1.8%), Mississippi (− 2.1%), Louisiana (− 2.5%), Alabama (− 3.0%), and Maine (− 4.9%).
Table 3.
Racial disparities in COVID-19 vaccination rates as of May 17, 2021 and state racism indices
| State | Black-White disparity | Hispanic-White disparity | ||
|---|---|---|---|---|
| Black vaccination rate–White vaccination rate | Black state racism index | Hispanic vaccination rate–White vaccination rate | Hispanic state racism index | |
| Alabama | − 3.0 | 35.0 | − 8.7 | 43.1 |
| Alaska | + 1.4 | 34.9 | + 20.5 | 26.2 |
| Arizona | − 14.8 | 27.4 | − 20.0 | 42.4 |
| California | − 16.8 | 53.1 | − 18.6 | 50.8 |
| Colorado | − 16.4 | 52.7 | − 29.8 | 55.4 |
| Connecticut | − 21.3 | 60.3 | − 18.2 | 74.7 |
| Delaware | − 14.9 | 37.0 | − 14.0 | 42.5 |
| Florida | − 20.5 | 35.2 | − 10.9 | 31.3 |
| Georgia | − 9.5 | 34.9 | − 13.6 | 33.4 |
| Hawaii | − 20.4 | 26.7 | 29.2 | |
| Idaho | − 1.8 | 28.0 | − 9.0 | 35.0 |
| Illinois | − 14.9 | 61.0 | − 10.6 | 45.2 |
| Indiana | − 13.4 | 41.9 | − 13.0 | 34.7 |
| Iowa | − 18.6 | 52.4 | − 11.2 | 42.7 |
| Kansas | − 10.6 | 48.5 | − 6.8 | 42.5 |
| Kentucky | − 8.5 | 25.6 | 22.0 | |
| Louisiana | − 2.5 | 41.1 | − 4.7 | 33.3 |
| Maine | − 4.9 | 42.8 | − 3.3 | 38.5 |
| Maryland | − 12.6 | 46.7 | − 15.1 | 35.0 |
| Massachusetts | − 16.2 | 51.5 | − 20.9 | 74.1 |
| Michigan | − 11.5 | 51.9 | − 10.9 | 34.4 |
| Minnesota | − 17.6 | 62.6 | − 17.1 | 48.9 |
| Mississippi | − 2.1 | 39.4 | − 7.1 | 38.2 |
| Missouri | − 8.9 | 39.3 | − 4.2 | 28.9 |
| Nebraska | − 12.8 | 58.2 | − 12.2 | 52.1 |
| Nevada | − 12.0 | 31.1 | − 6.0 | 29.2 |
| New Mexico | − 14.8 | 25.2 | − 14.6 | 46.3 |
| New York | − 17.0 | 58.5 | − 13.0 | 64.2 |
| North Carolina | − 6.8 | 38.6 | − 9.9 | 36.6 |
| North Dakota | − 22.9 | 50.7 | − 17.2 | 48.2 |
| Ohio | − 14.6 | 48.6 | − 10.7 | 41.5 |
| Oklahoma | − 8.6 | 37.3 | − 7.7 | 33.4 |
| Oregon | + 0.1 | 29.9 | − 16.2 | 29.0 |
| Pennsylvania | − 24.9 | 53.2 | − 19.9 | 61.3 |
| Rhode Island | − 17.5 | 50.6 | − 18.2 | 66.2 |
| South Carolina | − 7.4 | 43.4 | − 8.2 | 35.1 |
| South Dakota | − 24.0 | 36.2 | − 37.6 | 55.7 |
| Tennessee | − 6.6 | 33.7 | − 3.7 | 29.6 |
| Texas | − 12.0 | 34.7 | − 7.0 | 46.8 |
| Utah | − 12.3 | 50.8 | − 13.5 | 41.9 |
| Vermont | − 19.3 | 43.5 | + 7.3 | 33.6 |
| Virginia | − 6.6 | 42.8 | + 8.2 | 27.6 |
| Washington | − 7.2 | 33.0 | − 13.4 | 38.0 |
| West Virginia | − 6.8 | 33.4 | 18.1 | |
| Wisconsin | − 18.9 | 72.3 | − 15.0 | 50.9 |
Vaccination rates are the average of the three data sources: KFF, APM, and Bloomberg
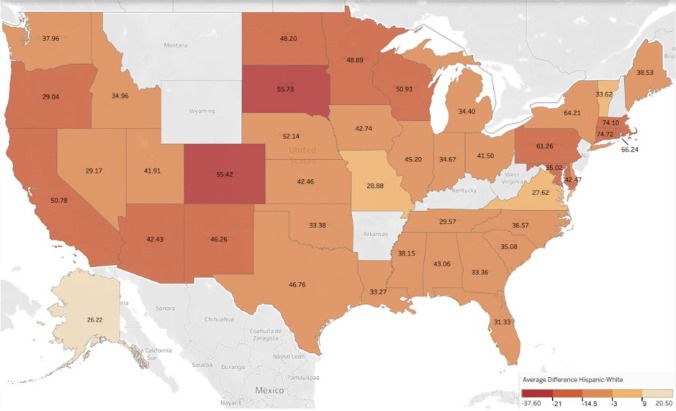
Similarly, of the 42 states with reliable data on the Hispanic-to-White vaccination rate difference, 38 states (90.5%) had negative differences in the proportion of Hispanic people who were vaccinated minus the proportion of White people who were vaccinated, indicating the presence of a Hispanic racial disparity (Table 3). Only four states (9.5%) did not have a Hispanic racial disparity. The five states with the highest Hispanic racial disparity were South Dakota (− 37.6%), Colorado (− 29.8%), Massachusetts (− 20.9%), Arizona (− 20.0%), and Pennsylvania (− 19.9%). The five states with the lowest Hispanic racial disparity were Alaska (+ 20.5%), Virginia (+ 8.2%), Vermont (+ 7.3%), Missouri (+ 4.2%), and Maine (− 3.3%).
We were able to calculate state racism indices for all 50 states for both Black and Hispanic populations. The Black state racism index ranged from a low of 23 in New Hampshire to a high of 72 in Wisconsin (Table 3). The five highest states were all located in the Midwest or Northeast: Wisconsin (72), New Jersey (66), Minnesota (63), Illinois (61), and Connecticut (60). The five states with the lowest Black state racism index were New Hampshire (23), New Mexico (25), Kentucky (26), Hawaii (27), and Arizona (27). The mean of the Black state racism index across the 50 states was 43, with a standard deviation of 12.
The Hispanic state racism index ranged from a low 18 in West Virginia to a high of 75 in Connecticut (Table 3). The five highest states were all located in the Northeast: Connecticut (75), Massachusetts (74), Rhode Island (66), New York (64), and Pennsylvania (61). Four of the five lowest states were located in the southern US: West Virginia (18), Kentucky (22), Arkansas (25), Alaska (26), and Virginia (28). The mean of the Hispanic state racism index across the 50 states was 41, with a standard deviation of 13.
Analytic Results
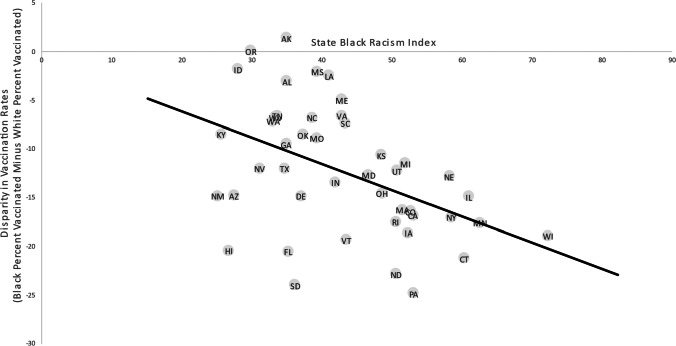
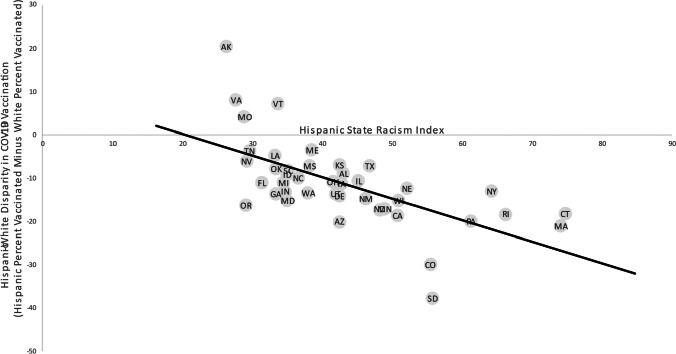
The relationship between the Black state racism index and the magnitude of the Black-White COVID-19 vaccination disparity is shown in heat map form (Fig. 1) and as a scatterplot (Fig. 3). Similarly, the relationship between the Hispanic state racism index and the magnitude of the Hispanic-White COVID-19 vaccination disparity is shown in heat map form (Fig. 2) and as a scatterplot (Fig. 4). In both cases, there is a clear positive relationship between these measures of structural racism and the magnitude of the racial disparity in COVID-19 vaccination at the state level (Figs. 1, 2, 3, and 4).
Fig. 1.
Heat map showing extent of Black-White disparity in COVID-19 vaccination rates in color gradations and Black state racism index for each state
Fig. 3.
Scatterplot of the magnitude of the Black-White COVID-19 vaccination disparity in each state in relation to the Black state racism index
Fig. 2.
Heat map showing extent of Hispanic-White disparity in COVID-19 vaccination rates in color gradations and Hispanic state racism index for each state
Fig. 4.
Scatterplot of the magnitude of the Hispanic-White COVID-19 vaccination disparity in each state in relation to the Hispanic state racism index
Based on the linear regression analyses, for each one standard deviation increase in the Black state racism index, the Black vaccination rate was 3.15 percentage point lower than the White vaccination rate (95% CI, − 1.27 to − 5.03) (Table 4). The overall racism index as well as two of its five components (the education and incarceration indices) had a statistically significant positive correlation with the magnitude of the Black-White vaccination rate disparity. For each one standard deviation increase in the education index, the Black vaccination rate was 3.55 percentage point lower than the White vaccination rate (95% CI, − 1.70 to − 5.40). The same increase in the incarceration index was associated with an increase in the difference between White and Black vaccination rates of 3.39 (95% CI, − 1.47 to − 5.30).
Table 4.
Relationship between structural racism and Black-White disparities in COVID-19 vaccination rates across 45 states
| Variable | Unadjusted coefficient (95% CI) | Adjusted coefficient (95% CI) |
|---|---|---|
| Black State Racism Index | − 3.15* (− 1.27 to − 5.03) | − 2.87* (− 0.84 to − 4.90) |
| Economic Index | − 1.96 (− 4.13 to + 0.22) | − 2.46* (− 4.63 to − 0.29) |
| Employment Index | − 0.81 (− 2.78 to + 1.16) | − 1.47 (− 3.42 to + 0.48) |
| Education Index | − 3.55* (− 1.70 to − 5.40) | − 2.73 (− 5.45 to + 0.00) |
| Incarceration Index | − 3.39* (− 1.47 to − 5.30) | − 2.98* (− 0.82 to − 5.14) |
| Segregation Index | + 0.14 (− 1.93 to + 2.22) | + 0.04 (− 1.99 to + 2.07) |
*Indicates coefficient is significant at the p < 0.05 level. Significant findings are shown in bold type
The adjusted analyses control for racial disparities in vaccine hesitancy and for the political affiliation in each state. Regression coefficients represent the change in the absolute percentage point difference between the Black and White vaccination rates for each one standard deviation increase in the structural racism index shown
We also analyzed the data after adjusting for vaccine hesitancy in White compared to minority populations and for the percentage of Trump votes in the state. After adjustment, a one standard deviation increase in the racism index for Black people in a state was associated with a 2.87 percentage point (95% CI, − 0.84 to − 4.90) increase in the difference between the proportion of the Black population that was vaccinated compared to the percentage of the White population that was vaccinated in that state (Table 4). The overall racism index and two of its five component indices were statistically significantly related to the magnitude of the racial disparity in vaccination rates. A one standard deviation increase in the economic index was associated with an increase of 2.46 percentage point (95% CI, − 0.29 to − 4.63) in the difference between White and Black vaccination rates. A one standard deviation increase in the incarceration index was associated with an increase of 2.98 percentage point (95% CI, − 0.82 to − 5.14) in the difference between White and Black vaccination rates. The regression coefficient for the education index was no longer statistically significant.
In the Hispanic population, a one standard deviation increase in the racism index was associated with a 6.27 percentage point (95% CI, − 3.79 to − 8.75) increase in the difference between the White and Hispanic vaccination rates (Table 5). In addition to the statistically significant positive correlation between the state Hispanic racism index and the difference between Hispanic and White vaccination rates, all five component indices were statistically significantly associated with a greater magnitude of the Hispanic-White vaccination rate disparity.
Table 5.
Relationship between structural racism and Hispanic-White disparities in COVID-19 vaccination rates across 45 states
| Variable | Unadjusted coefficient (95% CI) | Adjusted coefficient (95% CI) |
|---|---|---|
| Hispanic State Racism Index | − 6.27* (− 3.79 to − 8.75) | − 6.77* (− 3.89 to − 9.66) |
| Economic Index | − 3.27* (− 0.10 to − 6.44) | − 2.77 (− 6.26 to + 0.72) |
| Employment Index | − 4.58* (− 1.83 to − 7.33) | − 4.81* (− 1.68 to − 7.94) |
| Education Index | − 5.10* (− 2.53 to − 7.67) | − 5.08* (− 2.29 to − 7.86) |
| Incarceration Index | − 4.31* (− 1.62 to − 7.00) | − 4.15* (− 1.16 to − 7.13) |
| Segregation Index | − 4.82* (− 1.93 to − 7.71) | − 4.59* (− 1.60 to − 7.59) |
*Indicates coefficient is significant at the p < 0.05 level. Significant findings are shown in bold type
The adjusted analyses control for racial disparities in vaccine hesitancy and for the political affiliation in each state. Regression coefficients represent the change in the absolute percentage point difference between the Hispanic and White vaccination rates for each one standard deviation increase in the structural racism index shown
After adjustment, each one standard deviation increase in the state Hispanic racism index was associated with a 6.77 percentage point increase in the difference between White and Hispanic vaccination proportions (Table 5). Four of the five component indices (all except the economic index) were also significantly related to an increase in the difference between the White and Hispanic vaccination rates.
An increase in the Hispanic racism index had a larger effect on the difference between White and Hispanic vaccination rates than an increase in the Black racism index had on the difference between White and Hispanic vaccination rates (Tables 4 and 5).
The relationship between the Black racism index and the Black-White disparity in vaccination was unchanged no matter which of the three databases were relied upon (Table 6). In all three cases, a one standard deviation increase in the Black racism index was associated with an increase of between 2.64 and 3.39 percentage points in the difference between Black and White vaccination proportions.
Table 6.
Sensitivity analysis—relationship between structural racism and Black-White disparities in COVID-19 vaccination rates across 45 states based on three different databases
| Database | Unadjusted coefficient for Black State Racism Index (95% CI) |
|---|---|
| Average of all three | − 3.15* (− 1.27 to − 5.03) |
| Kaiser Family Foundation | − 3.39* (− 1.22 to − 5.56) |
| American Public Media | − 2.64* (− 0.63 to − 4.65) |
| Bloomberg | − 2.96* (− 0.95 to − 4.98) |
*Indicates coefficient is significant at the p < 0.05 level. Significant findings are shown in bold type
Regression coefficients represent the change in the absolute percentage point difference between the Black and White vaccination rates for each one standard deviation increase in the Black state racism index
The relationship between the Hispanic racism index and the Hispanic-White disparity in vaccination remained unchanged when relying upon the KFF or APM databases; however, the relationship was no longer statistically significant when using the Bloomberg data set (Table 7).
Table 7.
Sensitivity analysis—relationship between structural racism and Hispanic-White disparities in COVID-19 vaccination rates across 42 states based on three different databases
| Database | Unadjusted coefficient for Hispanic State Racism Index (95% CI) |
|---|---|
| Average of all three | − 6.27* (− 3.79 to − 8.75) |
| Kaiser Family Foundation | − 5.42* (− 3.06 to − 7.78) |
| American Public Media | − 5.30* (− 2.72 to − 7.87) |
| Bloomberg | − 2.13 (− 5.58 to + 1.32) |
*Indicates coefficient is significant at the p < 0.05 level. Significant findings are shown in bold type
Regression coefficients represent the change in the absolute percentage point difference between the Hispanic and White vaccination rates for each one standard deviation increase in the Hispanic state racism index
Discussion
To the best of our knowledge, this is the first published national study to quantify the level of the racial disparity in COVID-19 vaccination rates at the state level and to explore the relationship between structural racism and the differences in the magnitude of the observed racial disparities across states. We found that (1) racial disparities in COVID-19 vaccination were present for both the Black and Hispanic populations in the overwhelming majority of states; (2) there were vast differences between the states in the magnitude of the racial disparity in race-specific vaccination rates; (3) these differences between states were largely explained by differences in the level of structural racism in each state; and (4) the relationship between structural racism and the racial disparities in vaccination was not entirely explained by racial differences in vaccine hesitancy or political affiliation.
The first major implication of this paper is that we have documented the almost uniform presence of racial disparities in COVID-19 vaccination for both the Black and Hispanic populations. In some cases, the magnitude of the observed disparities is striking. For example, in Pennsylvania, there was a 25 percentage point difference between the proportions of Black people and White people who were vaccinated. In South Dakota, there was a 38 percentage point difference between the proportions of Hispanic people and White people who were vaccinated. These differences would be expected to exacerbate the existing racial disparities in COVID-19 morbidity and mortality as time goes on. Thus, our research predicts that the documented racial disparities in COVID-19 morbidity and mortality are likely to increase over time, not decrease.
An important finding of this research is that the states with the highest racism indices are concentrated in particular regions, mainly the Northeast and Midwest, while some of the states with the lowest indices are located in the South. Although some people perceive the South as being more racist, some of the most blatant forms of structural racism, such as redlining, housing exclusion, sundown towns, and mortgage discrimination were rampant in the Midwest and Northeast, areas that initially had fewer Black people and went to these extremes to maintain White hegemony.
One of the contributions of this paper is that it is the first to reveal the usefulness of the Hispanic state racism index by demonstrating that this index is strongly related to the level of the Hispanic-White disparity in COVID-19 vaccination across states. In fact, we found that all five dimensions of the racism index—economic, employment, incarceration, segregation, and education—were significantly related to differences in the Hispanic-White vaccination disparity; four of these remained significant even after controlling for vaccine hesitancy and political affiliation. The availability of this Hispanic racism index might lead to future research to explore whether it may also be associated with other health outcomes.
This paper documents that structural racism is strongly associated with differences in the magnitude of the observed racial disparities in COVID-19 vaccination for both the Black and Hispanic populations. The only other paper we are aware of that examined, this relationship did so at the county level and found that racial differences in median income were positively related to the Black-White disparity in vaccination rates [9].
Another important finding of this paper is that vaccine hesitancy does not appear to be the sole factor causing the observed racial disparities in COVID-19 vaccination. This finding is consistent with the study by Agarwal et al., which found that controlling for vaccine hesitancy did not explain county-level differences in the magnitude of the Black-White disparity in vaccination [9]. The problem appears to be more than just an individual-level one, but to involve a range of structural factors stemming from racist institutions and systems. For example, even if someone wants to be vaccinated, there may be structural barriers such as inability to take time off of work, inability to afford child care, lacking access to transportation, a lack of mass vaccination sites at locations that are publicly accessible, fear of interrogation about one’s immigration status, and even potential intimidation associated with the presence of law enforcement personnel at vaccination sites. Putting too much of an emphasis on vaccine hesitancy risks taking a victim-blaming perspective, when our findings suggest that the problem is more of a systemic one. Campaigns to reduce the racial disparity in vaccination should therefore focus not merely on trying to persuade people to get vaccinated, but on reducing the structural barriers that stand in the way. By continuing on the victim-blaming trajectory, we risk further exacerbating the previously documented disparities in COVID-19 morbidity and mortality, as more infectious and potentially dangerous variants (such as the Delta variant) pose even greater risks for unvaccinated people than may have been present during the early waves of the pandemic. As Stoler et al. recently concluded: “Health education programs focused on building medical trust may underperform if they do not address structural racism” [22], p.2]. Corbie-Smith went even further, suggesting that “vaccine hesitancy is a scapegoat for structural racism” [23].
Our results indicated that Alaska and Oregon were the only two states that did not report a disparity in COVID-19 vaccination between the non-Hispanic-White and Black populations. While it is beyond the scope of this paper to analyze the reasons for the achievement of racial equity in these two states on this measure, it is important to note the following. In Alaska, vaccine clinics were deliberately placed in underserved or disproportionately affected areas [24]. Specifically, Alaska used a CDC measure of social vulnerability—the Area Deprivation Index—to prioritize areas to preferentially target for vaccine distribution, which was done by partnering with federally qualified health centers and with other community-based organizations [24]. In Oregon, the state health department required all local jurisdictions to submit a plan detailing how they were going to eliminate racial/ethnic disparities in COVID-19 vaccination by August 31, 2021 [25]. Each local health department had to detail a plan to “close the specific vaccine equity gaps among specific racial and ethnic populations” [25]. In addition, both Alaska and Oregon have proportionately low Black and Hispanic populations.
Limitations
The most important limitation of this study is the absence of a uniform definition of race and ethnicity across the state health departments. Some of the states classified race alone and then separately classified ethnicity, while others classified race and ethnicity jointly. In the former case, what is being called the “White” population actually includes people who are also Hispanic. This is likely to reduce the observed disparities in vaccination rates between the Hispanic and White alone populations, since Hispanic people are being compared to a combination of Hispanic-White people and non-Hispanic-White people. Despite this limitation, we found that the regression coefficient for the state racism indices was similar when we stratified the analysis by the type of race/ethnicity classification used (i.e., conducting separate regressions for states with each type of classification system). For the Black-White disparity regressions, the regression coefficient for the state racism index remained significant at the p < 0.10 level for both models. For the Hispanic-White disparity regressions, the regression coefficients for the state racism index remained significant at the p < 0.05 level for both models. Therefore, we do not believe that the differences in race/ethnicity classification affect the validity of our conclusion that structural racism is associated with the magnitude of racial disparities in COVID-19 vaccination for both the Black and Hispanic populations.
A second limitation of the analysis is that there were missing data for five states for the Black-White disparity analysis and for eight states for the Hispanic-White disparity analysis. Therefore, our results cannot be generalized to all 50 states. However, the 45-state sample accounted for 95% of the population, and the 42-state sample accounted for 93% of the population.
A third limitation is that the vaccine hesitancy data are based on the U.S. Census Bureau’s Household Pulse Survey, which has an extremely low response rate in the range of 2 to 10% [26]. Moreover, one reason for non-response could be apprehension about reporting vaccine hesitancy to a government agency; thus, these estimates could be biased toward underestimating the actual degree of vaccine hesitancy.
Fourth, our structural racism index did not include any measure of disparities in health care access (such as differences in health insurance coverage). Thus, it may be missing an important aspect of structural racism that could be directly related to vaccination. Although the vaccine is free, people without trusted health care practitioners may be less likely to get vaccinated, despite the fact that it does not require health insurance.
Finally, two of the three data sources reported data for Pennsylvania that excluded the city of Philadelphia. Since Philadelphia is the largest city in the state and contains the largest Black and Hispanic populations of any city in the state, this could substantially skew the racial disparity estimates. Therefore, all data reported on Pennsylvania in this paper should be treated cautiously.
Conclusion
Despite these limitations, this paper demonstrates that there are marked racial disparities in COVID-19 vaccination throughout the USA and that structural racism is strongly associated with the magnitude of these disparities. Efforts to reduce these disparities must address not only individual behavior (e.g., “vaccine hesitancy”) but must confront the structural barriers, such as racial inequities in economic status, employment, education, incarceration, and segregation—resulting from decades of systemic racism—that are inhibiting equitable vaccine distribution.
Acknowledgements
Tableau Public was used in the creation of the map shown in Figs. 1 and 2. The use of Tableau Public is governed by the terms of service outlined at https://www.tableau.com/tos.
Abbreviations
- ACS
American Community Survey
- APM
American Public Media
- CDC
Centers for Disease Control and Prevention
- CI
Confidence interval
- COVID-19
Coronavirus disease 2019
- KFF
Kaiser Family Foundation
Data Availability and Material
The database produced in this research project is available from the corresponding author.
Code Availability
Not applicable.
Declarations
Conflict of Interest
The authors declare no competing interests.
Research Involving Human Participants and/or Animals
This is a secondary analysis of publicly available data obtained, analyzed, and reported at an aggregated state level. No human subject or identification data is collected or analyzed in this study.
Informed Consent
No human subject was involved in this study.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Centers for Disease Control and Prevention (CDC). Risk for COVID-19 infection, hospitalization, and death by race/ethnicity. Atlanta, GA: CDC; 2021. [Available from: https://www.cdc.gov/coronavirus/2019-ncov/covid-data/investigations-discovery/hospitalization-death-by-race-ethnicity.html]. Accessed 9 Aug 2021.
- 2.Siegel M, Critchfield-Jain I, Boykin M, Owens A. Actual racial/ethnic disparities in COVID-19 mortality for the non-Hispanic Black compared to non-Hispanic White population in 35 US states and their association with structural racism. J Racial Ethn Health Disparities. 2021, published April 27 [Available from: https://link.springer.com/content/pdf/10.1007/s40615-021-01028-1.pdf]. Accessed 13 Jul 2021. [DOI] [PMC free article] [PubMed]
- 3.Siegel M, Critchfield-Jain I, Boykin M, Owens A, Nunn T, Muratore R. Actual racial/ethnic disparities in COVID-19 mortality for the non-Hispanic Black compared to non-Hispanic White population in 353 US counties and their association with structural racism. J Racial Ethn Health Disparities (in press). [DOI] [PMC free article] [PubMed]
- 4.Laurencin CT, Valantine H, Yancy C, Phyllis Jones C, Bright C. The COVID-19 vaccine and the Black community: addressing the justified questions. J Racial Ethn Health Disparities. 2021, published June 18 [Available from: https://link.springer.com/article/10.1007/s40615-021-01082-9]. Accessed 9 Aug 2021. [DOI] [PMC free article] [PubMed]
- 5.Johnson JH, Jr, Bonds JM, Parnell AM, Bright CM. Coronavirus vaccine distribution: moving to a race conscious approach for a racially disparate problem. J Racial Ethn Health Disparities. 2021;8(4):799–802. doi: 10.1007/s40615-021-01051-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Laurencin CT. Addressing justified vaccine hesitancy in the Black community. J Racial Ethn Health Disparities. 2021, published March 30 [Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8009077/pdf/40615_2021_Article_1025.pdf]. Accessed 9 Aug 2021. [DOI] [PMC free article] [PubMed]
- 7.Painter EM, Ussery EN, Patel A, et al. Demographic characteristics of persons vaccinated during the first month of the COVID-19 vaccination program—United States, December- 14, 2020—January 14, 2021. MMWR Morb Mortal Wkly Rep. 2021;70(5):174–177. doi: 10.15585/mmwr.mm7005e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wong CA, Dowler S, Moore AF, et al. COVID-19 vaccine administration, by race and ethnicity—North Carolina, December 14, 2020—April 6, 2021. MMWR Morb Mortal Wkly Rep. 2021;70(28):991–996. doi: 10.15585/mmwr.mm7028a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Agarwal R, Dugas M, Ramaprasad J, Luo J, Li G, Gao G. Socioeconomic privilege and political ideology are associated with racial disparity in COVID-19 vaccination. Proc Natl Acad Sci U S A. 2021;118(33): e2107873118 [Available from: https://www.pnas.org/content/118/33/e2107873118.long]. Accessed 9 Aug 2021. [DOI] [PMC free article] [PubMed]
- 10.Kaiser Family Foundation (KFF). Latest data on COVID-19 vaccinations by race/ethnicity. San Francisco, CA: KFF; 2021 [Available from: https://www.kff.org/coronavirus-covid-19/issue-brief/latest-data-on-covid-19-vaccinations-race-ethnicity/]. Accessed 25 Jun 2021.
- 11.APM Research Lab. Inoculation nation: available COVID-19 vaccine data shows uneven access by race and ethnicity. St. Paul, MN: APM Research Lab; 2021 [Available from: https://www.apmresearchlab.org/covid/vaccines-by-race]. Accessed 25 Jun 2021.
- 12.Bloomberg. Maryland becomes fourth state to vaccinate 50% of Hispanic people: Covid-19 tracker. Bloomberg’s tracker shows which states are making the most week-by-week progress in closing their racial vaccination gaps. New York: Bloomberg; 2021 [Available from: https://www.bloomberg.com/graphics/covid-vaccine-tracker-global-distribution/us-vaccine-demographics.html]. Accessed 25 Jun 2021.
- 13.Smith AC, Woerner J, Perera R, Haeny AM, Cox JM. An investigation of associations between race, ethnicity, and past experiences of discrimination with medical mistrust and COVID-19 protective strategies. J Racial Ethn Health Disparities. 2021, published June 11 [Available from: https://link.springer.com/article/10.1007%2Fs40615-021-01080-x]. Accessed 9 Aug 2021. [DOI] [PMC free article] [PubMed]
- 14.Fridman A, Gershon R, Gneezy A. COVID-19 and vaccine hesitancy: a longitudinal study. PLoS ONE. 2021;16(4):e0250123 [Available from: 10.1371/journal.pone.0250123]. Accessed 9 Aug 2021. [DOI] [PMC free article] [PubMed]
- 15.Willis DE, Andersen JA, Bryant-Moore K, Selig JP, Long CR, Felix HC, Curran GM, McElfish PA. COVID-19 vaccine hesitancy: race/ethnicity, trust, and fear. Clin Transl Sci. 2021, published July 2 [Available from: 10.1111/cts.13077]. Accessed 9 Aug 2021. [DOI] [PMC free article] [PubMed]
- 16.Mesic A, Franklin L, Cansever A, Potter F, Sharma A, Knopov A, Siegel M. The relationship between structural racism and Black-White disparities in fatal police shootings at the state level. J Natl Med Assoc. 2018;110(2):106–116. doi: 10.1016/j.jnma.2017.12.002. [DOI] [PubMed] [Google Scholar]
- 17.Siegel M. Racial disparities in fatal police shootings: an empirical analysis informed by critical race theory. Boston Univ Law Rev. 2020;100:1069–1092. [Google Scholar]
- 18.Bureau of Justice Statistics. Prisoners in 2019. Washington, DC: U.S. Department of Justice; 2020. [Available from: https://www.bjs.gov/index.cfm?ty=pbdetail&iid=7106]. Accessed 30 Nov 2020.
- 19.United States Census Bureau. Household Pulse Survey Data Tables [Available from: https://www.census.gov/programs-surveys/household-pulse-survey/data.html]. Accessed 6 Jul 2021.
- 20.Politico. Election results by state [Available from: https://www.politico.com/2020-election/results/president/]. Accessed 6 Jul 2021.
- 21.Kates J, Tolbert J, Orgera K. The red/blue divide in COVID-19 vaccination rates. San Francisco, CA: Kaiser Family Foundation (KFF); September 14, 2021 [Available from: https://www.kff.org/policy-watch/the-red-blue-divide-in-covid-19-vaccination-rates/]. Accessed 14 Oct 2021.
- 22.Stoler J, Enders AM, Klofstad CA, Uscinski JE. The limits of medical trust in mitigating COVID-19 vaccine hesitancy among Black Americans. J Gen Intern Med. 2021, published 21 May [Available from: https://www.doi.org/10.1007/s11606-021-06743-3]. Accessed 18 Aug 2021. [DOI] [PMC free article] [PubMed]
- 23.Corbie-Smith G. Vaccine hesitancy is a scapegoat for structural racism. JAMA Health Forum. 2021;2(3):e210434 [Available from: https://jamanetwork.com/journals/jama-health-forum/fullarticle/2778073]. Accessed 14 Oct 2021. [DOI] [PubMed]
- 24.Ndugga N, Artiga S, Pham O. How are states addressing racial equity in COVID-19 vaccination efforts? San Francisco, CA: Kaiser Family Foundation (KFF); March 10, 2021 [Available from: https://www.kff.org/racial-equity-and-health-policy/issue-brief/how-are-states-addressing-racial-equity-in-covid-19-vaccine-efforts/]. Accessed 14 Oct 2021.
- 25.Oregon Health Authority. Equity Plan Submission Guidance May 2020; Updated 8/4/2021. Salem, OR: Oregon Health Authority; August 4, 2021 [Available from: https://www.oregon.gov/oha/covid19/EquityPlan/Equity-Plan-Submission-Guidance.pdf]. Accessed 14 Oct 2021.
- 26.U.S. Bureau of the Census. Household pulse survey nonresponse bias analysis. Tables B1-B2: response rates based on sampling geography [Available from: https://www2.census.gov/programs-surveys/demo/technical-documentation/hhp/TablesB1-B2_resp_rates_based_samp_geog-all-weeks.xlsx]. Accessed 12 Aug 2021.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The database produced in this research project is available from the corresponding author.
Not applicable.