Abstract
Objective:
Determining the prevalence of Tarlov cysts in low back pain patients.
Methods and materials:
The picture archiving & communication system (PACS) & hospital information system (HIS) of a corporate hospital were retrospectively analyzed to determine the percentage of Tarlov cysts among patients undergoing spinal MRI for back pain over 3 years (January 2017 to December 2019).
Results:
384 patients had undergone spinal MRI for back pain over the study period, and 25 of them (6.51%) had Tarlov cysts. Vast majority (15 cases) showed cysts located at S2/S3 level, and few were found at S1/S2 and other levels. Single cysts were found in most (=18) of the cases, while 7 cases of multiple / bilateral cysts were found. Cyst dimensions were higher in craniocaudal than anteroposterior or transverse directions. In case of multiple cysts, one or two cysts were noted as dominant, having higher dimensions than the others. The study data revealed no gender or age predilection.
Conclusions:
We conclude that including the entire sacrum with a T2 sagittal sequence in all MRI for low back pain can increase detection of Tarlov cysts, and thereby provide more data for further analysis.
Advances in knowledge:
We propose the concept of one “dominant” cyst when there are multiple Tarlov cysts. We recommend that diameter or size of Tarlov cysts be specified to their craniocaudal dimension. We also suggest reporting points for contextual structured reporting, viz. presence or absence of bony scalloping, neural foraminal narrowing, nerve root compression or extraforaminal extension.
Introduction
Tarlov cysts, more accurately termed as perineural root sleeve cysts, are defined as extradural, CSF-filled dilatations within the nerve root sheath, enclosed between endoneurium & perineurium, most often abutting or surrounding the junction of the posterior nerve root and the dorsal root ganglion, but having no connection with the perineural subarachnoid space.1–4 They are classified as type-II under Nabor’s criteria for meningeal cysts.5
Two words have been attached to Tarlov cysts for decades—rare and asymptomatic. Quantitatively, the prevalence of Tarlov cysts has been documented as <5% in most scientific literature.2,6–8
Although spinal imaging took a big leap in the 1980’s with the advent of the 1.5 T MRI, little use of the new technology was made thereafter to revise our older understanding of perineural cysts, which was knowingly limited due to technology. It is a matter of discomfort, therefore, that research on Tarlov cysts only exist as scattered case reports7 and very few epidemiological and case–control studies,9 till today. The picture is just as frustrating in Asia, too.
An alarming outcome of ignoring Tarlov cysts was noted by Murphy et al in their paper “Tarlov cysts: An overlooked clinical problem”, where they stated that many patients with overlooked/ignored Tarlov cysts have undergone disc surgery and even spinal fusion, followed by being classed as “failed back” when their symptoms persisted after the surgery.9
Other than that, Tarlov cysts have also been proven to be associated with serious quality of life issues like infertility, retrograde ejaculation and other sexual dysfunctions.10,11 They are also known as an important cause of spontaneous intracranial hypotension (SIH), in case the cyst ruptures.12
Furthermore, more than 10 case reports have identified “giant” Tarlov cysts, arbitrarily defined as those that are larger than 3 cm.13 However, some of these papers have reported cysts as large as 10 cm14 and several >5 cm.13 It has been noted that such large cysts protrude through neural foramina producing nerve root compression and can sometimes mimic pelvic or adnexal masses.13,15,16
All included, these very few studies—however small-scale, accompanied by continuous steady flow of case reports17—however scattered & infrequent—do clearly raise voice that it is time to change our perception on this entity.
Authors of these recent studies have differed with previous literature and determined that the prevalence of Tarlov cysts actually ranges between 5 and 9%.3,4 It also becomes apparent from some of these papers2,4,17 that particular symptoms preferentially indicate towards the presence of Tarlov cysts, such as coccydynia, perineal pain, paresthesia around anal region as well as altered bowel or bladder control.17 Some studies also suggest sacral radiculopathies, sciatica pain, lower limb weakness & paresthesia and even sexual dysfunctions to be associated with Tarlov cysts.2
Although most of these studies state the proportion of symptomatic lesions as between 1 and 2%,2,4 there are other papers which suggest that Tarlov cysts may be symptomatic in up to 25% of cases.7,17–19
In addition to symptoms and clinical significance, it has been noted that about 5% of Tarlov cysts may extend into the pelvic cavity through neural foramina, thus mimicking pelvic or adnexal mass.13,20
All known data indicate that Tarlov cysts need no specific treatment unless they are directly responsible for symptoms. However, no specific treatment protocol or approach has so far been agreed upon.21,22 An important cause of such uncertainty & vagueness is the scanty data available on which to found a solid protocol.19
The specific objectives of the present study were to determine the prevalence of incidentally discovered Tarlov cysts among patients presenting with back pain in Sylhet Division of Bangladesh, and to determine/identify potential factors that contributed to their incidental discovery. We have also been able to formulate suggestions for MRI sequences in low back pain patients so as to not miss or overlook Tarlov cysts. We also propose measurement methods and criteria for structured reporting when Tarlov cysts are identified on MRI. Conducted in a small corner of South-East Asia, it is hoped that this article will raise awareness and encourage more investigators to probe further into different aspects of spinal cysts and in different regions.
Methods and materials
This was a retrospective observational study carried out on all the spinal MRI stored in the PACS of Al Haramain Hospital Pvt Ltd (Sylhet, Bangladesh), over the first 3 years of its operation, from its inception on January 1, 2017 upto December 31, 2019. All the spinal MRI done for back pain were included in the study (n = 384). Patients who had history or complaints other than back pain (e.g. spinal neoplasm, infection etc) were excluded. Follow-up scans of the same patient at the same spinal segment done at different times were also excluded to avoid data duplication.
All the MRI were done with a 3.0 T equipment (Ingenia; Philips Medical Systems; Netherlands) following standard spinal imaging protocols as appropriate at different levels (cervical, thoracic, lumbar, sacral). The stored data sets contained T1 & T2 sagittal sections spanning the full width of vertebral column including paravertebral muscles, T1 & T2 axial images taken at disc, suprapedicle & infrapedicle levels, PROSET coronal images spanning from pre-vertebral plane upto tip of spinous process and a screening MRI of the whole spine (T2 sagittal, from C1-Co4).
The images were viewed using RadiAnt PACS-DICOM Viewer (Medixant; Poland) on medical-grade monitors (EliteDisplay E242; Hewlett-Packard; USA) with necessary adjustment of windowing, magnification & contrast along with maximum & minimum intensity projections (MIP, MinIP) as required. All the MRI were evaluated and reported by the Principal Investigator over the study period.
Tarlov cysts were identified as well-defined thin-walled sacs containing homogeneous CSF intensity content, often accompanied by scalloping of the bony outline of the spinal canal. Each cyst was measured in three dimensions (anteroposterior x craniocaudal x transverse) using RadiAnt Viewer’s “length” tool and an average diameter was calculated.
The number, measured & average diameters (in mm) of all the detected cysts were recorded in relation with their location (cervical, thoracic, lumbar, sacral), position (canal, foramen or both), side (right or left), vertebral level as well as patient’s age, gender, height, weight and presenting complaint. Presenting complaints were derived from the attending physician’s notes, as recorded in the hospital information system (HIS).
No personal identity data (name, address, ethnicity, religion) was retrieved or analyzed for the study. Only demographic & clinical data were used, e.g. age, gender, body weight, presenting complaint.
Ethical & technical aspects of the study were approved by the Dept of Medical Services, Al Haramain Hospital Pvt Ltd.
Results
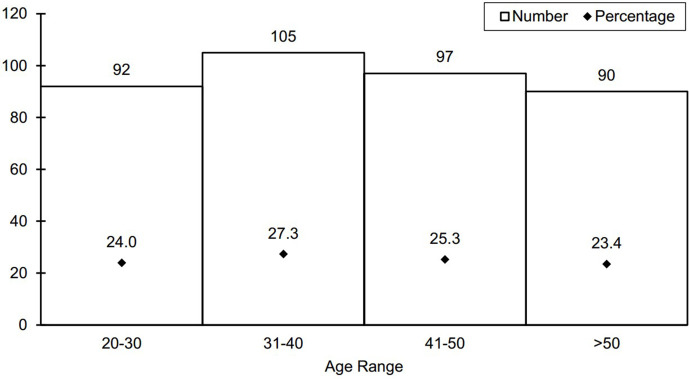
The study sample comprised a fairly equal proportion of females (202, 52.6%) and males (182, 47.4%) of all adult age groups (Figure 1). Mean age and BMI of the male patients who were advised spinal MRI for back pain was slightly higher (47.4 years; 23.15 kg/m2) than the females (39.98 years; 23.02 kg/m2).
Figure 1.
Age distribution of study subjects
A total of 25 patients (6.51%) were diagnosed with Tarlov cysts during the study period. Among them, multiple/bilateral cysts were found in 7 cases (28% of positive cases) (Figure 2). Males & females of all adult age groups were almost equally affected (Table 1).
Figure 2.
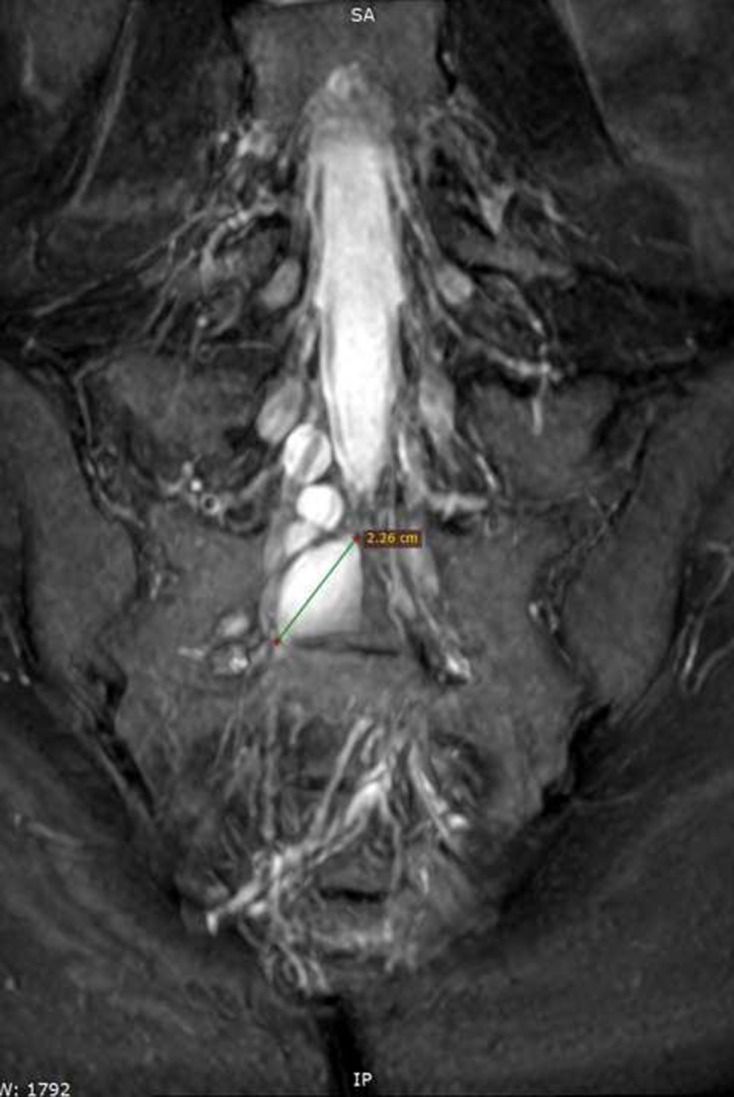
Coronal PROSET MRI at sacrum. Multiple bilateral cysts of variable sizes at L4, L5 & S1 levels. Dominant cyst on right side at S1/S2 level (measured between line marked with +--+).
Table 1.
Age & gender distribution of detected Tarlov cysts
| Age groups | TOTALS (by Gender) |
% Prevalence | ||||
|---|---|---|---|---|---|---|
| 20–30 | 31–40 | 41–50 | >50 | |||
| Male | 2 | 4 | 3 | 2 | 11 | 6.04 |
| Female | 3 | 3 | 4 | 4 | 14 | 6.93 |
| TOTALS (by age) |
5 | 7 | 7 | 6 | 25 | 6.51 |
Vast majority of the cysts were seen at S2/S3 level (15 cases, 60%), while few were seen at L5/S1 & S1/S2 levels (Figure 2). During the study period, only one cyst was discovered in the cervical region (Figure 3), and another in the thoracic region (Table 2)(Figure 4).
Figure 3.
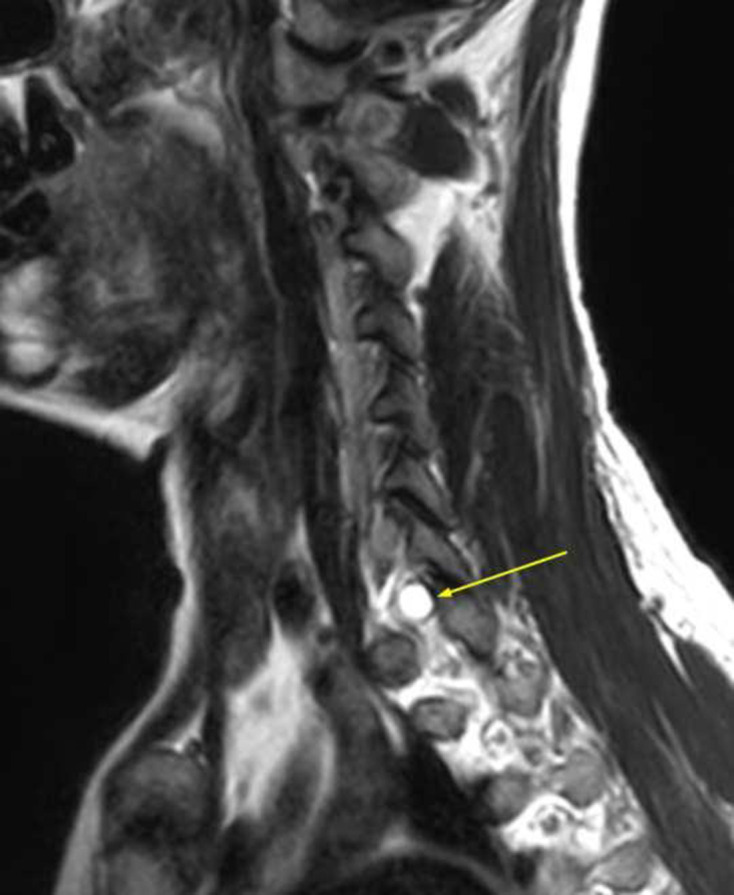
Sagittal T2 image. Well-defined cyst (arrow) at C7/D1 level.
Table 2.
Number & percentage of Tarlov cysts according to vertebral levels
| S2/S3 | S1/S2 | Lumbar | Thoracic | Cervical | TOTAL | |
|---|---|---|---|---|---|---|
| Single | 12 | 3 | 1 | 1 | 1 | 18 |
| Multiple | 3 | 2 | 2 | 0 | 0 | 7 |
| TOTAL | 15 | 5 | 3 | 1 | 1 | 25 |
| % | 60 | 20 | 12 | 4 | 4 |
Figure 4.
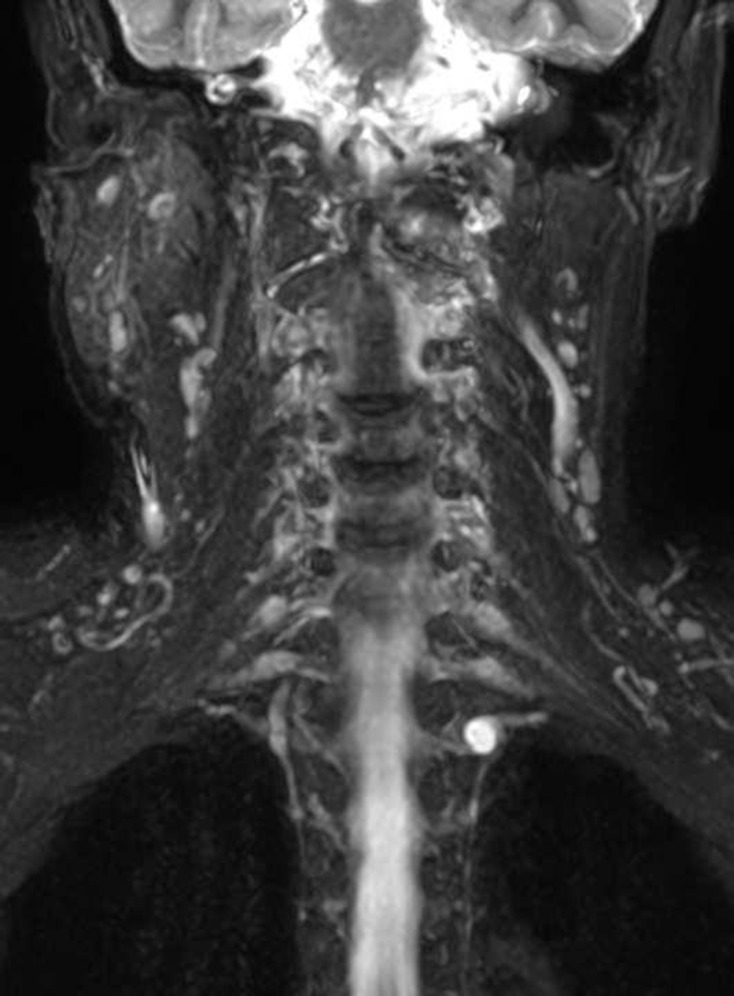
Coronal STIR image with MIP. Well-defined cyst on left side at D1/D2 level. MIP, maximum intensity projection; STIR, short-tau inversion recovery.
Cyst diameters were prominently higher in craniocaudal dimension than anteroposterior or transverse diameters, and represented the maximum dimension of the cysts in most cases (Table 3). In case of multiple cysts, one cyst was prominently larger than the others, and noted as “dominant cyst” (Figure 2). Anteroposterior and transverse diameters were essentially limited by the bony dimensions of the spinal canal at corresponding levels, accompanied by bony scalloping in some cases (Figure 5).
Table 3.
Maximum and mean ± SD of cyst diameters, in millimeters (mm)
| Craniocaudal | Sagittal | Transverse | |
|---|---|---|---|
| Males | 24.16 ± 10.24 | 9.36 ± 2.11 | 11.9 ± 2 |
| Females | 25.75 ± 9.66 | 9.63 ± 2.03 | 12 ± 2 |
| OVERALL | 24.98 ± 10.25 | 9.5 ± 2.07 | 12 ± 2 |
| Maximum | 30.3 | 11.3 | 14.7 |
SD, standard deviation.
Figure 5.

Sagittal bone window CT at sacrum. Bony remodeling/scalloping at posterior cortex of S2, due to Tarlov cyst (measured with line marked with +--+).
Maximal cyst diameters were not significantly different between the genders and different age groups.
Discussion
As noted earlier, scientific work on Tarlov cysts is limited to some scattered case reports7 and very few epidemiological and case–control studies.9 The picture is no different in the Indian subcontinent, or in Asia as a whole.
It has been discussed earlier that Tarlov cysts have long been set aside as rare lesions, having prevalence <5%.2,6–8 However, some recent papers have demonstrated that the actual prevalence is a bit higher,3,4 and state that many cases of Tarlov cysts remain undetected, undiagnosed, unreported or ignored.
Findings of the present study concur with the second group of studies (Table 4). Among them is the paper of Burdan et al,3 who conducted a 2 year retrospective observational study at a single hospital in Poland. They found 75 Tarlov cysts from among 842 spinal MRI (8.9%). Just like the present study, they also had found the maximum number of cysts at S2–S3 levels (56%) and only few at other levels. Similar to our study (Table 1), they found no age predilection.
Table 4.
Comparison of results with some related studies
However, in contrast with the present study, Burdan et al found a large proportion (53, 71%) of multiple and some bilateral cysts, whereas we found more single cysts (Table 2). They also found more cysts in females than in males, and stated that there is no size difference between single & multiple cysts. This is in stark contrast with our findings as well as of some others.
This difference is likely because Burdan et al did not point out that not all cysts are of the same size in a multiple cyst scenario. They did not highlight that anteroposterior and transverse diameters do not represent the true or maximum size of Tarlov cysts, as these are limited by the bony dimensions of the spinal canal. This may be the reason they missed out the concept of dominant cyst.
In fact, few authors if any have pointed this out so far, and most studies have measured only one diameter of Tarlov cysts. Multiple dimensions were measured by Gonzales et al in their cadaveric case report, where they stated that the “largest” cyst they found measured 3 × 2.5 cm,6 indicating that not all among the multiple cysts were of the same size.
Other than that, Paulsen et al7 conducted CT-guided aspiration of five patients whose symptoms were directly related to Tarlov cysts. Among them, two had multiple cysts. However, the authors only recorded cyst diameter or maximum cyst diameters without noting whether these were anteroposterior, craniocaudal or transverse diameters. Nonetheless, their use of such words as “multiple cysts with largest measuring 2.5 cm” indicate that their findings also included a dominant or largest cyst in multiple-cyst scenarios.
In 2018, Kleib et al23 reported a case of multiple sacral and a large thoracic Tarlov cyst which required surgical removal. The authors were not much concerned with cyst sizes and they did not measure any, but the MRI images they published show that the thoracic cyst spanned four vertebral levels (T7-11), having maximum measurement in craniocaudal direction. The sacral cysts also show greater size craniocaudally than anteroposteriorly, though the authors made no note of that.
Hence, through the present study, and in congruence with those mentioned above, we propose the presence of a “dominant cyst” when there are multiple Tarlov cysts. At the same time, our findings also show that maximum cyst diameters do not differ between single cysts and dominant cysts or between genders or age groups, a derivation shared by Boukobza et al as well.13
In addition to proposing the concept of “dominant cyst”, we also recommend that measurement of Tarlov cysts should always include craniocaudal length and/or extent of vertebral levels (e.g. 3.5 cm, S2–S3 levels), since craniocaudal is the only direction the cyst can grow freely. With regard to anteroposterior and transverse diameters, we recommend that these should be reported in the context of scalloping of surrounding bones and presence or absence of neural foraminal narrowing, nerve root compression or extraforaminal extension. This is because simply mentioning linear measurements in centimetres or millimetres do not reflect the potential implications of the measurements.
In 2017, Kuhn et al20 retrospectively assessed 1100 sacral MRI, that included 100 children & adolescents. They found Tarlov cysts in 132 adult patients, and none below 18 years. They also stated that prevalence of Tarlov cysts increases with age and that females were affected more than males (females 68%, i.e. ratio 2:1). This is perhaps the only study that records a >10% prevalence for Tarlov cysts, while most of the recent studies including ours found prevalence between 5 and 9%.3,4 However, it should be noted here that Kuhn et al based their study on dedicated sacral MRIs, whereas almost all other studies were based on lumbosacral MRIs. From here, it may be understood that dedicated sacral MRIs are more sensitive in detecting Tarlov cysts, an inference also drawn by Boukobza et al.13
Furthermore, the female predominance found by Kuhn et al is also shared by some authors,3,9,19,24 but not by some other authors.2,8 We think that this wide variation of findings is due to the very small number of positive cases, which cannot render reproducible or reliable statistics. There may also be a genetic or demographic background contributing to this difference, which may be evaluated in further studies.
In addition, although Kuhn et al found no Tarlov cysts below 18 years of age, Elsawaf et al25 listed two patients who underwent surgery at 7 years of age, to remove Tarlov cysts that had been symptomatic for 3–4 years. That means Tarlov cysts can develop in children below 5 years too!
Noticing that most studies regarding Tarlov cysts report so low numbers of detected cases that they cannot foster much statistical analysis, Langdown et al19 conducted a 5 year long survey over 3535 patients undergoing MRI for lumbosacral symptoms. They discovered only 54 cases, and determined that 7 (12.9%) of them had symptoms that could be directly attributed to Tarlov cysts. They found 38 (70%) of the 54 positives in females, as discussed above.
Findings of the present study also point to a conclusion that MRI for low back pain should always include the entire sacrum upto tip of the coccyx with a T2 sagittal sequence. This is because sacrum is the commonest location of Tarlov cysts and T2 sagittal is the best image to identify them. Such a derivation had earlier been made by several other authors as well.4,13,17,26 Furthermore, we also agree with the apparent or implied proposition in recent literature that the wide availability & use of MRI as well as routine use of PACS & DICOM viewers have played a good contributory role in the increased discovery of Tarlov cysts.2,3,7
It is true that the very low number of detected positive cases (=25) casts a limitation to the present study, but so is the case of most other studies on the topic. Another potential limitation is that Tarlov cyst is a histological diagnosis and requires the presence of neuronal fibers within the cyst or in its wall, which may not always be discernible on MRI. It has also not been possible in the present study to compare number & size of detected Tarlov cysts with symptoms, as none of the patients had Tarlov-associated symptoms recorded in the HIS. This is likely due to the fact that clinicians examining the patients usually consider such symptoms to be non-specific or generalize them under the umbrella term “back pain”.
Conclusions
Therefore, it is time to change our perception of brushing aside Tarlov cysts as insignificant, asymptomatic entities. It is essential to conduct further in-depth studies on the subject, in the form of case–control or cohort studies, to have an accurate understanding of the symptomatology of Tarlov cysts, to formulate grading criteria and to devise proper treatment approaches. At the moment, awareness needs to be raised among radiologists, radiographers as well as clinicians that MRI for low back pain should always extend upto tip of coccyx with a T2 sagittal image. We recommend that Tarlov cysts should always be measured in terms of craniocaudal length and/or extent of vertebral levels, and their anteroposterior and transverse dimensions be reported as presence or absence of bony scalloping, neural foraminal narrowing, nerve root compression or extraforaminal extension. It is also necessary to acquaint clinicians with Tarlov-associated symptoms, so that they can advise sacral MRI in these patients, and so that they do not ignore the MRI report when it says “Tarlov cyst”.
REFERENCES
- 1.Guo D, Shu K, Chen R, Ke C, Zhu Y, Lei T. Microsurgical treatment of symptomatic sacral perineurial cysts. Neurosurgery 2007; 60: 1059–66. doi: 10.1227/01.NEU.0000255457.12978.78 [DOI] [PubMed] [Google Scholar]
- 2.Lucantoni C, Than KD, Wang AC, Valdivia-Valdivia JM, Maher CO, La Marca F, et al. Tarlov cysts: a controversial lesion of the sacral spine. Neurosurg Focus 2011; 31: E14. doi: 10.3171/2011.9.FOCUS11221 [DOI] [PubMed] [Google Scholar]
- 3.Burdan F, Mocarska A, Janczarek M, Klepacz R, Łosicki M, Patyra K, et al. Incidence of spinal perineurial (Tarlov) cysts among East-European patients. PLoS One 2013; 8: e71514. doi: 10.1371/journal.pone.0071514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Elfaal M, Samir M. Tarlov cyst – an uncommon cause of back pain. Hamdan Medical Journal 2017; 10: 201. doi: 10.7707/hmj.695 [DOI] [Google Scholar]
- 5.Nabors MW, Pait TG, Byrd EB, Karim NO, Davis DO, Kobrine AI, et al. Updated assessment and current classification of spinal meningeal cysts. J Neurosurg 1988; 68: 366–77. doi: 10.3171/jns.1988.68.3.0366 [DOI] [PubMed] [Google Scholar]
- 6.Gonzales J, Iwanaga J, Topale N, Oskouian RJ, Tubbs RS. Multiple large perineural (Tarlov) cysts in the sacrum of a cadaver: a case report and review. Cureus 2017; 9: e1156: e1156. doi: 10.7759/cureus.1156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Paulsen RD, Call GA, Murtagh FR. Prevalence and percutaneous drainage of cysts of the sacral nerve root sheath (Tarlov cysts). AJNR Am J Neuroradiol 1994; 15: 293–7. [PMC free article] [PubMed] [Google Scholar]
- 8.Park H-J, Jeon Y-H, Rho M-H, Lee E-J, Park N-H, Park S-I, et al. Incidental findings of the lumbar spine at MRI during herniated intervertebral disk disease evaluation. AJR Am J Roentgenol 2011; 196: 1151–5. doi: 10.2214/AJR.10.5457 [DOI] [PubMed] [Google Scholar]
- 9.Murphy KJ, Nussbaum DA, Schnupp S, Long D. Tarlov cysts: an overlooked clinical problem. Semin Musculoskelet Radiol 2011; 15: 163–7. doi: 10.1055/s-0031-1275599 [DOI] [PubMed] [Google Scholar]
- 10.Singh PK, Singh VK, Azam A, Gupta S. Tarlov cyst and infertility. J Spinal Cord Med 2009; 32: 191–7. doi: 10.1080/10790268.2009.11760771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Marino D, Carluccio MA, Di Donato I, Sicurelli F, Chini E, Di Toro Mammarella L, et al. Tarlov cysts: clinical evaluation of an Italian cohort of patients. Neurol Sci 2013; 34: 1679–82. doi: 10.1007/s10072-013-1321-0 [DOI] [PubMed] [Google Scholar]
- 12.Ross JS. Diagnostic Imaging: Spine. Vol 4: Amirsys Incorporated; 2004. [Google Scholar]
- 13.Boukobza M, Roussel A, Fernandez-Rodriguez P, Laissy J-P. Giant multiple and bilateral presacral Tarlov cysts mimicking adnexal mass - imaging features. Int Med Case Rep J 2018; 11: 181–4. doi: 10.2147/IMCRJ.S147791 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ishii K, Yuzurihara M, Asamoto S, Doi H, Kubota M. A huge presacral Tarlov cyst. J Neurosurg 2007; 7: 259–63. doi: 10.3171/SPI-07/08/259 [DOI] [PubMed] [Google Scholar]
- 15.H'ng MWC, Wanigasiri UIDK, Ong CL, H’ng MWC, Perineural OCL. Perineural (Tarlov) cysts mimicking adnexal masses: a report of three cases. Ultrasound Obstet Gynecol 2009; 34: 230–3. doi: 10.1002/uog.6448 [DOI] [PubMed] [Google Scholar]
- 16.Saboo SS, Di Salvo D. Perineural cysts resembling complex cystic adnexal masses on transvaginal sonography. J Clin Ultrasound 2013; 41: 55–8. doi: 10.1002/jcu.20899 [DOI] [PubMed] [Google Scholar]
- 17.Murphy K, Oaklander AL, Elias G, Kathuria S, Long DM. Treatment of 213 patients with symptomatic Tarlov cysts by CT-guided percutaneous injection of fibrin sealant. AJNR Am J Neuroradiol 2016; 37: 373–9. doi: 10.3174/ajnr.A4517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sharma M, Velho V, Mally R, Khan SW. Symptomatic lumbosacral perineural cysts: a report of three cases and review of literature. Asian J Neurosurg 2015; 10: 222. doi: 10.4103/1793-5482.161177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Langdown AJ, Grundy JRB, Birch NC. The clinical relevance of Tarlov cysts. J Spinal Disord Tech 2005; 18: 29–33. doi: 10.1097/01.bsd.0000133495.78245.71 [DOI] [PubMed] [Google Scholar]
- 20.Kuhn FP, Hammoud S, Lefèvre-Colau M-M, Poiraudeau S, Feydy A. Prevalence of simple and complex sacral perineural Tarlov cysts in a French cohort of adults and children. J Neuroradiol 2017; 44: 38–43. doi: 10.1016/j.neurad.2016.09.006 [DOI] [PubMed] [Google Scholar]
- 21.Padma S, Palaniswamy SS. Multilocular disseminated Tarlov cysts: importance of imaging and management options. Indian J Nucl Med 2012; 27: 111. doi: 10.4103/0972-3919.110702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Prashad B, Jain AK, Dhammi IK. Tarlov cyst: case report and review of literature. Indian J Orthop 2007; 41: 401. doi: 10.4103/0019-5413.37007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kleib A-S, Salihy S-M, Hamdi H, Carron R, Soumaré O. A rare cause of thoracic spinal cord compression by multiple large Tarlov cysts. Korean J Neurotrauma 2018; 14: 35. doi: 10.13004/kjnt.2018.14.1.35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Oaklander AL. Tarlov cysts. Neurosurg Focus 2012; 32: E9. doi: 10.3171/2012.1.FOCUS11374 [DOI] [PubMed] [Google Scholar]
- 25.Elsawaf A, Awad TE, Fesal SS. Surgical excision of symptomatic sacral perineurial Tarlov cyst: case series and review of the literature. Eur Spine J 2016; 25: 3385–92. doi: 10.1007/s00586-016-4584-3 [DOI] [PubMed] [Google Scholar]
- 26.Rodziewicz GS, Kaufman B, Spetzler RF. Diagnosis of sacral perineural cysts by nuclear magnetic resonance. Surg Neurol 1984; 22: 50–2. doi: 10.1016/0090-3019(84)90228-3 [DOI] [PubMed] [Google Scholar]