Abstract
Background
Intolerance of uncertainty (IU), perceived attentional control (AC), and poor cognitive control abilities are risk factors for anxiety; however, few studies have examined their interactive effects in relation to anxiety. A more complete understanding of interplay between IU, perceived AC, and cognitive control could inform intervention efforts.
Methods
The current study examined the direct and interactive effects of IU and AC on anxiety in a sample of 280 community outpatients (M age = 36.01 years, SD = 16.17). Perceived AC was measured using self-report and cognitive control abilities were measured using a Go/No-Go task.
Results
Findings indicated a significant IU by perceived AC interaction predicting worry and GAD diagnoses. There was a positive relation between IU and worry/GAD diagnoses that was strongest among those with high perceived AC. Perceived AC was unrelated to cognitive control abilities, and cognitive control abilities did not interact significantly with IU. Cognitive control abilities were related to worry symptoms but not to GAD diagnoses.
Conclusions
These results indicate that at high levels of perceived AC, individuals with elevated IU report higher levels of worry, potentially due to the conscious use of worry as an emotion regulation strategy. Clinical implications and future directions are discussed.
Keywords: Generalized anxiety disorder, Anxiety, Attentional control, Intolerance of uncertainty
Generalized anxiety disorder (GAD), characterized by excessive and persistent worry spanning multiple domains (American Psychiatric Association, 2013), is one of the most common psychiatric disorders, with lifetime prevalence estimates of approximately 6% in the United States (Kessler et al., 2012). GAD is associated with significant personal distress and impairment, as evidenced by decreased scores on quality of life measures, role impairments, and economic costs (Alonso et al., 2018). Given the burden of GAD, research clarifying the role of risk and maintenance factors in the etiology of GAD is critical. Three crucial components contributing to worry are intolerance of uncertainty (IU), cognitive control, and attentional control (AC; Carleton, 2016a, 2016b; Derryberry & Reed, 2002; Paulus, 2015). Research is needed to consider these constructs together to determine their unique roles and interaction to inform novel intervention and prevention efforts.
IU is defined as “an individual’s dispositional incapacity to endure the aversive response triggered by the perceived absence of salient, key, or sufficient information, and sustained by the associated perception of uncertainty” (p. 31, Carleton, 2016a, 2016b). Individuals with elevated IU tend to view the potential of a negative event as unacceptable, even events with a low probability of occurring (Carleton, Norton, et al., 2007; Carleton, Sharpe, et al., 2007). Further, IU may lead individuals to experience distress and worry in ambiguous situations, as the perceived lack of sufficient information amplifies their subjective feeling of uncertainty. Due to distress related to feelings of uncertainty, individuals high in IU may seek to avoid uncertain situations altogether. Extant research provides initial support for IU as a risk factor for worry, as IU is related to worry cross-sectionally (Dugas et al., 2001; Yook et al., 2010), even after controlling for other risk factors (e.g., anxiety sensitivity, distress tolerance, neuroticism; Dugas et al., 2001; Norr et al., 2013; Norton & Mehta, 2007; Sexton et al., 2005). Additionally, experimental manipulations targeting IU have resulted in decreases in worry, suggesting a causal link between the two constructs (Ladouceur et al., 2000). Beyond predicting worry, IU is associated with GAD symptoms (Naragon-Gainey & Watson, 2018) and diagnoses (Dugas et al., 1998; Freeston et al., 1994; Gentes & Ruscio, 2011), highlighting the importance of IU in conferring risk for pathological worry (Shihata et al., 2016).
Cognitive control is another construct associated with GAD symptoms. Cognitive control includes processes involved in regulating, coordinating, and sequencing thoughts and actions to accomplish goals (Braver, 2012). Cognitive control is a multifaceted construct (Posner & Snyder, 2004), consisting of processes related to the conscious use of goal-relevant information to orient attention and processes related to correct behaviors to on a just-in-time basis (Braver, 2012). One cognitive control ability particularly relevant to anxiety is inhibition (Ansari & Derakshan, 2011), defined as the ability to hold back or stop an action based on situational information (Paulus, 2015). Inhibition abilities are commonly measured using performance tasks that require cognitive control over attention, such as Go/No-go tasks (Cieslik et al., 2015; Hampshire et al., 2010; Macatee et al., 2018). In Go/No-go tasks, participants are told to inhibit prepotent responses when presented with certain stimuli (e.g., a certain letter, a repeated letter) and respond to all other stimuli. Individuals with heightened anxiety often exhibit poorer performance on Go/No-go tasks (Ansari & Derakshan, 2011; Scholz et al., 2009), particularly for errors of omission (Wright et al., 2014). However, limited research has been conducted to determine how cognitive control abilities, such as inhibition, and IU may jointly relate to worry.
One facet of the broader cognitive control construct is AC, defined as the ability to regulate attention in the face of distraction (Derryberry & Reed, 2002). AC is conceptualized as the result of the voluntary attention system in the dual-process model of attention as advanced by Posner and Petersen (1990). Within the dual-process model of attention framework, AC involves the ability to disengage, shift, and focus attention based on current goals. The perceived ability to control attention (i.e., perceived AC) is typically assessed via self-report measures (Derryberry & Reed, 2002; Judah et al., 2020), and often correlates little with cognitive control abilities (Williams et al., 2017). From one perspective, poor cognitive control abilities are thought to confer risk for worry via a diminished capacity to disengage with worries and direct attention away from threatening stimuli (Derryberry & Reed, 2002; Eysenck et al., 2007). Another perspective is that difficulties controlling worry may result in the self-perception of having diminished AC (Wells, 1995), regardless of actual cognitive control abilities. Both perspectives are supported by evidence showing an association between worry and cognitive control abilities (Hallion et al., 2019; Stefanopoulou et al., 2014) and perceived AC (Armstrong et al., 2011; Fox et al., 2015; Judah et al., 2014, 2020; Moradi et al., 2014). Thus, research on the association between cognitive control and worry needs to examine both cognitive control abilities and perceived AC, as different interventions may be warranted to target cognitive control abilities and/or perceived AC.
Despite theoretical and empirical evidence identifying IU and cognitive control (both cognitive control abilities and perceptions of AC) as independent predictors of worry, few studies have examined the interplay between IU and cognitive control related to worry. Examining such interplay is important to delineate individuals at highest risk for deleterious effects of IU and cognitive control deficits. Dual-systems models of psychopathology (e.g., Ouimet et al., 2009) can be used as a framework to delineate how cognitive-affective risk factors interplay with cognitive abilities to lead to psychopathology. Specifically, cognitive-affective risk factors (such as IU) have a greater influence on symptoms of psychopathology among individuals with poorer abilities to control information processing (e.g., poorer abilities to inhibit thoughts and responses, such as poorer cognitive control and AC; Gyurak et al., 2011; Ouimet et al., 2009; Stefanopoulou et al., 2014; Zainal & Newman, 2018). Thus, cognitive control abilities may moderate the relation between IU and worry, in that IU may be most strongly related to worry among individuals that are less able to divert their attention away from threatening stimuli (i.e., individuals with poor cognitive control abilities).
In addition to cognitive control abilities, perceived AC has been found to moderate risk for GAD and other forms of psychopathology. For example, low levels of perceived AC are associated with a stronger prospective relation between overall worry and subsequent GAD symptoms (Mills et al., 2016), and attentional biases such that individuals with poor perceived AC attend more to threat-related stimuli (Derryberry & Reed, 2002; Peers & Lawrence, 2009; Susa et al., 2012; Taylor et al., 2016). These results suggest that more research is needed to understand how perceived AC may moderate risk for GAD. Such research has the potential to identify interventions (e.g., cognitive bias modification) that may be useful to reduce risk for GAD.
Although there is theoretical and empirical support for cognitive control constructs (i.e., cognitive control abilities, perceived AC) moderating the effect of cognitive biases on worry, no study has examined whether cognitive control moderates the influence of IU on worry or GAD symptoms. The current study was designed to examine the relations of IU with GAD and worry, and how those relations may interact with cognitive control abilities and perceived AC. Given evidence that perceived AC moderates associations between risk factors and psychopathology (e.g., Bardeen & Fergus, 2016) and theoretical proposals concerning the role of cognitive control in GAD, it was expected that perceived AC would moderate the relation of IU with worry and with GAD. Given AC is a component of cognitive control, it was expected that perceived AC would be positively related to cognitive control abilities, and that a similar pattern of results would emerge across cognitive control abilities and perceived AC.
Methods
Participants
Participants were 280 community adults presenting for participation in a clinical trial targeting risk factors for anxiety and mood disorders (ClinicalTrials.gov Identifier NCT01941862). Inclusionary criteria included being English speaking and scoring at or above the community mean on at least one of several risk factors for anxiety and mood disorders (i.e., anxiety sensitivity, thwarted belongingness, perceived burdensomeness). Exclusionary criteria included evidence of uncontrolled bipolar or psychotic spectrum disorders, serious suicidal intent that would warrant immediate hospitalization, unstable medication usage (i.e., not on a stable dose for at least three months prior to study entry), and/or participation in current psychotherapy.
Several individuals were removed from analyses due to participant non-compliance with experimenter instructions (n = 4), missing data (n = 2) or technical problems (n = 12). Individuals with performance at or below 50% (i.e., correct responses were at or below chance) on either Go or No-go trials were also removed (n = 8). This resulted in 254 participants (M age = 35.45, SD = 16.09; 57.1% female). Most of the sample identified as White (60.2%), with 25.6% identifying as Black, 2.8% Asian, 0.4% Pacific Islander, 0.4% American Indian, and 10.6% other (e.g. identifying with more than one race). Further, 28.3% of individuals identified as Veterans (n = 72). Most of the sample (90.2%) was diagnosed with at least one disorder, and 63% were diagnosed with two or more disorders (M diagnoses = 2.20, SD = 1.54, range: 0 – 8). Of note, 56.3% of the sample were diagnosed with a primary anxiety disorder or anxiety-related disorder (i.e., obsessive–compulsive disorder, post-traumatic stress disorder) and 23.2% were diagnosed with a primary unipolar mood disorder (i.e., major depressive disorder, persistent depressive disorder). All participants were screened for neurological conditions and visual impairments.
Measures
Intolerance of Uncertainty Scale-12 (IUS-12; Carleton, Sharpe, et al., 2007; Carleton, Norton, et al., 2007)
The IUS-12 is a 12-item self-report measure designed to assess IU (Carleton, Norton, et al., 2007; Carleton, Sharpe, et al., 2007). Participants rated how characteristic each item (e.g., Unforeseen events upset me greatly) was of them on a 5-point Likert scale ranging from 1 (not at all characteristic of me) to 5 (entirely characteristic of me), with higher scores indicating higher IU. The IUS-12 has demonstrated good psychometric properties (Carleton, Norton, et al., 2007; Carleton, Sharpe, et al., 2007). Reliability in the current study was excellent (α = 0.92).
Attentional Control Scale (ACS; Derryberry & Reed, 2002)
The ACS is a 20-item self-report measure designed to assess AC (Derryberry & Reed, 2002). Participants indicated how consistent each item (e.g., When I am working hard on something, I still get distracted by events around me) was with their experience of AC on a 5-point Likert scale ranging from 1 (almost never) to 5 (always), with higher scores representing superior perceived AC. The ACS has demonstrated strong psychometric properties (Derryberry & Reed, 2002). Reliability in the current study was adequate (α = 0.87).
Penn State Worry Questionnaire (PSWQ; Meyer et al., 1990)
The PSWQ is a 16-item self-report measure developed to capture pathological worry (Meyer et al., 1990). Participants indicated how often they experienced each item (e.g., I am always worrying about something) on a 5-point Likert scale ranging from 1 (not at all typical of me) to 5 (very typical of me), with higher scores indicating more severe worry. The PSWQ has demonstrated strong psychometric properties (Meyer et al., 1990). In the current study, the reliability of the PSWQ was adequate (α = 0.83).
Structured Clinical Interview for DSM-5-Research Version (SCID-5)
The SCID-5 is a semi-structured clinical interview used to evaluate the presence of DSM-5 diagnoses (First et al., 2015). The SCID-5 was administered by trained clinical psychology doctoral students. All SCID-5 administrations were reviewed by a licensed clinical psychologist to ensure diagnostic accuracy. The SCID-5 has demonstrated excellent interrater reliability in prior studies in the lab (κ = 0.77; Schmidt et al., 2014). The presence of GAD diagnoses was used as a binary outcome variable in the current study.
Procedures
Prior to enrolling in the clinical trial, participants completed a baseline session during which they were administered the SCID-5 and a packet of self-report questionnaires. Following the baseline session, participants attended a laboratory session in which they completed behavioral tasks. All data used in the present study were derived from the baseline and laboratory sessions prior to intervention randomization.
Behavioral tasks were completed in a dimly lit, sound-attenuated room. Stimuli were presented using a Dell OptiPlex 780 computer running E-Prime version 2.0.8.90. Stimuli were presented on a 21” CRT color monitor at a viewing distance of 100 cm, subtending a visual angle of 3.5°. The recording session lasted between 2.5 and 3 h and consisted of several different tasks, including the Go/No-go Complex Paradigm task used in the present study. The Go/No-go Complex Paradigm task was completed in the first 20–30 min of EEG recording, within recommendations for duration of EEG recording sessions (Miskin et al., 2015).
Go/No-go Complex Paradigm
Go/No-go tasks are commonly used paradigms designed to assess individual differences in response inhibition by requiring participants to respond to frequent signals (i.e., Go trials) and infrequently withhold a response when presented with pre-determined and distinct signals (i.e., No-go trials; Simmonds et al., 2008). Performance in Go/No-go tasks has been used to assess cognitive control abilities (Cieslik et al., 2015). In the current version of the task two different letters were presented serially (i.e., one at a time) in an alternating pattern. Participants were required to press one of two buttons to indicate which letter they saw but only when the letter was different than the previous letter (i.e., Go trials; Garavan et al., 2003; Hester et al., 2004; Kelly et al., 2004). No-go trials, in which participants were required to withhold a response, were trials in which the letter was the same as the previous letter (e.g., a response should be withheld for the fifth stimulus in the sequence X-Y-X-Y-Y-X). Letters were randomized by block, such that each block consisted of different letters (i.e., within-subject counterbalancing). The letters were presented in the same order across participants.
The Go/No-go Complex Paradigm included seven blocks comprised of 18 Go trials (75%) and six No-go trials (25%) for a total of 126 Go trials and 42 No-go trials. A distinct set of letters were used for each block. Prior to the beginning of each block, instructions regarding what button to press for each letter (e.g., whether to press the left or right button when the letter “X” appeared), and performance on the previous block were presented. Each Go and No-go signal (i.e., the letters) were presented for 296 ms immediately followed by a blue fixation point which was presented for the duration of the 1150 ms response window. The fixation cross did not terminate following a response to ensure that task parameters would not change based on participant reaction times. Feedback (i.e., correct or incorrect) was then presented for an additional 1000 ms. Inter-trial intervals were marked by a fixation point presented on the screen for 900 ms. This Go/ No-go paradigm has been previously used in investigations of cognitive control (Albanese et al., 2019; Macatee et al., 2018). The number of errors made on the Go/No-go task was used as a marker of cognitive control abilities.
Data Analytic Plan
Path analytic models were conducted in Mplus version 8.0 (Muthén & Muthén, 1998–2019) to examine the associations between IU, perceived AC, cognitive control abilities, age, sex, IU by perceived AC interaction, and IU by cognitive control abilities interaction. Full information maximum likelihood was used to account for missing values. Full information maximum likelihood estimation (Enders, 2001a) was used to handle missing data in these analyses. Full information maximum likelihood estimation provides less biased parameter estimates compared to listwise deletion, pairwise deletion, and mean imputation (Enders, 2001c) and provides nonbiased estimates under more conditions (e.g., when data is not missing completely at random, when data is nonnormal; Enders, 2001b, 2001c, 2008). Sensitivity analyses were conducted to determine whether item overlap between the ACS and PSWQ influenced the results. In the sensitivity analyses, items with overlapping content (i.e., ACS items that referred to concentration difficulties and distracting thoughts, PSWQ items that referred to uncontrollable worry and concentration) were removed. There was no substantive difference between the full scale results and the shortened scale results; therefore, results are presented using all ACS and PSWQ items.
Results
Descriptive Statistics and Correlations
Descriptive statistics and correlations for the study variables are provided in Table 1. Regarding missing data, four participants did not have IUS-12 data, 30 did not have ACS data, five were missing data on No-go errors, three did not have PSWQ data, and two did not have data on age, sex, or GAD diagnoses. With the exception of No-go errors, all variables were within acceptable skew and kurtosis limits for providing robust results in the context of structural equation modeling (i.e., absolute skew < 2, absolute kurtosis < 7; Curran et al., 1996). A transformation of No-go errors achieved acceptable skew and kurtosis and did not impact results, so the untransformed variables were included in all analyses. All other assumptions for path analytic models (i.e., linear relations, lack of multicollinearity, no autocorrelations, homoscedasticity) held for all analyses. A total of 25.4% of the sample had a current GAD diagnosis.
Table 1.
Descriptive statistics and correlations
| Variables | IU | Perceived AC | CC abilities | Age | Sex | Worry | GAD |
|---|---|---|---|---|---|---|---|
|
| |||||||
| IU | – | ||||||
| Perceived AC | −.43*** | – | |||||
| CC abilities | −.02 | .10 | – | ||||
| Age | −.002 | .07 | −.19** | – | |||
| Sex | .14* | −.10 | .16* | −.33*** | – | ||
| Worry | .52*** | −.34*** | .09 | −.12* | .15* | – | |
| GAD | .27*** | −.23*** | .04 | −.2*** | .26*** | .81*** | – |
| Mean (%) | 33.61 | 29.80 | 35.03 | 36.01 | 43.8% male | 67.89 | 25.4% |
| SD | 11.46 | 6.56 | 5.88 | 16.17 | 7.44 | ||
IU Intolerance of uncertainty, AC Attentional control, CC Cognitive control, GAD Generalized anxiety disorder
p < .001
p < .01
p < .05
Linear Regression Models for Worry Symptoms
The interaction effect between IU and cognitive control abilities was not significant and was therefore not included in the final model. Standardized model parameters are provided in the top panel of Table 2. IU was significantly associated with worry symptoms (β = 0.45, p < 0.001) as was perceived AC (β = −0.13, p = 0.01) and cognitive control abilities (β = 0.29, p = 0.01). A significant IU by perceived AC interaction (β = 0.02, p = 0.04) was found. Probing this interaction revealed that the relation between IU and worry symptoms was stronger at 1 SD above mean perceived AC (β = 0.55, p < 0.001) and weaker 1 SD below mean perceived AC (β = 0.35, p < 0.001; see Fig. 1). Overall, this model accounted for 43.2% of the variance in worry symptoms.
Table 2.
Regression analysis examining intolerance of uncertainty and attentional control variables predicting worry and generalized anxiety disorder
| B | SE | p | |
|---|---|---|---|
|
| |||
| Worry symptoms | |||
| IU | .57 | .07 | <.001 |
| Perceived AC | −.30 | .12 | .01 |
| CC abilities | .29 | .12 | .01 |
| Age | −.11 | .04 | .02 |
| Sex | 7.78 | 1.43 | <.001 |
| IU X perceived AC | .02 | .01 | .04 |
| GAD | |||
| IU | .06 | .02 | <.001 |
| Perceived AC | −.07 | .03 | .02 |
| CC abilities | −.004 | .03 | .87 |
| Age | −.03 | .01 | .01 |
| Sex | 1.17 | .41 | .01 |
| IU X perceived AC | .01 | .002 | .01 |
IU Intolerance of uncertainty, AC Attentional control, CC Cognitive control, GAD Generalized anxiety disorder, SE Standard error
Fig. 1.

The effects of intolerance of uncertainty (IU) on worry symptoms at 1 standard deviation (SD) below the mean (Low) and 1 SD above the mean (High) perceived attentional control (AC)
Logistic Regression Models for Generalized Anxiety Disorder
The same model was examined, substituting a current GAD diagnosis as the outcome variable. Again, the interaction between IU and cognitive control abilities was non-significant and was therefore not included in the final model. Output for this model is provided in unstandardized model parameters (see bottom panel of Table 2). IU was significantly associated with a GAD diagnosis (B = 0.06, p < 0.001, OR = 1.06) as was perceived AC (B = −0.07, p = 0.02, OR = 0.93). Cognitive control abilities were not significantly associated with a GAD diagnosis (B = −0.004, p = 0.47). A significant IU by perceived AC interaction (B = 0.01, p = 0.01) moderated the effect of IU such that the relation between IU and GAD was significant at 1 SD above mean perceived AC (B = 0.10, p < 0.001, OR = 1.11) but was not significant at 1 SD below the mean perceived AC (B = 0.02, p = 0.26, OR = 1.02; see Fig. 2). This model accounted for 39.1% of the variance in GAD diagnosis.
Fig. 2.
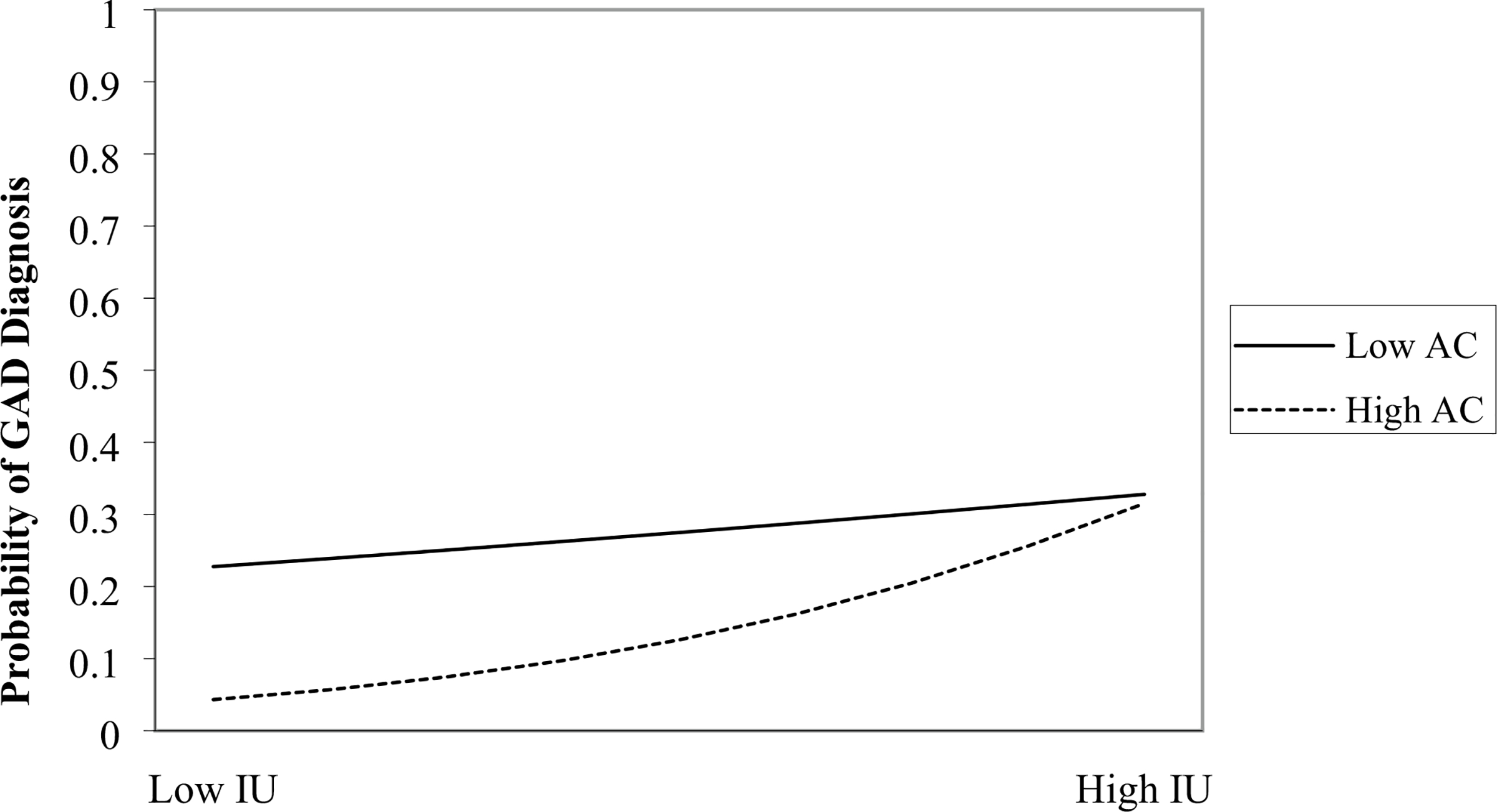
The effects of intolerance of uncertainty (IU) on the probability of meeting diagnostic criteria for GAD at 1 standard deviation (SD) below the mean (Low) and 1 SD above the mean (High) perceived attentional control (AC)
Discussion
The present study was designed to assess the moderating effect of cognitive control (both cognitive control abilities and perceived AC) on the association between IU and worry. It was expected that cognitive control abilities and perceived AC would moderate the relation between IU and worry. The results supported the hypothesis that perceived AC would influence the relation between IU and worry; in both models, IU was more strongly related to the outcomes at high levels of perceived AC compared to the relation between IU and outcomes at low levels of perceived AC. In contrast, there was no significant interaction between cognitive control abilities and IU in predicting worry or GAD diagnoses. Taken together, these results provide support for the moderating effect of perceived AC on the relation between IU, worry symptoms, and GAD diagnoses, but do not support cognitive control abilities moderating the relations between IU and worry/GAD diagnoses.
In the current study, perceived AC moderated the relations IU shared with worry and GAD such that the strongest relation between IU and worry was at high levels of perceived AC. These results contrast with two recent studies considering AC as a moderator of PTSD symptoms. In these cross-sectional studies, there was a negative interaction between perceived AC and risk factors, such that high perceived AC reduced the impact of anxiety sensitivity (the fear of anxiety symptoms; Albanese et al., 2018), distress tolerance (the ability to tolerate negative emotions), and experiential avoidance (avoiding uncomfortable thoughts, feelings, and sensations; Bardeen & Fergus, 2016) on symptoms of PTSD. However, our finding is consistent with literature finding antagonistic relations when examining the role of multiple risk factors on anxiety (e.g., Allan et al., 2015; Macatee et al., 2016). One possible explanation for discrepant results is that perceived AC may offer protective benefits at high levels of some risk factors, such as anxiety sensitivity (Albanese et al., 2018) and at low levels of other risk factors, such as IU. Additionally, individuals high in AC and in IU may choose to purposefully engage in worry as an emotion regulation strategy to cope with IU. The conscious use of worry as an emotion regulation strategy is consistent with several theoretical models of worry, such as the contrast avoidance model, that suggest paradoxical effects of effortful thought suppression/control, such that the choice to use worry as an emotion regulation technique leads to higher levels of worry (Behar et al., 2009; Newman & Llera, 2011). In keeping with those models, individuals with good cognitive control abilities may choose to engage in worry to regulate their emotions and prevent negative emotions in response to unexpected events.
In the current study, behavioral measures of cognitive control abilities did not interact with IU to predict worry symptoms or GAD diagnoses, despite independently predicting worry symptoms. The current results indicate possible distinct roles of perceived AC and cognitive control abilities in the context of worry and GAD. Wells (1995); (Wells & Matthews, 1996) proposed that difficulty controlling worry can lead to the perception of AC difficulties. Thus, an individual’s perception of AC difficulties may be compounded by worry, whereas their actual cognitive control abilities may not be affected. Our results build on past research by suggesting distinct roles of perceived AC and cognitive control abilities in the worry process. Alternatively, the ACS may share more common method variance (i.e., potentially inflated covariation when constructs are measured using the same method of measurement; Podsakoff et al., 2012) with the IUS-12 compared to Go/No-go task performance, making a perceived AC by IU interaction more likely. However, this explanation does not account for the clinician-assessed GAD diagnosis results that would not share common method variance with self-report measures. Another consideration is that the Go/No-go task does not represent a comprehensive measure of cognitive control abilities. A recent study found that GAD diagnosis and clinician rated severity were unrelated to Go/No-go performance but were associated with impaired Stroop performance (Hallion et al., 2017). These authors proposed that the lack of association between GAD diagnoses and Go/No-go performance was because Go/No-go performance is more representative of motor inhibition than cognitive inhibition, and cognitive inhibition is better reflected in Stroop performance. Thus, alternative behavioral measures may better reflect cognitive control abilities and should be used in future studies of risk for GAD.
Several limitations of the current study should be considered when interpreting these results. First, this was a cross-sectional study; thus, inferences about the temporal dynamics between IU, cognitive control, and worry cannot be determined. Additionally, this study was conducted in a sample with elevated psychopathology, so the results may not generalize to other populations. For example, the majority of participants in the current study diagnosed with GAD presented with other comorbid conditions (85.7% of participants were diagnosed with at least one comorbid condition). Also, trial-level behavioral data were not available for the current study; thus, reliability for the Go/No-go task was not presented. Although the version of the Go/No-go task used in this study produces reliable event-related potential components (Albanese et al., 2019), the authors were unable to calculate measures of reliability for cognitive control abilities. Future studies should include multiple measures of across units of analysis to form a reliable psychoneurometric index for cognitive control abilities (e.g., Yancey et al., 2016). Finally, only one self-report measure and one behavioral task were used to index AC in the current study. Given that perceived AC was unrelated to cognitive control abilities, future studies should include more specific measures of cognitive control abilities as related to AC to form a more comprehensive conceptualization of AC, such as Stroop performance or eye-tracking measures of AC abilities (Chen et al., 2015).
Despite these limitations, the results of the current study provide novel insight into the interplay of IU and AC in predicting worry and GAD. In addition, these results raise questions about the convergence between multiple methods of cognitive control, and the differential associations that these measures may have with cognitive vulnerabilities and psychopathology. Given the transdiagnostic nature of perceived AC and IU, research efforts should examine the combined effect of perceived AC and IU on other forms of psychopathology. In addition, the present study found evidence that high perceived AC may increase risk for individuals that also experience high IU, potentially because those participants are successful in employing maladaptive strategies to regulate emotions (e.g., worry). Thus, clinicians that work with individuals with high perceived AC may want to focus on developing adaptive emotion regulation skills during treatment to prevent the use of worry as a potential emotion regulation technique.
Footnotes
Conflict of interest The authors declare that they have no conflict of interest.
Informed Consent Informed consent was obtained from all individual participants included in the study.
Animal Rights No animals were used in the current study.
References
- Albanese BJ, Macatee RJ, Allan NP, Short NA, Norr AM, & Schmidt NB (2018). Interactive effects of anxiety sensitivity and attentional control on posttraumatic stress in community and clinical populations. Psychiatry (New York), 81(1), 71–84. 10.1080/00332747.2017.1309867 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Albanese BJ, Macatee RJ, Gallyer AJ, Stanley IH, Joiner TE, & Schmidt NB (2019). Impaired conflict detection differentiates suicide attempters from ideating nonattempters: Evidence from event-related potentials. Biological Psychiatry: Cognitive Neuroscience and Neuroimaging, 4(10), 902–912. 10.1016/j.bpsc.2019.05.015 [DOI] [PubMed] [Google Scholar]
- Allan NP, Norr AM, Macatee RJ, Gajewska A, & Schmidt NB (2015). Interactive effects of anxiety sensitivity and emotion regulation on anxiety symptoms. Journal of Psychopathology and Behavioral Assessment, 37(4), 663–672. 10.1007/s10862-015-9484-z [DOI] [Google Scholar]
- Alonso J, Mortier P, Auerbach RP, Bruffaerts R, Vilagut G, Cuijpers P, & WHO WMH-ICS Collaborators, on behalf of the W. W.I. (2018). Severe role impairment associated with mental disorders: Results of the WHO world mental health surveys international college student project. Depression and Anxiety, 35(9), 802–814. 10.1002/da.22778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders. (5th ed.). American Psychiatric Publishing. [Google Scholar]
- Ansari TL, & Derakshan N (2011). The neural correlates of impaired inhibitory control in anxiety. Neuropsychologia, 49(5), 1146–1153. 10.1016/j.neuropsychologia.2011.01.019 [DOI] [PubMed] [Google Scholar]
- Armstrong T, Zald DH, & Olatunji BO (2011). Attentional control in OCD and GAD: Specificity and associations with core cognitive symptoms. Behaviour Research and Therapy, 49(11), 756–762. 10.1016/j.brat.2011.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bardeen JR, & Fergus TA (2016). Emotional distress intolerance, experiential avoidance, and anxiety sensitivity: The buffering effect of attentional control on associations with posttraumatic stress symptoms. Journal of Psychopathology and Behavioral Assessment, 38, 320–329. 10.1007/s10862-015-9522-x [DOI] [Google Scholar]
- Behar E, DiMarco ID, Hekler EB, Mohlman J, & Staples AM (2009). Current theoretical models of generalized anxiety disorder (GAD): Conceptual review and treatment implications. Journal of Anxiety Disorders 10.1016/j.janxdis.2009.07.006 [DOI] [PubMed] [Google Scholar]
- Braver TS (2012). The variable nature of cognitive control: A dual mechanisms framework. Trends in Cognitive Sciences. 10.1016/j.tics.2011.12.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carleton NR, Sharpe D, & Asmundson GJGG (2007). Anxiety sensitivity and intolerance of uncertainty: Requisites of the fundamental fears? Behaviour Research and Therapy, 45, 2307–2316. 10.1016/j.brat.2007.04.006 [DOI] [PubMed] [Google Scholar]
- Carleton RN (2016a). Into the unknown: A review and synthesis of contemporary models involving uncertainty. Journal of Anxiety Disorders, 39, 30–43. 10.1016/j.janxdis.2016.02.007 [DOI] [PubMed] [Google Scholar]
- Carleton RN (2016b). Fear of the unknown: One fear to rule them all? Journal of Anxiety Disorders, 41, 5–21. 10.1016/j.janxdis.2016.03.011 [DOI] [PubMed] [Google Scholar]
- Carleton RN, Norton MAPJ, & Asmundson GJG (2007). Fearing the unknown: A short version of the intolerance of uncertainty scale. Journal of Anxiety Disorders, 21, 105–117. 10.1016/j.janxdis.2006.03.014 [DOI] [PubMed] [Google Scholar]
- Chen NTM, Clarke PJF, Watson TL, MacLeod C, & Guastella AJ (2015). Attentional bias modification facilitates attentional control mechanisms: Evidence from eye tracking. Biological Psychology, 104, 139–146. 10.1016/J.BIOPSYCHO.2014.12.002 [DOI] [PubMed] [Google Scholar]
- Cieslik EC, Mueller VI, Eickhoff CR, Langner R, & Eickhoff SB (2015). Three key regions for supervisory attentional control: Evidence from neuroimaging meta-analyses. Neuroscience and Biobehavioral Reviews. 10.1016/j.neubiorev.2014.11.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curran PJ, West SG, & Finch JF (1996). The robustness of test statistics to nonnormality and specification error in confirmatory factor analysis. Psychological Methods, 1, 16–29. 10.1037/1082-989X.1.1.16 [DOI] [Google Scholar]
- Derryberry D, & Reed MA (2002). Anxiety-related attentional biases and their regulation by attentional control. Journal of Abnormal Psychology, 111, 225–236. 10.1037//0021-843X.111.2.225 [DOI] [PubMed] [Google Scholar]
- Dugas MJ, Gagnon F, Ladouceur R, & Freeston MH (1998). Generalized anxiety disorder: A preliminary test of a conceptual model. Behaviour Research and Therapy, 36, 215–226. 10.1016/S0005-7967(97)00070-3 [DOI] [PubMed] [Google Scholar]
- Dugas MJ, Gosselin P, & Ladouceur R (2001). Intolerance of uncertainty and worry: Investigating specificity in a nonclinical sample. Cognitive Therapy and Research, 25, 551–558. 10.1023/A:1005553414688 [DOI] [Google Scholar]
- Enders CK (2001a). A primer on maximum likelihood algorithms available for use with missing data. Structural Equation Modeling, 8(1), 128–141. 10.1207/S15328007SEM0801_7 [DOI] [Google Scholar]
- Enders CK (2001b). The impact of nonnormality on full information maximum-likelihood estimation for structural equation models with missing data. Psychological Methods, 6(3), 352–370. 10.1037/1082-989x.6.4.352 [DOI] [PubMed] [Google Scholar]
- Enders CK (2001c). The performance of the full information maximum likelihood estimator in multiple regression models with missing data. Educational and Psychological Measurement, 61(5), 713–740. 10.1177/0013164401615001 [DOI] [Google Scholar]
- Enders CK (2008). A note on the use of missing auxiliary variables in full information maximum likelihood-based structural equation models. Structural Equation Modeling, 15(3), 434–448. 10.1080/10705510802154307 [DOI] [Google Scholar]
- Eysenck MW, Derakshan N, Santos R, & Calvo MG (2007). Anxiety and cognitive performance: Attentional control theory. Emotion, 7(2), 336–353. 10.1037/1528-3542.7.2.336 [DOI] [PubMed] [Google Scholar]
- First MB, Williams JBW, Karg RS, & Spitzer RL (2015). Structured clinical interview for DSM-5—Research version (SCID-5 for DSM-5, research version; SCID-5-RV). American Psychiatric Association. [Google Scholar]
- Fox E, Dutton K, Yates A, Georgiou GA, & Mouchlianitis E (2015). Attentional control and suppressing negative thought intrusions in pathological worry. Clinical Psychological Science, 3(4), 593–606. 10.1177/2167702615575878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freeston MH, Rhéaume J, Letarte H, Dugas MJ, & Ladouceur R (1994). Why do people worry? Personality and Individual Differences, 17, 791–802. 10.1016/0191-8869(94)90048-5 [DOI] [Google Scholar]
- Garavan H, Ross T, Kaufman J, & Stein E (2003). A midline dissociation between error-processing and response-conflict monitoring. NeuroImage, 20(2), 1132–1139. 10.1016/S1053-8119(03)00334-3 [DOI] [PubMed] [Google Scholar]
- Gentes EL, & Ruscio AM (2011). A meta-analysis of the relation of intolerance of uncertainty to symptoms of generalized anxiety disorder, major depressive disorder, and obsessive–compulsive disorder. Clinical Psychology Review, 31, 923–933. 10.1016/j.cpr.2011.05.001 [DOI] [PubMed] [Google Scholar]
- Gyurak A, Gross JJ, & Etkin A (2011). Explicit and implicit emotion regulation: A dual-process framework. Cognition and Emotion, 25(3), 400–412. 10.1080/02699931.2010.544160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hallion LS, Tolin DF, Assaf M, Goethe J, & Diefenbach GJ (2017). Cognitive control in generalized anxiety disorder: Relation of inhibition impairments to worry and anxiety severity. Cognitive Therapy and Research, 41(4), 610–618. 10.1007/s10608-017-9832-2 [DOI] [Google Scholar]
- Hallion LS, Tolin DF, Billingsley AL, Kusmierski SN, & Diefenbach GJ (2019). “Cold” cognitive control and attentional symptoms in anxiety: Perceptions versus performance. Behavior Therapy. 10.1016/j.beth.2019.04.002 [DOI] [PubMed] [Google Scholar]
- Hampshire A, Chamberlain SR, Monti MM, Duncan J, & Owen AM (2010). The role of the right inferior frontal gyrus: Inhibition and attentional control. NeuroImage, 50(3), 1313–1319. 10.1016/J.NEUROIMAGE.2009.12.109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hester R, Fassbender C, & Garavan H (2004). Individual differences in error processing: A review and reanalysis of three event-related fMRI studies using the Go/NoGo task. Cerebral Cortex, 14(9), 986–994. 10.1093/cercor/bhh059 [DOI] [PubMed] [Google Scholar]
- Judah MR, Grat DM, Mills AC, & Lechner WV (2014). Factor structure and validation of the attentional control scale. Cognition and Emotion, 28, 433–451. 10.1080/02699931.2013.835254 [DOI] [PubMed] [Google Scholar]
- Judah MR, Saulnier KG, Hager NM, & Allan NP (2020). A bifactor model of the straightforward attentional control scale. Journal of Psychopathology and Behavioral Assessment, 42(1), 127–136. 10.1007/s10862-019-09737-y [DOI] [Google Scholar]
- Kelly AMC, Hester R, Murphy K, Javitt DC, Foxe JJ, & Garavan H (2004). Prefrontal-subcortical dissociations underlying inhibitory control revealed by event-related fMRI. European Journal of Neuroscience, 19(11), 3105–3112. 10.1111/j.0953-816X.2004.03429.x [DOI] [PubMed] [Google Scholar]
- Kessler RC, Petukhova M, Sampson NA, Zaslavsky AM, & Wittchen H-U (2012). Twelve-month and lifetime prevalence and lifetime morbid risk of anxiety and mood disorders in the United States. International Journal of Methods in Psychiatric Research, 21, 169–184. 10.1002/mpr.1359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ladouceur R, Gosselin P, & Dugas MJ (2000). Experimental manipulation of intolerance of uncertainty: A study of a theoretical model of worry. Behaviour Research and Therapy, 38, 933–941. 10.1016/S0005-7967(99)00133-3 [DOI] [PubMed] [Google Scholar]
- Macatee RJ, Albanese BJ, Allan NP, Schmidt NB, & Cougle JR (2016). Distress intolerance as a moderator of the relationship between daily stressors and affective symptoms: Tests of incremental and prospective relationships. Journal of Affective Disorders, 206, 125–132. 10.1016/j.jad.2016.07.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macatee RJ, Albanese BJ, Clancy K, Allan NP, Bernat EM, Cougle JR, & Schmidt NB (2018). Distress intolerance modulation of neurophysiological markers of cognitive control during a complex Go/No-Go task. Journal of Abnormal Psychology, 127(1), 12–29. 10.1037/abn0000323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer TJ, Miller ML, Metzger RL, & Borkovec TD (1990). Development and validation of the penn state worry questionnaire. Behaviour Research and Therapy, 28, 487–495. 10.1016/0005-7967(90)90135-6 [DOI] [PubMed] [Google Scholar]
- Mills AC, Grant DMM, Judah MR, White EJ, Taylor DL, & Frosio KE (2016). Trait attentional control influences the relationship between repetitive negative thinking and psychopathology symptoms. Psychiatry Research, 238, 277–283. 10.1016/j.psychres.2016.02.055 [DOI] [PubMed] [Google Scholar]
- Miskin C, Carvalho KS, Valencia I, Legido A, & Khurana DS (2015). EEG duration: The long and the short of it. Journal of Child Neurology, 30(13), 1767–1769. 10.1177/0883073815579969 [DOI] [PubMed] [Google Scholar]
- Moradi M, Fata L, Abhari AA, & Abbasi I (2014). Comparing attentional control and intrusive thoughts in obsessive-compulsive disorder, generalized anxiety disorder and nonclinical population. Iranian Journal of Psychiatry, 9(2), 69–75 [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, & Muthén BO (1998). Mplus user’s guide (Seventh). Muthén & Muthén. [Google Scholar]
- Naragon-Gainey K, & Watson D (2018). What lies beyond neuroticism? An examination of the unique contributions of social-cognitive vulnerabilities to internalizing disorders. Assessment, 25, 143–158. 10.1177/1073191116659741 [DOI] [PubMed] [Google Scholar]
- Newman MG, & Llera SJ (2011). A novel theory of experiential avoidance in generalized anxiety disorder: A review and synthesis of research supporting a contrast avoidance model of worry. Clinical Psychology Review, 31(3), 371–382. 10.1016/J.CPR.2011.01.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norr AM, Oglesby ME, Capron DW, Raines AM, Korte KJ, & Schmidt NB (2013). Evaluating the unique contribution of intolerance of uncertainty relative to other cognitive vulnerability factors in anxiety psychopathology. Journal of Affective Disorders, 151, 136–142. 10.1016/j.jad.2013.05.063 [DOI] [PubMed] [Google Scholar]
- Norton PJ, & Mehta PD (2007). Hierarchical model of vulnerabilities for emotional disorders. Cognitive Behaviour Therapy, 36, 240–254. 10.1080/16506070701628065 [DOI] [PubMed] [Google Scholar]
- Ouimet AJ, Gawronski B, & Dozois DJA (2009). Cognitive vulnerability to anxiety: A review and an integrative model. Clinical Psychology Review, 29, 459–470. 10.1016/j.cpr.2009.05.004 [DOI] [PubMed] [Google Scholar]
- Paulus MP (2015). Cognitive control in depression and anxiety: Out of control? Current Opinion in Behavioral Sciences. 10.1016/j.cobeha.2014.12.003 [DOI] [Google Scholar]
- Peers PV, & Lawrence AD (2009). Attentional control of emotional distraction in rapid serial visual presentation. Emotion, 9(1), 140–145. 10.1037/a0014507 [DOI] [PubMed] [Google Scholar]
- Podsakoff PM, MacKenzie SB, & Podsakoff NP (2012). Sources of method bias in social science research and recommendations on how to control it. Annual Review of Psychology, 63, 539–569. 10.1146/annurev-psych-120710-100452 [DOI] [PubMed] [Google Scholar]
- Posner MI, & Petersen SE (1990). The attention system of the human brain. Annual Review of Neuroscience, 13(1), 25–42. 10.1146/annurev.ne.13.030190.000325 [DOI] [PubMed] [Google Scholar]
- Posner MI, & Snyder CRR (2004). Attention and cognitive control. In: Balota DA & Marsh EJ (Eds.), Cognitive psychology: Key readings in cognition (pp. 205–223). New York, NY: Taylor & Francis Books, Inc. Retrieved March 26, 2021 from https://books.google.com/books?hl=en&lr=&id=DcJAqyCK6T8C&oi=fnd&pg=PA205&dq=cognitive+control&ots=q5vh-2i6DO&sig=HEqIEEYY8oEK6bGt7VZpoo2Qi7A#v=onepage&q=cognitivecontrol&f=false [Google Scholar]
- Schmidt NB, Capron DW, Raines AM, & Allan NP (2014). Randomized clinical trial evaluating the efficacy of a brief intervention targeting anxiety sensitivity cognitive concerns. Journal of Consulting and Clinical Psychology, 82, 1023–1033. 10.1037/a0036651 [DOI] [PubMed] [Google Scholar]
- Scholz U, La Marca R, Nater UM, Aberle I, Ehlert U, Hornung R, & Kliegel M (2009). Go no-go performance under psychosocial stress: Beneficial effects of implementation intentions. Neurobiology of Learning and Memory, 91(1), 89–92. 10.1016/j.nlm.2008.09.002 [DOI] [PubMed] [Google Scholar]
- Sexton KA, Norton PJ, Walker JR, & Ron Norton G (2005). Hierarchical model of vulnerabilities for anxiety: Replication and extension with a clinical sample. Cognitive Behaviour Therapy, 34, 50–63. 10.1080/16506070410005401 [DOI] [PubMed] [Google Scholar]
- Shihata S, McEvoy PM, Mullan BA, & Carleton RN (2016). Intolerance of uncertainty in emotional disorders: What uncertainties remain? Journal of Anxiety Disorders, 41, 115–124. 10.1016/j.janxdis.2016.05.001 [DOI] [PubMed] [Google Scholar]
- Simmonds DJ, Pekar JJ, & Mostofsky SH (2008). Meta-analysis of Go/No-go tasks demonstrating that fMRI activation associated with response inhibition is task-dependent. Neuropsychologia, 46(1), 224–232. 10.1016/J.NEUROPSYCHOLO-GIA.2007.07.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stefanopoulou E, Hirsch CR, Hayes S, Adlam A, & Coker S (2014). Are attentional control resources reduced by worry in generalized anxiety disorder? Journal of Abnormal Psychology, 123(2), 330–335. 10.1037/a0036343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Susa G, Pitică I, Benga O, & Miclea M (2012). The self regulatory effect of attentional control in modulating the relationship between attentional biases toward threat and anxiety symptoms in children. Cognition and Emotion, 26(6), 1069–1083. 10.1080/02699931.2011.638910 [DOI] [PubMed] [Google Scholar]
- Taylor CT, Cross K, & Amir N (2016). Attentional control moderates the relationship between social anxiety symptoms and attentional disengagement from threatening information. Journal of Behavior Therapy and Experimental Psychiatry, 50, 68–76. 10.1016/J.JBTEP.2015.05.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wells A (1995). Meta-cognition and worry: A cognitive model of generalized anxiety disorder. Behavioural and Cognitive Psychotherapy, 23(3), 301–320. 10.1017/S1352465800015897 [DOI] [Google Scholar]
- Wells A, & Matthews G (1996). Modelling cognition in emotional disorder: The S-REF model. Behaviour Research and Therapy, 34(11–12), 881–888. 10.1016/S0005-7967(96)00050-2 [DOI] [PubMed] [Google Scholar]
- Williams PG, Rau HK, Suchy Y, Thorgusen SR, & Smith TW (2017). On the validity of self-report assessment of cognitive abilities: Attentional control scale associations with cognitive performance, emotional adjustment, and personality. Psychological Assessment, 29(5), 519–530. 10.1037/pas0000361 [DOI] [PubMed] [Google Scholar]
- Wright L, Lipszyc J, Dupuis A, Thayapararajah SW, & Schachar R (2014). Response inhibition and psychopathology: A meta-analysis of Go/No-Go task performance. Journal of Abnormal Psychology, 123(2), 429–439. 10.1037/a0036295 [DOI] [PubMed] [Google Scholar]
- Yancey JR, Venables NC, & Patrick CJ (2016). Psychoneurometric operationalization of threat sensitivity: Relations with clinical symptom and physiological response criteria. Psychophysiology, 53(3), 393–405. 10.1111/psyp.12512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yook K, Kim K-H, Suh SY, & Lee KS (2010). Intolerance of uncertainty, worry, and rumination in major depressive disorder and generalized anxiety disorder. Journal of Anxiety Disorders, 24, 623–628. 10.1016/j.janxdis.2010.04.003 [DOI] [PubMed] [Google Scholar]
- Zainal NH, & Newman MG (2018). Executive function and other cognitive deficits are distal risk factors of generalized anxiety disorder 9 years later. Psychological Medicine, 48(12), 2045–2053. 10.1017/S0033291717003579 [DOI] [PMC free article] [PubMed] [Google Scholar]


