Abstract
COVID-19 is associated with marked morbidity and mortality. COVID-19 symptoms ranged from mild symptoms to severe pneumonia requiring admission to intensive care unit. Imperial College reported that, this second wave in Khartoum is expected to be similar to the first wave. The aim of our study was to study the characteristics and severity of COVID-19 among Sudanese patients during the waves of the pandemic.
A hospital-based analytical Cross-Sectional study assessed the characteristics of COVID-19 patients who attended Imperial Hospital since November 2020, Khartoum, Sudan. Data were collected, retrospectively, from the medical records of COVID-19 patients. The characteristics of the patients were recorded. The statistical package for social sciences (SPSS-23) was used to describe and analyze the data. Descriptive statistics and chi-square test were used; tests were considered statistically significant when p < 0.05.
Of the 138 participants, 75.4% were aged above 60 years. Males were 61.6%. Severe cases were 37.7%, with higher rate in the third wave (p = 0.000). Duration of hospitalization was ≤ 5 days in 60.9% of the cases, majority were from the 2nd wave (p = 0.001). Comorbidities of COVID-19 patients were more among non-severe cases (p = 0.001). COVID-19 symptoms were more prevalent in non-severe cases. Complications were more in severe cases (p = 0.000). Odds ratio of having ischemic stroke was 6.833 [95%CI: 2.092–22.321] based on COVID-19 severity.
The elderly population were the majority. More males were getting admitted. Atypical symptoms were reported beside the common symptoms. Wider multi-center studies are recommended in order to complete the big picture of COVID-19 in Sudan.
Keywords: COVID-19, Severity, Characteristics, Pandemic, Waves, SARS-COV-2, Sudan, Sudanese patients
Introduction
Corona viruses are RNA viruses, enclosed in a spiked envelope giving them an appearance similar to crowns. In the year of 2019, a new coronavirus has appeared. This new virus can cause “Severe Acute Respiratory Syndrome” thus referred to as (SARS-CoV-2). Chinese Scientists and the world health organization (WHO) called it COVID-19 [1,2] The WHO has declared this outbreak as a pandemic in March 2020 [3]. COVID-19 was originated in bats [2,4] then transferred to humans with the first spread from Wuhan, China [4]. The symptoms of COVID-19 range from mild symptoms resulting in fever, cough, shortness of breath and fatigue to severe pneumonia requiring admission to intensive care unit (ICU) and mechanical ventilation [5]. Gastro intestinal (GI) symptoms were also reported [6]. All community members are susceptible to COVID-19 infection, but the vulnerable populations are children, old aged people and pregnant women [7]. As well as, people with comorbidities especially diabetes, which was associated with COVID-19 severity [8]. COVID-19 is associated with marked morbidity and mortality related mostly to respiratory conditions [9]. Since the start of COVID-19 infected cases in December 2019, the disease had spread worldwide causing increasing fatalities daily [10]. Imperial College at the United Kingdom, reported that, this second wave in Khartoum is expected to be of the same size as the first wave [11]. In Sudan, the federal ministry of health had reported COVID-19 cases on daily bases (http://sho.gov.sd/corona/). In this study, severity of infection was defined based on the cases admission; general ward cases were the non-severe cases and ICU cases were the severe cases. The aim of our study was to describe and compare the characteristics and severity of COVID-19 infection among patients at different waves of the pandemic. We focused on infection severity because of its economic impact on healthcare system and on the families of the patients, beside the risk of mortality.
Materials and methods
A hospital-based analytical Cross-Sectional study was implemented to compare the characteristics of the patients and the disease at the second wave and the third wave of the pandemic. The study assessed the characteristics of COVID-19 patients who attended Imperial Hospital, as well as, the infection severity and complications. Based on the reports of the Federal Ministry of Health in Sudan (http://sho.gov.sd/corona/), infection rate had increased in November and December 2020 indicating the second wave of the pandemic. Then another peak occurred in April till May, 2021indicar the third peak in Khartoum, Sudan. Imperial Hospital is a 60 bed hospital containing three isolation wards, two of them are general isolation wards and one is an isolation intensive care unit (ICU), each of the general wards had 10 beds capacity, while the ICU had 8 beds capacity. Data were collected retrospectively, through an anonymous data collection sheet. Data were extracted from the medical records of COVID-19 patients hospitalized at the time of the data collection. Out of total COVID-19 admitted cases which were 179 cases, a sample of 138 files of adult COVID-19 patients was collected through stratified random sampling technique from the hospital registry. Files were divided into two strata based on the date of admission; second wave and third wave. The equation of sample size estimation used for each stratum was n = N/1+Nd2, where n is the estimated sample size, N, the total number of patients records, d the degree of accuracy set at 0.05. The total number of patients admitted during the second wave (from November to December, 2020) were 143 patients; out of which, 105 patients were randomly selected. The total number of patients admitted during the third wave (between April and May, 2021) were 36 patients; out of which, 33 patients were randomly selected. Characteristics of patients as age, gender, associated comorbidities were recorded. The statistical package for social sciences (SPSS version 23) was used to describe and analyze the data. Chi-square test was done to assess the differences between variables, it was considered statistically significant when p ≤ 0.05. Confidentiality of participants was assured through the use of an anonymous research tool. Informed consents from the patients/ surrogate decision makers were obtained, voluntary, by contacting them through their registered phone numbers. The collected data were used strictly for the purpose of the study objectives.
Results
Characteristics of COVID-19 patients
138 patients were involved in this study. 24.6% of the patients were aged 60 years or below, while 75.4% were aged more than 60 years. No statistically significant difference was found in the age between the patients admitted in the second wave and the patients admitted in the third wave (p = 0.687). Regarding gender, 61.6% of the patients were males and 38.4% were females with no statistically significant difference(p = 0.586) between second and third waves of the pandemic. Patients who had comorbid conditions were 65.9%. Of those, 85.7% were admitted during the second wave, while, 14.3% were admitted in the third wave (p = 0.000). Admission of patients was classified into two based on the infection severity; general isolation ward for non-severe cases and intensive care unit (ICU) for severe cases. 98.8% of the patients admitted to the general isolation ward were from the second wave of the pandemic, while, only 1.2% were from the third wave. In the other hand, 38.55 of the severe cases were from the second wave and 61.5% were from the third wave (p = 0.000). Complications of COVID-19 were reported; patients who suffered from COVID-19 complications were 20.3%. Of those patients, 32.1% were from the second wave and 67.95 from the third wave (p = 0.000). Duration of hospital stay was recorded in days, patients who had hospital stay of 5 days or less were 60.9% of all the patients and patients who had > 5 days of hospital stay were 39.1%. Of the 105 patients of the 2nd wave, 33 patients had > 5 days duration of hospital stay. In the other hand, of the 33 patients admitted in the 3rd wave, 21 patients had >5 days of hospital stay (p = 0.001). Table 1 below shows the details.
Table 1.
Demographic characteristics of COVID-19 patients (n = 138).
|
COVID-19 wave |
|||||||||
|---|---|---|---|---|---|---|---|---|---|
| Characteristics | Second wave | % | Third wave | % | Total | % | Chi2 | p-value | |
| Age in years | |||||||||
| ≤ 60 Years | 25 | 73.5 | 9 | 26.5 | 34 | 24.6 | 0.162 | 0.687 | |
| >60 Years | 80 | 76.9 | 24 | 23.1 | 104 | 75.4 | |||
| Total | 105 | 76.1 | 33 | 23.9 | 138 | 100.0 | |||
| Gender | |||||||||
| Male | 66 | 77.6 | 19 | 22.4 | 85 | 61.6 | 0.296 | 0.586 | |
| Female | 39 | 73.6 | 14 | 26.4 | 53 | 38.4 | |||
| Total | 105 | 76.1 | 33 | 23.9 | 138 | 100.0 | |||
| Comorbidities of COVID-19 patients | |||||||||
| Yes | 78 | 85.7 | 13 | 14.3 | 91 | 65.9 | 13.61 | 0.000* | |
| No | 27 | 57.4 | 20 | 42.6 | 47 | 34.1 | |||
| Total | 105 | 76.1 | 33 | 23.9 | 138 | 100.0 | |||
| Admission | |||||||||
| General ward | 85 | 98.8 | 1 | 1.2 | 86 | 62.3 | 64.92 | 0.000* | |
| Isolation ICU | 20 | 38.5 | 32 | 61.5 | 52 | 37.7 | |||
| Total | 105 | 76.1 | 33 | 23.9 | 138 | 100.0 | |||
| Complications of COVID-19 | |||||||||
| Yes | 9 | 32.1 | 19 | 67.9 | 28 | 20.3 | 37.28 | 0.000* | |
| No | 96 | 87.3 | 14 | 12.7 | 110 | 79.7 | |||
| Total | 105 | 76.1 | 33 | 23.9 | 138 | 100.0 | |||
| Duration of hospital stay | |||||||||
| ≤5 days | 72 | 85.7 | 12 | 14.3 | 84 | 60.9 | 10.94 | 0.001* | |
| > 5 days | 33 | 61.1 | 21 | 38.9 | 54 | 39.1 | |||
| Total | 105 | 76.1 | 33 | 23.9 | 138 | 100.0 | |||
*Statistically significant.
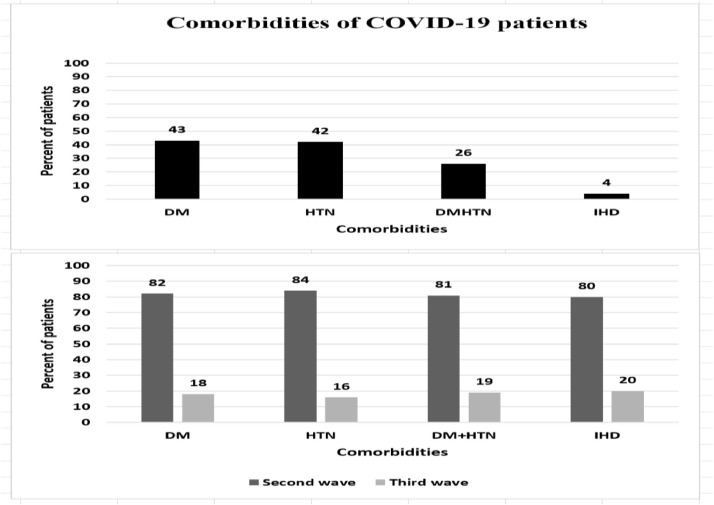
Comorbidities among COVID-19 patients
The most prevalent comorbidities were diabetes (DM) and hypertension (HTN) comprising 43% and 42% of participants, respectively. Of the diabetic patients, 82% were from the 2nd wave and 18% were from the 3rd wave (Chi2 =1.816, p = 0.178). While, among hypertensive patients, 84% were from the 2nd wave and 16% from the 3rd wave (Chi2 =3.876, p = 0.049). Patients who had both DM and hypertension were 26% and of those, 81% were from the 2nd wave and 19% from the 2nd wave (Chi2 =0.535, p = 0.465). Only 4% of the patients had ischemic heart disease (IHD), 80% of them from the 2nd wave, while 20% were from the 3rd wave (Chi2 =0.044, p = 0.834), Fig. 1 .
Fig. 1.
Comorbidities among COVID-19 patients.
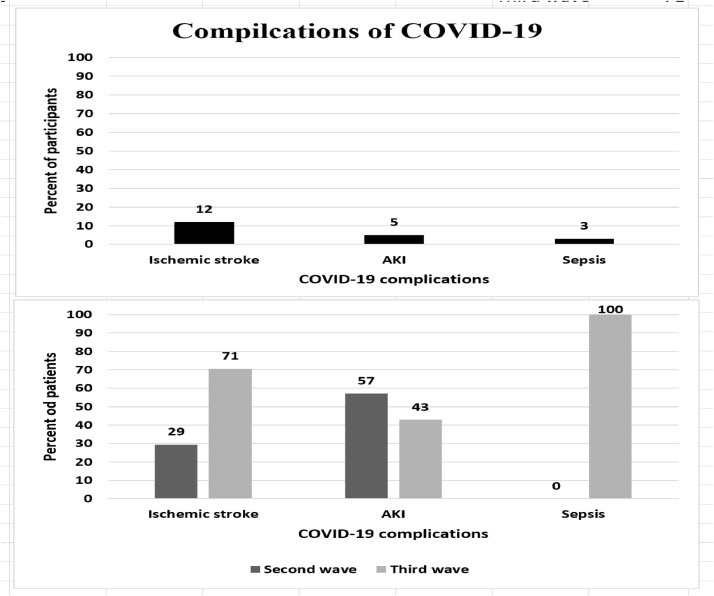
Complications of COVID-19 among patients
Only 20.3% of the COVID-19 patients developed complications. 12% of all the study participants had developed ischemic stroke, 71% of them were from the 3rd wave, while, only 29% were from the second wave (chi2= 23.215, p = 0.000). Acute kidney injury (AKI) was reported in 5% of all the patients, 57% from the second wave and 43% of the third wave (chi2 = 1.454, p = 0.228). In the other hand, sepsis was reported in 3% of the patients and all were from the third wave (Chi2 = 13,107, p = 0.000). Fig. 2 below illustrates the details.
Fig. 2.
COVID-19 complications among patients.
Assessment of COVID-19 characteristics and severity
Severity of the patient status was assessed based on the admission, general ward admission was for the non-severe cases, while, severe cases were admitted to the ICU.COVID-19 symptoms and complications were assessed with regards to severity. As well as characteristics of patients were assessed based on severity status.
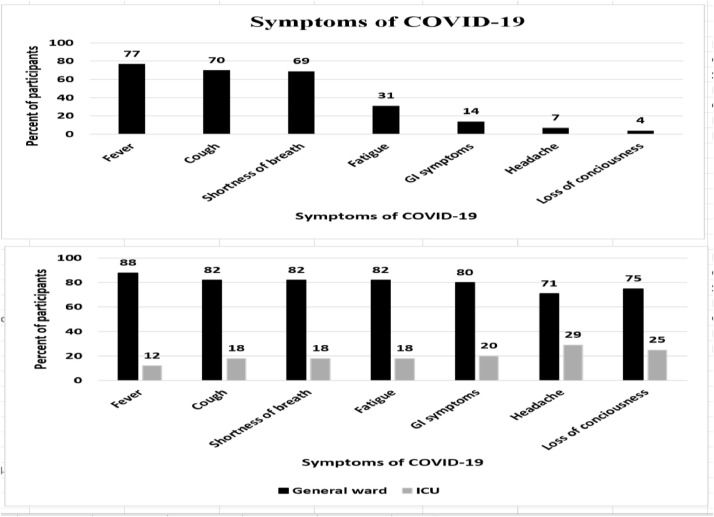
Symptoms of COVID-19 among patients based on severity of infection
Fever was the most prevalent symptom (77%); especially among the non-severe cases (88%) of the patients in the general ward (Chi2= 10.323, p = 0.001). Cough was the second frequently reported symptom (70%). Although, it was mostly prevalent in non-severe cases, no statistically significant difference was found between severe and non-severe cases (Chi2 = 0.356, p = 0.551). The third prevalent symptom reported was shortness of breath (69%), followed by fatigue (31%), gastro-intestinal (GI) symptoms (14%), headache (7%) and loss of consciousness (4%). All of these symptoms had no statistically significant difference between severe and non-severe cases (p > 0.05), Fig. 3 .
Fig. 3.
Symptoms of COVID-19 among patients.
Association between COVID-19 characteristics and severity
Characteristics of patients were assessed with regards to severity of COVID-19 infection. Both age and gender had no statistically significant difference between severe and non-severe cases (p > 0.05). Interestingly, comorbidities were more prevalent in the non-severe cases (74.7%, 65/87) than the severe cases (p = 0.001). In the other hand, COVID-19 complications were more prevalent ibn the severe cases (71.4%, 20/28) than the non-severe cases (p = 0.000). With regards to the duration of hospital stay, most of the cases (72.6%, 61/84) with short duration of stay (≤ 5 days) were non-severe cases. In the other hand, 53.7 (29/54) of the cases with longer duration of stay (> 5 days) were severe cases (p = 0.002). Table 2 below illustrates the results.
Table 2.
Association between COVID-19 characteristics and severity of infection (n = 138).
|
Severity |
||||||||
|---|---|---|---|---|---|---|---|---|
| Characteristics | Non-Severe | % | Severe | % | Total | % | Chi2 | p-value |
| Age in years | ||||||||
| ≤ 60 Years | 19 | 55.9 | 15 | 44.1 | 34 | 24.6 | 0.796 | 0.372 |
| > 60 Years | 67 | 64.4 | 37 | 35.6 | 104 | 75.4 | ||
| Total | 86 | 62.3 | 52 | 37.7 | 138 | 100.0 | ||
| Gender | ||||||||
| Male | 56 | 65.9 | 29 | 34.1 | 85 | 61.6 | 0.274 | 0.285 |
| Female | 30 | 56.6 | 23 | 43.4 | 53 | 38.4 | ||
| Total | 86 | 62.3 | 52 | 37.7 | 138 | 100.0 | ||
| Comorbidities among participants | ||||||||
| Yes | 65 | 74.7 | 22 | 25.3 | 87 | 63.0 | 11.851 | 0.001* |
| No | 20 | 44.4 | 25 | 55.6 | 45 | 32.6 | ||
| Total | 85 | 64.4 | 47 | 35.6 | 132 | 95.7 | ||
| Complications of COVID-19 | ||||||||
| Yes | 8 | 28.6 | 20 | 71.4 | 28 | 20.3 | 17.03 | 0.000* |
| No | 78 | 70.9 | 32 | 29.1 | 110 | 79.7 | ||
| Total | 86 | 62.3 | 52 | 37.7 | 138 | 100.0 | ||
| Duration of hospital stay | ||||||||
| ≤ 5 days | 61 | 72.6 | 23 | 27.4 | 84 | 60.9 | 9.699 | 0.002* |
| > 5 days | 25 | 46.3 | 29 | 53.7 | 54 | 39.1 | ||
| Total | 86 | 62.3 | 52 | 37.7 | 138 | 100.0 | ||
*Statistically significant.
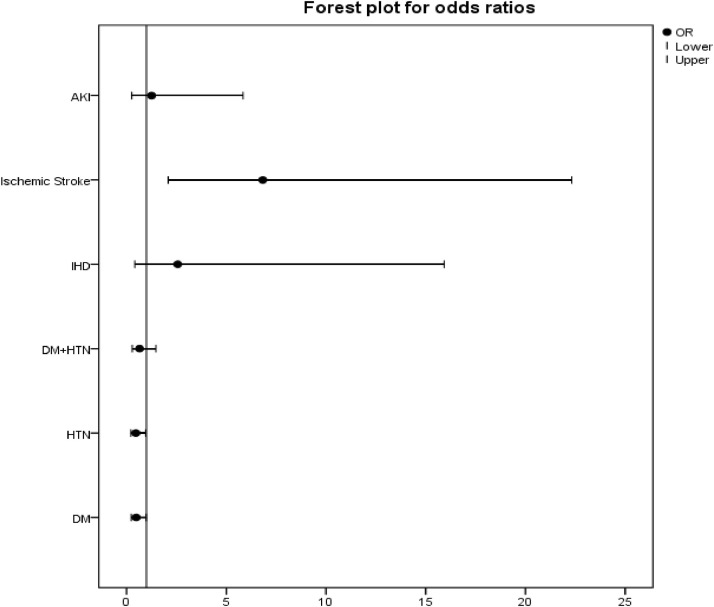
Comorbidities and COVID-19 complications related to infection severity
On detailing the comorbidities and complications in relation to infection severity, DM had an odds ratio of 0.486 being more prevalent in non-severe cases (p = 0.047). As well as, HTN (p = 0.037) with odds ratio of 0.466, other comorbidities had no statistically significant difference between severe and non-severe cases (p > 0.05), Table 3 , Fig. 4 . On assessing complications related to COVID-19 infection, ischemic stroke had odds ratio= 6.833 being more prevalent in severe cases (p = 0.000). Sepsis was reported for severe cases only (p = 0.009). Table 3 and Fig. 4 below show the details.
Table 3.
Association of comorbidities and complications to COVID-19 severity.
|
Severity |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Factors | Non-Severe | % | Severe | % | Total | % | Chi2 | p-value | OR (95%CI) | ||
| DM | |||||||||||
| Yes | 43 | 71.7 | 17 | 28.3 | 60 | 43.5 | 3.95 | 0.047* | 0.486 (0.237–0.995) | ||
| No | 43 | 55.1 | 35 | 44.9 | 78 | 56.5 | |||||
| Total | 86 | 62.3 | 52 | 37.7 | 138 | 100.0 | |||||
| HTN | |||||||||||
| Yes | 42 | 72.4 | 16 | 27.6 | 58 | 42.0 | 4.342 | 0.037* | 0.466 (0.226–0.961) | ||
| No | 44 | 55.0 | 36 | 45.0 | 80 | 58.0 | |||||
| Total | 86 | 62.3 | 52 | 37.7 | 138 | 100.0 | |||||
| DM+HTN | |||||||||||
| Yes | 25 | 69.4 | 11 | 30.6 | 36 | 26.1 | 1.053 | 0.305 | 0.655 (0.291–1.475) | ||
| No | 61 | 59.8 | 41 | 40.2 | 102 | 73.9 | |||||
| Total | 86 | 62.3 | 52 | 37.7 | 138 | 100.0 | |||||
| IHD | |||||||||||
| Yes | 2 | 40.0 | 3 | 60.0 | 5 | 3.6 | 1.101 | 0.294 | 2.571 (0.415–15.927) | ||
| No | 84 | 63.2 | 49 | 36.8 | 133 | 96.4 | |||||
| Total | 86 | 62.3 | 52 | 37.7 | 138 | 100.0 | |||||
| AKI | |||||||||||
| Yes | 4 | 57.1 | 3 | 42.9 | 7 | 5.1 | 0.084 | 0.772 | 1.255 (0.27–5.844) | ||
| No | 82 | 62.6 | 49 | 37.4 | 131 | 94.9 | |||||
| Total | 86 | 62.3 | 52 | 37.7 | 138 | 100.0 | |||||
| Ischemic stroke | |||||||||||
| Yes | 4 | 23.5 | 13 | 76.5 | 17 | 12.3 | 12.42 | 0.000* | 6.833 (2.092–22.321) | ||
| No | 82 | 67.8 | 39 | 32.2 | 121 | 87.7 | |||||
| Total | 86 | 62.3 | 52 | 37.7 | 138 | 100.0 | |||||
| Sepsis | |||||||||||
| Yes | 0 | 0.0 | 4 | 100.0 | 4 | 2.9 | 6.813 | 0.009* | |||
| No | 86 | 64.2 | 48 | 35.8 | 134 | 97.1 | |||||
| Total | 86 | 62.3 | 52 | 37.7 | 138 | 100.0 | |||||
*Statistically significant.
Fig. 4.
Forest plot of the odds ratios of comorbidities and complications related to infection severity (n = 138).
Discussion
The emergence of COVID-19 pandemic has represented a major crisis for populations around the world. Unfortunately, there is no enough published reports from Sudan and details about disease characteristics, severity, mortality and associated comorbidities remain unclear. Therefore, our study has examined the characteristic of COVID-19 disease during the waves of pandemic in Sudan. In this study, we found the majority of COVID-19 cases were males (61.6%), which could be attributed to the higher proportion of males during the second surge (77.6%), this was consistent with Fang et al. systematic review reporting increased percentages as high as 83% [12]. With regard to the third wave, there were no sex differences found in the number of cases and males comprised (57.6%, 19/33), giving almost equal percentages of males and females. Another meta-analysis study reported that males comprised 60% of COVID-19 patients [13]. Remarkably, 75.4% of our patients were elderly, aged more than 60 years that was in line with Fang et al. [12]. Compared with previous studies, a higher percentage of our hospitalized patients required ICU admission. 37.7% required ICU care compared with proportions of 5% up to 31.7% of patients mentioned in previous reports [14,15]. When assessing severity based on COVID-19 waves, the third wave had a very high percentage of ICU admission (61.5%) compared to the second wave (38.5%), p = 0.000. Both males and females in this study required ICU care with higher percentage among females (43.4%) more than males (34.1%), contradictory to a previous study [16], Gulati et al. reported that more males required ICU care. According to our data, the prevalence of COVID-19 infection was linked to underlying comorbidities, the most common of which was DM (43%) followed by HTN (42%). The majority of patients admitted to Imperial Hospital (65.9%) had co-morbidities and this percentage was notably higher than the percentage reported by Thai et al. where comorbidities were found to be 11.3% of their patients [15]. As in previous studies, 26% of all patients had both diabetes and Hypertension [12, 17]. On the other hand, around 40% of our study participants had either DM or HTN, and this percentage was higher than the findings reported in previously published study [14]. The most frequently reported COVID-19 symptoms were fever (77%), which agrees with the findings published in previous studies [1,13,[18], [19], [20]]. Moreover, cough was prevalent in 70% of our patients and this was almost similar to what recently reported by Gulati et al. and Tian et al. where 68.0% of COVID-19 patients had cough [16,20]. Harapan et al. described a higher prevalence with 81% of patients presenting with cough [18]. Furthermore, Shortness of breath was one of the most frequent clinical symptoms in our study (69%), this was higher than what previously published with percentages ranging from 18.6% to 55% [14]. Approximately 31.4% of our patients complained of fatigue in contrast to the published data. Describing fatigue as one of the most frequent symptoms (38.1% to 69.6%). The incidence of atypical GI symptoms such as vomiting, diarrhea and loss of appetite, was calculated as 14% in our study patients, consistent with previous studies [21,22], contrary to other studies indicated that GI symptoms were not as common [1,13,23]. All symptoms had no statistically significant difference in prevalence among severe and non-severe cases (p > 0.05), except for fever; it was more prevalent in non-severe cases with a statistically significant difference (p = 0.001). On assessing the complications associated with COVID-19 infection, acute kidney injury and ischemic stroke were reported among the two waves, as in many studies [22,[24], [25], [26], [27]]. 12% of our patients had developed ischemic stroke and this incidence was higher than ranges reported (0.9–2.7%, 8%) [28,29]. Interestingly, prevalence of ischemic stroke differed drastically between the second and third waves (29% and 71%), respectively (p = 0.000). As well as, sepsis had prevailed in patients of the third wave only (p = 0.000). In our study, 5% of patients had developed AKI, this was much lower than the incidence reported in study [25], in which, 46% of patients had developed AKI. As for the duration of hospital stay among our patients, 60.9% had duration of 5 days or less, this was much lower than the documented median duration of hospitalization (21 days) in a published study [15]. The novelty in this paper is that it studied a population that is unknown for the international scientific field. Sudanese population are understudied during the COVID-19 pandemic. Advances that have been done in our research were the analytical approach of comparing different COVID-19 surges to describe and assess changes in infection pattern through time. The limitations of this study included the retrospective nature of data collection; as this method depends on the quality of documentation. The study was a single-center study conducted at Imperial Hospital with a potential of selection bias.
Conclusions
Compared to other studies, COVID-19 pattern is changing in Sudan. The observed variations in patients’ characteristics were mainly in hospital and ICU admission of COVID-19 cases that has showed a significant increase. Elderly patients represented the majority of the study population. Nevertheless, the severity of infection had no statistically significant association to this age group. More males were getting admitted to Imperial Hospital during the second wave of COVID-19, but in the third wave, the admission rate was almost equal among males and females. In Sudan, infection severity had no statistically significant difference between males and females (p > 0.05). Of importance that, complications of COVID-19, ischemic stroke and sepsis, were more prevalent in ICU patients. No statistically significant association was found between symptoms and severity of COVID-19 infection.
Recommendations
Overall there are enormous clinical and academic efforts required to face the challenge of COVID-19. Wider multi-center studies similar to this one are recommended in order to complete the big picture of COVID-19 in Sudan and to shed light on the health effects associated with the pandemic. Our study provides essential information on patterns and characteristics of COVID-19 disease and associated mortality in Sudan. Despite all study limitations appointed, we are confident that our findings can serve as an informative starting point for further studies when data are available from a wide range of healthcare providers. During these pandemic waves, there were no significant demographic differences in the population and no statistically significant association to a specific age group or gender. These findings call for continuous efforts to prevent the transmission of COVID-19 by compliance with the preventive measures and the facilitation of vaccination coverage among the Sudanese population. In addition, complications of COVID-19 must be well addressed in order to manage them properly. Challenges to healthcare systems and concerned organizations will be; increasing the COVID-19 infection awareness and updating the knowledge of the community about the atypical presentations of this infection. The main goal should be to reduce ICU admission rate among COVID-19 cases in Sudan. All those issues are very sensitive in a country like Sudan. Like most African countries, the health sector is under-funded with a low government health expenditure resulting in poor healthcare services provided in Sudan .In order to aid the national authorities towards control of the pandemic in Sudan and to prevent the emergence of future outbreaks, consistent and regulated surveillance of COVID-19 infection is essential to obtain the necessary data.
Declarations
Ethics approval and consent to participate
Approval was firstly obtained from the Medical administration of Imperial Hospital. The study proposal was then submitted to the Administration of Innovation and Scientific Research at the State Ministry of Health (MOH), Khartoum. Expedited review was conducted by the IRB of the MOH and approval was granted. Another copy of the proposal was submitted to the Administration of Private Medical Facilities. Regarding participants, the data were collected retrospectively from the medical records. Confidentiality of participants was assured through the use of an anonymous research tool. Informed consents from the patients / surrogate decision makers were obtained, voluntary, by contacting them through their registered phone numbers. The collected data were used strictly for the purpose of the study objectives.
Consent for publication
All authors have read the final manuscript and gave their consent for the article to be published in this journal. No clinical details of participants that might compromise their anonymity were used in the development of this manuscript titled “Characteristics and Severity of COVID-19 among Sudanese patients during the waves of the pandemic“.
Availability of supporting data
All supporting data are available.
Funding
The authors bore all the costs related to the study.
Authors' contributions
All authors have read the final manuscript and gave their approval for publication.
GOHA: Conceptualization, Data curatiion, Methodology, Project administration, Formal Analysis, software, Writing original draft.
DSIM: Conceptualization, Data Curation, Investigation, Resources.
MAAY: Data Curation, Investigation, original draft writing.
HESE: Validation, Visualization, Review and editing.
CRediT authorship contribution statement
Ghada Omer Hamad Abd El-Raheem: Conceptualization, Data curation, Methodology, Project administration, Formal analysis, Writing – original draft. Doaa Salih Ibrahim Mohamed: Conceptualization, Data curation, Investigation, Resources. Maysoun Ahmed Awad Yousif: Data curation, Investigation, Writing – original draft. Hind Eltayeb Salih Elamin: Validation, Visualization, Writing – review & editing.
Declaration of Competing Interest
The authors declared no competing interest.
Acknowledgments
The authors are grateful to Shurouq O. H. Abdelraheem, Faculty of Engineering, University of Khartoum for her assistance in the data entry process. The authors also acknowledge the cooperation of the departments of Imperial Hospital during the data collection.
Editor: DR B Gyampoh
Footnotes
Edited by B Gyampoh.
References
- 1.Esakandari H., Nabi-Afjadi M., Fakkari-Afjadi J., Farahmandian N., Miresmaeili S.M., Bahreini E. A comprehensive review of COVID-19 characteristics. Biol. Proced. Online. 2020;22:19. doi: 10.1186/s12575-020-00128-2. Aug 4PMID: 32774178; PMCID: PMC7402395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yuen K.S., Ye Z.W., Fung S.Y., Chan C.P., Jin D.Y. SARS-CoV-2 and COVID-19: the most important research questions. Cell Biosci. 2020;10:40. doi: 10.1186/s13578-020-00404-4. Mar 16PMID: 32190290; PMCID: PMC7074995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Valencia D.N. Brief review on COVID-19: the 2020 pandemic caused by SARS-CoV-2. Cureus. 2020;12(3):e7386. doi: 10.7759/cureus.7386. Mar 24PMID: 32337113; PMCID: PMC7179986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Singhal T. A review of coronavirus disease-2019 (COVID-19) Indian J. Pediatr. 2020;87(4):281–286. doi: 10.1007/s12098-020-03263-6. AprEpubMar 13PMID: 32166607; PMCID: PMC7090728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Patel U., Malik P., Mehta D., Shah D., Kelkar R., Pinto C., Suprun M., Dhamoon M., Hennig N., Sacks H. Early epidemiological indicators, outcomes, and interventions of COVID-19 pandemic: a systematic review. J. Glob. Health. 2020;10(2) doi: 10.7189/jogh.10.020506. DecPMID: 33110589; PMCID: PMC7567430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Velavan T.P., Meyer C.G. The COVID-19 epidemic. Trop. Med. Int. Health. 2020;25(3):278–280. doi: 10.1111/tmi.13383. MarEpubFeb 16PMID: 32052514; PMCID: PMC7169770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tu H., Tu S., Gao S., Shao A., Sheng J. Current epidemiological and clinical features of COVID-19; a global perspective from China. J. Infect. 2020;81(1):1–9. doi: 10.1016/j.jinf.2020.04.011. JulEpub 2020 Apr 18. PMID: 32315723; PMCID: PMC7166041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kumar A., Arora A., Sharma P., Anikhindi S.A., Bansal N., Singla V., Khare S., Srivastava A. Is diabetes mellitus associated with mortality and severity of COVID-19? A meta-analysis. Diabetes Metab. Syndr. 2020;14(4):535–545. doi: 10.1016/j.dsx.2020.04.044. Jul-AugEpub 2020 May 6. PMID: 32408118; PMCID: PMC7200339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Geier M.R., Geier D.A. Respiratory conditions in coronavirus disease 2019 (COVID-19): important considerations regarding novel treatment strategies to reduce mortality. Med. Hypotheses. 2020;140 doi: 10.1016/j.mehy.2020.109760. JulEpub 2020 Apr 22. PMID: 32344310; PMCID: PMC7175905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McArthur L., Sakthivel D., Ataide R., Chan F., Richards J.S., Narh C.A. Review of burden, clinical definitions, and management of COVID-19 cases. Am. J. Trop. Med. Hyg. 2020;103(2):625–638. doi: 10.4269/ajtmh.20-0564. AugEpub 2020 Jul 1. PMID: 32618260; PMCID: PMC7410412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Watson O.J., Abdelmagid N., Ahmed A., et al. Imperial College London; 2020. Characterising COVID-19 Epidemic Dynamics and Mortality Underascertainment in Khartoum, Sudan. 01-12- [DOI] [Google Scholar]
- 12.Fang X., Li S., Yu H., Wang P., Zhang Y., Chen Z., Li Y., Cheng L., Li W., Jia H., Ma X. Epidemiological, comorbidity factors with severity and prognosis of COVID-19: a systematic review and meta-analysis. Aging. 2020;12(13):12493–12503. doi: 10.18632/aging.103579. (Albany NY)Jul 13Epub 2020 Jul 13. PMID: 32658868; PMCID: PMC7377860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Li L.Q., Huang T., Wang Y.Q., Wang Z.P., Liang Y., Huang T.B., Zhang H.Y., Sun W., Wang Y. COVID-19 patients' clinical characteristics, discharge rate, and fatality rate of meta-analysis. J. Med. Virol. 2020;92(6):577–583. doi: 10.1002/jmv.25757. JunEpub 2020 Mar 23. PMID: 32162702; PMCID: PMC7228329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tang D., Comish P., Kang R. The hallmarks of COVID-19 disease. PLoS Pathog. 2020;16(5) doi: 10.1371/journal.ppat.1008536. May 22PMID: 32442210; PMCID: PMC7244094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Thai P.Q., Toan D.T.T., Son D.T., Van H.T.H., Minh L.N., Hung L.X., Toan N.V., Hoat L.N., Luong D.H., Khue L.N., Khoa N.T., Huong L.T. Factors associated with the duration of hospitalisation among COVID-19 patients in Vietnam: a survival analysis. Epidemiol. Infect. 2020;148:e114. doi: 10.1017/S0950268820001259. Jun 10PMID: 32517822; PMCID: PMC7306545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gulati A., Pomeranz C., Qamar Z., Thomas S., Frisch D., George G., Summer R., DeSimone J., Sundaram B. A comprehensive review of manifestations of novel coronaviruses in the context of deadly COVID-19 global pandemic. Am. J. Med. Sci. 2020;360(1):5–34. doi: 10.1016/j.amjms.2020.05.006. JulEpub 2020 May 11PMID: 32620220; PMCID: PMC7212949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sun P., Lu X., Xu C., Sun W., Pan B. Understanding of COVID-19 based on current evidence. J. Med. Virol. 2020;92(6):548–551. doi: 10.1002/jmv.25722. JunEpub 2020 Mar 5PMID: 32096567; PMCID: PMC7228250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Harapan H., Itoh N., Yufika A., Winardi W., Keam S., Te H., Megawati D., Hayati Z., Wagner A.L., Mudatsir M. Coronavirus disease 2019 (COVID-19): a literature review. J. Infect. Public Health. 2020;13(5):667–673. doi: 10.1016/j.jiph.2020.03.019. MayEpub 2020 Apr 8. PMID: 32340833; PMCID: PMC7142680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lake M.A. What we know so far: COVID-19 current clinical knowledge and research. Clin. Med. 2020;20(2):124–127. doi: 10.7861/clinmed.2019-coron. (Lond)MarEpub 2020 Mar 5PMID: 32139372; PMCID: PMC7081812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tian S., Hu N., Lou J., Chen K., Kang X., Xiang Z., Chen H., Wang D., Liu N., Liu D., Chen G., Zhang Y., Li D., Li J., Lian H., Niu S., Zhang L., Zhang J. Characteristics of COVID-19 infection in Beijing. J. Infect. 2020;80(4):401–406. doi: 10.1016/j.jinf.2020.02.018. AprEpub 2020 Feb 27. PMID: 32112886; PMCID: PMC7102527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Musa A., Pendi K., Hashemi A., Warbasse E., Kouyoumjian S., Yousif J., Blodget E., Stevens S., Aly B., Baron D.A. Remdesivir for the treatment of COVID-19: a systematic review of the literature. West J. Emerg. Med. 2020;21(4):737–741. doi: 10.5811/westjem.2020.5.47658. May 20PMID: 32726230; PMCID: PMC7390571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lai C.C., Ko W.C., Lee P.I., Jean S.S., Hsueh P.R. Extra-respiratory manifestations of COVID-19. Int. J. Antimicrob. Agents. 2020;56(2) doi: 10.1016/j.ijantimicag.2020.106024. AugEpub 2020 May 22. PMID: 32450197; PMCID: PMC7243791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Azwar M.K., Kirana F., Kurniawan A., Handayani S., Setiati S. Gastrointestinal presentation in COVID-19 in Indonesia: a case report. Acta Med. Indones. 2020;52(1):63–67. JanPMID: 32291373. [PubMed] [Google Scholar]
- 24.Hess D.C., Eldahshan W., Rutkowski E. COVID-19-related stroke. Transl. Stroke Res. 2020;11(3):322–325. doi: 10.1007/s12975-020-00818-9. JunEpub 2020 May 7. PMID: 32378030; PMCID: PMC7202903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chan L., Chaudhary K., Saha A., Chauhan K., Vaid A., Zhao S., Paranjpe I., Somani S., Richter F., Miotto R., Lala A., Kia A., Timsina P., Li L., Freeman R., Chen R., Narula J., Just A.C., Horowitz C., Fayad Z., Cordon-Cardo C., Schadt E., Levin M.A., Reich D.L., Fuster V., Murphy B., He J.C., Charney A.W., Böttinger E.P., Glicksberg B.S., Coca S.G., Nadkarni G.N. Mount Sinai COVID informatics center (MSCIC), Li L. AKI in hospitalized patients with COVID-19. J. Am. Soc. Nephrol. 2020 doi: 10.1681/ASN.2020050615. Sep 3:ASN.2020050615Epub ahead of printPMID: 32883700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Avula A., Nalleballe K., Narula N., Sapozhnikov S., Dandu V., Toom S., Glaser A., Elsayegh D. COVID-19 presenting as stroke. Brain Behav. Immun. 2020;87:115–119. doi: 10.1016/j.bbi.2020.04.077. JulEpub 2020 Apr 28PMID: 32360439; PMCID: PMC7187846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Qi X., Keith K.A., Huang J.H. COVID-19 and stroke: a review. Brain Hemorrhages. 2020 doi: 10.1016/j.hest.2020.11.001. Nov 17Epub ahead of printPMID33225251PMCID: PMC7670261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tan Y.K., Goh C., Leow A.S.T., Tambyah P.A., Ang A., Yap E.S., Tu T.M., Sharma V.K., Yeo L.L.L., Chan B.P.L., Tan B.Y.Q. COVID-19 and ischemic stroke: a systematic review and meta-summary of the literature. J. Thromb. Thrombolysis. 2020;50(3):587–595. doi: 10.1007/s11239-020-02228-y. OctPMID: 32661757; PMCID: PMC7358286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Berger J.R. COVID-19 and the nervous system. J. Neurovirol. 2020;26(2):143–148. doi: 10.1007/s13365-020-00840-5. AprEpub 2020 May 23. PMID: 32447630; PMCID: PMC7245181. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All supporting data are available.
Funding
The authors bore all the costs related to the study.