Abstract
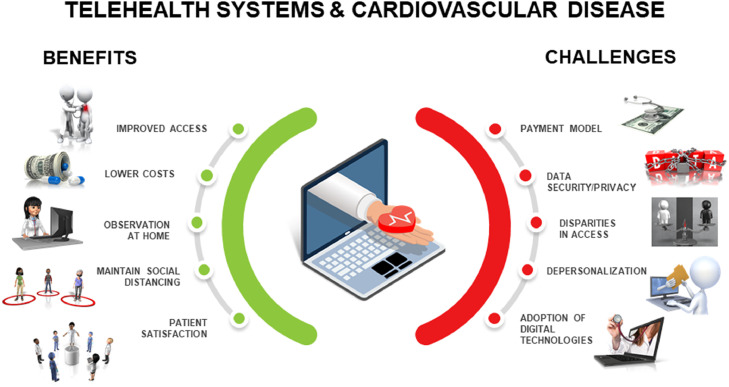
Before the coronavirus disease 2019 (COVID-19) pandemic, use of telehealth services had been limited in cardiovascular care. Potential benefits of telehealth include improved access to care, more efficient care management, reduced costs, the ability to assess patients within their homes while involving key caretakers in medical decisions, maintaining social distance, and increased patient satisfaction. Challenges include changes in payment models, issues with data security and privacy, potential depersonalization of the patient-clinician relationship, limitations in the use of digital health technologies, and the potential impact on disparities, including socioeconomic, gender, and age-related issues and access to technology and broadband. Implementation and expansion of telehealth from a policy and reimbursement practice standpoint are filled with difficult decisions, yet addressing these are critical to the future of health care.
Keywords: Cardiology, Cardiovascular disease, Health Policy, Telehealth, Telemedicine
Clinical Significance.
-
•
Prior to the coronavirus disease 2019 (COVID-19) pandemic, use of telehealth services has been limited in cardiovascular care.
-
•
Modalities available for implementing telehealth, the potential benefits of telehealth use, and several challenges in telehealth implementation in cardiovascular care are discussed.
-
•
Implementation and expansion of telehealth are fraught with difficult decisions, yet addressing these are critical to the future of health care, especially in light of the current pandemic.
Alt-text: Unlabelled box
“The COVID-19 pandemic and accompanying relaxation of regulatory barriers has occasioned an explosion in telemedicine use, vaulting it to the center of health care delivery.”—Newton N. Minow and Rick Boucher1
Introduction
The coronavirus disease 2019 (COVID-19) pandemic has impacted global economies and brought about unprecedented challenges to health care systems. Much of the morbidity and mortality of the pandemic has been borne by those with underlying medical conditions, including cardiovascular disease.2 , 3 Efforts to limit the spread of this viral illness, particularly within vulnerable populations through social distancing, resulted in rapid conversion from office-based visits to virtual visits. This transition also accelerated the adoption of telehealth services in the outpatient management of cardiovascular disease.
Before the COVID-19 pandemic, use of telehealth services had been limited in cardiovascular care. Reasons for this included lack of infrastructure, restrictions placed by insurance and government agencies, and limited reimbursement. Remote monitoring of vital signs and cardiac rhythm transmissions from mobile health devices had been modestly employed. Although these modalities did improve access for patients, infrastructural redesign was needed.
Established Platforms and Modalities Before COVID-19
Although used interchangeably, the terms “telehealth” and “telemedicine” should be distinguished. Telehealth is a broad, all-encompassing term that leverages the use of telecommunication services for the education, monitoring, and treatment of individuals. Telemedicine is a subset of telehealth that involves a clinician or health care professional using these telecommunication services to provide a more direct health service to patients. There are several methods for providing telehealth care. The 2 main categories under which telehealth services typically fall are direct-to-patient and clinician-to-clinician platforms.4
Direct-to-patient platforms include audiovisual telemedicine visits and may include remote patient monitoring.4 Remote patient monitoring (such as electrocardiogram [ECG] strips from a patient's Apple Watch) may be used during a telemedicine visit (synchronous) or between in-person visits (asynchronous).
Clinician-to-clinician or clinician-to-facility platforms, on the other hand, include asynchronous (“store and forward”) data transmission, remote clinicians providing tele-intensive care unit or inpatient care at a distance (via video, electronic health record [EHR], monitor data), and electronic consultations (e-consults) from specialists to distant clinicians.4 This may include electronic transmission of medical information and patient data such as diagnostic images, videos, documents, among other data.5 In the Massachusetts General Hospital's cardiology e-consult pilot, cardiologists reviewed patient's electronic data and images in the shared electronic medical record and provided detailed clinical recommendations without a cardiology office visit. Over 5 months, only 14.1% of consult requests resulted in an office visit because the question was not answerable by e-consult. Of the recommendations made by the consultant, 81.3% were implemented by the referring clinician. A total of 100% of clinicians endorsed the helpfulness of e-consults, and 77.8% believed the e-consult averted the need for a traditional in-person visit for their patients. Of the patients interviewed, 96.7% were “very satisfied” with the convenience of receiving a clinical recommendation without needing to visit with the cardiologist.6 When looking at e-consult volume for all specialties at their institution before the World Health Organization declared COVID-19 to be a pandemic on March 11, 2020, compared with those afterward, they found a significant absolute increase in e-consult proportion from 8.5% to 19.6% over ambulatory consults.7
Potential Benefits of Telehealth
Improved Access and Care Benefits
One of the main advantages of telehealth is the potential for a marked improvement in access (Table ; Figure ). In particular, telehealth affords options to patients with limited reliable transportation, financial or mobility constraints, or those who live in remote or rural areas.8 A systematic review of 44 studies that explored the association of telehealth with patient satisfaction noted that telehealth is capable of providing high-quality service, increased accessibility to care, and engages patients in shared decision-making related to the management of their chronic conditions.9
Table.
Potential Benefits and Logistical Challenges of Telehealth
| Benefits | Challenges |
|---|---|
Improved Access to Care
|
Payment Models
|
Reduced Costs
|
Data Security and Privacy
|
Assessing Patients Within Their Home
|
Potential Impact on Disparities
|
Maintain Social Distancing
|
Potential Depersonalization
|
Higher Patient Satisfaction
|
Adoption of Digital Technologies
|
COVID-19 = coronavirus disease 2019; EHR= electronic health record; HIPAA = Health Insurance Portability and Accountability Act.
Figure.
Telehealth systems and cardiovascular disease.
Reduced Costs
Although there is still a need for additional research to evaluate telemedicine's impact on administrative costs, multiple studies suggest an overall cost reduction in implementing telehealth. A meta-analysis of 21 randomized controlled trials between 2000 and 2009 on multidisciplinary heart failure management demonstrated a substantial reduction in health care resource utilization in the remote patient monitoring arm compared with usual care, primarily driven by decreased heart failure hospitalizations.10 A systematic review of 10 different heart failure telemonitoring systems also demonstrated a reduction in costs related to hospital admissions.11 Costs to a clinical practice may be reduced when a large number of visits are via telemedicine, creating opportunity for needed in-person visits.
Assessment and Monitoring of Patients Within Their Home Environment
An inherent feature of telemedicine is the ability to observe patients within their home environment and gather self-measured data outside the setting of a clinic or hospital, possibly equating to the modern-day version of a “house call.” Family members can more easily participate in visits, share observations, as well as support and contribute to care needs. In addition, remote monitoring and longitudinal telemedicine communication may be advantageous. The Telemedical Interventional Management in Heart Failure II (TIM-HF2) trial was a prospective randomized controlled trial that aimed to investigate the efficacy of remote patient management intervention on morbidity and mortality in patients with heart failure.12 The primary outcome was the percentage of days lost due to unplanned cardiovascular hospital admissions (or death from any cause), which was statistically reduced in patients allocated to remote management (4.88% or 17.8 days lost/year) compared with usual care (6.64% or 24.2 days lost/year).12
Several trials have analyzed outcomes of implantable hemodynamic monitoring in patients with heart failure, including the CardioMEMS Heart Sensor Allows Monitoring of Pressure to Improve Outcomes in NYHA Class III Heart Failure Patients (CHAMPION) trial, Pulmonary Artery Pressure by Implantable device Responding to Ultrasonic Signal (PAPIRUS) trial, Chronicle Offers Management to Patients with Advanced Signs and Symptoms of Heart Failure (COMPASS-HF) trial, and the ongoing Hemodynamic-GUIDEd management of Heart Failure (GUIDE-HF) trial.13 In a meta-analysis of 14 randomized controlled trials investigating device monitoring in heart failure (including cardiac pressure sensors, implantable cardioverter defibrillator (ICDs), impedance monitoring devices), there was no overall difference in heart failure-related admission rates or all-cause mortality, although in a subgroup analysis of only pressure sensor devices, there was a lower admission rate.14
Electrophysiology is another subspecialty in which telehealth has enhanced the delivery of cardiovascular care. During the pandemic, mobile devices such as mobile cardiac outpatient telemetry (MCT) have been used as an adjunctive approach to support inpatient care when hospitals have exceeded telemetry capacity or when conventional telemetry monitoring may not be feasible.15 Since the beginning of the pandemic, there has been an exponential growth of wireless communication with implantable electronic cardiac devices.15
Maintain Social Distancing
There have been several reviews highlighting the association of higher severity of COVID-19 infection in those with cardiovascular disease.3 The recent large-scale conversion to telemedicine during COVID-19 demonstrates its effectiveness and utility for social distancing in clinical and other settings.16
Patient Satisfaction
Improved efficiency, ease of access, and more personalized and greater coordination of care has the potential to increase both clinician and patient satisfaction, in addition to health outcomes. In a British Medical Journal (BMJ) systematic review prior to the COVID-19 pandemic that explored the association of telehealth and patient satisfaction in regard to efficiency and effectiveness, patients reported high levels of satisfaction.9 Several factors were shown to contribute to higher patient satisfaction, including improved outcomes, preferred modality, ease of use, low cost, improved communication, and decreased travel time.9 In a May 2020 poll of more than 1000 Medicare Advantage beneficiaries, 91% of respondents reported a favorable experience with telehealth, and 78% stated intentions to use telehealth again in the future.17
Challenges
Payment Models
Perhaps the most significant change for telehealth in the context of the COVID-19 pandemic has been payment parity between clinic-based care and telehealth (Table; Figure).18 Before the pandemic, many states required telehealth cost coverage by insurance without stipulation for payment parity, which was seen as disincentivizing its use. Payment equity is emerging as a concept to avoid undue incentivization of telehealth encounters while continuing to make it a feasible option for clinicians to implement.18 Medicaid programs and some private payers recognized the need for incentives and announced payment parity for telehealth for the duration of the pandemic.19 The Coronavirus Preparedness and Response Supplemental Appropriations Act of 2020 waived the geographic and site restrictions for Medicare reimbursement. As a result, the rapid implementation of telehealth in cardiovascular care occurred.
The Centers for Medicare and Medicaid Services (CMS) 2021 Physician Fee schedule, however, did not propose to continue audio-only visits after the conclusion of the COVID-19 public health emergency (PHE). It did add several new telehealth services that can be reimbursed under Medicare. Some of these services are included under Category 1, which makes coverage permanent, but services falling under Category 3 are temporary and will last until the end of the calendar year in which the COVID-19 PHE concludes. Cardiac rehabilitation is 1 such service that falls under Category 3 coverage. Remote patient monitoring will continue to be reimbursed for established (but not new) patients after the PHE ends.20
Before the pandemic, only 14,000 Medicare beneficiaries received Medicare telehealth services in a week, while more than 10.1 million beneficiaries received Medicare telehealth services between mid-March and early July 2020.21 It will be important to establish and maintain a revenue-neutral platform for physicians and clinical enterprises with emphasis on bettering patient care and quality.
Data Security and Privacy
One of the potential barriers to wider adoption of telehealth has been privacy regulations, in particular the Health Insurance Portability and Accountability Act of 1996 (HIPAA).18 The Office for Civil Rights (OCR) at the Department of Health and Human Services issued a notice of enforcement discretion in response to the COVID-19 pandemic, stating penalties will not be imposed for HIPAA violations that occur during good faith provision of telehealth during the COVID-19 emergency.22 This notice permits clinicians to use platforms that are not HIPAA-compliant, a practical approach given the need to increase telehealth services quickly.18 Facebook Live, Twitch, TikTok, and similar video communication applications are considered public-facing and should not be used in the provision of telehealth by covered health care providers.22 Overall, although timely care of patients should take priority over privacy during a crisis, it will be necessary to ensure privacy is addressed appropriately once the pandemic begins to resolve.
Potential Impact on Disparities (Particularly in Low-Socioeconomic and Rural Communities with Limited Access to High-Speed Internet)
A recent article explored inequities in cardiovascular care through telemedicine in 2940 patients. Inequitable access to medical care was noted in female patients, non-English speaking patients, older, and poorer patients.23 Non-English language was independently associated with >50% lower use of telemedicine, as was being female.23 Median household income <$50K was associated with lower video use, which as mentioned has higher rates of reimbursement compared to telephone-only visits.23 A December 2020 retrospective medical record review evaluating telemedicine access for primary and specialty ambulatory care visits among 148,402 patient encounters at a large academic health system during the early phase of the COVID-19 pandemic demonstrated that older age, Asian race, non-English language as the patient's preferred language, and Medicaid were independently associated with fewer completed telemedicine visits.24 Additionally, Latinx ethnicity, Black race, older age, female sex, and lower household income were associated with lower use of video for telemedicine care. Another realm of disparity is technological access. Access to broadband technologies that provide a high-speed connection to the Internet is a social determinant of health and is a public health issue.25 Broadband access has been referred to by several national organizations as a "super-determinant" of health, given its intersection with so many identified social determinants of health.25 However, access is far from universal, with approximately 24 million people in the United States without broadband access in 2019.25 The prevalence of Internet use in patients with atherosclerotic cardiovascular disease (ASCVD) is lower compared to the general population (63% vs 84%).26 Within this group, Black and Hispanic patients had lower Internet use compared with whites.26
There are ongoing efforts to bridge these disparities. Programs such as the Federal Communications Commission's Rural Health Care Program and the Department of Agriculture's Distance Learning and Telemedicine Program are expanding telehealth availability by funding broadband services in these areas.25 In addition to federal policies, state and local laws are imperative to facilitate broadband and telehealth expansion
Potential Depersonalization
One of the challenges of telemedicine is the possibility of depersonalization of the patient-physician relationship. A review in the Journal of Telemedicine and Telecare focused on the technical and interpersonal aspects of telemedicine suggests that as physicians increasingly rely on high-tech instruments for their encounters, the clinician-patient relationship becomes more impersonal.27 The same review notes that although video consultations are likely to be more impersonal than face-to-face office visits, they may be more personal than strictly telephone encounters.
Nonetheless, patient and clinician satisfaction with telehealth has been shown to be higher than in-person visits, even before the COVID-19 pandemic.28, 29, 30 Thus, it is still an open question whether telehealth will decrease—or could increase—clinician and patient/family engagement. Hybrid models combining some in-person care with virtual care are also important to consider.
Challenges of Adoption of Digital Technologies
Audio and video visits alone, while of some inherent value, may be missing medical information such as vital signs and other physiologic parameters that are available for in-person visits. This raises concern about the effectiveness of clinical management using telehealth unless there is a successful adoption of some digital technologies. Potential barriers to such adoption including accuracy of digital tools, avoiding overburden of data for clinicians, and reliance on patient self-report for symptoms and signs (eg, vs direct physical examination).
There is evidence that digital technologies (eg, wearable and nonwearable biosensors), including consumer digital health products, can be accurate and reliable in measuring vital signs or other physiologic metrics (eg, electrocardiogram). One specific area of growing evidence in this regard is remote blood pressure measurement and management. In a recent analysis of a cross-sectional audit of ambulatory care during the second quarter of 2020 compared with the prior 2 years, the authors report a substantial decrease in total primary care encounters, along with a dramatic increase in the proportion of those encounters conducted via telehealth than those conducted in person.31 However, there was a decline in blood pressure and cholesterol assessments during this period, owing to both fewer total visits and less frequent assessment during telemedicine encounters.31
Emerging technology is developing in the field of digital stethoscopes and mobile and point-of-care ultrasound that can augment the telemedicine experience and improve comprehensive care.32, 33, 34 Video-based telehealth appointments allow for some components of the physical examination to be performed such as general appearance, orientation, respiratory rate, and fair visualization of edema, neck veins, and cyanosis. A 31-patient study found both bedside and remote jugular venous pressure (JVP) estimates were significantly and comparably correlated with invasively measured right atrial pressures.35 Encouraging patients to participate in their physical examination, particularly in the more tangible maneuvers such as obtaining their vital signs or abdominal palpation, could also foster more engaging delivery of care. Biosensing wearables and other validated diagnostic tools are needed to bridge the limitations in the physical examination.
Conclusions and Future Directions
“It's taken this crisis to push us to a new frontier, but there's absolutely no going back."—Seema Verma, CMS Administrator36
Geographic rules that govern medical licensing have been a limitation to telehealth implementation across state lines. Amid the COVID-19 pandemic, some states have relaxed or eliminated certain licensure requirements.18 This trend toward a more permissive environment with a shift away from the geographic emphasis on licensure is essential to supporting the transition to implementing more telemedicine throughout the country and improving access to care.18
Patient data governance and privacy regulations are another realm in which policy change can be valuable. There exists the option of using secure databases that can make accessing patient health care information more seamless compared with current cumbersome EHR systems, as well as helping to prevent error, duplication, and waste.18 Integration of telehealth systems into the EHR systems is needed. Because telehealth visits tend to be shorter in duration than in-person visits and offer fewer diagnostic services, payment equity rather than payment parity could be another avenue for policy change.18 In particular, reimbursement of telehealth visits with identical rates as in-person visits could represent overpayment and disincentivize in-office visits leading to a financial threat to centers and practices continuing to practice in-person care.18
Several additional considerations may help to transform the implementation of telehealth practices. Telemedicine can be a platform for extending team-based care, involving other valued nonphysician members of the cardiac team. During this current PHE, nonphysician clinicians, and licensed social workers have been approved to perform and be reimbursed for virtual visits.37 Inpatient care may also benefit from implementing telemedicine. Cardiac care can adopt tele-intensive care unit team models, which use audiovisual communication to provide care to patients who are critically ill.38
Advancements in cardiac monitoring devices are needed for the expansion of telehealth implementation. Increased use of devices for ambulatory monitoring such as patches, smartphones, wristwatches, vests, headbands, necklaces, and eyeglasses may have an impact on early detection of life-threatening conditions, reducing health care costs and unnecessary hospitalizations, and personalizing medicine.39 , 40
Although borne out of the necessity of the pandemic, telehealth has offered many adaptations of clinical care that have the potential to improve cardiovascular health and enhance access to care with equity. As we continue to optimize the potential for telehealth in cardiovascular care, time will tell if it fulfills its promise to enhance our health care delivery goals.
Footnotes
Funding: None.
Authorship: All authors had access to the data and a role in writing this manuscript.
References
- 1.Minow NN, Boucher R. Congress should make sure telemedicine is here to stay. Available at: https://www.bostonglobe.com/2020/07/16/opinion/congress-should-make-sure-telemedicine-is-here-stay/. Accessed July 28, 2020.
- 2.Tenforde MW, Billig Rose E, Lindsell CJ, et al. Characteristics of adult outpatients and inpatients with COVID-19 — 11 academic medical centers, United States, March–May 2020. MMWR Morb Mortal Wkly Rep. 2020;69(26):841–846. doi: 10.15585/mmwr.mm6926e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Driggin E, Madhavan MV, Bikdeli B, et al. Cardiovascular considerations for patients, health care workers, and health systems during the COVID-19 pandemic. J Am Coll Cardiol. 2020;75(18):2352–2371. doi: 10.1016/j.jacc.2020.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.American College of Cardiology. Telehealth Primer For Cardiology Fellows. Available at: https://www.acc.org/membership/sections-and-councils/fellows-in-training-section/section-updates/2019/08/20/14/42/telehealth-primer-for-cardiology-fellows. Accessed July 30, 2020.
- 5.What Is Telehealth? Available at: https://catalyst.nejm.org/doi/full/10.1056/CAT.18.0268. Accessed June 25, 2020.
- 6.Wasfy JH, Rao SK, Chittle MD, Gallen KM, Isselbacher EM, Ferris TG. Initial results of a cardiac E-consult pilot program. J Am Coll Cardiol. 2014;64(24):2706–2707. doi: 10.1016/j.jacc.2014.09.061. [DOI] [PubMed] [Google Scholar]
- 7.Phadke NA, del Carmen MG, Goldstein SA, et al. Trends in ambulatory electronic consultations during the COVID-19 pandemic. J Gen Intern Med. 2020;35(10):3117–3119. doi: 10.1007/s11606-020-05878-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Poppas A, Rumsfeld JS, Wessler JD. Telehealth is having a moment: will it last? J Am Coll Cardiol. 2020;75(23):2989–2991. doi: 10.1016/j.jacc.2020.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kruse CS, Krowski N, Rodriguez B, Tran L, Vela J, Brooks M. Telehealth and patient satisfaction: a systematic review and narrative analysis. BMJ Open. 2017;7(8):1–12. doi: 10.1136/bmjopen-2017-016242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Klersy C, De Silvestri A, Gabutti G, et al. Economic impact of remote patient monitoring: An integrated economic model derived from a meta-analysis of randomized controlled trials in heart failure. Eur J Heart Fail. 2011;13(4):450–459. doi: 10.1093/eurjhf/hfq232. [DOI] [PubMed] [Google Scholar]
- 11.Seto E. Cost comparison between telemonitoring and usual care of heart failure: a systematic review. Telemed e-Health. 2008;14(7):679–686. doi: 10.1089/tmj.2007.0114. [DOI] [PubMed] [Google Scholar]
- 12.Koehler F, Koehler K, Deckwart O, et al. Efficacy of telemedical interventional management in patients with heart failure (TIM-HF2): a randomised, controlled, parallel-group, unmasked trial. Lancet. 2018;392(10152):1047–1057. doi: 10.1016/S0140-6736(18)31880-4. [DOI] [PubMed] [Google Scholar]
- 13.Ayyadurai P, Alkhawam H, Saad M, et al. An update on the CardioMEMS pulmonary artery pressure sensor. Ther Adv Cardiovasc Dis. 2019;13:1–11. doi: 10.1177/1753944719826826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Halawa A, Enezate T, Flaker G. Device monitoring in heart failure management: outcomes based on a systematic review and meta-analysis. Cardiovasc Diagn Ther. 2019;9(4):386–393. doi: 10.21037/cdt.2019.01.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Varma N, Marrouche NF, Aguinaga L, et al. HRS/EHRA/APHRS/LAHRS/ACC/AHA worldwide practice update for telehealth and arrhythmia monitoring during and after a pandemic. J Am Coll Cardiol. 2020;76(11):1363–1374. doi: 10.1016/j.jacc.2020.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bashshur R, Doarn CR, Frenk JM, Kvedar JC, Woolliscroft JO. Telemedicine and the COVID-19 pandemic, lessons for the future. Telemed e-Health. 2020;26(5):571–573. doi: 10.1089/tmj.2020.29040.rb. [DOI] [PubMed] [Google Scholar]
- 17.King R. Poll: Medicare Advantage Members Are Taking to Telehealth. Available at: https://www.fiercehealthcare.com/payer/poll-shows-ma-seniors-who-use-telehealth-are-excited-to-use-service-again. Accessed July 30, 2020.
- 18.Shachar C, Engel J, Elwyn G. Implications for telehealth in a postpandemic future: regulatory and privacy issues. JAMA. 2020;323(23):2375–2376. doi: 10.1001/jama.2020.7943. [DOI] [PubMed] [Google Scholar]
- 19.Center for Connected Health Policy. COVID-19 Telehealth Coverage Policies. Available at: https://www.cchpca.org/resources/covid-19-telehealth-coverage-policies. Accessed June 16, 2020.
- 20.Centers for Medicare & Medicaid Services. CMS-1734-P. Available at:https://www.cms.gov/medicaremedicare-fee-service-paymentphysicianfeeschedpfs-federal-regulation-notices/cms-1734-p. Accessed January 20, 2021. [PubMed]
- 21.Centers for Medicare & Medicaid Services. Trump Administration Proposes to Expand Telehealth Benefits Permanently for Medicare Beneficiaries Beyond the COVID-19 Public Health Emergency and Advances Access to Care in Rural Areas. Available at:https://www.cms.gov/newsroom/press-releases/trump-administration-proposes-expand-telehealth-benefits-permanently-medicare-beneficiaries-beyond. Accessed August 4, 2020.
- 22.US Department of Health and Human Services. Notification of Enforcement Discretion for Telehealth. Accessed at:https://www.hhs.gov/hipaa/for-professionals/special-topics/emergency-preparedness/notification-enforcement-discretion-telehealth/index.html. Accessed June 16, 2020.
- 23.Eberly LA, Khatana SAM, Nathan AS, et al. Telemedicine outpatient cardiovascular care during the COVID-19 pandemic: bridging or opening the digital divide? Circulation. 2020;142(5):510–512. doi: 10.1161/CIRCULATIONAHA.120.048185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Eberly LA, Kallan MJ, Julien HM, Haynes N, Khatana SAM. Patient characteristics associated with telemedicine access for primary and specialty ambulatory care during the COVID-19 pandemic. 2021;3(12):1-12. doi:10.1001/jamanetworkopen.2020.31640. [DOI] [PMC free article] [PubMed]
- 25.Bauerly BC, McCord RF, Hulkower R, Pepin D. Broadband access as a public health issue: the role of law in expanding broadband access and connecting underserved communities for better health outcomes. J Law, Med Ethics. 2019;47(2_suppl):39–42. doi: 10.1177/1073110519857314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Al Rifai M, Shapiro MD, Sayani S, et al. Racial and geographic disparities in internet use in the United States among patients with atherosclerotic cardiovascular disease. Am J Cardiol. 2020;134:146–147. doi: 10.1016/j.amjcard.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Miller EA. The technical and interpersonal aspects of telemedicine: effects on doctor-patient communication. J Telemed Telecare. 2003;9(1):1–7. doi: 10.1258/135763303321159611. [DOI] [PubMed] [Google Scholar]
- 28.Orlando JF, Beard M, Kumar S. Systematic review of patient and caregivers’ satisfaction with telehealth videoconferencing as a mode of service delivery in managing patients’ health. PLoS One. 2019;14(8):1–20. doi: 10.1371/journal.pone.0221848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Donelan K, Barreto EA, Sossong S, et al. Patient and clinician experiences with telehealth for patient follow-up care. Am J Manag Care. 2019;25(1):40–44. [PubMed] [Google Scholar]
- 30.Morgan DG, Kosteniuk J, Stewart N, O'Connell ME, Karunanayake C, Beever R. The telehealth satisfaction scale: reliability, validity, and satisfaction with telehealth in a rural memory clinic population. Telemed J E Health. 2014;20(11):997–1003. doi: 10.1089/tmj.2014.0002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Alexander GC, Tajanlangit M, Heyward J, Mansour O, Qato DM, Stafford RS. Use and content of primary care office-based vs telemedicine care visits during the COVID-19 pandemic in the US. JAMA Netw Open. 2020;3(10) doi: 10.1001/jamanetworkopen.2020.21476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Smallwood N, Dachsel M. Point-of-care ultrasound (POCUS): unnecessary gadgetry or evidence-based medicine? Clin Med (Lond) 2018;18(3):219–224. doi: 10.7861/clinmedicine.18-3-219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Swarup S, Makaryus AN. Digital stethoscope: technology update. Med Devices Evid Res. 2018;11:29–36. doi: 10.2147/MDER.S135882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lakhe A, Sodhi I, Warrier J, Sinha V. Development of digital stethoscope for telemedicine. J Med Eng Technol. 2016;40(1):20–24. doi: 10.3109/03091902.2015.1116633. [DOI] [PubMed] [Google Scholar]
- 35.Kelly SA, Schesing KB, Thibodeau JT, Ayers CR, Drazner MH. Feasibility of remote video assessment of jugular venous pressure and implications for telehealth. JAMA Cardiol. 2020;5(10):1194–1195. doi: 10.1001/jamacardio.2020.2339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dyrda L. “The genie's out of the bottle on this one”: Seema Verma hints at the future of telehealth for CMS beneficiaries. Available at:https://www.beckershospitalreview.com/telehealth/the-genie-s-out-of-the-bottle-on-this-one-seema-verma-hints-at-the-future-of-telehealth-for-cms-beneficiaries.html. Accessed August 7, 2020.
- 37.Gorodeski EZ, Goyal P, Cox ZL, et al. Virtual Visits for care of patients with heart failure in the era of COVID-19: a statement from the Heart Failure Society of America. J Card Fail. 2020;26(6):448–456. doi: 10.1016/j.cardfail.2020.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rincon TA, Bakshi V, Beninati W, et al. Describing advanced practice provider roles within critical care teams with Tele-ICUs: exemplars from seven US health systems. Nurs Outlook. 2020;68(1):5–13. doi: 10.1016/j.outlook.2019.06.005. [DOI] [PubMed] [Google Scholar]
- 39.Abraham WT, Anker S, Burkhoff D, et al. Primary results of the sensible medical innovations lung fluid status monitor allows reducing readmission rate of heart failure patients (smile) Trial. J Card Fail. 2019;25(11):938. doi: 10.1016/j.cardfail.2019.11.007. [DOI] [Google Scholar]
- 40.Sana F, Isselbacher EM, Singh JP, Heist EK, Pathik B, Armoundas AA. Wearable devices for ambulatory cardiac monitoring: JACC state-of-the-art review. J Am Coll Cardiol. 2020;75(13):1582–1592. doi: 10.1016/j.jacc.2020.01.046. [DOI] [PMC free article] [PubMed] [Google Scholar]