Abstract
While pandemic containment measures benefit public health, they may jeopardize the social structure of society. We hypothesize that lockdowns and prolonged social distancing measures hinder social support and invite norm violations, eroding social trust. We conducted a pre-registered pre-post study on a representative sample of the Dutch population (n = 2377; participation rate = 88.8%), measuring social trust reported by the same individuals before and after the first wave of the COVID-19 pandemic. Results show that social trust in the Netherlands suddenly dropped from its historically stable level, reaching one of its lowest points on record. The decline was stronger among residents belonging to official high-risk categories, especially if they perceived themselves as likely to become infected. Individuals who more strongly agreed with self-isolation norms or did not perceive a widespread compliance or agreement with such norms also reported a greater loss of trust.
Keywords: Social trust, COVID-19, Vulnerability, Social norms, Normative expectations
1. Introduction
Natural disasters enhance social trust by posing a common threat, boosting a sense of community, and reinforcing social bonds and group identity as people “come together” to help each other in difficult times (Calo-Blanco et al., 2017; Cassar et al., 2017; Dussaillant and Guzmán, 2014; Kang and Skidmore, 2018; Toya and Skidmore, 2014). Here we argue that pandemics may be different from other types of natural disasters (e.g., earthquakes) because the public health interventions that follow them may counteract otherwise positive solidarity effects. Specifically, lockdowns and prolonged social distancing measures hinder social support and invite rule violation, possibly harming the social structure of society.
Prior research shows that positive social interactions and informal contacts are important determinants of people's trust in their fellow citizens: while frequent socialization enhances people's willingness to rely on others, social isolation hinders their capacity to do so (Glanville et al., 2013; Putnam, 2000). Furthermore, the literature indicates a positive association between individual well-being and social trust (Helliwell and Putnam, 2004). Self-rated good health has been found to be associated with higher levels of social trust across a large body of studies, while worse physical health (e.g., obesity) is associated with a low propensity to trust – though the correlation is not statistically significant for other health issues (e.g., diabetes) (Jen et al., 2010; Kim et al., 2008; Riumallo-Herl et al., 2014; Rodgers et al., 2019; Wu et al., 2018). It has been argued that people incurring in worse health conditions may be less socially engaged and develop stronger feelings of uncertainty and insecurity, substantially hampering their ability to rely on strangers (Cornwell, 2009; Giordano and Lindström, 2016; Glanville et al., 2013; Helliwell and Putnam, 2004). In a similar vein, we argue that the pandemic forces individuals to actively isolate themselves for a sustained period of time, fueling doubt and skepticism towards strangers. This should be particularly true for people who are at higher medical risk or have already been infected because they are strongly encouraged to self-isolate at home and avoid social contacts. That is, as health risks and self-isolation needs increase, people's willingness to rely on others should deteriorate. We thus hypothesize:
The more vulnerable people are to the virus, the more their social trust in fellow citizens decreases during the pandemic [H1].
Contrary to other types of natural disasters, pandemics require strict norm compliance for successful containment (Chu et al., 2020; Dehning et al., 2020; Diekmann, 2020). Social trust could be undermined by recurrent selfish behaviors and frequent violations of lockdown norms (Horne and Mollborn, 2020; Posner, 2000; Van Bavel et al., 2020). However, what people think is the right thing to do (i.e., personal normative beliefs) might differ from what these people think their fellow citizens agree and comply with (i.e., perceived agreement and compliance) (Bicchieri, 2016; Bicchieri et al., 2014; de Wit and Lisciandra, 2020; Rauhut, 2013). Individuals who believe lockdown norms should be adhered to may gain trust if they perceive that their fellow citizens share this belief or comply with lockdown norms. However, these people may lose trust if they perceive that their fellow citizens do not share this belief or fail to comply with lockdown norms (Rauhut, 2013). In contrast, those who do not believe that lockdown norms should be followed may remain unaffected in their social trust by what they perceive others think and do with regard to lockdown norms. We thus hypothesize that discrepancies between people's normative beliefs regarding lockdown norms and these people's perceptions of others' compliance and agreement with lockdown norms will affect social trust as follows:
The more people view social distancing and self-isolation as appropriate and believe that only few fellow citizens comply [H2a] or agree [H3a] with such norms, the more their social trust decreases.
Social trust of people who do not view social distancing and self-isolation as appropriate is unaffected by their beliefs about fellow citizens' compliance [H2b] or agreement [H3b] with such norms.
To test these hypotheses, we conducted a pre-registered pre-post study on a representative sample of the Dutch population (n = 2377). We measured social trust in the same individuals before and after the first wave of the pandemic, while assessing the impact of virus exposure, vulnerability, as well as agreement with norms concerning self-isolation, and perceived compliance and agreement with such norms.
2. Materials and methods
Data were collected between July 6th, 2020 and July 28th, 2020 on a sample of the Dutch population well spread on the national territory, using the Longitudinal Internet studies for the Social Sciences (LISS) sample pool. The LISS panel consists of about 7500 respondents and has been active since 2007. The panel is based on a true probability sample of households drawn from the population register by Statistics Netherlands (CBS), and it is administered each year to the same individuals, covering several aspects of respondents' attitudes and living conditions (Scherpenzeel and Das, 2010).
Our gross sample (n = 2698) was a random sample of the active LISS panel members who answered the social trust question in May/June 2019 (Wave 11, Personality module of the LISS panel) and participated in the “Effects of the Outbreak of COVID-19” study conducted at the end of March 2020. This approach allowed us to realize the pre-post measurement on our variable of interest (social trust) and use answers to COVID-19 related questions. In total, we had 2405 participants of which 8 did not complete our survey (participation rate = 88.8%). After listwise deletion of missing values, our sample amounted to 2377. Responses were collected between the first and the second wave of the pandemic (see Supplementary Information - SI) using an Internet survey in line with LISS panel standard procedures. Social trust in May/June 2019 (pre-pandemic) and July 2020 (post-first wave) was measured using the standard 11-point scale (0 = “You can't be too careful”, 10 = “Most people can be trusted”). This measure of social trust has been widely used in the literature, showing a high level of test-retest reliability and a higher validity than its dichotomous version (Hout and Hastings, 2016; Lundmark et al., 2016; Nannestad, 2008) – see also Banerjee et al. (2021) for recent empirical evidence supporting a robust association between the self-reported measure of social trust using the 11-point scale and behaviors in the experimental trust game. Indicators of virus vulnerability, normative beliefs and perceptions rely on prior studies of social norms (Bicchieri, 2016; Bicchieri et al., 2014) and COVID-19 (de Bruin and Bennett, 2020; de Wit and Lisciandra, 2020; Van Bavel et al., 2020), as well as on guidelines provided by the National Institute for Public Health (RIVM, 2021). Table 1 summarizes the measures we used for the constructs mentioned in our hypotheses, while Table 2 provides descriptive statistics.
Table 1.
Measurement of main constructs.
| Construct | Measurement |
|---|---|
| Social Trust | Generally speaking, would you say that most people can be trusted, or that you can't be too careful in dealing with people? 0. You can't be too careful … 10. Most people can be trusted |
| Vulnerability to COVID-19 | According to the National Institute for Public Health, people who are older than 70, or have a long-term medical condition (e.g., lung diseases, heart diseases, diabetes, kidney diseases, obesity, etc.), or have immunodeficiencies are at a higher risk of getting very sick from the coronavirus. Are you in this high-risk category for the coronavirus? 1. Yes, 0. No Do you think you are or have been infected with the coronavirus? 1. Yes, 0. No How likely do you think that you will be infected in the next two months? (End of March) 1. No chance … 8. It already happened Do you know anyone among your close contacts (i.e., people with whom you discuss or share personal matters) who has tested positively for the coronavirus or has seen a doctor who confirmed that it is likely that he/she is or has been infected with the coronavirus? 1. Yes, 0. No |
| Agreement with lockdown-norms [A] and [B] | During the lockdown in April, it was appropriate for people in the Netherlands who had any [A]/no [B] symptoms of an infection (e.g., nose cold, sore throat, cough, fever) to stay home and avoid social contacts. 1. Strongly disagree … 5. Strongly agree |
| Perceived compliance with lockdown-norms [A] and [B] | Out of every 100 people who had any [A]/no [B] symptoms of an infection, how many do you think stayed home during the lockdown and avoided social contacts? Number: 0 … 100 |
| Perceived agreement with lockdown-norms [A] and [B] | Out of every 100 people, how many do you think agree with statement A/B? Number: 0 … 100 |
Note. Social Trust was measured in May/June 2019 and July 2020. Perceived chance of being infected was measured at the end of March 2020 in the “Effects of the Outbreak of COVID-19” study. All other variables were measured in July 2020.
Table 2.
Descriptive statistics.
| Variables | mean | sd | min | max |
|---|---|---|---|---|
| Social Trust July 2020 | 5.84 | 2.38 | 0 | 10 |
| Social Trust May 2019 | 5.97 | 2.19 | 0 | 10 |
| Social Trust change | −0.13 | 2.06 | −9 | 9 |
| Norm A: appropriate to isolate with symptoms | 4.40 | 0.93 | 1 | 5 |
| Perceived agreement with norm A | 7.64 | 1.82 | 0 | 10 |
| Perceived compliance with norm A | 7.13 | 2.07 | 0 | 10 |
| Norm B: appropriate to isolate with no symptoms | 3.79 | 1.05 | 1 | 5 |
| Perceived agreement with norm B | 6.47 | 2.00 | 0 | 10 |
| Perceived compliance with norm B | 5.80 | 2.22 | 0 | 10 |
| R is in a high-risk category | 0.34 | 0.47 | 0 | 1 |
| R has been infected | 0.07 | 0.26 | 0 | 1 |
| R has n contacts who are infected | 0.21 | 0.81 | 0 | 12 |
| Perceived chance of being infected | 4.00 | 1.12 | 1 | 8 |
Note. Perceived agreement and compliance were re-scaled from 0–100 to 0–10; n = 2377.
The representativeness of the LISS sample is periodically monitored and adjustments are made over time to maintain it. While our subsample has similar characteristics to the sample of LISS participants that routinely take part in the Personality module (which includes the social trust question), some differences from the general Dutch adult population can be observed (see SI). To address this, we computed sample weights using CBS Population Statistics, and re-ran all our analyses applying sample weights. Results are shown in the SI and are consistent with all our findings.
The pre-post design of our study enables us to assess the change in social trust before and after the first wave of the pandemic. We thus operationalized our dependent variable as the difference between respondents' levels of social trust in 2020 and 2019 (Allison, 1990). We treated this 19-category variable as continuous and employed OLS regression models. Regression coefficients are estimated with heteroscedasticity-robust standard errors and we set statistical significance at the 5% level (i.e., α = 0.05) for two-sided tests. To test our hypotheses, we use the COVID-19 related variables listed in Table 1. Further information on descriptive statistics, additional analyses, and robustness checks are available in the SI. The pre-registration and the questionnaire pertaining to our survey are available at the Open Science Framework (OSF) website. This study obtained ethical approval from the Ethics Committee of the Faculty of Social and Behavioural Sciences of Utrecht University.
3. Results
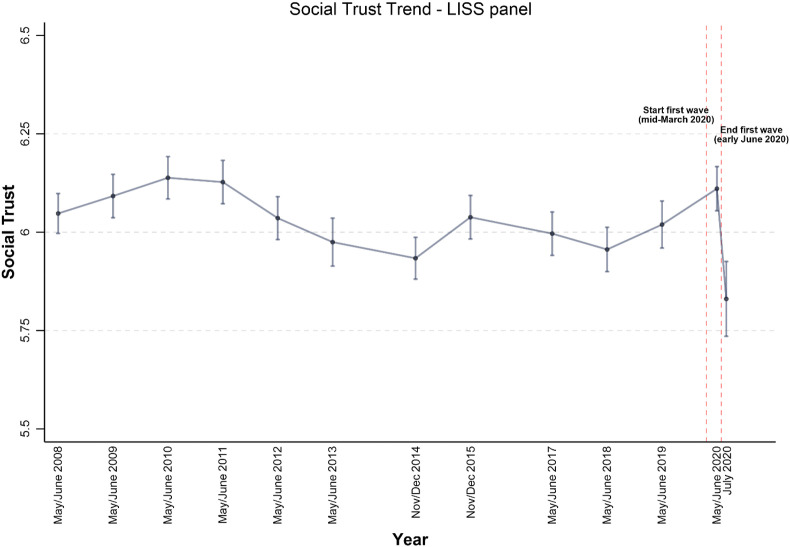
Results from a paired t-test indicate that, overall, trust significantly decreased by 0.13 points (Social Trust2020 = 5.84, SE = 0.05; Social Trust2019 = 5.97, SE = 0.05; t(2376) = -3.11, p < 0.01). Though relatively small, this drop is noteworthy considering that (a) social trust is a stable trait and its trend in the Netherlands has been steady in the last 20 years (Lo Iacono and Quaranta, 2019; Nannestad, 2008; Uslaner, 2002); (b) this is one of the lowest levels of social trust recorded in the Netherlands so far – see Fig. 1 .
Fig. 1.
Social Trust in the Netherlands – LISS panel. Sources: LISS panel Waves 1–12 (May/June 2008–May/June 2020) and current study (July 2020), European Center for Disease prevention and Control (ECDC) data; 95% CIs. Following the ECDC, we define the start/end of the first wave of the pandemic according to two criteria: the positivity test rate is above/below 4% (i.e. n COVID-19 cases/n COVID-19 tests) and more/less than 25 cases per 100,000 inhabitants are reported in the past 2 weeks (ECDC, 2021) – see SI. Note: Social trust ranges between 0 and 10.
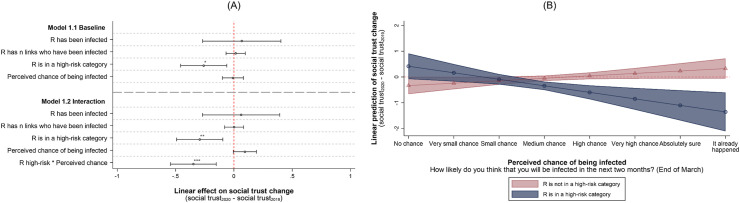
Table 3 and Fig. 2 show OLS regression results of the impact of having been infected (among survivors), number of infected close contacts, belonging to a high-risk category, and perceived chance of being infected at the end of March 2020 on social trust change, controlling for sociodemographic variables, geographical location, and date of fieldwork (see SI for details and robustness checks). Model 1.1 suggests that belonging to a high-risk group for COVID-19 significantly predicts the change in social trust. High-risk individuals reported 0.30 trust points less than in the pre-pandemic period (t = −3.69, p < 0.001), whereas individuals who were not at high-risk reported a statistically insignificant loss of 0.04 trust points (t = −0.82, p = 0.410), meaning that high-risk individuals lost 0.26 trust points more on average than people who were not at high-risk (t = −2.57, p < 0.05; Model 1.1). As the three other indicators of vulnerability do not predict social trust change, these results provide only partial support for H1. Model 1.2 tests, using a two-way interaction, whether belonging to the high risk-category has an effect on social trust change especially for people who think they have a high chance of being infected, under the assumption that objective vulnerability operates in conjunction with subjective perceptions of vulnerability. Results show that the interaction is indeed significant (t = −3.47, p < 0.001): a one-unit increase in perceived chance of being infected yields a loss of 0.35 in the dependent variable for people in the high-risk category in comparison to people who are not in the high-risk category. This is graphically illustrated in Fig. 2 Panel B, which indicates that the impact on social trust change for people in the high-risk category is indeed negative and substantial. Change in social trust in people who are not in the high-risk category is hardly contingent on their perception of getting infected. By contrast, as it can be seen from the blue line in Fig. 2 Panel B, among people in the high-risk category those who perceived infection chances to be the highest experienced a drop in social trust of 1.36 points (t = −3.53, p < 0.001) while those who perceived infection chances to be the lowest experienced a statistically insignificant increase of 0.42 trust points (t = 1.64, p = 0.101).
Table 3.
Effect of virus vulnerability on social trust change.
| DV: Social Trust2020 – Social Trust2019 | Model 1.1 | Model 1.2 | ||
|---|---|---|---|---|
| R has been infected | 0.067 | (0.171) | 0.062 | (0.169) |
| R has n contacts who are infected | 0.015 | (0.042) | 0.001 | (0.041) |
| R is in a high-risk category | −0.259* | (0.101) | −0.293** | (0.101) |
| Perceived chance of being infected | −0.008 | (0.046) | 0.094 | (0.051) |
| R is in high-risk*Perceived chance |
−0.348*** |
(0.100) |
||
| Demographics | Yes | Yes | ||
| Date of fieldwork | Yes | Yes | ||
| Province |
Yes |
Yes |
||
| Constant | 0.148 | (0.342) | 0.160 | (0.339) |
| N | 2377 | 2377 | ||
Note. OLS regressions with robust standard errors in parentheses. Perceived chance of being infected is centered around the mean. LISS sample, Netherlands 2019–2020. * = p < 0.05, ** = p < 0.01, *** = p < 0.001 (for two-sided tests).
Fig. 2.
Effect of virus vulnerability and exposure on the change of social trust within respondents. Panel A shows coefficients with 95% CIs from OLS regressions with robust standard errors. Panel B displays the predicted values of social trust change with 95% CIs by risk group and perceived chance of being infected. Perceived chance of being infected is centered around the mean. LISS sample, n = 2,377, Netherlands 2019–2020. * = p < 0.05, ** = p < 0.01, *** = p < 0.001 (for two-sided tests).
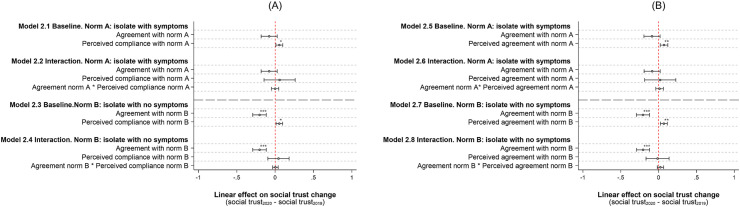
Table 4, Table 5 and Fig. 3 show OLS regression results of the impact of normative views (i.e. respondents' agreements with norms pertaining to self-isolation) and perceived compliance and agreement of others with such norms on social trust change, controlling for virus exposure and vulnerability, sociodemographic variables, geographical location, and date of fieldwork (see SI). We focus on two social norms: whether, during the lockdown in April 2020, it was appropriate to stay at home and avoid social contacts for people who had any COVID-19 symptoms (norm A) or had no symptoms (norm B). Perceived compliance and agreement concern these two norms. Baseline models show a significant negative impact of norm B (Models 2.3, 2.7), but not of norm A (Models 2.1, 2.5) – e.g., a one-unit increase of agreement with norm B produces a loss of 0.20 in social trust change (t = −4.55, p < 0.001).
Table 4.
Effect of normative views A and B and perceived compliance on social trust change.
| DV: Social Trust2020 – Social Trust2019 | Model 2.1 | Model 2.2 | Model 2.3 | Model 2.4 | ||||
|---|---|---|---|---|---|---|---|---|
| Norm A | −0.078 | (0.054) | −0.078 | (0.054) | ||||
| Perceived compliance with norm A | 0.054* | (0.023) | 0.058 | (0.103) | ||||
| Norm B | −0.204*** | (0.045) | −0.203*** | (0.045) | ||||
| Perceived compliance with norm B | 0.054* | (0.021) | 0.043 | (0.071) | ||||
| R has been infected | 0.054 | (0.171) | 0.054 | (0.171) | 0.047 | (0.170) | 0.046 | (0.170) |
| R has n contacts who are infected | 0.014 | (0.042) | 0.015 | (0.042) | 0.020 | (0.042) | 0.020 | (0.042) |
| R is in a high-risk category | −0.258* | (0.101) | −0.258* | (0.101) | −0.238* | (0.101) | −0.238* | (0.101) |
| Perceived chance of being infected | −0.002 | (0.046) | −0.002 | (0.046) | −0.001 | (0.046) | −0.001 | (0.046) |
| Norm A*Perceived compliance norm A | −0.001 | (0.024) | ||||||
| Norm B*Perceived compliance norm B |
0.003 |
(0.019) |
||||||
| Demographics | Yes | Yes | Yes | Yes | ||||
| Date of fieldwork | Yes | Yes | Yes | Yes | ||||
| Province |
Yes |
Yes |
Yes |
Yes |
||||
| Constant | 0.472 | (0.422) | 0.474 | (0.423) | 0.824* | (0.384) | 0.818* | (0.386) |
| N | 2377 | 2377 | 2377 | 2377 | ||||
Note. OLS regressions with robust standard errors in parentheses. Perceived compliance with norm A and B are centered around the mean. LISS sample, Netherlands 2019–2020. * = p < 0.05, ** = p < 0.01, *** = p < 0.001 (for two-sided tests).
Table 5.
Effect of normative views A and B and perceived agreement on social trust change.
| DV: Social Trust2020 – Social Trust2019 | Model 2.5 | Model 2.6 | Model 2.7 | Model 2.8 | ||||
|---|---|---|---|---|---|---|---|---|
| Norm A | −0.088 | (0.054) | −0.086 | (0.054) | ||||
| Perceived agreement with norm A | 0.072** | (0.026) | 0.021 | (0.105) | ||||
| Norm B | −0.207*** | (0.044) | −0.206*** | (0.044) | ||||
| Perceived agreement with norm B | 0.069** | (0.023) | −0.014 | (0.077) | ||||
| R has been infected | 0.048 | (0.170) | 0.047 | (0.170) | 0.050 | (0.168) | 0.047 | (0.168) |
| R has n contacts who are infected | 0.019 | (0.042) | 0.019 | (0.042) | 0.025 | (0.043) | 0.024 | (0.042) |
| R is in a high-risk category | −0.252* | (0.101) | −0.250* | (0.101) | −0.233* | (0.101) | −0.229* | (0.101) |
| Perceived chance of being infected | −0.005 | (0.046) | −0.005 | (0.046) | −0.003 | (0.046) | −0.000 | (0.046) |
| Norm A*Perceived agreement norm A | 0.013 | (0.026) | ||||||
| Norm B*Perceived agreement norm B |
0.024 |
(0.021) |
||||||
| Demographics | Yes | Yes | Yes | Yes | ||||
| Date of fieldwork | Yes | Yes | Yes | Yes | ||||
| Province |
Yes |
Yes |
Yes |
Yes |
||||
| Constant | 0.553 | (0.428) | 0.531 | (0.430) | 0.871* | (0.383) | 0.833* | (0.381) |
| N | 2377 | 2377 | 2377 | 2377 | ||||
Note. OLS regressions with robust standard errors in parentheses. Perceived agreement with norm A and B are centered around the mean. LISS sample, Netherlands 2019–2020. * = p < 0.05, ** = p < 0.01, *** = p < 0.001 (for two-sided tests).
Fig. 3.
Effect of normative views A and B, perceived compliance and agreement on the change of social trust within respondents. Panel A and B show coefficients with 95% CIs from OLS regressions with robust standard errors. Panel A displays results for perceived compliance, while Panel B displays results for perceived agreement. Perceived compliance and agreement with norm A and B are centered around the mean. LISS sample, n = 2,377, Netherlands 2019–2020. * = p < 0.05, ** = p < 0.01, *** = p < 0.001 (for two-sided tests).
Also, results show that social trust remained unchanged for individuals who perceived the vast majority of fellow citizens to agree or comply with norm A or B, while it dropped otherwise (Models 2.1, 2.3, 2.5, 2.7). For instance, individuals who perceived 50% of people to agree with norm B reported 0.23 trust points less than in the pre-pandemic period (t = −4.13, p < 0.001), whereas individuals who perceived 80% of people to agree with norm B experienced no significant trust loss (t = −0.48, p = 0.634). Nevertheless, interaction terms are never significant (Models 2.2, 2.4, 2.6, 2.8), indicating that the effect of normative views on social trust change does not depend on perceived compliance or agreement. These results fail to support H2a, H3a, H2b, and H3b.
4. Discussion
Our findings suggest that the COVID-19 pandemic unlike other natural disasters was followed by a loss of social trust. We found that social trust dropped in the Netherlands after the first wave of the COVID-19 pandemic, particularly for people at high-risk. However, exposure to the virus (among survivors) or infections amongst respondents' personal contacts had no impact on social trust.
Our study furthermore shows that trust loss after the first wave of the pandemic varied with objective and subjective vulnerability to COVID-19, as well as with normative views and perceived agreement and compliance with social distancing norms. People in official high-risk categories experienced a greater drop in trust, especially those who at the start of the pandemic perceived themselves as likely to become infected. People with a stronger normative view on self-isolation also lost trust in fellow citizens to a greater degree, along with individuals who did not expect a widespread compliance or agreement with such norms. However, contrary to our predictions, discrepancies between one's normative views and one's perceptions of what others think or do with regard to lockdown norms did not affect trust.
Our findings identify a paradoxical scenario that policy makers concerned with pandemic containment measures might face. On the one hand, strict lockdown norms help protect the lives and well-being of those most vulnerable to COVID-19. On the other hand, norms prescribing self-isolation and social distancing can undermine social trust and cohesion with yet unknown consequences for the fabric of society (Borkowska and Laurence, 2021). However, our study considers only potential consequences of COVID-19 on social trust in the short-term. Long-term consequences of lockdowns and other measures may be different. Furthermore, the causal nexus between the COVID-19 pandemic and social trust hinted in this research should be more thoroughly assessed with different study designs and datasets. Future research should continue to monitor the role of people's views and expectations regarding COVID-19 related norms (e.g., wearing a mask, getting vaccinated), investigate which interventions are less detrimental for social trust (in the short- and long-run), and whether similar mechanisms can be observed across countries.
Author contributions
S.L.I and W.P. contributed to study conceptualization, S.L.I. analyzed the data, S.L.I., W.P., V.B., R.C., and A.v.d.R. designed the research and wrote the paper.
Acknowledgments
We are grateful to the COVID-19 fast-track fund established by Utrecht University for financially supporting this project.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.socscimed.2021.114513.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Allison P.D. Change scores as dependent variables in regression analysis. Sociol. Methodol. 1990:93–114. [Google Scholar]
- Banerjee S., Galizzi M.M., Hortala-Vallve R. Trusting the trust game: an external validity analysis with a UK representative sample. Games. 2021;12(3):66. [Google Scholar]
- Bicchieri C. Oxford University Press; 2016. Norms in the Wild: How to Diagnose, Measure, and Change Social Norms. [Google Scholar]
- Bicchieri C., Lindemans J.W., Jiang T. A structured approach to a diagnostic of collective practices. Front. Psychol. 2014;5:1418. doi: 10.3389/fpsyg.2014.01418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borkowska M., Laurence J. Coming together or coming apart? Changes in social cohesion during the Covid-19 pandemic in England. Eur. Soc. 2021;23(Suppl. 1):S618–S636. [Google Scholar]
- Calo-Blanco A., Kovářík J., Mengel F., Romero J.G. Natural disasters and indicators of social cohesion. PLoS One. 2017;12 doi: 10.1371/journal.pone.0176885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cassar A., Healy A., Von Kessler C. Trust, risk, and time preferences after a natural disaster: experimental evidence from Thailand. World Dev. 2017;94:90–105. [Google Scholar]
- Chu D.K., Akl E.A., Duda S., Solo K., Yaacoub S., Schünemann H.J., et al. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet. 2020;395:1973–1987. doi: 10.1016/S0140-6736(20)31142-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornwell B. Good health and the bridging of structural holes. Soc. Network. 2009;31:92–103. doi: 10.1016/j.socnet.2008.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Bruin W.B., Bennett D. Relationships between initial COVID-19 risk perceptions and protective health behaviors: a national survey. Am. J. Prev. Med. 2020;59:157–167. doi: 10.1016/j.amepre.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Wit J.R., Lisciandra C. Measuring norms using social survey data. Econ. Philos. 2020:1–34. [Google Scholar]
- Dehning J., Zierenberg J., Spitzner F.P., Wibral M., Neto J.P., Wilczek M., et al. Inferring change points in the spread of COVID-19 reveals the effectiveness of interventions. Science. 2020;369 doi: 10.1126/science.abb9789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diekmann A. Emergence of and compliance with new social norms. Z. Soziol.: ZfS. 2020;49:236–248. [Google Scholar]
- Dussaillant F., Guzmán E. Trust via disasters: the case of Chile's 2010 earthquake. Disasters. 2014;38:808–832. doi: 10.1111/disa.12077. [DOI] [PubMed] [Google Scholar]
- ECDC 2021. https://www.ecdc.europa.eu/en/covid-19/situation-updates/weekly-maps-coordinated-restriction-free-movement
- Giordano G.N., Lindström M. Trust and health: testing the reverse causality hypothesis. J. Epidemiol. Community Health. 2016;70:10–16. doi: 10.1136/jech-2015-205822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glanville J.L., Andersson M.A., Paxton P. Do social connections create trust? An examination using new longitudinal data. Soc. Forces. 2013;92:545–562. [Google Scholar]
- Helliwell J.F., Putnam R.D. The social context of well–being. Phil. Trans. Roy. Soc. Lond. B Biol. Sci. 2004;359:1435–1446. doi: 10.1098/rstb.2004.1522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horne C., Mollborn S. Norms: an integrated framework. Annu. Rev. Sociol. 2020;46 [Google Scholar]
- Hout M., Hastings O.P. Reliability of the core items in the General Social Survey: estimates from the three-wave panels, 2006–2014. Sociol. Sci. 2016;3:971–1002. [Google Scholar]
- Jen M.H., Sund E.R., Johnston R., Jones K. Trustful societies, trustful individuals, and health: an analysis of self-rated health and social trust using the World Value Survey. Health Place. 2010;16:1022–1029. doi: 10.1016/j.healthplace.2010.06.008. [DOI] [PubMed] [Google Scholar]
- Kang S.H., Skidmore M. The effects of natural disasters on social trust: evidence from South Korea. Sustainability. 2018;10:2973. [Google Scholar]
- Kim D., Subramanian S.V., Kawachi I. Springer; 2008. Social Capital and Physical Health. Social Capital and Health; pp. 139–190. [Google Scholar]
- Lo Iacono S., Quaranta M. Contextual economic conditions, institutions and social trust: trends and cross-national differences in Europe, 2002–2017. Polis. 2019;33:185–214. [Google Scholar]
- Lundmark S., Gilljam M., Dahlberg S. Measuring generalized trust: an examination of question wording and the number of scale points. Publ. Opin. Q. 2016;80:26–43. doi: 10.1093/poq/nfv042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nannestad P. What have we learned about generalized trust, if anything? Annu. Rev. Polit. Sci. 2008;11:413–436. [Google Scholar]
- Posner E.A. 2000. Law and Social Norms: the Case of Tax Compliance; pp. 1781–1819. Virginia Law Review. [Google Scholar]
- Putnam R.D. Simon and Schuster; 2000. Bowling Alone: the Collapse and Revival of American Community. [Google Scholar]
- Rauhut H. Beliefs about lying and spreading of dishonesty: undetected lies and their constructive and destructive social dynamics in dice experiments. PLoS One. 2013;8 doi: 10.1371/journal.pone.0077878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riumallo-Herl C.J., Kawachi I., Avendano M. Social capital, mental health and biomarkers in Chile: assessing the effects of social capital in a middle-income country. Soc. Sci. Med. 2014;105:47–58. doi: 10.1016/j.socscimed.2013.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- RIVM 2021. https://www.rivm.nl/en/novel-coronavirus-covid-19/risk-groups
- Rodgers J., Valuev A.V., Hswen Y., Subramanian S. Social capital and physical health: an updated review of the literature for 2007–2018. Soc. Sci. Med. 2019;236 doi: 10.1016/j.socscimed.2019.112360. [DOI] [PubMed] [Google Scholar]
- Scherpenzeel A., Das J.W.M. In: Social and Behavioral Research and the Internet: Advances in Applied Methods and Research Strategies. Das J.W.M., Ester P., Kaczmirek L., editors. Taylor & Francis; Boca Raton: 2010. ‘True’ longitudinal and probability-based internet panels: evidence from The Netherlands; pp. 77–103. [Google Scholar]
- Toya H., Skidmore M. Do natural disasters enhance societal trust? Kyklos. 2014;67:255–279. [Google Scholar]
- Uslaner E.M. Cambridge University Press; 2002. The Moral Foundations of Trust. [Google Scholar]
- Van Bavel J.J., Baicker K., Boggio P.S., Capraro V., Cichocka A., Cikara M., et al. Using social and behavioural science to support COVID-19 pandemic response. Nat. Hum. Behav. 2020;4:460–471. doi: 10.1038/s41562-020-0884-z. [DOI] [PubMed] [Google Scholar]
- Wu Y.-H., Moore S., Dube L. Social capital and obesity among adults: longitudinal findings from the Montreal neighborhood networks and healthy aging panel. Prev. Med. 2018;111:366–370. doi: 10.1016/j.ypmed.2017.11.028. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.